Abstract
Background
Emphysematous pyelonephritis (EPN) is a potentially life-threatening disease with Escherichia coli (E. coli) being the most common aetiology. Infection can involve the renal parenchyma, collecting system and perinephric tissues, and is commonly encountered in patients with uncontrolled diabetes mellitus. EPN complicated by suppurative thrombophlebitis of the inferior vena cava is a rare occurrence. Our case had thrombosis of the right common iliac vein as well, which is first of its kind reported with EPN.
Case presentation
We describe a case of a 59-year-old male patient, with uncontrolled diabetes mellitus, who presented to the emergency department with a history of high-grade fever and left loin pain. Clinico-laboratory findings were diagnostic for diabetes mellitus, complicated by upper urinary tract infection with sepsis. A preliminary ultrasound of the abdomen was indicative of left hydronephrosis with features of emphysematous pyelonephritis. Abdominal computed tomography (CT) was done to ascertain the cause of hydronephrosis. Left ureteric calculus complicated by emphysematous pyelonephritis (type 3a) with intraluminal air in the left renal vein and inferior vena cava (IVC). Culture grew E. coli. Patient was started on insulin and intravenous (IV) antibiotics, and bilateral DJ stenting was done. Patient was symptomatically better and was discharged. A month later, he was readmitted with relapse of symptoms; repeat CT showed left perinephric abscess, with left renal vein, inferior vena cava and right common iliac vein thrombosis. Repeat culture grew E. coli, stent was replaced, and subsequently he underwent ultrasound-guided aspiration for left perinephric abscess. Haemodialysis along with IV antibiotics and anticoagulant therapy was started.
Conclusion
Suppurative thrombophlebitis of the inferior vena cava in association with EPN is rare; however, the same is associated with higher morbidity and mortality. Prompt diagnosis, drainage procedure, antibiotics coupled with anticoagulants are the mainstay of treatment for deep venous thrombophlebitis.
Similar content being viewed by others
Background
EPN complicated by suppurative thrombophlebitis of the inferior vena cava is a rare occurrence. Suppurative thrombophlebitis refers to the presence of venous thrombosis in the setting of infection, and pathologically there is venous thrombosis associated with inflammation and suppuration in the venous wall [1]. It is similar to Lemierre’s syndrome, and its occurrence in other clinical scenario, such as in EPN, has been considered as a variant presentation. While catheter-associated infections are commonly encountered, occurrence in the setting of the sepsis is rare [2].
EPN is commonly seen in uncontrolled diabetes mellitus patients with higher incidence in females. Obstructive uropathy is also an independent risk factor. Our patient had high blood sugar levels and also left obstructive uropathy secondary to a proximal ureteric calculus. A month later when he was readmitted, he had thrombosis in his left renal vein, IVC and right common iliac veins.
Case presentation
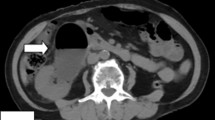
A 59-year-old male patient presented to clinic with left lumbar and iliac fossa pain, fever and increased frequency of micturition. He was a known type 2 diabetic, on medication. At presentation, the initial blood work-up revealed a random blood sugar—400 mg/dl, elevated total leukocyte counts (18,000/mm), urea (120 mg/dl) and creatinine (5.4 mg/dl). Urine microscopy was indicative of urinary tract infection with urine culture growth of E. coli (> 100,000 CFU/ml). In view of loin pain, an ultrasound of the abdomen was done. Bulky left kidney with mild hydronephrosis, and hypoechoic cortex with echogenic foci casting dirty shadows in the pelvicalyceal system were noted, indicative of possible emphysematous pyelonephritis. Patient underwent a non-contrast abdominal CT. Bulky left kidney with mild hydroureteronephrosis (HUN) secondary to 5-mm proximal ureteric calculus was noted. Locules of air in the left renal parenchyma, perinephric space, collecting system, left renal vein as well as within IVC were noted, which were signs of complicated emphysematous pyelonephritis, type 3a according to Huang-Tseng CT classification system (Fig. 1A, B). The patient underwent bilateral double J (DJ) stenting, followed by haemodialysis. He was started on insulin for glycaemic control. For three weeks, intravenous antibiotics (meropenem, ciplox and metronidazole) were administered. He improved clinically, became haemodynamically stable, and was afebrile; hence, he was discharged with instructions to take oral antibiotics for another two weeks.
