Abstract
Background
The role of screen time in promoting obesity among children has been reported in previous studies. However, the effects of different screen types and the dose–response association between screen time and obesity among children is not summarized yet. In the current meta-analysis we systematically summarized the association between obesity and screen time of different screen types in a dose–response analysis.
Methods
A systematic search from Scopus, PubMed and Embase electronic databases was performed. Studies that evaluated the association between screen time and obesity up to September 2021 were retrieved. We included 45 individual studies that were drawn from nine qualified studies into meta-analysis.
Results
The results of the two-class meta-analysis showed that those at the highest category of screen time were 1.2 times more likely to develop obesity [odds ratio (OR) = 1.21; confidence interval (CI) = 1.113, 1.317; I2 = 60.4%; P < 0.001). The results of subgrouping identified that setting, obesity status and age group were possible heterogeneity sources. No evidence of non-linear association between increased screen time and obesity risk among children was observed (P-nonlinearity = 0.310).
Conclusion
In the current systematic review and meta-analysis we revealed a positive association between screen time and obesity among children without any evidence of non-linear association. Due to the cross-sectional design of included studies, we suggest further studies with longitudinal or interventional design to better elucidate the observed associations.
Similar content being viewed by others
Background
Obesity is a major health problem among children and adolescents; overweight and obesity in children and adolescents increases the odds of adulthood obesity [1, 2]. Numerous factors are associated with childhood obesity including increased dietary intake of high-fat snacks and fast foods, large portion sizes, increased consumption of sugar sweetened beverages and other environmental and genetic factors [3,4,5]; however, lack of regular physical activity and sedentary lifestyle is one of the most important determinant of childhood obesity [6, 7]. Physical inactivity is prevalent among children; on average, children spent 41% and 51% of the after-school period in sedentary time when at after-school care and other locations (e.g. participation in afterschool programs, screen-based behaviors, homework/academics or social activities and motorized transport) respectively [8,9,10].
It is suggested that physical activity is one of the powerful treatments to help obesity prevention and to improve obesity-related risk factors among children; every one hour of moderate-to-vigorous physical activity is accompanied with 10% reduced risk of obesity development [11]. Although childhood obesity is a result of complex interaction between physical activity, dietary factors and metabolic and genetic factors [12, 13], the role of physical activity along with some other lifestyle modifications in reducing childhood obesity risk is further highlighted in numerous interventional studies [14,15,16]. Sedentary behaviors (SB) are defined as any activities that are less than or equal to 1.5 metabolic equivalents (MET); these kind of behaviors closely resemble energy expenditure of body while it is “at rest.” [17]. Several studies have targeted reducing SB as a therapeutic way to decrease childhood obesity [18,19,20,21].SBs are associated with increased risk of cardiovascular diseases (CVDs), diabetes and metabolic syndrome [22, 23]. Also, SBs increase the risk of obesity among children and most of the children nowadays, engage in sedentary behaviors like television (TV) viewing [24,25,26,27,28]. In a population-based cross-sectional study among four thousand one hundred and ninety-seven children aged 6 to 12 years, 62% of children watched TV 1 to 3 h per day. Children who spent more than 3 h per day watching TV were 1.8 times more likely to be obese [odds ratio (OR) = 1.8 (95% confidence interval (CI) = 1.2–2.8)] [29]. Screen time (ST), as a subgroup of SBs, is a term used for activities done in front of a screen, such as watching TV, working on a computer, or playing video games. Screen time is sedentary behavior, meaning you are being physically inactive while sitting down [30]. Screen time is dramatically increased as a results of development in technology, like increased electronic media use, TV watching and computer using by children [31, 32]. American Academy of Pediatrics recommends limiting screen-time among children and adolescents to less than 2 h per day with no screens for kids under 2, and less than an hour per day for kids 2 to 5 [33].
Numerous studies have been performed that evaluated the relationship between screen time and adiposity; but the obtained results are inconsistent. While several studies reported increased obesity risk among high-screen users [34,35,36], some others reported increased weight only among overweight youth [1], some others reported the obesity-promoting effects of TV and failed to report this effect for personal computer (PC) or other screens [36, 37]. Several studies reported no significant association between screen use and obesity [38, 39]; while several studies reported significant increase in weight only among PC-users [40, 41]. More surprisingly, some of the studies reported lower screen time among obese youth; in the study by Christofaro et al. [42], lower obesity risk was reported among boys with the highest ST versus those with the lowest ST. According to the review of literature, it is obviously clear that numerous factors determine the effects of screen on obesity among youth; these factors are duration of screen use, screen device type, the obesity status (e.g. overweight or obesity) and geographical distribution. Moreover, numerous studies have revealed the particular importance of childhood obesity in increased likelihood of later adulthood obesity, promotion of CVD risk factors and atherosclerosis progress throughout life [43,44,45].
