Abstract
Recent advances in veno-arterial (VA) and veno-venous (VV) extracorporeal membrane oxygenation (ECMO) technology and management have enabled us to support patients with cardiac and/or pulmonary failure, who may have previously been considered untreatable. VA ECMO and VV ECMO are by definition transient therapies and serve as a bridge to recovery, bridge to decision, bridge to transplant, or bridge to no recovery. Weaning ECMO should be considered for all patients once native cardiac and pulmonary function show signs of recovery. Currently, there are no universally accepted protocols for weaning VA and VV ECMO, and consequently, each individual center follows their own weaning protocols. The aim of this review article is to describe different approaches to safely wean from VA and VV ECMO.
Similar content being viewed by others
Veno-arterial ECMO
Overview
Veno-arterial extracorporeal membrane oxygenation (VA ECMO) is a powerful tool that now enables us to rescue many patients in cardiopulmonary extremis and potentially stabilize clinical situations that may have previously been considered unrecoverable. Indications for VA ECMO include, but are certainly not limited to, refractory cardiogenic shock, post cardiotomy shock, cardiac arrest (extracorporeal cardiopulmonary resuscitation (eCPR)), acute myocardial infarction with ventricular dysfunction, malignant arrhythmias, massive pulmonary embolism, and severe pulmonary hypertensive crisis. Previous cardiac surgical emergencies like post-infarct ventricular septal defect (VSD), acute severe mitral regurgitation, and cardiogenic shock secondary to severe aortic stenosis can also be temporized with VA ECMO to allow patient stabilization prior to definitive repair. Discussions regarding initiation of ECMO are intertwined with considerations for what the potential exit strategy may be for weaning off this form of temporary support. This typically falls into 3 main categories: “bridge to recovery,” “bridge to decision or intervention,” and “bridge to transplant or other advanced heart replacement therapy” (Fig. 1). Relative contraindications to ECMO support can be based on patient factors and/or anatomic considerations and are typically based on identifying those unlikely to obtain substantial benefit and low likelihood of being able to come off this temporary support either to recovery or transition to a more durable option. Patient factors which can be associated with worse prognosis with ECMO include advanced age, prolonged downtime, multiple medical comorbidities, poor functional status prior, malignancy, or other untreatable illnesses. Anatomic factors like poor vasculature make peripheral cannulation less likely to be readily achieved and associated with more peripheral limb complications and valvular disease such as aortic regurgitation can provide extremes of left ventricular (LV) loading and limit the ability to provide effective support.
Patient optimization prior to weaning
Optimizing the patient as much as possible prior to any planned decannulation is paramount. Many of the same factors or considerations when weaning from cardiopulmonary bypass are relevant, but we have a little more time to reach some of the targets. Treating underlying pathologies, that may be intervenable, prior to decannulation is first and foremost. VA ECMO provides an additional level of stability for these high-risk patients to undergo procedures including percutaneous coronary intervention (PCI), transcatheter aortic valve replacement (TAVR), electrophysiologic ablations for ventricular or atrial tachyarrhythmias, endovascular pulmonary embolectomies, and definitive surgical repairs. Many patients may not need or be candidates for these larger procedures, but more typical things like reestablishing sinus rhythm, if possible, loading anti-arrhythmics, optimizing volume status, and allowing recovery of other end-organ function can help to achieve successful decannulation. Particularly for patients with right ventricular dysfunction, volume status can be critical and the stability of ECMO support can provide time for significant diuresis or dialysis to achieve these optimal levels. Akin to the optimization of fluid status and volume removal, we also use the time on ECMO to try to normalize other lab abnormalities. Avoiding large administration of fluid or blood products post decannulation is also important to improve one’s chances of successful decannulation. While transfusion goals can be controversial, patients with unrevascularizable coronary disease, or marginal central venous saturation, may benefit from higher starting hemoglobin levels and we often aim to achieve a hemoglobin close to 10 mg/dl prior to decannulation in these patients and can often balance the administration of that extra volume with diuresis or dialysis prior to decannulation. Additional procedures such as bronchoscopy to improve pulmonary function or necessary line changes prior to decannulation are also often preferred to occur prior to planned decannulation to again have the additional stability of ECMO during this procedure. The risks of being anticoagulated and on ECMO also has to be considered and balanced in making these care management plans.
