Abstract
Background
Rib fractures are associated with considerable morbidity and mortality. Surgical stabilization of rib fractures (SSRF) can be performed to mitigate complications. Sarcopenia is in general known to be associated with poor clinical outcomes. We investigated if sarcopenia impacted number of days of mechanical ventilation, intensive care unit (ICU) stay, and total hospital stay in patients who underwent SSRF.
Methods
A retrospective single institutional review was performed including patients who underwent SSRF (2009–2017). Skeletal muscle index (SMI) was semiautomatically calculated at the L3 spinal level on computed tomography (CT) images and normalized by patient height. Sarcopenia was defined as SMI < 55 cm2/m2 in males and < 39 cm2/m2 in females. Demographics, operative details, and postoperative outcomes were reviewed. Univariate and multivariate analyses were performed.
Results
Of 238 patients, 88 (36.9%) had sarcopenia. There was no significant difference in number of days of mechanical ventilation (2.8 ± 4.9 versus 3.1 ± 4.3, p = 0.304), ICU stay (5.9 ± 6.5 versus 4.9 ± 5.7 days, p = 0.146), or total hospital stay (13.3 ± 7.2 versus 12.9 ± 8.2 days, p = 0.183) between sarcopenic and nonsarcopenic patients. Sarcopenic patients demonstrated increased modified frailty index scores (1.5 ± 1.1 versus 0.9 ± 0.9, p < 0.001) compared to nonsarcopenic patients.
Conclusions
For patients who underwent SSRF for rib fractures, sarcopenia did not increase the number of days of mechanical ventilation, ICU stay, or total hospital stay. Sarcopenia should not preclude the utilization of SSRF in these patients.
Similar content being viewed by others
Key points
-
Sarcopenia is a general risk factor for poor clinical outcomes.
-
Sarcopenic and non-sarcopenic patients who underwent surgical stabilization of traumatic rib fractures were compared.
-
Sarcopenic patients did not have greater number of days of mechanical ventilation, intensive care unit stay, or total hospital stay.
Background
Rib fractures are common following chest wall trauma and result in considerable morbidity and mortality, especially in those with diminished physiologic and pulmonary reserve [1]. Mortality after rib fractures is approximately 10% and increasing numbers of fractured ribs is associated with greater mortality and morbidity rates [2, 3]. In an effort to reduce morbidity and mortality associated with traumatic rib fractures, several investigators have shown benefits of surgical stabilization of rib fractures (SSRF), which include reductions in mechanical ventilation duration, mortality rates, development of pneumonia, pain, and long-term disability [4,5,6,7,8].
Sarcopenia is defined as the loss of skeletal muscle mass and function [9]. Multiple studies in a number of clinical and surgical scenarios have demonstrated that sarcopenic patients have worse outcomes than nonsarcopenic patients [9,10,11,12,13,14,15,16,17,18,19,20,21]. Furthermore, in patients with traumatic injuries, sarcopenia has been associated with increased mortality rates, duration of hospital stay, risk of complications, and more frequent patient discharges to a dependent facility [22, 23].
In this study, we aimed at evaluating the impact of sarcopenia in patients who underwent SSRF for traumatic rib fractures, hypothesizing that the presence of sarcopenia would impact short-term outcomes such as duration of mechanical ventilation, intensive care unit (ICU) stay, and total hospital stay.
Methods
Patient cohort
Institutional review board approval was obtained for this study, which was in compliance with the Health Insurance Portability and Accountability Act. A single institution retrospective review of patients who underwent SSRF for traumatic rib fractures from 2009 to 2017 at an American College of Surgeons (ACS) verified level I trauma center was performed. Institutional guidelines for SSRF include the following: flail chest; rib displacement greater than or equal to one rib width; clinically relevant and refractory pain in association with rib fracture(s); mobile rib fracture(s), i.e., “clicking”; and anticipated nonunion or malunion of fractures. Exclusion criteria included patients who did not consent for research and those that did not have an admission computed tomography (CT) scan that included the L3 vertebral body level.
CT scanning technique
Most exams were performed as part of an initial trauma evaluation and scanned on either a Siemens Flash scanner or Siemens Definition Edge scanner. Standard CT parameters for the trauma protocol were 2.0 mm slice thickness with 1.2 mm slice increment for the chest, with both a vascular optimized kernel (B30f) axial reconstruction and a dedicated high spatial resolution kernel for fracture evaluation (B70). The abdominopelvic portion of the exam was reconstructed with 3.0 mm slice thickness at 2.0 mm slice increment, with soft tissue kernel (I30) and a medium strength setting for SAFIRE. The chest and the abdominopelvic portions of the exam were reconstructed in both sagittal and coronal planes as well. The chest and the abdominopelvic acquisitions are done at fixed 120kVP, with Quality reference mAs of 240.
