Abstract
Hypoxic zones exist in solid tumors, where oxygen levels are significantly lower than in normal tissues. Hypoxia makes chemo-radiation therapeutics less effective and renders the metastatic potential more favorable. Emerging research has found that the transcriptional expression of hypoxia-inducible factor-1alpha (HIF-1α) promotes the transcription of vascular endothelial growth factor A (VEGF-A) and Hexokinase-I (HK-I), which are associated to cellular growth, angiogenesis, and metastatic invasion in many malignancies. However, it is still unclear whether VEGFA and HK-I expression has any influence on survival based on the intrinsic subtypes of breast cancer. Their prognostic significance remains a debatable topic. In the present study, quantitative Real-time polymerase chain reaction (qRT-PCR) was employed to check the relative expression of HIF-1α, VEGF-A and HK-I. The hazard ratios (HR) of breast cancer-specific and overall mortality were calculated using Cox proportional hazards model, which were adjusted for demographic, clinicopathological, and associated molecular variables, as well as the diagnosis year. The relative mRNA expression levels of HIF-1α (p = 0.0010) and VEGFA (p = 0.0119) were significantly higher in tumor tissues. The expression of both HIF-1α (p = 0.0111) and VEGFA (p = 0.0078) was higher in the TNBC group of breast cancers, while HK-I (p = 0.0106) was higher in ER/PR-positive, HER2-negative group. HIF-1α and HK-I overexpression were associated with a higher likelihood of survival, while overexpression of VEGFA was associated with a low survival rate, although it was not statistically significant.
Similar content being viewed by others
Introduction
Breast cancer is the most frequent malignancy in women. According to H. Sung and etal., cancer incidence rate is rising at an alarming rate, and one in every four individuals over 65 years will be a cancer survivor by 2040, making cancer one of the leading causes across the globe. In 2020, around 2.3 million females (or 11.7 percent of all cancer patients) were diagnosed with the disease worldwide. The incidence of breast cancer has now overtaken that of lung cancer. Breast cancer is the most frequent malignancy in terms of incidence and the fifth leading cause of cancer mortality, with 6,85,000 deaths globally, despite the fact that breast cancer may be effectively treated if diagnosed and treated at an early stage. Breast cancer is increasing at a rate of 3.1 percent every year. The highest incidence rate is seen in developed countries, whereas the lowest is found in developing and underdeveloped countries [1]. In India, Breast Cancer accounts for roughly a quarter of all female cancer cases. The total 178,361 new cases of breast cancer were found in 2020, which accounts for 13.5% of all cancer cases recorded. In India, about half of all breast cancer patients are under the age of 50 [2]. Even after achieving breakthroughs in diagnostics and therapeutics, it is the primary reason for cancer-related mortality in females globally. It has various subtypes that are linked with varying clinical outcomes [3, 4]. Understanding this variation is critical for developing personalized preventative and therapeutic approaches. One of the characteristics of breast cancer is metabolic reprogramming, which helps to maintain the malignant phenotype in response to the tumor microenvironment's selective pressure [5]. Low intratumoral oxygen levels (hypoxia) are linked to tumor aggressiveness, tumor invasion, and therapeutic resistance in breast cancer [6]. Hypoxia-inducible factor (HIF) is responsible for most transcriptional responses to hypoxia [7]. HIFs consist of two subunits: one that is oxygen-dependent (HIF-1α) and the other that is oxygen-independent (HIF-1β), with the former classified into three isoforms: HIF-1α, HIF-2α and HIF-3α [8]. HIF-1α is post-translationally degraded by prolyl hydroxylases (PHDs) under normoxia, but in hypoxic conditions, the α-subunit avoids degradation by binding to the β-subunit and forming a heterodimer, allowing it to exert hypoxic responses via binding to the RCGTG sequence, known as hypoxia response element (HRE) [9].
HIF-1α is anticipated to initiate a signal-transduction network in the hypoxic zone in solid tumors, enabling tumor cells to adapt to hypoxic circumstances and evolve into an aggressive phenotype [10, 11]. HIF-1α increases the expression of approximately 40 downstream proteins that are required for survival under hypoxia. Interestingly, one of the downstream proteins controlled by HIF-1α is vascular endothelial growth factor (VEGF), which promotes the tumor angiogenesis when upregulated [12]. Furthermore, solid tumors are subjected to hypoxic pressure and HIF-1α is implicated in tumor angiogenesis [13,14,15]. Since HIF-1α has been shown to play a crucial role in angiogenesis, blocking or silencing this pathway may make it more challenging for cells to form a robust vasculature and spread to other spots, even when they have an invasive character [16].
