Abstract
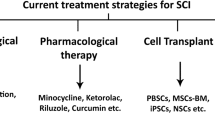
Following the traumatic spinal cord injury (SCI) and initial mechanical insult, a cascade of secondary cellular and molecular events occurs at the trauma site. This phenomenon develops a toxic lesion environment with an inhibitory effect on axonal regeneration. The complicated pathophysiology of SCI and limited central nervous system (CNS) to regeneration caused non-effective responses to drugs or beneficial treatments. Considering the necessity of SCI treatment as a critical issue in the medical field, finding novel therapeutic approaches and preclinical strategies to overcome secondary damage and functional recovery after SCI is the health system's priority. Different growth factors (GFs) are useful for treating SCI by promoting axonal regeneration and functional recovery. However, due to rapid degradation and dilution at the damaged site, direct administration of GFs is limited. In this regard, the type of delivered neurotrophic factors (NFs), administration mode, the time and location of application, and duration of treatment are critical factors in the therapy process. Also, in human studies adequate combination of NFs using cellular and viral vehicles with different tissue engineering materials is suggested to achieve satisfactory functional recovery following acute SCI. In this review, we summarize the finding of recent articles in the field of using different NFs and novel delivering systems for the treatment of SCI, which have been undertaken in rodent models.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a devastating chronic condition [1, 2]. The most serious complication following the spine injury leads to severe and dramatic dysfunction in the limbs below the injury site [3, 4]. Traumatic SCI showed extremely serious consequences; hence, despite the low rate of death following the SCI in recent years, it seems that the recovery rate of SCI is not acceptable [5]. According to literature, SCI brings great changes to patients’ life and their families and, on the other hand, brings extensive economic burdens to society and the health system [6, 7].
The pathophysiology of SCI involves two processes of primary and secondary damage. Initial traumatic events happen following the direct damage that includes disruption of neurons, axons, glia, and breakdown of the blood–spinal cord barrier. After that, the secondary damage cascade causes vascular damage, characterized by hypoxia, edema, inflammation, and oxidative stress, which leads to extensive neuronal death, demyelination, degeneration of axons, prominent glial scar formation, and cystic cavitation at the injured site in the different period [8,9,10]. Finally, these multiple adverse events resulted in irreversible injury to the spinal cord, followed by blocking nerve signal transduction and neural function retrieval [11]. The complicated pathophysiology of SCI, besides the limited spontaneous regeneration capacity through the central nervous system, resulted in a lack of the most effective drugs or beneficial treatments [12, 13]. Therefore, rehabilitation and treatment of SCI have become one of the significant issues in the medical field today [10]. So, progress in strategies of finding novel therapies to reduce determined outcomes following the secondary damage of SCI is very crucial for maintaining the remaining both sensory and motor functions.
Various neurotrophic factors effectively promote morphological and functional sparing/recovery following the SCI, which is delivered to the CNS differently. These neurotrophic factors have an active role in increasing neuronal survival, changing glia phenotype, and helping to enhance plasticity and axonal regrowth. Neurons contributing axons to different fiber systems (sensory and motor fibers) express different types of receptor [14, 15], and thus are sensitive to specific factors or special combination of factors [16]. Also, targeting the spinal cord neurons involved in various segmental or intersegmental circuits [14]. Most importantly, using different types or combinations of NTs for targeting glial cells could effectively attenuate the adverse effects of inflammation and scarring and promote remyelination [17]. At different times after SCI, an alteration in the expression of neurotrophic factors, chemokines, cytokines, and receptors in different neurons and glid was observed [18]. The fact of alteration of receptor expression based on place and time and sensitivity to different types of molecules play a crucial role in designing therapies based on neurotrophic factors [19].
Nerve growth factor (NGF) use in SCI
Nerve growth factor (NGF) is considered the earliest cell growth regulator found, which has a critical role in neuronal development, axonal growth, cellular apoptosis, and neurotransmitter synthesis [20]. Furthermore, NGF has a prominent role in inhibiting the apoptosis induced by cellular oxidative stress or toxicity [21]. Pathways involved in NGF-mediated neurogenesis and neuroprotection are intracellular phosphatidylinositol-3 kinase (PI3K)/Akt and mitogen-activated protein kinase (MAPK) pathways through the TrkA receptor [22]. The neuroprotective and neurotrophic ability of NGF is impaired in pathological conditions, followed by a reduction in the endogenous level. At the same time, its amount is preserved in the distal area of injury [23, 24]. In this context, NGF and all other neurotrophins are considered critical and promising therapeutic factors for the regeneration of neurons in various CNS disorders like stroke, Lou Gehrig’s disease, Alzheimer’s disease, and most notably in the SCI [25].
Previous studies reported that NGF has a crucial neuroprotective impact on SCI and promotes spinal cord recovery [21]. In the recent decade, many studies used exogenous neurotrophins to promote nerve regeneration by injecting them into lesion sites [26, 27]. However, temperature alteration, acidity, and alkalinity affect the NGF activity. Also, it is inactive in an aqueous solution, and biological enzymes degrade it in vivo. In addition, penetrating the blood–brain barrier (BBB) to reach the damaged site is difficult for NGF, so it is a limitation to applying the NGF [28]. So, founding a novel strategy for getting the NGF to the lesion site is the priority of most researchers to deliver it to the final target.
