Abstract
Objective
To more precisely estimate the association between the tumor necrosis factor ligand superfamily member 4 (TNFSF4) gene polymorphisms and systemic lupus erythematosus (SLE) susceptibility, we performed a meta-analysis on the association of the following single nucleotide polymorphisms (SNPs) of TNFSF4 with SLE: rs1234315, rs844648, rs2205960, rs704840, rs844644, rs10489265.
Methods
A literature-based search was conducted using PubMed, MEDLINE, Embase, Web of Science databases, and Cochrane Library databases to identify all relevant studies. And the association of TNFSF4 gene polymorphisms and SLE susceptibility was evaluated by pooled odds ratio (OR) with 95% confidence interval (CI).
Results
The meta-analysis produced overall OR of 1.42 (95% CI 1.36–1.49, P < 0.00001), 1.41 (95% CI 1.36–1.46, P < 0.00001) and 1.34 (95% CI 1.26–1.42, P < 0.00001) for the rs2205960, rs1234315 and rs704840 polymorphisms respectively, confirming these three SNPs confer a significant risk for the development of SLE. On the other hand, the meta-analysis produced overall OR of 0.92 (95% CI 0.70–1.21, P = 0.54) for the rs844644 polymorphism, suggesting no significant association. And no association was also found between either rs844648 1.11 (OR 1.11, 95% CI 0.86–1.43, P = 0.41) or rs10489265 (OR 1.17, 95% CI 0.94–1.47, P = 0.17) polymorphism with SLE susceptibility, respectively.
Conclusions
Our meta-analysis demonstrated that the TNFSF4 rs2205960, rs1234315 and rs844840 SNPs was significantly associated with an increased risk of SLE.
Similar content being viewed by others
Introduction
SLE is a chronic multisystem complex autoimmune disorder, which is characterized by pathogenic humoral and cellular immunity to self-antigen [1]. There are a series of SLE manifestations in clinic, such as a vast array of autoantibodies productions, arthritis, mucocutaneous manifestations, hematological disorders and so on [2, 3]. It is reported that the frequency of SLE occurrence is nine times higher in female than in male [4]. Although the etiology of SLE is still incompletely understood, the pathogenesis of SLE is partially owing to the loss of immune tolerance and the deposition of immune complexes. Additionally, the defective B cell suppression and excess T cell help are definitely involved in these process [5]. To our knowledge, the pathogenesis of SLE may largely be triggered by both genetic susceptibility and environmental predisposing factors [3]. And a great contribution of genetic factors to SLE susceptibility was confirmed in comparative studies between the concordance rate of monozygotic twins and dizygotic pairs [6].
Over the last decades, great efforts have been made to identify the genes and genomic regions of SLE susceptibility through genetic association studies, especially genome-wide association studies (GWAS). And numerous susceptibility genes of SLE have been widely addressed, including HLA class II haplotypes, STAT4, MHC-I, NCF2, FCGR2B, BLK, IRF5/TNPO3, TNFAIP3, and TNFSF4 [3]. As one of susceptibility genes for SLE involved in NF-κB signaling pathway, many studies have examined the association between TNFSF4 gene polymorphisms and the risk of SLE [7,8,9,10]. The tumor necrosis factor ligand superfamily member 4 (TNFSF4, also known as OX40 ligand, OX40L, and CD252) encodes the ligand for OX40 (TNFRSF4; also known as OX40 and CD134) [11]. And OX40L is mainly expressed on activated antigen-presenting cells (APCs), such as activated B cells, dendritic cells (DCs), macrophages. OX40 transiently expresses on both activated CD4 + T cells and CD8 + T cells. The engagement of OX40 with its ligand has a dual effect on T cell responses: it can enhance Th1-mediated immune response and promote generation and maintenance of Th2, but concomitantly antagonizes Treg generation and Treg-mediated suppression [11]. OX40-OX40L interaction also promotes the survive and expansion of CD8 + T cells and the recall response of CD8 + memory T cell in vivo [12]. Furthermore, OX40-OX40L may also augment B cell differentiation and proliferation. Therefore, OX40-OX40L blockade in vivo may ameliorate autoimmunity by preventing migration and proliferation of T cells, affecting T cell polarization, altering cytokine production [9, 12].