VA ECMO weaning trials
There are many different approaches and schools of thought which can be implemented during ECMO weaning (Fig. 2). ECMO speed and resultant flows can be gradually decreased on a daily or multiple times a day basis, as clinically appropriate, although leaving patients on lower flows for prolonged period of times could potentially increase risk of thrombus formation in oxygenator and circuit. Decreasing flows can at times be helpful to further reduce afterload on the ventricle and also reduce the incidence of chatter in patients with particularly acute ventricular dysfunction; you can often see the continuing increase in pulsatility of arterial line tracings as the heart is recovering. This can also be further confirmed with echocardiographic assessment. Regular echocardiograms can be quite valuable in determining when it may be appropriate to start looking towards decannulation. True ventricular function, however, can be difficult to assess if the ventricles are not adequately loaded. We typically perform turn down studies with echocardiographic assessment as we are getting closer to possible decannulation. These trials try to assess if patients are likely to be able to come off support successfully, both for prognosticating if there are no further support options, but also to assess if going directly to other advanced therapies is more appropriate, if they are an option. Preferably, turn down studies are performed when the patient is adequately anticoagulated so that flows can be reduced to 500 ml/min to 1 l/min for short periods of time without substantial risk to the patient or circuit. Echocardiographic images are obtained at the different levels of flow, i.e., 3 L per minute (LPM), 2LPM, 1LPM, and the corresponding vitals, filling pressures (central venous pressure — CVP, pulmonary artery pressure — PAP), and blood gases can also be obtained. Substantial decreases in blood pressure and corresponding increases in CVP or PA diastolic are unlikely to portend successful decannulation. Often, additional inotropic support may be added prior to an attempted wean, but there is also some hesitation in increasing support too much, particularly in patients that may have previously been prone to arrhythmias, or where significant escalation is needed acutely to maintain hemodynamics, which may suggest that the patient is not yet ready for decannulation. The frequency and urgency of weaning trials may also be driven by the patient’s stability on ECMO and possible complications they may be having, which may push to decannulate sooner rather than later in balancing the individual clinical situation and risks. Cardiac function certainly does not have to be fully recovered to proceed to decannulation, but it should at least be adequate to support the patient without the ECMO support and potentially with the addition of other adjunct medications and devices which may have a different risk profile.
Additional mechanical options to facilitate weaning off ECMO
Transitioning to another form of temporary mechanical support to have more time to recover and assess the patient’s ultimate support needs is also quite common with VA ECMO. As most are placed peripherally in the femoral groin vessels, there is a fair bit of hesitation to ambulate these patients, although there is data for safe ambulation in this cannulation strategy for both VA ECMO and VV ECMO with femoral cannulae [1]. Switching to upper body–based devices, including axillary Impella 5.5 and Protek duo cannulae, offers potential transition strategies for ongoing support. We utilize Impella 5.5 in patients on VA ECMO when LV venting is necessary (we use PA diastolic pressure > 20–25 mmHg and echocardiographic findings of LV dilatation and decreased aortic valve opening as an indication for LV unloading) and/or if we feel that LV support will be needed after discontinuing ECMO. This can help decrease the duration of the ECMO run. We routinely insert the Impella 5.5 device through the right axillary artery, after sewing a 10-mm graft. This also allows patients to potentially ambulate after they have come off VA ECMO. Furthermore, we have successfully transitioned patients with severe biventricular failure, from VA ECMO to Impella 5.5 and Protek Duo right ventricular assist device (RVAD). Patients with biventricular failure and multi-organ failure, who are not candidates for heart transplantation, are by definition extremely ill and weaning them from ECMO to peripheral biventricular assist devices (Bi-VADs) sometimes can be challenging. We prefer to stabilize these patients on ECMO, allow for the right ventricle (RV) to recover, and then attempt to wean. If not possible, and continued biventricular support is needed, we then proceed with peripheral or central extracorporeal VADs.
When LV venting is needed, we almost in every case insert an Impella 5.5 through a 10-mm graft sewn onto the right axillary artery. As previously mentioned, the Impella will also aid in ECMO weaning and continued support and LV unloading after discontinuing ECMO therapy. In rare instances, if an Impella cannot be inserted, we use an intra-aortic balloon pump (IABP) for unloading. If LV venting is needed in central ECMO with open chests, we place an LV vent in the right superior pulmonary vein and Y it into the ECMO circuit. We have also successfully used left atrial veno-arterial (LAVA) ECMO with the Tandem Heart for patients in cardiogenic shock secondary to acute aortic regurgitation.
An IABP can also be placed peri-decannulation, as it is the least invasive mechanical support that can usually be initiated, but as importantly, it can be readily removed at the bedside in an awake patient. The addition of a balloon pump can help augment the blood pressure, coronary perfusion, and some cardiac output in the peri-decannulation period and abate some of the potential hemodynamic effects of associated anesthesia, intubation, etc. This is obviously less helpful in patients with aortic insufficiency and is done with caution in patients with peripheral or aortic vascular disease. These can be placed at the time of decannulation, or in the days prior, as another tool to use in assessing the appropriateness for ECMO removal.
Transitioning a patient from VA ECMO to durable left ventricular assist device (LVAD) is usually not necessary and should be avoided, if possible, owing to overall poor short- and long-term LVAD outcomes. If a patient is on VA ECMO and only has LV failure, our preference is to transition to an Impella 5.5. If biventricular failure is present, a Protek Duo cannula can be utilized for RV support, in addition to the Impella. This allows us to assess a patient’s response to LV unloading and also evaluate the RV tolerance to a LVAD. It can also aid in optimizing a patient’s metabolic homeostasis and hematologic profile, in preparation for a durable LVAD. Furthermore, it gives us time to evaluate the patient’s candidacy and appropriateness for long-term LVAD therapy (right heart catheterization parameters, valvular function, appropriate psychosocial support, patient reliability, finances, etc.).