The study tried by Xia and colleagues [28], attempted to prepare NGF encapsulated by nanovesicles (NGF-NVs) designed by the macrophage RAW264 cell membrane to treat SCI. They showed that NGF-NVs had good targeting with a significant protective effect on neurons after SCI by activating PI3K/AKT signaling pathway. In recent research, transplanted genetically modified adipose-derived mesenchymal stem cells (ADSCs) most frequently have been used to deliver NGF at the injured site of the spinal cord to induce neuronal growth responses and repair it. Nevertheless, the healing procedure following transplantation of genetically modified cells is directly related to the sufficient secretion of NGF and potential activity along the regeneration period [29, 30]. Previous literature proposes treatment strategies based on tissue engineering and regenerative medicine as an alternative therapy for SCI. One of the novel promising approaches for the treatment of SCI is delivering of NTFs by genetically engineered MSCs in combination with biocompatible materials as a 3D-scaffold or cell-carrying biomaterials [31, 32]. Alizadeh and colleagues [33], used nerve growth factor (NGF)-overexpressing of human adipose-derived mesenchymal stem cells (hADSCs) encapsulated in injectable chitosan/β-glycerophosphate/hydroxyethylcellulose hydrogel for evaluating its effect on SCI regeneration. The results showed that it could repair the injured spinal cord and recover locomotor function.
In the novel delivery system, Xu and colleagues [34], used encapsulated NGF into nanoparticles (NPs) [n(NGF)] methacryloyloxyethyl phosphorylcholine to provide a CNS targeting approach in healthy mice after intravenous injection. For this purpose, PC12 cells, a neural cell line usually used to model CNS tissue in vitro, were treated with native NGF and NGF NPs to evaluate the NGF activity released from these nano-capsules. Following NGF release from NPs, a progressive differentiation and neurite outgrowth of these cells were observed in the intracellular pathways. After 21 days, a therapeutic benefit of n(NGF) was observed in a mouse model of compression-induced acute SCI. A significant functional recovery in locomotion without inducing the proinflammatory reactions and extended blood circulation half-life was reported in this study. The result of the investigations on neurogenesis effects of a novel polydopamine / polylactic acid-glycolic acid copolymer (PLGA)/ NGF (PDA-PLGA/NGF) nerve scaffold showed that this scaffold significantly induces the proliferation and neuronal differentiation of NSCs in vitro. Furthermore, following the scaffold implantation into the transected spinal cord of a rat led to a progressive recovery of nerve function [35]. Recovery of SCI is a multifactorial process that needs multiple growth factors (GFs) to participate in the tissue regeneration process. Hu and colleagues developed a delivery system based on GFs, consisting of nerve growth factor (NGF), basic fibroblast growth factor (bFGF), and heparin-poloxamer (HP) hydrogel. A continuous release of NGF and bFGF from HP following the single injection into the lesioned spinal cord could have a significant effect on improving the neuronal survival, axonal regeneration, suppressing the process of reactive astrogliosis, and recovery of locomotor function in comparison to free GFs or HP treatment [36]. Wu and colleagues [37], in the study on barrier-penetrating liposome targeted delivery of bFGF for repairing SCI, showed that bFGF-loaded dual-targeting liposome (bFGF@Lip-Cp&Rp) promote angiogenesis, BSCB repair, and M2 macrophages polarization. Moreover, a recovery of motor function was reported in SCI rats.
Yang and colleagues [38], in research on the function of polycaprolactone/gelatin (PCL/GE) composite fiber scaffold with NGF in the recovery of SCI, showed significant progress in motor and neurological functions in the hind limbs of SCI rats. Also, they reported an improvement in bladder dysfunction and recovery of axonal transport. They conclude that CL/GE composite fiber scaffold could upregulate GAP43 and NF200 levels in SCI site tissues. In addition to chemical intervention in improving SCI, some physical interventions like electrical and magnetic stimulation showed acceptable results with various effects on nerve damage in acute and chronic injuries. Overall, the biological basis of this intervention relies on protein synthesis, regulation of ion channels and growth factor secretion (Table 1).
Brain-derived neurotrophic factor (BDNF) uses in SCI
Brain-derived neurotrophic factor (BDNF) is one of the best-studied neurotrophic factors and has been shown to promote the growth, differentiation, survival, and synaptogenesis of central and peripheral neurons [39, 40]. BDNF exerts its physiological and pathological functions through two receptors: tropomyosin receptor kinase B (TrkB), which is a high affinity, and the p75 neurotrophin receptor (p75NTR), with low affinity. The ligand‐specific receptors of BDNF are widely distributed in many neurons in the spinal cord and primary afferent pathways [41]. BDNF binding to the TrkB receptor triggers several events, including TrkB receptor dimerization and autophosphorylation. So, it stimulates intracellular signaling cascades such as mitogen-activated protein kinase (MAPK), phospholipase C-γ, and phosphatidylinositol-3 kinase. Activation of these pathways causes a wide range of cellular actions, including synaptic modulation and neuroplasticity, cell survival, axonal elongation, and neurite outgrowth [42, 43]. Similarly, the activation of p75NTR produces various cellular events, neuronal differentiation, and the protection of neurons against apoptosis [44]. In addition, BDNF has been shown to mediate inflammatory and peripheral injury-induced pain. BDNF levels in the bladder and spinal of mice were significantly increased 4 weeks after SCI [45].