Moreover, HIF is important in controlling metabolic rewiring in cancers that rely on non-oxidative glucose breakdown rather than regular oxidative phosphorylation for energy production. Hexokinase-1 (HK-1) is one of the main target enzymes of HIF-1 in the glycolytic pathway. HIF-1α's impact on glycolytic metabolism has been extensively documented [17], HIF-1α stability drives the glycolysis in tumors, irrespective of the hypoxic environment [18]. Furthermore, HIF-1α allows cells to adjust to lower intracellular pH resulting from augmented anaerobic glycolysis and lactic acid production [19].
In the clinical settings, there has been no effective targeting of HIF-1 and its subsequent inhibition in angiogenesis and metabolism in the therapeutic context of breast cancer. In the present study, we evaluated the expression of hypoxia-associated metabolic and angiogenesis markers like HIF-1α, VEGFA, and Hexokinase-I in different sub groups of breast cancers with the intent whether anti-HIF-1 could be employed as a therapeutic target to impede the role of VEGFA and HK-I in tumor development and progression in different subtypes of BC.
Materials and methods
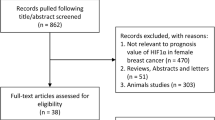
Patients and samples
A total of 56 histopathologically confirmed breast cancer samples and 56 normal blood samples were taken from the Department of Surgery & Surgical Oncology SKIMS Srinagar from 2018–2021. The study was performed in agreement with the principles of the Helsinki Declaration, 1964, with proper approval of the study from the Institutional Ethical Committee SKIMS (IEC Protocol No. 07/2019). Written informed consent was taken from the subjects in predesigned proforma. Only those patients were included in the study that were histologically and radiologically confirmed and were willing to participate while as those patients were excluded which had prior history of any other malignancy or history of cardiovascular or any other serious disease. Those patients were also excluded who had undergone chemo or radiotherapy and were not willing to participate.
RT-PCR
Trizol method was used to extract total RNA from breast tissues obtained after mastectomy or BCS and blood samples obtained during surgery. The expression of HIF-1α, VEGFA and Hexokinase-I mRNA was analyzed by Real-time Polymerase Chain Reaction (RT-PCR). The Revert Aid First Strand cDNA Synthesis Kit (ThermoScientific) was used to reverse transcribe 1–2 µg of RNA in a total reaction volume of 25 μL. The primer sequences of HIF-1α, VEGFA, Hexokinase-I, GAPDH and β-Actin are listed in Supplementary Table 1. The 2−ΔΔCT approach was applied to compute the relative expression of the different experimental sets, which was normalized to β-ACTIN and GAPDH expression. PCR was performed on Rotor-Gene Q (QIAGEN) by employing standard PCR conditions. Electrophoresis in 2% agarose gels separated the amplified fragments, which were then seen on gel doc under UV after being stained with ethidium bromide.
Immunohistochemistry (IHC)
Tissue samples obtained from subjects were processed for IHC to analyze the microscopic changes at the sub-cellular level. Briefly, paraffin-embedded tissue blocks were sliced into 3-5 μm thick sections and were put on charged slides. After de-paraffinization of tissue sections, slides were processed for hydration by successive ethanol treatment with decreasing concentrations. Antigen retrieval of tissue sections was performed in an autoclave at 95 °C for 25 min in a citrate-buffered solution (0.01 M, pH 6.0). Immunostaining was used to determine the expression and localization of HIF-1α (1:100) (GTX127309, Gene Tex) VEGF-A (1:100) (GTX102643, Gene Tex) and HK-I(1:200) (#8337 C35C4, CST) using commercially available antibodies. A horseradish peroxidase (HRP) labeled secondary antibody was used to visualize the antigen–antibody complex.