The human TNFSF4 gene is located at 1q25. A number of studies have examined the association between TNFSF4 gene polymorphisms and the risk of SLE. For example, Zhou et al. found TNFSF4 rs2205960 with SLE susceptibility in Chinese (P = 2.82 × 10–5) [13]. And Zhang confirmed the association between the TNFSF4 rs1234315 SNPs and the SLE (ORs of 1.45 and P values of 1.5 × 10–16) [14]. And a recent study also confirms TNFSF4 rsl234315 as a SLE susceptibility locus in a Chinese Guangxi population [1]. There once was a published meta-analysis about the association of TNFSF4 polymorphisms with SLE in 2012, which only focused on four common SNPs, rs2205960, rs1234315, rs844644, and rs844648 [6]. With rapid progress of SLE genetics study and massive new research data available during recent seven years, it’s extremely essential to make a meta-analysis update. Thus, in the present study, we performed a meta-analysis to investigate whether six identified TNFSF4 SNPs, rs1234315, rs844648, rs2205960, rs704840, rs844644 and rs10489265 polymorphisms confer susceptibility to SLE in different ethnic groups.
Materials and methods
Identification of eligible studies and data extraction
An exhaustive literature search was conducted using PubMed, MEDLINE, Embase, Web of Science databases, and Cochrane Library databases to examine the TNFSF4 polymorphisms in SLE patients and controls (until February 2021). The following keywords and subject terms were searched in different combinations: “TNFSF4” or “tumor necrosis factor ligand superfamily member 4” or “CD252” or “OX40L” or “OX40 ligand” and “systemic lupus erythematosus” or “SLE”. Additionally, potentially relevant studies were also traced from the reference lists of the identified articles. The eligible studies were included according to the following criteria: (1) it contained original data (independence among studies), (2) it used an unrelated case–control design, and (3) it provided sufficient data to calculate the odds ratio (OR). All patients included in these studies fulfilled the American College of Rheumatology criteria [15] or the ACR 1997 revised criteria [16]. When a study reported results on different subpopulations, we treated each subpopulation as a separate study in the meta-analysis. Exclusion criteria were as follows: (1) abstracts, reviews, and meta-analyses; (2) studies without patient samples; (3) studies without usable data; and for duplicate publications, only the most recent or most informative single article was included. Among these articles, the following data was extracted: (1) publication details, including first author’s name and publication year; (2) TNFSF4 polymorphisms details, including single-nucleotide polymorphisms (SNPs) and minor allele (MA); (3) characteristics of studied subjects, such as the country and ethnicity of study population, numbers of SLE cases and controls, and TNFSF4 polymorphisms minor allele frequencies(MAF); (4) ORs of associations between different SNPs and SLE susceptibility, as well as their 95% CIs and P value. And original data were requested from study authors if necessary.
Evaluation of statistical associations
Allele frequencies of the TNFSF4 rs1234315, rs844648, rs2205960, rs704840, rs844644 and rs10489265 polymorphisms from each respective study were determined using the allele-counting method. And ORs with 95% CIs were determined in each study to evaluate the correlation of SNPs polymorphisms and SLE susceptibility. The data heterogeneity was examined by Cochran’s Q test. When the studies contained no or moderate heterogeneity on the basis of Q test (P > 0.10), the fixed-effect model was adopted using the Mantel–Haenszel method, which assumes that genetic factors have similar effects on SLE susceptibility across all studies, and that observed variations between studies are caused by chance alone. By contrast, when a significant Q-statistic (P < 0.10) indicated heterogeneity across studies, the random effects model was applied, using the Der Simonian and Laird method, which assumes that different studies show substantial diversity, and assesses both within-study sampling errors and between-study variances. The random effects model is used in the presence of significant between-study heterogeneity. We also quantified the effect of heterogeneity using I2 = 100% × (Q − df)/Q. The I2-statistic measures the degree of inconsistency in the studies, and represents the proportion of inter-study variability attributable to heterogeneity rather than chance. Statistical analysis was performed by utilizing RevMan 5.3 software and STATA package version 12.0 (Stata Corporation, College Station, Texas, USA). The significance of pooled ORs was tested using the Z test (P < 0.05 was considered significant).