Neuroprotection and regeneration facilitated by the administration of exogenous neurotrophic growth factors have been considered a potential treatment for SCI. Ample literature confirmed that BDNF is an eminent candidate in spinal cord repair. Crowley and colleagues showed that injection of a single dose of BDNF mRNA nanomicelles prepared with polyethylene glycol polyamine acid block copolymer into the injured tissue mouse model of contusion SCI could improve motor function recovery and increase higher expression of the anti-inflammatory factors [46]. Noteworthy is a study by Ji and colleagues in which treatment with BDNF and neurotrophin-3 overexpression by adipose-derived stem cells combined with silk fibroin/chitosan scaffold were significantly increased BBB scores and formation of nerve fibers and were alleviated the injured morphology and pathological changes. Also, they found that GAP-43 expression significantly increased, while glial fibrillary acidic protein (GFAP) and caspase-3 expression significantly decreased in the rat SCI model [47]. Several studies reported that BDNF treatment leads to neuroprotection and promotion of regeneration and sprouting of axonal fibers [48]. Moreover, it was revolved in later research that BDNF suppressed apoptosis in neurons and oligodendrocytes following SCI [49, 50]. The results also revealed that BDNF is involved in regulating the immune response and has potent antioxidative effects after SCI [51]. In most studies, exogenously applied BDNF increases myelination [52] and diminishes atrophy of cortical, rubrospinal, and spinal neurons [53, 54]. Abdanipour and colleagues [55], showed that the use of lithium chloride in the spinal contusion rat model could effectively enhance locomotor function by increasing BDNF/TrkB expression and decreasing apoptosis cell death.
Recently, Cell-based therapies are gaining increasing attention for the treatment of SCI through the promotion of neurotrophic factors, especially BDNF. The acute phase of SCI is characterized by a pathophysiological cascade of events that result in neuronal loss in the gray matter through inflammatory and excitotoxic pathways. A study has been demonstrated that transplantation of boundary-cap derived neural crest stem cells to spinal cord neurons injured by N-methyl-D-aspartate (NMDA) exerted neuroprotective, anti-apoptotic, and anti-inflammatory (suppressed activation of both microglial cells and astrocytes) effects on SCI by secretion of BDNF [56]. BDNF is known to protect against excitotoxic damage by reducing NMDA-receptor signaling [57]. In another combinational treatment approach, Chen and colleagues showed that the transplantation of human urine stem cells combined with chondroitinase ABC into the impaired spinal cord promoted motor functional recovery as compared to controls which may be related to increased levels of BDNF and NGF [58].
Increased BDNF by exercise facilitated the recovery of motor function in patients with incomplete SCI [59]. In addition, several studies reported that treadmill exercise improved functional recovery by increasing BDNF and phosphorylated extracellular signal-regulated kinases 1/2 (p-ERK1/2) levels after SCI in rats [60, 61]. In a study by Kim and colleagues a combination of bone marrow stromal cells (BMSCs) transplantation (5 × 106 cell) with treadmill exercise (6 weeks) markedly reduced apoptosis and upregulated BDNF and TrkB expressions in the injured spinal cord. They found that the synergistic effect of treadmill exercise and BMSCs against SCI is through the activation of the BDNF-ERK1/2 pathway [62].
A biocompatible cell-penetrating peptide, KAFAKLAARLYRKALARQLGVAA (KAFAK), is known as an ideal biomaterial suppressing the syntheses of proinflammatory cytokines and tumor necrosis factor (TNF)-α through mitogen-activated protein kinase–activated protein kinase 2 after SCI [63]. It has been found that injection of KAFAK and BDNF via a hyaluronan-methylcellulose (HAMC) hydrogel delivery system into the injured site of the spinal cord decreased astrocyte reactive hyperplasia, cystic cavity, and inflammation in the lesion site. Moreover, this composite HAMC-KAFAK/BDNF hydrogel promoted neuronal survival and functional recovery as well as enhanced axonal regeneration [64]. Also, treatment with human neural stem cells overexpressing BDNF could effectively improve locomotor by an increased volume of spared myelination and decreased area of the cystic cavity. Human neural stem cells overexpressing BDNF therapy modulated inflammatory cells and glia activation and also improved the hyperalgesia following SCI [65].
Electrical stimulation is a physical therapy technique that promotes neurogenesis and recovery of function following central nervous system (CNS) injury [66]. Besides, electrical stimulation has a potential regenerative role in increasing the formation of newborn cells after SCI in animals expressing neural progenitor cell‐associated markers [67]. After SCI, applying epidural subthreshold electrical stimulation (0.3–0.6 mA, 0.1 ms, 100 Hz) at the T10 segment of SCI for 2 weeks increased protein levels of BDNF in rats [68].
Glial cell line-derived neurotrophic factor (GDNF) use in SCI
Glial cell line-derived neurotrophic factor (GDNF) belongs to the transforming growth factor-β superfamily, which is known to affect many aspects of neural development. The receptor for this factor is a multi-component complex that includes the molecule transfection (RET) tyrosine kinase receptor and one of two glycosylphosphatidylinositol (GPI)-linked ligand-binding components called GDNF family receptor alphas (GFRα-1 and GFRα-2) [69]. These receptors are found in the ventral horn of the spinal cord, the compacta region of the substantia nigra, thalamus, and hypothalamus [70]. GDNF is a potent survival factor for midbrain dopaminergic neurons and noradrenergic neurons of the locus coeruleus and also a survival factor for spinal motor neurons. It was shown to modulate astrogliosis [71].
