Abstract
Background
Phase angle (PhA) value is a useful tool for identifying cell membrane integrity dysfunction. It is known that metabolic syndrome (MetS) increases oxidative stress and inflammation; and consequently can promote cellular damage. We hypothesized that MetS and inflammatory blood markers could be associated with lower PhA values. Therefore, the aim of this study was to identify the association of PhA values with MetS and blood markers in individuals clinically screened for a lifestyle modification program.
Methods
In a cross-sectional study, 417 selected subjects (76 men and 341 women, 53.9 ± 9.4 years old) were evaluated. Assessments included clinics, anthropometric measures, body composition by bioimpedance, and laboratory blood markers, including plasma lipids, glucose, and C-reactive protein concentrations. According to the PhA median values, subjects were classified in low (≤6.3°) and high (>6.3°) PhA groups.
Results
Subjects with lower PhA values were older and showed lower body mass index, waist circumference, muscle mass index, creatinine, and uric acid; and higher gamma-GT and HDL cholesterol. Neither the presence of MetS nor the presence of the increasing number of MetS components was associated with PhA values. The logistic regression analysis adjusted for age, gender, body mass index, and muscle mass index showed that higher C-reactive protein concentrations (>3.0 mg/L) increased the odds of low PhA values (OR = 1.62; CI = 1.01–2.60).
Conclusion
Higher C-reactive protein concentrations increased the odds of low PhA independently of the presence of MetS. Additionally, contrary to our hypothesis, MetS was not associated with PhA values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The bioelectric impedance analysis is widely used for body composition and nutritional status assessment due to its simple, rapid, non-expensive, reproducible and non-invasive method. Beyond body composition, another important parameter obtained by bioelectrical impedance analysis (BIA) is the phase angle (PhA) value. PhA is the arc-tangent value from reactance and resistance and is considered an indicator of body cell mass and cell membrane integrity [1].
PhA has been used as a supporting tool for nutritional diagnostic in clinical practice and is used as a predictor of membrane integrity and cell mass [2]. Additionally, PhA has been associated with a number of clinical conditions, such as advanced liver fibrosis in patients chronically infected with hepatitis C virus [3], cancer [4], peritoneal dialysis [4], malnutrition [5], low muscle mass [6, 7], and higher mortality in patients with several diseases [8,9,10]. Recently, in hemodialysis patients, it was also observed that PhA values were associated with muscle function and overall quality of life [11].
Metabolic syndrome (MetS) is a clinical condition that predisposes the development of cardiovascular diseases and type-2 diabetes and is associated with higher risk of all-cause mortality [12]. MetS is closely related to increased body fat mass, visceral fat deposition, and insulin resistance, which constitute clinical conditions that require nutritional care. Additionally, MetS pathophysiology includes several comorbities such as inflammation, oxidative stress, pro-thrombotic, and pro-atherogenic processes [13,14,15,16].
As PhA value is a useful tool for identifying cell membrane integrity dysfunction and it is known that MetS increases oxidative stress and inflammation, which consequently can lead to cellular damage [15], we hypothesized that MetS and some blood markers related with this clinical condition could be associated with lower PhA values. Therefore, the aim of this study was to identify the association of PhA with MetS and blood markers in individuals clinically screened for a lifestyle modification program.
Methods
Individuals
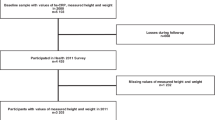
A cross-sectional study was conducted with individuals enrolled in the lifestyle-modification program “Mexa-se Pró-Saúde (Move for Health)” in Botucatu City, Brazil. This program offers primary care for non-communicable chronic diseases by promoting nutritional counseling and regular physical activity. Inclusion criteria were 35 years or older adults without metabolic or motor disabilities that could limit the practice of exercises. Exclusion criteria were the presence of other inflammatory diseases, such as cancer and rheumatoid arthritis; use of anti-inflammatory drugs; and those that did not realize all assessments. From a total of 587 subjects, 170 did not perform all assessments or were excluded during clinical evaluation. Then, 417 subjects (76 men and 341 women, 53.9 ± 9.4 years old) were studied. All subjects had signed an informed consent and the study was approved by the Human Research Ethics Committee of Botucatu Medical School (FMB), São Paulo State University (UNESP, Brazil) in accordance to the “Declaration of Helsinki” (Research Ethics Committee protocol 4049-2011).
Assessments
Body mass (kg) was measured by anthropometric scale platform (Filizola®) and height (m) was determined using a portable stadiometer (Seca®). Body mass index (BMI) was calculated (weight (kg)/height (m)2) and classified according to the World Health Organization [17]. Waist circumference (WC) was measured using the Sanny® steel anthropometric tape positioned at the midway point between the last rib and the iliac crest [17].
