Abstract
Diabetes mellitus (DM) is a global health problem owing to its high prevalence and increased morbidity and mortality. The prevalence of DM and impaired glucose tolerance in Uganda is approximately 4.1% and 6.6%, respectively. Medicinal plants are commonly used for the management of DM, especially in developing countries, such as Uganda. According to several ethnobotanical surveys conducted in Uganda, various medicinal plants are used in DM management. Meanwhile, ethnopharmacological studies have confirmed the anti-diabetic efficacy of various plants and plant-derived formulations from Uganda. However, these information remain highly fragmented without a single repository for plants used in the management and treatment of DM in Uganda, hindering further investigations. Therefore, this study aimed to comprehensively explore plants used for DM treatment in Uganda and retrieve relevant ethnopharmacological and ethnomedicinal information that can be used for DM therapy development. English peer-reviewed articles and books were searched in scientific databases, especially PubMed, Scopus, Google Scholar, Science Direct, SciFinder, and Medline, to retrieve information on medicinal plants used for DM treatment and management in Uganda. The databases were searched to obtain published literature on the anti-diabetic activities and safety of plants among the identified plants. The family name, plant parts used, anti-diabetic activities, dosage, and mechanisms of action of plant extracts were captured. In total, 46 species belonging to 26 families are used to treat DM in Uganda. Most species belonged to the Fabaceae (20%), Asteraceae (13%), and Solanaceae (7%) families. Anti-diabetic activities of 27 (59%) species have been scientifically investigated, whereas the rest have not been evaluated. This review indicated that various medicinal plants are used in the traditional treatment and management of DM across different regions in Uganda. Scientific investigations have revealed the anti-diabetic potential and safety of several of these plants. However, there is a need to validate the anti-diabetic potential of other unstudied plants. Additionally, isolating and characterizing active principles and elucidating the anti-diabetic mechanism of these plants and performing preclinical and clinical studies in the future could aid in the formulation of an effective and safe treatment for DM.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is referred to as heterogeneous disturbances of metabolism characterized by chronic hyperglycemia, which is caused by either insufficient insulin secretion in the pancreatic β-cells (type-1 diabetes mellitus (T1D)) or impaired insulin secretion and action (type-2 diabetes mellitus (T2D)) [1]. The disease and its complications continue to be a major global health threat [2]. In 2017, DM-associated complications resulted in approximately 4 million deaths worldwide and accounted for 6.8% of total deaths in Africa [3]. Additionally, DM is predicted to be among the top seven causes of death by 2030 [4]. The prevalence of DM has increased exponentially worldwide in the last four decades [5, 6], which is mainly attributed to the growing and aging population, high energy/high fat diet, as well as sedentary lifestyle [7]. Notably, more than 90% of all DM cases are T2D [8] and according to Noubiap et al. [9], approximately 425 million DM cases were recorded in 2017 globally. The caseload is predicted to increase by 48% with an estimated 629 million affected individuals by 2045 [9]. In the African population, approximately 19.8 million DM cases are recorded, and it is estimated that 75% of them have not been diagnosed [10]. The prevalence of DM and impaired glucose tolerance is approximately 4.1% and 6.6%, respectively, in Uganda [10]. Moreover, the prevalence of DM in Uganda is projected to increase by 166.9% between 2013 and 2035, which will exceed the prevalence of DM in most other countries [11]. The management and treatment of DM are challenging as currently available conventional drugs, like acarbose are expensive, inaccessible, associated with several undesirable side effects, and have high secondary treatment failure rates [12]. Moreover, a definitive cure for DM is currently unavailable [13]. To overcome these challenges in the management and treatment of DM, there is a need to employ multiple approaches to identify alternative therapeutic strategies. Medicinal plants have been historically used to treat and manage DM in several traditional medicine systems of many cultures worldwide, especially in developing countries such as Uganda [12]. The use of medicinal plants is popular for primary health care among the general population owing to cultural acceptability, compatibility with the human body, and less side effects [14]. The World Health Organization has recommended the use of medicinal plants for managing DM and suggested increased efforts to scientifically evaluate the hypoglycemic properties of diverse plant species [13]. Ethnopharmacological studies are, by definition, scientific approaches to the study of biological activities of preparations used by humans, which possess, either beneficial or toxic or other direct pharmacological effects [15] and thus, ethnopharmacology involves investigating the relationship between humans and plants in all its complexity [15]. Accordingly, several ethnobotanical surveys conducted in Uganda have revealed that various medicinal plants are used in the management of DM [16,17,18,19,20,21,22,23,24]. Indeed, ethnopharmacological studies have reported the anti-diabetic efficacy of some of these plants and their derived formulations [23, 25]. However, these information remain highly fragmented without a single repository for plants used in the management and treatment of DM in Uganda, hindering further investigations. Therefore, this review aimed to explore plants used for treatment and management of DM in Uganda including relevant ethnopharmacological and ethnomedicinal information, which could provide useful information for research on DM therapy.