Therefore, in the current systematic review and meta-analysis, we aimed to (a) evaluate the association between screen time and obesity among children and (b) to explore the role of different factors including geographical distribution, screen type, age grouping, obesity status (e.g. overweight, obesity), setting (school, community) and sample size of different studies in the screen time-obesity associations.
Materials and methods
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) was used for results’ presentation (Additional file 1: Table S1) [46].
Search strategy and selection of studies
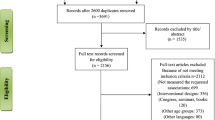
The search results from the Embase, Scopus and PubMed electronic databases through September 2021 provided a total of 6291 articles (Fig. 1). Search strategy was created as a result of combination of the MeSH (Medical Subject Headings) terms from the PubMed database and free text words and was adopted for each electronic database (Additional file 1: Table S2). Duplicate removal and exclusion of articles according to title/abstarct, retrieved a total of 2156 articles. Two independent investigators cheked all of the articles. Then, 2101 manuscripts were removed because of their irrelevant subject, design, involving other age gropus, other languages, being reviews conferences and seminars, and not evaluating the association of studied parameters. Any discrepancies between reviewers were resolved by discussion. As a consequent, 45 individual studies from nine articles were included in the meta-synthesis.
Inclusion and exclusion criteria
Inclusion criteria for studies were as follows (1) studies with observational designs (case control, cross-sectional or cohort studies with the baseline measurement of study parameters); (2) studies that evaluated the relationship (OR, RR or HR) between screen time and risk of obesity (3) the studies that were conducted only among children (≤ 9 years). Clinical trials, systematic reviews, meta-analysis, case-reports and case-series, experimental studies, short communication, letter to editors, and studies that examined the relations other than the relationship between screen time and obesity were excluded from the analysis.
Data extraction and quality assessment
A standard Excel extraction datasheet (Excel 2010, Microsoft Office; Redmond, Washington, USA) was used for data extraction and data extraction was performed independently by two authors. The information that was included into data sheet were the name of first author and journal, year of publication, country, setting, age range and number of participants, study design, adjusted covariate, gender, obesity and screen time definition, weight, height and screen time measurement tools, and main results of the studies. Any disagreements between reviewers were resolved by discussion. The methodological quality of studies were assessed using the Agency for Healthcare Research and Quality (AHRQ) checklist [47] (Table 1).
Statistical analysis
The studies that reported the odds ratio of obesity (OR) in those with highest screen time versus lowest screen time were included in the two-class meta-analysis. When the OR was not provided, we calculated prevalence odds ratios (PORs) as suggested by Pearce et al. as the best approach for measuring effect size in prevalence studies [48]: \(POR=\left[\frac{P1}{1-P1}\right]/\left[\frac{P0}{1-P0}\right]\). While P0 and P1 are the prevalence in exposed and non-exposed groups. Cochran's Q and I-squared tests were used to identify between-study heterogeneity. The possible sources of heterogeneity were identified using subgrouping and meta-regression analysis. STATA version 13 (STATA Corp LLC, College Station, TX, USA), was used for data analysis and P-values less than 0.05 were considered as statistically significant.
Only the studies that reported at least three categories for screen time and the odds or prevalence of obesity were included in the dose–response meta-analysis. Accordingly, thirteen individual studies in five articles were included [49,50,51,52,53,54,55,56,57,58,59,60,61]. The median point in each screen time category was identified and when medians were not reported, then approximate medians using the midpoint of the lower and upper limits were estimated. When the lowest or highest screen time categories were open-ended, the screen time was calculated by assuming the similar interval for those categories and estimating the mid-point. The reference category was the lowest one assuming OR and CIs of 1 for it. The potential non- linear associations were assessed using random‐effects dose‐response meta‐analysis by defining the restricted cubic splines with three knots at fixed percentiles (10%, 50% and 90%) of distribution and were used to calculate study‐specific odds ratios. Cochran's Q and I-squared tests were used to identify between-study heterogeneity. The possible sources of heterogeneity were identified using subgrouping approach. Begg’s funnel plot was used to evaluate the publication bias followed by the Egger's regression asymmetry test and Begg's adjusted rank correlation.
Definitions
Screen time is defined according to the world health organization (WHO) definition of the time that is spent passively watching screen-based entertainment (TV, computer, mobile devices). This definition does not include some of the active games which involves physical activity or movement [62]. Thus, TV watching, usinig smart phone, internet and computer and some of the video games that are played in sedentary position are included as screen time. Child is defined as age under 10 years of as previously described by WHO [62]. In the studies that were included in the current meta-analysis, overweight and obesity were defined as folows: (1) Overweight was defined as having a Z score of BMI for age with the cut-off points of > 1 to ≤ 2 standard deviations while obesity was defined as Z score values > 2 standard deviations [63]; (2) according to the international age and sex specific cut- offs of BMI [≥ 85th percentile and less than 95th percentile for overweight and ≥ 95th for obesity and [64] (3) as BMI cut-off of overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 [65]. Two-class meta-analysis in the current study is a meta-analysis approach of the comparison of an outcome variable between two study groups.
