Abstract
Background
Numerous cardio-metabolic risk factors influence screen-related behaviors in children and adolescents. Numerous studies with inconsistent results revealed a relationship between blood pressure and screen time in the children and adolescents. This systematic review and meta-analysis summarized the data regarding the relationship between screen time and hypertension (HTN) in children and adolescents.
Methods
We examined three electronic databases, including Scopus, PubMed, and Embase to find the recent research on the relationship between screen time and HTN up to 19 July 2022. Twenty papers were included in the final two-class and dose–response meta-analysis. We conducted subgrouping to identify the source of heterogeneity.
Results
The highest category of screen time increased the odds of HTN by 8% [odds ratio (OR): 1.15; 95% confidence interval (CI): 1.08, 1.23; P < 0.001; I2 = 83.20%] and 1.9 mmHg increase in systolic blood pressure [weighted mean difference (WMD): 1.89; 95% CI: 0.18–3.62; P = 0.030; I2 = 83.4]. However, there was no significant difference in diastolic blood pressure. Moreover, screen time in hypertensive children and adolescents was 0.79 h (47.4 min) higher than normotensive subjects (WMD: 0.79; 95% CI: 0.02, 1.56; P = 0.046; I2 = 92.8). A departure from linearity was observed between increased screen time [digital video discs, personal computers, and video games and HTN (Pnonlinearity = 0.049).
Conclusion
This systematic meta-analysis review is the first to demonstrate a positive correlation between screen time and HTN in children and adolescents.
Similar content being viewed by others
Introduction
Hypertension (HTN) and high blood pressure have been considered major health problems among children and adolescents in recent decades [1]. Both pre-HTN and HTN are on the rise globally. In this respect, the results of a recent meta-analysis conducted on more than 54,196 participants showed that the pooled prevalence of hypertension was 5.5% (95% CI: 4.2–6.9), while the prevalence of slightly increased blood pressure among children and teenagers aged two to19 was 12.7% (95% CI: 2.1–30.4) [2, 3].
HTN in childhood is associated with early cardiovascular events like congestive heart failure (CHF), left ventricular hypertrophy (LVH), and increased morbidity and mortality in adulthood [4, 5]. Affecting more than 2.5–17.3% of adolescents [6], HTN in childhood and adolescence is described to track into adulthood and is associated with major cardiovascular problems such as heart failure, stroke, and congestive heart disease [1, 7]. In recent years, the increasing prevalence of HTN among children and adolescents in numerous areas has been a major concern [1, 8], which highlights the further need for health-related interventions.
Sedentary behaviors are well-known risk factors of non-communicable diseases and are associated with high cardiovascular-related mortalities in prospective longitudinal studies [9]. In fact, sedentary behaviors are independent risk factors for chronic cardiovascular disease, meaning that being “sedentary” is associated with the prevalence of numerous diseases, even among those who do enough exercise [10,11,12].
More importantly, screen time dramatically increased during the COVID-19 pandemic. In this regard, several studies warned about the health consequences of this issue and warranted the need for health programs like encouraging regular physical activity, promoting educational opportunities, and increasing social support during the COVID-19 pandemic [13,14,15,16].
Among all the sedentary behaviors, screen-based sitting activities (such as using a computer, watching TV, and playing video games) need specific interventions because they are major contributors to overall sedentary time and are highly prevalent among children and adolescents [17,18,19,20,21]. The American Academy of Pediatrics (AAP) recommended reducing the daily screen time of children and teenagers to less than two hours, with no screen time for children under the age of two and less than one hour per day for children aged two to five [22, 23].
Screen-related behaviors are associated with a high prevalence of HTN, particularly among boys [17, 24]. The underlying mechanisms include increased arteriolar narrowing [25], obesity and poor sleep quality related to excessive screen use [24], increased stress, amygdala activation, as well as altering both sympathetic efferent output and responsiveness of hypothalamic–pituitary–adrenal axis [26, 27].
Several studies have been conducted on the correlation between HTN and screen time in children and adolescents. However, the achieved results regarding the role of screen type, gender, age, and geographic location are highly inconsistent. There is no summarized analysis of the quantity and quality of the correlation between screen time and HTN in children. Accordingly, this systematic review study was conducted to evaluate the relationship between screen time and HTN in children and adolescents. Also, in a dose–response meta-analysis, we further investigated the role of different factors such as screen type, age group, gender, time, and geographical distributions.
Materials and methods
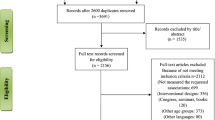
The results of this systematic review and meta-analysis were reported using the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) (Additional file 1: Table S1) [28]. The PRISMA 2020 statement includes a checklist to guide reporting of systematic reviews and consists of a 27-item checklist and a four-phase flow diagram. These items have been adapted for use by researchers conducting systematic reviews. Also, the abstract was developed using the PRISMA extension's comprehensive 12-item checklist. [29].