Palliative care
Communication and interactions with the patients and their families are also a critical part of ECMO support, and even more so when determining next steps and discontinuation of support is being considered. We minimize sedation on intubated patients on ECMO, as much as possible, and work to extubate patients as appropriate, which further allows us to be able to interact and communicate with them. This can be extremely important in assessing their potential candidacy and interest in pursuing advanced therapies like transplant and LVAD. We also use these opportunities to have discussions with the patients and their healthcare proxies about important medical decisions, if they are not able to speak for themselves at other points in their care. Regular meetings with the critical care, medical and surgical teams, and palliative care provide important updates to the families and reinforces the short-term nature of the ECMO support and risks associated with remaining on support, while discussing potential next steps. In patients that have no other potential outs from temporary ECMO support, we have very frank discussions prior to decannulation to set the expectation if the patient does not do well and starts to deteriorate after decannulation and that ECMO support would not be reinitiated, given there is no potential out from this situation (“bridge to nowhere”). In recent years, with our growing experience of VA ECMO in adult patients and the availability of easily placed percutaneous devices that can reliably support both ventricles with flows > 4–5 l, multiple VA ECMO runs have become uncommon. In our experience, if patients are truly ready to be weaned off ECMO, if the underlying etiology of shock has been treated or optimized and patients are not “forced” off ECMO during their weaning trial, it is very unlikely that a second ECMO run would be necessary. Essentially, this can be avoided when patients and ECMO are appropriately managed during the first run. As already mentioned, the availability of extracorporeal biventricular mechanical support, mainly Impella 5.5, has certainly alleviated the need for second VA ECMO runs. Recurrence of shock, after coming off ECMO the first time, may also imply that the patient was not an appropriate candidate for VA ECMO in the first place and that VA ECMO therapy is futile. Compassionate use of second-run VA ECMO is sometimes difficult to refuse, but the outcomes are dismal, with mortality rates > 60–70%. These can be very difficult conversations to have and often the weaning trials discussed above can be informative to guide our discussions in how likely we think the patient may be able to tolerate the decannulation. In patients that are fully dependent on ECMO support and have no further options, discussions of discontinuing support are obviously very difficult but important aspect of understanding both the power and limitations of this support and potential to prolong a situation, where there is no exit strategy.
Another controversial topic is the optimal duration of VA ECMO in post cardiotomy cardiogenic shock. We feel that the decision to continue or discontinue VA ECMO on post cardiotomy shock should not be duration driven, but rather depends on whether there is a pathway to recovery. Obviously, the sooner a patient can be weaned off VA ECMO, the better. The purpose of post cardiotomy shock VA ECMO is to get the patient out of the operating room (OR), to re-assess, allow the heart to recover, and eventually be able to close the sternotomy. Once the chest is closed, if the patient is still in cardiogenic shock/ongoing ventricular failure, we make every attempt to transition ECMO to percutaneous VADs. When hospitals do not offer advanced surgical heart failure therapies, post cardiotomy shock on VA ECMO patients should be transferred to more experienced institutions with such options. The time to discontinue VA ECMO for futility is when patients go into multi-organ failure and/or there is no chance of cardiac function recovery and there are no options for durable LVAD or heart transplantation.
ECMO decannulation
The actual mechanics of ECMO decannulation depends on the patient, the cannulation strategy, and many other factors. Once the weaning trials look promising, or if the clinical situation otherwise pushes us towards decannulation, we proceed with plans for decannulation. We do not stop anticoagulation during ECMO weaning. We will continue heparin infusion as we assess the patient in the OR off ECMO, while maintaining ECMO circulation after connecting the arterial and venous limbs. We also allow the cannulae to bleed every 2 min, so that they do not clot either. We discontinue VA ECMO in the OR, under transesophageal echocardiography (TEE) guidance and usually stay in the OR for about an hour as we assess LV/RV contractility, ventricular unloading, and aortic valve opening. We also check blood pressure, venous oxygen saturation (SvO2), lactate, and Swan-Ganz numbers. If all parameters are acceptable with the patient off ECMO for an hour, we proceed with decannulation. We routinely proceed with a cutdown and primary repair of the artery. Direct cutdowns can be of varying complexity depending on the location of vascular access, the cannula size, and femoral anatomy. In general, we prefer to cannulate the femoral artery and vein on different sides. If the same side vein is cannulated, we also primarily repair the vein. If the venous cannula is on the contralateral side, we pull the cannula and close the skin with a figure of eight stitch and then hold pressure for 10–15 min. Only after the patient is decannulated do we reverse heparin with protamine. With this strategy, we rarely see hemorrhagic or thrombotic complications. In a similar fashion, in patients with central cannulation, we administer protamine after decannulation.