Results
Study characteristics
The general characteristics of included studies are presented in Table 2. In the two-class meta-analysis, totally, 45 individual studies obtained from nine articles were included; the details of 45 individual studies are reported here: the study by Zulfiqar et al. [66], provided results for three age groups of 4–5, 6–7, 8–9 and for TV use in weekdays, electronic game playing in weekdays, TV use in weekends and electronic game playing in weekends among boys and girls separately; therefore, the results were included as 24 studies in the analysis. According to their results, electronic game playing more than one hour among 4–5 years old immigrant boys from high income countries (HICs) was associated with reduced risk of obesity (OR = 0.61; CI = 0.49–0.89), while TV watching more than 3 h per day of weekdays was associated with increased risk of obesity (OR = 1.4; CI = 1.0–1.9). Among immigrant girls from HICs in ages of 4–5 and 6–7 years old, electronic game playing of more than 1 h per day in weekdays was associated with reduced risk of obesity (OR = 0.39; CI = 0.17, 0.92), while TV watching in weekends of more than 3 h per day among age groups of 6–7, 7–8 and 9–10 years old was associated with increased risk of obesity OR = 1.6; CI = 1.2,2.1, OR = 1.4; CI = 1.1,1.8 and OR = 1.5; CI = 1.1,1.9 respectively. In the study by Hu et al. [67], was sub grouped for both 1–3 years old and 4–5 years old and higher TV watching hours was positively associated with obesity among those with 4–5 years old (OR = 1.72, 95% CI: 1.16–2.54). The results of the study by Armoon et al. [68] was reported as separate results for TV and PC users. Therefore, it was included as two separate studies and there was a positive association between odds of obesity and TV or PC use of more than 2 h per day (for TV users: OR = 3.51; CI = 1.20–8.66; P = 0.01 and PC users OR = 3.40; CI = 1.24–7.32; P = 0.01). The study by Tester et al. [69] reported the results for TV, PC, and VG among overweight, obese and severe obese children separately and therefore, the results were included as six separate studies in the analysis. According to their results, children with total screen time of more than 4 h were more likely to be overweight [OR = 1.5; CI = 1.2 to 1.9)] or obese [OR = 2.0; CI = 1.2 to 3.3]. The study by Irish-Hauser et al. [70], reported the association between overweight and TV watching during dinner with rarely/ sometimes or much users so the results were reported as three independent studies. The study by De Jong et al. [71] was reported as four studies of TV watchers of 1–1.5 and more than 1.5 h and PC users of less than 30 min/day and more than 30 min per day. In the study by Stettler [60], obesity was increased by higher TV watching hours and electronic game playing [OR = 1.92; CI = 1.27 to 2.90; P = 0.002 and OR = 2.56; CI = 1.55 to 4.23; P < 0.001 respectively]. The age range of participants was 4–11 years old. 4 studies out of 45 were school based and all of the studies were performed in combination of girls and boys.
Results of meta-analysis
The results of the two-class meta-analysis (Fig. 2) showed that being at the highest category of screen time was associated with 20% increase in obesity risk (OR = 1.21; CI = 1.113, 1.317; P < 0.001). The heterogeneity was identified as I-squared (variation in ES attributable to heterogeneity) of 60.4%. For finding the source of heterogeneity, we performed subgrouping and the results are shown in Table 3. As presented, a minimal reduction in heterogeneity was observed after subgrouping according to setting, obesity status and age group; so, these parameters might be considered as possible heterogeneity sources. The results of dose–response relationship between screen time and obesity among children is presented in Fig. 3. There was no evidence of non-linear association between increased screen time and obesity risk among children (P-nonlinearity = 0.310). The details of dose–response association is also presented in Table 4. It can be inferred from the Table that by 50, 100 and 150 min increments in screen time, there is 7%, 16% and 35% increase in the odds of obesity among children; although these values were not statistically significant (Table 4).
The results of quality assessment and publication bias
The results of the quality assessment according to AHRQ checklist (Table 1) revealed that all of the included studies had moderate quality scores. Publication bias was assessed with the funnel plot (Fig. 4). Moreover, the Begg’s and the Egger’s regression tests were further used to better clarify the publication bias. Accordingly, an evidence of publication bias was achieved for study parameters [OR of obesity and screen time: Egger’s test (P = 0.001) and Begg’s test (P = 0.001). Therefore, trim and fill analysis was performed (Fig. 5); accordingly, the obtained results were as follows: OR = 1.187; CI = 0.883, 1.491; P < 0.001).
