Abstract
Background
It is unknown whether knee flexor strength recovers after anterior cruciate ligament (ACL) reconstruction with a hamstring tendon (HT) autograft and whether persistent knee flexor strength asymmetry is associated to a second ACL injury.
Objective
We aimed to systematically review (1) whether knee flexor strength recovers after ACL reconstruction with HT autografts, and (2) whether it influences the association with a second ACL injury. A third aim was to summarize the methodology used to assess knee flexor strength.
Design
Systematic review and meta-analysis reported according to PRISMA.
Methods
A systematic search was performed using the Cochrane Library, Embase, Medline, PEDRo, and AMED databases from inception to December 2021 and until completion in January 2023. Human clinical trials written in English and conducted as randomized controlled trials, longitudinal cohort, cross-sectional, and case–control studies on patients with index ACL reconstructions with HT autografts harvested from the ipsilateral side were considered. Knee flexor strength was measured isokinetically in both the reconstructed and uninjured limb to enable the calculation of the limb symmetry index (LSI). The Risk of Bias Assessment Tool for Non-Randomized Studies was used to assess risk of bias for non-randomized studies and the revised Cochrane Risk of Bias tool was used for randomized controlled trials. For the meta-analysis, the LSI (mean ± standard error) for concentric knee flexor strength at angular velocities of 60°/second (s) and 180°/s preoperatively and at 3 months, 6 months, 12 months, and 24 months were pooled as weighted means with standard errors.
Results
The search yielded 64 studies with a total of 8378 patients, which were included for the assessment of recovery of knee flexor strength LSI, and a total of 610 patients from four studies that investigated the association between knee flexor strength and second ACL injuries. At 1 year after ACL reconstruction, the knee flexor strength LSI had recovered to 89.0% (95% CI 87.3; 90.7%) and 88.3% (95% CI 85.5; 91.1%) for the velocities of 60°/s and 180°/s, respectively. At 2 years, the LSI was 91.7% (95% CI 90.8; 92.6%) and 91.2% (95% CI 88.1; 94.2%), for velocities of 60°/s and 180°/s, respectively. For the association between knee flexor strength and second ACL injuries, there was insufficient and contradictory data.
Conclusions
There was low to very low certainty of evidence indicating that the recovery of knee flexor strength LSI, defined as ≥ 90% of the uninjured side, takes up to 2 years after ACL reconstruction with HT autografts. Whether knee flexor strength deficits influence the association of second ACL injuries is still uncertain. There was considerable heterogeneity in the methodology used for knee flexor strength assessment, which together with the low to very low certainty of evidence, warrants further caution in the interpretation of our results.
Registration number: CRD42022286773.
Key Points
-
Achieving knee flexor strength limb symmetry requires up to 2 years in patients who have undergone ACL reconstruction with a HT autograft.
-
The association between knee flexor strength asymmetry and the occurrence of second ACL injuries is largely unknown due to insufficient and contradictory data.
-
There is great heterogeneity and a lack of reporting of the methodology when assessing knee flexor strength after ACL reconstruction.
Similar content being viewed by others
Background
Recovering muscle strength in the knee extensors and flexors after anterior cruciate ligament (ACL) reconstruction is considered important as it helps to increase the likelihood of returning to knee-demanding activities [1, 2]. The knee extensors provide shock absorption and are responsible for controlling knee flexion, while the knee flexors are thought to limit excessive anterior tibial translation and provide rotational stability of the knee joint [3]. Consequently, the recovery of knee extension and flexion strength is regarded as a cornerstone during the rehabilitation process after an ACL injury, where the strength relative to the uninjured side expressed as a percentage [limb symmetry index (LSI)] is commonly used as guidance [4]. An expert consensus statement suggested a cut-off value of ≥ 90% in the LSI for the knee extensors and flexors as a proxy for a “successful” outcome [4]. While achieving an LSI of ≥ 90% for knee extension strength might reduce the risk of a second ACL injury after returning to sports [5,6,7], the question of whether a similar relationship exists for knee flexor strength has not been well studied.
A standardized assessment of knee flexor strength after ACL reconstruction is the first step in investigating the possible relevance of knee flexor strength symmetry for secondary ACL injuries. The knee flexors are a biarticular muscle group with functions over both the hip and the knee joints, which influence the interpretation of knee flexor strength assessments [8]. There are several aspects to consider with regard to the measurement of knee flexor strength, e.g., knee flexor peak torque has been reported to be lower at greater angles of knee flexion [9] and at more extended hip angles, such as in a prone or a supine position compared with a seated position [10,11,12]. Knee flexor strength may also be affected by the choice of autograft, with hamstring tendon (HT) autografts causing greater knee flexor strength deficits than both patellar tendon autografts and quadriceps tendon autografts [13, 14].
Collectively, knee flexor strength results are influenced by both the methodology for measuring knee flexor strength and the choice of autograft. In addition, there is a lack of knowledge relating to the role played by knee flexor strength for second ACL injuries.
The aim of this systematic review was therefore to summarize the available evidence regarding (1) the recovery of knee flexor strength, (2) the association between knee flexor strength and second ACL injuries, and (3) the methodology used when assessing knee flexor strength in patients after ACL reconstruction treated with an HT autograft.
Methods
The Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement [15] was followed when reporting the present systematic review. This review was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration ID CRD42022286773.
Eligibility Criteria
The eligibility criteria were as follows: (1) studies written in English; (2) original clinical human studies designed as randomized controlled trials (RCT), prospective or retrospective longitudinal cohort studies, cross-sectional studies, and case–control studies; (3) studies presenting data on the LSI (mean ± standard deviation) for isokinetically measured knee flexor strength; and (4) studies investigating index ACL reconstructions with HT autografts harvested from the ipsilateral side. For the second aim, we included studies presenting data on knee flexor strength before second ACL injuries, after index ACL reconstruction with an HT autograft harvested from the ipsilateral side. Studies were excluded if (1) the entire population was < 16 years old, due to strength differences between the pediatric and adult populations [16]; (2) they solely investigated the effects of passive treatment (e.g., immobilization) or femoral nerve blockade on knee flexor strength, which could act as a confounding factor; (3) separate data for HT grafts could not be extracted due to reporting together with other graft types; and (4) the full text was not accessible. Furthermore, studies presenting LSI data for subgroups such as anterior knee pain and the incomplete regeneration of the HT were excluded, as well as literature reviews, systematic reviews, meta-analyses, case studies, conference abstracts, chapters from textbooks, opinion pieces, and editorials.
Information Sources and Search Strategy
The literature search was performed by a medical librarian with expertise in electronic searches at the Biomedical Library at the University of Gothenburg, Gothenburg, Sweden. A systematic search was performed in December 2021 and a second search for the second aim in January 2022 using the Cochrane Library, Embase, Medline, PEDRo, and AMED databases. An updated systematic search was performed in January 2023 to include any recently published studies. A similar search strategy was used with adaptation to each database configuration (Additional file 1: The Search Strategy, Online resources 1–3). The search combined the use of medical subject headings (MeSH) with free-text terms including ACL, ACL reconstruction, semitendinosus, hamstring tendon autograft, harvest, knee flexor strength, muscle strength assessment, second ACL injury, subsequent, second, and synonyms. In addition, the reference lists of the included studies were screened for potential studies not previously identified.
Selection Process
Two authors (JH and JL) independently reviewed all the titles and abstracts to determine eligibility. Studies deemed as eligible were then read in full text before potential inclusion. Any disagreement between the two authors was resolved by a discussion with the senior author (EHS). Data consisting of title, author, year of publication, journal, study type, purpose, conclusion, sample size, patient sex, patient age, sport, activity level, graft type, patients lost to follow-up, test equipment, contraction mode, test position, knee angle, angular velocity, timepoint of assessment after ACL reconstruction, relative strength and/or absolute strength, time of return to sport (RTS), time of injury after RTS, ipsilateral ACL injuries, contralateral ACL injuries, and other injuries were extracted into Excel (version 16; Microsoft Corporation, Redmond, Washington, USA).
