Abstract
Background
Globally, sexual and reproductive health is a significant public health issue for women of the reproductive age group. A modern contraceptive method enables individuals and families to manage fertility by reducing unintended pregnancies, abortions, pregnancy-related morbidity, and death. A modern contraceptive method is a drug or medical treatment that prevents sexual activity from leading to pregnancy. However, there is limited reliable and updated data on factors associated with modern contraceptive utilization among reproductive-age women at the national level in Kenya. So, the major goal of this study was to evaluate factors associated with modern contraceptive utilization among women of reproductive age in Kenya at the national level, as evidenced by the 2022 Kenyan demographic and health survey.
Methods
The most recent datasets from the Kenyan Demographic and Health Survey were used for secondary data analysis. In all, 14,987 women of reproductive age participated in the investigation. Data for multivariable analysis on the factors influencing modern contraceptive utilization among Kenyan women of reproductive age can be obtained from the Kenyan Demographic and Health Survey. Finally, the odd ratio and percentages were presented along with their 95% confidence intervals.
Result
This study includes a total weighted sample of 14,987 reproductive-age women from the Kenyan demographic and health survey. Of the total contraceptive use, 90.1% of the study participants used modern contraceptives. Being married [AOR: 1.593, 95% CI (1.302, 1.948)], living in an urban area [AOR: 1.230, 95% CI (1.060, 1.428)], reading a magazine [1.002, 95% CI (0.921, 1.091)], listening to radio [AOR: 1.265, 95% CI (1.101, 1.454)], not breastfeeding [AOR: 1.296, 95% CI (1.114, 1.507), and having more than two children [AOR: 2.350, 95% CI (1.603, 3.445)] were the factors that promote modern contraceptive utilization. Conversely, having a history of terminated pregnancy [AOR: 0.767, 95% CI (0.657, 0.897), being Muslim [AOR: 0.566, 95% CI (0.418, 0.766)], and being in the 35–39 age range [AOR: 0.766, 95% CI (0.605, 0.971)] were all associated with a lower use of modern contraceptives.
Conclusion
Certain factors such as marriage, living in urban areas, having more than two children, having a female-led household, belonging to the middle class, reading magazines, listening to the radio, and not breastfeeding have a positive correlation with the use of modern contraceptives. Conversely, being a Muslim, aged between 35 and 39, and having a history of miscarriages are negatively correlated with the use of modern contraceptives. This indicates that addressing socioeconomic, geographic, and cultural barriers could improve the effectiveness of modern contraceptive.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Contraception enables individuals and families to manage fertility by reducing unintended pregnancy, abortions, pregnancy-related morbidity, and death [1]. Contraceptive method is a practice that helps individuals or couples to attain their desired children as their plan, and available methods of contraception should be customized to individual needs with a range of options that are acceptable to all [2]. A modern contraceptive method is a drug or medical treatment that prevents sexual activity from leading to pregnancy. Modern contraceptive methods include barrier methods such as male and female condoms, diaphragms, cervical caps, and sponges; hormonal contraceptives that include oral, injectable, transdermal, vaginal ring, and implants; and intrauterine devices (IUD) [3, 4]. Hormonal methods of birth control (contraception) contain either estrogen and progestin or progestin-only; they are a safe and reliable way to prevent pregnancy for most people [5].
Globally, 1.9 billion women between the ages of 15 and 49 require family planning, which is predicted to rise. Of them, 842 million utilize contraceptives, and 270 million still need contraceptives [6]. A modern contraceptive method of family planning was used by 58% of married or in-union women of reproductive age worldwide in 2017, accounting for 92% of all contraceptive users [7]. Substantial progress has been made in Kenya toward achieving universal access to FP. But women’s unmet need for FP continues [8, 9]. Pregnancies in Kenya are unplanned in 43% of cases. Adolescents have the greatest unmet need for family planning [10]. Globally, sexual and reproductive health is a significant public health issue for women of reproductive age. Women in low and middle-income countries (LMICs) are at higher risk of dying due to pregnancy-related complications [11, 12]. Numerous studies have demonstrated that the utilization of modern contraceptives has a significant association with factors such as marital status, number of living children, religion, education, and place of residence [13,14,15].
