Abstract
Background
Development of novel biomarkers for multiple sclerosis (MS) is of utmost importance to improve the capability to predict disease progression and disability. Transcranial ultrasonography (TCS) is a noninvasive imaging technique that allows the visualization of major parenchymal structures. This study aimed to evaluate the role of parenchymal transcranial sonography as a predictor for disease severity and progression in MS patients. Sixty patients with clinically definite Multiple sclerosis divided into two groups, relapsing–remitting MS (RRMS) group and chronic progressive MS (CPMS) group were included.
Results
There was a statistically significant increase in the mean diameters of the third ventricle, both frontal horns of lateral ventricle in RRMS and CPMS group compared to control values, and in CPMS group compared to RRMS group. Expanded Disability Status Scale (EDSS) score was significantly positively correlated with the diameter of right frontal horn of lateral ventricle in CPMS group. Linear regression analysis revealed that diameters of right frontal horn of lateral ventricle and third ventricle were independent predictors for MS severity.
Conclusions
TCS can be used as a simple noninvasive tool for prediction of disease severity and progression in MS patients.
Similar content being viewed by others
Background
Multiple sclerosis (MS) is a chronic autoimmune–inflammatory disease of the central nervous system (CNS). Clinically, MS is characterized by a variable combination of symptoms. Demyelination can be abrupt or have an insidious onset and variable severity [1]. Large numbers of biomarkers have been tested in last years to try to predict response, disease progression, prognosis and outcome of MS. The markers are broadly divided into immunogenetic, laboratory or imaging-based [2]. Despite the diverse number of these biomarkers, they lack simplicity and clinical applicability [3]. Parenchymal Transcranial sonography (TCS) is a technique that displays the brain parenchyma and the intracranial ventricular system through the intact skull [4]. TCS has evolved as a sensitive and reliable method in measuring widths of third and lateral ventricles which was markedly widened in various primary neurodegenerative disorders [5]. The detection of central brain atrophy (accounted for by ventricular system widening) in MS has been addressed as an important determinant of clinical disease burden and was regarded as has become a clinically relevant biologic marker of MS disease process [6, 7]. Brain atrophy is evident even in the earliest stages of MS. Ventricular diameter was found to correlate well to MS duration, disease severity and disability as assessed by EDSS [8]. Hence, this study was conducted to investigate the role of parenchymal transcranial sonography (TCS) as a simple bedside predictor of disease severity and progression in MS patients.
Methods
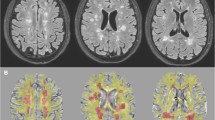
This is a cross-sectional study conducted on 60 Egyptian patients (from both sexes) with clinically definite Multiple sclerosis (according to the revised McDonald diagnostic criteria 2017) [9]. Sample size calculation was performed using G*POWER (3.1.9.7) Statistical software. Patients were recruited from neurology department and Multiple Sclerosis Unit, Cairo University hospitals, between November 2019 and January 2021. MS patients were divided into two groups: RRMS group which included 30 patients with relapsing–remitting MS and CPMS group which included 30 patients with chronic progressive MS. Exclusion criteria included: patients with a relapse in the past 3 months, patients with MS mimics as Neuro Myelitis Optica (NMOSD), Systemic Lupus Erythematosus (SLE), Sarcoidosis, patients with other medical disorders causing brain atrophy (vasculitis, recurrent strokes, uncontrolled diabetes, hypertension). Participants in this study were subjected to: (1) assessment of clinical disability: using the Expanded Disability Status Scale (EDSS) [10]. (2) B-mode transcranial sonography (TCS) for assessment of brain parenchyma. TCS was carried out at the neuro-sonology unit, of the Neurology department, Cairo University hospitals. TCS was performed by a single experienced certified neurosonographer, who was blinded to the subjects’ clinical data throughout the entire study. The study was done using a high-resolution ultrasonography instrument (PHILIPS IU22x MATRIX, California, US, L 1–5 transducer), equipped with a 2.5 MHz Phased array transducer. Via the transtemporal window, assessment was performed across the thalamic plane to assess the diameter of 3rd ventricle, right and left frontal horns of the lateral ventricle. Assessment of brain atrophy parameters was done by measurement of diameter (cm) of the third ventricle and both frontal horns of lateral ventricles. The sonographic assessment was carried through the ventricular plane (plane of the thalamus). For sonographic approach of this plane, the transducer should be upwards tilted about 20° starting from the axial midbrain plane. The landmark structure of this plane is represented by the highly echogenic pineal gland [8]. Measurements of width of the ventricles were performed if the frozen image was zoomed two to threefold from the ipsilateral to the contralateral inner layers of the hyperechogenic ependyma. Each frontal horn was assessed contralateral to the side of insonation (Rt. frontal horn is assessed via Lt trans temporal window and vice versa). For the exact site of obtaining measurements, it was recommended for the third ventricular width to measure the minimum width insonated and for the contralateral frontal