Search strategy
In this study, three electronic databases, including Scopus, PubMed, and Embase, were searched systematically to find the existing analyses of the association between screen time and HTN up to 19 July 2022. There search was limited to English language articles. Also, we manually searched the reference lists of all the retrieved systematic reviews, papers, and meta-analyses for any publications that may have been overlooked.
Our search method for each of these electronic databases was based on a combination of PubMed's MeSH (Medical Subject Headings) phrases and free-text words. The PubMed search method was as follows: [(hypertension) OR (HTN) OR (systolic blood pressure) OR (diastolic blood pressure) OR (SBP) OR (DBP) OR (blood pressure) OR (hypertension) AND (child) OR (children) OR (teen) OR (adolescent) OR (boy) OR (girl) OR) OR (pediatric) OR (youth) OR (teenager) OR (toddler) AND ((sedentary behavior) OR (screen time) OR (sitting time) OR (sitting time) OR (television view) OR (watching television) OR (computer use) OR (internet use) OR (smartphone) OR (video game) OR (electronic game) OR (depress) (Additional file 1: Table S2).
Study selection
Our search approach generated 2821 articles in total. We imported the remaining papers (n = 2519) into EndNote after deleting the duplicates. Two investigators checked all articles independently (SA, MAF). Then, out of 1396 manuscripts that remained for full-text screening, 1376 articles were rejected due to inappropriate subjects, different designs, involving other age groups and languages, being conference and seminar reviews, investigating other chronic diseases not related to metabolic abnormalities (like asthma, intellectual disabilities, depression), and evaluating different parameters. Any disagreements between reviewers were settled through dialogue. The final meta-synthesis included 20 manuscripts (Fig. 1).
Inclusion and exclusion criteria
The following conditions were considered as inclusion criteria: (1) observational research (case–control, cross-sectional, or cohort studies with baseline assessment of study parameters); (2) studies examining the correlation between screen time and hypertension or blood pressure (isolated systolic or diastolic HTN or total HTN, systolic or diastolic blood pressure); (3) research conducted on children and adolescents aged 18 or older; and (4) studies presenting the odds ratio of the relationship between HTN and screen time or providing mean ± standard deviation (SD) of systolic blood pressure (SBP) and diastolic blood pressure (DBP). Only cross-sectional data from cohort studies (at baseline or after a period of follow-up) that reported odds ratio (OR) were considered. Studies that did not provide an OR or mean (SD) blood pressure values were also disqualified. These included clinical trials, systematic reviews, meta-analyses, case reports, case series, experiments, short communications, letters to the editor, and those that considered the associations other than the one between screen time and HTN.
Data extraction and quality assessment of included studies
Two researchers independently extracted data using a normal Excel extraction datasheet. The following information was extracted from each article: first author, journal name, nation, publication year, age range of subjects, research design, final sample size and the number of participants in each category of screen time or blood pressure, adjusted covariate, gender, setting, blood pressure, screen time definition, blood pressure and screen time measurement tools, and major findings. Discrepancies between reviewers were resolved by discussion.
The Agency for Healthcare Research and Quality (AHRQ) checklist was used to evaluate the listed studies for their methodological quality [30]. The AHRQ guidance on evaluating the strength of evidence differentiates between the evaluation of precision and risk of bias. The types of bias that the AHRQ checklist evaluates include selection bias, performance bias, attrition bias, detection bias, and reporting bias [31]. For each item, one point was given for a "YES" response, and zero point was given for a "NO" or "UNCLEAR" response. Overall, the quality ranged from poor (a score of 0–3) to satisfactory (a score of 4–7) or excellent (a score of 8 and greater). In addition, the quality of studies was not considered for including or excluding the articles (Additional file 1: Table S3). We also evaluated the certainty of evidence using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework (Additional file 1: Table S4) [32, 33].
Statistical analysis
We utilized STATA version 13 (STATA Corp, College Station, TX, USA) to analyze data. Also, p values less than 0.05 were regarded as statistically significant.
Statistical analysis of two-class meta-analysis
Two-class meta-analysis is the comparison of an outcome variable between two study groups regardless of the nature of variable. The present study identified three approaches to two-class meta-analysis as a bivariate analysis: first, the studies examining the relationship between odds of total or isolated HTN and screen time; second, the investigations reporting the comparison between SBP or DBP [mean (SD)] in those with the highest versus lowest screen times; and third, the studies evaluating the comparison of screen time [mean (SD)] in hypertensive versus normotensive children and adolescents. Therefore, the OR and 95% confidence interval (CI) or the mean and SD of the variable were used to determine the unstandardized effect size calculated by the pooled estimate of the OR or the weighted mean difference (WMD) with 95% CI.