Data Items
The primary outcome of interest was the recovery of knee flexor strength presented as the LSI. We used the recommended cut-off value of ≥ 90% in the LSI to be considered as “recovered” [4]. The second outcome was the possible association between knee flexor strength and second ACL injuries after ACL reconstruction with an HT autograft. The third outcome of interest was the methodology used to measure knee flexor strength, including test apparatus, type of muscle contraction, range of motion, angular velocity, the number of repetitions, rest between attempts, and when the testing was performed in relation to ACL reconstruction.
Risk of Bias Assessment
Two authors (JH and RP) independently graded the risk of bias of all included studies. To grade the risk of bias for non-randomized studies, the Risk of Bias Assessment Tool for Non-Randomized Studies (RoBANS) was used [17]. Six domains constitute the RoBANS assessment tool: (1) patient selection, (2) confounding variables, (3) measurement of exposure, (4) blinding of the outcome assessments, (5) incomplete outcome data, and (6) selective outcome reporting. Each domain is evaluated and rated as either low risk of bias, unclear risk of bias, or high risk of bias [17]. In the event of disagreement between the two authors (JH and RP), a consensus discussion was held with the senior author (EHS).
To grade the risk of bias for RCTs, the revised version of the Cochrane Risk of Bias tool (RoB (2) was used [18]. The RoB 2 consists of the following domains: (1) risk of bias arising from the randomization process, (2) risk of bias due to deviations from the intended intervention, (3) missing outcome data, (4) risk of bias in the measurement of the outcome, and (5) risk of bias in the selection of the reported result. Each domain includes signal questions with the following responses: “yes,” “probably yes,” “probably no,” “no,” and “no information,” which is summarized to produce a collected risk of bias within each domain. In the end, a summary of the risk of bias for each domain leads to an overall risk of bias for the respective study. Risk of bias was interpreted as follows: (1) low risk of bias if all the domains were judged as low risk of bias, (2) some concerns if no domain was judged as high risk and at least one domain was judged as some concerns, and (3) high risk of bias if at least one domain was judged as high risk of bias or if the study was judged to have some concerns in multiple domains that substantially lowered confidence in the result [19].
Data Synthesis
To perform the meta-analysis, the LSI (mean ± standard error) from studies that had reported data on knee flexor strength at the angular velocities of 60°/seconds (s) and 180°/s in preoperative tests and at 3 months, 6 months, 12 months, and 24 months postoperatively were pooled as weighted means with standard errors in forest plots separated by the angular velocity of 60°/s and 180°/s created in MedCalc (MedCalc Software Ltd, Ostend, Belgium). The standard error was calculated from the standard deviation and sample size using Microsoft Excel. A confidence interval of 95% was used. The angular velocities of 60°/s and 180°/s, and the preoperative, and 3-month, 6-month, 12-month, and 24-month postoperative timepoints were chosen, as they were most frequently used and consequently yielded more data for pooling. Other velocities and/or other timepoints for assessment were summarized in tables and presented as the LSI (mean + standard deviations).
Assessments ± 1 month of individual follow-ups (3 months, 6 months, 12 months, and 24 months) were included. If studies presented the follow-up time in days, the number of days was divided by 30 to approximate the time in months. If studies presented the follow-up time in years, the number of years was divided by 12 to approximate the time in months. For the sake of homogeneity, the eccentric contraction strength results were not included in the meta-analysis but summarized in tables. Due to high estimated clinical heterogeneity in study design, population, and outcomes, a random effect model was used in the meta-analysis [20]. When performing the meta-analysis, the statistical heterogeneity was calculated and assessed according to the I2-index with the following reference values: 0–24.9% = no heterogeneity, 25–49.9% = low heterogeneity, 50–74.9% = moderate heterogeneity, and 75–100% = high heterogeneity [20]. To present the association between knee flexor strength and second ACL injuries, and for the methodology of measuring knee flexor strength, a qualitative synthesis methodology was used due to clinical heterogeneity and limited data [21]. First, study characteristics including authors, publication year, population size and age, type of graft, and time of follow-up were summarized in tables. Second, the results of knee flexor strength and second ACL injury were summarized. Finally, for the third aim, the methodology to assess knee flexor strength was summarized in tables to explore whether a consistent theme in methodology might emerge. In the event of missing data in the included studies, an email was sent to the corresponding author.
Certainty of Evidence Assessment
The Grading of Recommendations Assessment Development and Evaluation (GRADE) working group methodology was applied for assessing certainty of evidence for the outcomes studied [22]. The assessment of certainty of evidence started with evaluating the study designs of included studies for the outcome of interest. Certainty of evidence was defined as “high” for RCTs or non-randomized controlled trials, and “low” for observational studies. In the case of merged study designs for the outcome studied, the certainty of evidence was rated as “low.” Following the assessment of study designs, the certainty of evidence could be downgraded (one or two levels, e.g., from high to moderate or high to low) on the basis of:
- (A)
-
(B)
Inconsistency assessed by the heterogeneity measured by the I2-index.
-
(C)
Indirectness by evaluating the generalizability of our results by considering differences in study populations, knee flexor strength assessment methodology, and outcome measures.
-
(D)
Imprecision assessed by the 95% confidence interval range for the pooled outcome and the sample size of included studies for the respective outcome.
-
(E)
Risk of publication bias assessed by a funnel plot.
Finally, on the basis of the assessment above, the certainty of evidence was rated as high, moderate, low, or very low.
Results
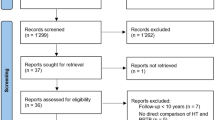
The initial search generated 3606 studies and the second 2021 studies, of which 1747 and 591, respectively, were duplicates. The updated search generated 5073 studies, of which 3944 were duplicates. All the studies were uploaded to the Rayyan QCRI web application for a systematic review for the selection process [23]. The initial search was screened by title and abstract and 254 studies were read in full text, of which 53 studies were included to assess the recovery of knee flexor strength symmetry, while 2 studies were included to assess the association between knee flexor strength and subsequent ACL injuries from the two first searches. The updated search resulted in 11 new studies to assess the recovery of knee flexor strength symmetry and 2 studies to assess the association between knee flexor strength and subsequent ACL injuries. Figure 1 illustrates the selection process.
Recovery of Knee Flexor Strength Symmetry
In total, 8378 patients in the 64 studies were included to assess the recovery of knee flexor strength symmetry. For an overview of study characteristics, see Table 1.
Risk of Bias Assessment for Knee Flexor Strength Recovery
Of the 64 studies included, 51 (80%) studies were non-randomized and 13 (20%) were RCTs. Of the non-randomized studies, addressing confounding variables and selective outcome reporting were the items with greatest risk of bias (Table 2). Of the 13 RCTs assessed with the Cochrane RoB 2 tool, one study was regarded as having a low risk of bias [59], seven as having some concerns [27, 37, 40, 44, 45, 55, 79], and five as having a high risk of bias [24, 29, 48, 56, 68]. The selection of the reported result was the item with greatest risk of bias (Table 3).
Recovery of LSI for Knee Flexor Strength
There were 36 studies that assessed knee flexor strength symmetry isokinetically with an angular velocity of 60°/s [24, 25, 28, 30, 40,41,42,43,44, 47, 50,51,52, 55, 57, 59, 60, 62, 64, 65, 69,70,71, 73,74,75,76, 78, 79, 81,82,83, 85,86,87,88] and 21 studies with an angular velocity of 180°/s [28,29,30, 38, 41, 42, 44, 52, 59,60,61,62, 65, 70, 75, 76, 78,79,80, 88]. For 60°/s, the LSI calculated as the weighted mean with standard error was 80.8% ± 2.5% (95% CI 75.9; 85.7%, I2 = 89.5%) preoperatively, 81.7% ± 2.8% (95% CI 76.2; 87.2%, I2 = 95.4%) at 3 months, 88.6% ± 2.0% (95% CI 84.6; 92.6%, I2 = 93.3%) at 6 months, 89.0% ± 0.9% (95% CI 87.3; 90.7%, I2 = 66.2%) at 12 months, and 91.7% ± 0.5% (95% CI 90.8; 92.6%, I2 = 5.4%) at 24 months. The certainty of evidence assessed with the GRADE was very low for all timepoints of assessment except for the 24-month follow-up, of which the certainty of evidence was regarded as low. The inclusion of different study designs, risk of bias, and moderate-to-high statistical heterogeneity lowered the certainty of evidence.
