Abstract
Veno-venous extracorporeal membrane oxygenation (V–V ECMO) has an established evidence base in acute respiratory distress syndrome (ARDS) and has seen exponential growth in its use over the past decades. However, there is a paucity of evidence regarding the approach to weaning, with variation of practice and outcomes between centres. Preconditions for weaning, management of patients’ sedation and mechanical ventilation during this phase, criteria defining success or failure, and the optimal duration of a trial prior to decannulation are all debated subjects. Moreover, there is no prospective evidence demonstrating the superiority of weaning the sweep gas flow (SGF), the extracorporeal blood flow (ECBF) or the fraction of oxygen of the SGF (FdO2), thereby a broad inter-centre variability exists in this regard. Accordingly, the aim of this review is to discuss the required physiological basis to interpret different weaning approaches: first, we will outline the physiological changes in blood gases which should be expected from manipulations of ECBF, SGF and FdO2. Subsequently, we will describe the resulting adaptation of patients’ control of breathing, with special reference to the effects of weaning on respiratory effort. Finally, we will discuss pertinent elements of the monitoring and mechanical ventilation of passive and spontaneously breathing patients during a weaning trial. Indeed, to avoid lung injury, invasive monitoring is often required in patients making spontaneous effort, as pressures measured at the airway may not reflect the degree of lung strain. In the absence of evidence, our approach to weaning is driven largely by an understanding of physiology.
Take home message
Successful weaning from veno-venous ECMO requires understanding and consideration of the complex physiological interactions between the native and the extracorporeal lung. We describe our understanding of the physiological adaptations of the patient as extracorporeal support is weaned and outline the implications for clinical practice.
Similar content being viewed by others
Introduction
Veno-venous extracorporeal membrane oxygenation (V–V ECMO) is a technique that can support gas exchange and enable a reduction in the mechanical power applied to the injured lung in patients with acute severe and refractory, but potentially reversible, respiratory failure.
The increasing emphasis on reducing ergotrauma, the technological improvements in the extracorporeal devices, and the viral pandemics (i.e. H1N1 influenza and SARS-CoV 2) have resulted in an exponential growth in ECMO utilization over the last decade [1]. The possible applications of V–V ECMO are wide, including severe Acute Respiratory Distress Syndrome (ARDS), near fatal asthma, severe air leak syndromes, interstitial lung disease or as a bridge to lung transplantation [2,3,4,5,6].
In contrast to the abundance of data on indications, complications and prognostic factors for ECMO survival [1,2,3], consensus guidelines on weaning [6] are based on limited direct evidence on the criteria to initiate a weaning trial, how to monitor patients undergoing weaning and how to adjust mechanical ventilation to optimally support patients during this phase.
In Table 1 [3, 6, 8,9,10,11,12,13,14,15,16,17,18,19,20], we summarize the different approaches to weaning of V–V ECMO reported in the literature. Most centres wean the sweep gas flow (SGF) to zero but variable practice regarding manipulation of extracorporeal blood flow (ECBF) or the fraction of oxygen of the SGF (FdO2) is apparent between centres. Furthermore, the monitoring criteria and duration of a weaning trial are extremely variable, with few centres reporting objective assessment of respiratory drive and effort.
This variation in practice may contribute to inter-centre heterogeneity in V–V ECMO outcome [1]. Identifying strategies which can accelerate the safe liberation of patients from ECMO are essential to reduce length of stay and risk of complications, as well as ensuring equity of access at times of strain on healthcare resources [7].
A sound understanding of the physiological interactions between the extracorporeal circuit, the patient and the ventilator is required to guide physicians throughout the process of weaning. Accordingly, this review aims to describe a possible physiological approach to weaning from V–V ECMO.
Physiology of weaning from V–V ECMO
The extracorporeal circuit
V’O2ML, V’CO2ML and the effects of weaning
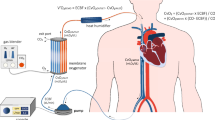
The extracorporeal circuit is depicted in Fig. 1. Table 2 summarizes the effects of weaning different ECMO parameters on V’O2ML and V’CO2ML. There are three main settings which can be manipulated during the weaning or trial off V–V ECMO [21]:
The anatomy and physiology of the extracorporeal circuit, depicted in a femoral–jugular configuration. Blood is drained from the central venous system (CV) via a cannula and centrifugal pump which generates extracorporeal blood flow (ECBF). Pre-oxygenator blood is a mixture of central venous (Cv) and recirculating (QR) blood. It is pumped across hollow fibres within the membrane oxygenator across which there is sweep gas flow (SGF). Post-oxygenator blood passes through the return lumen where it becomes mixed with the CV blood in the right ventricle and pulmonary arteries to form the mixed venous blood (CVmixed) before being distributed through the native pulmonary circulation. Mixed central venous bloods oxygen content (CVmixedO2) will be determined by: the central venous oxygen content (CvO2), the post-oxygenator blood’s oxygen content (Cpost-oxy O2), the extracorporeal blood flow (ECBF), recirculation flow (QR) and overall cardiac output (Qt) according to the formula: CVmixedO2·Qt = [CvO2·(Qt-ECBF + Qr)] + [Cpost-oxyO2·(ECBF-QR)]. Although the ECBF contributes to the calculation of the overall CO2 clearance of the membrane lung [V’CO2ML = (Cpost-oxyCO2 − Cpost-oxyCO2)·ECBF·25)], during the usual V–V ECMO ECBF levels (> 2.5 L) the primary determinant of V’CO2ML is the SGF rate which generates the gradient for CO2 diffusion and resulting difference in pre- and post-oxygenator CO2 content
Effects of reducing ECBF
The ECBF rate has differing effects on the oxygen delivery (V’O2ML) and CO2 clearance of the membrane lung (V’CO2ML). With a well-functioning circuit, nearly all haemoglobin passing through the membrane lung will become 100% saturated even at very low SGF rates. Consequently, if the FdO2 is unchanged, the ECBF is the main titratable variable which can affect the V’O2ML. However, the nature of the relationship between ECBF and the V’O2ML is affected by the amount of recirculated blood flow (QR):
-
1.