Evaluation of publication bias
Potential publication bias was assessed by the funnel plot and Begg’s and Egger’s test in which an asymmetric plot suggests a possible publication bias. Egger’s linear regression test was used to measure the funnel plot asymmetry on the natural logarithm scale of the OR. The significance of the intercept was determined by the t test, and a P < 0.05 was considered to indicate significant statistical publication bias.
Results
Characteristics of the included studies
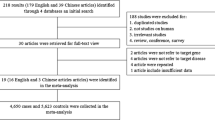
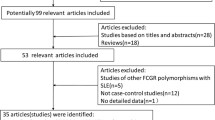
As showed in Fig. 1, 92 articles were retrieved at the beginning. Based on the described search criteria, 72 articles were collected for the initial screening after excluding the duplicate articles. Next, 24 records were excluded because they failed to provide patient samples or usable data, since they were abstracts, reviews, meta-analyses or others. And a total of 34 articles were identified as original research. Full-text articles were downloaded and carefully read for eligibility. Among them, 22 studies were excluded because of non-eligible patient samples, non-eligible experimental validations, or non-eligible outcomes. Ultimately, the searches retrieved a total of 12 studies which met the inclusion criteria to be included in the meta-analysis. All SLE patients met the diagnostic criteria of the American College of Rheumatology and Newcastle–Ottawa Quality Assessment Scale (NOS) Scores were 6–8. The characteristics of the included studies are summarized in Table 1.
Subjects were stratified in independent subgroups, and the data of each subgroup were treated as an independent study in the meta-analysis. Therefore, five relevant studies including five separate comparisons on the TNFSF4 rs1234315 polymorphism; two relevant studies including five separate comparisons on the TNFSF4 rs844648 polymorphism; eight relevant studies including ten separate comparisons on the TNFSF4 Rs2205960 polymorphism; three relevant studies including five separate comparisons on the TNFSF4 rs704840 polymorphism; two relevant studies including five separate comparisons on the TNFSF4 rs844644 polymorphism; and two relevant studies including five separate comparisons on the TNFSF4 rs10489265 polymorphism and SLE were identified, respectively. Additionally, a total of 20 separate comparisons, involving 20,114 patients and 35,136 controls (4 European, 13 Asian, 2 African American, and 1 Latin-American populations) were included in our meta-analysis. The main characteristics of each study are described in Table 2.
Meta-analysis of the association between the TNFSF4 rs2205960, rs1234315 and rs704840 polymorphisms and SLE
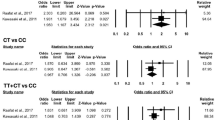
Firstly, Table 3 showed a summary of the meta-analysis findings on the association between TNFSF4 polymorphisms and SLE. When the allelic effect was examined, the meta-analysis revealed an association between the TNFSF4 rs2205960 T allele and SLE in all subjects (OR 1.42, 95% CI 1.36–1.49, P < 0.00001) (Fig. 2a). And the analysis by ethnicity stratification detected a significant association with the rs2205960 polymorphism in both the Asian-derived samples (OR 1.42, 95%CI 1.35–1.49), and the African-derived samples (OR 1.45, 95% CI 1.30–1.62). The consistency of these findings may suggest some genetic homogeneity of SLE rs2205960 SNPs among the populations. For the rs1234315 SNP, an association was also found between SLE and the T allele in the meta-analysis (OR 1.41, 95% CI 1.36–1.46, P < 0.00001) (Fig. 2b). However, owing to the limited data available in the literature, those results are all from Asian-derived samples. Similarly, as for the rs704840 SNP, an association was also found in Asian-derived samples between SLE and the G allele in the meta-analysis (OR 1.34, 95% CI 1.26–1.42, P < 0.00001) (Fig. 2c). To sum up, overall OR for the three SNPs confer a significant risk for the development of SLE.