Body composition measurements
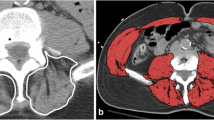
One board-certified radiologist (DAD) and one radiology fellow (FIB) examined the admission CT scan and identified the single axial image at the level of the third lumbar vertebrae on which both transverse processes were fully visualized. These images were then analyzed in a semiautomatic process using the software BodyCompSlicer (developed at Mayo Clinic, Rochester, MN) [24]. BodyCompSlicer automatically placed three boundary lines between external air and subcutaneous fat, between subcutaneous fat and abdominal wall/paraspinal muscles, and between abdominal wall/paraspinal muscles and visceral fat. An example of a CT slice with boundary lines is included in Fig. 1. The reviewers then carefully inspected the boundaries and manually corrected the boundaries when necessary. The following muscles were outlined: psoas, erector spinae, quadratus lumborum, and the abdominal wall (including rectus abdominis, transverse abdominis, and internal and external oblique muscles). The software then calculated the skeletal muscle area, the area containing pixels between boundaries two and three excluding the spine, and having a CT attenuation value of -30 to 150 HU. The skeletal muscle area was then divided by the height of the patient squared (m2) to calculate the skeletal muscle index (SMI). Patients were categorized as sarcopenic according to international gender-specific consensus definitions (SMI = two standard deviations or less below the mean for healthy young adults aged 20–40), with male SMI lower than 55 cm2/m2 and female SMI lower than 39 cm2/m2 [25]. Figures 2 and 3 demonstrate CT slices of a sarcopenic patient and a nonsarcopenic patient.
Example of segmentation of a computed tomography image with boundary lines between external air and subcutaneous fat (1), between subcutaneous fat and abdominal wall/paraspinal muscles (2), and between abdominal wall/paraspinal muscles and visceral fat (3). The box around the paraspinal muscles allows the algorithm to separately calculate the paraspinal muscle area (if this information is desired)
Data collection
Clinicopathological variables were collected which included age, sex, height, weight, body mass index, admission date, mechanism of injury, operating room date, time from admission to surgery, duration of operation, number of ribs plated, and number of plates used. The presence/absence of smoking history, chronic obstructive pulmonary disease, other sustained fractures, hemothorax, pneumothorax, chest tube placement, pneumonia, tracheostomy, and flail chest were recorded. Furthermore, the number of ribs fractured, number of total fractures, Rib score [26], ICU length of stay, total hospital length of stay, and the duration (days) of mechanical ventilation were documented. The Blunt Pulmonary Contusion-18 score [27], which is calculated by quantifying the degree of pulmonary contusion for each of the three zones in both lungs on a scale of zero to three, and modified frailty index, which has been proven to adequately reflect frailty and predict mortality and morbidity [28], were documented.
Statistical analysis
Comparisons of patient demographics and clinical characteristics of patients with and without sarcopenia were made using t test, χ2 test, and Fisher’s exact test. Odds ratio and 95% CI were calculated. Multivariable logistic regression models were used to examine sarcopenia as a predictor of length of ICU and hospital stay, adjusted for age, body mass index, gender, and number of ribs fractured. Analyses were conducted using SAS (version 9.4; Cary, NC).
Results
A total of 277 patients that sustained traumatic rib fractures underwent SSRF between 2009 and 2017. After exclusion criteria, the cohort consisted of 238 patients. Among the study population, 160 (67.2%) were male. The age was 60.4 ± 17.4 years (mean ± standard deviation). Considering the total of 238 patients included, the mechanism of initial injury was as follows: 104 (43.7%) automobile involved accidents (99 motor vehicle/motorcycle collisions, four automobile-pedestrian collisions, and one automobile-bike/ski collision), 90 (37.8%) falls, and 44 (18.5%) miscellaneous incidents. The miscellaneous category refers to mechanisms that do not occur with enough frequency to fall into a separate category. A few examples include penetrating injury secondary to farm equipment, explosion/blast injury, pedestrian-train collision, and crush injury. Out of the 104 patients involved in automobile accidents, 82 were nonsarcopenic, and 22 were sarcopenic. Out of the 90 patients involved in falls, 43 were nonsarcopenic and 47 were sarcopenic. Out of the 44 patients in the miscellaneous category, 25 were nonsarcopenic and 19 were sarcopenic.