Statistical analysis
The findings in this study were analyzed to evaluate the association between VEGF-A, HIF-1α and HK-1 expression and known histopathologic risk factors in breast cancer, as well as the prognostic importance of their expression. The χ2 test was used to examine the associations between VEGF-A, HIF-1α and HK-1 expression and stage, cancer type, tumor size, histological grade, and lymph node metastasis. A log-rank test was used to assess overall survival curves based on whether VEGF-A, HIF-1α and HK-1 were expressed. The Cox proportional hazards regression model was employed to undertake a multivariate analysis of the prognostic impact of all of these covariates. In this investigation, p value less than 0.05 (p < 0.05) was considered statistically significant. Statistical analysis was performed using GraphPad Prism 5 Application (Version 5.0.0.288).
Results
Clinical data
A total of 56 breast cancer patients were studied over four years, from 2018 to 2021. Out of 56 patients, 31 (55.35%) were under 50 and 25 (44.65%) were over 50 years old. The average age of patients was 51.6 ± 12.62 (Range 32-80yrs). Most patients had an active lifestyle, accounting for 42 (75%) of the total number of patients, whereas 14 (25%) had a sedentary lifestyle. Out of all patients, 06 (10.7%) had a family history of either breast cancer or other solid malignancy and 50 (89.3%) patients had no family history of any malignancy. Most of the patients had normal body mass 42 (75%), except a few patients who were lean 05 (8.93%) and obese 09 (16.07%). Only 21 (37.5%) of the patients were from Kashmir's urban districts, while 35 (62.5%) were from rural areas (Table 1).
HIF-1α, VEGFA and HK-I expression in BC
HIF-1α (p = 0.0010) and VEGFA (p = 0.0119) transcriptional expression was found to be higher in tumor tissues and blood of the patients than in surrounding normal/peritumor tissues and normal blood samples, respectively, whereas HK-I (p = 0.9842) was also higher in tumor tissues but not statistically significant. HIF-1α (p = 0.0111) and VEGFA (p = 0.0078) relative mRNA expression were greater in TNBC and Her2 + breast tumors (Fig. 1).
mRNA expression of HIF-1α, VEGFA & HK-I in breast cancer and its subtypes. A Relative mRNA expression profile of HIF-1α, VEGFA & HK-I in breast cancer tissues. B HIF-1α mRNA expression in breast cancer subtypes correlated with normal tissue. C VEGFA mRNA expression in breast cancer subtypes correlated with normal tissues. D HK-I mRNA expression in breast cancer subtypes correlated with normal tissues. - - - represents TNBC. + + + represents Estrogen, Progesterone & Her2 positive. + + - represents Estrogen, Progesterone positive & Her2 negative. - - + represents Estrogen, Progesterone negative & Her2 positive
The HIF-1α expression in the BC subgroups was significantly higher (p = 0.0176), with the TNBC group having the highest expression and the ER + /PR + group having expression value between TNBC and HER2 + . The expression of VEGFA was also found to be higher in TNBC (p = 0.0119) and HER2 + (p = 0.0078) sub-group. While as the expression of HK-I was significantly higher in ER/PR + , HER2– group (p = 0.0106) than other sub groups of BC respectively (Fig. 1).
HIF-1α, VEGFA and HK-I immunoexpression in breast carcinoma cases
Positive HIF-1α immuno-expression was observed in 33 (62.26%) of the 53 samples, whereas positive VEGFA expression was found in 38 (71.69%) of the samples, and this was perceived to be statistically linked with higher histopathological grade (p = 0.0006) and positive lymph node metastasis (p = 0.031). The HK-1 immuno-expression was positive in 27 (50.9%) of the 53 samples. HIF-1α immuno-expression was predominantly found in the nucleus. However, it was also seen in cytoplasm, where it may operate as a transcription factor, VEGFA and HK-I were mostly found in the cytoplasm (Figs. 2, 3 and 4).
Immunohistochemical expression of hypoxia-inducible factor-1 alpha (HIF-1α) with increasing grade in Breast Carcinoma. The expression of HIF-1α was mostly nuclear, but in some cells, cytoplasmic positivity was also observed. A Normal tissue (10X), B Normal tissue (40X), C Grade I(10X), D Grade I(40X), E Grade II(10X), F Grade II(40X), G Grade III(10X), H Grade III(40X)
Association between HIF-1α, VEGF-A and HK-I expression and clinicopathological variables
The increased expression of HIF-1α is known to increase the expression of VEGFA and HK-I. Results of the Spearman correlation indicated that there is a non-significant yet positive relationship between HIF-1α and VEGFA, (r = 0.208, p = 0.186) HIF-1α and HK-I (r = 0.121, p = 0.447) and a non-significant, negative relationship between HK-I and VEGFA (r = 0.039, p = 0.806) (Fig. 5).