The closure of these wounds can also be challenging as often the skin surrounding the cannulae may not be entirely intact. The wounds are copiously irrigated after decannulation and vessel repair and then closed meticulously in layers to provide as much coverage as possible over the vessels. The options for the skin closure can vary depending on the quality of the tissues and skin, and have included typical subcuticular closure with interrupted monofilament absorbable sutures or staples, or a negative pressure wound vacuum to the deep dermal layers. The former cannula tracts are often packed and can be later included in wound vacuum dressing when and if appropriate. It is imperative to closely watch these incisions, particularly in the groin, because they can be susceptible to breakdown in these ill and malnourished patients. We have found better success with healing of the oblique incisions above the crease, rather than the vertical incisions crossing the crease, if possible.
Other closure approaches include pre-closing arterial cannula access with Perclose devices and leaving loose sutures secured while the patient is on support, or just deploying these devices at the time of decannulation [2], or newer large bore closure systems like Manta [3]. These can obviously have the advantage of obviating the need for an open surgical procedure, but Percloses left in places for longer periods of times may increase risk of infection and bleeding from the sites, while the patients are on support.
For patients who go directly to LVAD or transplant from their VA ECMO support, or even a definitive cardiac surgery such as valve repair/replacement and VSD closure, we will often utilize the same cannulae for cardiopulmonary bypass, often with an additional central venous cannula for bicaval cannulation and potentially another aortic cannula. Once the patients are successfully weaned off cardiopulmonary bypass (CPB) and do not appear that they will need support after, we can then proceed to cutdown and remove the femoral cannulae.
Veno-venous ECMO
Overview
Since its inception in the early 1970s, veno-venous extracorporeal membrane oxygenation (VV ECMO) has been a boon to countless patients in respiratory failure [4]. However, in recent years, questions have arisen regarding the appropriate application of this resource-intensive therapy for maximum patient benefit, in the context of increasing pressure on healthcare systems, while optimizing the risk–benefit equilibrium for patients. These concerns have only been intensified with the onset of the global Corona Virus Disease-19 (COVID-19) pandemic, beginning in early 2020, spurred by soaring ECMO demand in the setting of skyrocketing numbers of patients in extremis secondary to COVID-19 acute respiratory distress syndrome (ARDS). Suddenly, questions of who should receive ECMO and for how long, in intensive care units (ICUs), where demand far outstripped supply, took on a fresh urgency.
According to the Extracorporeal Life Support Organization (ELSO), which maintains the world’s largest ECMO database, data shows that since its inception in 1989, 46,523 adult VV ECMO patients have been submitted to the registry, with an overall survival of 58% [5]. In 2019, there was increased speculation that ECMO utilization had reached its ceiling due to the resource constraints required. For the first time since 2008, the number of total cases and reporting centers decreased, from 13,394 cases and 435 centers in 2018 to 12,850 cases and 430 centers in 2019. Unfortunately, the COVID-19 pandemic arrived in 2020 and revealed in no uncertain terms that systems still had capacity for ECMO expansion, resulting in a sharp ascent of VV ECMO utilization. The latest year for which data was available was 2021 and showed a combined (all forms of ECMO including neonatal, pediatric, and adult cases) total of 17,777 runs reported at 543 ECMO centers. As expected, due to the magnitude and severity of the COVID-19 pandemic, ECMO survival in this population is significantly lower, with the most current data showing an in-hospital mortality of 47% out of 14,166 confirmed COVID-19 ECMO cases, 94% of whom were given veno-venous support [6].
Patient selection
Although the focus of this review is ECMO “weaning,” much of that attendant strategy begins with patient selection and their pre-ECMO disease process and comorbidities. The last 15 years have seen a number of trials which have both stoked excitement regarding VV ECMO as a heroic therapy, but have also offered cautionary tales regarding factors which predispose patients to poor outcomes and provided guidance on patient selection. Chief among these were the Conventional Ventilatory Support vs Extracorporeal Membrane Oxygenation Severe Adult Respiratory Failure (CESAR) and Extracorporeal Membrane Oxygenation to Rescue Lung Injury in Severe Acute Respiratory Distress Syndrome (EOLIA) trials. Published in 2009, the CESAR trial enrolled 180 patients in the UK and randomized them to early referral for consideration of ECMO within 7 days of mechanical ventilation versus standard medical therapy. While questions of patient crossover and inconsistent management of ventilator settings and pressures dogged the study, this focus on early ECMO referral resulted in significantly improved survival in the ECMO group, with a 6-month survival in the ECMO group of 63% compared to that of 47% in the group randomized to medical management [7].