For 180°/s, the LSI calculated as the weighted mean with standard error was 75.6% ± 9.8% (95% CI 56.4; 94.8%, I2 = 97.6%) preoperatively, 88.8% ± 1.4% (95% CI 86.2; 91.5%, I2 = 58.4%) at 3 months, 91.3% ± 1.9% (95% CI 87.5; 95.1%, I2 = 94.7%) at 6 months, 88.3% ± 1.4% (95% CI 85.5; 91.1%, I2 = 80.3%) at 12 months, and 91.2% ± 1.5% (95% CI 88.1; 94.2%, I2 = 82.6%) at 24 months (Figs. 2, 3, 4, 5, 6). The certainty of evidence assessed with the GRADE was very low for all timepoints of assessment. The inclusion of different study designs, risk of bias, and moderate-to-high statistical heterogeneity lowered the certainty of evidence.
The recovery of knee flexor strength symmetry presented as the limb symmetry index (LSI) preoperatively. The LSI mean value is presented with the standard error and a 95% confidence interval using a random effect model. A limb symmetry index of 90% is represented by the black line. Knee flexor strength at 60°/second was 80.8% ± 2.5% (95% CI 75.9; 85.7%, I2 = 89.5%) and at 180°/second 75.6% ± 9.8% (95% CI 56.4; 94.8%, I2 = 97.6%). Baba et al. 2019 A [25] = Surgery < 1 months; Baba et al. 2019 B [25] = Surgery 1–3 months; Baba et al. 2019 C [25] = Surgery > 3 months; Harilainen et al. 2005 A [44] = Transfix; Harilainen et al. 2005 B [44] = Interference screw; Suh et al. 2021 A [80] = Dominant leg; Suh et al. 2021 B [80] = Non-dominant leg; Tsuda et al. 2009 A [85] = Women; Tsuda et al. 2009 B [85] = Men
The recovery of knee flexor strength symmetry presented as the limb symmetry index (LSI) at 3 months. The LSI mean value is presented with the standard error and a 95% confidence interval using a random effect model. A limb symmetry index of 90% is represented by the black line. Knee flexor strength at 60°/second was 81.7% ± 2.8% (95% CI 76.2; 87.2%, I2 = 95.4%) and at 180°/second 88.8% ± 1.4% (95% CI 86.2; 91.5%, I2 = 58.4%). Iriuchishima et al. 2010 A [51] = Standard rehabilitation; Iriuchishima et al. 2010 B [51] = Accelerated rehabilitation; Koutras et al. 2013 A [60] = Anteromedial portal; Koutras et al. 2013 B [60] = Transtibial portal; Sengoku et al. 2022 A [77] = Semitendinosus alone; Sengoku et al. 2022 B [77] = Semitendinosus + gracilis; Tsuda et al. 2009 A [85] = Women; Tsuda et al. 2009 B [85] = Men
The recovery of knee flexor strength symmetry presented as the limb symmetry index (LSI) at 6 months. The LSI mean value is presented with the standard error and a 95% confidence interval using a random effect model. A limb symmetry index of 90% is represented by the black line. Knee flexor strength at 60°/second was 89.0% ± 0.9% (95% CI 87.3; 90.7%, I2 = 66.2%) and at 180°/second 91.3% ± 1.9% (95% CI 87.5; 95.1%, I2 = 94.7%). Carter and Edinger 1999 A [29] = Semitendinosus alone; Carter and Edinger 1999 B [29] = Semitendinosus + gracilis; Iriuchishima et al. 2010 A [51] = Standard rehabilitation; Iriuchishima et al. 2010 B [51] = Accelerated rehabilitation; Królikowska et al. 2019 A [62] = Supervised < 6 months; Królikowska et al. 2019 B [62] = Supervised > 6 months; Koutras et al. 2013 A [60] = Anteromedial portal; Koutras et al. 2013 B [60] = Transtibial portal; Sengoku et al. 2022 A [77] = Semitendinosus alone; Sengoku et al. 2022 B [77] = Semitendinosus + gracilis; Severyns et al. 2022 A [78] = No graft failure; Severyns et al. 2022 B [78] = Graft failure; Suh et al. 2021 A [80] = Dominant leg; Suh et al. 2021 B [80] = Non-dominant leg; Tsuda et al. 2009 A [85] = Women; Tsuda et al. 2009 B [85] = Men
The recovery of knee flexor strength symmetry presented as the limb symmetry index (LSI) at 12 months. The LSI mean value is presented with the standard error and a 95% confidence interval using a random effect model. A limb symmetry index of 90% is represented by the black line. Knee flexor strength at 60°/second was 89.0% ± 0.9% (95% CI 87.3; 90.7%, I2 = 66.2%) and at 180°/second 88.3% ± 1.4% (95% CI 85.5; 91.1%, I2 = 80.3%). Araki et al. 2011 A = Single-bundle; Araki et al. 2011 B; Double-bundle; Harilainen et al. 2005 A [44] = Transfix; Harilainen et al. 2005 B [44] = Interference crew; Suh et al. 2021 A [80] = Dominant leg; Suh et al. 2021 B [80] = Non-dominant leg; Tsuda et al. 2009 A [85] = Women; Tsuda et al. 2009 B [85] = Men
The recovery of knee flexor strength symmetry presented as the limb symmetry index (LSI) at 24 months. The LSI mean value is presented with the standard error and a 95% confidence interval using a random effect model. A limb symmetry index of 90% is represented by the black line. Knee flexor strength at 60°/second was 91.7% ± 0.5% (95% CI 90.8; 92.6%, I2 = 5.4%) and at 180°/second 91.2% ± 1.5% (95% CI 88.1; 94.2%, I2 = 82.6%). Baba et al. 2019 [25] A = Surgery < 1 month, Baba et al. 2019 B [25] = Surgery 1–3 months; Baba et al. 2019 C [25] = Surgery > 3 months; Gifstad et al. 2013 A [40] = Ezloc; Gifstad et al. 2013 B [40] = Bone mulch; Hamada et al. 2001 A [42] = Single-socket; Hamada et al. 2001 B [42] = Bi-socket; Harilainen et al. 2005 A [44] = Transfix; Harilainen et al. 2005 B [44] = Interference screw; Inagaki et al. 2013 A [50] = Semitendinosus alone; Inagaki et al. 2013 B [50] = Semitendinosus + gracilis; Koga et al. 2015 A [55] = 0°; Koga et al. 2015 B [55] = 20°; Koga et al. 2015 A [55] = 45°; Kondo et al. 2012 A [57] = Endobutton-CL; Kondo et al. 2012 B [57] = Endobuttion-CL-BTB; Kouloumentas et al. 2019 A [59] = Semitendinosus alone; Kouloumentas et al. 2019 B [59] = Semitendinosus + gracilis; Nakamura et al. 2002 A [70] = Semitendinosus alone; Nakamura et al. 2002 B [70] = Semitendinosus + gracilis; Nishio et al. 2018 A [71] = > 40 years; Nishio et al. 2018 B [71] = < 40 years
Furthermore, 14 studies presented data for knee flexor strength symmetry at 90°/s, 240°/s, or 300°/s instead of 60°/s or 180°/s [27, 29, 33,34,35,36,37, 46, 48, 49, 54, 66, 72, 87], while 2 studies used three velocities (60°/s, 90°/s, and 180°/s) and did not explicitly report whether the results, as a mean LSI, were an average based on all three velocities or the result of a specific velocity [31, 32]. A total of 18 studies presented data at different follow-ups (ranging from 6 to 168 ± 52.8 months) than preoperatively and at 3 months, 6 months, 12 months, and 24 months [26, 27, 35, 39, 45, 48, 51, 53, 56, 58, 62, 63, 67, 68, 72, 75, 84, 85]. Studies presenting data for knee flexor strength symmetry as the LSI at velocities other than 60°/s and 180°/s and at timepoints other than preoperatively and 3 months, 6 months, 12 months, and 24 months postoperatively are presented in Additional file 2: Complementary Result Tables, Table S1.