Thus, without reaching any conclusive statistical significance, the mRNA expression of HIF-1α was evaluated, and it was found to be higher in the lower age group (≤ 50 years), moreover the mRNA expression of VEGFA and HK-I was found to be statistically significant in the higher age group (≥ 50 years) (Fig. 6A). The expression of HIF-1α was also statistically higher in pre-menopausal women, whereas VEGFA expression was higher in post-menopausal women and HK-I was slightly higher in pre-menopausal group without reaching any statistical significance (Fig. 6B). The transcriptional expression levels of HIF-1α, VEGFA and HK-I were found to be higher with increasing grade (Grade II & III) (Fig. 6C).
Correlations between HIF-1α, VEGF-A, HK-I, and clinicopathological data were examined using χ2 test to calculate the clinical prominence in BC. Relatively high continuous mRNA expression levels of VEGFA and HIF-1α were not linked to any of the clinicopathological parameters, while HK-I expression was significantly related to different subtypes of BC (p = 0.036) and necrosis of tumor tissue (p = 0.029) & in Table 2.
Prognostic value of HIF-1α, VEGFA and HK-I
The survival analysis was performed by using Kaplan–Meier approach to assess the relationship between overall survival rates and mRNA expression of HIF-1α, VEGFA and HK-I. The overall survival rates for high and low expression of HIF-1α, VEGFA and HK-I were 71.1% & 64%, 65.71% & 84%, and 70.74% & 62.5% respectively. The cox-regression hazard model was used to identify independent prognostic determinants. High levels of VEGFA were also linked to poor prognosis for BC (HR = 1.88). While HIF-1α (HR = 0.808) and HK-I (0.7884) levels were not linked with the prognosis. The study found that high VEGFA expression, lymph node involvement, TNBC type, advanced grade and stage (II & III) are independent prognostic variables for BC (Fig. 7).
Kaplan–Meier plots depicting overall survival (OS) in breast cancer (A) OS in BC patients (B) Survival analysis correlating expression to overall survival HIF-1α (C) VEGFA (D) HK-I (E) Survival analysis correlating expression to the histological Grade (F) Survival analysis correlating expression to Lymph Node metastasis
During the survival analysis, it was observed that patients with HIF-1α and HK-I overexpression had favorable prognosis and patients with VEGFA overexpression had a worse prognosis. In oncological research, a lot of work is being put into targeting metabolic pathways that are active in cancerous cells. Hypoxia is a well-recognised process to accelerate glycolysis and promotes the expression of various metabolism-related genes; therefore specifically targeting biochemical pathways might kill hypoxic cells or make them more sensitive to conventional chemotherapy or a specialized targeted treatment. This may pave theway towards personalized medicine.
Heat map plot analysis also represented the differential expression of the HIF-1α, VEGFA, and HK-I along with the classification based on the ER, PR and Her2. Columns of the plot represent the genes and the rows represent samples (Fig. 8A-E). Moreover, the gene–gene interaction analysis of HIF-1α, VEGFA, and HK-I revealed that EPAS,CUL2,SLC2A1, FLT1, ARNT, HIF1AN and VHL showed maximum interaction (Fig. 9). These genes might play a role in BC progression and could be explored for future studies.
Heat map plot of HIF-1α, VEGFA and HK-I as in (A) along with the classification based on the ER, PR and Her2 status as in (B-E). Columns of the plot represent the genes and the rows represent samples. + + - represents Estrogen, Progesterone positive & Her2 negative. - - - represents TNBC. - - + represents Estrogen, Progesterone negative & Her2 positive. + + + represents Estrogen, Progesterone & Her2 positive
Discussion
The present study explored the expression pattern of HIF-1α, VEGFA, and HK-I in BC patients, to evaluate if they had any prognostic or predictive capabilities and whether there were any correlations with clinical and immunohistochemical markers.