Methods
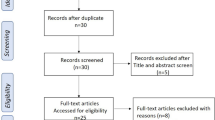
To get information on medicinal plants used in the management and treatment of DM in Uganda, Scientific databases namely, PubMed, Scopus, Google Scholar, Science Direct, SciFinder, and Medline were searched to retrieve relevant English peer-reviewed articles and books. Additional articles were found after tracking citations of the already accessed publications. Various attributes captured included species, family, local name, parts used, mode of preparation, habitat, and other diseases treated. Following this, the same databases were searched to obtain information on the anti-diabetic potential and safety of the identified plants. In this regard, research articles reporting anti-diabetic activities and safety of these plants were reviewed and findings recorded. During the search process, initially, the key words; ‘’ethnomedicine’’, ‘’ethnopharmacology’’, ‘’traditional medicine’’, ‘’herbal medicine’’, ‘’medicinal plant’’, ‘’phytomedicine”, ‘’ethnobotany’’ were combined with “diabetes mellitus”, “Uganda”. Next, each plant name identified from the above search were paired with “phytochemicals”, ‘’extract’’, ‘’isolation’’, ‘’efficacy’’, ‘’safety’’, ‘’toxicity’’, “antidiabetic”, “diabetes mellitus”, “hyperglycemic”, “hypoglycemic”, “mechanism of action,” “antihyperglycemic”, ‘’antilipidemic’’. The medicinal plants were then categorized based on their anti-diabetic activity investigation status. Additionally, ethnomedicinal uses of the identified plants in other countries neighbouring Uganda namely, Kenya, Tanzania, Democratic Republic of the Congo, Rwanda, and Sudan were obtained. Thereafter, the collected data were summarized and presented accordingly.
Results and discussion
Traditional concept of DM in Uganda
Generally, the understanding of DM is associated with several misconceptions, including its prevention, causes, signs, and treatment. A large portion of the population is aware of DM, especially in urban areas. However, nonfactual information on DM exists in the Ugandan population. For instance, DM symptoms are associated with witchcraft [26] and most people seek medical help when the symptoms of DM are severe, resulting in increased morbidity and mortality [27]. The use of traditional medicine inluding medicinal plants for treatment of DM is widespread in Uganda [28].
Plants used for treating DM in Uganda
The literature review identified 46 species of plants belonging to 26 families that are used to treat DM in Uganda (Table 1). The most commonly used species belonged to the Fabaceae (20%), Asteraceae (13%), and Solanaceae (7%) families (Fig. 1). The predominant use of plant species from these families to treat DM and its complications is attributed to a wide range of bioactive compounds, which make them largely effective in the treatment of human diseases [29, 30]. The widespread use of medicinal plants for DM treatment and management among the Ugandan population is due to low cost, easy accessibility, cultural acceptability, and the perceived less side effects [28]. This suggests that medicinal plants are key alternatives to the currently available conventional DM medicines. Consistent with our findings, several other researchers have also reported dominant use of plant species belonging to Fabaceae and Asteraceae families for treatment of DM in other countries, such as Nigeria and Tanzania [13, 31, 32]. Furthermore, studies have also shown that same plants are used similarly for DM treatment in neighboring and other countries (Table 2), for instance, the use of Erythrina abyssinica DC. (Fabaceae) and Bidens pilosa L. (Asteraceae) for treatment of DM were reported in Kenya [31]. Vernonia amygdalina Del., Aspilia africana (Pers.) C.D.Adams, and Ageratum conyzoides (L.) L. (all in Asteraceae) were documented to be used traditionally for treating DM in Nigeria [31, 33]. Cajanus cajan (L.) Huth (Fabaceae) has been used to treat DM in Tanzania [32].