Knee Flexor Strength and Second ACL Injuries
In total, there were 610 patients in four studies investigating the association between knee flexor strength and second ACL injuries (Table 4). All the studies compared knee flexor strength in patients who sustained a second ACL injury with those who did not. In addition, Yamanashi et al. [89] performed a covariance structure analysis and presented low negative covariance values of −0.09 for the hamstring-to-quadriceps ratio at 3 months and −0.1 at 6 months. Collectively, there was insufficient and contradictory data to allow firm conclusions to be drawn in terms of the association between knee flexor strength and second ACL injuries.
Risk of Bias Assessment for Studies Investigating Knee Flexor Strength and Second ACL Injuries
The studies included in the analysis of the association between knee flexor strength and second ACL injuries consisted of one case series [83], two retrospective cohort studies [78, 89], and one case–control study [28]. Incomplete outcome data and selective outcome reporting were the items with greatest risk of bias (Table 5).
Association Between Knee Flexor Strength and Second ACL Injuries
A total of 72 second ACL injuries were reported across the four included studies, of which 63 were ipsilateral and 9 contralateral [28, 78, 83, 89]. The studies presented data for knee flexor strength for the ACL re-injured group ranged from 3 months [89] to 12 months postoperatively [28] (Table 6).
Methodology for Measuring Knee Flexor Strength
To assess knee flexor strength, 22 studies used a Cybex dynamometer [25, 29, 31, 32, 42, 47, 48, 51, 54,55,56,57,58, 65, 67, 68, 70, 71, 82, 83, 85, 87], 19 used a Biodex dynamometer [24, 26, 27, 40, 41, 43, 49, 59, 64, 66, 69, 72, 75, 80, 81, 84, 88,89,90], 9 used a HUMAC dynamometer [28, 30, 52, 61, 62, 73, 74, 76, 79], 4 used an IsoSport dynamometer [34,35,36,37], 3 used a Lido Multijoint dynamometer [44, 45, 63], 2 used a Genu Plus dynamometer [38, 86], 2 used a Con-Trex dynamometer [39, 78], 1 used a Kin-Com dynamometer [50], 1 used an Orthrotron [53], and 1 study did not report the test equipment that was used [60]. A total of 23 studies specified the contraction mode, with 21 studies using a concentric contraction [27, 34, 36, 39, 41, 49, 52, 54, 61,62,63,64, 66, 72, 73, 76, 80, 82, 84, 85, 89], 2 studies investigating both concentric and eccentric contractions [46, 79], and 42 studies not specifying the contraction mode [24,25,26, 28,29,30,31,32,33, 35, 37, 38, 40, 43,44,45, 47, 50, 51, 53, 55,56,57,58,59,60, 65, 67,68,69,70,71, 74, 75, 78, 81, 83, 86,87,88]. Regarding the position at the time of testing, 22 studies specified the test position as a seated position [26,27,28,29,30, 36, 41, 46, 49, 51, 52, 61,62,63,64, 72,73,74, 76, 78, 80, 84], 2 studies used a supine position [27, 72], and 43 studies did not specify the position [24, 25, 31,32,33,34,35, 37,38,39,40, 42,43,44,45, 47, 48, 50, 53,54,55,56,57,58,59,60, 65,66,67,68,69,70,71, 75, 79, 81,82,83, 85,86,87,88,89].
Collectively, the methods of knee flexor strength assessment appear to vary substantially. Further information regarding the methodology for measuring knee flexor strength is summarized in Additional file 2: Complementary Result Tables, Table S2 for studies assessing the recovery of knee flexor strength, and in Additional file 2: Complementary Result Tables, Table S3 for studies assessing the association between knee flexor strength and second ACL injuries.
Discussion
The main finding of this systematic review and meta-analysis was, based on very low to low certainty of evidence, an incomplete recovery of knee flexor strength symmetry for up to a year after ACL reconstruction with an HT autograft, with regard to the 90% LSI reference cut-off value to be classified as “recovered.” The isokinetic knee flexor strength LSI then appears to be recovered at 2 years after ACL reconstruction at both 60°/s and 180°/s of angular velocity. Despite knee flexor strength asymmetry persisting as late as 1 year after ACL reconstruction, it is still unknown whether knee flexor strength asymmetry affects the occurrence of a second ACL injury, as there was a general lack of data on the association between knee flexor strength and second ACL injuries. In addition to the lack of reported second ACL injuries, the heterogeneity in the methodology used to measure knee flexor strength after ACL reconstruction with HT autografts presents a problem for scientists and clinicians alike. Given the fairly well-accepted role of the knee flexors as synergists to the ACL, the need to bridge this evidence gap is apparent.
Knee Flexor Strength Recovery
In our systematic review and meta-analysis, we used the commonly recommended cut-off value of ≥ 90% in LSI for an individual to be classified as “recovered.” At 1 year after ACL reconstruction, the average LSI for concentric knee flexor strength at an angular velocity of 60°/s was 89.0% ± 0.9% (95% CI 87.3; 90.7%), increasing to 91.7% ± 0.5% (95% CI 90.8; 92.6%) at 2 years. However, while the recovery of knee flexor strength at 1 year was regarded as “incomplete” and at 2 years as “complete,” the clinical relevance of the difference between 89.0% and 91.7% is questionable. The knee flexor strength recovery after ACL reconstruction with an HT autograft is not well defined and the logical foundation for the recommendation of a cut-off value of ≥ 90% in LSI is not entirely clear, despite being routinely used. First, one may argue that a higher angular velocity, e.g., ≥ 180°/s, imposes a different demand for knee flexor strength than angular velocities of ≤ 60°/s. Undheim et al. [91] reported that torque output increases when angular velocities decrease and thus, to assess maximum strength, angular velocities of ≤ 60°/s were recommended. On the contrary, the differences between 60°/s and 180°/s for up to 2 years after ACL reconstruction were very small and can hardly be considered clinically relevant. Furthermore, the recommendation of ≥ 90% in the LSI for knee flexor strength after ACL reconstruction does not take into account the persistent graft differences in donor-site morbidity. Harvesting the semitendinosus tendon alone or in combination with the gracilis will likely result in a change in morphological properties upon regeneration, and the tendon often inserts more proximally compared with preoperatively [92]. The altered structure of the semitendinosus muscle and tendon will in turn influence the mechanical properties and consequently influence the assessment of knee flexor strength, e.g., with larger knee flexor deficits at more extended hip angles and deeper knee angles [12]. It has been suggested that the biceps femoris long and short head, as well as the semimembranosus, may compensate for the semitendinosus during knee flexor strength assessments [93]. Hence, it can be argued that the LSI cut-off value for knee flexor strength should be even higher in patients with HT autografts, with the changes in the morphological and mechanical properties of the semitendinosus in mind. Importantly, we found that a persisting knee flexor strength deficit defined as < 90% LSI at 1 year has the potential to recover beyond 1 year after ACL reconstruction with HT autograft. Patients with a persistent knee flexor strength deficit between 12 months and 24 months after ACL reconstruction can increase their strength significantly with progressive strength training [94]. Additionally, patients randomized to an accelerated rehabilitation protocol may recover their knee flexor strength symmetry (≥ 90% LSI) as early as 6 months postoperatively without adverse events [37]. Taken together, these considerations suggest there might be an underloading issue in patients with ACL reconstruction treated with HT autograft resulting in persisting knee flexor strength asymmetry. Consequently, on the basis of our findings and the literature, earlier introduction and with a progressive increase in knee flexor strength demands are advocated to resolve the impairments in knee flexor strength after ACL reconstruction with HT autografts.