Several studies were conducted in Kenya related to modern contraceptive utilization in different settings with small sample sizes. However, few studies were conducted at the national level. In addition to this, the Kenyan DHS reports simply report the proportion or frequency of certain events without considering the factors associated with them. The major objective of this study was to evaluate factors associated with modern contraceptive utilization among reproductive women in Kenya at the national level by using the Kenyan demographic and health survey. The findings of this study would also provide better evidence for policymakers and other stakeholders, which in turn might enable the designing and execution of appropriate intervention programs at different levels to promote modern contraceptive utilization that reduces maternal and child morbidity and mortality.
Methods and material
Study setting and period
Kenya is a country located in East Africa with a population of over 47.6 million, according to the 2019 census. It is the 28th most populous country in the world and the 7th most populous in Africa. Nairobi is Kenya’s capital and largest city. Kenya shares borders with South Sudan to the northwest, Ethiopia to the north, Somalia to the east, Uganda to the west, Tanzania to the south, and the Indian Ocean to the southeast [16]. The 2022 Kenya Demographic and Health Survey (2022 KDHS) was implemented by the Kenya National Bureau of Statistics (KNBS) in collaboration with the Ministry of Health (MoH) and other stakeholders. This is the 7th KDHS implemented in the country. Data collection took place from 17 February to 31 July 2022 [17].
Data source/extraction
After permission was secured through an online request explaining the aim of the study, the data were taken from the Measure Demographic and Health Surveys (DHS) website (http://www.dhsprogram.com/).
Study design
A community-based cross-sectional study design was employed. The 2022 KDHS employed a two-stage stratified sample design, where in the first stage 1,692 clusters were selected from the Kenya Household Master Sample Frame (K-HMSF) using the Equal Probability Selection Method (EPSEM). The clusters were selected independently in each sampling stratum. Household listing was carried out in all the selected clusters, and the resulting list of households served as a sampling frame for the second stage of selection, where 25 households were selected from each cluster. Therefore, all households from these clusters were selected for the sample. This resulted in 42,022 households being sampled for the 2022 KDHS. Details about the study design and sampling techniques were available in the final Kenyan demographic health survey reports [17].
Study population
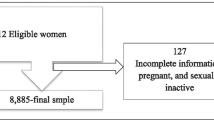
All women aged 15–49 who were either permanent residents of the selected households or visitors who stayed in the household the night before the survey were eligible to be interviewed. The Woman’s Questionnaire was used to collect information from all eligible women aged 15–49. The total number of eligible women that were interviewed was 32,156. 13,143 of the 32,156 women were from an urban area, as opposed to 19,013, who were from a rural area. Of the total interviewed women, 14,987 used contraceptives, and the remaining 17,169 didn’t. So, they were excluded from this analysis. Modern contraceptive utilization among women of reproductive age was the outcome variable for this study. So, the total number of samples used in this analysis was 14,987 [17].
Study variables
The outcome variable for this study was modern contraceptive utilization. If the women utilized modern contraceptives, which were coded as “0,” if they utilized another method of contraceptive (traditional and folkloric), it was coded as “1.”.
Predictor variables
Age group, place of residence, educational status, marital status, religion, sex of household head, wealth index, reading newspapers, listening to radio, watching television, history of terminated pregnancy, currently breastfeeding, and number of children.
Data management and analysis
In all of our analyses, we took weighting, stratification, and clustering into account to consider the complex survey design. We pooled and compared data from different regions with varying target population sizes to normalize the weights. We divided the national total of women and the standard weights of women by the proportion of survey samples that corresponded to them to arrive at this result. We used STATA version 14 for data extraction, recording, and both descriptive and analytical analysis. We conducted bivariate analyses on various variables, including age group, place of residence, educational status, marital status, religion, sex of household head, wealth index, reading newspapers, listening to radio, watching television, history of a terminated pregnancy, current breast-feeding, and number of children. We used the results of the bivariate analysis to select variables for the multivariate analysis. For the multivariate analysis, we only considered factors with p-values of less than 0.05.