A Coronal non-contrast CT section of abdomen showing mildly dilated left ureter filled with air and a 5-mm proximal ureteric calculus (arrow). Left perinephric fat stranding seen. Air is seen in left renal parenchyma and left renal vein. B Minimum intensity projection image showing air in the left renal vein, IVC, left kidney and in left perinephric space
A month later he again presented to the emergency department with complaints of fever and epigastric pain. Blood picture showed elevated leukocyte count of 22,000/mm and D-dimer of 7.5 mg/L FEU. His blood sugar levels, urea and creatinine were significantly elevated. He was taken for haemodialysis, and a contrast-enhanced CT abdomen study was done for reassessment. It showed left pyelonephritis with perinephric emphysematous collection of about 30 cc (Fig. 2). Suppurative thrombosis of the left renal vein along with segmental partial thrombosis of IVC at and below the level of the renal vein was seen; speck of air was noted within the IVC thrombus (Fig. 3). There was thrombosis of the right common iliac vein as well. The right common femoral vein and rest of the veins were normal (Fig. 4). Chest X-ray, ECG and echocardiogram were normal. Patient was admitted to the intensive care unit; low molecular weight heparin and IV antibiotics were started. Ultrasound-guided aspiration of perinephric collection was done and was sent for culture and sensitivity; significant E. coli growth was reported. Patient recovered with medical management and was discharged after 4 weeks.
Discussion
EPN is a rare urologic emergency characterized by an acute necrotizing parenchymal and perirenal infection caused by gas-forming organisms. Reported cases are more common in females, with female-to-male ratio of 5.9:1, and left kidney has higher predilection compared to right [3]. Up to 95% of the cases with EPN have underlying uncontrolled diabetes mellitus [4]. The risk of developing EPN secondary to a urinary tract obstruction is about 25–40% [5]. E. coli is the most common causative pathogen in about 70% of the reported cases [6], others being Klebsiella pneumonia, Proteus mirabilis and Pseudomonas aeruginosa.
As to the aetiopathogenesis of EPN, it has been postulated that high tissue glucose levels in diabetic patients provide the substrate for microorganisms such as Escherichia coli, which are able to produce gas by fermenting the sugar [7]. Untreated cases of EPN may be fatal with mortality rates ranging from 13 to 25%. Medical treatment alone may result in uncontrolled sepsis, necessitating surgical intervention. EPN can be complicated by abscess formation; renal and perinephric, sepsis and renal failure are other complications. The incidence of suppurative thrombophlebitis of renal vein or IVC thrombus in EPN is rare [8].Only four reported cases of EPN with venous thrombosis were found on literature search, all were females and renal vein was most commonly involved [9].
CT is the preferred modality of radiological investigation in a suspected case of EPN, as it is highly sensitive in identifying air and in defining the extent of disease [9, 10]. Huang JJ & Tseng CC came up with a clinicoradiological classification system based on CT findings, which guided in the management of emphysematous pyelonephritis. They classified it into four grades, primarily based on the air distribution, higher the grade the more severe was the disease and higher was the mortality. In Class 1, the gas is present in the collecting system; in Class 2, the gas is present in the renal parenchyma, without extension to the extrarenal area; in Class 3A, gas or abscess is present in the perinephric space; in Class 3B, gas or abscess is present in the pararenal space; and in Class 4 air is seen bilaterally or disease is seen in the solitary kidney [3]. They concluded that for localized EPN (class 1 or 2), percutaneous drainage (PCD) and/or relief of the urinary tract obstruction (if it exists) combined with antibiotic treatment had better outcome. For extensive EPN (class 3 or 4), PCD combined with antibiotic treatment may be attempted. However, nephrectomy can provide the best management outcome and should be promptly attempted for extensive EPN with a fulminant course or for cases with an unsuccessful PCD [3].
Perkins et al. and Jeyaraman et al. both reported the cases of EPN complicated by suppurative thrombophlebitis of the renal vein/IVC, with the former also showing involvement of the pulmonary artery [10, 11]. Dong et al. described a case of a 52-year-old diabetic woman with unilateral EPN with air bubbles in the uterine veins secondary to infection by E. coli. Cases that have been documented so far in the literature have all been treated conservatively with supportive measures, broad-spectrum antibiotics, percutaneous drainage therapy, and/or open drainage [9]. Outcomes in these cases have been good, except for the patient with involvement of pulmonary artery who succumbed.
