Abstract
In tissue engineering, bioactive materials play an important role, providing structural support, cell regulation and establishing a suitable microenvironment to promote tissue regeneration. As the main component of extracellular matrix, collagen is an important natural bioactive material and it has been widely used in scientific research and clinical applications. Collagen is available from a wide range of animal origin, it can be produced by synthesis or through recombinant protein production systems. The use of pure collagen has inherent disadvantages in terms of physico-chemical properties. For this reason, a processed collagen in different ways can better match the specific requirements as biomaterial for tissue repair. Here, collagen may be used in bone/cartilage regeneration, skin regeneration, cardiovascular repair and other fields, by following different processing methods, including cross-linked collagen, complex, structured collagen, mineralized collagen, carrier and other forms, promoting the development of tissue engineering. This review summarizes a wide range of applications of collagen-based biomaterials and their recent progress in several tissue regeneration fields. Furthermore, the application prospect of bioactive materials based on collagen was outlooked, aiming at inspiring more new progress and advancements in tissue engineering research.
Graphical Abstract

Similar content being viewed by others
1 Introduction
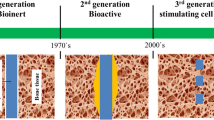
In recent years, bioactive materials have played a pivotal role in tissue engineering, which generally provides supporting structures to guide and sustain cells through the use of bioactive ingredients and therapeutic molecules [1]. Bioactive materials should have appropriate mechanical properties, good biocompatibility, and a degradation rate well-matched with the healing process of the body to help restoring the inherent function of tissues [2]. Bioactive materials used to build microstructures that resemble natural tissues [3] can guide morphogenesis, preserve homeostasis and provide tissue healing cues for endogenous/exogenous cells [4], thus creating a microenvironment suitable for cell growth and development. As a natural bioactive material, the extracellular matrix (ECM) plays a significant role in tissue remodeling [5] by providing biological cues that can induce the stimulation of cellular responses, such as cell adhesion, migration and proliferation [6]. Therefore, natural bioactive substrates derived from ECM components can prove to be potential tissue regeneration materials.
As the most abundant bioactive fibrous protein in the ECM, collagen effectively modulates the biological behavior of cells to stimulate native tissue repair [7, 8]. Collagen has a triple helical structure of peptide chains and regulates intracellular signaling and cell activities including morphogenesis, ECM deposition, and tissue remodeling [9, 10] through multiple cell-material interaction pathways [11]. Many cell surface receptors that bind to collagen have been characterized. For instance, cell surface integrins bind to the peptide sequence of collagen and activate the extracellular signal-regulated kinase (ERK) 1/2 mitogen-activated protein kinase (MAPK) signal transduction pathway, promoting cell adhesion, survival, and migration [1]. The amino acid repeats of collagen are specific to immunoglobulin (Ig)-like receptors and G6B-B receptors associated with leukocytes and inhibit immune cell differentiation [12]. Osteoclast associated receptor (OSCAR), an immune receptor specific to the structure of the triple helix peptide, enables the activated T nuclear factor (NFAT) signal transduction, regulates the development of osteoclast (bone resorptive cells), and targets abnormal immune responses [13, 14].
Based on these attributes, collagen has been widely used in the repair of various tissue defects. For instance, mineralized collagen or structured collagen scaffolds have been implanted to induce or guide bone regeneration [15, 16]. Cross-linked collagen, collagen complex, and lyophilized sponge scaffolds have shown promising results in the regeneration of cartilage defects [17, 18]. The use of collagen membrane and drug-loaded collagen scaffolds helps regenerating skin and hair follicles [19]. Collagen-based artificial vascular scaffolds or hydrogels also display great potential in promoting cardiovascular regeneration [20]. In addition, collagen-based bioactive materials also have good application perspectives in gynecology, reproductive medicine [8, 21], plastic repair [22, 23], cornea regeneration [24,25,26] among others. Collagen scaffolds provide a bionic microenvironment to maintain the structural integrity of regenerated tissues [27], which has an important influence on the cell behavior and tissue repair. As a result, collagen-based biomaterials may be considered as potential candidates for both basic research and clinical applications.
2 Basic structure and types of collagen
2.1 Sources of collagen
Collagen can be derived from animal skin, Achilles tendon, rat-tail tendon, fish skin, recombinant protein production system, synthetic collagen-like peptides, etc., with good biocompatibility and biodegradation properties. Collagen derived from the skin and Achilles tendon of pigs, cattle, sheep and other animals has been widely used in different studies, owing to the low cost and high yield [28]. However, animal-derived collagen is a highly cross-linked biomaterial with limited solubility [29], large batch to batch variation, immunogenicity, and risk of pathogen transmission [30] which has stimulated the investigation of marine collagen, human recombinant collagens and collagen-like synthetic peptides. The fish skin contains a large amount of collagen and has a low manufacturing cost [31], meanwhile leads to a better approach for waste utilization and for a cleaner marine environmental [32]. For this reason, marine collagen has attracted great scientific and industrial interest [33] but there are limited studies in tissue engineering [34, 35]. Recombinant collagen are candidates for a variety of medical applications [36] and synthetic collagen-like peptides [37] that mimic the properties of collagen can overcome the batch variability, potential immunogenicity [38] and viruses [39] of animal-derived collagen. However, for recombinant humanized protein, enormous efforts still need to be made to achieve successful translation from bench to clinic [40], considering high cost [41], low yield [42] and susceptibility to enzymatic degradation [43] as compared to animal-derived collagen. The different collagen sources and their characteristics are summarized in Table 1.
2.2 Types of collagens
The different types of collagens are named according to the date of discovery [44]. They are mainly classified into different subfamilies based on their structure and function as shown in Table 2. The subfamilies include fibrillar collagens, fibril associated collagens with interrupted triple helices, beaded filament-forming collagen, basement membrane collagens, transmembrane collagens and other collagen with unique functions [4].
The fibrillar collagens constitute about 90% of the total collagen and represent the most abundant and widespread family of collagens including type I, type II, type III, type V and type XI collagen. These collagens are characterized by their ability to assemble into highly oriented supramolecular aggregates with characteristic superstructures. Type I and Type V collagen fibers contribute to the structural skeleton of bone, while type II and XI collagen mainly participate in the fibrous matrix of articular cartilage. Type III collagen is widely distributed in collagen I containing tissues with the exception of bone [45]. Recombinant human collagen type III is also used as three-dimensional (3D) printing ink to produce thin layers crosslinked by EDC:NHS crosslinking for corneal tissue engineering [46]. Type V collagen typically forms heterofibrils with types I and III collagens and contributes to the organic bone matrix, corneal stroma and the interstitial matrix of muscles, liver, lungs, and placenta [47]. Type XI collagen co-distributes with type II collagen in the articular cartilage.
Different types of collagens also affect or cause genetic diseases in humans. For example, a mutation in the exon of type II collagen gene COL2A1 leads to a serine replacement of glycine, resulting in avascular necrosis of the femoral head [48]. Besides, collagen VI is particularly important in skeletal muscle [49]. Collagen VI-related congenital muscular dystrophies is caused by mutations in any of the three genes coding for collagen type VI (COL6A1, COL6A2, COL6A3) [50].
2.3 Structure and function of collagen
As shown in Fig. 1a, collagen is made up of three protein chains (α chains), which are wound together to form a characteristic triple helix. Each alpha (α) chain contains about 1000 amino acids with a molecular weight of about 100 kDa, and is composed of a specific set of amino acids repeating sequence (Gly-Xaa-Yaa)n [8], where the glycine residues are in every third position. Since glycine is the smallest amino acid with only a hydrogen atom as its side chain, it becomes a part of the center of the super spirochetes without any steric hindrance. This brings the three helical α chains tightly together to form the final super spirochetes with hydrophobic cores. The other two amino acids in Xaa and Yaa positions are often proline and hydroxyproline.
Structure of collagen. a The four-dimensional structure of collagen fibers. Reproduced with permission from[2]; b1, b2 Molecular structure and synthesis of collagen I. Following intracellular post translational modifications, three polypeptide chains assemble into procollagen (b1), which is then exocytosed into the extracellular space. Collagen I tropocollagen is 300 nm (corresponding to 4.4 D) in length and 1.5 nm in diameter (b2). Reproduced with permission from [4]
Collagen is cleaved from precursor molecule (procollagen) as shown in Fig. 1b [51,52,53]. A key regulatory step in collagen assembly is the C-terminal proteolytic processing of soluble procollagen precursors [54]. Procollagen N-proteinase and procollagen C-proteinase are essential for procollagen processing. The C-proteinase specifically cleaves native and denatured types I, II and III procollagens [55]. The N-proteinase has the unusual property of cleaving the N-propeptides from type I and type II procollagens if the proteins are in a native conformation, but not if the proteins are partially unfolded so that the N-telopeptides are no longer in a hair-pin configuration.
Collagen maintains the structural integrity of tissues and organs and acts as the main functional skeleton in connective tissues, especially bone and cartilage [56]. In addition, collagen interacts with cells mediated by its specific peptide repeat unit and triple helix structure, and regulates their adhesion, proliferation, differentiation, and signal response [44] by binding to specific receptors such as integrins, glycoproteins, and proteoglycan receptors [57, 58]. Collagen further contributes to the local storage and delivery of loaded and endogenous growth factors and cytokines, providing a suitable microenvironment for exogenous/endogenous cells involved in organ development, wound healing, and tissue repair [59].