The French EOLIA trial enrolled 249 patients randomized to either early ECMO or standard medical therapy, with the option for salvage ECMO in the case of deterioration, and sought to clarify some of the questions born out of the CESAR trial. The trial established strict inclusion criteria into the ECMO group and, like the CESAR trial, focused on early ECMO referral (less than 7 days), postulating that reducing ventilator-induced trauma would portend better outcomes. Regrettably, the trial stopped prematurely because the difference between the groups did not reach statistical significance regarding the primary endpoint of 60-day mortality. However, the interim analysis showed a clear trend towards improved primary endpoint outcomes in the ECMO group vs. the standard therapy group, with 65% vs. 54% 60-day survival, respectively (p = 0.09). There was also significant crossover from the medical management group to the ECMO group, likely further preventing the full realization of ECMO benefit [8]. Importantly, the trial established clear inclusion criteria which are the bedrock of the selection criteria at the author’s institution and are at the heart of the recent ELSO guidelines on patient selection. These are summarized as published in the ASAIO Journal in (Fig. 3) [9]:
Algorithm for management of acute respiratory distress syndrome, including indications for ECMO. With respiratory rate increased to 35 breaths per minute and mechanical ventilation settings adjusted to keep a plateau airway pressure of < 32 cm H2O. †Consider neuromuscular blockade. ‡There are no absolute contraindications that are agreed upon except end-stage respiratory failure when lung transplantation will not be considered; exclusion used in the EOLIA trial can be taken as a conservative approach to ECMO contraindications. ∫For example, neuromuscular blockade, high PEEP strategy, inhaled pulmonary vasodilators, recruitment maneuvers, and high-frequency oscillatory ventilation. ¶Recommend early ECMO as per EOLIA trial criteria; salvage ECMO, which involves deferral of ECMO initiation until further decompensation (as in the crossovers to ECMO in the EOLIA control group), is not supported by the evidence but might be preferable to not initiating ECMO at all in such patients. Credit: Abrams et al. ECMO, extracorporeal membrane oxygenation; EOLIA, Extracorporeal Membrane Oxygenation to Rescue Lung Injury in Severe Acute Respiratory Distress Syndrome; PaCO2, partial pressure of carbon dioxide in arterial blood; PaO2:FiO2, ratio of partial pressure of oxygen in arterial blood to the fractional concentration of oxygen in inspired air; PEEP, positive end-expiratory pressure.6
It is important to note that at the author’s center, in line with the recommendations of major societies, there have been no hard exclusion criteria beyond that of devastating neurologic injury or disseminated, incurable malignancy. Rather, we have adopted an inclusive, multidisciplinary approach which takes into account the patients’ entire clinical picture. Body mass index (BMI) and age, two frequent disqualifiers at many centers, are examined in the context of comorbidities and functional status, as recent data supports the notion that class III obesity (BMI > 40 kg/m2) have comparable outcomes to less obese patients and should not be precluded from ECMO consideration [10]. This seems to be especially true in the COVID-19 VV ECMO population. Obviously, it is incumbent on the ECMO center to ensure that selection criteria match their available resources.
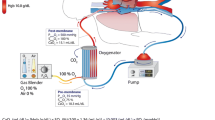
While the technical considerations and management strategies of VV ECMO are beyond the scope of this paper, it is appropriate to comment briefly on our approach. We use a multidisciplinary approach to patient selection, generally consisting of pulmonology, ICU, and cardiac surgery attending physicians. Venous access is typically placed in both the right internal jugular and one of the femoral veins under ultrasound guidance at the first inkling of ECMO candidacy. This allows for expeditious commencement of ECMO therapy if inclusion criteria are met, which is in keeping with the findings of the CESAR and EOLIA trials, which support improved outcomes with early ECMO initiation. Increasingly, we have also been adopting the increased use of dual lumen cannulae, when expertise and fluoroscopy availability allow. This improves ambulation and rehabilitation opportunities are important in all patients, but especially crucial in transplant candidates [11]. Regarding management strategies, our center adheres to the standard protocols recommended by ELSO, including anticoagulation targets, regardless of COVID-19 status [12].
Central to the discussion surrounding ECMO initiation is a clear and frank discussion with the patient’s family and surrogates regarding endpoints and expectations. There must be agreement that once ECMO therapy is initiated, a reasonable amount of time must be allotted for the efficacy of therapy to declare itself. Barring any major status changes, we make these multidisciplinary assessments and updates with the family on at least a weekly basis. Conversely, it is made clear to the patient’s decision makers that if at any time, ECMO is determined to be futile that it will be discontinued. Also, family must be willing for early tracheostomy and percutaneous endoscopic gastrostomy (PEG) tube insertion, allowing for sedation wean and improved pulmonary toilet. Although a non-transplant site should not automatically disqualify a bridge to transplant ECMO patients, discussions with lung transplant centers should begin early in the ECMO course, preferably prior to cannulation. Discontinuation of ECMO therapy must be agreed upon, if the patient is initiated on ECMO as a presumed bridge to transplant or bridge to decision patient, but is subsequently found not to be a transplant candidate. Our institution has also found the early inclusion of the palliative care service as invaluable in navigating these discussions [13, 14].