Meta-analysis of the association between the TNFSF4 rs844644, rs844648 and rs10489265 polymorphisms and SLE
When the allelic effect was examined, the meta-analysis produced overall ORs of 0.92 (95% CI 0.70–1.21, P = 0.54) for the rs844644 polymorphism based on Asian-derived samples, European-derived samples, and Latin American-derived samples, which suggested that rs844644 SNP did not confer a significant risk for the development of SLE in those three ethnicities (Fig. 3a). The meta-analysis of rs844648 polymorphism also contained the samples from Asian, European, and Latin American. And the overall OR of rs844648 polymorphism was 1.11 (95% CI 0.86–1.43, P = 0.41) (Fig. 3b), suggesting no significant association at all. As for the rs10489265 SNP, no association was also found in Asian-derived samples between SLE and the G allele in the meta-analysis (OR 1.17, 95% CI 0.94–1.47, P = 0.17) (Fig. 3c). And the analysis by ethnicity stratification detected a significant association with the rs10489265 SNP in Asian-derived samples (OR 1.33, 95%CI 1.14–1.55, P < 0.001), but not in European-derived samples (OR 1.06, 95%CI 0.99–1.12, P = 0.11), which might suggest genetic heterogeneity of rs10489265 SNP among the populations. Due to the small number of studies available to date, it is difficult to assess this SNP in other populations. In conclusion, no statistically significant findings were observed on the association of rs844644, rs844648 and rs10489265 polymorphisms and SLE in our analysis.
Heterogeneity and publication bias
The P value of the Q test showed between-study heterogeneity in the overall analysis (Table 2). We conducted analyses using the random-effects models. In the analysis for the rs2205960 and rs704840 polymorphisms, no between-study heterogeneity was found. Therefore, the fixed-effects models were performed. Egger’s linear regression test was used to assess the publication bias. Based on our results, there was no publication bias in all comparisons.
Discussion
In the current study, we investigated whether the major confirmed genetic risk loci of TNFSF4 gene were associated with SLE susceptibility. To our knowledge, the rs1234315 and rs2205960 in the TNFSF4 gene were both identified as a genetic risk factor for SLE, which is also consist with previous reported [6]. Since the genetic determinants often show discrepancies in different ethnic populations, overall OR for the rest four SNPs: the rs844648, rs704840, rs844644 and rs10489265 polymorphisms in the TNFSF4 gene did not confer a significant risk for the development of SLE. The replication study of different populations to clarify the genetic basis of SLE is still urgently need.
The importance of TNFSF4 as a SLE susceptibility gene was firstly underlined using both a family-based and a case–control study design [25]. It revealed that there was a single risk haplotype for SLE in the upstream region of TNFSF4, which is related to the up-expression of both cell-surface TNFSF4 and the TNFSF4 transcript, probably resulting in augmenting T cell-APC interaction [25]. Consistently, several studies have demonstrated up-regulation of OX40L expression in SLE patients or SLE animal models [10, 26]. In one study the serum level of OX40L, and the percentages of OX40 + CD4 + T cells were suggested as indicators of lupus nephritis, and SLE, respectively [10]. Clement et al. reported that the frequency of blood active phenotype T follicular helper cells is increased in active SLE patients [27]. Several genes recently identified in WGA studies are components of B cell pathways, like OX4OL [28]. OX40-OX40L interaction may quantitatively enhance B cell proliferation, and augment the B cell hyperactivity, contributing to excess autoantibodies generation through promoting aberrant Tfh cells immunity response. Therefore, targeting OX40-OX40L interaction by blockade either OX40 or OX40L have the potential therapy for SLE [27]. Zhou et al. reported the therapeutic effect of anti-OX40L mAb in lupus-prone BXSB mice, with attenuation of concanavalin A (ConA)-induced proliferation, decrease of T helper cell cytokine secretion like IFN-γ and IL-6, and down-regulation of anti-dsDNA antibody production, by blocking the OX40-OX40L co-stimulatory pathway [29]. Collectively, those results confirmed a vital role of OX40L in the pathogenesis of SLE.
