Abstract
Background
In utero intestinal volvulus with intestinal atresia is a rare and life-threatening condition that can cause torsion of the dilated bowel. The management and outcomes of this disease remain unclear.
Case presentation
A 19-year-old woman noticed a decrease in fetal motion at 35 weeks. Fetal ultrasound showed dilated fetal bowel and the whirlpool sign. The patient was referred to our hospital for an emergency cesarean section. The neonate’s abdomen was dark and severely distended, and a laparotomy was performed. Necrotic ileum and cord-type intestinal atresia (Type II) were observed in the dilated terminal ileum. The necrotic ileum was resected, and a second-look surgery was performed the following day. Then, we anastomosed the remaining intestine, and the total intestine length was 52 cm. There were no surgical complications, and the patient was discharged without requiring total parenteral nutrition or fluid infusion. The patient’s height and weight were within the − 2 standard deviation range of the growth curve at 5 months.
Conclusions
Emergency and appropriate management of intestinal volvulus in utero causing torsion of the dilated bowel resulted in good outcomes in a patient with intestinal atresia. Perinatal physicians should be aware of this emergency condition and plan their treatment approach accordingly.
Similar content being viewed by others
Background
In utero intestinal volvulus is a life-threatening condition, and delayed diagnosis contributes to a high incidence of morbidity and mortality [1, 2]. Dilated bowel torsion in intestinal atresia is a recognized postnatal emergency complication [3], which necessitates various therapeutic procedures depending on the condition of the intestines. However, in utero cases are extremely rare, and the management and outcomes remain unclear.
Prenatal diagnosis of intestinal atresia is frequently characterized by bowel distension and can be accompanied by meconium peritonitis [4]. However, the complications associated with in utero intestinal atresia are poorly documented, and the need for prompt intervention is not widely acknowledged.
Herein, we present the case of a successfully treated patient with ileal atresia and intestinal volvulus in utero with subsequent torsion of the dilated bowel.
Case presentation
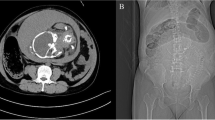
The patient was a 19-year-old pregnant woman without any prior abnormalities during her pregnancy. A decrease in fetal motion was noticed at 35 weeks. Fetal ultrasound showed dilated fetal bowel and the whirlpool sign (Fig. 1). The patient was referred to our hospital the same day. Cardiotocography showed a decreased variability and absence of deceleration. Because of fetal indications, such as bowel ischemia, an emergency cesarean section was performed. A girl was delivered at 35 weeks with a birth weight of 2752 g. The Apgar scores were 3 and 7 at 1 min and 5 min, respectively. The neonate’s abdomen was dark and severely distended (Fig. 2a). The neonate was intubated immediately. The abdominal X-ray was gasless with a distended abdomen (Fig. 2b). In the blood test, the white blood cell count was 37,520/μL, and the hemoglobin level was 9.6 g/dL. The patient’s aspartate transferase and alanine transferase levels were elevated at 185 U/L and 41 U/L, respectively. There were no findings of renal dysfunction or coagulopathy.
We performed a laparotomy on the newborn 2 h after birth (5 h after the mother arrived at our hospital). We observed massive ascites with dark fluid, and almost the entire small intestine was twisted around the axis of the dilated intestine. (Fig. 3a). While de-twisting the ileum, a cord-type intestinal atresia (Type II) was detected in the dilated terminal ileum (Fig. 3b). We resected only the obvious necrotic ileum (40 cm) while excluding uncertain ischemic regions. Bilateral intestinal stamps were temporally closed and returned to the abdominal cavity. Then, 24 h after the initial surgery, a second-look surgery was performed, and we resected a 5-cm necrotic proximal intestine and a cord-type atretic portion on the distal intestine. Consequently, the remaining small intestine was 52 cm. Nearly the entire jejunum and approximately 2 cm of the terminal ileum were preserved after resection. We anastomosed these segments end-to-end to avoid an ileostomy and to preserve the ileocecal valve and intestine. The pathological findings of resected intestines were hemorrhage within mucosa and inflammation in all layers. No other abnormalities were noted (Fig. 4). The neonate’s respiratory function worsened due to elevated bilateral diaphragms, and the abdominal wall was treated using the silo procedure with an open abdomen. Respiratory function improved 1 week after the second surgery, and the abdominal wall was closed.
The patient started feeding at 2 weeks after the anastomosis. There were no surgical complications, and the patient was discharged 3 months later without requiring total parenteral nutrition or fluid infusion. The patient showed growth beyond the growth curve, and at 5 months of age, her height and weight were within the − 2 standard deviation range.
Discussion
Since intestinal volvulus in utero with torsion of the dilated bowel in patients with ileal atresia is rare, surgical treatments and their outcomes are uncertain. Our patient was treated with emergency interventions, which preserved the growth and development of intestinal autonomy.
Intestinal volvulus in utero is reported as a rare neonatal surgical emergency [1, 5,6,7]. Prenatal diagnosis and sonographic findings include dilated bowel loops, the whirlpool, coffee bean, kinked loop signs, and polyhydramnios [2, 8]. The sensitivity and specificity of the whirlpool sign after birth are 45.4% and 99%, respectively [9]. Similarly, the specificity in utero may be high. In a literature review by Ohuoba et al., it was reported that of the fourteen in utero intestinal volvulus cases, nine were born by vaginal delivery and five by cesarean section, with all cases surviving [1]. However, the relationship between the length of the remaining intestinal tract and the delivery method is unclear. In the present case, despite the absence of severe distress during fetal monitoring, we elected to perform an emergency cesarean section due to fetal indication. Almost the entire small intestine was twisted around the axis of the dilated intestine. Our choice of delivery method might explain the good outcome for our patient.