horn, the width was obtained at the most frontal position at which the bilateral frontal horns were in junction [8]. In this study, we used the Egyptian cutoff values, the third ventricle diameter was considered dilated if ≥ 0.23 cm, the left frontal horn of lateral ventricle was considered dilated if > 0.37 cm, and the right frontal horn of lateral ventricle was considered dilated if > 0.36 cm [11]. Data were coded and entered using the statistical package for the Social Sciences (SPSS) version 25 (IBM Corp., released 2017, Armonk, NY, USA). Data were summarized using mean, standard deviation, median, minimum and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were done using unpaired t test in normally distributed quantitative variables, while non-parametric Mann–Whitney test was used for non-normally distributed quantitative variables. For comparing categorical data, Chi square (χ2) test was performed. Correlations between quantitative variables were done using Spearman correlation coefficient. Linear regression analysis was done to predict EDSS using significant sonar parameters. p values less than 0.05 were considered as statistically significant.
Results
The age in RRMS group ranged from 20 to 45 with a mean age 30.33 ± 7.19 years, while in CPMS group, it ranged from 20 to 47 years with a mean age 33.62 ± 7.34 years. There was no significant difference in mean age between both groups, (p = 0.104). RRMS group included 13 males (43.3%) and 17 females (56.7%), while CPMS group included 20 males (66.7%) and 10 females (33.3%), the difference in sex distribution between both groups was statistically significant (p = 0.04). The age of disease onset, duration of MS and EDSS scores of the study groups are represented in Table 1. There was a significantly longer disease duration and higher disability scores in the CPMS group compared to RRMS group (p = 0.020 and < 0.001, respectively). The range and mean of measured sonographic parameters in the studied groups are represented in Table 2. There was significant differences between the mean values of measured sonographic parameters mean in RRMS and CPMS groups compared to normal values (p < 0.001). Moreover, there was a statistically significant difference between RRMS and CPMS regarding all measured sonographic parameters (p < 0.001), as shown in Table 3. There was no correlation between EDSS score and sonographic parameters in RRMS group, while in CPMS group, EDSS scores was significantly positively correlated with the diameter of right frontal horn of lateral ventricle (r = 0.530, p = 0.008), Table 4. Linear regression analysis revealed that diameters of third ventricle and right frontal horn of lateral ventricle were independent predictors of EDSS in MS patients (p = 0.03 and < 0.001, respectively), Table 5.
Discussion
Increasing evidence has demonstrated that neuronal and axonal damage within the central nervous system (CNS) contributes substantially to the development of permanent disability in patients with MS. Characteristic reliable biomarkers for recognition of MS progression are extremely important. Recognizing biomarkers of disease progression and severity is one of the key objectives of MS-related research. The possibility to use those biomarkers would significantly facilitate clinical decisions at the stage of diagnosis and treatment. These markers, which predict the course and prognosis, will enable choosing optimum treatment and its escalation at the relevant stage [12]. Transcranial sonography allows for indirect assessment of brain atrophy by the measurement of the width of the third ventricle, which reflects an early and bedside biomarker for disease subtle progression [13]. Evidence suggests MS patients exhibit significant gray matter atrophy from the early stages of MS with significant ventricular system widening that has been detected in patients with clinically isolated syndrome [14]. Measurement of ventricular diameter has become a clinically relevant biomarker of MS disease process [6]. Assessment of ventricular diameters by TCS is a reliable tool to monitor brain atrophy and associated ventricular enlargement [15], particularly in MS patients [16]. In the present study, we found that patients with CPMS had a significant longer third ventricular and wider right and left frontal horn of lateral ventricles compared to patients with RRMS, a finding which was in accordance with Puz et al. [12]. A prospective 2-year follow-up study of patients with MS conducted by Kallman et al. [17] indicated progression of disability in patients whose third ventricle diameter was > 5 mm than those whose third ventricle width was < 5 mm at the baseline. Moreover, Schminke et al. [18] revealed a statistically significant increase in the mean diameter of the third ventricle among people with MS when measured with TCS as compared to controls. The current study revealed that measures of the third ventricle and lateral ventricles assessed by TCS were significantly correlated with EDSS scores. This was in agreement with Puz et al. [12] who reported a significant correlation between the diameters of the third ventricle and the frontal horns of the lateral ventricles, and EDSS scores among the patients with MS. Moreover, Guenter et al. [19] reported that third ventricle width measured with TCS was correlated with physical disability and cognitive performance in MS patients. In this study, linear regression analysis revealed that diameters of right frontal horn of lateral ventricles and third ventricle were independent predictors of severity of MS. To the best of our knowledge, no previous study examined this relationship.