Weaning from veno-venous (VV) ECMO
VV ECMO therapy by definition is transient and serves as a bridge to recovery. Additionally, for a subset of patients with end-stage lung disease, VV ECMO can be utilized as a bridge to lung transplant, until the patient’s condition allows for listing and/or until a suitable organ becomes available [15]. Weaning from VV ECMO should be considered for patients as soon as the native lungs show signs of recovery. This usually occurs when lung compliance and gas exchange improve and can also coincide with improvement in radiological findings. Currently, there are no universally accepted protocols for weaning VV ECMO. Consequently, each individual center follows their own weaning process.
Weaning for bridge to recovery
Treating the underlying cause of lung failure is the first step in the weaning process. Prior to weaning, it is also critical to prevent and manage multi-organ failure and other ECMO-related complications. Furthermore, patients should be close to their dry weight or at least euvolemic, which usually can be achieved with appropriate fluid balance management and diuretic therapy.
At our institution, we favor keeping flows higher (generally > 3.5–4 l/min) and preferentially wean the sweep off gradually with compensatory ventilator support changes. As the sweep gas is weaned, we establish a consensus regarding acceptable pH, partial pressure of oxygen (PaO2), and partial pressure of carbon dioxide (PaCO2) parameters. In general, we accept pH ≥ 7.30. We consider CO2 clearance as a more important marker of native lung recovery than oxygenation. We aim to maintain plateau pressures < 30 mmHg, in order to avoid barotrauma. When the sweep is off, arterial blood gases (ABGs) are checked every 1–2 h for at least 8–12 h or for 24 h, when patients are coming off longer ECMO runs. If a patient is able to tolerate no sweep gas for 12 h, based on ABGs, lung compliance, and work of breathing, VV ECMO is discontinued. It is advantageous to also consider performing a bronchoscopy the day of decannulation to ensure that retained secretions do not create a significant problem after decannulation.
Few centers around the world have reported their approach for weaning from VV ECMO. The Karolinska Institute [16] has described assessing readiness to wean by adding CO2 to the sweep gas, when the sweep gas has been reduced to 2 l/min. The ability of the native lung to clear CO2 is assessed by comparing pre and post oxygenator ABGs. When the pCO2 difference is less than 3 mmHg, the patient is considered equilibrated, which means the membrane is neither clearing nor adding CO2 and the patient’s native lungs are essentially able to clear the CO2 that is produced. At that point, the sweep gas is turned off overnight. If ABGs are appropriate, ECMO is discontinued and the patient is decannulated. At the University Hospital Regensburg [13] in Germany, the ECMO flow is stepwise reduced to 1.5 l/min and the sweep is tapered in parallel to the pump flow and then turned off for 60 min. If gas exchange remains stable, the patient is decannulated. The ECMO center at San Raffaele Hospital in Italy has reported reducing their ECMO flows to 2.5–3 l and then gradually tapering the sweep gas and fraction of inspired oxygen (FiO2) to off [16].
The ESLO has also published guidelines for weaning VV ECMO [5]. They recommend a stepwise reduction in fraction of delivered O2 (FDO2) from 1.0 to 0.21 in decrements of 20%, followed by reduction in sweep gas flow by 0.5–1 l/min to a goal of 1 l/min. Concomitantly, adjustments are made to the ventilator by gradually increasing tidal volumes to 6 ml/kg or inspiratory pressures to no more than 28 cm H2O and appropriately increasing the FiO2. If ABGs remain acceptable, without an increase in work of breathing, an off-sweep gas challenge for at least 2–3 h is performed. The whole weaning can occur over several hours to days.
There are several ways for successfully weaning from VV ECMO, but these differences in weaning strategies are based on expert opinions rather than evidence [16,17,18,19,20,21]. While some centers will keep the pump flow over 3 l, which prevents clotting of the circuit and also mitigates the need for anticoagulation, other institutions will drop flows to a minimum of 1 l. In the author’s opinion, it is not necessary to reduce flows when the sweep is at zero, given that there is no diffusion gradient between the sweep gas and the patient’s blood flow. This “diffusion equilibrium” minimizes the significance of ECMO flows during the weaning process [16].
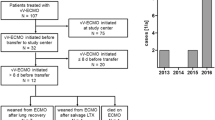
Bridge to lung transplantation
In cases of irreversible lung disease, VV ECMO can be considered for decompensated patients who are candidates for lung transplantation [15, 22,23,24]. A small subset of lung transplant candidates with severe primary or secondary pulmonary hypertension and associated right ventricular dysfunction may require VA ECMO support instead. Most centers will initiate VV ECMO therapy for worsening gas exchange in already intubated patients who are previously listed for transplant, or who are potential transplant candidates. Recent data supports superior outcomes of pre-lung transplant ambulatory patients [25, 26]. As a result, some lung transplant programs, when indicated, will initiate VV ECMO on non-intubated patients [26,27,28]. The utilization of a single dual-lumen cannula in an upper body vein is certainly advantageous, since it allows patients to participate in pre-transplant physical therapy. Patients can remain on VV ECMO during their transplant workup and while on the waiting list. VV ECMO can be continued after lung transplantation when primary graft dysfunction occurs, in cases of marginal donor lungs or for early cellular or antibody mediated rejection.