Discussion
In the current work, we identified that children at the highest category of screen time were 1.2 times more likely to develop obesity. Most of the included studies (e.g. 26 studies) used TV as the most commonly used screen and were community-based studies. The results of previous studies evaluating the association between TV viewing and childhood obesity are inconsistent; several studies reported positive association between TV viewing and obesity risk among children [67, 68, 71]; while several others reported a dose–response association between TV viewing and childhood obesity [72, 73] and several others reported no associations between them [41, 74]. In the current meta- analysis, we summarized the results obtained from 28,675 individuals and the final result was a positive association between screen time and childhood obesity. This positive association was not observed for VG alone with a reasonably acceptable number of included studies e.g. [13]. Surprisingly, several studies have reported the negative effect of active video games on obesity. In the study by Zulfiqar et al. [66], electronic games more than 1 h in weekend was associated with reduced risk of obesity among children 4–5 years old [OR = 0.61; CI = 0.41,0.89; P < 0.001]. In the other study by Hernandez et al. [75] only TV viewing was associated increased obesity risk and no association was found between video games or any other types of video time with obesity risk. Several other studies also revealed the positive effects of some active video games in increasing physical activity and reducing obesity risk [76,77,78]. In other study by Strahan et al. [79], active video games reduced the chance of obesity among youth. The reason is that some of the video games possibly increase physical activity and physical health; in a meta-analysis by Primack et al. [80], video games were associated with 69% improve in psychological therapy outcomes and 50% improve in physical activity outcomes. In another study by Williams et al. [81], active video games were suggested as effective therapeutic tools to improve physical activity among adolescents and were considered as a more acceptable and sustainable approach than many other conventional methods.
The obesity-promoting effects of increased screen-time can be explained by this fact that increased screen activities are associated with increased food intake; numerous studies have revealed that television watching increases motivated response to food intake and snacking behavior among children and adolescents [82,83,84,85,86]; this is also true for video games [87,88,89,90] and personal computer use [91, 92]. More important, several food-related advertisement in television can potentially affects children’s food behaviors by promoting junk food and fast food consumption and increasing obesity [93,94,95,96,97,98,99]. Therefore, the association between obesity and screen use is a multi-dimensional factor that all of its aspects needs to clearly studied. Several limitations of the current meta-analysis should also be addressed; first of all, the results of included studies were reported in a combination of males and females therefore, it was not possible to give gender-specific results; moreover, there are relatively low number of studies in several subgroups and their results could not be generalized. The screen time was subjectively assessed by questionnaire that stems for recall bias; finally, the cross-sectional design of the included studies, make it impossible to infer the causality.
Conclusion
In the current systematic review and meta-analysis we observed increased obesity risk in those with the highest screen time versus those with the lowest screen time. This association was not non-linear and TV was the most common obesity-promoting screen in the included studies. Moreover, community based studies with greater sample size showed the strongest associations. Since the results were not separable for boys and girls, and also due to the observational design of the included studies, further studies with separate results for males and females and different screen devices with longitudinal or interventional designs are needed to better explore the obtained results.
Implications for practice section
In an updated systematic review and meta-analysis, we found a positive association between screen time and obesity risk among children. Therefore, this is a health alarm for families to manage their children’s screen time, for policy makers to develop policies for management of media use and screen related behaviors among children [100].
Availability of data and materials
All of the data are available with reasonable request from the corresponding author.
Change history
22 August 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1186/s41043-023-00432-z
References
Vrijkotte TGM, Oostvogels AJJM, Stronks K, Roseboom TJ, Hof MHP. Growth patterns from birth to overweight at age 5–6 years of children with various backgrounds in socioeconomic status and country of origin: the ABCD study. Pediatr Obes. 2020;15(8):58.
Tang D, Bu T, Feng Q, Liu Y, Dong X. Differences in overweight and obesity between the North and South of China. Am J Health Behav. 2020;44(6):780–93.
Taghizadeh S, Farhangi MA. The effectiveness of pediatric obesity prevention policies: a comprehensive systematic review and dose–response meta-analysis of controlled clinical trials. J Transl Med. 2020;18(1):1–21.
Abbasalizad FM, Mohammadi TA, Jahangiri L, Nikniaz Z, Nikniaz L. Sugar-sweetened beverages intake and the risk of obesity in children: an updated systematic review and dose–response meta-analysis. Pediatr Obes. 2022;5:e12914.