3 Development of collagen-based biomaterials
Natural collagen has characteristics for befittingly matching with tissue. However, due to the destruction of the natural assembly structure and cross-linking of collagen in the process of extraction, purification and synthesis [60], the mechanical properties and stability of extracted collagen are lower than its natural counterpart, resulting in its low durability and limited potentiality in biotechnology applications [61]. Therefore, a variety of different strategies have been pursued to reconstruct and enhance the structure and properties of collagen.
3.1 Cross-linked collagen
Considering that the natural cross-linking pathway of collagen does not occur in vitro [62], exogenous cross-linking is introduced to optimize collagen-based materials. The introduction of additional cross-links prevents collagen molecules from sliding against each other under stress [63], thereby increasing the mechanical strength of collagen fibers. Further, the potential modification of collagen is limited by its structural complexity and biocompatibility requirements [64]. Common cross-linking methods are presented in Fig. 2. However, there is currently no standardized cross-linking methods to prepare a strong, biocompatible collagen matrix.
Cross-linked collagen. a Localization of modified amino acids in the 3D-structure of COL BS modified biopolymers using the I-TASSER server. Reproduced with permission from [65]; b A new strategy of dialdehyde starch-based nanoparticles were developed to crosslink collagen. Reproduced with permission from [66]; c Stepwise illustration of the chemical reactions in the development of the effectivity of double-crosslinking with both EDC and GTA. Reproduced with permission from [67]; d Topographical, lateral amplitude of d1 non-cross-linked d2 cross-linked with EDC-NHS. Reproduced with permission from [68]; e collagen model peptides cross-linked by oxime bonds between 4-aminooxyproline and 4-oxoacetamidoproline. Reproduced with permission from [69]
3.1.1 Physical cross-linking of collagen
Physical cross-linking using ionizing radiation, ultraviolet (UV) light treatment, dehydrogenation heat treatment (DHT), or photo-oxidation in generally considered to be a simple and safe method to prepare a cross-linked collagen matrix [61]. For example, Pien et al. described the introduction of modified photo-crosslinkable groups into the 3D structure of proteins (Fig. 2a). Proteomic analysis was used to quantify photo-crosslinking through the identification and localization of modified peptides, which is critical for repeatability and regulation of biomaterials [65]. Wang et al. used UV radiation and DHT to improve the properties of collagen casings (a form of collagen film). UV treatment, DHT, and their combination significantly increased the tensile strength and decreased the elongation at break of collagen casings, among which DHT had a significant effect [70]. In summary, physical cross-linking successfully enables the development of biomaterials with better mechanical properties and excellent biocompatibility without the use of exogenous toxic chemicals [45]. However, physical cross-linking are often associated with collagen denaturation (especially the DHT treatment), imposing the need for introduction of chemical crosslinkers [30].
3.1.2 Chemical cross-linking of collagen
The most widely used chemical crosslinking agents are aldehydes. Glutaraldehyde (GTA) has been shown to extensively stabilize collagen materials because of its self-polymerization capacity but still controversial due to its toxicity [71]. For this reason, research interests are focusing on alternative strategies. Xu et al. [66] developed dialdehyde cross-linked collagen with starch-based nanoparticles as a new strategy. Dialdehyde cholesterol modified starch self-assembled into nanoparticles and cross-linked with collagen to fabricate collagen hydrogels as shown in Fig. 2b. Islam et al. [67] evaluated the effect of double-crosslinking with both EDC and GTA together with the capability of sodium metabisulfite (SM) and sodium borohydride (SB) to neutralize the toxicity and restore biocompatibility after cross-linking, as reported in Fig. 2c. Nair et al. [68] employed 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide/N-hydroxysuccinimide (EDC-NHS) to form structurally and mechanically stable collagen scaffolds and investigated its effect on collagen piezoelectricity. The topography and lateral amplitude was shown in Fig. 2d. Hentzen et al. reported the cross-linking of model collagen peptides by oxime bonds between 4-aminooxyproline and 4-oxoacetamidoproline placed in coplanar Xaa and Yaa positions of neighboring strands (Fig. 2e) [69]. Compared to GTA, these natural cross-linking agents had lower toxicity and better biocompatibility but possessed limitations including storage instability and low degree of cross-linking [71]. For example, naturally-derived chemical crosslinking agents, such as genipin, are also attracting research attention, owing to their interesting pharmacological properties (i.e., anti-inflammatory, anti-angiogenic, anti-cancer, among others) [72].
Click chemistry approach provides new ideas for collagen architectures and assembly behaviors. These conjugate strategies with collagen mimetic peptides as the building blocks present exciting stimuli responsive or spontaneously assembly behavior [73]. Byrne et al. [74] established modular synthesis of end-stapled homo- and hetero-triple helical peptides, generating “clicked” macro-assemblies with enhanced thermal stability. Collagen can also be functionalized by click chemistry to play a greater role in tissue regeneration. Lee et al. [75] studied the chemical coupling of growth factors to collagen using click chemistry and discovered that it had significant effects on epithelial cell attachment and proliferation. Click chemistry-based reaction can connect, more accurately, the various functional groups, so that the cross-linking reaction can proceed in the direction as expected.
3.1.3 Enzyme-induced cross-linking of collagen
Enzyme cross-linking has emerged in recent years because of its excellent specificity and precise reaction kinetics [76]. Perez-Puyana et al. [77] developed a hybrid scaffold made from the mixture of two biopolymers (collagen and chitosan) and compared the effect of GTA as a cross-linking agent with three different cross-linking methods (chemical: genipin; physical: temperature and enzymatic: transglutaminase) to look for a promising candidate to substitute it. Enzymatic cross-linking avoids the disadvantages of physical and chemical cross-linking, but it is expensive.
3.2 Mineralized collagen
Mineralized collagen is an organic–inorganic composite material formed from collagen molecules and nano-calcium phosphate minerals [78]. It is used as a universal template in biomineralization [79]. The inorganic components closely related to collagen are limited to a few minerals: amorphous silica, calcium carbonate polycrystalline, and carbonate apatite [80] and may precipitate within (intrafibrillar mineralization) and between collagen fibrils (interfibrillar/extrafibrillar mineralization) [81]. As bone largely consists of intrafibrillar hydroxyapatite (HAp) crystals, the formation of intrafibrillar HAp in a collagen matrix was investigated [82]. During intrafibrillar mineralization, large contractile forces occur within the collagen regardless of the mineral type, thus giving bone its unusual combination of mechanical properties [83].
Biomineralized collagen composites have the potential to be used as a substitute for current synthetic bone implants by providing biomimetic components that are very similar to natural bone [87]. More effective mineralization methods and detailed mineralization mechanisms are under investigation. Song et al. found that a polyelectrolyte polyacrylic acid (PAA) is capable of caching calcium and hydrogen phosphate ion complexes into chain-like aggregates along the surface of the macromolecule (Fig. 3a) when it is introduced into a supersaturated calcium phosphate (CaP) mineralization medium, as well as concentrating the precursors for more efficacious intrafibrillar mineralization [79]. Zhang et al. [85] analyzed the biological mineralization of natural bone and found a correlation between calcium concentration and collagen production (Fig. 3c). The translocation-associated membrane protein 2 (TRAM2) was identified as an intermediate factor that modulates the activity of calcium-ATPase type 2 in the sarco-/endoplasmic reticulum (SERCA2b) to couple calcium enrichment with collagen biosynthesis, to be involved in bone matrix mineralization. Shao et al. found that citrate molecules adsorbed on collagen fibrils could significantly reduce the interface energy between biological matrix and amorphous calcium phosphate (ACP) precursor (Fig. 3d), enhance their wetting effect during early-stage biomineralization, and successfully promote the formation of HAp fibrils to generate inorganic–organic complexes. This finding demonstrates the importance of interfacial controls in biomineralization [86]. As presented in Fig. 3b, the further study in the design of mineralized collagen should have a satisfactory analog structure and appropriate biological properties for bone regeneration [84].
The mineralized collagen. a Mineralized high–molecular weight polyacrylic acid (HPAA)–cross-linked collagen sponges. Reproduced with permission from [79]; b The natural bone formation process and the bionic strategy of bone repair scaffold. Reproduced with permission from [84]; c Schematic representation of the calcium–collagen coupling. Reproduced with permission from [85]; d Schematic of the functional citrate treatment on the mineralization of collagen fibrils. Reproduced with permission from [86]
3.3 Collagen-based blends
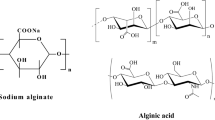
Blends can be prepared based on synthetic and natural polymers as well as two (or more) biopolymers. It is expected that blending two polymers can lead to the development of a new class of materials with improved mechanical properties and biocompatibility when compared with a single component material [29]. Collagen has certain limitations related to its applications in tissue repair, such as strong contraction, weak mechanical properties, and poor cell phenotypic orientation [4]. Therefore, collagen-based blends are expected to prepare complex hydrogels with improved practical performances. To this aim, collagen-based blends have been widely used to study the interaction of cells with their microenvironment and as scaffolds for biomedical and tissue engineering applications [92, 93].