During the lung transplant procedure, patients already on VV ECMO will be transitioned to VA ECMO. This is accomplished by adding an arterial cannula, either in the ascending aorta, when sternotomy or clamshell incision is utilized, or in the femoral or axillary artery for anterior thoracotomy approaches. Lung transplantation is then performed on VA ECMO, or on full CPB, when VA ECMO is not tolerated, or based on the surgeon’s preference. If initial graft function allows, recipients can be weaned off ECMO immediately prior to leaving the OR. In cases of marginal lung graft function, ECMO can again be converted from VA to VV and recipients can be weaned in the same fashion as bridge to recovery patients, once the lungs have recovered.
Bridge to decision
For patients with end-stage lung failure where lung transplant candidacy is unknown, ECMO can be initiated under the indication of “bridge to decision.” This should occur in the context of an ongoing multidisciplinary approach towards lung transplantation, but also considering at the same time the potential to wean VV ECMO.
VV ECMO bridge to no recovery — discontinue for futility
A significant number of patients that receive VV ECMO therapy will not recover. Mortality rates following VV ECMO have been reported as high as 50%, depending on the underlying etiology of lung failure and the patient’s co-morbidities [17, 19, 29,30,31]. When VV ECMO cannot achieve its goal as a bridge to recovery, bridge to decision or lung transplant, it then functions as a bridge to no recovery [14].
Advances in mechanical circulatory support technology, including VV ECMO, have allowed us to substantially extend the duration of ECMO therapy, even when treatment is considered futile. The term medical futility is utilized to describe situations where patients have no chance of survival to discharge and whose dying process is prolonged by some form of life support [31, 32]. Discontinuing VV ECMO support for futility should be decided on a case to case basis but should be considered in the following situations: (a) patients with a pre-existing diagnosis of irreversible lung disease that have been on prolonged VV ECMO support and are not able to wean after multiple attempts; (b) patients without any chance of lung recovery, who are not candidates for lung transplantation; (c) irreversible neurological injury or brain stem death; (d) patients with new respiratory illness which is severe or progressive and precludes any meaningful chance of recovery, especially when associated with VV ECMO-related complications, such as sepsis, disabling stroke, hemorrhage, and multi-organ failure; (e) when directed by the patient’s previously expressed wishes/advance directives. Borderline cases, that do not fulfill any of the above indications, can be very challenging when attempting to determine futility. By definition, patients on VV ECMO have intact cardiac function, which makes cardiac death unlikely, unless device malfunction or complications occur. Furthermore, most patients receiving futile VV ECMO support do not fulfill criteria for brain stem death which further complicates the decision-making process. In these situations, the responsible physicians and the patient’s family members or surrogates are faced with difficult conversations and decisions about withdrawing care and terminating VV ECMO support. We have found that frequent and honest communication with families about goals and limitations of VV ECMO are paramount during this process. End-of-life discussions with family members or with patients themselves when they are alert and able to communicate should involve a multidisciplinary team of critical care/ECMO physicians, palliative medicine, and medical ethics specialist. The more unified, skilled, and empathetic the medical team is in its approach, the more likely family members are to understand the limitations and futility of continuing VV ECMO support [32].
References
Pasrija C, Mackowick KM, Raithel M, et al. Ambulation with femoral arterial cannulation can be safely performed on venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg. 2019;107:1389–94.
Majunke N, Mangner N, Linke A, et al. Comparison of percutaneous closure versus surgical femoral cutdown for decannulation of large-sized arterial and venous access sites in adults after successful weaning of veno-arterial extracorporeal membrane oxygenation. J Invasive Cardiol. 2016;28:415–9.
Hassan MF, Lawrence M, Lee D, Velazco J, Martin C, Reddy R. Simplified percutaneous VA ECMO decannulation using the MANTA vascular closure device: initial US experience. J Card Surg. 2020;35:217–21. https://doi.org/10.1111/jocs.14308.
Hill JD, O’Brien TG, Murray JJ, et al. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson membrane lung. N Engl J Med. 1972;286:629–34.
Extracorporeal Life Support Organization – about us. https://www.elso.org. Accessed 16 Sept 2022
Extracorporeal Life Support Organization - international summary. https://www.elso.org/Registry/Statistics/InternationalSummary.aspx. April 2022. Report Accessed 16 September 2022
Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–63.
Combes A, Hajage D, Capellier G, et al. EOLIA Trial Group, REVA, and ECMONet. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–75.
Badulak J, Anotnini MV, Stead CM, et al. ELSO COVID-19 Working Group Members. Extracorporeal membrane oxygenation for COVID-19: updated 2021 guidelines from the Extracorporeal Life Support Organization. ASAIO J. 2021;67:485–495.
Powell EK, Haase DJ, Lankford A, et al. Body mass index does not impact survival in COVID-19 patients requiring veno-venous extracorporeal membrane oxygenation. Perfusion. 2022. https://doi.org/10.1177/02676591221097642.
