Abstract
Currently, there is no summative study evaluating the association between central obesity and screen time. This systematic review and meta-analysis aimed to summarize the results of studies evaluating the association between screen time and central obesity among children and adolescents. To this end, we performed a systematic search in three electronic databases, including Scopus, PubMed, and Embase to retrieve the related studies up to March 2021. Nine studies were eligible to be included in the meta-analysis. There was no association between odds of central obesity and screen time [odds ratio (OR) 1.136; 95% CI 0.965–1.337; P = 0.125]; however, waist circumference (WC) was 1.23 cm higher in those with highest screen time versus those in the lowest screen time category [weighted mean difference (WMD) = 1.23; 95% 95% CI 0.342–2.112; P = 0.007; Fig. 3]. Moreover, the possible sources of heterogeneity in the included studies were continent and sample size. No evidence of publication bias was reported. For the first time, the current systematic review and meta-analysis revealed that those with the highest screen time had higher WC compared with those with the lowest screen time. Although, there was no association between odds of central obesity and screen time. Due to the observational design of the included studies, it is impossible to infer the cause-effect relationship. Therefore, further interventional and longitudinal studies are warranted to better elucidate the causality of these associations.
Similar content being viewed by others
Introduction
In recent years, technological developments and socio-demographic progress have been introduced as the inevitable reasons for the growing prevalence of obesity due to a sedentary lifestyle and the so-called “obesogenic environment” [1,2,3]. The World Health Organization (WHO) recommends children and adolescents to have at least one hour of moderate to vigorous physical activity per day and vigorous-intensity physical activity at least three times per week [4]. Nonetheless, nowadays, the time spent actively is increasingly being replaced by screen-based media, and screen time has increased in both children and adolescents with a pronounced role in obesity promotion worldwide [5,6,7,8].
Among obesity measurements, central obesity or abdominal obesity is an important prognostic factor of metabolic disorders, including hypertension, insulin resistance, fatty liver, and diabetes among children and adolescents [9, 10]. Moreover, people with higher body adiposity are more susceptible to cardio-metabolic risk factors. According to the results of the Bogalusa Heart Study, abdominal fat distribution, determined by high waist circumference (WC) among 5–17-year-old children and adolescents, was associated with abnormal levels of serum lipids [11,12,13]. In a systematic review of more than 3966 articles, high WC among children and adolescents was associated with high blood pressure and dyslipidemia [14]. A sedentary life style is associated with central obesity; according to the findings of a community-based study among 124,113 children (9.9 ± 1.1 years old, 51% boys), sedentary activities were associated with increased odds of central obesity [odds ratio (OR) 1.10, 95% CI 1.07–1.14] [15].
Reduced physical activity and increased sedentary behaviors are serious health problems among children and adolescents [16, 17]. Some recent studies reported that 10–12-year-old children had 8 h of sedentary behaviors per day and they spent more than 2 h per day in front of computer or television (TV) screens [18,19,20]. One of the important sedentary behaviors among children is screen time, which collectively refers to the time spent on watching television, playing video games, and working with a computer [21]. Screen time is dramatically increased as a result of increased use of technology, such as electronic media, TV, video, computer, tablet, and internet games, or the use of cell phones full of built-in games [22]. The American Academy of Pediatrics (AAP) recommends limiting screen time among children and adolescents to less than 2 h per day with no screens for kids under two years old, and less than an hour per day for kids aged 2–5 years [23, 24].
Although numerous studies have investigated the relationship between screen time and general obesity, limited studies have evaluated the association between screen time and central obesity and reported inconsistent results. In a cross-sectional study including 930 adolescents, Castro JAC et al. [9] evaluated the association between TV, personal computer (PC), and video games with central obesity (defined as having WC ≥ 85th percentile for age and sex), and reported that TV time more than 2 h per day was associated with increased odds of central obesity (OR 2.11; 95% CI 1.08–4.13; P < 0.01). However, no association was found between using PC and playing video games with central obesity. In another study by Berentzen NE et al. [25], those with the highest WC had significantly higher screen time (P = 0.0001). However, several other studies did not report a positive association between screen time and central obesity, or they reported a non-significant association. For example, Kerkadi A et al. [26, 27] reported a non-significant increase in the odds of central obesity in individuals with screen time higher than 2 h per day compared to those with screen time lower than 2 h per day.