Examples of different collagen-based blends are shown in Fig. 4. For instance, Chen et al. developed an injectable self-crosslinking hyaluronic acid (HA-SH)/type I collagen (Col I) blend hydrogels for in vitro development of an engineered cartilage as present in Fig. 4a [88]. For cornea regeneration, Chen et al. designed a bio-orthogonal hyaluronic acid-collagen hydrogel for sutureless corneal defect repair (Fig. 4b). The results showed improved mechanical properties and excellent cytocompatibility and support for epithelialization in vitro and in vivo [89]. Rafat et al. [90] developed a collagen-based composite hydrogels (Fig. 4c) as implants to restore corneal transparency while serving as a possible reservoir for cells and drugs. Zheng et al. designed a genipin-cross-linked injectable composite collagen hydrogel as shown in Fig. 4d, which was used as a scaffold for incorporating bone marrow-derived mesenchymal stem cells (BMSC) and cadmium selenide quantum dots for cartilage repair [91]. It has been emphasized that collagen plays a significant role in tissue engineering, and thus, numerous products based on this material have been developed so far.
Application of collagen-based blends. a An injectable self-cross-linking HA-SH/Col I blend hydrogels for in vitro construction of engineered cartilage. Reproduced with permission from [88]; b Application of hydrogel for sutureless repair of corneal wounds: (b1) Hyaluronate-collagen hydrogel cross-linked via strain-promoted azide-alkyne cycloaddition (SPAAC); (b2) Sutureless repair of corneal wounds. Reproduced with permission from [89]; c Postoperative neovascularization in a collagen-based composite hydrogel as implants and autograft corneas. Reproduced with permission from [90]; d The fabrication process of collagen–genipin–quantum dot (CGQ) composite hydrogels. Reproduced with permission from [91]
3.4 Structured collagen
Over the past two decades, problems associated with regenerating natural collagen fibers include the inability to achieve sufficient tensile strength and replicate or reproduce the internal fibrillary structure due to the loss of properties of the hierarchies consistent with natural collagen [96]. Modern technology enables to make highly ordered collagen scaffolds or a matrix with a structure similar to the matrix present in living organisms, as shown in Fig. 5 [98].
Modern technology used in structured collagen. a Schematic diagram of the sequential steps involved in the printing process of a new material for tissue regeneration. Reproduced with permission from [94]; b Schematic of electrospinning technique of poly electrospun fibers. Reproduced with permission from [95]; c A block diagram of one-step fabrication of 3D fibrous collagen-based macrostructure with high water uptake capability by coaxial electrospinning. Reproduced with permission from [96]; d Scheme illustration of 3D polymeric grid patterned scaffolds decorated with visible-light photocatalyst as nerve guidance conduits (NGCs) for promoting peripheral neural regeneration. Reproduced with permission from [97]
The ability of the electrospinning to fabricate custom-built nanofibers (Fig. 5b) from collagen-based composites may be the main reason that made it the most applied method to mimic the structure of the collagen in native tissues [96]. However, there are several challenges for collagen electrospinning, such as poor mechanical strength, reduced elasticity, high hydrophilicity of the obtained fibers, and difficulty in solubilizing collagen while preserving its native tertiary structure [95]. Indeed, natural collagen fibers may lose their structural characteristics while processing. For this reason, further modifications are warranted to counter the negative effects of processing [96].
3D printing is one of the most famous additive manufacturing technologies in the field of tissue and organ bio-manufacturing, and the sequential steps involved in the printing process are shown in Fig. 5a [94]. Compared with traditional techniques, 3D printing offers the possibility of creating replicable, customizable and functional structures with precisely controlled composition and microstructure that can effectively promote the regeneration of different tissues [99]. However, due to the low mechanical stability, collagen is typically printed in preformed molds, inside other materials serving as a support or stabilized by additional cross-linking steps after printing [100, 101].
The melt near-field direct writing technology overcomes some of the defects of spinning methods in terms of disorder and control and enables the fabrication of micro/-nanowires with precisely controlled morphology (Fig. 5d) [97]. Further optimizations in the design of structured collagen are required to reproduce the natural organization and biomimetic function and achieve better results in tissue regeneration applications.
3.5 Collagen-based delivery vehicles
Collagen suspensions can be easily prepared and used as delivery vectors for macro-and micro drug molecules. Methods such as supercritical fluid extraction, electrospraying, spray drying, layer-by-layer self-assembly, lyophilization and microemulsification can be used to introduce drugs into delivery systems [102]. Sun et al. [103] developed a recombinant SDF-1α containing collagen-binding domain which could specifically bind to collagen and achieve controlled release of SDF-1α for in situ tendon regeneration. Kanematsu et al. [104] investigated the use of natural and synthetic collagenous matrices as carriers of exogenous growth factors, which could actively promote tissue regeneration. Collagen-based delivery systems also need to possess optimal degradation rate and drug dispersion properties to achieve better effects [105].
4 Applications of collagen-based biomaterials
4.1 Bone regeneration
The excellent mechanical properties of bone come from the orderly embedding of nano mineral crystals into the collagen matrix, thus forming a complex ordered hierarchical structure [106]. The organic matrix of bone mainly comprises collagen fibrils, specifically type I collagen. Therefore, type I collagen is widely used in bone repair as a naturally occurring matrix in the form of hydrogel and scaffold [107]. However, the low mechanical strength and limited osteogenecity of collagen limit its wide application in bone regeneration [15]. Therefore, by adding some bioceramics similar to the inorganic components of natural bone [108], the mechanical properties, porosity, structural stability, osteogenic/osteoinductive features, and other properties of the collagen matrix can be greatly improved [16]. For instance, Kang et al. fabricated graphene oxide (GO)-collagen (GO-COL) scaffold crosslinked by EDC as shown in Fig. 6a for osteogenic differentiation of human mesenchymal stem cells [109]. Zhong et al. [110] developed a Zn/Sr ion doped collagen scaffold co-assembled HAp as reported in Fig. 6b to induce favorable bone immune microenvironment by stimulating macrophages to promote osteogenic differentiation of BMSCs. This biomimetic combination of organic and inorganic components mimics the biochemical and biophysical properties of the bone matrix [111] and can be used to develop promising candidates for applications in bone regeneration.
Application of collagen in bone/cartilage repair. a A schematic illustrating the covalent conjugation of the carboxyl groups of GO flakes to the amine groups of the collagen scaffolds. Reproduced with permission from [109]; b Synthesis of a Zn/Sr ion doped collagen scaffold co-assembled hydroxyapatite to promote osteogenic differentiation of BMSC. Reproduced with permission from [110]; c Polyphosphate-cross-linked collagen scaffold used in treatment of post-extraction bleeding and alveolar bone loss after tooth extraction. Reproduced with permission from [113]; d Preparation of polysaccharide/collagen hydrogel with BMSC recruitment function for cartilage repair. Reproduced with permission from [120]; e A new bi-layer scaffold containing Col I and BCP ceramics for regeneration in osteochondral defects. Reproduced with permission from [121]; f An injectable self-crosslinking thiolated HA-SH/Col I blend hydrogel and BCP ceramics combined with rabbit bone mesenchymal stem cells (rBMSCs)/chondrocytes used to fabricate a new bi-layer scaffold for the repair of rabbit condylar osteochondral defects. Reproduced with permission from [122]
Dentine, a bonelike matrix, is also a hard tissue of mineralized collagen [112]. Therefore, collagen-based materials are also widely used in dentistry. Gu et al. developed a collagen scaffold covalently cross-linked using polyphosphate as shown in Fig. 6c with better hemostasis and bone regeneration ability [113]. It controlled the bleeding and enabled alveolar bone retention after tooth extraction. Furthermore, absorbable barrier collagen membranes have been widely used for regeneration of periodontal defects in oral surgery because of their biocompatibility and ability to promote wound healing and help to avoid a second surgery [114].
4.2 Cartilage regeneration
Hyaline articular cartilage lacks blood vessels, lymphatics, and nerves, and has cells with a low replication potential, which limits its ability to heal [115]. As the main component of articular cartilage, collagen acts as structural and functional support [116] and is widely used in cartilage repair. Collagen-based biomaterials are generally used in the form of hydrogel or freeze-dried scaffolds, supplemented by seed cells or growth factors to form a suitable microenvironment for cartilage tissue regeneration [117]. Type II collagen is the main constituent of hyaline cartilage [118]. However, extracted type II collagen is usually not gelled by itself and is added as a cue to induce tissue regeneration [119].
In terms of cartilage repair, collagen-based scaffolds play an important role in cartilage tissue engineering. Li et al. prepared injectable cartilage repair hydrogels by polysaccharides and collagen, which had good effects on recruiting stem cells and promoting the chondrogenic differentiation of stem cells (Fig. 6d) [120]. Collagen was also used for subchondral bone repair and osteochondral full-layer repair. Cai et al. used Col I and biphasic calcium phosphate (BCP) ceramics to fabricate a new bi-layer scaffold for regeneration in osteochondral defects (Fig. 6e) [121]. Wang et al. developed an injectable self-crosslinking thiolated HA-SH/Col I blend hydrogel and BCP ceramics, combined with rabbit bone mesenchymal stem cells (rBMSCs)/chondrocytes used to fabricate a new bi-layer scaffold to simulate specific structure of rabbit condylar osteochondral defects as reported in Fig. 6f [122]. Levingstone et al. developed a multi-layer bionic collagen scaffold and implanted the scaffold into goat joints to study the long-term ability to repair osteochondral defects in large animal models [123]. Studies have shown that composite scaffolds generally have a better potential to induce cartilage regeneration than single-component scaffolds [124]. The composition and structural design of the scaffolds based on the physiological structure of cartilage aims at long-term and effective repair.