Hypoxia is a common hallmark of poor-prognosis tumors [20]; thus, identifying common in-vivo hypoxia-related genes is important for patient prognostic classification and the development of new therapeutics. Although prognostic indicators for hypoxia have been established and there are differences across research, necessitating the application of strong tools in large meta-analyses to create broadly applicable signatures. As it is well acknowledged that HIF-1 and VEGF are significant regulators of angiogenesis, [21]. HIF-1α is a master regulator of hypoxia that is hydroxylated by Prolyl hydroxylases (PHD) under normoxic circumstances, which guides it to post-translational ubiquitination and subsequently to proteasomal degradation, but in hypoxic conditions, HIF-1α gets stabilized and binds to HIF-1β resulting in the formation of a heterodimer that passages to nucleus and binds to Hypoxia Response Element (HRE) to initiate target gene transcription [22]. This complex facilitates tumor development and metastasis by activating genes implicated in cell proliferation, angiogenesis, and survival [21, 23] (Fig. 10). In addition, HIF1α frequently regulates HK as a target molecule to maintain elevated metabolic needs. Identifying new potential anti-HIF-1α targets in BC is quiet attractive, particularly for malignancies like TNBC, for which there is currently no targeted therapy. As a result, we looked at the relative mRNA expression, protein localization, and expression profiling of HIF-1α and other angiogenesis/metabolic factors in subtypes of breast cancer mentioned above. Our findings demonstrated that HER2-positive tumors differed marginally from the other categories with statistically insignificant to non-existent differences. Moreover, TNBC shows increased expression levels across the investigated variables.
The elevated levels of HIF-1α in inherited BRCA1 mutant cancers in 90% of cases led to the anticipation of HIF-1α amplification in TNBC [24]. Knowing that BRCA1-coupled BC commonly corresponds to the TNBC type and each generally displays the indications of hypoxic morphology might be the reason to anticipate an increased expression of HIF-1α in TNBC [25, 26]. HIF-1α seems to work in conjunction with HER2 in HER2 + enhanced tumors where hypoxia is not a significant histological attribute, adding to aggressive tumour development and metabolism [27]. Overexpression of HER2, a transmembrane tyrosine kinase receptor, is essential for tumor development and metastasis in breast cancer [28]. Under normoxic circumstances, HER2 seems to activate tyrosine kinase receptors, stabilizing HIF-1α and stimulating VEGFA expression [29]. It has been recently demonstrated that HIF-1α has a part to play in HER2 upregulation and tumorigenesis by controlling anoikis [30]. As a result, the increased expression of HIF-1α and HER2 overexpression may be complementary instead of the result of hypoxia. Regardless of the mechanism behind HIF-1α elevated expression, its presence appears to aid in the aggressiveness of tumor behavior.
It's also remarkable that in the present study, there was no significant difference between ER + and TNBC group; when compared to TNBC and HER2- enhanced breast carcinomas, ER + /PR + /HER2- breast cancers are less aggressive [31]. Even though ER expression encourages breast cancer development, it is mostly a sign of better differentiation, which renders a tumor more susceptible to anti-ER treatment [32]. HIF-1α seems to downregulate ERα in this situation, adding to Tamoxifen resistance and deteriorating prognosis.
In conclusion, the present study explored HIF-1α, VEGF-A, and HK-I expression patterns in BC patients. Our findings demonstrated that HER2-positive tumors differed marginally from the other categories with statistically insignificant to non-existent difference. Moreover TNBC shows increased expression levels across the investigated variables. Overall, our study successfully addressed the association of HIF-1α, VEGF-A, and HK-I with various clinicopathological parameters in our patients. Despite the availability of treatment options, chemoresistance to the Rx’d drugs are the major deterrent in the better prognosis of breast cancer. Thus, the chance of relapse of cancer continues to be a challenge and therefore paves the quest to identify cellular pathways and pinpoint novel therapeutic targets. Although, HIFs and the downstream metabolic and angiogenic changes despite playing a significant role in the development, severity and therapeutic resistance to breast cancer, prove to be tough targets in the clinical set-up. This study may help in the identification of novel targets for combinatorial therapeutic modalities of BC further providing a rationale for improving existing cancer therapies. Thus a combinatorial approach of innovative anti-angiogenic (VEGFA) and metabolic partners (HK1) with standard treatments together with non-pharmaceutical strategies seems the potentially viable approach. Together, these findings may pave the way for developing newer potential drugable targets and their application in early non-invasive diagnostic modality thus enhancing the overall prognosis in BC patients. However, the small sample size is the limitation of this study.
Availability of data and materials
All data generated and/or analysed during this study are available from the corresponding author upon reasonable request.