Knee Flexor Strength and Second ACL Injuries
A safe return to sport or a return to knee-strenuous activity and minimizing the risk of a second ACL injury are the ultimate aims of clinicians with each unique patient. Recovering ≥ 90% in the LSI is frequently used as part of the assessment criteria prior to returning to sports or knee-strenuous activities [7]. While it appears logical that recovering knee flexor strength LSI to ≥ 90% would be protective, as the knee flexors act as synergists to the ACL, only 4 of 4418 unique identified studies reported knee flexor strength separately for patients who sustained a second ACL injury [28, 78, 83, 89]. Moreover, although several studies that reported second ACL injuries were identified, these studies unfortunately excluded patients who sustained second ACL injuries from the knee flexor strength assessments during the study process, contributing to the limited available data regarding the possible protective role of knee flexor strength in relation to second ACL injuries [75, 95,96,97,98]. Interestingly, in a cohort of 210 patients after ACL reconstruction with an HT autograft, Blucher et al. [28] reported that only 45–47% managed to pass ≥ 90% in LSI for knee flexor strength at 1 year assessed isokinetically at both angular velocities of 60°/s and 180°/s. However, there was no significant difference in LSI for knee flexor strength between patients who sustained a second ACL and those who did not (92–94% versus 90–92%, respectively) [28]. In contrast, Severyns et al. [78] reported a significantly lower LSI for knee flexor strength in patients who would go on to sustain a second ACL injury at 6 months compared with patients who did not (71.6% ± 10.9% versus 95.0% ± 17.5%) in a cohort of 104 patients. Collectively, there is a remarkable lack of data regarding the proposed role of strong knee flexors in reducing the risk of second ACL injuries. It is therefore yet to be determined whether passing the cut-off value of ≥ 90% in the LSI for knee flexor strength is important when it comes to reducing second ACL injuries.
One of the included studies presented a significantly reduced hamstring-to-quadriceps strength ratio at 3 months and 6 months for patients who sustained an ipsilateral ACL injury compared with patients who did not sustain a second ACL injury [89]. A lower hamstring-to-quadriceps strength ratio has previously been reported as a risk factor for a primary ACL injury in females [99] and for a second ACL injury among both patellar tendon and HT autografts [6]. Consequently, the relationship between the knee extensors and the flexors may be of greater importance in reducing the risk of second ACL injuries than striving to achieve ≥ 90% LSI knee flexor strength. However, the way we should measure knee flexor strength and how strong the knee flexors should be in relation to the knee extensors to reduce second ACL injuries are other as yet unanswered questions. In addition, whether the hamstring-to-quadriceps ratio and/or knee flexor strength symmetry are important in reducing the risk of second ACL injuries is currently also unclear, due to the general lack of data.
Knee Flexor Strength Measurement Methodology
There was both great heterogeneity and a general lack of detail in the methodology for measuring knee flexor strength, with only 34% of the included studies specifying which position was used for assessing knee flexor strength. This is a matter of concern, as hip position will affect the peak torque of the reconstructed limb after ACL reconstruction with an HT autograft, with a more extended hip position leading to greater knee flexor strength deficits compared with a more flexed position [12]. Consequently, the fact that so many studies did not specify the test position induces some degree of uncertainty in the interpretation of knee flexor strength symmetry values in the present systematic review and meta-analysis. In addition, there was a lack of reporting of the type of muscle contraction, range of motion, number of repetitions, and rest between each set when there was more than one set. Worryingly, 8 years ago, Undheim et al. [91] reported that there was no standardized isokinetic protocol for measuring strength after ACL reconstruction, which still appears to be the case.
Limitations
Firstly, our choice to summarize studies with knee flexor strength assessments with the velocities of 60°/s and 180°/s in a forest plot was made as they were the most frequently used velocities and consequently enabled more studies to be included in the meta-analysis. However, the sample sizes for the included studies in the meta-analysis were small in overall terms, ranging from 10 to 281 individuals. The exclusion of studies with languages other than English, and which used other velocities in the pooling of data involved studies with larger sample sizes than the included studies, e.g., Cristiani et al. [33] with 3788 individuals, thereby missing important information on knee flexor strength recovery. Secondly, the inclusion of different study designs together with the heterogeneity in the methodology for knee flexor strength assessment may limit the internal validity of our results. Only 35% of the included studies specified the contraction type, 34% specified the test position, and 52% specified how many repetitions the patients performed during the knee flexor strength assessment. The lack of reporting of methodology for assessing knee flexor strength not only affects the investigation of knee flexor strength recovery, but also further limits the interpretation of whether knee flexor strength influences second ACL injuries. To address the heterogeneity in methodology, statistical heterogeneity was assessed with the I2 index ranging from 58.4% to 97.6%, except for 60°/second at 24 months, with a value of 5.4%. Consequently, the overall statistical heterogeneity was high, indicating variability in the available data, which may affect the certainty of our results. Furthermore, there was a major limitation in the number of available studies to address the second study aim relating to the association between knee flexor strength and second ACL injuries. In 3 of 4 studies, the time range for assessing knee flexor strength was 3–6 months after ACL reconstruction, although the typical time frame for a return to sport is 9–12 months [100]. This means that we do not know the level of knee flexor strength at the time of a return to sport or the timepoint of the second ACL injury. Finally, the low to very low certainty of evidence assessed by GRADE warrants further caution in the interpretation of our results.
Future Research
Future research should firstly summarize the methodology used to reach a consensus on how knee flexor strength should be measured after ACL reconstruction in patients with HT autografts. After reaching a consensus, the second step should be to investigate whether knee flexor strength symmetry is an important factor for knee function and the occurrence of a second ACL injury, or whether the strength relationship between the knee extensors and flexors is a better milestone to strive for.
Conclusions
The recovery of knee flexor strength symmetry appears to take up to 2 years after ACL reconstruction using HT autograft considering ≥ 90% in LSI with a low to very low certainty of evidence. The relevance of persistent knee flexor asymmetry at 1 year in terms of the risk of second ACL injuries is not known due to limited data. Consequently, standardized assessments and more research are needed to clarify whether achieving knee flexor strength symmetry influences the occurrence of a second ACL injury.
Availability of Data and Materials
All included studies constituting the present systematic review and meta-analysis are cited in the manuscript. The dataset is available upon reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- HT:
-
Hamstring tendon
- LSI:
-
Limb symmetry index
- RoBANS:
-
Risk of bias assessment tool for non-randomized studies
- RCT:
-
Randomized controlled trial
- ROB:
-
Risk of bias
References
Keays SL, Mellifont DB, Keays AC, Stuelcken MC, Lovell DI, Sayers MGL. Long-term return to sports after anterior cruciate ligament injury: reconstruction vs no reconstruction-a comparison of 2 case series. Am J Sports Med. 2022;50(4):912–21. https://doi.org/10.1177/03635465211073152.
Diermeier T, Rothrauff BB, Engebretsen L, Lynch AD, Ayeni OR, Paterno MV, et al. Treatment after anterior cruciate ligament injury: panther symposium ACL treatment consensus group. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2390–402. https://doi.org/10.1007/s00167-020-06012-6.
Solomonow M, Baratta R, Zhou BH, Shoji H, Bose W, Beck C, et al. The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. Am J Sports Med. 1987;15(3):207–13. https://doi.org/10.1177/036354658701500302.
Lynch AD, Logerstedt DS, Grindem H, Eitzen I, Hicks GE, Axe MJ, et al. Consensus criteria for defining “successful outcome” after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49(5):335–42. https://doi.org/10.1136/bjsports-2013-092299.
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–8. https://doi.org/10.1136/bjsports-2016-096031.
Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–51. https://doi.org/10.1136/bjsports-2015-095908.
Turk R, Shah S, Chilton M, Thomas TL, Anene C, Mousad A, et al. Critical criteria recommendations: return to sport after ACL reconstruction requires evaluation of time after surgery of 8 months, >2 functional tests, psychological readiness, and quadriceps/hamstring strength. Arthrosc J Arthroscop Relat Surg. 2022. https://doi.org/10.1016/j.arthro.2022.08.038.
Yanagisawa O, Fukutani A. Muscle recruitment pattern of the hamstring muscles in hip extension and knee flexion exercises. J Hum Kinet. 2020;72:51–9. https://doi.org/10.2478/hukin-2019-0124.
Makihara Y, Nishino A, Fukubayashi T, Kanamori A. Decrease of knee flexion torque in patients with ACL reconstruction: combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):310–7. https://doi.org/10.1007/s00167-005-0701-2.