4.3 Skin tissue regeneration
Intricate bundles of collagen create a 3D network of fibers in the human skin [19]. Collagen regulates dermal matrix assembly and fibroblast movement, in turn fibroblast and derived matrix metalloproteinase (MMP)-14 regulate collagen homeostasis in the skin [125, 126]. Procollagen types I, III and VI are the major collagenous products of cultured human skin fibroblasts [127]. Collagen XII is a homotrimer with short collagenous domains that confer binding to the surface of collagen I-containing fibrils and extended flexible arms, therefore helps to maintain collagen suprastructure and to absorb stress [128].
Full-thickness skin defects are difficult to heal naturally due to their size and loss of vasculature and are highly susceptible to bacterial infection [129]. Usually, hemostatic sponges and wound dressings are used to stop bleeding and form a barrier with the outside. Traditional dressings, such as sterile gauze, medical skimmed cotton etc. can only serve as a simple physical barrier, and cannot effectively promote skin wound healing, and traditional wound dressings are easy to adhere to the wound, causing secondary damage when changing the dressing [130]. Collagen wound dressings are currently used for burns [131], trauma, infectious and surgical skin injuries, and chronic trauma procedures due to their anti-inflammatory, analgesic, and hemostatic effects, biodegradability, absorbability, strong water absorption capacity, which can help providing support for cell attachment [132,133,134]. To cite an example, Han et al. developed a tea-polyphenol treated skin collagen achieving hydro-structural adaptability, mechanical intelligence and shape-memory advantages for further skin-care products as shown in Fig. 7a [135]. Zheng et al. [136] used the polydopamine- modified collagen sponge scaffold as a new dermal regeneration template to continuously release platelet-rich plasma to accelerate skin repair (Fig. 7c). Yan et al. [137] prepared a Bletilla striata polysaccharide modified collagen composite sponge and studied its hemostatic properties.
Application of collagen in regeneration of skin tissue and cardiovascular repair. a A tea-polyphenol treated skin collagen. Reproduced with permission from [135]; b Diagram of accelerating wound healing based on CS-based hydrogels functionalized by CA-TA-ZA NSs. Reproduced with permission from [138]; c Polydopamine-modified collagen sponge scaffold as a novel dermal regeneration template with sustained release of platelet-rich plasma to accelerate skin repair. Reproduced with permission from [136]; d Acellular vascular grafts generated from collagen and elastin analogs. Reproduced with permission from [20]; e Schematic illustration of the electrospun bilayer vascular graft with an aligned PCL/collagen inner layer and a randomly distributed PCL/silica outer layer. Reproduced with permission from [142]
Many skin tissue engineering methods employ easy-to-handle and sizing methods to enhance the mechanical strength of collagen. By resisting shrinkage, the enhanced collagen hydrogel can maintain coverage of the wound throughout the healing process as shown in Fig. 7b [138, 139]. Further, the compression of collagen hydrogels following cell encapsulation can also improve their mechanical strength, stiffness, and tensile strength values closer to those of natural skin. These hydrogels could also maintain high cellular viability, which is more favorable to the response of dermal fibroblasts and keratinocytes [140, 141].
4.4 Cardiovascular repair
Collagen's hypoallergenic nature enables its application as a vascular implant (Fig. 7d) or stent, a component of artificial heart valves and a coating for cardiovascular stents [143]. However, the thrombogenic properties and in vivo calcification of collagen limit its application [20], and collagen-based stents generally do not meet the mechanical requirements of a dynamic cardiovascular environment. To address some of the mechanical limitations of natural polymers like collagen, composites have been developed with improved strength of while maintaining biological activity. Heydarkhan-Hagvall et al. designed a 3D electrospinning hybrid scaffold based on collagen/elastin/polycaprolactone (PCL) for cardiovascular tissue engineering [144]. Park et al. [142] developed a small-diameter PCL vascular graft (Fig. 7e) with a functional, bilayered PCL/collagen and PCL/silica nanofibrous structure and a composition that enables a suitable healing process and gradual degradation/replacement by natural blood vessels. The main problem with creating artificial arteries outside the body is that arteries have a complex natural structure that requires materials with adequate strength and elasticity, as well as durability for long-term use after implantation.
4.5 Other areas of tissue repair
Different adaptive forms of collagen applied in different tissue repair fields, as already mentioned, are summarized in Table 3. Besides, collagen-based bioactive materials also have good application perspectives in the fields of gynecology, reproductive medicine, plastic repair and cornea regeneration. Collagen has an impact on the important biological functions and stability of ECM, which in turn has a dynamic influence on the menstrual cycle and pregnancy. This makes collagen advantageous in gynecology and genitourinary field. In the 1990s, Jackson et al. [145] found that genitourinary prolapse was associated with a reduction in total collagen content and a decrease in collagen solubility, and suggested the development of agents to inhibit collagenolytic activity to help the treatment of this condition. In recent years, collagen-based materials have been widely developed. Collagen-based biomaterials, such as collagen hydrogels, decellularized ECM (dECM) and bioengineering techniques, 3D bioprinting of collagen, may replace hormone therapy and hold promise in reproductive organ reconstruction. Grimm et al. [146] performed clinical trials to evaluate the efficacy of a collagen-fibrin patch for the prevention of symptomatic lymphoceles after pelvic lymphadenectomy in women with gynecologic malignancies. Furthermore, as a natural component of skin, collagen are regarded as gold standard in dermal tissue reconstruction [147] and have been used in plastic surgery and cosmetic surgery for many years, and it is still in continuous innovation and development.
5 Future perspectives
Collagen has been widely used in bone/cartilage regeneration, skin repair, cardiovascular repair and other regenerative medicine applications. However, different sources and production methods lead to large variation in collagen batches, which has a serious impact on the functional stability of collagen products. In addition, the price of collagen is still very high, and the potential immunogenicity to the implanted objects warrants an urgent need to develop an effective standard production methodology and testing. The disadvantage of large batch variation of animal-derived collagen can be circumvented using biocompatible recombinant human collagen with low variability and immunogenicity. Recombinant collagen is particularly attractive as it enables the production and purification of uncommon collagen types. However, recombinant human collagen also has a few disadvantages, such as high cost, low yield and stability issues. In recent years, marine collagen sourced from marine organisms, such as fish skin and scales, has come into the spotlight. The source of marine collagen is sustainable and environmentally friendly, but its specific properties and applications need to be explored further.
Another hassle is the damage of the natural structure of collagen during the extraction process, which results in poor mechanical properties and weak gel-forming capability, thereby limiting its use in tissue engineering applications. Cross-linked collagen, collagen-based blends, mineralized collagen and structured collagen are optimized in different ways to improve the performance of collagen and meet the functional requirements in clinical applications. Cross-linking collagen can effectively improve its mechanical properties and stability, but the cross-linking method should be carefully chosen to avoid toxicity and inadvertent changes to the structure of collagen itself. Currently, there are no standard cross-linking agents available. Compared to single-component collagen, composite collagen scaffolds provide a more suitable microenvironment for tissue regeneration. However, the design of composite materials needs to be further optimized. Mineralized collagen contains both organic and inorganic components that mimic natural bone structure, but the mineralization process in vivo needs a precise regulation. Several novel technologies have been reported to develop scaffold materials, using structured collagen suitable for personalized medicine. Further research is required to achieve careful control at the microstructure level of structured collagen to preserve the ligand sites along the collagen chain. With the development of preparation processes that preserve the inherent collagen structure and chemistry, these collagen-based materials will emerge as versatile candidates for breakthrough applications in the field of tissue regeneration, complex structure mimic construction, and drug delivery.
Availability of data and materials
The datasets analyzed in this review are available as quoted and listed in the "References" section which have been specified in the article. We have obtained permission from the copyright holder to reproduce figures (or tables) that have previously been published elsewhere.
Abbreviations
- ECM:
-
Extracellular matrix
- ERK:
-
Extracellular signal-regulated kinase
- 3D:
-
Three-dimensional
- MAPK:
-
Mitogen-activated protein kinase
- Ig:
-
Immunoglobulin
- OSCAR:
-
Osteoclast associated receptor
- NFAT:
-
Activated T nuclear factor
- UV:
-
Ultraviolet
- DHT:
-
Dehydrogenation heat treatment
- GTA:
-
Glutaraldehyde
- EDC:
-
1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide
- NHS:
-
N-hydroxysuccinimide
- SM:
-
Sodium metabisulfite
- SB:
-
Sodium borohydride
- HAp:
-
Hydroxyapatite
- PAA:
-
Polyacrylic acid
- CaP:
-
Calcium phosphate
- HPAA:
-
High–molecular weight polyacrylic acid
- TRAM2:
-
Translocation-associated membrane protein 2
- SERCA2b:
-
Calcium-ATPase type 2 in the sarco-/endoplasmic reticulum
- ACP:
-
Amorphous calcium phosphate
- SPAAC:
-
Strain-promoted azide-alkyne cycloaddition
- BMSC:
-
Bone marrow-derived mesenchymal stem cells
- HA:
-
Hyaluronic acid
- Col I:
-
Type I collagen
- BCP:
-
Biphasic calcium phosphate
- NGCs:
-
Nerve guidance conduits
- GO:
-
Graphene oxide
- HA-SH:
-
Self-crosslinking hyaluronic acid
- rBMSCs:
-
Rabbit bone mesenchymal stem cells
- PCL:
-
Poly-ε-caprolactone
- dECM:
-
Decellularized ECM
References
Joyce K, Fabra GT, Bozkurt Y, Pandit A. Bioactive potential of natural biomaterials: Identification, retention and assessment of biological properties. Signal Transduct Target Ther. 2021;6(1):122.