Ethical consideration
Since the secondary survey data we used for this investigation came from readily available demographic and health survey programs, neither an ethical review nor participant agreement were required. We received authorization from the DHS Program to utilize the information we collected from their website, and they provided us with access to their website.
Socio-demographic factors of the study participants
A total of 14,987 reproductive age women were involved in this study. About 3451 (23.0%) were found between the age ranges of 15–19 years old. The majority of respondents 8740 (58.3%) were live in rural area, 6208(41.4%) were protestant, 6004(40.1%) were attending primary educations, 9567(63.8%) were married, 10,180(67.9%) were male headed households, 10,967(73.2%) were poor, 3014(20.1%) were reading magazine, 11,360 (81.2%) were listening radio, 10,422(69.5%) were watching television, 2099 (14.0%) had history of terminated pregnancy, 3698 (24.7%) were breast feeding, had less than or equal to two children14347(95.7%) and from the total contraceptive utilizer, modern contraceptive utilization accounts for 13,501 (90.1%) (Table 1).
Factors analysis associated with modern contraceptive utilization
Age group, place of residence, educational status, marital status, religion, sex of household head, wealth index, reading newspapers, listening to radio, watching television, history of a terminated pregnancy, current breastfeeding, and number of children were all taken into account in the bivariate analysis. The results of the bivariate analysis showed that among women of reproductive age, modern contraceptive utilization was statistically and significantly associated with age group, place of residence, educational status, marital status, religion, sex of household head, wealth index, reading newspapers, listening to radio, watching television, history of a terminated pregnancy, currently breastfeeding, and number of children.The multivariable logistic regression analysis also revealed that age group, place of residence, educational status, marital status, religion, sex of household head, wealth index, reading newspapers, listening to radio, watching television, history of terminated pregnancy, currently breastfeeding, and number of children were significantly associated with modern contraceptive utilization among reproductive-age women.
The results of this study reveal that, when compared to women between the ages of 15 and 19, the odds of modern contraceptive utilization were 0.766 times lower among those between the ages of 35 and 39 [AOR: 0.766, 95% CI (0.605, 0.971); P = 0.010]. Women living in urban areas were 1.230 times more likely to use modern contraceptives than women living in rural areas [AOR: 1.230, 95% CI (1.060, 1.428); P = 0.006]. In comparison to women who were Catholic, the odds of modern contraceptive usage were 0.566 times lower among Islamic women [AOR: 0.566, 95% CI (0.418, 0.766); P = 0.000].
In comparison to male-heeded households, female-headed households had a 1.016-fold higher likelihood of using modern contraceptives [AOR: 1.016(0.892, 1.158); P = 0.042]. Among married women, the probability of using modern contraception was 1.593 times higher [AOR: 1.593, 95% CI (1.302, 1.948); P = 0.000] in comparison to women who had never been married. In comparison to women with a poor wealth index, the odds of modern contraceptive usage were 1.084 more likely among those with a middle wealth index [AOR: 1.084 (0.920, 1.277); P = 0.001].
Women who read magazines [AOR: =1.002 (0.921, 1.091); P = 0.015] and listed radio [AOR: 1.265 (1.101, 1.454); P = 0.004] had higher odds of using modern contraceptives than their counterparts, respectively. Women with a history of pregnancy termination were 0.767 times less likely to use modern contraceptives [AOR: 0.767 (0.657, 0.897); P = 0.007] than women without a history of pregnancy termination. Compared to women who were breastfeeding, the likelihood of modern contraceptive use among currently non-breastfeeding women was 1.296 times higher [AOR: 1.296, 95% CI (1.114, 1.507; P = 0.000)]. When compared to women who had less than or equal to two children, the likelihood of modern contraceptive usage was 2.350 more likely among those who had more than two children [AOR: 2.350, 95% CI (1.603, 3.445); P = 0.000] (Table 2).