When ORs were not provided but information about exposure to the variable across groups was available, we used the prevalence odds ratios (PORs) proposed by Pearce N as the most accurate way to gauge the magnitude of an effect [34] as follows: \(\mathrm{POR}=\left[\frac{P1}{1-P1}\right]/\left[\frac{P0}{1-P0}\right]\). In this formula, P0 and P1 represent the prevalence in exposed and non-exposed groups, respectively. The approach proposed by Hozo et al. [35] was utilized when the median and range were reported rather than the mean and SD. In this method, the median values are regarded to be the best approximation of the mean when the sample size is greater than 25 and the SD is determined as follows: \({S}^{2}\approx (\frac{1}{12}(\frac{{\left(a-2m+b\right)}^{2}}{4}+{\left(b-a\right)}^{2}\)) [35]; while m is median, a and b are low and high end of the ranges, respectively.
The method proposed by Walter and Yao as an upgraded version of the "range" method was applied for missing SDs. In this method, SD is calculated as follows: SD = (b−a)/4 [36, 37], where a and b are low and high end of the ranges, respectively. We assumed that each category would have an equal number of participants if the number of participants in each category was not provided.
All the screen time data were converted to min/day for dose–response meta-analysis or hours/day for two-class meta-analysis. Cochran's Q and I2 tests were utilized to identify the heterogeneity between the studies as follows: I2 ˂ 25%, no heterogeneity; I2 = 25–50%, moderate heterogeneity; and I2 > 50%, high heterogeneity [38]. The heterogeneity was considered significant if either the Q statistic had P < 0.1 or I2 > 50%.
As suggested by Riley et al. [39], the random-effects model was used due to the high heterogeneity values. We used subgrouping to identify the possible sources of heterogeneity based on the continent, screen type, HTN type, gender, age group, screen time measurement tool, setting, sample size, and quality of the study. Publication bias was evaluated using the Begg's funnel plots, Begg's adjusted rank correlation, and Egger's regression asymmetry tests.
Statistical analysis of dose–response meta-analysis
The dose–response meta-analysis included studies that examined at least three categories for screen time and the odds or prevalence of HTN as a multivariate analysis. Accordingly, nine individual studies in five articles were included [6, 24, 26, 40, 41]. If possible, the isolate dose–response meta-analysis was applied to the variables included in at least three individual studies. For example, a separate dose–response analysis was applied for the studies performed among children, adolescents, or a combination of both, as well as for the studies that evaluated watching TV, using personal computers (PC), and playing video games (VG).
The median point for each category of screen time was determined. If medians were not supplied, they were calculated using the midpoint of the minimum and maximum values. When the minimum or maximum screen time categories were undefined, the screen time was estimated by assuming a similar interval and calculating the midpoint. Assuming ORs and CIs of 1, the lowest category was the reference category.
By creating limited cubic splines with three knots at defined percentiles (10%, 50%, and 90%) of distribution, we were able to examine the potential nonlinear relationships using random-effects dose–response meta-analysis and derive study-specific ORs, which were reported as ORs of HTN for every 1, 50, 100, and 200 min increment in screen time.
Results
Characteristics of included studies
Table 1 provides the details of the evaluated studies. We included 20 studies in the two-class meta-analysis with a total number of 151,763 participants [4, 6, 17,18,19,20, 24, 26, 40,41,42,43,44,45,46,47,48,49,50,51]. Several studies reported the results in different subgroups of HTN, isolated SBP or DBP, genders, or age groups. The results were therefore isolated as individual studies.
Solomon-Moore et al. [42] evaluated the correlation between inactivity and blood pressure in primary school children. This study comprised eight subgroups that individually evaluated isolated systolic and diastolic HTN at ages nine and 11 in both girls and boys. The researchers reported a positive correlation between inactivity and high isolated systolic HTN among girls [OR: 1.08 (1.01 to 1.16)].
Pedersen et al. [40], in a cross-sectional study of Odense Child Cohort study, reported the relationship between parent-reported screen time either in daytime or before bedtime with hypertension in children aged five; prolonged exposure to screen before bedtime (two to five days/week and more than six days/week) was positively correlated with high blood pressure [OR: 1.57 (95% CI: 1.02–2.42) and OR: 1.82 (95% CI: 1.18–2.89), respectively].
Oliveira et al. [6] analyzed the correlation between several components of screen time, such as watching television, playing video games, and/or using the PC for less than two hours, two to four hours, and more than four hours in both genders. So, a total of four studies demonstrating a positive correlation between TV television and HTN in boys, but not girls, were included in the analysis.