Lin K, Zhang D, Macedo MH, Cui W, Sarmento B, Shen G. Advanced collagen-based biomaterials for regenerative biomedicine. Adv Funct Mater. 2019;29(3):1804943.
Friess W. Collagen: biomaterial for drug delivery. Eur J Pharm Biopharm. 1998;45(2):113–36.
Xu Q, Torres JE, Hakim M, Babiak PM, Pal P, Battistoni CM, Nguyen M, Panitch A, Solorio L, Liu JC. Collagen- and hyaluronic acid-based hydrogels and their biomedical applications. Mater Sci Eng R Rep. 2021;146:100641.
Bunting MD, Vyas M, Requesens M, Langenbucher A, Schiferle EB, Manguso RT, Lawrence MS, Demehri S. Extracellular matrix proteins regulate nk cell function in peripheral tissues. Sci Adv. 2022;8(11):eabk3327.
Ma CY, Wang HT, Chi YJ, Wang YL, Jiang L, Xu N, Wu Q, Feng QL, Sun XD. Preparation of oriented collagen fiber scaffolds and its application in bone tissue engineering. Appl Mater Today. 2021;22:100902.
Sorushanova A, Delgado LM, Wu Z, Shologu N, Kshirsagar A, Raghunath R, Mullen AM, Bayon Y, Pandit A, Raghunath M, Zeugolis DI. The collagen suprafamily: from biosynthesis to advanced biomaterial development. Adv Mater. 2019;31(1):e1801651.
Chen H, Xue L, Gong G. Collagen-based materials in reproductive medicine and engineered reproductive tissues. J Leather Sci Eng. 2022;4(3):1–15.
Ramshaw JA, Werkmeister JA, Glattauer V. Collagen-based biomaterials. Biotechnol Genet Eng Rev. 1996;13:335–82.
Ramshaw JA, Peng YY, Glattauer V, Werkmeister JA. Collagens as biomaterials. J Mater Sci Mater Med. 2009;20(Suppl 1):S3-8.
Xue J, Wu T, Qiu J, Rutledge S, Tanes ML, Xia Y. Promoting cell migration and neurite extension along uniaxially aligned nanofibers with biomacromolecular particles in a density gradient. Adv Funct Mater. 2020;30(40):2002031.
Lebbink RJ, Raynal N, de Ruiter T, Bihan DG, Farndale RW, Meyaard L. Identification of multiple potent binding sites for human leukocyte associated Ig-like receptor LAUR on collagens II and III. Matrix Biol. 2009;28(4):202–10.
Zhou L, Hinerman JM, Blaszczyk M, Miller JL, Conrady DG, Barrow AD, Chirgadze DY, Bihan D, Farndale RW, Herr AB. Structural basis for collagen recognition by the immune receptor oscar. Blood. 2016;127(5):529–37.
Haywood J, Qi J, Chen CC, Lu G, Liu Y, Yan J, Shi Y, Gao GF. Structural basis of collagen recognition by human osteoclast-associated receptor and design of osteoclastogenesis inhibitors. Proc Natl Acad Sci U S A. 2016;113(4):1038–43.
Ferreira AM, Gentile P, Chiono V, Ciardelli G. Collagen for bone tissue regeneration. Acta Biomater. 2012;8(9):3191–200.
Zhang D, Wu X, Chen J, Lin K. The development of collagen based composite scaffolds for bone regeneration. Bioact Mater. 2018;3(1):129–38.
Kwon H, Brown WE, Lee CA, Wang D, Paschos N, Hu JC, Athanasiou KA. Surgical and tissue engineering strategies for articular cartilage and meniscus repair. Nat Rev Rheumatol. 2019;15(9):550–70.
Parmar PA, Chow LW, St-Pierre JP, Horejs CM, Peng YY, Werkmeister JA, Ramshaw JA, Stevens MM. Collagen-mimetic peptide-modifiable hydrogels for articular cartilage regeneration. Biomaterials. 2015;54:213–25.
Liu W, Ou-Yang W, Zhang C, Wang Q, Pan X, Huang P, Zhang C, Li Y, Kong D, Wang W. Synthetic polymeric antibacterial hydrogel for methicillin-resistant staphylococcus aureus-infected wound healing: nanoantimicrobial self-assembly, drug- and cytokine-free strategy. ACS Nano. 2020;14(10):12905–17.
Kumar VA, Caves JM, Haller CA, Dai E, Liu L, Grainger S, Chaikof EL. Acellular vascular grafts generated from collagen and elastin analogs. Acta Biomater. 2013;9(9):8067–74.
Liu R, Dai M, Gong G, Chen M, Cao C, Wang T, Hou Z, Shi Y, Guo J, Zhang Y, Xia X. The role of extracellular matrix on unfavorable maternal–fetal interface: focusing on the function of collagen in human fertility. J Leather Sci Eng. 2022. https://doi.org/10.1186/s42825-022-00087-2.
Xu C, Wang Q, Chen J, Wu Y, Zhao L. Collagen matrix for periodontal plastic surgery procedures: a meta-analysis update. Int J Periodontics Restor Dent. 2019;39(4):e129–55.
Atieh MA, Alsabeeha N, Tawse-Smith A, Payne AG. Xenogeneic collagen matrix for periodontal plastic surgery procedures: a systematic review and meta-analysis. J Periodontal Res. 2016;51(4):438–52.
McTiernan CD, Simpson FC, Haagdorens M, Samarawickrama C, Hunter D, Buznyk O, Fagerholm P, Ljunggren MK, Lewis P, Pintelon I, Olsen D, Edin E, Groleau M, Allan BD, Griffith M. Liqd cornea: pro-regeneration collagen mimetics as patches and alternatives to corneal transplantation. Sci Adv. 2020. https://doi.org/10.1126/sciadv.aba2187.
Majumdar S, Wang X, Sommerfeld SD, Chae JJ, Athanasopoulou E-N, Shores LS, Duan X, Amzel LM, Stellacci F, Schein O, Guo Q, Singh A, Elisseeff JH. Cyclodextrin modulated type I collagen self-assembly to engineer biomimetic cornea implants. Adv Funct Mater. 2018;28(41):1804076.
Lei M, Zhang S, Zhou H, Wan H, Lu Y, Lin S, Sun J, Qu X, Liu C. Electrical signal initiates kinetic assembly of collagen to construct optically transparent and geometry customized artificial cornea substitutes. ACS Nano. 2022;16(7):10632–46.
Yang J, Tang Z, Liu Y, Luo Z, Xiao Y, Zhang X. Comparison of chondro-inductivity between collagen and hyaluronic acid hydrogel based on chemical/physical microenvironment. Int J Biol Macromol. 2021;182:1941–52.
Meyer M. Processing of collagen based biomaterials and the resulting materials properties. Biomed Eng Online. 2019;18(1):24.
Sionkowska A. Collagen blended with natural polymers: recent advances and trends. Prog Polym Sci. 2021;122:101452.
Sorushanova A, Delgado LM, Wu Z, Shologu N, Kshirsagar A, Raghunath R, Mullen AM, Bayon Y, Pandit A, Raghunath M, Zeugolis DI. The collagen suprafamily: from biosynthesis to advanced biomaterial development. Adv Mater. 2019;31(1):1801651.
Selvakumar G, Kuttalam I, Mukundan S, Lonchin S. Valorization of toxic discarded fish skin for biomedical application. J Clean Prod. 2021;323:129147.
Govindharaj M, Roopavath UK, Rath SN. Valorization of discarded marine eel fish skin for collagen extraction as a 3D printable blue biomaterial for tissue engineering. J Clean Prod. 2019;230:412–9.
Salvatore L, Gallo N, Natali ML, Campa L, Lunetti P, Madaghiele M, Blasi FS, Corallo A, Capobianco L, Sannino A. Marine collagen and its derivatives: versatile and sustainable bio-resources for healthcare. Mater Sci Eng C. 2020;113:110963.
Yoon J, Yoon D, Lee H, Lee J, Jo S, Kym D, Yim H, Hur J, Chun W, Kim G, Cho YS. Wound healing ability of acellular fish skin and bovine collagen grafts for split-thickness donor sites in burn patients: characterization of acellular grafts and clinical application. Int J Biol Macromol. 2022;205:452–61.
Subhan F, Hussain Z, Tauseef I, Shehzad A, Wahid F. A review on recent advances and applications of fish collagen. Crit Rev Food Sci Nutr. 2021;61(6):1027–37.