In this study, we assumed that high screen time among children and adolescents might be associated with increased odds of central obesity. Accordingly, this systematic review and meta-analysis and we have two study questions: (1) what is the association between screen time and central obesity among children and adolescents? and (2) how do the different parameters like screen device type, screen time measurement tool, and the demographic characteristics of studies’ participants including participants’ age, geographical distribution, and setting of the studies affect the association between screen time and central obesity among children and adolescents?
Materials and methods
To report the results, we used the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) (Additional file 1: Table S1) [28]. The project’s registration code in PROSPERO was CRD42021233899.
Search strategy and selection of studies
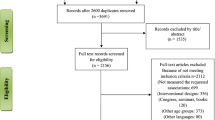
An updated systematic search was performed in three electronic databases, including PubMed, Scopus, and Embase up to March 2021, and a total of 6298 articles were obtained (Fig. 1). The search strategy used a combination of the MeSH (Medical Subject Headings) terms from the PubMed database and free text words (Additional file 1: Table S2). To avoid missing the studies that measured central obesity as a secondary or tertiary measurement variable, we also included some keywords related to general obesity like body mass index (BMI), body fatness, obesity, and overweight. After removing the duplicate studies, we screened the titles and abstracts of the remainig studies. As a result, 2156 articles remained for further analysis. Also, two independent researchers checked the references independently. Then, we removed 2141 manuscripts due to irrelevant subject, irrelevant design, involving other age groups, published in other languages, and not evaluating the association between the study parameters. Meanwhile, we excluded all review, conference, and seminar papers. Any discrepancies between reviewers were resolved by discussion.
Inclusion and exclusion criteria
The following inclusion criteria were applied in our research: (1) studies with an observational design (case–control, cross-sectional, or cohort studies with the baseline measurement of study parameters); (2) studies evaluating the relationship between screen time and central obesity (3); studies including children and adolescents (≤ 18 years); (4) studies providing the mean ± standard deviation (SD) of WC or waist to hip ratio (WHR) among highest versus lowest screen users or those reporting the odds of central obesity in the highest versus lowest screen users.
All clinical trials, systematic reviews, meta-analyses, case reports, case series, experimental studies, short communications, and letters to editors were excluded. Moreover, we excluded the studies published in languages other than English and studies not examining the relationship between screen time and obesity.
Data extraction and quality assessment
We extracted the following data from the included studies: first author’s name, journal name, year of publication, participants’ age range, gender, and health status, study design, sample size, setting, definition of central obesity and screen time, screen time measurement tool, and the main results. The methodological quality of the included studies was assessed using the Agency for Healthcare Research and Quality (AHRQ) checklist [29] (Table 1).
Definitions
According to the definition by the Oxford English Dictionary, screen time is “the time spent using a device such as a computer or games console” [30]. In the current meta-analysis, screen time was defined as “time spent passively watching screen-based entertainment (TV, computer, mobile devices). As defined by the WHO, this does not include active screen-based games where the physical activity or movement is required” [31].
In the current meta-analysis, a child was defined as an age under 10 years old and an adolescent as an age of 10–19 years old, as previously described by the WHO [32].
Central obesity was defined by the international age and sex specific cut-offs of WC [≥ 85th percentile and more than 90th percentile] and the thresholds of WHR [WHR ≥ 0.5] [9, 33, 34].