Complete clinical, demographic, and injury characteristics of included patients are seen in Table 1. A total of 88/238 (36.9%) patients were classified as sarcopenic. Sarcopenic patients were older than nonsarcopenic patients, aged 69.1 ± 16.3 years (mean ± SD) versus 55.3 ± 16.0 years (p < 0.001). Sarcopenic patients demonstrated a lower mean body mass index compared to nonsarcopenic patients (27.2 ± 5.6 kg/m2 versus 31.6 ± 5.7 kg/m2, p < 0.001) and sarcopenic patients demonstrated significantly increased modified frailty index scores (1.5 ± 1.1 versus 0.9 ± 0.9, p < 0.001) but decreased Blunt Pulmonary Contusion-18 scores (1.2 ± 1.3 versus 1.8 ± 1.4, p < 0.001) compared to nonsarcopenic patients.
Comparison of those with and without sarcopenia demonstrated no significant difference in duration of ICU stay (5.9 ± 6.5 versus 4.9 ± 5.7 days, p = 0.146) or duration of total hospital stay (13.3 ± 7.2 versus 12.9 ± 0.2 days, p = 0.183). The number of days of mechanical ventilation was not significantly different in those with or without sarcopenia (2.8 ± 4.9 versus 3.1 ± 4.3 days, p = 0.304). A total of 11/88 (12.5%) sarcopenic patients and 21/150 (14.0%) nonsarcopenic patients developed pneumonia (p = 0.743), while 5/88 (5.7%) sarcopenic and 11/150 (7.3%) nonsarcopenic patients received a tracheostomy (p = 0.623) Out of the 149 patients with flail chest, 50 (33.6%) were sarcopenic and 99 (66.4%) were nonsarcopenic (p = 0.158). There was no significant difference in the numbers of ribs fractured between those with and without sarcopenia (7.8 ± 4.3 versus 8.0 ± 4.0, p = 0.697). Furthermore, there was no significant difference in the time to SSRF between those with and without sarcopenia (3.8 ± 1.9 versus 4.4 ± 3.6 days, p = 0.292). The number of ribs fractured was a significant predictor of hospital (p < 0.001) and ICU length of stay (p = 0.003).
A total of four patients died while in the hospital after a prolonged duration of total hospital stay (range 10–20 days) and ICU stay (range 7–17 days) and a number of days of mechanical ventilation (range 4–10 days), all of them being sarcopenic. Fisher’s exact test demonstrated a p value of 0.018, with an odds ratio of 1.048 (95% confidence interval 1.000–1.010), revealing that sarcopenic patients in the cohort had a significant increased mortality risk when compared to nonsarcopenic patients.
Discussion
To our knowledge, this is the first study to explore whether sarcopenia affected short-term outcomes in patients who underwent SSRF after sustaining traumatic rib fractures. In our cohort, there was no statistical significant difference in duration of stay in the ICU, total duration of stay in the hospital, and duration of mechanical ventilation in sarcopenic patients when compared to nonsarcopenic patients. These results are in contradiction to prior studies in the emergency surgery and trauma population, which have demonstrated that patients with sarcopenia have longer durations of stay in the ICU and hospital as well as a longer duration of mechanical ventilation [16, 23, 29].
However, sarcopenic patients did have a significant greater modified frailty index. The modified frailty index has been proven to reflect frailty and predict mortality and morbidity, identifying patients who are more susceptible to complications after surgical procedures [28]. Furthermore, sarcopenia has also been proven to negatively impact outcomes in many populations, including the surgical and trauma populations [16, 23, 30, 31]. Thus, it is interesting that the sarcopenic patients in our cohort had an increased modified frailty index, but did not have increased duration of stay in the ICU or hospital and did not have a longer duration of mechanical ventilation.
A total of four patients died while in the hospital, and all were sarcopenic. While our data did demonstrate that this was statistically significant (p = 0.018), the odds ratio [95% CI] was 1.048 [1.000, 1.010]; thus, this is likely of minimal clinical significance and death is nearly equally likely to occur in patients with sarcopenia and without sarcopenia. Even though more sarcopenic patients died in this cohort, this is not a novel and has been demonstrated on numerous prior studies, including studies focusing on patients undergoing emergency surgery and patients involved in trauma [16, 22, 23]. Additionally, all of these patients who died did have prolonged stays in the ICU and hospital with numerous days of mechanical ventilation. Thus, it is unclear if our data concerning duration of stay in the ICU and hospital as well as duration of mechanical ventilation when comparing sarcopenic and nonsarcopenic patients would have changed had all sarcopenic patients survived. However, we expect that the change in our data would have been minimal, as these patients had already spent considerable time in the ICU and hospital and on mechanical ventilation.