GDNF is vital for peripheral nervous system development and has been shown to enhance functional recovery and promote axon regeneration. It has been reported that a combinational approach consisting of hydrogel scaffolds containing Schwann cells (SC) that overexpressed GDNF promoted regional axon regeneration, remyelination, and functional improvement after spinal cord transection in rats [72]. Moreover, it has been observed that polysialylation enhances the integration and migration of transplanted SC and GDNF delivery to permit entering astrocytes to SC grafts and consequently improve integration [73]. Jiao and colleagues examined the role of silk fibroin/alginate GDNF scaffold seeded with human umbilical cord MSCs (hUCMSCs) for a thoracic contusion injury in a rat model. They found that treatment with the hUCMSCs on silk fibroin/alginate GDNF composite scaffolds for 2 months led to functional improvement, neuroprotection, increased neuronal markers expression, and decreased expression of inflammatory cytokines [74].
Lu and colleagues, used placental-derived mesenchymal stem cells (PMSCs) plus GDNF versus bone marrow-derived MSCs (BMSCs) plus GDNF accompanied by copolymer scaffolds. There was no significant difference between group PMSCs expressing GDNF compared to BMSCs expressing GDNF in their SCI repair capability. Interestingly, the transfer of GDNF promotes the ability of these cells for SCI repair [75]. Similarly, combination therapy, including emu oil-loaded polycaprolactone/collagen electrospun scaffolds + GDNF overexpressing adipose-derived stem cells reduced the cavity size, glial scar formation, and axonal demyelination while improved locomotor recovery following contusive SCI in rats [76].
Neurotrophin-3 (NT-3) use in SCI
Neurotrophin-3 (NT-3) can promote developing neurons' survival, proliferation, and differentiation. NT-3 promotes sprouting of spared axons and injured axons regeneration after damage [77]. Besides, it amplifies the oligodendrocyte progenitor’s proliferation in vivo [78]. NT-3 has been shown directly bind to tropomyosin kinase receptor type C (TrkC) with high affinity. Nevertheless, it can also activate less efficiently the other Trk receptors [79]. It can also signal through the promiscuous neurotrophin receptor p75, which generates both pro-survival and pro-apoptotic states [80]. The level of NT3 and its receptors is extremely reduced following a few days post-SCI [81].
In the early stage of SCI, increased levels of autophagy cause irreversible neuron injury, hindering the recovery of motor function, and inhibition of autophagy overexpression in neural cells contributes to locomotor function recovery [82]. Intraspinal administration of NT-3 promoted oligodendrocyte proliferation and nerve function recovery after SCI via inhibiting autophagy. Rapamycin, an autophagy activator, reduced the effects of NT-3 on oligodendrocyte survival [83].
It has been demonstrated that NT-3 decreases the death of oligodendrocytes after SCI [84]. It was found that the glucose content, creatinine, and Na + were increased, while the K + content was decreased in the SCI group. Treatment with NT-3 reversed them. Additionally, it has been proved that treatment with NT-3 reduces myeloperoxidase activity and content of IL-1, IL-6, and tumor necrosis factor-β, indicating that NT-3 inhibits inflammatory response caused by SCI. This protective effect of NT-3 on SCI mediates through the mitogen-activated protein kinase signaling pathway [85]. Sun and colleagues, found that NT-3-loaded multichannel nanofibrous scaffolds promoted anti-inflammation, neuronal differentiation, and functional recovery after SCI [86]. Positive effects of NT-3 on myelination have been reported, possibly related to infiltrating SC [84, 87].
In recent studies, other ways of functional improvement following SCI have been demonstrated. In the research conducted by Lu and colleagues [88], they used a combination of pro-regenerative therapies and rehabilitation for SCI rats and reported a significantly greater functional and anatomical recovery than alone treatment after SCI. Another study showed that after administration of orally bioavailable and specific inhibitor AZD1236, a drug developed by AstraZeneca, within 24 h after SCI and for only 3 days, reduced secondary damage post-SCI. AZD1236 led to suppression of SCI‐ induced edema, neuropathic pain, BSCB breakdown, and infiltration of macrophages into the lesion site. Furthermore, it has a beneficial effect on the improvement of electrophysiological, sensory, and locomotor function, and most importantly, axon regeneration [89].
Conclusion
Considering the importance of NFs in the treatment process and healing of the lesion site in the SCI and limitation in direct administration, providing novel delivery systems to get the best therapeutic outcome is the priority in SCI treatment. Regarding this issue, this review tried to evaluate the administration mode, timing, location, and type of the used NFs and type of SCI models in recent literature. Generally, most studies report significant success in improving SCI if NFs applied in or close to the injured site after SCI and during the acute phase of injury. The research discussed various strategies of delivering systems, including osmotic minipumps, hydrogels, scaffolds, cell-mediated delivery, polymer release vehicles, encapsulated NFs in NPs, and gene therapy to modify neuron glial cells or precursor/stem cells.
Availability of data and materials
Not applicable.
References
Abolhasanpour N, Eidi A, Hajebrahimi S, Reyhani-Rad S, Hashim H. Effect of cerebrolysin on bladder function after spinal cord injury in female Wistar rats. Int J Urol. 2019;26(9):917–23.
Salehi-Pourmehr H, Nouri O, Naseri A, Roshangar L, Rahbarghazi R, Sadigh-Eteghad S, et al. Clinical application of stem cell therapy in neurogenic bladder: a systematic review and meta-analysis. Int Urogynecol J. 2022;33(8):2081–97.
O’Shea TM, Burda JE, Sofroniew MV. Cell biology of spinal cord injury and repair. J Clin Investig. 2017;127(9):3259–70.