Statistical analysis
STATA software version 13 (STATA Corp, College Station, TX, USA) was used for data analysis, and P-values less than 0.05 were considered statistically significant. We included the studies that reported the comparison between WC or WHR [mean (SD)] in the highest versus lowest screen time category and the studies that evaluated the odds of central obesity in the meta-analysis. Therefore, the weighted mean difference (WMD) or the odds ratio (OR) with a 95% confidence interval (CI) was reported. The method of Hozo et al.[35] was used when the median and range were reported instead of mean and SD, and the median values were considered as best estimates of mean when the sample size of the study was more than 25 and the SD was calculated as follows: \(S^{2} \approx \left( {\frac{1}{12}(\frac{{\left( {a - 2m + b} \right)^{2} }}{4} + \left( {b - a} \right)^{2} } \right)\). Also, Walter and Yao’s method was used for calculating the missing SDs, as follows: SD = (b − a)/4 [36, 37]. If the number of participants in categories was not provided, an equal number of participants in each category was assumed. Cochran's Q and I-squared tests were used to identify between-study heterogeneity. The possible sources of heterogeneity were identified using subgrouping and meta-regression analysis. Begg’s Funnel plots followed by Begg's adjusted rank correlation and Egger's regression asymmetry tests were used to assess the publication bias.
Results
Study characteristics
Nine individual studies were included in the two-class meta-analysis of the association between increased screen time and odds of central obesity [9, 26, 33, 34, 38, 39] (Table 2). Since the study by Castro JAC et al. [9] reported the results related to three screen devices (TV, PC, and VF) separately, they were included as three independent studies. Similarly, the study by Huang HM et al. [34] reported separate results for TV and PC, and the study by Byun et al. [33] reported separate results for TV and PC/video games. Hence, these studies were included as two independent studies.
The meta-analysis included 8484 individuals. One study reported significantly higher odds of central obesity in children and adolescents with a screen time higher than 2 h per day compared to those with a screen time lower than 2 h per day (OR 1.67; 95% CI 1.17–2.61; P = 0.005). Other studies reported non-significant higher odds of central obesity in children and adolescents in the high screen time category [9, 26, 34, 38, 39].
Regarding the comparison of WC between highest versus lowest screen time categories, six individual studies with a total number of 10,791 participants were included (Table 3). In the study by Castro JAC et al.[9], the results of three screen devices (i.e., TV, PC, and VG) were reported as three independent studies. According to their results, WC was higher only among those playing video games for more than 2 h per day (P = 0.01); for other types of screens, no significant difference was observed. Berentzen et al. [25] conducted a community-based study among 1447 children and adolescents aged 10–14 years and reported a significantly higher WC in the highest versus lowest quintile of centrally obese children and adolescents (P = 0.0001). The age range of participants was 9–19 years old. Screen time and screen time-based sedentary behavior was investigated using validated questionnaires for children and adolescents of that particular region. The screen time was reported separately for TV, PC, and video games on weekdays and weekends; then the results were summed up to report the total screen time. All the mentioned studies involved a combination of male and female healthy children and adolescents. In addition, two studies were recruited in Brazil [9, 38], one in China [39], one in Qatar [26], one in Taiwan [34], one in Germany [40], one in the Netherlands [25], one in Iran [41], and one in South Korea [33].
Results of the meta-analysis
According to the results of the current meta-analysis, there was no association between odds of central obesity and screen time in children and adolescents (OR 1.136; 95% CI 0.965–1.337; P = 0.125) (Fig. 2). Since between-study heterogeneity was higher than 50%, we performed subgrouping. The results showed that continent and age range were the possible sources of the observed between-study heterogeneity (Table 4). Also, in a sensitivity analysis using the leave-one-out method, by removing the video game result of the study by Castro JAC et al. [9], the results were significant (OR 1.196; 95% CI 1.024–1.397; P = 0.024). Moreover, WC was 1.23 cm higher in children and adolescents with the highest screen time compared to those with the lowest screen time (WMD = 1.23; 95% CI = 0.342–2.112; P = 0.007; Fig. 3). The results of subgrouping indicated no heterogeneity for studies with a sample size of more than 1000 people (Table 5). In addition, no evidence of publication bias was reported according to the visual asymmetry of funnel plots and the results of Begg’s and Egger’s tests [95% OR of central obesity and screen time: Egger’s test (P = 0.162) and Begg’s test (P = 0.677); WC in the highest versus lowest screen time category: Egger’s test (P = 0. 0.213) and Begg’s test (P = 0.188) (Additional file 1: Fig. S1)].