Discussions
The multivariable logistic regression analysis also revealed that age group, place of residence, educational status, religion, marital status, wealth index, sex of household head, reading newspaper, listening to radio, history of terminated pregnancy, current breastfeeding, and number of children were significantly associated with hormonal contraceptive utilization among reproductive-age women. This finding was in line with study that was conducted in Kenya [5], in Ethiopia [14], and in Uganda [18].
According to the study’s results, women between the ages of 15 and 19 were more likely than those between the ages of 35 and 39 to use modern contraceptives. This finding was in line with study that was conducted in Uganda [18], and in sub-Saharan countries [19]. It is possible that infrequent sexual activity and the conviction that there is no risk of pregnancy contribute to the lower likelihood of using modern contraception as people age [20, 21]. It is possible that women between the ages of 15 and 19 are still in school and are in the early stages of their reproductive lives. In order to meet their academic objectives, they might use contraception given their education and lack of desire to start a family.
Women of reproductive age who lived in urban areas were more likely than those who lived in rural areas to use modern contraceptives. This finding was in line with study that was conducted in Yemen [22], in Ethiopia [23,24,25] and in Pakistan [26]. This discrepancy may have existed due to the great availability of family planning services and the rising number of health institutions in urban areas. However, most women face several barriers to obtaining and using modern contraceptives, particularly those who live in rural areas [27] such as, low educational attainment, low economic status, deep rooted cultural belief [28], poor spousal communication, sociocultural norms, the husband’s role as the primary decision-maker, fear of side-effects, a lack of knowledge [29, 30], long distances to healthcare facilities, and inadequate stock of preferred types of modern contraceptives [31, 32]. Additionally, rural women require a larger number of children to assist them in their fieldwork, which negatively impacts their use of modern contraceptive methods [33, 34].
Compared to women who were Catholic, the likelihood of modern contraceptive use was lower among Muslim women. Compared to women who were Catholic, the likelihood of modern contraceptive use was lower among Muslim women. This finding was in line with studies that were conducted in Ghana [35], in Liberia [36]. This variations could be because religious resistance to their use may be more evident in Islam than in other religions [37, 38]. Additionally, most people who believed that family planning was incompatible with their beliefs declared that they had a duty to have as many children as God would allow them to have. In contrast to this, others thought family planning was appropriate given their moral obligation to raise and safeguard their children by reducing the number of children [38].
Married women were more likely than single women to use modern contraceptives. These findings were in line with studies that were conducted in Ethiopia [14], in Tanzania [39], and in Ethiopia [40]. The possible explanation is that women who were never in a union might not be in any sexual relationship, therefore resulting in their low use of modern contraceptives. Furthermore, from the perspective of males as a potential factor that influences the usage of modern contraceptives for fertility control, these differences may have arisen [41].
The likelihood of using modern contraceptives was higher among women with a middle wealth index than among those with a low wealth index. This finding was in line with the studies which were conducted in Nigeria [42], and in Ethiopia [43]. The contributing factors for these disparities were that the usage of contraceptives has a financial cost associated with it; women with a middle wealth index might be able to avoid any financial barriers to using modern contraceptives, while poor women might not [44, 45]; the level of household wealth has a significant impact on access to education, basic healthcare services, and health information [46].
In comparison, women who read magazines and listed radio stations were more likely to use modern contraceptives. This finding was in line with studies that were conducted in sub-Saharan Africa [47], in Ethiopia [48], Sierra Leone [49], Senegal [50] and Nigeria [51]. This may be because the media can enormously impact increasing awareness, intention, and use of reversible modern methods. After all, it constantly provides women with information and encouragement to continue using contraceptives.
Comparatively speaking, women who had previously terminated a pregnancy used modern contraception more frequently than those who had not. This finding was in line with a study that was conducted in Ethiopia [52]. This could be because women who have had their pregnancies terminated tend to use contraceptives less frequently. After all, they intend to become pregnant.
Compared to breastfeeding women, non-breastfeeding women were more likely to use modern contraceptives. This finding was in line with a study that was conducted in Ethiopia [53]. Menstruation not returning or low risk of fertility; fear of side effects; spouse disapproval; and fear of changing the composition of breast milk were the reasons for not using contraceptives [54,55,56].. Additionally, it is possible that this difference could be attributed to exclusive breastfeeding, which is a natural form of birth control. When a woman gives birth to her child, her body naturally stops ovulating if she exclusively breastfeeds and feeds her baby at least every four hours during the day and every six hours at night. If a woman misses her ovulation, she cannot become pregnant.