Koutras G, Bernard M, Terzidis IP, Papadopoulos P, Georgoulis A, Pappas E. Comparison of knee flexion isokinetic deficits between seated and prone positions after ACL reconstruction with hamstrings graft: Implications for rehabilitation and return to sports decisions. J Sci Med Sport. 2016;19(7):559–62. https://doi.org/10.1016/j.jsams.2015.07.018.
Elmlinger BS, Nyland JA, Tillett ED. Knee flexor function 2 years after anterior cruciate ligament reconstruction with semitendinosus-gracilis autografts. Arthroscopy. 2006;22(6):650–5. https://doi.org/10.1016/j.arthro.2006.03.010.
Ogborn D, McRae S, Larose G, Leiter J, Brown H, MacDonald P. Knee flexor strength and symmetry vary by device, body position and angle of assessment following ACL reconstruction with hamstring grafts at long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2021. https://doi.org/10.1007/s00167-021-06712-7.
Johnston PT, Feller JA, McClelland JA, Webster KE. Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2022;30(4):1300–10. https://doi.org/10.1007/s00167-021-06565-0.
Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134(10):1417–28. https://doi.org/10.1007/s00402-014-1992-x.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Dotan R, Mitchell C, Cohen R, Klentrou P, Gabriel D, Falk B. Child-adult differences in muscle activation–a review. Pediatr Exerc Sci. 2012;24(1):2–21. https://doi.org/10.1123/pes.24.1.2.
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–14. https://doi.org/10.1016/j.jclinepi.2012.09.016.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898. https://doi.org/10.1136/bmj.l4898.
Gagnier JJ, Moher D, Boon H, Beyene J, Bombardier C. Investigating clinical heterogeneity in systematic reviews: a methodologic review of guidance in the literature. BMC Med Res Methodol. 2012;12:111. https://doi.org/10.1186/1471-2288-12-111.
Schick-Makaroff K, MacDonald M, Plummer M, Burgess J, Neander W. What synthesis methodology should I use? A review and analysis of approaches to research synthesis. AIMS Publ Health. 2016;3(1):172–215. https://doi.org/10.3934/publichealth.2016.1.172.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. 2011;35(3):439–46. https://doi.org/10.1007/s00264-010-1110-9.
Baba R, Iwasaki K, Joutoku Z, Onodera T, Iwasaki N, Kondo E, et al. Impact of surgical timing on clinical outcomes in anatomic double-bundle anterior cruciate ligament reconstruction using hamstring tendon autografts. Orthop J Sports Med. 2019. https://doi.org/10.1177/2325967119880553.
Barenius B, Webster WK, McClelland J, Feller J. Hamstring tendon anterior cruciate ligament reconstruction: Does gracilis tendon harvest matter? Int Orthop. 2013;37(2):207–12. https://doi.org/10.1007/s00264-012-1672-9.
Beaudoin A, Ogborn D, McRae S, Larose G, Brown H, McCormack R, et al. No differences found in long-term outcomes of a randomized controlled trial comparing ipsilateral versus contralateral hamstring graft in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2022;30(11):3718–25. https://doi.org/10.1007/s00167-022-06980-x.
Blucher NC, Feller JA, Devitt BM, Klemm HJ, Whitehead TS, McClelland JA, et al. Is there an association in young patients between quadriceps or hamstring strength after ACL reconstruction and graft rupture? Orthop J Sports Med. 2022;10(6):23259671221101004. https://doi.org/10.1177/23259671221101003.
Carter TR, Edinger S. Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy. 1999;15(2):169–72. https://doi.org/10.1053/ar.1999.v15.0150161.
Chantrelle M, Menu P, Crenn V, Grondin J, Daley P, Louguet B, et al. Consequences of anterior knee pain after anterior cruciate ligament reconstruction: a 2015–2020 cohort study. PLoS ONE. 2023;18(1): e0280146. https://doi.org/10.1371/journal.pone.0280146.
Chen C-H, Chang C-H, Su C-I, Wang K-C, Liu H-T, Yu C-M, et al. Arthroscopic single-bundle anterior cruciate ligament reconstruction with periosteum-enveloping hamstring tendon graft: clinical outcome at 2 to 7 years. Arthrosc J Arthrosc Relat Surg. 2010;26(7):907–17. https://doi.org/10.1016/j.arthro.2009.11.011.
Chen C-H, Chen W-J, Shih C-H, Chou S-W. Arthroscopic anterior cruciate ligament reconstruction with periosteum-enveloping hamstring tendon graft. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2004;12(5):398–405.
Cristiani R, Mikkelsen C, Forssblad M, Engström B, Stålman A. Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3461–70. https://doi.org/10.1007/s00167-019-05396-4.
Ebert JR, Annear PT. ACL reconstruction using autologous hamstrings augmented with the ligament augmentation and reconstruction system provides good clinical scores, high levels of satisfaction and return to sport, and a low retear rate at 2 years. Orthop J Sports Med. 2019;7(10):2325967119879079. https://doi.org/10.1177/2325967119879079.
Ebert JR, Nairn R, Breidahl W, Annear PT. Double-bundle anterior cruciate ligament reconstruction using autologous hamstrings with LARS augmentation demonstrates comparable outcomes to hamstrings alone, without evidence of synovitis or early osteoarthritis. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2021. https://doi.org/10.1007/s00167-021-06801-7.
Ebert JR, Edwards P, Joss B, Annear P, Radic R, D’Alessandro P. Isokinetic torque analysis demonstrates deficits in knee flexor and extensor torque in patients at 9–12 months after anterior cruciate ligament reconstruction, despite peak torque symmetry. Knee. 2021;32:9–18. https://doi.org/10.1016/j.knee.2021.07.003.
Ebert JR, Edwards P, Joss B, Annear PT. A structured accelerated versus control rehabilitation pathway after anterior cruciate ligament reconstruction using autologous hamstrings demonstrates earlier improvement in physical outcomes without increasing graft laxity: a randomized controlled trial. Phys Therapy Sport Off J Assoc Chart Physiother Sports Med. 2022;55:271–81. https://doi.org/10.1016/j.ptsp.2022.05.005.
Fabbriciani C, Milano G, Mulas PD, Ziranu F, Severini G. Anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendon graft in rugby players. Knee Surg Sports Traumatol Arthrosc. 2005;13(1):2–7. https://doi.org/10.1007/s00167-004-0505-9.
Fischer F, Fink C, Hoser C, Hepperger C, Gfoller P, Herbst E, et al. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2018;26(2):418–25. https://doi.org/10.1007/s00167-017-4522-x.
Gifstad T, Sole A, Drogset JO, Strand T, Uppheim G, Grontvedt T. Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):576–83. https://doi.org/10.1007/s00167-012-1947-0.
Guney-Deniz H, Harput G, Kaya D, Nyland J, Doral MN. Quadriceps tendon autograft ACL reconstructed subjects overshoot target knee extension angle during active proprioception testing. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2020;28(2):645–52. https://doi.org/10.1007/s00167-019-05795-7.
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, et al. Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy. 2001;17(8):801–7. https://doi.org/10.1053/jars.2001.25251.
Hanada M, Yoshikura T, Matsuyama Y. Muscle recovery at 1 year after the anterior cruciate ligament reconstruction surgery is associated with preoperative and early postoperative muscular strength of the knee extension. Eur J Orthop Surg Traumatol. 2019;29(8):1759–64. https://doi.org/10.1007/s00590-019-02479-3.
Harilainen A, Sandelin J, Jansson KA. Cross-pin femoral fixation versus metal interference screw fixation in anterior cruciate ligament reconstruction with hamstring tendons: results of a controlled prospective randomized study with 2-year follow-up. Arthroscopy. 2005;21(1):25–33. https://doi.org/10.1016/j.arthro.2004.09.013.
Harilainen A, Sandelin J, Linko E. Randomized prospective study of ACL reconstruction with interference screw fixation in patellar tendon autografts versus femoral metal plate suspension and tibial post fixation in hamstring tendon autografts: 5-year clinical and radiological follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14(6):517–28. https://doi.org/10.1007/s00167-006-0059-0.