At present, conservative approach with percutaneous drainage and antibiotics is the preferred initial management compared with open drainage and/or emergency nephrectomy [12]. In a subset of patients with thrombocytopenia, > 50% renal parenchymal destruction, altered mental status and renal failure as risk factors early surgical intervention substantially reduces morbidity and mortality [13]. Nephrectomy should be reserved as the last resort for those who fail to respond to conservative therapy.
Conclusion
Complicated EPN with suppurative thrombophlebitis involving the deep venous system is rare, and co-occurrence of air in the venous system followed by thrombosis in the renal vein, IVC and common iliac vein has not been reported till date. This case illustrates that patients with EPN, post-DJ stent, despite good antibiotic therapy and clinical recovery, could nevertheless experience an infection relapse a month later. Therefore, until they fully recover, these patients require continuous supervision with frequent follow-up corroborated by laboratory results. In our patient, conservative management alone was sufficient to salvage the kidneys.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to privacy of the study participant.
Abbreviations
- EPN:
-
Emphysematous pyelonephritis
- E. coli :
-
Escherichia coli
- CT:
-
Computed tomography
- IVC:
-
Inferior vena cava
- HUN:
-
Hydroureteronephrosis
- DJ:
-
Double J
- PCD:
-
Percutaneous drainage
References
Levi M, Schultz M, van der Poll T (2013) Sepsis and thrombosis. SeminThrombHemost 39:559–566
Lipe DN, Foris LA, King KC. Septic Thrombophlebitis. [Updated 2023 Feb 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430731/
Huang JJ, Tseng CC (2000) Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 160(6):797–805
Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II (2007) Risk factors for mortality in patients with emphysematous pyelonephritis: a meta-analysis. J Urol 178:880–885
Michaeli J, Mogle S, Perlberg S, Heiman S, Caine M (1984) Emphysematous pyelonephritis. J Urol 131:203–207
Khaira A, Gupta A, Rana DS, Gupta A, Bhalla A, Khullar D (2009) Retrospective analysis of clinical profile, prognostic factors and outcomes of 19 patients of emphysematous pyelonephritis. Int Urol Nephrol 41:959–966
Tang HJ, Li C, Yen MY et al (2001) Clinical characteristics of emphysematous pyelonephritis. J MicrobiolImmunol Infect 34:125–130
Ubee SS, McGlynn L, Fordham M (2011) Emphysematous pyelonephritis. BJU Int 107(9):1474–1478
Dong X, You S, Zhang H, Wang D, Pan W, Zhang B, Huang S, Li X, Pang J, Ji W (2022) Venous gas caused by emphysematous pyelonephritis: a case report and review of literature. BMC Urol 22(1):154
Jeyaraman R, Karunamoorthy R, Ahmed-Marzook S (2013) Emphysematous pyelonephritis with IVC thrombus in new onset diabetes mellitus. Indian J Urol 29:348–350
Perkins TA, Rogman A, Ankem MK (2020) Emphysematous pyelonephritis with air bubble in the inferior vena cava. Afr J Urol 26(1):1–3
Pontin AR, Barnes RD (2009) Current management of emphysematous pyelonephritis. Nat Rev Urol 6:272–279
Kapoor R, Muruganandham K, Gulia AK et al (2010) Predictive factors for mortality and need for nephrectomy in patients with emphysematous pyelonephritis. BJU Int 105:986–989
Acknowledgements
I sincerely thank our esteemed institution JSS Academy of Higher Education and Research, Mysore, for encouraging and providing support in all our endeavours. I also take this opportunity to express my gratitude to all the faculty, postgraduates, technical and supporting staff of Department of Radiology.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Dr SKD did study conception and design, and supervision of the project. Dr AC and Dr SPS done study conception and design, and draft manuscript preparation. Dr BG and Dr RH contributed to draft manuscript preparation and supervision of the project. Dr VP was involved in draft manuscript preparation. All authors discussed the case report and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was waived off by the Ethics committee of JSS Academy of Higher Education and Research, Mysuru, India, for single patient case report, and written informed consent for publication was obtained from the patient. Only anonymized data and images were used.
Consent for publication
Written informed consent was obtained from the patient for the publication and only anonymized data and images were used.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chandrappa, A., Das, S.K., Shetty, S.P. et al. Lemierre’s syndrome variant with inferior vena cava and right common iliac vein thrombosis secondary to emphysematous pyelonephritis. Egypt J Radiol Nucl Med 54, 129 (2023). https://doi.org/10.1186/s43055-023-01075-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01075-0