Recirculation occurs when arterialized blood returned to the venous system after passing through the membrane lung is aspirated straight back into the circuit (see Fig. 1), lowering the gradient between the pre- and post-membrane blood oxygen content and therefore the V’O2ML. Effective ECBF, equal to total ECBF minus QR, is linearly related to V’O2ML [21] but QR cannot be easily quantified at the bedside.
-
2.
The proportion of QR may be higher at higher ECBF. If a given decrease in ECBF during weaning disproportionately reduces QR then the change in V’O2ML may not be as anticipated. For example, if the QR reduces from 1 L to 250 mL when the ECBF is weaned by 25% from 4 to 3 L/min, then the effective ECBF has only changed from 3 L to 2.75 L. Conversely, when QR is minimal decreasing the total ECBF will decrease the V’O2ML linearly [21].
The effect of weaning the ECBF upon the systemic oxygenation will depend on the cardiac output and venous admixture: as the proportion of the total cardiac output captured into the ECBF falls, the mixed venous oxygen content will decrease, and the final effect upon systemic oxygenation will be determined by native lung function.
In contrast to V’O2ML, the relationship between ECBF and V’CO2ML is not linear, but follows a natural logarithmic curve with ECBF > 0.5 mL/min, which plateaus at > 1.0 L/min [22, 23]. The impact of the ECBF on V’CO2ML is also affected by the ratio of SGF:ECBF and the surface area of the membrane lung [22]. Accordingly, step-wise decreases in ECBF have minimal independent effect on the V’CO2ML until reaching very low levels- which are generally avoided to prevent circuit thrombosis.
Effects of reducing SGF rate without altering the FdO2
Nearly complete saturation of haemoglobin can be achieved even with very low SGF rates (< 0.5 L/min) particularly when FdO2 is maintained at 1.0 [21]. For this reason, step decreases in SGF do not affect V’O2ML until SGF is almost off. Moreover, even the small amount of SGF can affect ECMO dependency for another reason: V–V ECMO causes a mixed venous ‘hyperoxia’, blunting or abolishing the physiological hypoxic pulmonary vasoconstriction [24]. This results in an increased native lung venous admixture, with lower than expected ventilation to perfusion (Va/Q) ratio [24,25,26]. Accordingly, when the SGF is turned to zero at the last step of a weaning trial, patients are abruptly totally dependent on the native lungs capacity to transfer oxygen (V’O2NL), but the biphasic response of the pulmonary vasculature to hypoxia requires minutes to hours to occur [27]. Delayed hypoxic vasoconstriction increases the effective venous admixture, worsening V/Q matching and potentially leading to hypoxaemia which might be avoided with a slower transition.
In contrast to oxygenation, step-wise decreases in SGF are associated with a progressive reduction in V’CO2ML [22]. SGF drives bulk transfer of CO2 out of the artificial membrane and increases the gradient for CO2 in the venous blood to diffuse across the membrane. Accordingly, step decreases in SGF, result in a higher CO2 in the pulmonary vasculature and greater load to the native lung (V’CO2NL), whose exchange capacity will affect PaCO2. Several indices have been proposed for a bedside evaluation of the CO2 clearance capacity of the natural lung, as summarized in Table 3 [19, 20, 28, 29]. Interestingly, the partial pressure of end tidal to arterial PCO2 ratio (PET:PaCO2), an index of global gas-exchange efficiency [30], was the best predictor of weaning outcome in a recent study [together with a measure of ventilatory efficiency (ratio of respiratory effort to V’CO2NL)] [20].
When SGF is set to zero, V–V ECMO makes no contribution to gas exchange and, after the restoration of hypoxic pulmonary vasoconstriction, a true assessment of native lung function can occur. A special case in which a sudden reduction in arterial oxygenation is unrelated to a lung function and severe hypoxaemia occurs when there is an intracardiac shunt: in this case, the flow from the return cannula can force blood through the shunt, bypassing the native lung and potentially leading to profound desaturation when SGF falls to zero. This will become evident if ECBF is not concomitantly reduced to < 1 L/min when no compensatory oxygen is added from the extracorporeal circuit [31].
Effects of reducing the FdO2 prior to reducing the SGF
Gradually reducing the FdO2 leads to a sequential decrease in V’O2ML, while V’CO2ML remains unaltered. The progressive decrease in FdO2 has the advantage of allowing time to restore hypoxic pulmonary vasoconstriction [21]. This will prevent rapid desaturations and provides a more accurate assessment of the oxygen exchange capacity of the native lung. The effect on systemic oxygenation of a reduction in V’O2ML through step decreases in FdO2 will largely depend on the ratio of ECBF to cardiac output and on the venous admixture of the native lung.
However, reductions in FdO2 may have counter-intuitive effects on the alveolar oxygen partial pressure. If FdO2 is weaned in isolation (i.e. SGF is maintained constant), the contribution of V’O2ML to total V’O2 falls, whilst the proportion of the total metabolically produced CO2 cleared by the natural lung remains largely unchanged, or even decreased if metabolic CO2 production increases with the hypoxic drive, and the native lung is unable to increase CO2. In this case, the CO2 removed extracorporeally proportionally increases. This means that the respiratory quotient of the natural lung (RQNL = V’CO2NL: V’O2NL) will be reduced [32]. The implications of this can be seen from the alveolar gas equation:
where PAO2 and PACO2 are the alveolar partial pressures of oxygen and carbon dioxide, respectively, and PiO2 is the pressure of inspired oxygen.
The greater the reduction in RQNL from the V’CO2ML, the lower the PAO2. In other words, if PaCO2 is static, the V’CO2ML entails a relative alveolar hypoventilation. This leads to uptake of O2 by the lungs which is not compensated for by bulk gas transfer, resulting in a lower PAO2. However, the clinical significance of this effect during weaning from V–V ECMO should be put into context:
-
1.