Discussion
In this meta-analysis, we provided the quantified results of the association between increased screen time and odds of central obesity in children and adolescents. Considering the results of more than 12,563 children and adolescents, we found no significant association between odds of central obesity and screen time. However, WC was significantly higher (1.2 cm) in those with the highest screen time compared to those with the lowest screen time. Most of the included studies were performed on adolescents and only two studies were performed among both children and adolescents.
One important reason for performing the current meta-analysis was the discrepancy between the results of different studies. For example, in the study by Castro JA et al. [9], only those with TV time of more than 2 h per day had greater odds of abdominal obesity while higher PC use or video games were associated with a non-significantly lower chance of abdominal obesity. In contrast, several other studies revealed higher odds of central obesity by increased time of using PCs or playing video games [33, 34, 42]. Therefore, it was necessary to perform a summative study to obtain more accurate results.
The role of several confounders like age, gender, and physical activity level should also be mentioned. In the current meta-analysis, all the included studies were performed in both genders; so, it was impossible to infer a gender-specific result. Although females seemed to have higher body fatness [43], some evidence showed that the prevalence of abdominal obesity was increasing in males [44, 45]; therefore, there is no consensus about the association between central obesity and gender [46]. In another study, boys had a higher screen time compared to girls; at the same time, boys also had higher physical activity levels [47].
Although most of the included studies were adjusted for confounders, including age, gender, diet, and physical activity, there was still an association between obesity and screen time after this adjustment [9, 33, 38, 39]. This further confirms that the association between screen and central obesity is independent of confounders. It should also be noted that the included studies were performed between 2012 and 2020; in this period, the prevalence of screen use has dramatically increased among children and adolescents. According to the report entitled “Children and parents: media use and attitudes report 2019”, the screen use and ownership among children aged 5–15 years increased from 35% in 2015 to 45% in 2019, which is mostly attributed to tablet and mobile cellphone use [48]. At the same time, the increased prevalence of central obesity occurred among children and adolescents [49, 50]; therefore, studying the association between central obesity and screen time could not be affected by time.
Due to the relatively limited number of included studies, the results of subgrouping might not be representative. However, community-based studies are more reliable than school-based studies because they show a greater relationship between central obesity and screen time.
We sub-grouped our results according to the type of screen. In our meta-analysis, by removing the results of video games reported in the study by Castro JAC et al. [9], there was a significant change in the results. In the literature review, we witnessed this inconsistency in the health effects of video games in different studies. While one study reported higher WC among those playing video games for more than 2 h per day, in a meta-analysis by Gao Z et al. [51], playing active video games was associated with beneficial health effects like increased heart rate, energy expenditure, and oxygen consumption. However, the effect size was only meaningful when playing active video games was compared with sedentary behaviors and not with regular physical activities. Therefore, they could only be suggested as a good alternative to sedentary behavior. Further studies are needed to better elucidate the association between video games and health among children and adolescents [52].