Nikniaz L, Abbasalizad-Farhangi M, Vajdi M, Nikniaz Z. The association between Sugars Sweetened Beverages (SSBs) and lipid profile among children and youth: a systematic review and dose-response meta-analysis of cross-sectional studies. Pediatr Obes. 2021;16(7):e12782.
Taghizadeh S, Khodayari-Zarnaq R, Farhangi MA. Childhood obesity prevention policies in Iran: a policy analysis of agenda-setting using Kingdon’s multiple streams. BMC Pediatr. 2021;21(1):1–11.
Haghjoo P, Siri G, Soleimani E, Farhangi MA, Alesaeidi S. Screen time increases overweight and obesity risk among adolescents: a systematic review and dose-response meta-analysis. BMC Primary Care. 2022;23(1):1–24.
Lutz M, Vargas C, Stojanova J, Arancibia M. Diet and depressive disorders. Arch Clin Psychiatry (São Paulo). 2021;48:117–22.
Ji M, An R, Qiu Y, Guan C. The impact of natural disasters on dietary intake. Am J Health Behav. 2020;44(1):26–39.
Arundell L, Fletcher E, Salmon J, Veitch J, Hinkley T. A systematic review of the prevalence of sedentary behavior during the after-school period among children aged 5–18 years. Int J Behav Nutr Phys Act. 2016;13(1):1–9.
Headid RJ III, Park S-Y. The impacts of exercise on pediatric obesity. Clin Exp Pediatr. 2021;64(5):196.
Pietrobelli A, Malavolti M, Battistini NC, Fuiano N. Metabolic syndrome: a child is not a small adult. Int J Pediatr Obes. 2008;3(sup1):67–71.
Abbasalizad Farhangi M, Dehghan P, Jahangiry L. Mental health problems in relation to eating behavior patterns, nutrient intakes and health related quality of life among Iranian female adolescents. PLoS ONE. 2018;13(4):e0195669.
Sola K, Brekke N, Brekke M. An activity-based intervention for obese and physically inactive children organized in primary care: feasibility and impact on fitness and BMI: a one-year follow-up study. Scand J Prim Health Care. 2010;28(4):199–204.
Lisón JF, Real-Montes JM, Torró I, Arguisuelas MD, Álvarez-Pitti J, Martínez-Gramage J, et al. Exercise intervention in childhood obesity: a randomized controlled trial comparing hospital-versus home-based groups. Acad Pediatr. 2012;12(4):319–25.
Berleze A, Valentini NC. Intervention for children with obesity and overweight and motor delays from low-income families: fostering engagement, motor development, self-perceptions, and playtime. Int J Environ Res Public Health. 2022;19(5):2545.
Saelens BE. Helping individuals reduce sedentary behavior. Obes Etiol Assess Treat Prev. 2003;2:217–38.
Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–7.
Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154(3):220–6.
Faith MS, Berman N, Heo M, Pietrobelli A, Gallagher D, Epstein LH, et al. Effects of contingent television on physical activity and television viewing in obese children. Pediatrics. 2001;107(5):1043–8.
Farhangi MA, Emam-Alizadeh M, Hamedi F, Jahangiry L. Weight self-stigma and its association with quality of life and psychological distress among overweight and obese women. Eat Weight Disord-Stud Anorexia Bulimia Obes. 2017;22(3):451–6.
Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41(5):1338–53.
Dempsey PC, Owen N, Biddle SJ, Dunstan DW. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr DiabRep. 2014;14(9):1–11.
Robinson TN. Television viewing and childhood obesity. Pediatr Clin N Am. 2001;48:1017–25.
Rossi CE, Albernaz DO, De Vasconcelos FDAG, De Assis MAA, Di Pietro PF. Television influence on food intake and obesity in children and adolescents: a systematic review. Revista de Nutricao. 2010;23(4):607–20.
Leman MA, Claramita M, Rahayu GR. Predicting factors on modeling health behavior: a systematic review. Am J Health Behav. 2021;45(2):268–78.
Ulaganathan V, Kandiah M, Shariff ZM. A case–control study on the association of abdominal obesity and hypercholesterolemia with the risk of colorectal cancer. J Carcinog. 2018;2:17.
Kamolthip R, Fung XC, Lin C-Y, Latner JD, O’Brien KS. Relationships among physical activity, health-related quality of life, and weight stigma in children in Hong Kong. Am J Health Behav. 2021;45(5):828–42.
Ruangdaraganon N, Kotchabhakdi N, Udomsubpayakul U, Kunanusont C, Suriyawongpaisal P. The association between television viewing and childhood obesity: a national survey in Thailand. J Med Assoc Thailand. 2002;85(Suppl 4):S1075-80.
Wachira LJM, Muthuri SK, Ochola SA, Onywera VO, Tremblay MS. Screen-based sedentary behaviour and adiposity among school children: Results from international study of childhood obesity, lifestyle and the environment (iscole)-Kenya. PloS One. 2018;13(6):51.
Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Int J Obes. 2005;2005(2):29–39.
Schroeder K, Kubik MY, Sirard JR, Lee J, Fulkerson JA. Sleep is inversely associated with sedentary time among youth with obesity. Am J Health Behav. 2020;44(6):756–64.
Pappas S. What do we really know about kids and screens? Am Phsychol Assoc. 2020;5:874.
Tsuchiya M, Momma H, Sekiguchi T, Kuroki K, Kanazawa K, Watanabe M, et al. Excessive game playing is associated with poor toothbrushing behavior among athletic children: a cross-sectional study in Miyagi, Japan. Tohoku J Exp Med. 2017;241(2):131–8.
Kelishadi R, Mozafarian N, Qorbani M, Maracy MR, Motlagh ME, Safiri S, et al. Association between screen time and snack consumption in children and adolescents: the CASPIAN-IV study. J Pediatr Endocrinol Metab. 2017;30(2):211–9.
Börnhorst C, Wijnhoven TMA, Kunešová M, Yngve A, Rito AI, Lissner L, et al. WHO European Childhood Obesity Surveillance Initiative: associations between sleep duration, screen time and food consumption frequencies. BMC Public Health. 2015;15(1):71.
Alghadir AH, Gabr SA, Iqbal ZA. Television watching, diet and body mass index of school children in Saudi Arabia. Pediatr Int. 2016;58(4):290–4.
Hoffmann B, Kobel S, Wartha O, Kettner S, Dreyhaupt J, Steinacker JM. High sedentary time in children is not only due to screen media use: a cross-sectional study. BMC Pediatr. 2019;19(1):154.
Werneck AO, Silva DR, Agostinete RR, Fernandes RA, Ronque ERV, Cyrino ES. Social, behavioral and biological correlates of cardiorespiratory fitness according to sex, nutritional status and maturity status among adolescents. A cross-sectional study. Sao Paulo Med J. 2018;136(3):237–44.
Safiri S, Kelishadi R, Qorbani M, Abbasi-Ghah-Ramanloo A, Motlagh ME, Ardalan G, et al. Screen time and its relation to cardiometabolic risk among children and adolescents: The CASPIAN-III study. Iran J Public Health. 2015;44(1):35–44.
Appelhans BM, Fitzpatrick SL, Li H, Cail V, Waring ME, Schneider KL, et al. The home environment and childhood obesity in low-income households: Indirect effects via sleep duration and screen time. BMC Public Health. 2014;14(1):58.
Christofaro DGD, De Andrade SM, Mesas AE, Fernandes RA, Farias Júnior JC. Higher screen time is associated with overweight, poor dietary habits and physical inactivity in Brazilian adolescents, mainly among girls. Eur J Sport Sci. 2016;16(4):498–506.
Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med. 2011;45(11):866–70.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73.
Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17(1):1–24.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res. 2017;61:1600324.
Par N. Effect measures in prevalence studies. Environ Health Perspect. 2004;112:1047–50.
Li L, Shen T, Wen LM, Wu M, He P, Wang Y, et al. Lifestyle factors associated with childhood obesity: a cross-sectional study in Shanghai China. BMC Res Notes. 2015;8(1):89.
Bhadoria AS, Kapil U, Kaur S. Association of duration of time spent on television, computer and video games with obesity amongst children in national capital territory of Delhi. Int J Prev Med. 2015;3:748.
Bingham DD, Varela-Silva MI, Ferrão MM, Augusta G, Mourão MI, Nogueira H, et al. Socio-demographic and behavioral risk factors associated with the high prevalence of overweight and obesity in portuguese children. Am J Hum Biol. 2013;25(6):733–42.
Koleilat M, Harrison GG, Whaley S, McGregor S, Jenks E, Afifi A. Preschool enrollment is associated with lower odds of childhood obesity among WIC participants in LA County. Matern Child Health J. 2012;16(3):706–12.
Taylor AW, Winefield H, Kettler L, Roberts R, Gill TK. A population study of 5 to 15 year olds: full time maternal employment not associated with high BMI. The importance of screen-based activity, reading for pleasure and sleep duration in children’s BMI. Matern Child Health J. 2012;16(3):587–99.
Balaban G, Motta ME, Silva GA. Early weaning and other potential risk factors for overweight among preschool children. Clinics (Sao Paulo, Brazil). 2010;65(2):181–7.
Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ. Television viewing, computer use, and BMI among U.S. children and adolescents. J Phys Act Health. 2009;6(51):528–35.
Khader Y, Irshaidat O, Khasawneh M, Amarin Z, Alomari M, Batieha A. Overweight and obesity among school children in Jordan: prevalence and associated factors. Matern Child Health J. 2009;13(3):424–31.