Liu W, Lin H, Zhao P, Xing L, Li J, Wang Z, Ju S, Shi X, Liu Y, Deng G, Gao G, Sun L, Zhang X. A regulatory perspective on recombinant collagen-based medical devices. Bioact Mater. 2022;12:198–202.
Sun Y, Li X, Zhao M, Chen Y, Xu Y, Wang K, Bian S, Jiang Q, Fan Y, Zhang X. Bioinspired supramolecular nanofiber hydrogel through self-assembly of biphenyl-tripeptide for tissue engineering. Bioact Mater. 2022;8:396–408.
Chen Z, Fan D, Shang L. Exploring the potential of the recombinant human collagens for biomedical and clinical applications: a short review. Biomed Mater. 2020;16(1):012001.
Yang Y, Campbell Ritchie A, Everitt NM. Recombinant human collagen/chitosan-based soft hydrogels as biomaterials for soft tissue engineering. Mater Sci Eng C. 2021;121:111846.
Wang J, Qiu H, Xu Y, Gao Y, Tan P, Zhao R, Liu Z, Tang Y, Zhu X, Bao C, Wang H, Lin H, Zhang X. The biological effect of recombinant humanized collagen on damaged skin induced by uv-photoaging: an in vivo study. Bioact Mater. 2022;11:154–65.
Olsen D, Yang C, Bodo M, Chang R, Leigh S, Baez J, Carmichael D, Perala M, Hamalainen ER, Jarvinen M, Polarek J. Recombinant collagen and gelatin for drug delivery. Adv Drug Deliv Rev. 2003;55(12):1547–67.
Wang T, Lew J, Premkumar J, Poh CL, Win NM. Production of recombinant collagen: state of the art and challenges. Eng Biol. 2017;1(1):18–23.
Majsterek I, McAdams E, Adachi E, Dhume ST, Fertala A. Prospects and limitations of the rational engineering of fibrillar collagens. Protein Sci. 2003;12(9):2063–72.
Gelse K, Poschl E, Aigner T. Collagens–structure, function, and biosynthesis. Adv Drug Deliv Rev. 2003;55(12):1531–46.
Walimbe T, Calve S, Panitch A, Sivasankar MP. Incorporation of types I and III collagen in tunable hyaluronan hydrogels for vocal fold tissue engineering. Acta Biomater. 2019;87:97–107.
Gibney R, Patterson J, Ferraris E. High-resolution bioprinting of recombinant human collagen type III. Polymers. 2021;13(17):2973.
Birk DE, Fitch JM, Babiarz JP, Linsenmayer TF. Collagen type I and type V are present in the same fibril in the avian corneal stroma. J Cell Biol. 1988;106(3):999–1008.
Liu YFCW, Lin YF, Yang RC, Lin MW, Li LH, Chang YH, Jou YS, Lin PY, Su JS, Huang SF, Hsiao KJ, Fann CSJ, Hwang HW, Chen YT, Tsai SF. Type II collagen gene variants and inherited osteonecrosis of the femoral head. Engl J Med. 2005;352:2294–301.
Lamande SR, Bateman JF. Collagen vi disorders: Insights on form and function in the extracellular matrix and beyond. Matrix Biol. 2018;71–72:348–67.
Bolduc VSK, Sarathy A, Zou Y, Bönnemann CG. 150. Further development of an allele-specific gene silencing strategy to correct a dominant-negative mutation causing collagen vi-related muscular dystrophy. Mol Ther. 2016;24(Suppl 1):S60.
Church RL, Pfeiffer SE, Tanzer ML. Collagen biosynthesis: synthesis and secretion of a high molecular weight collagen precursor (procollagen). Proc Natl Acad Sci U S A. 1971;68(11):2638–42.
Tanzer MLCR, Yaeger JA, Wampler DE, Park ED. Procollagen: intermediate forms containing several types of peptide chains and non-collagen peptide extensions at nh2 and cooh ends. Proc Natl Acad Sci. 1974;71(8):3009–13.
Bornstein P, Ehrlich HP, Wyke AW. Procollagen: conversion of the precursor to collagen by a neutral protease. Science. 1972;175(4021):544–6.
Bourhis JM, Vadon-Le Goff S, Afrache H, Mariano N, Kronenberg D, Thielens N, Moali C, Hulmes DJ. Procollagen C-proteinase enhancer grasps the stalk of the C-propeptide trimer to boost collagen precursor maturation. Proc Natl Acad Sci U S A. 2013;110(16):6394–9.
Prockop DJSA, Li SW. Procollagen n-proteinase and procollagen c-proteinase. Two unusual metalloproteinases that are essential for procollagen processing probably have important roles in development and cell signaling. Matrix Biol. 1998;16(7):399–408.
Dong C, Lv Y. Application of collagen scaffold in tissue engineering: recent advances and new perspectives. Polymers. 2016;8(2):42.
An B, Lin YS, Brodsky B. Collagen interactions: drug design and delivery. Adv Drug Deliv Rev. 2016;97:69–84.
Siljander PR, Munnix IC, Smethurst PA, Deckmyn H, Lindhout T, Ouwehand WH, Farndale RW, Heemskerk JW. Platelet receptor interplay regulates collagen-induced thrombus formation in flowing human blood. Blood. 2004;103(4):1333–41.
Yamaguchi Y, Mann DM, Ruoslahti E. Negative regulation of transforming growth factor-beta by the proteoglycan decorin. Nature. 1990;346(6281):281–4.
Ricard-Blum S. The collagen family. CSH Perspect Biol. 2011;3(1):a004978.
Gu L, Shan T, Ma YX, Tay FR, Niu L. Novel biomedical applications of crosslinked collagen. Trends Biotechnol. 2019;37(5):464–91.
Delgado LM, Bayon Y, Pandit A, Zeugolis DI. To cross-link or not to cross-link? Cross-linking associated foreign body response of collagen-based devices. Tissue Eng Part B Rev. 2015;21(3):298–313.
Bailey AJ, Light ND, Atkins ED. Chemical cross-linking restrictions on models for the molecular organization of the collagen fibre. Nature. 1980;288(5789):408–10.
Charulatha V, Rajaram A. Influence of different crosslinking treatments on the physical properties of collagen membranes. Biomaterials. 2003;24(5):759–67.
Pien N, Bray F, Gheysens T, Tytgat L, Rolando C, Mantovani D, Dubruel P, Vlierberghe SV. Proteomics as a tool to gain next level insights into photo-crosslinkable biopolymer modifications. Bioact Mater. 2022;17:204–20.
Xu Z, Yuan L, Liu Q, Li D, Mu C, Zhao L, Li X, Ge L. Crosslinking effect of dialdehyde cholesterol modified starch nanoparticles on collagen hydrogel. Carbohydr Polym. 2022;285:119237.
Islam MM, AbuSamra DB, Chivu A, Argueso P, Dohlman CH, Patra HK, Chodosh J, Gonzalez-Andrades M. Optimization of collagen chemical crosslinking to restore biocompatibility of tissue-engineered scaffolds. Pharmaceutics. 2021;13(6):832.
Nair M, Calahorra Y, Kar-Narayan S, Best SM, Cameron RE. Self-assembly of collagen bundles and enhanced piezoelectricity induced by chemical crosslinking. Nanoscale. 2019;11(32):15120–30.
Hentzen NB, Smeenk LEJ, Witek J, Riniker S, Wennemers H. Cross-linked collagen triple helices by oxime ligation. J Am Chem Soc. 2017;139(36):12815–20.
Wang W, Zhang Y, Ye R, Ni Y. Physical crosslinkings of edible collagen casing. Int J Biol Macromol. 2015;81:920–5.
Delgado LM, Fuller K, Zeugolis DI. Collagen cross-linking: biophysical, biochemical, and biological response analysis. Tissue Eng Part A. 2017;23(19–20):1064–77.
Petta D, D’Amora U, D’Arrigo D, Tomasini M, Candrian C, Ambrosio L, Moretti M. Musculoskeletal tissues-on-a-chip: role of natural polymers in reproducing tissue-specific microenvironments. Biofabrication. 2022;14:042001.
He L, Theato P. Collagen and collagen mimetic peptide conjugates in polymer science. Eur Polym J. 2013;49(10):2986–97.
Byrne C, McEwan PA, Emsley J, Fischer PM, Chan WC. End-stapled homo and hetero collagen triple helices: a click chemistry approach. Chem Commun. 2011;47(9):2589–91.
Lee HJ, Fernandes-Cunha GM, Putra I, Koh WG, Myung D. Tethering growth factors to collagen surfaces using copper-free click chemistry: surface characterization and in vitro biological response. ACS Appl Mater Interfaces. 2017;9(28):23389–99.
Heck T, Faccio G, Richter M, Thony-Meyer L. Enzyme-catalyzed protein crosslinking. Appl Microbiol Biotechnol. 2013;97(2):461–75.
Perez-Puyana V, Jimenez-Rosado M, Romero A, Guerrero A. Crosslinking of hybrid scaffolds produced from collagen and chitosan. Int J Biol Macromol. 2019;139:262–9.
Wu S, Chen Y, Guo X, Wu Y. Collagen mineralization and its applications in hard tissue repair. Mater Chem Front. 2021;5(19):7071–87.