Abolhasanpour N, Hajebrahimi S, Ebrahimi-Kalan A, Mehdipour A, Salehi-Pourmehr H. Urodynamic parameters in spinal cord injury-induced neurogenic bladder rats after stem cell transplantation: a narrative review. Iran J Med Sci. 2020;45(1):2–15.
Assinck P, Duncan GJ, Hilton BJ, Plemel JR, Tetzlaff W. Cell transplantation therapy for spinal cord injury. Nat Neurosci. 2017;20(5):637–47.
Dias DO, Kim H, Holl D, Solnestam BW, Lundeberg J, Carlén M, et al. Reducing pericyte-derived scarring promotes recovery after spinal cord injury. Cell. 2018;173(1):153–65.
Salehi-Pourmehr H, Rahbarghazi R, Mahmoudi J, Roshangar L, Chapple CR, Hajebrahimi S, et al. Intra-bladder wall transplantation of bone marrow mesenchymal stem cells improved urinary bladder dysfunction following spinal cord injury. Life Sci. 2019;221:20–8.
Mothe AJ, Tam RY, Zahir T, Tator CH, Shoichet MS. Repair of the injured spinal cord by transplantation of neural stem cells in a hyaluronan-based hydrogel. Biomaterials. 2013;34(15):3775–83.
Yong CS, Choi JS, Quan Q-Z, Rhee J-D, Kim C-K, Lim S-J, et al. Effect of sodium chloride on the gelation temperature, gel strength and bioadhesive force of poloxamer gels containing diclofenac sodium. Int J Pharm. 2001;226(1–2):195–205.
Moon YJ, Lee JY, Oh MS, Pak YK, Park KS, Oh TH, et al. Inhibition of inflammation and oxidative stress by Angelica dahuricae radix extract decreases apoptotic cell death and improves functional recovery after spinal cord injury. J Neurosci. 2012;90(1):243–56.
An Y, Tsang KK, Zhang H. Potential of stem cell based therapy and tissue engineering in the regeneration of the central nervous system. Biomed Mater. 2006;1(2):R38.
Silver J, Schwab ME, Popovich PG. Central nervous system regenerative failure: role of oligodendrocytes, astrocytes, and microglia. Cold Spring Harb Perspect Biol. 2015;7(3): a020602.
Tator CH. Review of treatment trials in human spinal cord injury: issues, difficulties, and recommendations. Neurosurgery. 2006;59(5):957–87.
Boyce VS, Mendell LM. Neurotrophins and spinal circuit function. Front Neural Circuits. 2014;8:59.
Hollis ER, Tuszynski MH. Neurotrophins: potential therapeutic tools for the treatment of spinal cord injury. Neurotherapeutics. 2011;8(4):694–703.
Blesch A, Fischer I, Tuszynski MH. Gene therapy, neurotrophic factors and spinal cord regeneration. Handb Clin Neurol. 2012;109:563–74.
Plemel JR, Keough MB, Duncan GJ, Sparling JS, Yong VW, Stys PK, et al. Remyelination after spinal cord injury: is it a target for repair? Prog Neurobiol. 2014;117:54–72.
Hougland MT, Harrison BJ, Magnuson DS, Rouchka EC, Petruska JC. The transcriptional response of neurotrophins and their tyrosine kinase receptors in lumbar sensorimotor circuits to spinal cord contusion is affected by injury severity and survival time. Front Physiol. 2013;3:478.
Hodgetts S, Harvey A. Neurotrophic factors used to treat spinal cord injury. Vitam Horm. 2017;104:405–57.
Salinas M, Diaz R, Abraham NG, de Galarreta CMR, Cuadrado A. Nerve growth factor protects against 6-hydroxydopamine-induced oxidative stress by increasing expression of heme oxygenase-1 in a phosphatidylinositol 3-kinase-dependent manner. J Biol Chem. 2003;278(16):13898–904.
Zhang H, Wu F, Kong X, Yang J, Chen H, Deng L, et al. Nerve growth factor improves functional recovery by inhibiting endoplasmic reticulum stress-induced neuronal apoptosis in rats with spinal cord injury. J Transl Med. 2014;12(1):1–15.
Diering GH, Numata Y, Fan S, Church J, Numata M. Endosomal acidification by Na+/H+ exchanger NHE5 regulates TrkA cell-surface targeting and NGF-induced PI3K signaling. Mol Biol Cell. 2013;24(21):3435–48.
Anand P, Terenghi G, Warner G, Kopelman P, Williams-Chestnut R, Sinicropi D. The role of endogenous nerve growth factor in human diabetic neuropathy. Nat Med. 1996;2(6):703–7.
Anand P, Terenghi G, Birch R, Wellmer A, Cedarbaum JM, Lindsay RM, et al. Endogenous NGF and CNTF levels in human peripheral nerve injury. NeuroReport. 1997;8(8):1935–8.
Weissmiller AM, Wu C. Current advances in using neurotrophic factors to treat neurodegenerative disorders. Transl Neurodegener. 2012;1(1):1–9.
Gordon T. The physiology of neural injury and regeneration: the role of neurotrophic factors. J Commun Disord. 2010;43(4):265–73.
Li R, Wu J, Lin Z, Nangle MR, Li Y, Cai P, et al. Single injection of a novel nerve growth factor coacervate improves structural and functional regeneration after sciatic nerve injury in adult rats. Exp Neurol. 2017;288:1–10.