Karatzi et al. [4] investigated the correlation between screen time and isolated systolic hypertension (ISH), isolated diastolic hypertension (IDH), and total HTN separately for boys and girls; therefore, it was included as six isolate studies in the meta-analysis. According to the results, only boys with higher ISH had higher screen time (P = 0.002). Also, a higher screen time was correlated with significantly higher odds of ISH [OR: 1.13 (CI: 1.04–1.23)]. Meanwhile, no association among girls was reported.
Wyszyńska et al. [43] analyzed the correlation between screen time and HTN in intellectually disabled children compared with the control group. So, we only included the results of healthy children and adolescents. The results were included as six individual studies analyzing the correlation between screen time and odds of HTN in school days and weekends in normotensive, pre-hypertensive, and hypertensive children and adolescents. According to the results, screen time of more than 2 h/day on school days was correlated with higher odds of HTN [2.74 (1.25–6.04)].
Two separate studies demonstrating a relationship between screen time and the risk of pre-HTN and HTN, such as that conducted by Gui et al. [43], were included in the meta-analysis. In this study, subjects with a screen time of more than 2 h/day had 5% and 6% higher risks of pre-HTN and HTN, respectively.
The study by Berendes et al. [18] evaluated the correlation between HTN and TV/video games or PC separately and reported higher odds of HTN in people with high screen-related behaviors. Similarly, Byun et al. [48] conducted two individual studies on the association between HTN and TV or PC/video games and reported higher odds of HTN among those with more than 2 h/day TV and video CD activity and more than 0.5 h/day PC exposure (P < 0.001). Carson et al. [41] reported the association between TV or PC and HTN, which was included as two studies. The authors reported no significant relationship between the odds of HTN and screen behaviors.
Hardy et al. [50] investigated the odds of ISH, IDH, and total HTN in adjusted and unadjusted models for boys and girls. So, five individual data sets were extracted to be included in the two-class meta-analysis; a significant association was only reported for the OR of higher DBP in boys with more than 2 h/day screen-related behaviors [OR: 3.30; CI: 1.35–8.12; P < 0.001)].
Five other studies [20, 24, 26, 45, 51] were included as single studies; for example, the study by Zou et al. [24], which reported a significant correlation between smartphone addiction and HTN among junior school students in China [OR: 2.205, 95% CI: 1.273–3.820].
The results of the two-class meta-analysis
The present two-class meta-analysis demonstrated the correlation between OR of HTN and screen time (Fig. 2A). High levels of screen time were correlated with an increased risk of HTN by about 15% (OR: 1.153; CI: 1.076, 1.234; P < 0.001; I2 = 83.2%).
Association between screen time and A pooled odds ratio (OR) of hypertension; B weighted mean difference (WMD) with 95% confidence interval (CI) of SBP, C weighted mean difference (WMD) with 95% confidence interval (CI) of DBP, and D weighted mean difference (WMD) with 95% confidence interval (CI) for the screen time in hypertensive versus normotensive youth. I2 represents the degree of heterogeneity
The comparison of SBP and DBP between the highest and lowest categories of screen time using a two-class meta-analysis is presented in Fig. 2B, C. As can be seen, the maximum level of screen time was associated with a 1.9 mmHg increase in SBP (WMD: 1.898; CI: 0.181, 3.616; P = 0.030; I2 = 83.4); however, 1.42 mmHg increase in DBP in the highest versus lowest screen time categories was not statistically significant (WMD = 1.420; CI = − 0.383, 3.223; P = 0.123; I2 = 89.3).
Figure 2D presents the results of the two-class meta-analysis of the comparison of screen time in hypertensive versus normotensive children and adolescents. As can be seen, hypertensive children and adolescents had 0.79 h (47.4 min) higher screen time compared with normotensive children and adolescents (WMD: 0.791; CI: 0.015, 1.566; P = 0.046; I2 = 92.8).
Subgrouping was performed to find the source of heterogeneity (Table 2). Subgroupings according to the continent, HTN type, or age group were accompanied by a slight reduction in heterogeneity; however, there was no heterogeneity in the case of girls, as well as the studies that used an accelerometer to measure screen time. Also, in subgrouping according to sample size, there was a reduction in heterogeneity values in all the subgroups (e.g., 1000>, 1000–5000, and 5000≤).
The results of dose–response meta-analysis
Figure 3 displays the dose–response relationship between screen time and hypertension, indicating a nonlinear correlation between longer periods of watching TV or playing video games and the development of hypertension (Pnonlinearity = 0.049). However, there was no deviation from linearity in the link between HTN and screen time among teenagers (Additional file 1: Figure S1A), children + adolescents (Additional file 1: Figure S1B), and TV (Additional file 1: Figure S1C). A separate analysis for children was not possible because the number of studies was not sufficient for figuring at least three cubic display-knots. The dose–response associations for all subgroupings were statistically significant except for those studies that assessed only TV as the screen type (P < 0.05).