Polymorphisms in the TNFSF4 gene have been widely studied to assess the association with an increased risk for autoimmune diseases (ADs) susceptibility. A recent study confirmed the significant association between TNFSF4 rs1234315 polymorphisms and SLE and rheumatoid arthritis (RA) susceptibility both in allelic and genotypic levels in a Chinese Guangxi population [1]. Similarly, Zhang et al. also confirmed the association between the SNP and the SLE susceptibility [ORs = 1.45 and P = 1.5 × 10–16] by genotyping the SNPs rs1234315 near the TNFSF4 gene in 1,344 SLE patients and 4,315 controls of Chinese population [14]. Furthermore, the association was also confirmed in populations from East Asians, and Europeans [1]. However, some controversial results were also existed. Chua et al. did not find any significant correlation between alleles of TNFSF4 rs1234315 with SLE, and the OR values of the minor T allele in Indian, Chinese, and Malay populations were 1.45 (95% CI: 0.73–2.87), 1.20 (95% CI: 0.97–1.48), and 1.02 (95% CI: 0.70–1.49), respectively [8]. Besides the controversial results about rs1234315 polymorphisms, other TNFSF4 SNPs rs2205960, rs844644 or rs844648 polymorphisms also have the same situation. For example, Delgado-Vega et al. conducted replicated study in four countries including Germany, Italy, Spain and Argentina, and they found that rs844648 polymorphisms were strongly associated with SLE in the Argentineans and Italians, and displayed only weak association in the Germans, however, there was no statistical significance in the Spanish set, which was quite different from the first study they reported [20]. As SLE is distributed worldwide, some candidate gene and GWAS conducted in European- and Asian-derived SLE patients have identified several TNFSF4 SNPs conferring susceptibility to SLE [30,31,32,33], however, one study among those GWAS did not replicate this conclusion in African- and Hispanic-derived SLE patients [30]. Additionally, another GWAS carried out in Latin Americans failed to identify the association between TNFSF4 SNPs and SLE susceptibility [34]. Moreover, although two candidate gene studies which identified the association between TNFSF4 SNPs (rs2205960 and rs1234315) and SLE susceptibility included Mexican patients, the number of Mexican SLE patients was not well defined [22, 35]. To our knowledge, the disparity of those findings may be partially attributable to the existence of genetic heterogeneity of SLE among the populations. To validate the association, it is necessary to put the emphasis on replication in a larger scale of populations with different genetic backgrounds, especially the Latin Americans owing to limited data available currently. Besides, meta-analysis is recommended to augment sample size by the pooling of data from individual association studies, so that the statistical power to analyze genetic effects will be enhanced.
Accordingly, we summarized previously published related studies and performed a meta-analysis on the association of the TNFSF4 rs1234315, rs844648, rs2205960, rs704840, rs844644, rs10489265 polymorphisms and SLE susceptibility. Although detailed mechanisms of TNFSF4 SNPs in pathogenesis of SLE still need further explored, our study provided further potential evidence for TNFSF4 as a risk factor of SLE, which might possess some potential diagnostic and therapeutic implications and help to give some reference for SLE patients therapy.
Conclusions
Our meta-analysis demonstrated that the TNFSF4 rs2205960, rs1234315 and rs704840 SNPs was significantly associated with an increased risk of SLE in the overall population samples. It provides further evidence that the TNFSF4 gene plays a significant role in the etiology of SLE. However, despite those advantages, certain limitations were also existed in our meta-analysis. For instance, the number of included studies, and the investigative genotypes of the included studies were limited, so our attempt to conduct a more detailed subgroup analysis may also be limited. Therefore, further large-scale studies are needed to promote our understanding of the association between TNFSF4 polymorphisms and SLE susceptibility.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- TNFSF4:
-
Tumor necrosis factor ligand superfamily member 4
- SLE:
-
Systemic lupus erythematosus
- SNPs:
-
Single nucleotide polymorphisms
- ORs:
-
Odds ratios
- CIs:
-
Confidence intervals
- GWAS:
-
Genome-wide association studies
- APCs:
-
Antigen-presenting cells
- DCs:
-
Dendritic cells
- MA:
-
Minor allele
- MAF:
-
Minor allele frequencies
- LN:
-
Lupus nephritis
- ConA:
-
Concanavalin A
- ADs:
-
Autoimmune diseases
- RA:
-
Rheumatoid arthritis
References
Xu J, He Y, Wang J, Li X, Huang L, Li S, et al. Influence of the TNFSF4 rs1234315 polymorphism in the susceptibility to systemic lupus erythematosus and rheumatoid arthritis. Hum Immunol. 2019;80(4):270–5. https://doi.org/10.1016/j.humimm.2018.11.006.