Xia N, Gao Z, Hu H, Li D, Zhang C, Mei X, et al. Nerve growth factor loaded macrophage-derived nanovesicles for inhibiting neuronal apoptosis after spinal cord injury. J Biomater Appl. 2021;36(2):276–88.
Zarrinpour V, Hajebrahimi Z, Jafarinia M. Expression pattern of neurotrophins and their receptors during neuronal differentiation of adipose-derived stem cells in simulated microgravity condition. Iran J Basic Med Sci. 2017;20(2):178.
Nagahara AH, Bernot T, Moseanko R, Brignolo L, Blesch A, Conner JM, et al. Long-term reversal of cholinergic neuronal decline in aged non-human primates by lentiviral NGF gene delivery. Exp Neurol. 2009;215(1):153–9.
Boido M, Ghibaudi M, Gentile P, Favaro E, Fusaro R, Tonda-Turo C. Chitosan-based hydrogel to support the paracrine activity of mesenchymal stem cells in spinal cord injury treatment. Sci Rep. 2019;9(1):1–16.
Mu M, Li X, Tong A, Guo G. Multi-functional chitosan-based smart hydrogels mediated biomedical application. Expert Opin Drug Deliv. 2019;16(3):239–50.
Alizadeh A, Moradi L, Katebi M, Ai J, Azami M, Moradveisi B, et al. Delivery of injectable thermo-sensitive hydrogel releasing nerve growth factor for spinal cord regeneration in rat animal model. J Tissue Viability. 2020;29(4):359–66.
Xu D, Wu D, Qin M, Nih LR, Liu C, Cao Z, et al. Efficient delivery of nerve growth factors to the central nervous system for neural regeneration. Adv Mater. 2019;31(33):1900727.
Pan S, Zhao Y, Qiao X, Qi Z, Fu C, Kong W, et al. PLGA porous scaffolds by polydopamine-assisted immobilization of NGF for spinal cord injury repair. Mater Res Express. 2019;6(4): 045024.
Hu X, Li R, Wu Y, Li Y, Zhong X, Zhang G, et al. Thermosensitive heparin-poloxamer hydrogel encapsulated bFGF and NGF to treat spinal cord injury. J Cell Mol Med. 2020;24(14):8166–78.
Wu F, Wang P, Wei X, Yang Y, Al Mamun A, Zhang X, et al. Barrier-penetrating liposome targeted delivery of basic fibroblast growth factor for spinal cord injury repair. Mater Today Bio. 2023;18:100546.
Yang S, Zhang N, Dong Y, Zhang X. Research on polycaprolactone-gelatin composite scaffolds carrying nerve growth factor for the repair of spinal cord injury. Dis Markers. 2022;2022:1.
Ruitenberg MJ, Blits B, Dijkhuizen PA, te Beek ET, Bakker A, van Heerikhuize JJ, et al. Adeno-associated viral vector-mediated gene transfer of brain-derived neurotrophic factor reverses atrophy of rubrospinal neurons following both acute and chronic spinal cord injury. Neurobiol Dis. 2004;15(2):394–406.
Kwon BK, Liu J, Lam C, Plunet W, Oschipok LW, Hauswirth W, et al. Brain-derived neurotrophic factor gene transfer with adeno-associated viral and lentiviral vectors prevents rubrospinal neuronal atrophy and stimulates regeneration-associated gene expression after acute cervical spinal cord injury. Spine. 2007;32(11):1164–73.
Garraway SM, Huie JR. Spinal plasticity and behavior: BDNF-induced neuromodulation in uninjured and injured spinal cord. Neural Plast. 2016;2016:9857201.
Wang X, Ratnam J, Zou B, England PM, Basbaum AI. TrkB signaling is required for both the induction and maintenance of tissue and nerve injury-induced persistent pain. J Neurosci. 2009;29(17):5508–15.
Blum R, Konnerth A. Neurotrophin-mediated rapid signaling in the central nervous system: mechanisms and functions. Physiology. 2005;20(1):70–8.
Jeronimo A, Diogenes M, Ribeiro J, Sebastiao A, editors. BDNF effect upon apoptosis induced by amyloid-beta peptide: changes in TRKB receptors expression. Front Neurosci Conference Abstract: 11th Meeting of the Portuguese Society for Neuroscience https://doi.org/10.3389/conf neuro; 2009.
Wada N, Shimizu T, Shimizu N, Kurobe M, de Groat WC, Tyagi P, et al. Therapeutic effects of inhibition of brain-derived neurotrophic factor on voiding dysfunction in mice with spinal cord injury. Am J Physiol Ren Physiol. 2019;317(5):F1305–10.
Crowley ST, Fukushima Y, Uchida S, Kataoka K, Itaka K. Enhancement of motor function recovery after spinal cord injury in mice by delivery of brain-derived neurotrophic factor mRNA. Mol Ther Nucleic Acids. 2019;17:465–76.
Ji W-C, Li M, Jiang W-T, Ma X, Li J. Protective effect of brain-derived neurotrophic factor and neurotrophin-3 overexpression by adipose-derived stem cells combined with silk fibroin/chitosan scaffold in spinal cord injury. Neurol Res. 2020;42(5):361–71.
Jin Y, Fischer I, Tessler A, Houle JD. Transplants of fibroblasts genetically modified to express BDNF promote axonal regeneration from supraspinal neurons following chronic spinal cord injury. Exp Neurol. 2002;177(1):265–75.