Table 3 depicts the details of the dose–response association. It can be inferred that by 50-, 100-, and 150-min increments in screen time, there is 17%, 38%, and 92% increased risk of hypertension among children, 8%, 17%, and 32% in teenagers, and 14%, 31%, and 72% in the combination of children and adolescents. Accordingly, a 4%, 10%, and 21% increase in the odds of HTN was observed with 50-, 100-, and 150-min increases in screen time of TV, video games, and PC; these increments for TV were 13%, 27%, and 63%, respectively.
The results of quality assessment and publication bias
According to the quality evaluation results based on the AHRQ checklist (Additional file 1: Table S3), while 18 individual studies had average quality scores, 26 studies had very high quality. Publication bias was assessed using the OR funnel plot for HTN (Additional file 1: Figure S1). Additionally, the publication bias was clarified using Begg's and Egger's regression tests.
We found no evidence of publication bias for any of the measured variables [OR of HTN and screen time: Egger’s test (P = 0.811) and Begg’s test (P = 0.800); SBP in highest versus lowest screen time category: Egger’s test (P = 0.600) and Begg’s test (P = 0.624); DBP in highest versus lowest screen time category: Egger’s test (P = 0.771) and Begg’s test (P = 0.497); and screen time in hypertensive versus normotensive children and adolescents: Egger’s test (P = 0.072) and Begg’s test (P = 0.435)].
Discussion
This systematic review and meta-analysis evaluated the findings of studies examining the association between screen time and blood pressure in children and adolescents. The results revealed that high screen time increased the odds of HTN by 7% and SBP by 1.898 mmHg. This warrants the need for educational or therapeutic interventional programs to overcome this health issue among children and adolescents.
Increased blood pressure among children due to sedentary behaviors is associated with increased brachio-ankle pulse wave velocity and intima-media thickness [52, 53]. Although the correlation between HTN and screen time was attributed to obesity and overweight in several studies [54, 55], in some other studies, the relationship between screen time and HTN was independent of body weight status. While Tebar et al. [56] reported that the association between HTN and sedentary behavior was more pronounced among normal-weight rather than obese children, Wennberg et al. [57] stated that TV watching was associated with HTN independent of BMI status [57]. Several other studies also reported similar results [58, 59].
In our subgrouping according to gender, the correlation between HTN and screen time was only significant among boys or the combination of both genders, but not among girls. Generally, boys have a higher tendency toward screen-related behaviors compared with girls. This was more pronounced in engagement in video games, videocassette recorder (VCR) playing [60], and television watching [61]; also, boys were more engaged in long-lasting screen-related activities [62,63,64]. In addition, the prevalence of HTN varies based on gender; generally, boys have higher baseline SDP and DBP compared with girls because of higher stroke volume and higher total peripheral resistance during stressful situations [18, 65, 66].
In subgrouping the results according to age, the relationship between HTN and screen time was only significant among children, but not adolescents; it seems that children at lower ages are at greater risk of sleep disturbance and low sleep duration due to screen-related behaviors [67,68,69], and sleep disorder is one of the leading causes of childhood HTN [70, 71].
In subgrouping by continent, the results for studies done in Europe and the United States were statistically significant, whereas the results for other groups were insignificant. This may be explained by the greater volume of investigations conducted on these two continents.
The nonlinear association was observed in the correlation between high screen time for DVD, PC, and video games and HTN (Pnonlinearity = 0.049). This nonlinear association revealed the highest odds of HTN (~1.4) in 100–150-min/day screen time of DVDs, PC, and video games, which is compatible with the recommendations of the AAP on reducing the daily screen time of children and teenagers to less than two hours [22].
The current study had some limitations. First, we only included observational studies in the meta-analysis, which makes causal inference impossible. Second, there was no study evaluating the separate effects of video games. So, the pure effect of video games as a screen type on blood pressure could not be extracted.
In conclusion, the findings of this review can be helpful because of the growing tendency to screen-related behaviors during the COVID-19 pandemic, which limited the usual physical activities of children and adolescents outdoors and made them follow their school lessons online. So, policymakers should be aware of the future health consequences of limited physical activity, even at young ages, and design programs to substitute children’s screen-addictive behaviors with regular physical activities either at home or outside. Another critical issue is the high prevalence of overeating behaviors and higher intakes of junk and fast foods during screen watching, which is a strong promoter of obesity, metabolic syndrome, and HTN independently of body weight status [72,73,74,75,76,77]. Therefore, educating families to improve dietary behaviors and reduce “empty calorie” eating is essential.
Availability of data and materials
The data are available upon reasonable request from the corresponding author.
References
Karatzi K, Protogerou AD, Moschonis G, et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: the Healthy Growth Study. Atherosclerosis. 2017;259:128–33.
Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, Nansseu JR. Prevalence of elevated blood pressure in children and adolescents in Africa: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e375–86.
Tang D, Bu T, Feng Q, Liu Y, Dong X. Differences in overweight and obesity between the North and South of China. Am J Health Behav. 2020;44(6):780–93.
Karatzi K, Moschonis G, Botelli S, et al. Physical activity and sedentary behavior thresholds for identifying childhood hypertension and its phenotypes: the Healthy Growth Study. J Am Soc Hypertens. 2018;12(10):714–22.
Putrawan HA, Antariksa B, Yunus F, Basalamah MA, Nurwidya F. Prevalence of pulmonary hypertension in Indonesian patients with stable chronic obstructive pulmonary disease. J Nat Sci Biol Med. 2019;10(1):49.
Oliveira L, Ritti-Dias RM, Farah BQ, et al. Does the type of sedentary behaviors influence blood pressure in adolescents boys and girls? A cross-sectional study. Cien Saude Colet. 2018;23(8):2575–85.
Ulaganathan V, Kandiah M, Shariff ZM. A case–control study on the association of abdominal obesity and hypercholesterolemia with the risk of colorectal cancer. J Carcinog. 2018;17:4.
Laurent S, Mancia G, Morales-Olivas F. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens. 2009;27:1719–42.
Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blair SN. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42(5):879.
Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005.
Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. J Am Coll Cardiol. 2011;57(3):292–9.
Kar S, Khandelwal B. Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J Nat Sci Biol Med. 2015;6(2):356.
Nagata JM, Abdel Magid HS, Pettee Gabriel K. Screen time for children and adolescents during the coronavirus disease 2019 pandemic. Obesity. 2020;28(9):1582–3.
Qin F, Song Y, Nassis GP, et al. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. Int J Environ Res Public Health. 2020;17(14):5170.
Guan H, Okely AD, Aguilar-Farias N, et al. Promoting healthy movement behaviours among children during the COVID-19 pandemic. Lancet Child Adolescent Health. 2020;4(6):416–8.
Zhou J, Li Z, Meng H, Chang Y-C, Peng N-H, Wei B. Chinese parental awareness of Children’s COVID-19 protective measures. Am J Health Behav. 2021;45(4):657–64.
Barstad LH, Júlíusson PB, Johnson LK, Hertel JK, Lekhal S, Hjelmesæth J. Gender-related differences in cardiometabolic risk factors and lifestyle behaviors in treatment-seeking adolescents with severe obesity. BMC Pediatr. 2018;18(1):1–8.
Berendes A, Meyer T, Hulpke-Wette M, Herrmann-Lingen C. Association of elevated blood pressure with low distress and good quality of life: results from the nationwide representative German Health Interview and Examination Survey for Children and Adolescents. Psychosom Med. 2013;75(4):422–8.
Berentzen NE, Smit HA, Van Rossem L, et al. Screen time, adiposity and cardiometabolic markers: mediation by physical activity, not snacking, among 11-year-old children. Int J Obes. 2014;38:1317–23.
Christofaro DGD, De Andrade SM, Cardoso JR, Mesas AE, Codogno JS, Fernandes RA. High blood pressure and sedentary behavior in adolescents are associated even after controlling for confounding factors. Blood Press. 2015;24(5):317–23.
Fairman RT, Weaver SR, Akani BC, Dixon K, Popova L. “ You have to vape to make it through”: E-cigarette outcome expectancies among youth and parents. Am J Health Behav. 2021;45(5):933–46.
Pappas S. What do we really know about kids and screens? 2020; Available from: https://www.apa.org/monitor/2020/04/cover-kids-screens. Accessed: 2020
Kamolthip R, Fung XC, Lin C-Y, Latner JD, O’Brien KS. Relationships among physical activity, health-related quality of life, and weight stigma in children in Hong Kong. Am J Health Behav. 2021;45(5):828–42.
Zou Y, Xia N, Zou Y, Chen Z, Wen Y. Smartphone addiction may be associated with adolescent hypertension: a cross-sectional study among junior school students in China. BMC Pediatr. 2019;19(1):310.
Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: literature review and case study. Environ Res. 2018;164:149–57.
Pardee PE, Norman GJ, Lustig RH, Preud’homme D, Schwimmer JB. Television viewing and hypertension in obese children. Am J Prev Med. 2007;33(6):439–43.
Storz MA. The role of vegan diets in lipotoxicity-induced beta-cell dysfunction in type-2-diabetes. J Popul Ther Clin Pharmacol. 2020;27(SP2):e22–38.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Beller EM, Glasziou PP, Altman DG, et al. PRISMA for abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10(4): e1001419.
Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res. 2017;61:1600324.