Song Q, Jiao K, Tonggu L, Wang LG, Zhang SL, Yang YD, Zhang L, Bian JH, Hao DX, Wang CY, Ma YX, Arola DD, Breschi L, Chen JH, Tay FR, Niu LN. Contribution of biomimetic collagen-ligand interaction to intrafibrillar mineralization. Sci Adv. 2019;5(3):eaav9075.
Oosterlaken BM, Vena MP, de With G. In vitro mineralization of collagen. Adv Mater. 2021;33(16):e2004418.
Wu L, Wang Q, Li Y, Yang M, Dong M, He X, Zheng S, Cao CY, Zhou Z, Zhao Y, Li Q-L. A dopamine acrylamide molecule for promoting collagen biomimetic mineralization and regulating crystal growth direction. ACS Appl Mater Interfaces. 2021;13(33):39142–56.
Liu Y, Kim YK, Dai L, Li N, Khan SO, Pashley DH, Tay FR. Hierarchical and non-hierarchical mineralisation of collagen. Biomaterials. 2011;32(5):1291–300.
Ping H, Wagermaier W, Horbelt N, Scoppola E, Li C, Werner P, Fu Z, Fratzl P. Mineralization generates megapascal contractile stresses in collagen fibrils. Science. 2022;376(6589):188–92.
Li Z, Du T, Ruan C, Niu X. Bioinspired mineralized collagen scaffolds for bone tissue engineering. Bioact Mater. 2021;6(5):1491–511.
Zhang J, Ji Y, Jiang S, Shi M, Cai W, Miron RJ, Zhang Y. Calcium-collagen coupling is vital for biomineralization schedule. Adv Sci. 2021;8(15):e2100363.
Shao C, Zhao R, Jiang S, Yao S, Wu Z, Jin B, Yang Y, Pan H, Tang R. Citrate improves collagen mineralization via interface wetting: a physicochemical understanding of biomineralization control. Adv Mater. 2018;30(8):1704876.
de Melo PD, Davison N, Habibovic P. Human osteoclast formation and resorptive function on biomineralized collagen. Bioact Mater. 2022;8:241–52.
Chen Y, Sui J, Wang Q, Yin Y, Liu J, Wang Q, Han X, Sun Y, Fan Y, Zhang X. Injectable self-crosslinking HA-SH/Col I blend hydrogels for in vitro construction of engineered cartilage. Carbohydr Polym. 2018;190:57–66.
Chen F, Le P, Fernandes-Cunha GM, Heilshorn SC, Myung D. Bio-orthogonally crosslinked hyaluronate-collagen hydrogel for suture-free corneal defect repair. Biomaterials. 2020;255:120176.
Rafat M, Xeroudaki M, Koulikovska M, Sherrell P, Groth F, Fagerholm P, Lagali N. Composite core-and-skirt collagen hydrogels with differential degradation for corneal therapeutic applications. Biomaterials. 2016;83:142–55.
Zheng L, Liu S, Cheng X, Qin Z, Lu Z, Zhang K, Zhao J. Intensified stiffness and photodynamic provocation in a collagen-based composite hydrogel drive chondrogenesis. Adv Sci. 2019;6(16):1900099.
Khan SA, Shah LA, Shah M, Jamil I. Engineering of 3D polymer network hydrogels for biomedical applications: a review. Polym Bull. 2022;79(4):2685–705.
Irastorza A, Zarandona I, Andonegi M, Guerrero P, de la Caba K. The versatility of collagen and chitosan: from food to biomedical applications. Food Hydrocoll. 2021;116:106633.
Wlodarczyk-Biegun MK, Del Campo A. 3D bioprinting of structural proteins. Biomaterials. 2017;134:180–201.
Madruga LYC, Kipper MJ. Expanding the repertoire of electrospinning: new and emerging biopolymers, techniques, and applications. Adv Healthc Mater. 2022;11(4):e2101979.
Bazrafshan Z, Stylios GK. Spinnability of collagen as a biomimetic material: a review. Int J Biol Macromol. 2019;129:693–705.
Zhang Z, Jørgensen ML, Wang Z, Amagat J, Wang Y, Li Q, Dong M, Chen M. 3D anisotropic photocatalytic architectures as bioactive nerve guidance conduits for peripheral neural regeneration. Biomaterials. 2020;253:120108.
Shekhter AB, Fayzullin AL, Vukolova MN, Rudenko TG, Osipycheva VD, Litvitsky PF. Medical applications of collagen and collagen-based materials. Curr Med Chem. 2019;26(3):506–16.
Lee A, Hudson AR, Shiwarski DJ, Tashman JW, Hinton TJ, Yerneni S, Bliley JM, Campbell PG, Feinberg AW. 3d bioprinting of collagen to rebuild components of the human heart. Science. 2019;365(6452):482–7.
Gloria A, Russo T, D’Amora U, Santin M, De Santis R, Ambrosio L. Customised multiphasic nucleus/annulus scaffold for intervertebral disc repair/regeneration. Connect Tissue Res. 2020;61(2):152–62.
D’Amora U, D’Este M, Eglin D, Safari F, Sprecher CM, Gloria A, De Santis R, Alini M, Ambrosio L. Collagen density gradient on three-dimensional printed poly(ε-caprolactone) scaffolds for interface tissue engineering. J Tissue Eng Regen Med. 2018;12(2):321–9.
Jacob J, Haponiuk JT, Thomas S, Gopi S. Biopolymer based nanomaterials in drug delivery systems: a review. Mater Today Chem. 2018;9:43–55.
Sun J, Mou C, Shi Q, Chen B, Hou X, Zhang W, Li X, Zhuang Y, Shi J, Chen Y, Dai J. Controlled release of collagen-binding sdf-1α from the collagen scaffold promoted tendon regeneration in a rat achilles tendon defect model. Biomaterials. 2018;162:22–33.
Kanematsu A, Yamamoto S, Ozeki M, Noguchi T, Kanatani I, Ogawa O, Tabata Y. Collagenous matrices as release carriers of exogenous growth factors. Biomaterials. 2004;25(18):4513–20.
Agrawal G, Agrawal R. Functional microgels: recent advances in their biomedical applications. Small. 2018;14(39):e1801724.
Olszta MJ, Cheng X, Jee SS, Kumar R, Kim Y-Y, Kaufman MJ, Douglas EP, Gower LB. Bone structure and formation: a new perspective. Mater Sci Eng R Rep. 2007;58(3):77–116.
Oliveira MR, Martins E, Célio-Mariano R, Sonoda CK, Rangel Garcia I Jr, de Melo WM. Tissue engineering: using collagen type I matrix for bone healing of bone defects. J Craniofac Surg. 2013;24(4):e394-396.
Li X, Chen M, Wang P, Yao Y, Han X, Liang J, Jiang Q, Sun Y, Fan Y, Zhang X. A highly interweaved ha-ss-nhap/collagen hybrid fibering hydrogel enhances osteoinductivity and mineralization. Nanoscale. 2020;12(24):12869–82.
Kang S, Park JB, Lee T-J, Ryu S, Bhang SH, La W-G, Noh M-K, Hong BH, Kim B-S. Covalent conjugation of mechanically stiff graphene oxide flakes to three-dimensional collagen scaffolds for osteogenic differentiation of human mesenchymal stem cells. Carbon. 2015;83:162–72.
Zhong Z, Wu X, Wang Y, Li M, Li Y, Liu X, Zhang X, Lan Z, Wang J, Du Y, Zhang S. Zn/sr dual ions-collagen co-assembly hydroxyapatite enhances bone regeneration through procedural osteo-immunomodulation and osteogenesis. Bioact Mater. 2022;10:195–206.
Lu G, Xu Y, Liu Q, Chen M, Sun H, Wang P, Li X, Wang Y, Li X, Hui X, Luo E, Liu J, Jiang Q, Liang J, Fan Y, Sun Y, Zhang X. An instantly fixable and self-adaptive scaffold for skull regeneration by autologous stem cell recruitment and angiogenesis. Nat Commun. 2022;13(1):2499.
Zhang Y, Huang Y, Pang Y, Zhu Z, Zhang Y, Liu Q, Zhang X, Liu Y. Modification of collagen with proanthocyanidins by mimicking the bridging role of glycosaminoglycans for dentine remineralization. Mater Des. 2021;210:110067.
Gu JT, Jiao K, Li J, Yan JF, Wang KY, Wang F, Liu Y, Tay FR, Chen JH, Niu LN. Polyphosphate-crosslinked collagen scaffolds for hemostasis and alveolar bone regeneration after tooth extraction. Bioact Mater. 2022;15:68–81.
Sbricoli L, Guazzo R, Annunziata M, Gobbato L, Bressan E, Nastri L. Selection of collagen membranes for bone regeneration: a literature review. Materials. 2020;13(3):786.
Yao Y, Wang P, Li X, Xu Y, Lu G, Jiang Q, Sun Y, Fan Y, Zhang X. A di-self-crosslinking hyaluronan-based hydrogel combined with type i collagen to construct a biomimetic injectable cartilage-filling scaffold. Acta Biomater. 2020;111:197–207.
Responte DJ, Natoli RM, Athanasiou KA. Collagens of articular cartilage: structure, function, and importance in tissue engineering. Critical reviews™. Biomed Eng. 2007;35(5):363–411.