Harput G, Ozer H, Baltaci G, Richards J. Self-reported outcomes are associated with knee strength and functional symmetry in individuals who have undergone anterior cruciate ligament reconstruction with hamstring tendon autograft. Knee. 2018;25(5):757–64. https://doi.org/10.1016/j.knee.2018.06.007.
Hasebe Y, Tanabe Y, Yasuda K. Anterior-cruciate-ligament reconstruction using doubled hamstring-tendon autograft. J Sport Rehabil. 2005;14(4):279–93. https://doi.org/10.1123/jsr.14.4.279.
Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38(3):448–54.
Hogberg J, Bergentoft E, Piussi R, Wernbom M, Beischer S, Simonson R, et al. Persistent knee flexor strength deficits identified through the NordBord eccentric test not seen with “gold standard” isokinetic concentric testing during the first year after anterior cruciate ligament reconstruction with a hamstring tendon autograft. Phys Therapy Sport Off J Assoc Chart Physiother Sports Med. 2022;55:119–24. https://doi.org/10.1016/j.ptsp.2022.03.004.
Inagaki Y, Kondo E, Kitamura N, Onodera J, Yagi T, Tanaka Y, et al. Prospective clinical comparisons of semitendinosus versus semitendinosus and gracilis tendon autografts for anatomic double-bundle anterior cruciate ligament reconstruction. J Orthop Sci. 2013;18(5):754–61. https://doi.org/10.1007/s00776-013-0427-9.
Iriuchishima T, Horaguchi T, Morimoto Y, Negishi S, Kubomura T, Motojima S, et al. Intensity of physiotherapy after anterior cruciate ligament reconstruction: a comparison of two rehabilitation regimen. Arch Orthop Trauma Surg. 2010;130(8):1053–8. https://doi.org/10.1007/s00402-010-1134-z.
Johnston PT, McClelland JA, Webster KE, Feller JA. Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2021. https://doi.org/10.1007/s00167-021-06565-0.
Karlson JA, Steiner ME, Brown CH, Johnston J. Anterior cruciate ligament reconstruction using gracilis and semitendinosus tendons. Comparison of through-the-condyle and over-the-top graft placements. Am J Sports Med. 1994;22(5):659–66.
Kılınç BE, Kara A, Camur S, Oc Y, Celik H. Isokinetic dynamometer evaluation of the effects of early thigh diameter difference on thigh muscle strength in patients undergoing anterior cruciate ligament reconstruction with hamstring tendon graft. J Exerc Rehabil. 2015;11(2):95–100. https://doi.org/10.12965/jer.150100.
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M, et al. Effect of posterolateral bundle graft fixation angles on clinical outcomes in double-bundle anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2015;43(5):1157–64. https://doi.org/10.1177/0363546514567069.
Koga H, Muneta T, Yagishita K, Watanabe T, Mochizuki T, Horie M, et al. Mid- to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2015;31(1):69–76. https://doi.org/10.1016/j.arthro.2014.07.020.
Kondo E, Yasuda K, Miyatake S, Kitamura N, Tohyama H, Yagi T. Clinical comparison of two suspensory fixation devices for anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1261–7. https://doi.org/10.1007/s00167-011-1687-6.
Kondo E, Yasuda K, Kitamura N, Onodera J, Yokota M, Yagi T, et al. Effects of initial graft tension on clinical outcome after anatomic double-bundle anterior cruciate ligament reconstruction: comparison of two graft tension protocols. BMC Musculoskelet Disord. 2016;17:65. https://doi.org/10.1186/s12891-016-0909-y.
Kouloumentas P, Kavroudakis E, Charalampidis E, Triantafyllopoulos GK, Kavroudakis D. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2019;27(11):3592–8. https://doi.org/10.1007/s00167-019-05456-9.
Koutras G, Papadopoulos P, Terzidis IP, Gigis I, Pappas E. Short-term functional and clinical outcomes after ACL reconstruction with hamstrings autograft: transtibial versus anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1904–9. https://doi.org/10.1007/s00167-012-2323-9.
Królikowska A, Reichert P, Czamara A, Krzemińska K. Peak torque angle of anterior cruciate ligament-reconstructed knee flexor muscles in patients with semitendinosus and gracilis autograft is shifted towards extension regardless of the postoperative duration of supervised physiotherapy. PLoS ONE. 2019;14(2): e0211825. https://doi.org/10.1371/journal.pone.0211825.
Królikowska A, Sikorski Ł, Czamara A, Reichert P. Are the knee extensor and flexor muscles isokinetic parameters affected by the duration of postoperative physiotherapy supervision in patients eight months after ACL reconstruction with the use of semitendinosus and gracilis tendons autograft? Acta Bioeng Biomech. 2018;20(4):89–100.
Lautamies R, Harilainen A, Sandelin J, Kettunen J, Kujala UM. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2008;16(11):1009–16. https://doi.org/10.1007/s00167-008-0598-7.
Lee D-H, Lee J-H, Jeong H-J, Lee S-J. Serial changes in knee muscle strength after anterior cruciate ligament reconstruction using hamstring tendon autografts. Arthrosc J Arthrosc Relat Surg. 2015;31(5):890–5. https://doi.org/10.1016/j.arthro.2014.12.005.
Lee JK, Lee S, Lee MC. Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med. 2016;44(9):2323–9. https://doi.org/10.1177/0363546516650666.
Lesevic M, Kew ME, Bodkin SG, Diduch DR, Brockmeier SF, Miller MD, et al. The affect of patient sex and graft type on postoperative functional outcomes after primary ACL reconstruction. Orthop J Sports Med. 2020;8(6):2325967120926052. https://doi.org/10.1177/2325967120926052.
Maeda A, Shino K, Horibe S, Nakata K, Buccafusca G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am J Sports Med. 1996;24(4):504–9. https://doi.org/10.1177/036354659602400416.
Matsumoto A, Yoshiya S, Muratsu H, Kurosaka M, Yagi M, Iwasaki Y, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(2):213–9. https://doi.org/10.1177/0363546505279919.
Murray MM, Kalish LA, Fleming BC, Flutie B, Freiberger C, Henderson RN, et al. Bridge-enhanced anterior cruciate ligament repair: two-year results of a first-in-human study. Orthop J Sports Med. 2019. https://doi.org/10.1177/2325967118824356.
Nakamura N, Horibe S, Sasaki S, Kitaguchi T, Tagami M, Mitsuoka T, et al. Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy. 2002;18(6):598–602. https://doi.org/10.1053/jars.2002.32868.
Nishio Y, Kondo E, Onodera J, Onodera T, Yagi T, Iwasaki N, et al. Double-bundle anterior cruciate ligament reconstruction using hamstring tendon hybrid grafts in patients over 40 years of age: comparisons between different age groups. Orthop J Sports Med. 2018;6(5):2325967118773685. https://doi.org/10.1177/2325967118773685.
Ogborn D, McRae S, Larose G, Leiter J, Brown H, MacDonald P. Knee flexor strength and symmetry vary by device, body position and angle of assessment following ACL reconstruction with hamstring grafts at long-term follow-up. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2021. https://doi.org/10.1007/s00167-021-06712-7.
Riesterer J, Mauch M, Paul J, Gehring D, Ritzmann R, Wenning M. Relationship between pre- and post-operative isokinetic strength after ACL reconstruction using hamstring autograft. BMC Sports Sci Med Rehabil. 2020;12(1):68. https://doi.org/10.1186/s13102-020-00215-7.
Roman DP, Ness BM, Giampetruzzi N, Cleland JA, Weaver A. Knee strength outcomes in adolescents by age and sex during late-stage rehabilitation after anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;51:102–9. https://doi.org/10.1016/j.ptsp.2021.07.004.
Sanada T, Iwaso H, Fukai A, Honda E, Yoshitomi H, Inagawa M. Anatomic anterior cruciate ligament reconstruction using rectangular bone-tendon- bone autograft versus double-bundle hamstring tendon autograft in young female athletes. Arthrosc Sports Med Rehabil. 2021;3(1):e47–55. https://doi.org/10.1016/j.asmr.2020.08.008.