Steele RM, Van Sluijs EMF, Cassidy A, Griffin SJ, Ekelund U. Targeting sedentary time or moderate- and vigorous-intensity activity: Independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr. 2009;90(5):1185–92.
Da Costa RI, Taddei JAAC, Colugnatti F. Obesity among children attending elementary public schools in Sao Paulo, Brazil: a case-control study. Public Health Nutr. 2003;6(7):659–63.
Lagiou A, Parava M. Correlates of childhood obesity in Athens. Greece Public Health Nutr. 2008;11(9):940–5.
Stettler N, Signer TM, Suter PM. Electronic games and environmental factors associated with childhood obesity in Switzerland. Obes Res. 2004;12(6):896–903.
Utter J, Scragg R, Schaaf D. Associations between television viewing and consumption of commonly advertised foods among New Zealand children and young adolescents. Public Health Nutr. 2006;9(5):606–12.
World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. 2020. Available from: https://apps.who.int/iris/handle/10665/311664.
Do M. The new WHO child growth standards. Paediatr Croat Suppl. 2008;52(Suppl.1):13–7.
Watharkar A, Nigam S, Martolia DS, Varma P, Barman SK, Sharma RP. Assessment of risk factors for overweight and obesity among school going children in Kanpur, Uttar Pradesh. Indian J Commun Health. 2015;27(2):216–22.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ (Clinical Research Ed). 2000;320:1240–3.
Zulfiqar T, Strazdins L, Dinh H, Banwell C, D’Este C. Drivers of overweight/obesity in 4–11 year old children of Australians and immigrants; evidence from growing up in Australia. J Immigr Minor Health. 2019;21(4):737–50.
Hu J, Ding N, Yang L, Ma Y, Gao M, Wen D. Association between television viewing and early childhood overweight and obesity: a pair-matched case-control study in China. BMC Pediatr. 2019;19(1):78.
Armoon B, Karimy M. Epidemiology of childhood overweight, obesity and their related factors in a sample of preschool children from Central Iran. BMC Pediatr. 2019;19(1):159.
Tester JM, Phan TT, Tucker JM, Leung CW, Dreyer Gillette ML, Sweeney BR, et al. Characteristics of children 2 to 5 years of age with severe obesity. Pediatrics. 2018;141(3):74.
Hauser SI, Economos CD, Nelson ME, Goldberg JP, Hyatt RR, Naumova EN, et al. Household and family factors related to weight status in first through third graders: a cross-sectional study in Eastern Massachusetts. BMC Pediatr. 2014;14:167.
De Jong E, Visscher TLS, Hirasing RA, Heymans MW, Seidell JC, Renders CM. Association between TV viewing, computer use and overweight, determinants and competing activities of screen time in 4- to 13-year-old children. Int J Obes. 2013;37(1):47–53.
Braithwaite I, Stewart AW, Hancox RJ, Beasley R, Murphy R, Mitchell EA. The worldwide association between television viewing and obesity in children and adolescents: cross sectional study. PLoS ONE. 2013;8(9):e74263.
Rincón-Pabón D, Urazán-Hernández Y, González-Santamaría J. Association between the time spent watching television and the sociodemographic characteristics with the presence of overweight and obesity in Colombian adolescents (secondary analysis of the ENSIN 2010). PLoS ONE. 2019;14(5):e0216455.
Montoye AH, Pfeiffer KA, Alaimo K, Betz HH, Paek HJ, Carlson JJ, et al. Junk food consumption and screen time: association with childhood adiposity. Am J Health Behav. 2013;37(3):395–403.
Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra-Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico city. Int J Obes Relat Metabol Disord. 1999;23(8):845–54.
Adamo KB, Rutherford JA, Goldfield GS. Effects of interactive video game cycling on overweight and obese adolescent health. Appl Physiol Nutr Metabol. 2010;35(6):805–15.
Alon D, Sousa CV, Baranowski T, Barreira TV, Cabrera-Perez R, Chiu K, et al. The impact of narratives and active video games on long-term moderate-to-vigorous physical activity: a randomized controlled trial protocol. Contemp Clin Trials. 2020;2:96.
Baranowski T, Baranowski J, Thompson D, Buday R, Jago R, Griffith MJ, et al. Video game play, child diet, and physical activity behavior change a randomized clinical trial. Am J Prev Med. 2011;40(1):33–8.
Strahan BE, Elder JH. Video game playing effects on obesity in an adolescent with autism spectrum disorder: a case study. Autism Res Treat. 2015;89:2015.
Primack BA, Carroll MV, McNamara M, Klem ML, King B, Rich M, et al. Role of video games in improving health-related outcomes: a systematic review. Am J Prev Med. 2012;42(6):630–8.