Whole-body bioelectrical impedance analysis was performed using a tetrapolar bioimpedance (Biodynamics®, Model 450, USA) applying an alternating electric current of 800 μA and 50 kHz. The measurements were in accordance with the procedures described by the National Institutes of Health Technology Assessment Conference Statement [18]. PhA in degrees (o) was calculated by using the equation (reactance/resistance) × (180/л). Since there is no consensus for PhA cutoff, we decided to use the PhA median value of our sample (6.3°) as the cut point, as described before [6]. The same cutoff was used for men and women since we tested and found no difference in PhA values according to sex (men 6.8 ± 0.8° vs. women 6.3 ± 0.8°, p = 0.57). This median value is supported by another study evaluating the same age group [19].
Subjects were previously instructed to not perform vigorous physical exercises for 24 h, to avoid alcohol and caffeinated drinks for 72 h before testing and previous emptying of the bladder. Women that were not at post-menopausal period were instructed to avoid menstrual period for analysis. Individuals with abnormal hydration status were excluded considering the normal values of total body water per lean mass of 69 to 75%, according to the bioimpedances’s manufacturer recommendations, ensuring greater reliability in the PhA values. Muscle mass was estimated using Janssen et al.’s equation [20] and muscle mass index (MMI) was calculated as MM (kg)/height2 [21].
Subjects were submitted to clinical evaluation for assessments of systolic (SBP) and diastolic (DBP) blood pressures as described previously [22].
Blood samples were collected after an overnight fasting in the same morning that BIA evaluation was performed. Laboratory analyses of lipid parameters (total, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol, and triglycerides), glucose, uric acid, urea, γ-glutamyl transferase (gamma-GT), and albumin were measured by dry chemistry (Vitros® 5600, Ortho Clinical Diagnostics, Johnson & Johnson Company, Raritan, NJ, USA) within 4 h after blood collection. Serum C-reactive protein (CRP) concentrations were measured by high-sensitivity immuno-nephelometric assay (Siemens Healthcare Diagnostics, Marburg, Germany).
MetS diagnosis was in accordance with NCEP-ATPIII criteria [23]. High waist circumference (WC >102 cm for men and >88 cm for women), hyperglycemia (FBG ≥100 mg/dL), hypertriglyceridemia (TG ≥150 mg/dL), reduced HDL-C (<40 mg/dL for men and <50 mg/dL for women), and hypertension (SBP ≥130 mmHg and/or DBP ≥85 mmHg) were considered as MetS components. MetS was diagnosed when three or more of these components were altered [23]. Low-grade inflammation was determined when CRP values were >3.0 mg/L [24]. Abnormal values of total cholesterol (≥200 mg/dL) and LDL cholesterol (≥130 mg/dL) were set according to the last Brazilian guidelines for dyslipidemia and atherosclerosis prevention (2013) [25] .
Statistical analyses
Statistical analyses were performed at SAS software, version 9.1.3. Descriptive data were presented as mean ± standard deviation (parametric variables) or median and interquartile range (non-parametric variables). We tested the differences between lower PhA (≤6.3°) and higher PhA (>6.3°) groups for parametric variables using independent t test, whereas for non-parametric variables using Mann-Whitney’s test. Chi-square was performed to evaluate the prevalence of MetS according to PhA groups. One-way ANOVA was performed to compare PhA values according to the number of altered MetS components. Logistic regression was used to determine the odds for lower PhA (≤6.3°) according to MetS and blood biomarkers, adjusted for age, sex, BMI, and muscle mass index. Statistical significance was set as 5% (p < 0.05) for all analyses.
Results
Among the entire sample, 28% of individuals were of normal weight; 30% overweight; and 42% obese. The total proportion of individuals with MetS was 52%, whereas in the higher PhA values group, MetS prevalence was 44% and in the lower PhA values, it was 56%, but no differences were found between groups (p > 0.05). Additionally, there was no difference in PhA values according to the increasing number of MetS components (Fig. 1).
Subjects with lower PhA values were older and showed lower BMI, WC, MMI, and diastolic blood pressure. The HDL cholesterol and gamma-GT concentrations were significantly higher in those with lower PhA values, whereas creatinine and uric acid concentrations were significantly lower in this group (Table 1). Additional individual’s characterization can be found in our previous research [6].
Logistic regression analysis showed that higher CRP concentration was the only parameter associated with lower PhA (Table 2). Those individuals with CRP ≥3.0 mg/L showed 62% more chance of having lower PhA values even after adjustment for age, sex, BMI, and MMI (OR = 1.62; 95%CI: 1.01–2.60). The presence of MetS and the other biochemical parameters showed no association with lower PhA values in all models analyzed.