Koda M, Murakami M, Ino H, Yoshinaga K, Ikeda O, Hashimoto M, et al. Brain-derived neurotrophic factor suppresses delayed apoptosis of oligodendrocytes after spinal cord injury in rats. J Neurotrauma. 2002;19(6):777–85.
Nakajima H, Uchida K, Yayama T, Kobayashi S, Guerrero AR, Furukawa S, et al. Targeted retrograde gene delivery of brain-derived neurotrophic factor suppresses apoptosis of neurons and oligodendroglia after spinal cord injury in rats. Spine. 2010;35(5):497–504.
Ji X-C, Dang Y-Y, Gao H-Y, Wang Z-T, Gao M, Yang Y, et al. Local injection of Lenti–BDNF at the lesion site promotes M2 macrophage polarization and inhibits inflammatory response after spinal cord injury in mice. Cell Mol Neurobiol. 2015;35(6):881–90.
Zhao T, Yan W, Xu K, Qi Y, Dai X, Shi Z. Combined treatment with platelet-rich plasma and brain-derived neurotrophic factor-overexpressing bone marrow stromal cells supports axonal remyelination in a rat spinal cord hemi-section model. Cytotherapy. 2013;15(7):792–804.
Brock JH, Rosenzweig ES, Blesch A, Moseanko R, Havton LA, Edgerton VR, et al. Local and remote growth factor effects after primate spinal cord injury. J Neurosci. 2010;30(29):9728–37.
Sasaki M, Radtke C, Tan AM, Zhao P, Hamada H, Houkin K, et al. BDNF-hypersecreting human mesenchymal stem cells promote functional recovery, axonal sprouting, and protection of corticospinal neurons after spinal cord injury. J Neurosci. 2009;29(47):14932–41.
Abdanipour A, Moradi F, Fakheri F, Ghorbanlou M, Nejatbakhsh R. The effect of lithium chloride on BDNF, NT3, and their receptor mRNA levels in the spinal contusion rat models. Neurol Res. 2019;41(6):577–83.
Schizas N, König N, Andersson B, Vasylovska S, Hoeber J, Kozlova E, et al. Neural crest stem cells protect spinal cord neurons from excitotoxic damage and inhibit glial activation by secretion of brain-derived neurotrophic factor. Cell Tissue Res. 2018;372(3):493–505.
Lau D, Bengtson CP, Buchthal B, Bading H. BDNF reduces toxic extrasynaptic NMDA receptor signaling via synaptic NMDA receptors and nuclear-calcium-induced transcription of inhba/activin A. Cell Rep. 2015;12(8):1353–66.
Chen H, Li J, Yan H. The transplantation of human urine stem cells combined with chondroitinase ABC promotes brain-derived neurotrophic factor and nerve growth factor following spinal cord injury in rats. Int J Clin Exp Pathol. 2018;11(8):3858.
Leech KA, Hornby TG. High-intensity locomotor exercise increases brain-derived neurotrophic factor in individuals with incomplete spinal cord injury. J Neurotrauma. 2017;34(6):1240–8.
Oh M-J, Seo TB, Kwon K-B, Yoon S-J, Elzi DJ, Kim BG, et al. Axonal outgrowth and Erk1/2 activation by training after spinal cord injury in rats. J Neurotrauma. 2009;26(11):2071–82.
Jung S-Y, Seo T-B, Kim D-Y. Treadmill exercise facilitates recovery of locomotor function through axonal regeneration following spinal cord injury in rats. J Exerc Rehabil. 2016;12(4):284.
Kim Y-M, Jin J-J, Lee S-J, Seo T-B, Ji E-S. Treadmill exercise with bone marrow stromal cells transplantation facilitates neuroprotective effect through BDNF-ERK1/2 pathway in spinal cord injury rats. J Exerc Rehabil. 2018;14(3):335.
Brugnano JL, Chan BK, Seal BL, Panitch A. Cell-penetrating peptides can confer biological function: regulation of inflammatory cytokines in human monocytes by MK2 inhibitor peptides. J Control Release. 2011;155(2):128–33.
He Z, Zang H, Zhu L, Huang K, Yi T, Zhang S, et al. An anti-inflammatory peptide and brain-derived neurotrophic factor-modified hyaluronan-methylcellulose hydrogel promotes nerve regeneration in rats with spinal cord injury. Int J Nanomed. 2019;14:721.
Chang D-J, Cho H-Y, Hwang S, Lee N, Choi C, Lee H, et al. Therapeutic effect of BDNF-overexpressing human neural stem cells (F3 BDNF) in a contusion model of spinal cord injury in rats. Int J Mol Sci. 2021;22(13):6970.
Huang Y, Li Y, Chen J, Zhou H, Tan S. Electrical stimulation elicits neural stem cells activation: new perspectives in CNS repair. Front Hum Neurosci. 2015;9:586.
Becker D, Gary DS, Rosenzweig ES, Grill WM, McDonald JW. Functional electrical stimulation helps replenish progenitor cells in the injured spinal cord of adult rats. Exp Neurol. 2010;222(2):211–8.
Ghorbani M, Shahabi P, Karimi P, Soltani-Zangbar H, Morshedi M, Bani S, et al. Impacts of epidural electrical stimulation on Wnt signaling, FAAH, and BDNF following thoracic spinal cord injury in rat. J Cell Physiol. 2020;235(12):9795–805.
Eigenbrot C, Gerber N. X-ray structure of glial cell-derived neurotrophic factor at 1.9 A resolution and implications for receptor binding. Nat Struct Biol. 1997;4(6):435–8.