Abbreviations
- BC:
-
Breast cancer
- HIF-1α:
-
Hypoxia-inducible factor-1alpha
- VEGF-A:
-
Vascular endothelial growth factor A
- HK-I:
-
Hexokinase-I
- qRT-PCR:
-
Quantitative Real-time polymerase chain reaction
- HR:
-
Hazard ratios
- HRE:
-
Hypoxia Responsive Element
- GAPDH:
-
Glyceraldehyde phosphate dehydrogenase
- PHD:
-
Prolyl hydroxylases
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Youn HJ, Han W. A review of the epidemiology of breast cancer in Asia: focus on risk factors. Asian Pac J Cancer Prev. 2020;21(4):867–80.
Coughlin SS. Epidemiology of Breast Cancer in Women. Adv Exp Med Biol. 2019;1152:9–29.
Dietze EC, Sistrunk C, Miranda-Carboni G, O’Regan R, Seewaldt VL. Triple-negative breast cancer in African-American women: disparities versus biology. Nat Rev Cancer. 2015;15(4):248–54.
Romero-Garcia S, Lopez-Gonzalez JS, Báez-Viveros JL, Aguilar-Cazares D, Prado-Garcia H. Tumor cell metabolism: an integral view. Cancer Biol Ther. 2011;12(11):939–48.
de Heer EC, Jalving M, Harris AL. HIFs, angiogenesis, and metabolism: elusive enemies in breast cancer. J Clin Invest. 2020;130(10):5074–87.
Semenza GL. Expression of hypoxia-inducible factor 1: mechanisms and consequences. Biochem Pharmacol. 2000;59(1):47–53.
Courtnay R, Ngo DC, Malik N, Ververis K, Tortorella SM, Karagiannis TC. Cancer metabolism and the Warburg effect: the role of HIF-1 and PI3K. Mol Biol Rep. 2015;42(4):841–51.
Nakayama K, Qi J, Ronai Z. The ubiquitin ligase Siah2 and the hypoxia response. Mol Cancer Res. 2009;7(4):443–51.
Gao T, Li JZ, Lu Y, Zhang CY, Li Q, Mao J, et al. The mechanism between epithelial mesenchymal transition in breast cancer and hypoxia microenvironment. Biomed Pharmacother. 2016;80:393–405.
Kappler M, Taubert H, Eckert AW. Oxygen sensing, homeostasis, and disease. N Engl J Med. 2011;365(19):1845–6; author reply 1846.
Shan B, Gerez J, Haedo M, Fuertes M, Theodoropoulou M, Buchfelder M, et al. RSUME is implicated in HIF-1-induced VEGF-A production in pituitary tumour cells. Endocr Relat Cancer. 2012;19(1):13–27.
De Francesco EM, Lappano R, Santolla MF, Marsico S, Caruso A, Maggiolini M. HIF-1α/GPER signaling mediates the expression of VEGF induced by hypoxia in breast cancer associated fibroblasts (CAFs). Breast Cancer Res. 2013;15(4):R64.
Ferrara N. VEGF and the quest for tumour angiogenesis factors. Nat Rev Cancer. 2002;2(10):795–803.
Zeng W, Liu P, Pan W, Singh SR, Wei Y. Hypoxia and hypoxia inducible factors in tumor metabolism. Cancer Lett. 2015;356(2 Pt A):263–7.
Azoitei N, Becher A, Steinestel K, Rouhi A, Diepold K, Genze F, et al. PKM2 promotes tumor angiogenesis by regulating HIF-1α through NF-κB activation. Mol Cancer. 2016;6(15):3.
Maxwell PH, Pugh CW, Ratcliffe PJ. The pVHL-hIF-1 system. A key mediator of oxygen homeostasis. Adv Exp Med Biol. 2001;502:365–76.
Agrawal A, Guttapalli A, Narayan S, Albert TJ, Shapiro IM, Risbud MV. Normoxic stabilization of HIF-1alpha drives glycolytic metabolism and regulates aggrecan gene expression in nucleus pulposus cells of the rat intervertebral disk. Am J Physiol Cell Physiol. 2007;293(2):C621-631.
Chiche J, Brahimi-Horn MC, Pouysségur J. Tumour hypoxia induces a metabolic shift causing acidosis: a common feature in cancer. J Cell Mol Med. 2010;14(4):771–94.