Women who had more than two children were more likely than those who had less than or equal to two children to use modern contraceptives. This finding was in line with studies that were conducted in Ethiopia [57], in Uganda, Malawi [58] and north west Ethiopia [59]. This may be the case because it may be necessary for women who are childless to have children to reach the optimal number of children. On the other hand, a possible reason might be that women who have achieved the desired number of children want to space out or limit further pregnancies by using modern contraceptives. One explanation for this could be that women who have already had two or more children are more likely to want to use modern contraceptives to prevent unplanned pregnancies because they are more aware of the difficulties and responsibilities that come with raising a child. Additionally, women without children might not feel as comfortable using contraceptives because they lack pregnancy and childbirth experience. Another argument is that women with two or more children might have better access to and knowledge of contemporary contraceptives through community outreach programs or healthcare providers, while women without children might not have as many opportunities to learn about and obtain these resources.
Conclusions and recommendations
The factors that had a positive association with modern contraceptives were being married, living in an urban area, having more than two children, being in a female-headed household, having a middle-class income index, reading periodicals, listening to the radio, and not breastfeeding. However, using modern contraceptives has a negative association with being Muslim, between the ages of 35 and 39, and having a history of miscarriages. This suggests that addressing socioeconomic, geographic, and cultural hurdles may increase the efficiency of modern contraceptive use. As a result of this, the Kenyan government, along with other stakeholders, should greatly strengthen its efforts to disseminate information about the use of modern contraceptives and their importance for the health of mothers and their children. Special attention should be given to women who are in the lowest quintile of household income, live in rural areas, have a history of miscarriages, and have never attended formal education.
Strengths and limitations of this study
-
The DHS has a similar design with identical variables in a different environment; the result may, therefore, apply to other similar locations.
-
The study used a sufficiently large sample size at the national level to ensure its representativeness.
-
Recall bias is one of the potential drawbacks, especially for retrospective data based on experiences.
-
The magnitude of the bias is often unknown, and correcting for the bias is difficult.
-
Since this study was a cross-sectional study, it doesn’t show temporal relationships between independent and dependent variables.
Data availability
No datasets were generated or analysed during the current study.
References
Vu LTH, Oh J, Bui QTT, Le ATK. Use of modern contraceptives among married women in Vietnam: a multilevel analysis using the Multiple Indicator Cluster Survey (2011) and the Vietnam Population and Housing Census (2009). Glob Health Action. 2016;9(1):29574.
Organization WH. Family planning in health services: report of a WHO expert committee [meeting held in Geneva from 24 to 30 November 1970]. 1971.
Almalik M, Mosleh S, Almasarweh I. Are users of modern and traditional contraceptive methods in Jordan different? East Mediterr Heal J. 2018;24(4):377–84.
Ahissou NCA, Benova L, Delvaux T, Gryseels C, Dossou JP, Goufodji S et al. Modern contraceptive use among adolescent girls and young women in Benin: a mixed-methods study. BMJ Open [Internet]. 2022;12(1):e054188. Available from: http://bmjopen.bmj.com/content/12/1/e054188.abstract.
Lunani LL, Abaasa A, Omosa-Manyonyi G. Prevalence and Factors Associated with contraceptive use among Kenyan women aged 15–49 years. AIDS Behav. 2018;22(Suppl 1):125–30.
Booklet D. Family Planning and the 2030 Agenda for Sustainable Development (Data Booklet). Fam Plan 2030 Agenda Sustain Dev (Data Booklet). 2020.
UNDESA. World Family Planning 2017 Highlights. Econ Soc Aff [Internet]. 2017;1–43. Available from: https://www.un.org/en/development/desa/population/publications/pdf/family/WFP2017_Highlights.pdf.
Munga B, Nyanjom O, Onsomu E, Mwabu G, Kenya. Youth Employ Sub-Saharan Afr Work but Poor. 2014;303–55.