The extended alveolar equation has a supplementary term (in bold here below) which, accounting for changes in alveolar gas volume during breathing, blunts the deleterious effect of low RQ on PAO2, especially if the FiO2 from the native lung is high [33, 34]:
$${\mathrm{PAO}}_{2}={\mathrm{PiO}}_{2}-\frac{{\mathrm{PACO}}_{2}}{{\mathrm{RQ}}_{\mathrm{NL}}}+\mathrm{ Fi}{\mathrm{O}}_{2}\bullet \mathrm{ PAC}{\mathrm{O}}_{2}\bullet \frac{1-{\mathrm{RQ}}_{\mathrm{NL}}}{{\mathrm{RQ}}_{\mathrm{NL}}}.$$ -
2.
The reduction in PAO2 at low RQNL is most clinically relevant during extracorporeal CO2 removal (ECCO2R) [32], where ECBF is < 1 L/min. However, this will be less evident during weaning of V–V ECMO where the ECBF is much higher: indeed, even at FdO2 0.21, there may still be a substantial V’O2ML [21].
The patient
The patient’s response to a weaning trial is dictated by the physiology of breathing control and, particularly, by the effects of variations in gas-exchange on the output of the respiratory centres.
Physiology of breathing control
A simple, yet effective model describing the control of breathing has been proposed by Georgopoulos et al. [35] and subsequently adopted by others [36]. As depicted in Fig. 2 [35,36,37,38], this model describes the interdependence between the arterial partial pressure of CO2 (PaCO2) and the minute ventilation (VE) by plotting them in the same graph according to three different curves: (1) the metabolic hyperbola, describing the relationship between PaCO2 and VE at a given V’CO2NL and dead space (Vd/Vt); (2) the CO2 sensitivity curve (also called the brain curve), describing the change in VE that the respiratory centres desire when PaCO2 deviates from its set-point; (3) the ventilation curve, depicting the corresponding change in VE that the respiratory system can actually achieve for a given PaCO2. In health, the brain and ventilation curves are synonymous.
Georgopolous model of breathing control during weaning. A Reflects health, were the brain and ventilation curve are synonymous, thereby eupneic and actual PaCO2 coincide. Possible contributors to the position of the brain curve, ventilation curve and metabolic hyperbola, and the varying slope of the latter (larger ∆VE required to achieve a given ∆PaCO2 when ventilation is higher) are also shown. B Represents a possible SGF weaning trial off: as the CO2 cleared by the membrane lung (V’CO2ML) is reduced the metabolic hyperbola shifts upwards and to the right, while the brain and ventilation curve shift in parallel to the left to maintain the eupneic PaCO2. C Represents a possible FdO2 or ECBF weaning trial off: as the oxygen provided by the membrane lung (V’O2ML) is reduced during weaning any hypoxaemia would shifts the position and slope of the brain curve a new eupneic PaCO2. This new equilibration point will drive non-metabolic CO2 from body stores into the bloodstream possibly shifting the metabolic hyperbola upward and to the right. D Depicts possible weaning-induced changes in the relative position of the brain and ventilation curves (maintained synonymous for simplicity in all other Panels): note that any deviation between the two curves induces a difference between the actual and eupneic CO2. MV: mechanical ventilation, PaCO2: the partial pressure of arterial carbon dioxide, V’CO2NL: the total CO2 to be cleared by the natural lung, Vd/Vt the dead space fraction of the tidal volume, V’CO2ML: the CO2 cleared by the membrane lung
The intersection between the brain curve and the metabolic hyperbola gives the ‘eupneic’ PaCO2, i.e. the PaCO2 set-point of the respiratory centres. Conversely, the intersection between the ventilation curve and the metabolic hyperbola gives the actual PaCO2 of the patient. Panel A in Fig. 2 describes physiological and pathological determinants of the slopes and positions of these three curves [35, 36].
Effects of weaning on respiratory centres output
According to the Georgopoulos model, weaning may affect the respiratory centres’ output through the following mechanisms.
Step decreases in SGF may change the position of the metabolic hyperbola
Normally, around 6–7 L/min of VE is sufficient to maintain a PaCO2 at 40 mmHg at physiologic VCO2NL. During V–V ECMO, VCO2NL decreases and the metabolic hyperbola shifts downward and to the left (i.e. lower VE is required to maintain the same PaCO2). Conversely, during weaning, step decreases in SGF rate reduce V’CO2ML and the total metabolic V’CO2 increases at higher work of breathing. For both reasons, V’CO2NL is expected to increase, shifting the metabolic hyperbola upward and to the right (see Panel B in Fig. 2).
Step decreases in FdO2 or ECBF may change the set-point of the brain curve
Normally, the brain is set to maintain a PaCO2 around 40 mmHg. However, chemical (PaO2 and pH), reflex (lung and chest wall receptors) and cortical (wakefulness, sedation, agitation) inputs can change the set-point to lower or higher values. In ARDS, stimulation of lung mechanoceptors and inflammation contribute to a low PaCO2 set-point even in normoxia. For this reason, even with maximal V’CO2ML it is uncommon to induce apnoea during V–V ECMO for ARDS [39]. During weaning, step decreases in V’O2ML, may induce hypoxemia, thereby lowering the PaCO2 set-point. This will result in the brain curve shifting to the left and increasing its slope (see Panel C in Fig. 2).
Changes in breathing pattern may affect the ventilation curve
In health, ventilation satisfies the activity of the respiratory centres, thereby the ventilation and brain curve overlap and the actual PaCO2 matches the eupnoeic PaCO2. In ARDS, the descending pathway from the brain to the lung is altered. Dissociation between the two curves results in dyspnoea and further increasing the already high respiratory centres output. During weaning, elicited natural lung ventilation might decrease lung elastance (intra-tidal recruitment) [40] or resistances (inversely correlated with tidal volume [41]), thereby partially re-establishing the matching between the brain and the ventilation curve. On the other hand, neuromechanical uncoupling may worsen if PEEP is increased without corresponding recruitment [42] or if muscular fatigue is associated with inadequate support. Accordingly, the dissociation between the brain and the ventilation curve may increase (see Panel D in Fig. 2).