Williams WM, Ayres CG. Can active video games improve physical activity in adolescents? a review of RCT. Int J Environ Res Public Health. 2020;17(2):669.
Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85(2):355–61.
Borghese M, Tremblay M, Leduc G, Boyer C, Belanger P, LeBlanc A, et al. Television viewing and food intake pattern of normal weight, overweight, and obese 9–11 year-old Canadian children. Obes Rev. 2014;15:232.
Taveras EM, Sandora TJ, Shih MC, Ross-Degnan D, Goldmann DA, Gillman MW. The association of television and video viewing with fast food intake by preschool-age children. Obesity (Silver Spring, Md). 2006;14(11):2034–41.
Domoff SE, Sutherland E, Yokum S, Gearhardt AN. The association of adolescents’ television viewing with Body Mass Index percentile, food addiction, and addictive phone use. Appetite. 2021;6:157.
Mariona P, Roy A. Survey on lifestyle and food habits of patients with PCOS and obesity. J Complem Med Res. 2021;11(5):93.
Chaput JP, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93(6):1196–203.
Cessna T, Raudenbush B, Reed A, Hunker R. Effects of video game play on snacking behavior. Appetite. 2007;49(1):282.
Chaput JP, Tremblay A, Pereira B, Boirie Y, Duclos M, Thivel D. Food intake response to exercise and active video gaming in adolescents: effect of weight status. Br J Nutr. 2015;115(3):547–53.
Jontony N, Hill EB, Taylor CA, Boucher LC, O’Brien V, Weiss R, et al. Diet quality, carotenoid status, and body composition in NCAA division I athletes. Am J Health Behav. 2020;44(4):432–43.
Shi L, Mao Y. Excessive recreational computer use and food consumption behaviour among adolescents. Ital J Pediatr. 2010;36(1):1–4.
Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ. Television viewing, computer use, and BMI among US children and adolescents. J Phys Act Health. 2009;6(s1):S28–35.
Gilbert-Diamond D, Emond JA, Lansigan RK, Rapuano KM, Kelley WM, Heatherton TF, et al. Television food advertisement exposure and FTO rs9939609 genotype in relation to excess consumption in children. Int J Obes. 2017;41(1):23–9.
Ustjanauskas AE, Harris JL, Schwartz MB. Food and beverage advertising on children’s web sites. Pediatr Obes. 2014;9(5):362–72.
Lee B, Kim H, Lee SK, Yoon J, Chung SJ. Effects of exposure to television advertising for energy-dense/nutrient-poor food on children’s food intake and obesity in South Korea. Appetite. 2014;81:305–11.
Dibildox J. Analysis of TV, advertising and other behavioral determinants of overweight and obesity in childhood. Salud Publica Mex. 2014;56(Suppl 2):s162–6.
Kar S, Khandelwal B. Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J Nat Sci Biol Med. 2015;6(2):356.
Chen YT, Holahan CK, Castelli DM. Sedentary behaviors, sleep, and health-related quality of life in middle-aged adults. Am J Health Behav. 2021;45(4):785–97.
Tang D, Bu T, Liu Y, Dong X. The impact of mothers’ dietary patterns on children’s nutritional status in China. Am J Health Behav. 2020;44(5):719–31.
Maisano MS, Shonkoff ET, Folta SC. Multiple health behavior change for weight loss: a scoping review. Am J Health Behav. 2020;44(5):559–71.
Veldhuis L, Vogel I, Renders CM, van Rossem L, Oenema A, HiraSing RA, et al. Behavioral risk factors for overweight in early childhood; the “Be active, eat right” study. Int J Behav Nutr Phys Act. 2012;9:74.
Abdelkafi Koubaa A, Younes K, Gabsi Z, Bouslah A, Maalel I, el May WMK, et al. Risk factors of children overweight and obesity. Tunisie Medicale. 2012;90(5):387–93.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript; SHA, supervised the project, performed the search, extraction and wrote the first draft of the manuscript and analyzed the data. AARC and WJA were involved in search, extraction and revision of the paper. MT and ATJ were involved in data analysis. ASA and NS were involved in data extraction and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of the current work has been approved by the ethics committee of Mustaqbal University College (ID: 4565/13).
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1186/s41043-023-00432-z
Supplementary Information
Additional file 1
. Table S1. PRISMA Checklist; Table S2. Search strategies and the number of records according to different electronic database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ramírez-Coronel, A.A., Abdu, W.J., Alshahrani, S.H. et al. RETRACTED ARTICLE: Childhood obesity risk increases with increased screen time: a systematic review and dose–response meta-analysis. J Health Popul Nutr 42, 5 (2023). https://doi.org/10.1186/s41043-022-00344-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-022-00344-4