Midgut malrotation is the most common cause of intestinal volvulus in utero [5]. We found four cases of intestinal volvulus with intestinal atresia [1, 10,11,12]. Reported cases include intestinal atresia with volvulus, and meconium peritonitis and intestinal atresia with volvulus and intussusception [13]. The whirlpool sign was detected in two cases (50%). Unlike volvulus with malrotation, the whirlpool sign might be difficult to detect because the degree and mechanisms of torsion vary. In our case, we made a diagnosis with sufficient ultrasonographic evidence, which enabled us to treat the patient promptly.
Dilated bowel torsion in intestinal atresia after birth necessitates emergency surgery [3, 14], requires various technically challenging surgical techniques, and long-term outcomes should be considered. Thus, to prevent short bowel syndrome, it is essential to resect necrotic areas or malfunctioning bowel, and also plicate the intestine and evaluate the need for an ileostomy. The same principle applies in utero, and we believe emergency procedures should be mandatory protocol. We performed immediate laparotomy while being careful not to resect uncertain intestinal segments. Although the bowel was not entirely healthy, we performed intestinal anastomosis during the second-look surgery. It is difficult to preserve the ileocecal valve if an ileostomy is created. We believe immediate and appropriate interventions, such as intestinal autonomy without needing home parenteral nutrition, are crucial for a good prognosis.
A prenatal diagnosis of intestinal atresia, characterized by bowel distension, is common, and most cases are delivered electively. However, an emergency cesarean section might be required if an intestinal volvulus is present. Obstetricians, neonatologists, anesthesiologists, surgeons, and other physicians involved in perinatal care should be aware of this disease and be prepared for emergency intervention.
Conclusions
The patient in the current case presented with intestinal atresia, which caused intestinal volvulus in utero with torsion of the dilated bowel. However, emergency interventions and appropriate surgical procedures resulted in good outcomes. Perinatal physicians should aim to understand intestinal atresia in utero and plan accordingly in an emergency.
Availability of data and materials
Not applicable.
References
Ohuoba E, Fruhman G, Olutoye O, Zacharias N. Perinatal survival of a fetus with intestinal volvulus and intussusception: a case report and review of the literature. AJP Rep. 2013;3:107–12.
Chen J, Wu D. Prenatal diagnosis of fetal midgut volvulus: a case description. Quant Imaging Med Surg. 2022;12:4326–30.
Shin HB, Kim JK, Jeong YJ. Torsion of proximal pouch in ileal atresia presenting as a large abdominal cyst. Pediatr Neonatol. 2021;62:331–2.
Hemming V, Rankin J. Small intestinal atresia in a defined population: occurrence, prenatal diagnosis and survival. Prenat Diagn. 2007;27:1205–11.
Sciarrone A, Teruzzi E, Pertusio A, Bastonero S, Errante G, Todros T, et al. Fetal midgut volvulus: report of eight cases. J Matern Neonat Med. 2016;29:1322–7.
Yang L, Chen H, Lv G, Li F, Liao J, Ke L. Evaluation of ultrasonography in fetal intestinal malrotation with midgut volvulus. Ginekol Pol. 2022;93:296–301.
Bhartiya A, Maqsood H, Naeem H, Nazar MW. Reversed intestinal malrotation presenting as bowel obstruction in pregnancy: case report and literature review. Ann Med Surg (Lond). 2022;82: 104570.
Li X, Huang T, Zhou M, Zhang C. Prenatal diagnosis of midgut volvulus using two-dimensional and three-dimensional ultrasound. Am J Transl Res. 2022;14:1859–67.
Orzech N, Navarro OM, Langer JC. Is ultrasonography a good screening test for intestinal malrotation? J Pediatr Surg. 2006;41:1005–9.
Best EJ, O’Brien CM, Carseldine W, Deshpande A, Glover R, Park F. Fetal midgut volvulus with meconium peritonitis detected on prenatal ultrasound. Case Rep Obstet Gynecol. 2018;2018:5312179.
Lee JH, Im SA, Lee G. Evolution of sonographic findings in a fetus with ileal atresia. J Clin Ultrasound. 2011;39:359–62.
Yu W, Ailu C, Bing W. Sonographic diagnosis of fetal intestinal volvulus with ileal atresia: a case report. J Clin Ultrasound. 2013;41:255–7.
Yine CSC, Krishnan A, Bahari MB. A rare case of intrauterine intussusception causing ileal atresia. Med J Malay. 2020;75:304–6.
Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA. Intestinal atresia and stenosis: a 25-year experience with 277 cases. Arch Surg. 1998;133:490–7.
Funding
The authors declare that they have not received any funding for this report.
Author information
Authors and Affiliations
Contributions
CT: drafted the manuscript. YS, SI, and TM treated the patient. KN, an associate professor at our department, reviewed the literature. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the procedures were performed in accordance with the ethical standards of the appropriate version of the Declaration of Helsinki.
Consent for publication
Informed consent was obtained from the patient/parent for the publication of this report.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Toyama, C., Segawa, Y., Iijima, S. et al. Intestinal volvulus in utero causing torsion of dilated bowel with ileal atresia: a case report. surg case rep 9, 65 (2023). https://doi.org/10.1186/s40792-023-01645-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-023-01645-4