The main limitations of this study were: the significant difference between both groups regarding sex distribution; however, previous studies addressed that female sex is clearly predominant in RRMS, with a sex ratio between 2 and 3. While in progressive MS, the sex ratio almost balances out, or sometimes male progressive cases outnumber females [20, 21]. Moreover, the effect of sex on TCS parameters is controversial and several studies reported no influence of sex on TCS measurements [22]. Another limitation was that transcranial atrophy parameters depend mainly on the quality of the temporal acoustic window and its dependency on the experience and skills of the investigator [15].
Conclusion
Parenchymal TCS can be used as simple prognostic marker for disease progression and severity in MS patients. Advantages of TCS are low costs, short investigation times, noninvasiveness, unlimited repeatability, bedside availability and lower dependency on patient’s compliance. It is supposed that frequent evaluation of brain atrophy by TCS would be of great benefit in assessing progression of the disease and following the response to a given therapy. Future research is needed to study the correlation between TCS and brain MRI findings to suggest the possibility of using TCD for early detection of disability and progression in MS patients.
Availability of data and materials
The data sets generated and/or analyzed during the current study are not publicly available due to the current Cairo University regulations and Egyptian legislation but they are available by a reasonable request from the corresponding author.
Abbreviations
- MS:
-
Multiple sclerosis
- TCS:
-
Transcranial ultrasonography
- RRMS:
-
Relapsing–remitting MS
- CPMS:
-
Chronic progressive MS patients
- EDSS:
-
Expanded Disability Status Scale
- CNS:
-
Central nervous system
- NMOSD:
-
Neuro myelitis optica spectrum disorder
- SLE:
-
Systemic lupus erythematosus
- SPSS:
-
Statistical package for the social sciences
- MRI:
-
Magnetic resonance imaging
References
Safarpour Y, Mousavi T, Jabbari B. Botulinum toxin treatment in multiple sclerosis-a review. Curr Treat Options Neurol. 2017;19(10):33.
Fernandes DB, Raza AS, Nogueira RG, Wang D, Callegaro D, Hood DC, et al. Evaluation of inner retinal layers in patients with multiple sclerosis or neuromyelitis optica using optical coherence tomography. Ophthalmology. 2013;120(2):387–94.
Harris VK, Sadiq SA. Disease biomarkers in multiple sclerosis. Mol Diagn Ther. 2009;13(4):225–44.
Walter U, Dressler D, Lindemann C, Slachevsky A, Miranda M. Transcranial sonography findings in welding-related Parkinsonism in comparison to Parkinson’s disease. Mov Disord. 2008;23(1):141–5.
Stern MB. Introductory remarks on the history and current applications of TCS. Int Rev Neurobiol. 2010;90:2–5.
Zivadinov R, Minagar A. Evidence for gray matter pathology in multiple sclerosis: a neuroimaging approach. J Neurol Sci. 2009;282(1–2):1–4.
Müller M, Esser R, Kötter K, Voss J, Müller A, Stellmes P. Third ventricular enlargement in early stages of multiple sclerosis is a predictor of motor and neuropsychological deficits: a cross-sectional study. BMJ Open. 2013;3(9): e003582.
