Abstract
Background
Emphysematous pyelonephritis (EPN) with gas in the inferior vena cava (IVC) is a rare presentation and to our knowledge, this is the first case report in the urologic literature.
Case presentation
A 35-Year-old obese diabetic Hispanic female presented to the emergency room with a clinical picture of septic shock. Prompt computerized tomography scan revealed EPN with gas throughout the right renal parenchyma and extending to the right renal vein, IVC, and pulmonary artery. She died before surgical intervention
Conclusion
This case demonstrates that patients presenting with severe EPN have a high mortality risk and providers should acknowledge that septic shock, endogenous air emboli, or a combination of both could result in cardiovascular collapse and sudden death.
Similar content being viewed by others
1 Background
Emphysematous pyelonephritis (EPN) is a rare but severe, fulminant infection of the renal parenchyma and the surrounding tissues that most often occurs in patients with uncontrolled diabetes mellitus and/or debilitated state. The infection usually caused by gas forming organisms (Escherichia coli and K. pneumoniae) with air in the collecting system, renal parenchyma, and/or perirenal structures [1]. The disease process can be lethal if not diagnosed and managed promptly as mortality rates up to 40% have been reported [2]. Initial management includes fluid resuscitation of the patient, broad spectrum antibiotics. Multiple percutaneous nephrostomies or urgent nephrectomy may be needed for successful management of severe EPN [3,4,5]. We describe a case of severe EPN with air bubble in the IVC where emergent nephrectomy was planned.
2 Case presentation
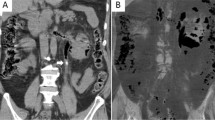
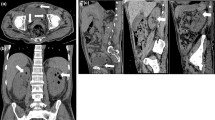
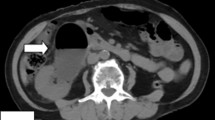
A 35-year-old obese Hispanic female with past medical history of poorly controlled insulin-dependent diabetes mellitus (Hb A1c: 11.3%) presented to emergency room with change in mental status and frequent vomiting. She was febrile and hemodynamically unstable with clinical picture of septic shock. She coded in the emergency room requiring five minutes of cardiopulmonary resuscitation and endotracheal intubation. Prompt CT scan revealed EPN with air bubbles extending to the renal vein, inferior vena cava (IVC), and pulmonary artery (Figs. 1, 2). The patient was subsequently admitted to the intensive care unit, and a urology consultation was sought for further evaluation and management. Subsequently, she was transported to operating for an emergent nephrectomy. On the operating table, she went into cardiac arrest and cardiopulmonary resuscitation was administered according to American Heart Association guidelines. Despite sustained efforts, the patient died after 40 min of commencement of CPR.
3 Discussion
The presented case report describes the unfortunate lethal complication of a patient suffering from an E. coli-induced grade 3 EPN [1, 5] scheduled for an emergency nephrectomy. EPN is a rare but potentially fatal renal infection most prevalent in diabetic, alcoholic, and immuno-compromised patients [1,2,3,4,5,6]. CT scan is the gold standard for diagnosis of EPN and provides valuable information for planning further treatment [1,2,3,4,5,6]. Although controversial, conservative management and renal preservation using percutaneous drainage and high dose antibiotics are considered in mild cases (classification class I–II) [1, 3, 5], nephrectomy is the treatment of choice in severe cases (class III–IV) with a mortality rate of 20% compared to 80% in medically managed patients [5]. Two clinical scenarios may explain the quick hemodynamic deterioration and fatal outcome despite all efforts. A more likely cause of the patient’s demise was hemodynamic collapse secondary to septic shock. Another contributor may have been air emboli originating from gas in the renal vein and inferior vena cava (IVC), which may have mobilized during transport causing acute right heart failure. Preclinical studies suggest that large quantities of gas (over 50 ml) are required to cause abrupt acute cor pulmonale, asystole, or both [7, 8]. The results of the CT scan reveal air in the vascular system and large quantities of air within the kidney. An estimation by planimetry of the CT scan acquired hours before the transport suggests an air volume of approximately 177 ml in the kidney and renal collecting ducts and approximately 4 ml in the IVC. Air emboli may occur during orthopedic procedures [9] vascular procedures, neurosurgical interventions [10], or laparoscopic surgeries [11, 12]. In contrast, our case of EPN might present an unreported incident of an endogenously developed air embolus from the kidney. Lastly, a combination of severe septic shock and multiple air emboli may have caused the hemodynamic collapse. However, only an autopsy would bring light to the actual reason of death. Unfortunately, autopsy was declined by the family. Therefore, the cause of death remains speculative.