San Jose AT, Maniar N, Timmins RG, Beerworth K, Hampel C, Tyson N, et al. Explosive hamstrings strength asymmetry persists despite maximal hamstring strength recovery following anterior cruciate ligament reconstruction using hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2022. https://doi.org/10.1007/s00167-022-07096-y.
Sengoku T, Nakase J, Asai K, Yoshimizu R, Sakurai G, Yoshida S, et al. The effect of gracilis tendon harvesting in addition to semitendinosus tendon harvesting on knee extensor and flexor strength after anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2022;142(3):465–70. https://doi.org/10.1007/s00402-021-03877-1.
Severyns M, Plawecki S, Odri GA, Vendeuvre T, Depiesse F, Flez JF, et al. Correlation of isokinetic testing and ACL failure with the short graft tape suspension technique at six months. Arthrosc Sports Med Rehabil. 2022;4(2):e585–90. https://doi.org/10.1016/j.asmr.2021.11.020.
Sinding KS, Nielsen TG, Hvid LG, Lind M, Dalgas U. Effects of autograft types on muscle strength and functional capacity in patients having anterior cruciate ligament reconstruction: a randomized controlled trial. Sports Med. 2020;50(7):1393–403. https://doi.org/10.1007/s40279-020-01276-x.
Suh DK, Rhim HC, Cho I-Y, Han S-B, Lee JH, Jang K-M. Comparison of muscle strength and neuromuscular control up to 1 year after anterior cruciate ligament reconstruction between patients with dominant leg and non-dominant leg injuries. Knee. 2021;29:15–25. https://doi.org/10.1016/j.knee.2021.01.006.
Tajima T, Yamaguchi N, Morita Y, Nagasawa M, Ota T, Nakamura Y, et al. Clinical and radiographic outcomes of double-bundle anterior cruciate ligament reconstruction for Asian patients with bone-patellar tendon-bone and Gracilis tendon grafts: a matched-control comparison. J Knee Surg. 2021;34(14):1545–54. https://doi.org/10.1055/s-0040-1710376.
Taketomi S, Inui H, Yamagami R, Shirakawa N, Kawaguchi K, Nakagawa T, et al. Bone-patellar tendon-bone autograft versus hamstring tendon autograft for anatomical anterior cruciate ligament reconstruction with three-dimensional validation of femoral and tibial tunnel positions. J Knee Surg. 2018;31(9):866–74. https://doi.org/10.1055/s-0037-1615813.
Tanaka Y, Yonetani Y, Horibe S, Kitaguchi T, Sato N, Takeshita S, et al. Retear of anterior cruciate ligament grafts in female basketball players: a case series. Sports Med Arthrosc Rehabil Therapy Technol. 2010;2(1):7. https://doi.org/10.1186/1758-2555-2-7.
Tim-Yun Ong M, Fu SC, Mok SW, Franco-Obregon A, Lok-Sze Yam S, Shu-Hang YP. Persistent quadriceps muscle atrophy after anterior cruciate ligament reconstruction is associated with alterations in exercise-induced myokine production. Asia-Pac J Sports Med Arthrosc Rehabil Technol. 2022;29:35–42. https://doi.org/10.1016/j.asmart.2022.05.001.
Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S. Comparable results between lateralized single- and double-bundle ACL reconstructions. Clin Orthop Relat Res. 2009;467(4):1042–55. https://doi.org/10.1007/s11999-008-0604-x.
Ueda Y, Matsushita T, Shibata Y, Takiguchi K, Ono K, Kida A, et al. Satisfaction with playing pre-injury sports 1 year after anterior cruciate ligament reconstruction using a hamstring autograft. Knee. 2021;33:282–9. https://doi.org/10.1016/j.knee.2021.10.013.
Witvrouw E, Bellemans J, Verdonk R, Cambier D, Coorevits P, Almqvist F. Patellar tendon vs. doubled semitendinosus and gracilis tendon for anterior cruciate ligament reconstruction. Int Orthop. 2001;25(5):308–11. https://doi.org/10.1007/s002640100268.
Sengoku T, Nakase J, Asai K, Yoshimizu R, Sakurai G, Yoshida S, et al. The effect of gracilis tendon harvesting in addition to semitendinosus tendon harvesting on knee extensor and flexor strength after anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2021. https://doi.org/10.1007/s00402-021-03877-1.
Yamanashi Y, Mutsuzaki H, Iwai K, Ikeda K, Kinugasa T. Failure risks in anatomic single-bundle anterior cruciate ligament reconstruction via the outside-in tunnel technique using a hamstring autograft. J Orthop. 2019;16(6):504–7. https://doi.org/10.1016/j.jor.2019.04.015.
Cristiani R, Sarakatsianos V, Engström B, Samuelsson K, Forssblad M, Stålman A. Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):381–8. https://doi.org/10.1007/s00167-018-5029-9.
Undheim MB, Cosgrave C, King E, Strike S, Marshall B, Falvey É, et al. Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: Is there an association? A systematic review and a protocol recommendation. Br J Sports Med. 2015;49(20):1305–10. https://doi.org/10.1136/bjsports-2014-093962.
Dhillon MS, Rajnish RK, Dhillon S, Kumar P. Is there significant regeneration of the hamstring tendons after harvest for ACL reconstruction? A systematic review of literature. J Clin Orthop Trauma. 2021;16:208–18. https://doi.org/10.1016/j.jcot.2021.02.011.
Tampere T, Victor J, Luyckx T, Vermue H, Arnout N, Witvrouw E, et al. Biceps femoris compensates for semitendinosus after anterior cruciate ligament reconstruction with a hamstring autograft: a muscle functional magnetic resonance imaging study in male soccer players. Am J Sports Med. 2021;49(6):1470–81. https://doi.org/10.1177/03635465211003309.
Bregenhof B, Aagaard P, Nissen N, Creaby MW, Thorlund JB, Jensen C, et al. The effect of progressive resistance exercise on knee muscle strength and function in participants with persistent hamstring deficit following ACL reconstruction: a randomized controlled trial. J Orthop Sports Phys Ther. 2023;53(1):40–8. https://doi.org/10.2519/jospt.2022.11360.
Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J. Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 36 years. Am J Sports Med. 2017;45(6):1326–32. https://doi.org/10.1177/0363546516688665.
Cristiani R, Mikkelsen C, Stalman A, Engstrom B, Wange P, Olsson D. Autograft type affects muscle strength and hop performance after ACL reconstruction. A randomised controlled trial comparing patellar tendon and hamstring tendon autografts with standard or accelerated rehabilitation. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2021;29(9):3025–36. https://doi.org/10.1007/s00167-020-06334-5.
Drogset JO, Strand T, Uppheim G, Odegard B, Boe A, Grontvedt T. Autologous patellar tendon and quadrupled hamstring grafts in anterior cruciate ligament reconstruction: a prospective randomized multicenter review of different fixation methods. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1085–93. https://doi.org/10.1007/s00167-009-0996-5.
Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35(3):384–94. https://doi.org/10.1177/0363546506294361.
Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3–8. https://doi.org/10.1097/JSM.0b013e318190bddb.
Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1966–74. https://doi.org/10.1007/s00167-017-4747-8.
Acknowledgements
None.
Funding
Open access funding provided by University of Gothenburg. No sources of funding were used to assist in the preparation of this article.
Author information
Authors and Affiliations
Contributions
JH drafted the initial version of the manuscript. JH and EHS were responsible for drafting the manuscript and revising it critically for important intellectual content. JL contributed substantially during the selection process and RP during the critical appraisal of included studies and the assessment of certainty of evidence. MW, RS, and KS made large contributions to the revision and design of the work. JH and EHS were responsible for the concept of design. All authors read and approved the final version.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
The authors declare they have no conflicts of interest relevant to the content of this review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The Search Strategy.
Additional file 2.
Complementary Result Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Högberg, J., Piussi, R., Lövgren, J. et al. Restoring Knee Flexor Strength Symmetry Requires 2 Years After ACL Reconstruction, But Does It Matter for Second ACL Injuries? A Systematic Review and Meta-analysis. Sports Med - Open 10, 2 (2024). https://doi.org/10.1186/s40798-023-00666-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-023-00666-5