Discussion
The main finding of this research was that higher concentrations of CRP increased the odds of low PhA regardless of sex, age, BMI, and MMI. Furthermore, contrary to our hypothesis, MetS was not associated with PhA. To the best of our knowledge, this is the first study showing such associations in individuals clinically screened for a lifestyle modification program.
A lower PhA value is considered a marker for reduced cell membrane integrity [2]. The inflammatory process is a well-known condition related to tissue injury and consequently cell membrane integrity disarrangement [26], and several studies with different clinical conditions also reported associations between PhA values and inflammatory markers [27,28,29]. Interestingly, adipose tissue seems to be the greatest target for leukocyte infiltration and also a source of inflammatory cytokines such as tumor necrosis factor alpha (TNF-α) [30]. TNF-α is a well-recognized apoptosis inductor, and more recently, a mechanistic process involving cell membrane integrity induced by activation of the TNF-α receptor was reported [31]; however, in our data, inflammation was associated with PhA independently of BMI. Additionally, we adjusted for BMI, and not for waist circumference, due to our research group has already shown that waist circumference is not associated with PhA [6]. Another hypothesis for the inverse association between PhA and inflammation could be an indirect effect of oxidative stress. High CRP concentrations is related to increased free radicals [32], which can lead to cellular damage [33] and probably could decrease PhA values. Although we have not evaluated specific oxidative stress markers, PhA was not associated with uric acid, that is responsible for 2/3 of total plasma antioxidant capacity [13]. Therefore, the probably mechanism for the observed relation between CRP and PhA may not be dependent of the increased oxidative stress; however, this affirmation cannot be concluded only based on uric acid concentration and more studies are necessary to evaluate the influence of oxidative stress on PhA.
In our descriptive analysis, it was noted that individuals with higher PhA values showed higher levels of uric acid and lower HDL-c. However, these biochemical variables were not associated with PhA, which shows that individuals with higher values of PhA also had higher waist circumference and BMI [6], and these biochemical variables were higher due to higher amount of adiposity in this group [34, 35]; therefore, there were no direct association between PhA with uric acid and HDL-c.
The presence of MetS is well recognized as related to low-grade inflammation and insulin resistance development [14]. However, even though the CRP were associated with PhA, as demonstrated, PhA values were not associated with the increasing number of MetS components and with other blood biomarkers. Recently, a cohort study also did not find association between some MetS components and PhA values [36], reinforcing our findings. Therefore, our data suggests that PhA values could be associated with an unspecific pro-inflammatory process and may be a useful tool for indirectly accessing it, independently of the presence of MetS.
We evaluated the odds to present PhA lower than 6.3°, a value that corroborates with the findings of Barbosa-Silva et al. (2005) [19] who studied the same age group of healthy subjects and found values of 7.3 ± 0.89° (6.12°; 8.68°) for men and 6.5 ± 0.87° (5.48°; 7.96°) for women. Although it is known that PhA values are higher in men [19], the median values were not different between sexes in our population. However, to avoid the influence of sex in our results, all analyses were adjusted for this variable. Other important adjusted variable was age, which is also known to be related with PhA [19] and MetS [37]. Additionally, a recent study [38] showed that age, fat-free mass, and height are the most important variables that explain PhA variances in healthy individuals. It is important to remember that we adjusted the analysis for muscle mass, which was estimated by an equation that has resistance value as one of the variables, such as PhA calculation. Therefore, this does not seem to be a limitation in our data because even after adjustments for MMI, the association remained significant, which showed that MMI did not indirectly adjusted PhA itself. Therefore, we showed that CRP was associated with PhA independently of these important confounding variables.
Some limitations should be illustrated at present study. This is a cross-sectional study; therefore, the cause-effect relationship between CRP and PhA values cannot be determined. Furthermore, our sample had higher proportion of females and is not representative of a larger community. This difference occurred because all subjects were spontaneously engaged with a lifestyle change program, and it is known that women are more concerned to change their lifestyle than men [39]. However, all analyses were adjusted for sex, ensuring the statistical control for this discrepancy. In addition, only one inflammatory marker was evaluated. Although CRP is considered the most powerful unspecific marker for inflammation, we did not analyze TNF-α, a pro-inflammatory cytokine that seems to be more related with cell plasma membrane instability [31]. However, we reinforce that this was the first study reporting the association between PhA values and low-grade inflammation marked by plasma CRP concentrations, independently of body composition and MetS diagnosis. Specificity and sensitivity of PhA values as well as cut points for detect inflammatory processes still need to be determined and should be carried out in future studies.