In the current study, odds of central obesity was not associated with screen time that might be attributed to the high heterogeneity values of the included studies (62%). In sensitivity analysis, using the leave-one-out method, by removing the video game result of the study by Castro JAC et al. [9], the results were significant (OR 1.196; 95% CI 1.024–1.397; P = 0.024). This further clears that the diverse screen tools might show different results and further studies in different screen tools with help to better clarify the screen time and central obesity association. We observed higher WC in those with the highest versus lowest screen time. High screen time, as a sedentary behavior, could be associated with increased obesity risk via increased fat deposition in vessels or adipose tissue, particularly the visceral abdominal area [53,54,55]. Second, increased screen activities are associated with increased food intake. Numerous studies confirmed that watching television increases motivated response to food intake and snacking behavior among children and adolescents [56,57,58,59]; this is also true for video games [60,61,62] and PC use [63, 64]. Therefore, the association between screen time and increased central or general obesity is bidirectional. Due to the cross-sectional design of the included studies in this meta-analysis, reverse or reciprocal causality is possible, where adiposity or obesity may lead to increased screen time. More importantly, food-related advertisements on TV can potentially affect children’s food behaviors by promoting junk food and fast food consumption, and increase obesity risk [65,66,67,68,69,70]. Therefore, the association between central obesity and screen use is a multi-dimensional problem and all its aspects need to be studied.
Conclusion
For the first time, this meta-analysis study revealed higher WC in children and adolescents with highest screen time versus lowest screen time. Although, odds of central obesity was not associated with screen time in this age group. This might be attributed to high heterogeneity of the included studies and the diversity of screen tools that were used in different studies. Therefore, further studies with interventional or observational design will help to evaluate this association more logically. Also, due to the observational design of the included studies, by recruiting further interventional or longitudinal studies, the causality inference will be possible in the future.
References
Górnicka M, Hamulka J, Wadolowska L, Kowalkowska J, Kostyra E, Tomaszewska M, Czeczelewski J, Bronkowska M. Activity–inactivity patterns, screen time, and physical activity: the association with overweight, central obesity and muscle strength in Polish teenagers. Report from the ABC of healthy eating study. Int J Environ Res Public Health. 2020;17(21):1–21.
Tang D, Bu T, Liu Y, Dong X. The impact of mothers’ dietary patterns on children’s nutritional status in China. Am J Health Behav. 2020;44(5):719–31.
Farhangi MA, Jahangiry L, Asghari-Jafarabadi M, Najafi M. Association between dietary patterns and metabolic syndrome in a sample of Tehranian adults. Obes Res Clin Pract. 2016;10:S64–73.
World Health Organization, Global Recommendations on Physical Activity for Health. 2010, Genève, Switzerland.
Paladugu N, Rayiti R, Nutakki S, Gadde R, Sailaja K, Ghanta VK, Kanagala VS. Factors associated with body mass index in children: a community-based study. Asian J Pharm Clin Res. 2021;14(1):176–81.
Lopez-Gonzalez D, Partida-Gaytán A, Wells JC, Reyes-Delpech P, Avila-Rosano F, Ortiz-Obregon M, Gomez-Mendoza F, Diaz-Escobar L, Clark P. Obesogenic lifestyle and its influence on adiposity in children and adolescents, evidence from Mexico. Nutrients. 2020;12(3):819.
Lai L, Zhang T, Zeng X, Tan W, Cai L, Chen Y. Association between physician-diagnosed asthma and weight status among Chinese children: the roles of lifestyle factors. Int J Environ Res Public Health. 2020;17(5):1599.
Farhangi MA, Ostadrahimi A, Mahboob S. Serum calcium, magnesium, phosphorous and lipid profile in healthy Iranian premenopausal women. Biochemia Medica. 2011;21(3):312–20.
Castro JAC, Nunes HEG, Silva DAS. Prevalence of abdominal obesity in adolescents: association between sociodemographic factors and lifestyle. Revista Paulista de Pediatria. 2016;34(3):343–51.
Ulaganathan V, Kandiah M, Shariff ZM. A case–control study on the association of abdominal obesity and hypercholesterolemia with the risk of colorectal cancer. J Carcinogenesis 2018;17.
Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr. 2007;86:33–40.
Paul R, Mukkadan J. Modulation of blood glucose, oxidative stress, and anxiety level by controlled vestibular stimulation in prediabetes. J Nat Sci Biol Med. 2020;11:111–7.