There are other important interactions which are particularly relevant in the spontaneously breathing patient:
-
1.
With increasing VCO2NL, shifting the metabolic hyperbola upward and to the right would result in increased PaCO2 if the brain curve did not concomitantly change position (see Fig. 2 Panel B). However, it has been experimentally shown that PaCO2 remains constant at decreasing SGF, unless extreme effort is reached [20]. A similar behaviour of the respiratory centres occurs in exercise, where increasing VCO2NL is associated with a parallel leftward shift of the brain curve (at constant slope) to maintain constant PaCO2 (isocapnic hyperpnea) [37]. The underlying mechanism explaining this phenomenon remains debated [43].
-
2.
When the brain curve shifts to lower PaCO2 set points, the entire pool of CO2 body stores must equilibrate with the new PaCO2 (see Fig. 2 panel C). This requires displacement of a vast amount of non-metabolic CO2 from peripheral tissues into the bloodstream increasing V’CO2NL [44] and further shifting the metabolic hyperbola upward and to the right. The higher the pool of total body CO2 stores (for example due to prior permissive hypercapnia), the greater the amount of CO2 displaced to reach equilibrium and therefore the greater V’CO2NL which may be required to maintain the new set-point.
-
3.
The slope of the metabolic hyperbola, describing how much VE must change to obtain a given change in PaCO2 (the so-called “plant gain”) has two characteristics which are relevant to weaning. First, it is lower at higher VE [38] (see Fig. 2 panel A). Therefore, during weaning, higher changes in VE are required to achieve a new PaCO2 set-point if the patient is already hyperventilating prior to the trial. This might be one reason why high breathing effort before or during a weaning trial has been associated with weaning failure [19, 20]. Second the slope decreases when the V’CO2ML is decreased [37]. Accordingly reaching a new PaCO2 set-point (e.g. because of hypoxaemia) requires much more effort during the later stages of a weaning trial. For both reasons, avoiding hypoxaemia, distress or any other cause for a shift in the eupneic threshold is important during a weaning trial.
Monitoring respiratory centres output
Respiratory centres can express their output in terms of timing or intensity: the timing is reflected by respiratory rate, while the intensity of output is referred to as respiratory drive. Respiratory rate significantly increases only when respiratory drive is 3–4 times elevated [35, 36]. Similarly, clinical signs of high effort occur when drive is already excessive. For this reason, invasive assessment of drive is necessary to predict the success or failure of weaning prior to the development of overt distress. Directly measuring the rate of change of the electrical activity of the brain centres is not feasible in routine practice, thereby surrogates need to be employed. These surrogates relate more or less directly to respiratory drive (the electrical activity of the diaphragm, EAdi [45]), others with respiratory effort (P0.1 [46], the swing in oesophageal, ∆Peso, and transdiaphragmatic pressure, ∆Pdi [47], or the muscle pressure, Pmusc, and the occlusion pressure, Pocc [48]), others with lung stress (dynamic transpulmonary pressure, ∆PL [47, 48]). If the descending pathway is altered (neuromuscular impairment, increased respiratory system elastance), as typically seen in patient undergoing V–V ECMO, a dissociation between these indices might occur, thereby complicating the assessment of the respiratory centres output.
The ventilator
We have discussed the effects of weaning extracorporeal parameters on V’O2ML and V’CO2ML together with the resulting interactions with the patient’s respiratory centres. In the following section, we will discuss the approach to mechanical ventilation during a weaning trial.
Passive controlled patients
In fully sedated patients in controlled modes, changes in extracorporeal gas exchange may be directly reflected in the systemic arterial blood gases if concomitant changes in mechanical ventilation are not made. For safe decannulation from V–V ECMO, maintenance of gas exchange must not be at the cost of excessive risk of ventilator induced lung injury (VILI). Overall, protective ventilation during V–V ECMO is debated [49]. The holistic concept of mechanical power [50] particularly highlights the harms of respiratory rate as well as driving pressure [51], though safety thresholds are unclear [52, 53]. Associations between mortality and the use of higher driving pressure [54], and mechanical power [55] during V–V ECMO have been made from cohort studies and a period of total lung rest with zero driving pressure was correlated with lower plasma biomarkers of lung injury in a recent small randomized trial [56]. However, ultra-protective ventilation may be unnecessarily cautious when patients have improved to the point of a weaning trial off. Finally, increased sedation or even neuromuscular blockade may be required to maintain synchrony if ventilation is not adequately adjusted to match the demands of the brain curve.
Spontaneously breathing patients
The spontaneously breathing patient’s respiratory centre’s output will dynamically increment to maintain gas exchange as extracorporeal support is weaned. Changes in respiratory centres output during weaning translate into breathing effort and lung stress which is the main contributor to patient self-induced lung injury (P-SILI) [57]. The role of the ventilator in reducing breathing effort and stress is crucial and can be divided into two components:
Manoeuvres reducing effort and stress
Any manoeuvre shifting the CO2 sensitivity curve to higher PaCO2 or improving the matching between the ventilation and the brain curve may reduce breathing effort and lung stress [35, 36]. The use of sedation, shifting the CO2 sensitivity curve to the right, is a typical ‘non-ventilatory’ strategy in this regard. Increasing FiO2 and PEEP (if associated with recruitment) may have beneficial effects. However, increasing PEEP may worsen neuromechanical uncoupling [42] and it can increase the static stress to the lung contributing to the total mechanical power of ventilation [50, 58]. Manoeuvres improving patient–ventilator synchrony also have the potential to reduce effort and regional stress [57].