4 Conclusion
This case demonstrates that patients presenting with severe EPN have a high mortality risk and providers should acknowledge that septic shock, endogenous air emboli mobilized from the kidney, or a combination of both can result in cardiovascular collapse. Hemodynamic optimization and concise cardiac monitoring is of utmost importance to increase the chance of survival during the perioperative period.
Availability of data and materials
Upon acceptance the authors agree to the copyright rules of the African Journal of Urology Case Reports.
Abbreviations
- EPN:
-
Emphysematous pyelonephritis
- IVC:
-
Inferior vena cava
- CT:
-
Computerized tomography scan
References
Huang JJ, Tseng CC (2000) Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 160(6):797–805
Wang JM, Lim HK, Pang KK (2007) Emphysematous pyelonephritis. Scand J Urol Nephrol 41(3):223–229
Lin WR, Chen M, Hsu JM, Wang CH (2014) Emphysematous pyelonephritis: patient characteristics and management approach. Urol Int 93(1):29–33
Pontin AR, Barnes RD (2009) Current management of emphysematous pyelonephritis. Nat Rev Urol 6(5):272–279
Ubee SS, McGlynn L, Fordham M (2011) Emphysematous pyelonephritis. BJU Int 107(9):1474–1478
Wan YL, Lee TY, Bullard MJ, Tsai CC (1996) Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome. Radiology 198(2):433–438
Kostadima E, Zakynthinos E (2007) Pulmonary embolism: pathophysiology, diagnosis, treatment. Hell J Cardiol 48(2):94–107
Goldhaber SZ, Elliott CG (2003) Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. Circulation 108(22):2726–2729
Spiess BD, Sloan MS, McCarthy RJ, Lubenow TR, Tuman KJ, Matz SD et al (1988) The incidence of venous air embolism during total hip arthroplasty. J Clin Anesth 1(1):25–30
Tobias JD, Johnson JO, Jimenez DF, Barone CM, McBride DS Jr (2001) Venous air embolism during endoscopic strip craniectomy for repair of craniosynostosis in infants. Anesthesiology 95(2):340–342
Otsuka Y, Katagiri T, Ishii J, Maeda T, Kubota Y, Tamura A et al (2013) Gas embolism in laparoscopic hepatectomy: what is the optimal pneumoperitoneal pressure for laparoscopic major hepatectomy? J Hepatobiliary Pancreat Sci 20(2):137–140
Sood J (2014) Advancing frontiers in anaesthesiology with laparoscopy. World J Gastroenterol 20(39):14308–14314
Acknowledgements
None.
Funding
There is no funding for this report.
Author information
Authors and Affiliations
Contributions
All the authors (TAP, AR, and MKA) made substantial contributions to the conception of the idea, preparing the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Verbal consent was obtained from the husband of the patient to publish the case report as the patient passed away.
Consent for publication
All authors consent for publication if accepted. Verbal Consent for publication was obtained from the next of kin (husband) as the subject died. Written informed consent was not obtained as the family moved out of town and no forwarding address available.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Perkins, T.A., Rogman, A. & Ankem, M.K. Emphysematous pyelonephritis with air bubble in the inferior vena cava. Afr J Urol 26, 69 (2020). https://doi.org/10.1186/s12301-020-00081-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-020-00081-2