Wang Q, Li X, Wang P, Yao Y, Xu Y, Chen Y, Sun Y, Jiang Q, Fan Y, Zhang X. Bionic composite hydrogel with a hybrid covalent/noncovalent network promoting phenotypic maintenance of hyaline cartilage. J Mater Chem B. 2020;8(20):4402–11.
Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461–8.
Li X, Bian S, Zhao M, Han X, Liang J, Wang K, Jiang Q, Sun Y, Fan Y, Zhang X. Stimuli-responsive biphenyl-tripeptide supramolecular hydrogels as biomimetic extracellular matrix scaffolds for cartilage tissue engineering. Acta Biomater. 2021;131:128–37.
Li Z, Cao H, Xu Y, Li X, Han X, Fan Y, Jiang Q, Sun Y, Zhang X. Bioinspired polysaccharide hybrid hydrogel promoted recruitment and chondrogenic differentiation of bone marrow mesenchymal stem cells. Carbohydr Polym. 2021;267:118224.
Cai H, Yao Y, Xu Y, Wang Q, Zou W, Liang J, Sun Y, Zhou C, Fan Y, Zhang X. A Col I and BCP ceramic bi-layer scaffold implant promotes regeneration in osteochondral defects. RSC Adv. 2019;9(7):3740–8.
Wang H, Xu Y, Wang P, Ma J, Wang P, Han X, Fan Y, Bai D, Sun Y, Zhang X. Cell-mediated injectable blend hydrogel-BCP ceramic scaffold for in situ condylar osteochondral repair. Acta Biomater. 2021;123:364–78.
Levingstone TJ, Ramesh A, Brady RT, Brama PAJ, Kearney C, Gleeson JP, O’Brien FJ. Cell-free multi-layered collagen-based scaffolds demonstrate layer specific regeneration of functional osteochondral tissue in caprine joints. Biomaterials. 2016;87:69–81.
Cai H, Wang P, Xu Y, Yao Y, Liu J, Li T, Sun Y, Liang J, Fan Y, Zhang X. BMSCs-assisted injectable Col I hydrogel-regenerated cartilage defect by reconstructing superficial and calcified cartilage. Regen Biomater. 2020;7(1):35–45.
Theocharidis G, Drymoussi Z, Kao AP, Barber AH, Lee DA, Braun KM, Connelly JT. Type VI collagen regulates dermal matrix assembly and fibroblast motility. J Invest Dermatol. 2016;136(1):74–83.
Zigrino P, Brinckmann J, Niehoff A, Lu Y, Giebeler N, Eckes B, Kadler KE, Mauch C. Fibroblast-derived MMP-14 regulates collagen homeostasis in adult skin. J Invest Dermatol. 2016;136(8):1575–83.
Olsen DR, Peltonen J, Jaakkola S, Chu ML, Uitto J. Collagen gene expression by cultured human skin fibroblasts. Abundant steady-state levels of type VI procollagen messenger RNAs. J Clin Invest. 1989;83(3):791–5.
Schonborn K, Willenborg S, Schulz JN, Imhof T, Eming SA, Quondamatteo F, Brinckmann J, Niehoff A, Paulsson M, Koch M, Eckes B, Krieg T. Role of collagen XII in skin homeostasis and repair. Matrix Biol. 2020;94:57–76.
Han Y, Hu J, Sun G. Recent advances in skin collagen: Functionality and non-medical applications. J Leather Sci Eng. 2021;3(1):4.
Peng W, Li D, Dai K, Wang Y, Song P, Li H, Tang P, Zhang Z, Li Z, Zhou Y, Zhou C. Recent progress of collagen, chitosan, alginate and other hydrogels in skin repair and wound dressing applications. Int J Biol Macromol. 2022;208:400–8.
Rnjak-Kovacina J, Wise SG, Li Z, Maitz PKM, Young CJ, Wang Y, Weiss AS. Electrospun synthetic human elastin: collagen composite scaffolds for dermal tissue engineering. Acta Biomater. 2012;8(10):3714–22.
Cui B, Zhang C, Gan B, Liu W, Liang J, Fan Z, Wen Y, Yang Y, Peng X, Zhou Y. Collagen-tussah silk fibroin hybrid scaffolds loaded with bone mesenchymal stem cells promote skin wound repair in rats. Mater Sci Eng C. 2020;109:110611.
Prelipcean A-M, Iosageanu A, Gaspar-Pintiliescu A, Moldovan L, Craciunescu O, Negreanu-Pirjol T, Negreanu-Pirjol B, Mitran R-A, Marin M, D’Amora U. Marine and agro-industrial by-products valorization intended for topical formulations in wound healing applications. Materials. 2022;15(10):3507.
Tripathi D, Rastogi K, Tyagi P, Rawat H, Mittal G, Jamini A, Singh H, Tyagi A. Comparative analysis of collagen and chitosan-based dressing for haemostatic and wound healing application. AAPS Pharm Sci Tech. 2021;22(3):76.
Han Y, Jiang Y, Hu J. Tea-polyphenol treated skin collagen owns coalesced adaptive-hydration, tensile strength and shape-memory property. Int J Biol Macromol. 2020;158:1–8.
Zheng Z, Li M, Shi P, Gao Y, Ma J, Li Y, Huang L, Yang Z, Yang L. Polydopamine-modified collagen sponge scaffold as a novel dermal regeneration template with sustained release of platelet-rich plasma to accelerate skin repair: a one-step strategy. Bioact Mater. 2021;6(8):2613–28.
Yan X, Chen Y, Dan W, Dan N, Li Z. Bletilla striata polysaccharide modified collagen fiber composite sponge with rapid hemostasis function. J Leather Sci Eng. 2022;4(1):5.
Sun X, Jia P, Zhang H, Dong M, Wang J, Li L, Bu T, Wang X, Wang L, Lu Q, Wang J. Green regenerative hydrogel wound dressing functionalized by natural drug-food homologous small molecule self-assembled nanospheres. Adv Funct Mater. 2022;32(7):2106572.
Helary C, Bataille I, Abed A, Illoul C, Anglo A, Louedec L, Letourneur D, Meddahi-Pellé A, Giraud-Guille MM. Concentrated collagen hydrogels as dermal substitutes. Biomaterials. 2010;31(3):481–90.
Pensalfini M, Ehret AE, Studeli S, Marino D, Kaech A, Reichmann E, Mazza E. Factors affecting the mechanical behavior of collagen hydrogels for skin tissue engineering. J Mech Behav Biomed Mater. 2017;69:85–97.
Sohutskay DO, Buno KP, Tholpady SS, Nier SJ, Voytik-Harbin SL. Design and biofabrication of dermal regeneration scaffolds: role of oligomeric collagen fibril density and architecture. Regen Med. 2020;15(2):1295–312.
Park S, Kim J, Lee M-K, Park C, Jung H-D, Kim H-E, Jang T-S. Fabrication of strong, bioactive vascular grafts with PCL/collagen and PCL/silica bilayers for small-diameter vascular applications. Mater Des. 2019;181:108079.
Yang L, Wu H, Lu L, He Q, Xi B, Yu H, Luo R, Wang Y, Zhang X. A tailored extracellular matrix (ECM): mimetic coating for cardiovascular stents by stepwise assembly of hyaluronic acid and recombinant human type III collagen. Biomaterials. 2021;276:121055.
Heydarkhan-Hagvall S, Schenke-Layland K, Dhanasopon AP, Rofail F, Smith H, Wu BM, Shemin R, Beygui RE, MacLellan WR. Three-dimensional electrospun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials. 2008;29(19):2907–14.
Jackson SR, Avery NC, Tarlton JF, Eckford SD, Abrams P, Bailey AJ. Changes in metabolism of collagen in genitourinary prolapse. Lancet. 1996;347(9016):1658–61.
Grimm C, Polterauer S, Helmy-Bader S, Zikan M, Cibula D, Heitz F, Harter P, Giese A, Reinthaller A, Tempfer C. A collagen-fibrin patch for the prevention of symptomatic lymphoceles after pelvic lymphadenectomy in women with gynecologic malignancies: a randomized clinical trial. Gynecol Oncol. 2018;149(1):140–5.
Schwab R, Heller M, Pfeifer C, Unger RE, Walenta S, Nezi-Cahn S, Al-Nawas B, Hasenburg A, Brenner W. Full-thickness tissue engineered oral mucosa for genitourinary reconstruction: a comparison of different collagen-based biodegradable membranes. J Biomed Mater Res B Appl Biomater. 2021;109(4):572–83.
Acknowledgements
This work was supported by National Key R&D Project of China (Grant No. 2018YFC1105900), National Natural Science Foundation of China (32071352 and 81860392) and Sichuan University Innovation Spark Project (2018SCUH0089).
Author information
Authors and Affiliations
Contributions
YS and UD made substantial contributions to the conception, design and revision of this review. JZ wrote the manuscript. ZL and YZ downloaded and summarized related literatures. GL, AR and JL designed and retouched all figures and tables. YF and XZ participated in the corrections and the design of figures. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
All authors declare no financial interest competition.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, J., Li, Z., Zou, Y. et al. Advanced application of collagen-based biomaterials in tissue repair and restoration. J Leather Sci Eng 4, 30 (2022). https://doi.org/10.1186/s42825-022-00102-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42825-022-00102-6