Farhangi MA, Najafi M. Dietary inflammatory index: a potent association with cardiovascular risk factors among patients candidate for coronary artery bypass grafting (CABG) surgery. Nutr J. 2018;17(1):1–10.
Kelishadi R, Mirmoghtadaee P, Najafi H, Keikha M. Systematic review on the association of abdominal obesity in children and adolescents with cardio-metabolic risk factors. J Res Med Sci. 2015;20(3):294–307.
Grigorakis DA, Georgoulis M, Psarra G, Tambalis KD, Panagiotakos DB, Sidossis LS. Prevalence and lifestyle determinants of central obesity in children. Eur J Nutr. 2016;55(5):1923–31.
Chen YT, Holahan CK, Castelli DM. Sedentary behaviors, sleep, and health-related quality of life in middle-aged adults. Am J Health Behav. 2021;45(4):785–97.
Farhangi MA, Mesgari-Abbasi M, Nameni G, Hajiluian G, Shahabi P. The effects of vitamin D administration on brain inflammatory markers in high fat diet induced obese rats. BMC Neurosci. 2017;18(1):1–8.
Cheng L, Pohlabeln H, Ahrens W, Lauria F, Veidebaum T, Chadjigeorgiou C, Molnár D, Eiben G, Michels N, Moreno LA, Page AS, Pitsiladis Y, Hebestreit A. Cross-sectional and longitudinal associations between physical activity, sedentary behaviour and bone stiffness index across weight status in European children and adolescents. Int J Behav Nutr Phys Act. 2020;17(1):1–3.
Leman MA, Claramita M, Rahayu GR. Predicting factors on modeling health behavior: a systematic review. Am J Health Behav. 2021;45(2):268–78.
Maisano MS, Shonkoff ET, Folta SC. Multiple health behavior change for weight loss: a scoping review. Am J Health Behav. 2020;44(5):559–71.
Wachira LJM, Muthuri SK, Ochola SA, Onywera VO, Tremblay MS. Screen-based sedentary behaviour and adiposity among school children: results from international study of childhood obesity, lifestyle and the environment (iscole) - Kenya. PLoS ONE. 2018;13(6):e0199790.
Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Int J Obes (Lond). 2005;2:29–39.
Pappas S. What do we really know about kids and screens? 2020 [cited 2020; Available from: https://www.apa.org/monitor/2020/04/cover-kids-screens.
Jontony N, Hill EB, Taylor CA, Boucher LC, O’Brien V, Weiss R, Spees CK. Diet quality, carotenoid status, and body composition in NCAA division I athletes. Am J Health Behav. 2020;44(4):432–43.
Berentzen NE, Smit HA, van Rossem L, Gehring U, Kerkhof M, Postma DS, Boshuizen HC, Wijga AH. Screen time, adiposity and cardiometabolic markers: mediation by physical activity, not snacking, among 11-year-old children. Int J Obes (Lond). 2014;38(10):1317–23.
Kerkadi A, Sadig AH, Bawadi H, Thani AAMA, Chetachi WA, Akram H, Al-Hazzaa HM, Musaiger AO. The relationship between lifestyle factors and obesity indices among adolescents in Qatar. Int J Environ Res Public Health. 2019;16(22):4428.
Ji M, An R, Qiu Y, Guan C. The impact of natural disasters on dietary intake. Am J Health Behav. 2020;44(1):26–39.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res. 2017;61:1600324.
Oxford University Press, Oxford English Dictionary. 2020, Oxford, UK. : Oxford University Press.
World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. . 2020; Available from: https://apps.who.int/iris/handle/10665/311664.
Organization, W.H. Adolescent health in the South-East Asia Region. 2020; Available from: https://www.who.int/southeastasia/health-topics/adolescent-health.
Byun W, Dowda M, Pate RR. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27(4):388–94.