Luan H, Li P, Cao C, Li C, Hu C, Zhang S, et al. A single-nucleotide polymorphism of the STAT4 gene is associated with systemic lupus erythematosus (SLE) in female Chinese population. Rheumatol Int. 2012;32(5):1251–5.
Teruel M, Alarcon-Riquelme ME. Genetics of systemic lupus erythematosus and Sjogren’s syndrome: an update. Curr Opin Rheumatol. 2016;28(5):506–14.
Zuo XB, Sheng YJ, Hu SJ, Gao JP, Li Y, Tang HY, et al. Variants in TNFSF4, TNFAIP3, TNIP1, BLK, SLC15A4 and UBE2L3 interact to confer risk of systemic lupus erythematosus in Chinese population. Rheumatol Int. 2014;34(4):459–64.
Mok CC, Lau CS. Pathogenesis of systemic lupus erythematosus. J Clin Pathol. 2003;56(7):481.
Lu MM, Xu WD, Yang J, Ye QL, Feng CC, Li J, et al. Association of TNFSF4 polymorphisms with systemic lupus erythematosus: a meta-analysis. Mod Rheumatol. 2013;23(4):686–93.
Lee YH, Song GG. Associations between TNFSF4 and TRAF1-C5 gene polymorphisms and systemic lupus erythematosus: a meta-analysis. Hum Immunol. 2012;73(10):1050–4.
Chua KH, Ooh YY, Chai HC. TNFSF4 polymorphisms are associated with systemic lupus erythematosus in the Malaysian population. Int J Immunogenet. 2016;43(5):303–9.
Webb GJ, Hirschfield GM, Lane PJ. OX40, OX40L and Autoimmunity: a Comprehensive Review. Clin Rev Allergy Immunol. 2016;50(3):312–32.
Farres MN, Al-Zifzaf DS, Aly AA, Abd Raboh NM. OX40/OX40L in systemic lupus erythematosus: association with disease activity and lupus nephritis. Ann Saudi Med. 2011;31(1):29–34.
Ishii N, Takahashi T, Soroosh P, Sugamura K. OX40–OX40 ligand interaction in t-cell-mediated immunity and immunopathology. 2010;105:63–98.
Sugamura K, Ishii N, Weinberg AD. Therapeutic targeting of the effector T-cell co-stimulatory molecule OX40. Nat Rev Immunol. 2004;4(6):420–31.
Zhou XJ, Lu XL, Nath SK, Lv JC, Zhu SN, Yang HZ, et al. Gene-gene interaction of BLK, TNFSF4, TRAF1, TNFAIP3, and REL in systemic lupus erythematosus. Arthritis Rheum. 2012;64(1):222–31.
Zhang SQ, Han JW, Sun LD, Lu WS, Yin XY, Zhang XJ, et al. A single-nucleotide polymorphism of the TNFSF4 gene is associated with systemic lupus erythematosus in Chinese Han population. Rheumatol Int. 2011;31(2):227–31.
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25(11):1271–7.
Hochberg MC. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725–1725.
Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, et al. Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet. 2009;41(11):1234–7.
Yang W, Shen N, Ye DQ, Liu Q, Zhang Y, Qian XX, et al. Genome-wide association study in Asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet. 2010;6(2):e1000841.
Chang YK, Yang W, Zhao M, Mok CC, Chan TM, Wong RW, et al. Association of BANK1 and TNFSF4 with systemic lupus erythematosus in Hong Kong Chinese. Genes Immun. 2009;10(5):414–20.
Delgado-Vega AM, Abelson AK, Sanchez E, Witte T, D’Alfonso S, Galeazzi M, et al. Replication of the TNFSF4 (OX40L) promoter region association with systemic lupus erythematosus. Genes Immun. 2009;10(3):248–53.
Gupta V, Kumar S, Pratap A, Singh R, Kumari R, Kumar S, et al. Association of ITGAM, TNFSF4, TNFAIP3 and STAT4 gene polymorphisms with risk of systemic lupus erythematosus in a North Indian population. Lupus. 2018;27(12):1973–9.