Manoeuvres reducing effort but not stress
Any manoeuvre unloading the respiratory muscles (e.g. increasing pressure support) has the potential to reduce breathing effort, but not lung stress. Indeed, when the respiratory centres are set to maintain a certain PaCO2, pressure support leads to a decreased workload to the respiratory muscles, but the total ventilation required to maintain PaCO2 does not change (i.e. stress will not decrease) [59].
Irrespective of the manoeuvre performed, general principles of lung protection during a weaning trial in spontaneously breathing patients are similar to those in fully sedated patients under controlled ventilation (Table 4 [14, 19, 20, 57] summarizes possible stopping criteria of a weaning trial from V–V ECMO). However, some important specifics must be highlighted:
-
1.
The presence of active muscular contraction, variable between inspiration and expiration, confounds the estimation of chest wall compliance. One implication is that whole respiratory system indices like driving pressure might less reliably reflect lung stress than during passive ventilation. Additionally, abdominal muscle contraction may both reduce the static stress associated with PEEP [60, 61] and alter the estimation of effort with oesophageal pressure if gastric pressure is not concomitantly measured [47].
-
2.
Indices of effort represent an “average” measurement of the stress applied to the lung. Indeed, in spontaneous breathing, significant regional changes in oesophageal and transpulmonary pressure can occur [62]. This may elicit pendelluft and negative pressure alveolar oedema, worsening P-SILI [57]. Although PEEP can increase lung homogeneity counteracting these effects [63, 64], its downsides must be kept in mind.
Importantly, if the patient is spontaneously breathing, the development of hypercapnia or respiratory distress are late signs (panel B Fig. 3). Accordingly, measurement of drive and effort is essential to optimize mechanical ventilation and avoid exposing the patient to P-SILI and premature decannulation. Even with ‘protective’ parameters measured from the airway, the spontaneous effort to maintain normocapnia can generate enormous transpulmonary pressures [65]. Increased tidal volumes (driven by increased dead space) and new tachycardia predicted unsafe decannulation in a recent case series, but ∆Pes of > 16 cmH2O had the greatest accuracy [20].
Our process of weaning V–V ECMO. A Sequence for V–V ECMO weaning. Throughout, monitor for stopping criteria. B As SGF is weaned, the proportion of metabolically produced CO2 cleared by the natural lung (V’CO2NL/V’CO2tot) increases. In patients who are not yet suitable for decannulation, this load can only be managed with excessive effort (see next panels). Ventilatory efficiency can be expressed as the ratio of the effort (or minute ventilation) to the V’CO2NL. In patients who fail a weaning trial ventilatory efficiency is usually worse, and may deteriorate as the demands on the respiratory system rise. If they are not able to clear all of the metabolically produced CO2 then hypercapnia ensues. C Monitoring drive and effort during a weaning trial. Waveforms during a pressure supported breath, an expiratory occlusion throughout an inspiratory cycle and an end inspiratory occlusion. D Targets to maintain during a trial off V–V ECMO including measures of drive (P0.1), effort (Pocc or ∆Pes if available), stress (∆PL or DP if not available) and native lung ventilator efficiency (∆Pes/V’CO2NL, end tidal CO2 to arterial CO2 ratio (ETCO2:PaCO2) or the ratio of minute ventilation to clearance (VE/ V’CO2NL). At our centre, volumetric capnography from the ventilator and pre- and post- oxygenator blood gases are used to calculate the V’CO2NL and V’CO2ML, respectively. Unfortunately, during weaning the V’O2NL is not routinely measured. However, this is done in individual patients who have a pulmonary artery catheter for measurement of CVmixedO2 or a receive calorimetric measurements. FdO2: the fraction of oxygen of the sweep gas flow (SGF), TV: tidal volume, P0.1: pressure deflection during 100 ms of occlusion, Pocc: maximal pressure deflection during occlusion, ∆Pes oesophageal pressure swing, ∆Paw: plateau after inspiratory inclusion, including the PMI: rebound pressure from relaxing inspiratory muscles, ∆PL: transpulmonary pressure
A proposed approach to weaning
Our approach to weaning is represented in Fig. 3 [14]. Prior to commencing weaning comprehensive assessment of respiratory drive, effort, mechanical ventilation and the CO2 clearance capacity of the lung should take place, both to optimize mechanical assistance and as a baseline measure. The V’CO2NL should be at least 50% of the total metabolically produced carbon dioxide. Our preference is for patients to be on a spontaneous or assisted mode of ventilation. First the FiO2 is set to 0.6 in anticipation of reducing V’O2ML and to avoid alveolar hypoxia as the respiratory quotient is changed during weaning. The ECBF is held static unless there is suspicion of an intracardiac shunt. Next, the FdO2 is sequentially weaned in 5-min intervals, allowing for re-establishment of hypoxic pulmonary vasoconstriction and potentially increasing native ventilatory efficiency with improved V/Q matching. If an FdO2 of 0.21 is tolerated, next the SGF is sequentially decreased to zero in 5–10 min intervals. As the V’CO2ML falls, monitoring continues to ensure increasing V’CO2NL is not at the cost of injurious effort or stress. In all patients, the total V’CO2 will rise due to the increasing work of breathing to manage the load from the V’CO2ML. Depending on the pulmonary mechanics and ventilatory efficiency, in some patients the native lungs will not be capable of managing this load and they will demonstrate increasing respiratory drive, effort, minute ventilation, sympathetic activation and ultimately hypercapnia. Time to equilibrate at each step is essential in order to fully assess response and prevent P-SILI. Throughout, multimodal monitoring is continued, and the weaning test is ceased if there are indices of concern (see Table 3 and Fig. 3). As decannulation itself often produces a systemic inflammatory response in the following days, our preference is for a conservative approach to decannulation and a trial off SGF of 24 h.