Ellison TA, Kilic A, Choi CW, Bush EL. Extracorporeal membrane oxygenation and short-term mechanical circulatory support. In: Baumgartner WA, Jacobs JP, Darling GE, eds. Adult and Pediatric Cardiac Surgery. STS Cardiothoracic Surgery E-Book. Chicago: Society of Thoracic Surgeons; 2020. ebook.sts.org. Accessed 24 Sept 2022.
McMichael, Ali B.V.; Ryerson, Lindsay M.; Ratano, Damian; Fan, Eddy; Faraoni, David; Annich, Gail M.∥. 2021 ELSO adult and pediatric anticoagulation guidelines. ASAIO Journal. 2022;68:303–310.
Annich GM, Extracorporeal Life Support Organization. ECMO : extracorporeal cardiopulmonary support in critical care, Red Book. Extracorporeal Life Support Organization;2012
Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. 2014;145:876–82.
Tsiouris A, Budev MM, Yun JJ. Extracorporeal membrane oxygenation as a bridge to lung transplantation in the United States: a multicenter survey. ASAIO J. 2018;64:689–93.
Broman LM, Malfertheiner MV, Montisci A, Pappalardo F. Weaning from veno-venous extracorporeal membrane oxygenation: how I do it. J Thorac Dis. 2018;10:S692–7.
Tonna JE, Abrams D, Brodie D, et al. Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the Extracorporeal Life Support Organization (ELSO). ASAIO J. 2021;67:601–10.
Seiler F, Trudzinski FC, Hörsch SI, et al. Weaning from prolonged veno-venous extracorporeal membrane oxygenation (ECMO) after transfer to a specialized center: a retrospective study. J Artif Organs. 2018;21:300–7.
Short BL, Williams L. editors. ECMO Specialist training manual 3rd ed. Extracorporeal Life Support Organization, Ann Arbor, MI, USA
Brogan TV, Lequier L, Lorusso R, MacLaren G, Peek G. editors. Red book 5th ed. Extracorporeal Life Support Organization, Ann Arbor, MI, USA
The Alfred Health Guideline on Extracorporeal Membrane Oxygenation (ECMO). Available online: http://www.alfredicu.org.au/assets/Documents/ICU-Guidelines/ECMO/ECMOGuideline.pdf
Biscotti M, Gannon WD, Agerstrand C, et al. Awake extracorporeal membrane oxygenation as bridge to lung transplantation: a 9-year experience. Ann Thorac Surg. 2017;104:412–9.
Nosotti M, Rosso L, Tosi D, et al. Extracorporeal membrane oxygenation with spontaneous breathing as a bridge to lung transplantation. Interact Cardiovasc Thorac Surg. 2013;16:55–9.
Olsson KM, Simon A, Strueber M, et al. Extracorporeal membrane oxygenation in nonintubated patients as bridge to lung transplantation. Am J Transplant. 2010;10:2173–8.
Keshavamurthy S, Bazan V, Tribble TA, Baz MA, Zwischenberger JB. Ambulatory extracorporeal membrane oxygenation (ECMO) as a bridge to lung transplantation. Indian J Thorac Cardiovasc Surg. 2021;37:366–79. https://doi.org/10.1007/s12055-021-01210-4.
Lehr CJ, Zaas DW, Cheifetz IM, Turner DA. Ambulatory extracorporeal membrane oxygenation as a bridge to lung transplantation: walking while waiting. Chest. 2015;147:1213–8.
Yeo HJ, Lee S, Yoon SH, et al. Extracorporeal life support as a bridge to lung transplantation in patients with acute respiratory failure. Transplant Proc. 2017;49:1430–5.
Fuehner T, Kuehn C, Hadem J, et al. Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med. 2012;185:763–8.
Smith DE, Chang SH, Geraci TC, et al. One-year outcomes with venovenous extracorporeal membrane oxygenation support for severe COVID-19. Ann Thorac Surg. 2022;114:70–5.
Kim JH, Pieri M, Landoni G, et al. Venovenous ECMO treatment, outcomes, and complications in adults according to large case series: a systematic review. Int J Artif Organs. 2021;44:481–8.
Rubin E, Courtwright A. Medical futility procedures: what more do we need to know? Chest. 2013;144:1707–11.
Mulaikal TA, Nakagawa S, Prager KM. Extracorporeal membrane oxygenation bridge to no recovery. Circulation. 2019;139:428–30.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics committee approval
This is a review article; therefore, ethical approval is not mandated.
Informed consent
Being a review, informed consent from participants was not necessary.
Statement of human and animal rights
Not applicable.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsiouris, A., Protos, A.N., Saikus, C.E. et al. Fundamentals of weaning veno-arterial and veno-venous extracorporeal membrane oxygenation. Indian J Thorac Cardiovasc Surg 39 (Suppl 1), 123–133 (2023). https://doi.org/10.1007/s12055-023-01474-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-023-01474-y