Sanchez E, Webb RD, Rasmussen A, Kelly JA, Riba L, Kaufman KM, et al. Genetically determined Amerindian ancestry correlates with increased frequency of risk alleles for systemic lupus erythematosus. Arthritis Rheum. 2010;62(12):3722–9.
Sanchez E, Comeau ME, Freedman BI, Kelly JA, Kaufman KM, Langefeld CD, et al. Identification of novel genetic susceptibility loci in African American lupus patients in a candidate gene association study. Arthritis Rheum. 2011;63(11):3493–501.
Orozco G, Eyre S, Hinks A, Bowes J, Morgan AW, Wilson AG, et al. Study of the common genetic background for rheumatoid arthritis and systemic lupus erythematosus. Ann Rheum Dis. 2011;70(3):463–8.
Cunninghame Graham DS, Graham RR, Manku H, Wong AK, Whittaker JC, Gaffney PM, et al. Polymorphism at the TNF superfamily gene TNFSF4 confers susceptibility to systemic lupus erythematosus. Nat Genet. 2008;40(1):83–9.
Yoshioka T, Nakajima A, Akiba H, Ishiwata T, Asano G, Yoshino SI et al. Contribution of ligand interaction to the pathogenesis of rheumatoid arthritis. Eur J Immunol 2000; 30(10):2815–2823
Jacquemin C, Schmitt N, Contin-Bordes C, Liu Y, Narayanan P, Seneschal J, et al. OX40 ligand contributes to human lupus pathogenesis by promoting T follicular helper response. Immunity. 2015;42(6):1159–70.
Manku H, Graham DSC, Vyse TJ. Association of the co-stimulator OX40L with systemic lupus erythematosus. J Mol Med. 2009;87(3):229–34.
Zhou Y-B, Ye R-G, Li Y-J, Xie C-M, Wu Y-H. Effect of anti-CD134L mAb and CTLA4Ig on ConA-induced proliferation, Th cytokine secretion, and anti-dsDNA antibody production in spleen cells from lupus-prone BXSB mice. Autoimmunity. 2008;41(5):395–404.
Langefeld CD, Ainsworth HC, Graham DSC, Kelly JA, Comeau ME, Marion MC, et al. Transancestral mapping and genetic load in systemic lupus erythematosus. Nat Commun. 2017;8:16021.
Graham DSC, Graham RR, Manku H, Wong AK, Whittaker JC, Gaffney PM, et al. Polymorphism at the TNF superfamily gene TNFSF4 confers susceptibility to systemic lupus erythematosus. Nat Genet. 2008;40:83–9.
Lee H-S, Kim T, Bang SY, Na YJ, Kim I, Kim K, et al. Ethnic specificity of lupus-associated loci identified in a genome-wide association study in Korean women. Ann Rheum Dis. 2014;73:1240.
Yang W, Shen N, Ye DQ, Liu Q, Zhang Y, Qian XX, et al. Asian Lupus Genetics, Genome-wide association study in Asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet. 2010;6:e1000841.
Alarcón-Riquelme ME, Ziegler JT, Molineros J, Howard TD, Moreno-Estrada A, Sánchez-Rodríguez E, et al. Genome-wide association study in an amerindian ancestry population reveals novel systemic lupus erythematosus risk loci and the role of european admixture. Arthrit Rheumatol. 2016;68:932–43.
Manku H, Langefeld CD, Guerra SG, Malik TH, Alarcon-Riquelme M, Anaya JM, et al. Trans-ancestral studies fine map the SLE-susceptibility locus TNFSF4. PLoS Genet. 2013;9:e1003554.
Acknowledgements
Not applicable.
Funding
This work was supported by Fundamental Research Funds for the Central Universities (7110300056).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Yu Fu; Managed the database: Yu Fu; Contributed materials/analysis tools: Qing Lin and Zhi-rong Zhang; Analyzed the data and wrote the paper: Yu Fu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fu, Y., Lin, Q. & Zhang, Zr. Association of TNFSF4 polymorphisms with systemic lupus erythematosus: a meta-analysis. Adv Rheumatol 61, 59 (2021). https://doi.org/10.1186/s42358-021-00215-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-021-00215-2