Tang M, Bolderson E, O’Byrne KJ, Richard DJ. Tumor Hypoxia Drives Genomic Instability. Front Cell Dev Biol. 2021;9:626229.
Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, et al. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol. 1996;16(9):4604–13.
Cerychova R, Pavlinkova G. HIF-1, Metabolism, and Diabetes in the Embryonic and Adult Heart. Front Endocrinol (Lausanne). 2018;9:460.
Semenza GL. HIF-1: using two hands to flip the angiogenic switch. Cancer Metastasis Rev. 2000;19(1–2):59–65.
van der Groep P, Bouter A, Menko FH, van der Wall E, van Diest PJ. High frequency of HIF-1alpha overexpression in BRCA1 related breast cancer. Breast Cancer Res Treat. 2008;111(3):475–80.
Schwab LP, Peacock DL, Majumdar D, Ingels JF, Jensen LC, Smith KD, et al. Hypoxia-inducible factor 1α promotes primary tumor growth and tumor-initiating cell activity in breast cancer. Breast Cancer Res. 2012;14(1):R6.
Yehia L, Boulos F, Jabbour M, Mahfoud Z, Fakhruddin N, El-Sabban M. Expression of HIF-1α and Markers of Angiogenesis Are Not Significantly Different in Triple Negative Breast Cancer Compared to Other Breast Cancer Molecular Subtypes: Implications for Future Therapy. PLoS One. 2015;10(6):e0129356.
Toikkanen S, Helin H, Isola J, Joensuu H. Prognostic significance of HER-2 oncoprotein expression in breast cancer: a 30-year follow-up. J Clin Oncol. 1992;10(7):1044–8.
Ménard S, Tagliabue E, Campiglio M, Pupa SM. Role of HER2 gene overexpression in breast carcinoma. J Cell Physiol. 2000;182(2):150–62.
Konecny GE, Meng YG, Untch M, Wang HJ, Bauerfeind I, Epstein M, et al. Association between HER-2/neu and vascular endothelial growth factor expression predicts clinical outcome in primary breast cancer patients. Clin Cancer Res. 2004;10(5):1706–16.
Whelan KA, Schwab LP, Karakashev SV, Franchetti L, Johannes GJ, Seagroves TN, et al. The oncogene HER2/neu (ERBB2) requires the hypoxia-inducible factor HIF-1 for mammary tumor growth and anoikis resistance. J Biol Chem. 2013;288(22):15865–77.
Li SP, Padhani AR, Taylor NJ, Beresford MJ, Ah-See MLW, Stirling JJ, et al. Vascular characterisation of triple negative breast carcinomas using dynamic MRI. Eur Radiol. 2011;21(7):1364–73.
Bos R, Zhong H, Hanrahan CF, Mommers EC, Semenza GL, Pinedo HM, et al. Levels of hypoxia-inducible factor-1 alpha during breast carcinogenesis. J Natl Cancer Inst. 2001;93(4):309–14.
Acknowledgements
All authors acknowledge all the participants for their contribution in this study and DA, MF acknowledge Department of Science and Technology, Govt. of India for financial assistance.
Funding
This research was supported by Grant provided by Department of Science and Technology (DST-SERB), New Delhi, India for Grant (EMR/2016/004794) and Institutional Intramural grant (SKIMS).
Author information
Authors and Affiliations
Contributions
MF and DA conceived the concept, MF carried out all the experiments. MF, GRB, DA performed the data analysis. NT, SZ provided the clinical samples, SB helped in immunohistochemistry analysis. BR, IM, RAR, SD, MAM, AAB helped in the technical refinement of the manuscript. DA finally refined the manuscript. Finally all the authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Committee Sher-i- Kashmir Institute of Medical Sciences, Srinagar (IEC/SKIMS Protocol # RP 07/2019). A written informed consent has been obtained from each participant. All procedures performed involving human participants were in accordance with the ethical standards of the Institutional Ethics Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standard.
Consent for publication
Our manuscript does not contain any individual person’s data in any form (including any individual details, images or videos).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farooq, M., Bhat, G.R., Besina, S. et al. Expression of HIF-1α and markers of angiogenesis and metabolic adaptation in molecular subtypes of breast cancer. transl med commun 8, 2 (2023). https://doi.org/10.1186/s41231-023-00135-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41231-023-00135-x