Walter U, Wagner S, Horowski S, Benecke R, Zettl UK. Transcranial brain sonography findings predict disease progression in multiple sclerosis. Neurology. 2009;73(13):1010–7.
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–73.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
El Fayomy NM, Mohamed HH, Kamal MM, Alsayyad AH, Alsayyad EH, Shamloul RM. Signs of neuroinflammation outweigh neurodegeneration as predictors for early conversion to MS. Egypt J Neurol Psychiatr Neurosurg. 2021;57:1–6.
Puz P, Lasek-Bal A, Radecka P. Transcranial sonography of subcortical structures in patients with multiple sclerosis. Acta Neurol Scand. 2017;136(1):24–30.
Berardelli A, Wenning GK, Antonini A, Berg D, Bloem BR, Bonifati V, et al. EFNS/MDS-ES/ENS [corrected] recommendations for the diagnosis of Parkinson’s disease. Eur J Neurol. 2013;20(1):16–34.
Henry RG, Shieh M, Amirbekian B, Chung S, Okuda DT, Pelletier D. Connecting white matter injury and thalamic atrophy in clinically isolated syndromes. J Neurol Sci. 2009;282(1–2):61–6.
Becker G, Bogdahn U, Strassburg HM, Lindner A, Hassel W, Meixensberger J, Hofmann E. Identification of ventricular enlargement and estimation of intracranial pressure by transcranial color-coded real-time sonography. J Neuroimaging. 1994;4(1):17–22.
Berg D, Mäurer M, Warmuth-Metz M, Rieckmann P, Becker G. The correlation between ventricular diameter measured by transcranial sonography and clinical disability and cognitive dysfunction in patients with multiple sclerosis. Arch Neurol. 2000;57(9):1289–92.
Kallmann BA, Sauer J, Schliesser M, Warmuth-Metz M, Flachenecker P, Becker Dagger G, Rieckmann P, Mäurer M. Determination of ventricular diameters in multiple sclerosis patients with transcranial sonography (TCS)–a two year follow-up study. J Neurol. 2004;251(1):30–4.
Schminke U, Lorenz L, Kirsch M, von Sarnowski B, Khaw AV, Kessler C, Dressel A. Diameter assessment of the third ventricle with transcranial sonography in patients with multiple sclerosis. J Neuroimaging. 2010;20(1):53–7.
Guenter W, Betscher E, Bonek R. Predictive value of the third ventricle width for neurological status in multiple sclerosis. J Clin Med. 2022;11(10):2841.
Rommer PS, Ellenberger D, Hellwig K, Haas J, Pöhlau D, Stahmann A, Scientific Advisory Group of the German MS-Register by the German MS Society, et al. Relapsing and progressive MS: the sex-specific perspective. Ther Adv Neurol Disord. 2020;13:1756286420956495.
Luetic GG, Menichini ML, Vrech C, Pappolla A, Patrucco L, Cristiano E, et al. Clinical and demographic characteristics of male MS patients included in the national registry-RelevarEM. Does sex or phenotype make the difference in the association with poor prognosis? Mult Scler Relat Disord. 2022;58:103401.
Thibeault CM, Thorpe S, Canac N, Wilk SJ, Hamilton RB. Sex-based differences in transcranial Doppler ultrasound and self-reported symptoms after mild traumatic brain injury. Front Neurol. 2019;11(10):590.
Acknowledgements
The authors acknowledge subjects for their participation and cooperation in this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EMF: analyzed research idea, data acquisition, data analysis and interpretation, and manuscript writing and reviewing, HH: analyzed research idea, data acquisition, data analysis and interpretation, NM: performed TCS workup, NAM: performed data acquisition, data analysis and interpretation. RSI: analyzed research idea, data acquisition and interpretation and manuscript writing and reviewing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the research ethics committee (REC), Faculty of medicine Cairo University, Date: 8/12/2019, Code: MD-174-2019. The aim and procedures of the study were explained and written consents were taken from patients prior to participation in the study.
Consent for publication
Not applicable.
Competing interests
None of the authors has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fahmy, E., Helmy, H., Merghany, N.A. et al. Transcranial ultrasonography as a predictor of disease progression in multiple sclerosis. Egypt J Neurol Psychiatry Neurosurg 60, 16 (2024). https://doi.org/10.1186/s41983-024-00787-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-024-00787-y