There was no statistical significance in the numbers of ribs fractured, the number of patients with flail chest, and the number of days between the trauma and the rib fixation surgery between patients with sarcopenia and patients without sarcopenia. However, the number of ribs fractured was a significant predictor of hospital and ICU length of stay. This confirms earlier results revealing that increasing number of fractured ribs is associated with greater morbidity and mortality [3].
There are limitations to this study. This is a single institution, retrospective review, and while our institution does have criteria for SSRF, there is a potential for selection bias in choosing patients suitable for an operation. Furthermore, since this study involved patients with traumatic rib fractures, many of them likely had concomitant injuries within the chest, abdomen, pelvis, brain, and spine which would play a role in their overall condition and ultimately their disposition.
In conclusion, sarcopenic patients in our cohort had statistically significant higher modified frailty indices, without longer hospital or ICU lengths of stay, or more days of mechanical ventilation. Thus, sarcopenia should not preclude patients with traumatic rib fractures from undergoing SSRF. We feel that this is quite important as numerous other studies have demonstrated that sarcopenic patients have worse outcomes. However, more research needs to be completed in regards to this topic before definitive conclusions are drawn. For example, a case-matched control study, and ultimately a randomized controlled study, comparing patients who underwent SSRF and those who did not would be important next steps in verifying our results.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due because the dataset is a private institutional data set but are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- SMI:
-
Skeletal muscle index
- SSRF:
-
Surgical stabilization of rib fractures
References
Kent R, Woods W, Bostrom O (2008) Fatality risk and the presence of rib fractures. Ann Adv Automot Med 52:73–82
Bassett JS, Gibson RD, Wilson RF (1968) Blunt injuries to the chest. J Trauma 8:418–429. https://doi.org/10.1097/00005373-196805000-00008
Sirmali M, Turut H, Topcu S et al (2003) A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg 24:133–138. https://doi.org/10.1016/s1010-7940(03)00256-2
Doben AR, Eriksson EA, Denlinger CE et al (2014) Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care 29:139–143. https://doi.org/10.1016/j.jcrc.2013.08.003
Wada T, Yasunaga H, Inokuchi R et al (2015) Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: a propensity score-matched analysis. J Crit Care 30:1227–1231. https://doi.org/10.1016/j.jcrc.2015.07.027
Slobogean GP, MacPherson CA, Sun T, Pelletier ME, Hameed SM (2013) Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 216:302–311 e1. https://doi.org/10.1016/j.jamcollsurg.2012.10.010
de Moya M, Bramos T, Agarwal S et al (2011) Pain as an indication for rib fixation: a bi-institutional pilot study. J Trauma 71:1750–1754. https://doi.org/10.1097/TA.0b013e31823c85e9
Mouton W, Lardinois D, Furrer M, Regli B, Ris HB (1997) Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg 45:242–244. https://doi.org/10.1055/s-2007-1013735
Kumar A, Moynagh MR, Multinu F et al (2016) Muscle composition measured by CT scan is a measurable predictor of overall survival in advanced ovarian cancer. Gynecol Oncol 142:311–316. https://doi.org/10.1016/j.ygyno.2016.05.027
Martin L, Birdsell L, Macdonald N et al (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 31:1539–1547. https://doi.org/10.1200/JCO.2012.45.2722
Psutka SP, Carrasco A, Schmit GD et al (2014) Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer-specific and all-cause mortality. Cancer 120:2910–2918. https://doi.org/10.1002/cncr.28798
Del Fabbro E, Parsons H, Warneke CL et al (2012) The relationship between body composition and response to neoadjuvant chemotherapy in women with operable breast cancer. Oncologist 17:1240–1245. https://doi.org/10.1634/theoncologist.2012-0169
Sabel MS, Lee J, Cai S, Englesbe MJ, Holcombe S, Wang S (2011) Sarcopenia as a prognostic factor among patients with stage III melanoma. Ann Surg Oncol 18:3579–3585. https://doi.org/10.1245/s10434-011-1976-9