Conclusions
The rationale for the use of V–V ECMO in ARDS and other forms of severe respiratory failure is becoming clearer. However, variation in mortality between centres [8] and a lack of prospective randomized evidence regarding the management of patients on V–V ECMO means there is a strong scientific rationale for further study. Early, safe liberation from V–V ECMO has the potential to hasten patient’s recovery and maintain equity of access to other patients who may benefit from this effective, but resource-intensive treatment. Although there is not yet high-grade evidence to guide clinicians, we have outlined an approach to weaning underpinned by physiology. The feasibility of weaning from V–V ECMO should be considered daily. We advocate separating the ability of the natural lung to provide O2 and remove CO2 by weaning the FdO2 prior to the SGF. The complex interactions between the determinants of respiratory drive, the patient’s effort and ventilatory assistance, their lung mechanics and efficiency of V’CO2NL will determine the outcome of a weaning trial. Care must be taken to avoid occult P-SILI in patients making spontaneous effort and we advocate multimodal assessment of drive, effort and stress throughout the weaning process.
Availability of data and materials
Not applicable to this narrative review.
References
Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH et al (2015) Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med 191:894–901. https://doi.org/10.1164/rccm.201409-1634OC
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM et al (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374:1351–1363. https://doi.org/10.1016/S0140-6736(09)61069-2
Combes A, Hajage D, Capellier G, Demoule A, Lavoue S, Guervilly C et al (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 378:1965–1975. https://doi.org/10.1056/NEJMoa1800385
Combes A, Peek GJ, Hajage D, Hardy P, Abrams P, Schmidt M et al (2020) ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med 46:2048–2057. https://doi.org/10.1007/s00134-020-06248-3
Warren A, Chiu YD, Villar SS, Fowles JA, Symes N, Barker J et al (2020) Outcomes of the NHS England National Extracorporeal Membrane Oxygenation Service for adults with respiratory failure: a multicentre observational cohort study. Br J Anaesth 125:259–266
Tonna JE, Abrams D, Brodie D, Greenwood JC, Mateo-Sidron JAR, Usman A et al (2021) Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the extracorporeal life support organization (ELSO). ASAIO J 67:601–610. https://doi.org/10.1097/MAT.0000000000001432
Gannon WD, Stokes JW, Francois SA, Patel YJ, Pugh ME, Benson C et al (2022) Association between availability of extracorporeal membrane oxygenation and mortality in patients with COVID-19 eligible for extracorporeal membrane oxygenation: a natural experiment. Am J Respir Crit Care Med 205:1354–1357. https://doi.org/10.1164/rccm.202110-2399LE
Sen A, Callisen HE, Alwardt CM et al (2016) Adult venovenous extracorporeal membrane oxygenation for severe respiratory failure: current status and future perspectives. Ann Card Anaesth 19:97–111. https://doi.org/10.4103/0971-9784.173027
Reeb J, Olland A, Pottecher J et al (2017) Extracorporeal membrane oxygenation for acute respiratory distress syndrome after pneumonectomy. Ann Thorac Surg 103:881–889. https://doi.org/10.1016/j.athoracsur.2016.11.038
Broman LM, Walfertheiner MV, Montisci A, Pappalardo F (2018) Weaning from veno-venous extracorporeal membrane oxygenation: how I do it. J Thorac Dis 10:S692–S697. https://doi.org/10.21037/jtd.2017.09.95
Grant AA, Hart VJ, Lineen EB, Badiye A, Byers PM, Patel A et al (2018) A weaning protocol for venovenous extracorporeal membrane oxygenation with a review of the literature. Artif Organs 42:605–610. https://doi.org/10.1111/aor.13087
Seiler F, Trudzinski FC, Horsch SI et al (2018) Weaning from prolonged veno-venous extracorporeal membrane oxygenation (ECMO) after transfer to a specialized center: a retrospective study. J Artif Organs 21:300–307. https://doi.org/10.1007/s10047-018-1046-1
Chaves RCF, Rabello Filho R, Timenetsky KT et al (2019) Extracorporeal membrane oxygenation: a literature review. Rev Bras Ter Intensiva 31:410–424. https://doi.org/10.5935/0103-507X.20190063
Vasques F, Romitti F, Gattinoni L, Camporata L (2019) How I wean patients from veno-venous extra-corporeal membrane oxygenation. Crit Care 23:316. https://doi.org/10.1186/s13054-019-2592-5
Li X, Guo Z, Li B et al (2020) Extracorporeal membrane oxygenation for coronavirus disease 2019 in Shanghai, China. ASAIO J 66:475–481. https://doi.org/10.1097/MAT.0000000000001172
Gannon WD, Stokes JW, Bloom S, Sherrill W, Bacchetta M, Rice TW et al (2021) Safety and feasibility of a protocolized daily assessment of readiness for liberation from venovenous extracorporeal membrane oxygenation. Chest 160:1693–1703. https://doi.org/10.1016/j.chest.2021.05.066
Teijeiro-Paradis R, Tiwari P, Spriel A, Del Sorbo L, Fan E (2021) Standardized liberation trials in patients with COVID-19 ARDS treated with venovenous extracorporeal membrane oxygenation: when ready, let them breathe! Intensive Care Med 47:1494–1496. https://doi.org/10.1007/s00134-021-06523-x
Belliato M, Cremascoli L, Epis F et al (2021) Carbon dioxide elimination during veno-venous extracorporeal membrane oxygenation weaning: a pilot study. ASAIO J 67:700–708. https://doi.org/10.1097/MAT.0000000000001282