Viswanathan, M., M. Ansari, N. Berkman, et al. Assessing the risk of bias of individual studies when comparing medical interventions. Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Publication No. 12-EHC047-EF. Available: http://www.effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports.2012.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Grgic J, Grgic I, Pickering C, Schoenfeld BJ, Bishop DJ, Pedisic Z. Wake up and smell the coffee: caffeine supplementation and exercise performance—an umbrella review of 21 published meta-analyses. Br J Sports Med. 2020;54(11):681–8.
Pearce N. Effect measures in prevalence studies. Environ Health Perspect. 2004;112:1047–50.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):1–10.
Weir CJ, Butcher I, Assi V, et al. Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol. 2018;18(1):25.
Walter S, Yao X. Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007;60(8):849–52.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342: d549.
Pedersen, J., M.G. Rasmussen, M. Neland, A. Grøntved. Screen-based media use and blood pressure in preschool-aged children: A prospective study in the Odense Child Cohort. Scandinavian journal of public health. 2020: 1403494820914823.
Carson V, Janssen I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: a cross-sectional study. BMC Public Health. 2011;11:274.
Solomon-Moore E, Salway R, Emm-Collison L, et al. Associations of body mass index, physical activity and sedentary time with blood pressure in primary school children from south-west England: a prospective study. PLoS ONE. 2020;15(4): e0232333.
Wyszyńska, J., J. Podgórska-Bednarz, K. Dereń, A. Mazur. The relationship between physical activity and screen time with the risk of hypertension in children and adolescents with intellectual disability. BioMed Res Int. 2017. 2017.
Gui ZH, Zhu YN, Cai L, et al. Sugar-sweetened beverage consumption and risks of obesity and hypertension in Chinese children and adolescents: a national cross-sectional analysis. Nutrients. 2017;9(12):1302.
Cureau FV, Ekelund U, Bloch KV, Schaan BD. Does body mass index modify the association between physical activity and screen time with cardiometabolic risk factors in adolescents? Findings from a country-wide survey. Int J Obes (Lond). 2017;41(4):551–9.
Safiri S, Kelishadi R, Qorbani M, et al. Screen time and its relation to cardiometabolic risk among children and adolescents: the CASPIAN-III study. Iran J Public Health. 2015;44(1):35–44.
Stamatakis E, Coombs N, Jago R, et al. Type-specific screen time associations with cardiovascular risk markers in children. Am J Prev Med. 2013;44(5):481–8.
Byun W, Dowda M, Pate RR. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27(4):388–94.
Ullrich-French SC, Power TG, Daratha KB, Bindler RC, Steele MM. Examination of adolescents’ screen time and physical fitness as independent correlates of weight status and blood pressure. J Sports Sci. 2010;28(11):1189–96.
Hardy LL, Denney-Wilson E, Thrift AP, Okely AD, Baur LA. Screen time and metabolic risk factors among adolescents. Arch Pediatr Adolesc Med. 2010;164(7):643–9.
Lazarou C, Panagiotakos DB, Matalas AL. Lifestyle factors are determinants of children’s blood pressure levels: the CYKIDS study. J Hum Hypertens. 2009;23(7):456–63.
Fujiwara H, Nakajima H, Inoue F, Kosaka K, Asano H, Yoshii K. Arterial stiffness in junior high school students: longitudinal observations. Pediatr Int. 2018;60(2):127–35.
Leman MA, Claramita M, Rahayu GR. Predicting factors on modeling health behavior: a systematic review. Am J Health Behav. 2021;45(2):268–78.
Gopinath B, Baur LA, Garnett S, Pfund N, Burlutsky G, Mitchell P. Body mass index and waist circumference are associated with blood pressure in preschool-aged children. Ann Epidemiol. 2011;21(5):351–7.
Garoufi A, Grammatikos EE, Kollias A, Grammatikos E, Stergiou GS, Soldatou A. Associations between obesity, adverse behavioral patterns and cardiovascular risk factors among adolescent inhabitants of a Greek island. J Pediatr Endocrinol Metab. 2017;30(4):445–54.
Tebar WR, Ritti Dias RM, Scarabottolo CC, et al. Sedentary behavior is more related with cardiovascular parameters in normal weight than overweight adolescents. J Public Health. 2020;42(3):215–22.
Wennberg P, Gustafsson PE, Dunstan DW, Wennberg M, Hammarström A. Television viewing and low leisure-time physical activity in adolescence independently predict the metabolic syndrome in mid-adulthood. Diabetes Care. 2013;36(7):2090–7.