Huang HM, Chien LY, Yeh TC, Lee PH, Chang PC. Relationship between media viewing and obesity in school-aged children in Taipei, Taiwan. J Nurs Res. 2013;21(3):195–203.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
Weir CJ, Butcher I, Assi V, Lewis SC, Murray GD, Langhorne P, Brady MC. Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol. 2018;18(1):25.
Walter S, Yao X. Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007;60(8):849–52.
De Lima TR, Moraes MS, Andrade JHC, De Farias JM, Silva DAS. Associated factors with the isolated and simultaneous presence of overweight and abdominal obesity in adolescents. Revista Paulista de Pediatria 2020;38.
Zhang Y, Zhang X, Li J, Zhong H, Pan CW. Associations of outdoor activity and screen time with adiposity: findings from rural Chinese adolescents with relatively low adiposity risks. BMC Public Health. 2020;20(1):1–9.
Suchert V, Hanewinkel R, Isensee B. Screen time, weight status and the self-concept of physical attractiveness in adolescents. J Adolesc. 2016;48:11–7.
Safiri S, Kelishadi R, Qorbani M, Abbasi-Ghah-Ramanloo A, Motlagh ME, Ardalan G, Shafiee G, Ahadi Z, Sanaei M, Asayesh H, Larijani B, Heshmat R. Screen time and its relation to cardiometabolic risk among children and adolescents: The CASPIAN-III study. Iran J Public Health. 2015;44(1):35–44.
Khan W, Augustine D, Rao RS, Patil S, Awan KH, Sowmya SV, Haragannavar VC, Prasad K. Lipid metabolism in cancer: a systematic review. J Carcinogenesis 2021;20.
Taylor RW, Grant AM, Williams SM, Goulding A. Sex differences in regional body fat distribution from pre- to postpuberty. Obesity (Silver Spring). 2010;18:1410–6.
Schroder H, Ribas L, Koebnick C, Funtikova A, Gomez SF, Fito M. Prevalence of abdominal obesity in Spanish children and adolescents: Do we need waist circumference measurements in pediatric practice? PLoS ONE. 2014;9:e87549.
Silva DA, Pelegrini A, Silva AF, Grigollo LR, Petroski EL. Abdominal obesity and associated factors among adolescents: comparison of two economically different Brazilian regions. Arq Bras Endocrinol Metabol. 2012;56:291–9.
De Moraes AC, Fadoni RP, Ricardi LM, Souza TC, Rosaneli CF, Nakashima AT. Prevalence of abdominal obesity in adolescents: a systematic review. Obes Rev. 2011;12:69–77.
Wynne C, Comiskey C, Hollywood E, Quirke MB, O’Sullivan K, McGilloway S. The relationship between body mass index and health-related quality of life in urban disadvantaged children. Qual Life Res. 2014;23(6):1895–905.
Parliament U. Screen use and health in young people. PostNote. 2020;635:1–7.
Wong M, Huang J, Wang J, Chan PS, Lok V, Chen X, Leung C, Wang HH, Lao XQ, Zheng Z-J. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. 2020;35(7):673–83.
Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol. 2020;49(3):810–23.
Gao Z, Chen S, Pasco D, Pope Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes Rev. 2015;16(9):783–94.
Kracht CL, Joseph ED, Staiano AE. Video games, obesity, and children. Curr Obes Rep. 2020;9(1):1–14.
Pitanga FJG, Alves CFA, Pamponet ML, Medina MG, Aquino R. Screen time as discriminator for overweight, obesity and abdominal obesity in adolescents. Revista Brasileira de Cineantropometria e Desempenho Humano. 2016;18(5):539–47.
Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, Wilmot EG. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS ONE. 2012;7(4): e34916.
Schroeder K, Kubik MY, Sirard JR, Lee J, Fulkerson JA. Sleep is inversely associated with sedentary time among youth with obesity. Am J Health Behav. 2020;44(6):756–64.
Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85(2):355–61.