Wafula SW. Regional differences in unmet need for contraception in Kenya: insights from survey data. BMC Womens Health. 2015;15(1):1–9.
Population Reference Bureau. Kenya. Reproductive Transitions: Unmet Need for Family Planning. 2010;2009:2. Available from: http://www.prb.org/pdf14/kenya-unmet-need-contraception.pdf.
Kundu S, Kundu S, Rahman MA, Kabir H, Al Banna MH, Basu S, et al. Prevalence and determinants of contraceptive method use among Bangladeshi women of reproductive age: a multilevel multinomial analysis. BMC Public Health. 2022;22(1):2357.
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Glob Heal Sci Pract. 2016;4(2):191–210.
Ouédraogo S. Prevalence and factors associated with the use of modern contraceptive methods in the health district of Djibo, Sahel region in Burkina Faso. J Interv Epidemiol Public Heal. 2023;6(2).
Zeleke GT, Zemedu TG. Modern contraception utilization and associated factors among all women aged 15–49 in Ethiopia: evidence from the 2019 Ethiopian Mini Demographic and Health Survey. BMC Womens Health [Internet]. 2023;23(1):51. https://doi.org/10.1186/s12905-023-02203-8.
Beyene KM, Bekele SA, Abu MK. Factors affecting utilization of modern contraceptive methods among women of reproductive age in Ethiopia. PLoS ONE. 2023;18(11):e0294444.
STATISTICS KNBO. THE 2019 KENYA POPULATION AND HOUSING CENSUS RESULTS. 2019.
Survey H. Kenya. Vol. 1. 2022.
Asiimwe JB, Ndugga P, Mushomi J. With older women in Uganda. Determ Contracept Use Uganda. 2014;67(February):23–36.
Negash WD, Eshetu HB, Asmamaw DB. Predictors of modern contraceptive use among reproductive age women in high fertility countries in sub-saharan Africa: evidence from demographic and health surveys. BMC Womens Health. 2022;22(1):1–10.
Mohammed A, Woldeyohannes D, Feleke A, Megabiaw B. Determinants of modern contraceptive utilization among married women of reproductive age group in North Shoa Zone, Amhara Region, Ethiopia. Reprod Health. 2014;11:1–7.
Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Stud Fam Plann. 2014;45(2):151–69.
Boah M, Adokiya MN, Hyzam D. Prevalence and factors associated with the utilisation of modern contraceptive methods among married women of childbearing age in Yemen: a secondary analysis of national survey data. BMJ Open [Internet]. 2023;13(6):e071936. Available from: http://bmjopen.bmj.com/content/13/6/e071936.abstract.
Mankelkl G, Kinfe B. Spatial variations and multilevel mixed effect analysis on determinants factors of modern contraceptive utilization among reproductive age women in Ethiopia; proven by Ethiopian mini demographic health survey 2019. BMC Womens Health [Internet]. 2023;23(1):77. https://doi.org/10.1186/s12905-022-02030-3.
Gebre MN, Edossa ZK. Modern contraceptive utilization and associated factors among reproductive-age women in Ethiopia: evidence from 2016 Ethiopia demographic and health survey. BMC Womens Health [Internet]. 2020;20(1):61. https://doi.org/10.1186/s12905-020-00923-9.
Belachew TB, Negash WD, Asmamaw DB, Fetene SM, Addis B, Baykeda TA et al. Prevalence and predictors of post-abortion modern contraceptive utilization among reproductive age women in Ethiopia. Sci Rep [Internet]. 2023;13(1):15932. https://doi.org/10.1038/s41598-023-42911-7.
Planning F. The 2030 agenda for Sustainable Development (data booklet). New York United Nations Dep Econ Soc Aff; 2019.
Osinowo K, Ekholuenetale M, Ojomo O, Hassan A, Ladipo OA. Patterns of triggers, ideation and motivational factors of contraceptive utilization among women and gate-keepers in Nigeria: a scoping study on the resilient and accelerated scale up of DMPA-SC in Nigeria (RASUDIN). Contracept Reprod Med. 2020;5(1):1–10.