Conclusions
In conclusion, higher C-reactive protein concentrations increased the odds of low PhA independently of the presence of MetS. Additionally, contrary to our hypothesis, MetS was not associated with PhA values. Longitudinal studies are needed to confirm these results.
Abbreviations
- BF:
-
Body fat
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- gamma-GT:
-
γ-Glutamyltransferase
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- MetS:
-
Metabolic syndrome
- MMI:
-
Muscle mass index
- PhA:
-
Phase angle
- TNF-α:
-
Tumor necrosis factor alpha
- WC:
-
Waist circumference
References
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, et al. Bioelectrical impedance analysis—part I: review of principles and methods. Clin Nutr. 2004;23(5):1226–43.
Selberg O, Selberg D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol. 2002;86(6):509–16.
Dorna MS, Santos LA, Gondo FF, Augusti L, de Campos Franzoni L, Sassaki LY, Romeiro FG, de Paiva SA, Minicucci MF, Silva GF. Phase angle is associated with advanced fibrosis in patients chronically infected with hepatitis C virus. Life Sci. 2016;154:30–3.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430–53.
Kyle UG, Soundar EP, Genton L, Pichard C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Clin Nutr. 2012;31(6):875–81.
de França NAG, Callegari A, Gondo FF, Corrente JE, Mclellan KCP, Burini RC, de Oliveira EP. Higher dietary quality and muscle mass decrease the odds of low phase angle in bioelectrical impedance analysis in Brazilian individuals. Nutr Diet. 2016;73(5):474–81.
Dorna MS, Costa NA, de Oliveira EP, Sassaki LY, Romeiro FG, Paiva SAR, Minicucci MF, Silva GF. Association between phase angle, anthropometric measurements, and lipid profile in HCV-infected patients. Clinics. 2013;68(12):1555–8.
Norman K, Stobaus N, Zocher D, Bosy-Westphal A, Szramek A, Scheufele R, Smoliner C, Pirlich M. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am J Clin Nutr. 2010;92(3):612–9.
Ruiz-Margain A, Macias-Rodriguez RU, Duarte-Rojo A, Rios-Torres SL, Espinosa-Cuevas A, Torre A. Malnutrition assessed through phase angle and its relation to prognosis in patients with compensated liver cirrhosis: a prospective cohort study. Dig Liver Dis. 2015;47(4):309–14.
Wilhelm-Leen ER, Hall YN, Horwitz RI, Chertow GM. Phase angle, frailty and mortality in older adults. J Gen Intern Med. 2014;29(1):147–54.
Beberashvili I, Azar A, Sinuani I, Shapiro G, Feldman L, Stav K, Sandbank J, Averbukh Z. Bioimpedance phase angle predicts muscle function, quality of life and clinical outcome in maintenance hemodialysis patients. Eur J Clin Nutr. 2014;68(6):683–9.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97(7):2482–8.
de Oliveira EP, Burini RC. High plasma uric acid concentration: causes and consequences. Diabetol Metab Syndr. 2012;4:12.
Moreto F, de Oliveira EP, Manda RM, Torezan GA, Teixeira O, Michelin E, Burini RC. Pathological and behavioral risk factors for higher serum C-reactive protein concentrations in free-living adults—a Brazilian community-based study. Inflammation. 2013;36(1):15–25.
Roberts CK, Sindhu KK. Oxidative stress and metabolic syndrome. Life Sci. 2009;84(21–22):705–12.
Takahashi MM, de Oliveira EP, de Carvalho AL, de Souza Dantas LA, Burini FH, Portero-Mclellan KC, Burini RC. Metabolic syndrome and dietary components are associated with coronary artery disease risk score in free-living adults: a cross-sectional study. Diabetol Metab Syndr. 2011;3:7.
Report of a WHO Expert Committee. Physical status: the use and interpretation of anthropometry. World Health Organ Tech Rep Ser. 1995;854:1–452.
Bioelectrical impedance analysis in body composition measurement: National Institutes of Health Technology Assessment Conference Statement. Am J Clin Nutr 1996, 64(3 Suppl):524S-532S.
Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson Jr RN. Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr. 2005;82(1):49–52.
Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. 2000;89:465–71.
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159(4):413–21.
Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão Arterial. Rev Bras Hipertens. 2010;17(1):4-64.
de Lemos AS, Wolfe ML, Long CJ, Sivapackianathan R, Rader DJ. Identification of genetic variants in endothelial lipase in persons with elevated high-density lipoprotein cholesterol. Circulation. 2002;106(11):1321–6.
Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107(3):363–9.