Al-Fares AA, Ferguson ND, Ma J, Cypel M, Keshavjee S, Fan E et al (2021) Achieving safe liberation during weaning from V–V ECMO in patients with severe ARDS: the role of tidal volume and inspiratory effort. Chest 160:1704–1713. https://doi.org/10.1016/j.chest.2021.05.068
Lazzari S, Romitti F, Busana M, Vassalli F, Bonifazi M, Macrí MM et al (2022) End-tidal to arterial PACO2 ratio as guide to weaning from veno-venous extra-corporeal membrane oxygenation. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.202201-0135OC
Ficial B, Vasques F, Zhang J, Whebell S, Slattery M, Lamas T et al (2021) Physiological basis of extracorporeal membrane oxygenation and extracorporeal carbon dioxide removal in respiratory failure. Membranes (Basel) 11:225. https://doi.org/10.3390/membranes11030225
Karagiannidis C, Strassmann S, Brodie D, Ritter P, Larsson A, Borchardt R, Windisch W (2017) Impact of membrane lung surface area and blood flow on extracorporeal CO2 removal during severe respiratory acidosis. Intensive Care Med Exp 5:34. https://doi.org/10.1186/s40635-017-0147-0
Duscio E, Cipulli F, Vasques F, Collino F, Rapetti F, Romitti F, Behnemann T, Niewenhuys J, Tonetti T, Pasticci I, Vassalli F, Reupke V, Moerer O, Quintel M, Gattinoni L (2019) Extracorporeal CO2 removal: the minimally invasive approach, theory, and practice. Crit Care Med 47:33–40. https://doi.org/10.1097/CCM.0000000000003430
Marshall BE, Marshall C (1985) A model for hypoxic constriction of the pulmonary circulation. J Appl Physiol 1988(64):68–77. https://doi.org/10.1152/jappl.1988.64.1.68
Bishop MJ, Cheney FW (1983) Effects of pulmonary blood flow and mixed venous O2 tension on gas exchange in dogs. Anesthesiology 58:130–135. https://doi.org/10.1097/00000542-198302000-00005
Domino KB, Wetstein L, Glasser SA, Lindgren L, Marshall C, Harken A, Marshall BE (1983) Influence of mixed venous oxygen tension (PVO2) on blood flow to atelectatic lung. Anesthesiology 59:428–434. https://doi.org/10.1097/00000542-198311000-00012
Tarry D, Powell M (2017) Hypoxic pulmonary vasoconstriction. BJA Educ 17:208–213. https://doi.org/10.1093/bjaed/mkw076
Sinha P, Calfee CS, Beitler JR, Soni N, Ho K, Matthay MA et al (2019) Physiologic analysis and clinical performance of the ventilatory ratio in acute respiratory distress syndrome. Am J Respir Crit Care Med 199:333–341. https://doi.org/10.1164/rccm.201804-0692OC
Suarez-Sipmann F, Villar J, Fernando C, Sanchez-Giralt JA, Tusman G (2021) Monitoring expired CO2 kinetics to individualize lung-protective ventilation in patients with the acute respiratory distress syndrome. Front Physiol 12:785014. https://doi.org/10.3389/fphys.2021.785014
Bonifazi M, Romitti F, Busana M, Palumbo MM, Steinberg I, Gattarello S et al (2021) End-tidal to arterial PCO2 ratio: a bedside meter of the overall gas exchanger performance. Intensive Care Med Exp 9:21. https://doi.org/10.1186/s40635-021-00377-9
Gillon SA, Barrett NA, Ioannou N, Camporota L, Victor K, Gowland A et al (2016) Intracardiac right-to-left shunt impeding liberation from veno-venous extracorporeal membrane oxygenation: two case studies. Crit Care Med 44:e583–e586. https://doi.org/10.1097/CCM.0000000000001619
Gattinoni L, Coppola S, Camporota L (2022) Physiology of extracorporeal CO2 removal. Intensive Care Med 48:1322–1325. https://doi.org/10.1007/s00134-022-06827-6
Cipriani E, Langer T, Bottino N, Brusatori S, Carlesso E, Colombo SM et al (2020) Key role of respiratory quotient to reduce the occurrence of hypoxemia during extracorporeal gas exchange: a theoretical analysis. Crit Care Med 12:e1327–e1331. https://doi.org/10.1097/CCM.0000000000004619
Dickstein ML (2020) Extracorporeal CO2 removal and the alveolar gas equation. Am J Respir Crit Care Med 1(202):1057–1058. https://doi.org/10.1164/rccm.202005-1609LE
Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D (2020) Respiratory drive in critically ill patients. Pathophysiology and clinical implications. Am J Respir Crit Care Med 201:20–32. https://doi.org/10.1164/rccm.201903-0596SO
Spinelli E, Mauri T, Beitler JR, Pesenti A, Brodie D (2020) Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med 46:606–618. https://doi.org/10.1007/s00134-020-05942-6
Asmussen E, Nielsen M (1957) Ventilatory response to CO2 during work at normal and at low oxygen tensions. Acta Physiol Scand 39:27–35. https://doi.org/10.1111/j.1748-1716.1957.tb01406.x
Haouzi P (2022) Revisiting the effects of the reciprocal function between alveolar ventilation and CO2 partial pressure (PACO2) on PACO2 homeostasis at rest and in exercise. J Appl Physiol (1985). https://doi.org/10.1152/japplphysiol.00058.2022
Spinelli E, Mauri T, Lissoni A, Crotti S, Langer T, Albanese N et al (2020) Spontaneous breathing patterns during maximum extracorporeal CO2 removal in subjects with early severe ARDS. Respir Care 65:911–919. https://doi.org/10.4187/respcare.07391
Yoshida T, Fujino Y, Amato MBP, Kavanagh BP (2017) Fifty Years of Research in ARDS. Spontaneous breathing during mechanical ventilation. Risks, mechanisms, and management. Am J Respir Crit Care Med 195:985–992. https://doi.org/10.1164/rccm.201604-0748CP
Briscoe WA, Dubois AB (1958) The relationship between airway resistance, airway conductance and lung volume in subjects of different age and body size. J Clin Invest 37:1279–1285. https://doi.org/10.1172/JCI103715
Jansen D, Jonkman AH, de Vries HJ, Wennen M, Elshof J, Hoofs MA et al (2021) Positive end-expiratory pressure affects geometry and function of the human diaphragm. J Appl Physiol (1985) 131(4):1328–1339. https://doi.org/10.1152/japplphysiol.00184.2021
Forster HV, Haouzi P, Dempsey JA (2012) Control of breathing during exercise. Compr Physiol 2:743–777. https://doi.org/10.1002/cphy.c100045