Psutka SP, Boorjian SA, Moynagh MR et al (2016) Decreased skeletal muscle mass is associated with an increased risk of mortality after radical nephrectomy for localized renal cell cancer. J Urology 195:270–276. https://doi.org/10.1016/j.juro.2015.08.072
Tan BH, Birdsell LA, Martin L, Baracos VE, Fearon KC (2009) Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res 15:6973–6979. https://doi.org/10.1158/1078-0432.CCR-09-1525
Rangel EL, Rios-Diaz AJ, Uyeda JW et al (2017) Sarcopenia increases risk of long-term mortality in elderly patients undergoing emergency abdominal surgery. J Trauma Acute Care Surg 83:1179–1186. https://doi.org/10.1097/TA.0000000000001657
Joglekar S, Asghar A, Mott SL et al (2015) Sarcopenia is an independent predictor of complications following pancreatectomy for adenocarcinoma. J Surg Oncol 111:771–775. https://doi.org/10.1002/jso.23862
Englesbe MJ, Patel SP et al (2010) Sarcopenia and mortality after liver transplantation. J Am Coll Surg 211:271–278. https://doi.org/10.1016/j.jamcollsurg.2010.03.039
Reisinger KW, van Vugt JL, Tegels JJ et al (2015) Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg 261:345–352. https://doi.org/10.1097/SLA.0000000000000628
Otsuji H, Yokoyama Y, Ebata T et al (2015) Preoperative sarcopenia negatively impacts postoperative outcomes following major hepatectomy with extrahepatic bile duct resection. World J Surg 39:1494–1500. https://doi.org/10.1007/s00268-015-2988-6
Peng YC, Wu CH, Tien YW, Lu TP, Wang YH, Chen BB (2020) Preoperative sarcopenia is associated with poor overall survival in pancreatic cancer patients following pancreaticoduodenectomy. Eur Radiol. https://doi.org/10.1007/s00330-020-07294-7
Yoo T, Lo WD, Evans DC (2017) Computed tomography measured psoas density predicts outcomes in trauma. Surgery 162:377–384. https://doi.org/10.1016/j.surg.2017.03.014
DeAndrade J, Pedersen M, Garcia L, Nau P (2018) Sarcopenia is a risk factor for complications and an independent predictor of hospital length of stay in trauma patients. J Surg Res 221:161–166. https://doi.org/10.1016/j.jss.2017.08.018
Takahashi N, Sugimoto M, Psutka SP, Chen B, Moynagh MR, Carter RE (2017) Validation study of a new semi-automated software program for CT body composition analysis. Abdom Radiol (NY) 42:2369–2375. https://doi.org/10.1007/s00261-017-1123-6
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495. https://doi.org/10.1016/S1470-2045(10)70218-7
Chapman BC, Herbert B, Rodil M et al (2016) RibScore: A novel radiographic score based on fracture pattern that predicts pneumonia, respiratory failure, and tracheostomy. J Trauma Acute Care Surg 80:95–101. https://doi.org/10.1097/TA.0000000000000867
Tyburski JG, Collinge JD, Wilson RF, Eachempati SR (1999) Pulmonary contusions: quantifying the lesions on chest X-ray films and the factors affecting prognosis. J Trauma 46:833–838. https://doi.org/10.1097/00005373-199905000-00011
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM (2018) New 5-factor modified frailty index using American College of Surgeons NSQIP Data. J Am Coll Surg 226:173–181 e8. https://doi.org/10.1016/j.jamcollsurg.2017.11.005
Moisey LL, Mourtzakis M, Cotton BA et al (2013) Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit Care 17:R206. https://doi.org/10.1186/cc12901
Dirks RC, Edwards BL, Tong E et al (2017) Sarcopenia in emergency abdominal surgery. J Surg Res 207:13–21. https://doi.org/10.1016/j.jss.2016.08.015
Du Y, Karvellas CJ, Baracos V, Williams DC, Khadaroo RG (2014) Sarcopenia is a predictor of outcomes in very elderly patients undergoing emergency surgery. Surgery 156:521–527. https://doi.org/10.1016/j.surg.2014.04.027
Funding
Funding was obtained from the radiology department for statistical analyses
Author information
Authors and Affiliations
Contributions
DD, BK, MH, and FB performed the chart review. NT, MM, KG, and DD analyzed the sarcopenia results. DD, BK, MH, and AF interpreted all of the data and helped derive conclusions. DD and MH were major contributors in writing the manuscript. All authors read, made changes to, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval was obtained for this retrospective chart review. All patients consented for research.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doolittle, D.A., Hernandez, M.C., Baffour, F.I. et al. CT-derived sarcopenia should not preclude surgical stabilization of traumatic rib fractures. Eur Radiol Exp 5, 9 (2021). https://doi.org/10.1186/s41747-021-00206-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41747-021-00206-4