Xavier HT, Izar MC, Faria Neto JR, Assad MH, Rocha VZ, Sposito AC, Fonseca FA, dos Santos JE, Santos RD, Bertolami MC, et al. V Brazilian Guidelines on Dyslipidemias and Prevention of Atherosclerosis. Arq Bras Cardiol. 2013;101(4 Suppl 1):1–20.
Lowe GD, Fowkes FG, Dawes J, Donnan PT, Lennie SE, Housley E. Blood viscosity, fibrinogen, and activation of coagulation and leukocytes in peripheral arterial disease and the normal population in the Edinburgh Artery Study. Circulation. 1993;87(6):1915–20.
Emerenziani S, Biancone L, Guarino MPL, Balestrieri P, Stasi E, Ribolsi M, Rescio MP, Altomare A, Cocca S, Pallone F, Cicala M. Nutritional status and bioelectrical phase angle assessment in adult Crohn disease patients receiving anti-TNFalpha therapy. Dig Liver Dis. 2017;49(5):495–9.
Demirci MS, Demirci C, Ozdogan O, Kircelli F, Akcicek F, Basci A, Ok E, Ozkahya M. Relations between malnutrition-inflammation-atherosclerosis and volume status. The usefulness of bioimpedance analysis in peritoneal dialysis patients. Nephrol Dial Transplant. 2011;26(5):1708–16.
Beberashvili I, Azar A, Sinuani I, Kadoshi H, Shapiro G, Feldman L, Sandbank J, Averbukh Z. Longitudinal changes in bioimpedance phase angle reflect inverse changes in serum IL-6 levels in maintenance hemodialysis patients. Nutrition. 2014;30(3):297–304.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404.
Cai Z, Jitkaew S, Zhao J, Chiang HC, Choksi S, Liu J, Ward Y, Wu LG, Liu ZG. Plasma membrane translocation of trimerized MLKL protein is required for TNF-induced necroptosis. Nat Cell Biol. 2014;16(1):55–65.
Kotani K, Sakane N. C-reactive protein and reactive oxygen metabolites in subjects with metabolic syndrome. J Int Med Res. 2012;40(3):1074–81.
Janssen YM, Van Houten B, Borm PJ, Mossman BT. Cell and tissue responses to oxidative damage. Lab Invest. 1993;69(3):261–74.
de Oliveira EP, Manda RM, Torezan GA, Corrente JE, Burini RC. Dietary, anthropometric, and biochemical determinants of plasma high-density lipoprotein-cholesterol in free-living adults. Cholesterol. 2011;2011:851750.
de Oliveira EP, Moreto F, Silveira LV, Burini RC. Dietary, anthropometric, and biochemical determinants of uric acid in free-living adults. Nutr J. 2013;12:11.
Piglowska M, Kostka T, Drygas W, Jegier A, Leszczynska J, Bill-Bielecka M, Kwasniewska M. Body composition, nutritional status, and endothelial function in physically active men without metabolic syndrome—a 25 year cohort study. Lipids Health Dis. 2016;15:84.
de Oliveira EP, Mclellan KC, Vaz De Arruda Silveira L, Burini RC. Dietary factors associated with metabolic syndrome in Brazilian adults. Nutr J. 2012;11:13.
Gonzalez MC, Barbosa-Silva TG, Bielemann RM, Gallagher D, Heymsfield SB. Phase angle and its determinants in healthy subjects: influence of body composition. Am J Clin Nutr. 2016;103(3):712–6.
Figueiredo W. Assistência à saúde dos homens: um desafio para os serviços de atenção primária. Ciênc Saúde Coletiva. 2005;10(1):105–9.
Funding
The work was supported by CAPES and CNPq.
Author information
Authors and Affiliations
Contributions
FM participated in the collection and interpretation of the data and wrote the manuscript. NAGF participated in the collection of data and revised the manuscript. FFG and AC collaborated in the collection and interpretation of the data. JEC carried out the statistical analysis. RCB contributed in revising the manuscript. EPO carried out the conception and design of the study, participated in the interpretation of the data, wrote and contributed to the revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
The study was approved by the Human Research Ethics Committee of Botucatu Medical School (FMB), São Paulo State University (UNESP, Brazil) in accordance with the “Declaration of Helsinki” (Research Ethics Committee protocol 4049-2011).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Moreto, F., de França, N.A.G., Gondo, F.F. et al. High C-reactive protein instead of metabolic syndrome is associated with lower bioimpedance phase angle in individuals clinically screened for a lifestyle modification program. Nutrire 42, 15 (2017). https://doi.org/10.1186/s41110-017-0043-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-017-0043-0