Giosa L, Busana M, Bonifazi M, Romitti F, Vassalli F, Pasticci I et al (2021) Mobilizing carbon dioxide stores. An experimental study. Am J Respir Crit Care Med 203:318–327. https://doi.org/10.1164/rccm.202005-1687OC
Dres M, Demoule A (2020) Monitoring diaphragm function in the ICU. Curr Opin Crit Care 26(1):18–25. https://doi.org/10.1097/MCC.0000000000000682
Sato R, Hasegawa D, Hamahata NT, Narala S, Nishida K et al (2021) The predictive value of airway occlusion pressure at 100 msec (P0.1) on successful weaning from mechanical ventilation: a systematic review and meta-analysis. J Crit Care 63:124–132. https://doi.org/10.1016/j.jcrc.2020.09.030
Kassis EB, Talmor D (2021) Clinical application of esophageal manometry: how I do it. Crit Care 25:6. https://doi.org/10.1186/s13054-020-03453-w
Bertoni M, Telias I, Urner M, Long M, Del Sorbo L, Fan E et al (2019) A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit Care 23:346. https://doi.org/10.1186/s13054-019-2617-0
Abrams D, Schmidt M, Pham T, Beitler JR, Fan E, Goligher EC et al (2020) Mechanical ventilation for acute respiratory distress syndrome during extracorporeal life support: research and practice. Am J Respir Crit Care Med 201:514–525
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O et al (2016) Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 42:1567–1575. https://doi.org/10.1007/s00134-016-4505-2
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372:747–755. https://doi.org/10.1056/NEJMsa1410639
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM et al (2018) Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med 44:1914–1922
Romitti F, Busana M, Palumbo MM, Bonifazi M, Giosa L, Vassalli F et al (2022) Mechanical power thresholds during mechanical ventilation: an experimental study. Physiol Rep 10:e15225. https://doi.org/10.14814/phy2.15225
Neto AS, Schmidt M, Azevedo LCP, Bein T, Brochard L, Beutel G et al (2016) Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: a pooled individual patient data analysis: mechanical ventilation during ECMO. Intensive Care Med 42:1672–1684. https://doi.org/10.1007/s00134-016-4507-0
Chiu LC, Lin SW, Chuang LP, Li HH, Liu PH, Tsai FC et al (2021) Mechanical power during extracorporeal membrane oxygenation and hospital mortality in patients with acute respiratory distress syndrome. Crit Care 25:13. https://doi.org/10.1186/s13054-020-03428-x
Del Sorbo L, Goffi A, Tomlinson G, Pettenuzzo T, Facchin F, Vendramin A et al (2020) Effect of driving pressure change during extracorporeal membrane oxygenation in adults with acute respiratory distress syndrome: a randomized crossover physiologic study. Crit Care Med 48:1771–1778. https://doi.org/10.1097/CCM.0000000000004637
Goligher EC, Jonkman AH, Dianti J, Vaporidi K, Beitler JR, Bhakti K et al (2020) Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med 46:2314–2326. https://doi.org/10.1007/s00134-020-06288-9
Vassalli F, Pasticci I, Romitti F, Duscio E, Aßmann J, Grünhagen H et al (2020) Does iso-mechanical power lead to iso-lung damage? An experimental study in a porcine model. Anesthesiology 132:1126–1137. https://doi.org/10.1097/ALN.0000000000003189
Bellani G, Grasselli G, Teggia-Droghi M, Mauri T, Coppadoro A, Brochard L et al (2016) Do spontaneous and mechanical breathing have similar effects on average transpulmonary and alveolar pressure? A clinical crossover study. Crit Care 20:142. https://doi.org/10.1186/s13054-016-1290-9
Shi ZH, Jonkman A, de Vries H, Jansen D, Ottenheijm C, Girbes A et al (2019) Expiratory muscle dysfunction in critically ill patients: towards improved understanding. Intensive Care Med 45:1061–1071. https://doi.org/10.1007/s00134-019-05664-4
Chandra A, Coggeshall JW, Ravenscraft SA, Marini JJ (1994) Hyperpnea limits the volume recruited by positive end-expiratory pressure. Am J Respir Crit Care Med 150:911–917. https://doi.org/10.1164/ajrccm.150.4.7921462
Yoshida T, Amato MBP, Grieco DL, Chen L, Lima CAS, Roldan R et al (2018) Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med 197:1018–1026. https://doi.org/10.1164/rccm.201709-1806OC
Sang L, Zhao Z, Yun PJ, Frerichs I, Möller K, Fu F et al (2020) Qualitative and quantitative assessment of pendelluft: a simple method based on electrical impedance tomography. Ann Transl Med. 8:1216. https://doi.org/10.21037/atm-20-4182
Morais CCA, Koyama Y, Yoshida T, Plens GM, Gomes S, Lima et al (2018) High positive end-expiratory pressure renders spontaneous effort noninjurious. Am J Respir Crit Care Med 197:1285–1296. https://doi.org/10.1164/rccm.201706-1244OC
Mauri T, Langer T, Zanella A, Grasselli G, Pesenti A (2016) Extremely high transpulmonary pressure in a spontaneously breathing patient with early severe ARDS on ECMO. Intensive Care Med 42:2101–2103. https://doi.org/10.1007/s00134-016-4470-9
Acknowledgements
All figures created using Biorender. Figure 1 adapted from a template created by Dr. Yevgeniy Brailovsky from Sidney Kimmel School of Medicine.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the text. PC formulated the figures with input from co-authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This narrative review did not require ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Collins, P.D., Giosa, L., Camarda, V. et al. Physiological adaptations during weaning from veno-venous extracorporeal membrane oxygenation. ICMx 11, 7 (2023). https://doi.org/10.1186/s40635-023-00493-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-023-00493-8