Borghese M, Tremblay M, Leduc G, Boyer C, Belanger P, LeBlanc A, Francis C, Chaput J. Television viewing and food intake pattern of normal weight, overweight, and obese 9–11 year-old Canadian children. Obes Rev. 2014;15:232.
Taveras EM, Sandora TJ, Shih MC, Ross-Degnan D, Goldmann DA, Gillman MW. The association of television and video viewing with fast food intake by preschool-age children. Obesity (Silver Spring). 2006;14(11):2034–41.
Domoff SE, Sutherland E, Yokum S, Gearhardt AN. The association of adolescents’ television viewing with Body Mass Index percentile, food addiction, and addictive phone use. Appetite. 2021;157:104990.
Chaput JP, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A, Astrup A, Sjödin A. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93(6):1196–203.
Cessna T, Raudenbush B, Reed A, Hunker R. Effects of video game play on snacking behavior. Appetite. 2007;49(1):282.
Chaput JP, Tremblay A, Pereira B, Boirie Y, Duclos M, Thivel D. Food intake response to exercise and active video gaming in adolescents: effect of weight status. Br J Nutr. 2015;115(3):547–53.
Shi L, Mao Y. Excessive recreational computer use and food consumption behaviour among adolescents. Ital J Pediatr. 2010;36(1):1–4.
Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ. Television viewing, computer use, and BMI among US children and adolescents. J Phys Act Health. 2009;6(s1):S28–35.
Gilbert-Diamond D, Emond JA, Lansigan RK, Rapuano KM, Kelley WM, Heatherton TF, Sargent JD. Television food advertisement exposure and FTO rs9939609 genotype in relation to excess consumption in children. Int J Obes (Lond). 2017;41(1):23–9.
Ustjanauskas AE, Harris JL, Schwartz MB. Food and beverage advertising on children’s web sites. Pediatr Obes. 2014;9(5):362–72.
Lee B, Kim H, Lee SK, Yoon J, Chung SJ. Effects of exposure to television advertising for energy-dense/nutrient-poor food on children’s food intake and obesity in South Korea. Appetite. 2014;81:305–11.
Dibildox J. Analysis of TV, advertising and other behavioral determinants of overweight and obesity in childhood. Salud Publica Mex. 2014;56(Suppl 2):s162–6.
Kar S, Khandelwal B. Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J Natl Sci Biol Med. 2015;6(2):356.
Lutz M, Vargas C, Stojanova J, Arancibia M. Diet and depressive disorders. Arch Clin Psychiatry (São Paulo). 2021;48:117–22.
Berentzen NE, Smit HA, Van Rossem L, Gehring U, Kerkhof M, Postma DS, Boshuizen HC, Wijga AH. Screen time, adiposity and cardiometabolic markers: mediation by physical activity, not snacking, among 11-year-old children. Int J Obes. 2014;38:1317–23.
Acknowledgements
We wish to thank the Student Research Committee of Tabriz University of Medical Sciences for the financial support (Grant Number: 68709; Identifier: IR.TBZMED.VCR.REC.1400.373).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of the current study was registered in the PROSPERO system (Registration Number: CRD42021243523). Also, the research was approved by the ethics committee of Tabriz University of Medical Sciences, Tabriz, Iran (Code: IR.TBZMED.VCR.REC.1400.373).
Competing interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. PRISMA Checklist. Table S2. Search strategies and the number of records according to different electronic database. Figure S1. Begg’s funnel plot (with pseudo 95% CIs) of the odds ratios of the association between screen time and central obesity among children and adolescents (A); the comparison of waist circumference (WC) between highest versus lowest screen time categories (B).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ghasemirad, M., Ketabi, L., Fayyazishishavan, E. et al. The association between screen use and central obesity among children and adolescents: a systematic review and meta-analysis. J Health Popul Nutr 42, 51 (2023). https://doi.org/10.1186/s41043-023-00391-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00391-5