Walker MJ, Xu X-M. History of glial cell line-derived neurotrophic factor (GDNF) and its use for spinal cord injury repair. Brain Sci. 2018;8(6):109.
Deng L-X, Hu J, Liu N, Wang X, Smith GM, Wen X, et al. GDNF modifies reactive astrogliosis allowing robust axonal regeneration through Schwann cell-seeded guidance channels after spinal cord injury. Exp Neurol. 2011;229(2):238–50.
Chen BK, Madigan NN, Hakim JS, Dadsetan M, McMahon SS, Yaszemski MJ, et al. GDNF Schwann cells in hydrogel scaffolds promote regional axon regeneration, remyelination and functional improvement after spinal cord transection in rats. J Tissue Eng Regen Med. 2018;12(1):e398–407.
Zipser CM, Cragg JJ, Guest JD, Fehlings MG, Jutzeler CR, Anderson AJ, et al. Cell-based and stem-cell-based treatments for spinal cord injury: evidence from clinical trials. Lancet Neurol. 2022;21:659.
Jiao G, Lou G, Mo Y, Pan Y, Zhang Z, Guo R, et al. A combination of GDNF and hUCMSC transplantation loaded on SF/AGs composite scaffolds for spinal cord injury repair. Mat Sci Eng C. 2017;74:230–7.
Lu Y, Gao H, Zhang M, Chen B, Yang H. Glial cell line-derived neurotrophic factor-transfected placenta-derived versus bone marrow-derived mesenchymal cells for treating spinal cord injury. Med Sci Monit. 2017;23:1800.
Nejati K, Mehdi D, Ghareghomi S, Mostafavi E, Ebrahimi-Kalan A, Biglari A, et al. GDNF gene-engineered adipose-derived stem cells seeded Emu oil-loaded electrospun nanofibers for axonal regeneration following spinal cord injury. J Drug Deliv Sci Technol. 2020;60: 102095.
Bamber NI, Li H, Lu X, Oudega M, Aebischer P, Xu XM. Neurotrophins BDNF and NT-3 promote axonal re-entry into the distal host spinal cord through Schwann cell-seeded mini-channels. Eur J Neurosci. 2001;13(2):257–68.
Kumar S, Kahn MA, Dinh L, de Vellis J. NT-3-mediated TrkC receptor activation promotes proliferation and cell survival of rodent progenitor oligodendrocyte cells in vitro and in vivo. J Neurosci Res. 1998;54(6):754–65.
Huang EJ, Reichardt LF. Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci. 2001;24(1):677–736.
Chu G, Yu W, Fehlings M. The p75 neurotrophin receptor is essential for neuronal cell survival and improvement of functional recovery after spinal cord injury. Neuroscience. 2007;148(3):668–82.
Arvanian V. Role of neurotrophins in spinal plasticity and locomotion. Curr Pharm Des. 2013;19(24):4509–16.
Bisicchia E, Latini L, Cavallucci V, Sasso V, Nicolin V, Molinari M, et al. Autophagy inhibition favors survival of rubrospinal neurons after spinal cord hemisection. Mol Neurobiol. 2017;54(7):4896–907.
Cong Y, Wang C, Wang J, Li H, Li Q. NT-3 promotes oligodendrocyte proliferation and nerve function recovery after spinal cord injury by inhibiting autophagy pathway. J Surg Res. 2020;247:128–35.
Thomas AM, Seidlits SK, Goodman AG, Kukushliev TV, Hassani DM, Cummings BJ, et al. Sonic hedgehog and neurotrophin-3 increase oligodendrocyte numbers and myelination after spinal cord injury. Integr Biol. 2014;6(7):694–705.
Ye J, Xue R, Ji Z, Zou C, Chen Y, Wang J, et al. Effect of NT-3 on repair of spinal cord injury through the MAPK signaling pathway. Eur Rev Med Pharmacol Sci. 2020;24(5):2165.
Sun X, Zhang C, Xu J, Zhai H, Liu S, Xu Y, et al. Neurotrophin-3-Loaded multichannel nanofibrous scaffolds promoted anti-inflammation, neuronal differentiation, and functional recovery after spinal cord injury. ACS Biomater Sci Eng. 2020;6(2):1228–38.
Yang Z, Zhang A, Duan H, Zhang S, Hao P, Ye K, et al. NT3-chitosan elicits robust endogenous neurogenesis to enable functional recovery after spinal cord injury. Proc Natl Acad Sci. 2015;112(43):13354–9.
Lu P, Freria CM, Graham L, Tran AN, Villarta A, Yassin D, et al. Rehabilitation combined with neural progenitor cell grafts enables functional recovery in chronic spinal cord injury. JCI Insight. 2022;7(16).
Ahmed Z, Alhajlah S, Thompson AM, Fairclough RJ. Clinic-ready inhibitor of MMP-9/-12 restores sensory and functional decline in rodent models of spinal cord injury. Clin Transl Med. 2022;12(5): e884.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
ND was the major contributor to the writing and ideation of this topic belongs to her; SH searched comprehensively among different databases and contributed to writing the manuscript; and MR contributed to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deznabi, N., Hosseini, S. & Rajabi, M. Neurotrophic factors-based therapeutic strategies in the spinal cord injury: an overview of recent preclinical studies in rodent models. Egypt J Neurol Psychiatry Neurosurg 59, 63 (2023). https://doi.org/10.1186/s41983-023-00661-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00661-3