Jan M, Akhtar S. An analysis of decision-making power among married and unmarried women. Stud Home Community Sci. 2008;2(1):43–50.
Nyarko SH. Spatial variations and socioeconomic determinants of modern contraceptive use in Ghana: a bayesian multilevel analysis. PLoS ONE. 2020;15(3):e0230139.
Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 2012;380(9837):111–25.
Mushy SE, Tarimo EAM, Fredrick Massae A, Horiuchi S. Barriers to the uptake of modern family planning methods among female youth of Temeke District in Dar Es Salaam, Tanzania: a qualitative study. Sex Reprod Healthc off J Swed Assoc Midwives. 2020;24:100499.
Ramírez GR, Bravo PE, Vivaldi MIM, Manríquez IP, Pérez TG. [Adolescents’ access to contraception: perceptions of health workers in Huechuraba, Chile]. Rev Panam Salud Publica. 2017;41:e77.
Johnson OE. Determinants of modern contraceptive uptake among Nigerian women: evidence from the national demographic and health survey. Afr J Reprod Health. 2017;21(3):89–95.
Fort AL, Kothari MT, Abderrahim N. DHS Working Papers. Calvert Macro Int. 2008;1–47.
Crissman HP, Adanu RM, Harlow SD. Women’s sexual empowerment and contraceptive use in Ghana. Stud Fam Plann. 2012;43(3):201–12.
Tsegaw M, Mulat B, Shitu K. Modern contraceptive utilization and Associated factors among Married women in Liberia: evidence from the 2019 Liberia Demographic and Health Survey. Open Access J Contracept. 2022;13:17–28.
Alsaleem MA, Khalil SN, Siddiqui AF, Alzahrani MM, Alsaleem SA. Contraceptive use as limiters and spacers among women of reproductive age in southwestern, Saudi Arabia. Saudi Med J. 2018;39(11):1109.
Asresie MB, Fekadu GA, Dagnew GW. Contraceptive use among women with no fertility intention in Ethiopia. PLoS ONE. 2020;15(6):e0234474.
Nkenguye W, Ismail H, Urassa EP, Yongolo NM, Kagoye S, Msuya SE. Factors Associated with Modern Contraceptive Use among out of School adolescent girls in Majengo and Njoro Wards of Moshi Municipality, Tanzania. East Afr Heal Res J. 2023;7(1):32–9.
Jima GH, Kaso MK, Biesma-Blanco RG, Sendekie TY, Stekelenburg J. Factors associated with modern contraceptives uptake during the first year after birth in Ethiopia: A systematic review and meta-analysis. PLoS One. 2023;18(2):e0270055. https://doi.org/10.1371/journal.pone.0270055.
Asa SS, Titilayo A, Kupoluyi JA. Assessment of Contraceptive Use by Marriage Type Among Sexually Active Men in Nigeria. Int Q Community Health Educ. 2018;38(3):181–94. https://doi.org/10.1177/0272684X17749800.
Fadeyibi O, Alade M, Adebayo S, Erinfolami T, Mustapha F, Yaradua S. Household Structure and Contraceptive Use in Nigeria [Internet]. Vol. 3, Frontiers in Global Women’s Health. 2022. Available from: https://www.frontiersin.org/article/https://doi.org/10.3389/fgwh.2022.821178.
Tsehay CT. Factors associated with modern contraceptive demands satisfied among currently married/in-union women of reproductive age in Ethiopia: a multilevel analysis of the 2016 demographic and Health Survey. BMJ Open. 2022;12(2).
Ahinkorah BO. Predictors of modern contraceptive use among adolescent girls and young women in sub-saharan Africa: a mixed effects multilevel analysis of data from 29 demographic and health surveys. Contracept Reprod Med. 2020;5(1):1–12.
Ahinkorah BO, Seidu AA, Appiah F, Budu E, Adu C, Aderoju YBG, et al. Individual and community-level factors associated with modern contraceptive use among adolescent girls and young women in Mali: a mixed effects multilevel analysis of the 2018 Mali demographic and health survey. Contracept Reprod Med. 2020;5(1):1–12.