Christofaro DGD, Ritti-Dias RM, Chiolero A, Fernandes RA, Casonatto J, de Oliveira AR. Physical activity is inversely associated with high blood pressure independently of overweight in Brazilian adolescents. Scand J Med Sci Sports. 2013;23(3):317–22.
de Moraes ACF, Carvalho HB, Rey-López JP, et al. Independent and combined effects of physical activity and sedentary behavior on blood pressure in adolescents: gender differences in two cross-sectional studies. PLoS ONE. 2013;8(5):e62006.
Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico city. Int J Obes Relat Metab Disord. 1999;23(8):845–54.
Dowda M, Ainsworth BE, Addy CL, Saunders R, Riner W. Environmental influences, physical activity, and weight status in 8- to 16-year-olds. Arch Pediatr Adolesc Med. 2001;155(6):711–7.
Wang Y, Liang H, Tussing L, Braunschweig C, Caballero B, Flay B. Obesity and related risk factors among low socio-economic status minority students in Chicago. Public Health Nutr. 2007;10(9):927–38.
Anderson SE, Economos CD, Must A. Active play and screen time in US children aged 4 to 11 years in relation to sociodemographic and weight status characteristics: a nationally representative cross-sectional analysis. BMC Public Health. 2008;8:1–13.
Lagiou A, Parava M. Correlates of childhood obesity in Athens, Greece. Public Health Nutr. 2008;11(9):940–5.
Syme C, Abrahamowicz M, Leonard GT, et al. Sex differences in blood pressure and its relationship to body composition and metabolism in adolescence. Arch Pediatr Adolesc Med. 2009;163(9):818–25.
Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemogr Soc Biol. 2015;61:1–17.
Álvarez C, Lucia A, Ramírez-Campillo R, et al. Low sleep time is associated with higher levels of blood pressure and fat mass in Amerindian school children. Am J Hum Biol. 2019;31(6):e23303.
Zhou M, Lalani C, Banda JA, Robinson TN. Sleep duration, timing, variability and measures of adiposity among 8- to 12-year-old children with obesity. Obes Sci Pract. 2018;4(6):535–44.
Guerrero MD, Barnes JD, Chaput J-P, Tremblay MS. Screen time and problem behaviors in children: exploring the mediating role of sleep duration. Int J Behav Nutr Phys Act. 2019;16(1):105.
DelRosso LM, Mogavero MP, Ferri R. Effect of sleep disorders on blood pressure and hypertension in children. Curr Hypertens Rep. 2020;22(11):88.
Tavasoli A, Saeidi M, Hooman N. Correlation between sleep quality and blood pressure changes in Iranian children. J Compr Ped. 2015;6:ee24805.
Azemati B, Kelishadi R, Ahadi Z, et al. Association between junk food consumption and cardiometabolic risk factors in a national sample of Iranian children and adolescents population: the CASPIAN-V study. Eat Weight Disord. 2020;25(2):329–35.
Chaput JP, Visby T, Nyby S, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93(6):1196–203.
Delgado-Floody P, Caamaño-Navarrete F, Guzmán-Guzmán IP, Jerez-Mayorga D, Martínez-Salazar C, Álvarez C. Food habits and screen time play a major role in the low health related to quality of life of ethnic ascendant schoolchildren. Nutrients. 2020;12(11):1–14.
Schroeder K, Kubik MY, Sirard JR, Lee J, Fulkerson JA. Sleep is inversely associated with sedentary time among youth with obesity. Am J Health Behav. 2020;44(6):756–64.
Lutz M, Vargas C, Stojanova J, Arancibia M. Diet and depressive disorders. Arch Clin Psychiatry (São Paulo). 2021;48:117–22.
Mariona P, Roy A. Survey on lifestyle and food habits of patients with PCOS and obesity. J Complement Med Res. 2021;11(5):93–93.
Acknowledgements
This work was supported by Tabriz University of Medical Sciences (Grant No. 68713). The study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1401.024).
Funding
The Vice Chancellor for Research and Technology at Tabriz University of Medical Sciences provided funding for this study (identifier: IR.TBZMED.REC.1401.024).
Author information
Authors and Affiliations
Contributions
MAF contributed to hypothesis generation and data analysis; MAF and EFA contributed to manuscript writing and quality assessment. AM was involved in statistical analysis. FR and ASH were involved in hypothesis generation, quality assessment and extraction. All of the authors were involved in quality assessment and manuscript writing. Also, all of them read and approved the final manuscript to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of the study was registered in the PROSPERO system (Registration number: CRD42021243523). Also, the research was approved by the ethics committee of Tabriz University of Medical Sciences (Identifier: 68713).
Consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Tables and Figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farhangi, M.A., Fathi Azar, E., Manzouri, A. et al. Prolonged screen watching behavior is associated with high blood pressure among children and adolescents: a systematic review and dose–response meta-analysis. J Health Popul Nutr 42, 89 (2023). https://doi.org/10.1186/s41043-023-00437-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00437-8