Shagaro SS, Gebabo TF, Mulugeta BT. Four out of ten married women utilized modern contraceptive method in Ethiopia: a multilevel analysis of the 2019 Ethiopia mini demographic and health survey. PLoS ONE. 2022;17(1):e0262431.
Ahinkorah BO, Budu E, Aboagye RG, Agbaglo E, Arthur-Holmes F, Adu C et al. Factors associated with modern contraceptive use among women with no fertility intention in sub-Saharan Africa: evidence from cross-sectional surveys of 29 countries. Contracept Reprod Med [Internet]. 2021;6(1):22. https://doi.org/10.1186/s40834-021-00165-6.
Ahmed M, Seid A. Association between exposure to mass media family planning messages and utilization of modern contraceptive among urban and rural youth women in Ethiopia. Int J Womens Health. 2020;719–29.
Agbadi P, Tagoe E, Akosua AF, Owusu S. A multilevel analysis of predictors of modern contraceptive use among reproductive age women in Sierra Leone: insight from demographic and Health surveys. Center for Open Science; 2019.
Jacobs J, Marino M, Edelman A, Jensen J, Darney B. Mass media exposure and modern contraceptive use among married west African adolescents. Eur J Contracept Reprod Heal Care. 2017;22(6):439–49.
Measurement L. Evaluation of the Nigerian urban reproductive health initiative (NURHI) program. Stud Fam Plann. 2017;48(3):253–68.
Ebrahim OA, Zeleke EG, Muluneh AG. Geographic variation and associated factors of long-acting contraceptive use among reproductive-age women in Ethiopia: a multi-level and spatial analysis of Ethiopian Demographic and Health Survey 2016 data. Reprod Health. 2021;18(1):122.
Berta M, Feleke A, Abate T, Worku T, Gebrecherkos T. Utilization and Associated factors of modern contraceptives during extended Postpartum Period among women who gave birth in the last 12 months in Gondar Town, Northwest Ethiopia. Ethiop J Health Sci. 2018;28(2):207–16.
Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. 2017;39.
Abera Y, Mengesha ZB, Tessema GA. Postpartum contraceptive use in Gondar town, Northwest Ethiopia: a community based cross-sectional study. BMC Womens Health. 2015;15(1):1–8.
Bwazi C, Maluwa A, Chimwaza A, Pindani M. Utilization of postpartum family planning services between six and twelve months of delivery at Ntchisi District Hospital, Malawi. Health (Irvine Calif). 2014;2014.
Belachew TB, Negash WD, Bitew DA, Asmamaw DB. Modern contraceptive utilisation and its associated factors among reproductive age women in high fertility regions of Ethiopia: a multilevel analysis of Ethiopia Demographic and Health Survey. BMJ Open. 2023;13(2):9–11.
Palamuleni ME, Adebowale AS. Women empowerment and the current use of long acting and permanent contraceptive: evidence from 2010 Malawi demographic and Health Survey. Malawi Med J. 2014;26(3):63–70.
Oumer M, Manaye A, Mengistu Z. Modern Contraceptive Method Utilization and Associated factors among women of Reproductive Age in Gondar City, Northwest Ethiopia. Open Access J Contracept. 2020;11:53–67.
Acknowledgements
The authors would like to thank Measure of the DHS for their permission to access the Kenyan demographic and health survey 2022 datasets.
Funding
For this study, the authors did not receive any financial support.
Author information
Authors and Affiliations
Contributions
G.M.,A.B.K..and B.K. Worked on this study from start to finish, including design, data extraction, and data cleaning and coding, data analysis and interpretation, and composing and revising the manuscript. B.K. then completed the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethical clearance and consent to participate
No applicable.
Consent for publication
No applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mankelkl, G., Kassaw, A.B. & Kinfe, B. Factors associated with modern contraceptive utilization among reproductive age women in Kenya; evidenced by the 2022 Kenyan demographic and health survey. Contracept Reprod Med 9, 10 (2024). https://doi.org/10.1186/s40834-024-00271-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-024-00271-1