Plant parts used, preparation, and mode of administration
The leaf (44%) was the most commonly used part, followed by the root (20%), fruit (12%), seed (9%), stem (8%), whole plant (3%), flowers (2%), and other unspecified parts (2%) (Fig. 2). The high use of leaves for DM treatment compared to other plant parts might be accounted to their potency associated with higher accumulation of bioactive compounds, ease of harvest, and quick ability to regenerate [30]. The extensive use of leaves for the treatment of DM corroborates with the findings of Skalli et al. [104] and Mohammed et al. [31] who also reported highest use of leaves for DM management compared to other plant parts. The most common modes of herbal preparation include decoction [17, 24] and infusion [21, 24] (Table 1). Decoctions are prepared by boiling plant materials in a specific quantity of water for 15–20 min and after, the mixtures are allowed to cool before administration. For example, Canarium schweinfurthii Engl. (stem barks), Cymbopogon citratus Stapf (leaves), Cajanus cajan (L.) Huth (leaves), and Hallea rubrostipulata (K. Schum.) J-F. Leroy (roots) are all prepared by decoction before administration. Infusion involves pouring hot or warm water onto the plant material and allowing the mixture to cool prior to administration. Plants such as Bidens pilosa L. (leaves, whole plant, roots) and Schkuhria pinnata (Lam.) Kuntze ex Thell. (leaves) are prepared through infusion for treatment of DM. Meanwhile, example of plants that are consumed directly for purposes of treating DM include Oxalis corniculata L. and Carissa macrocarpa (Eckl.) A.DC.. As observed, some medicinal plant parts are prepared through maceration; this involves crushing plant materials of a single species or a combination to extract a liquid before consumption. A case in point is Vigna unguiculata (L.) Walp. preparation. The common employment of decoction as a mode of preparation is attributed to the fact that boiling enables extraction of ingredients and preserves the herbal remedy longer compared to when cold water is used [30]. In some instances, other methods of preparation are more valuable because boiling leads to remarkable degradation of phytochemicals more so, aromatic compounds when done for a longer time [30]. This implies that no single mode of extraction is suitable for all medicinal plant preparation. Several other studies have reported similar modes of herbal preparation for treatment of DM [13, 31]. The solvent used for these herbal preparations is water and all prepared herbal medicines for DM treatment are orally administered (Table 1). Worth mentioning is that majority of these plants (about 63%) are obtained from the wild (Table 1). This is an indication that there is heavy dependence on wild source or natural environment in obtaining these medicinal plants; suggesting need to adopt propagation strategies (both macro and micro methods) for the plants for massive and sustainable supply of these medicinal materials. This finding is consistent with ethnobotanical study reports from other countries including Mexico [105], Ethiopia [106], and Turkey [107].
Knowledge dynamics of antidiabetic plants in Uganda
Through generations, knowledge of traditional medicine and medicinal plants are orally transferred from elders to young ones in Uganda [108]. Similar trend of traditional medicine knowledge transfer has been recorded in other African countries like Kenya and Ghana [109, 110]. At present, to the best of our knowledge, there are no exclusive indigenous knowledge systems or databases for Ugandan traditional medicines, except the highly fragmented reports of ethnobotanical studies conducted in Uganda. However, at African level, some active databases for African traditional medicine are available with non being specific to DM or any other disease (Table 3). Consequently, due to a wide range of biodiversity among countries, antidiabetic use of most plants registered in this study are not found in these general databases; although some plants are available with similar uses. For example, use of Acacia constricta for treatment of DM and other ailments is documented in PRELUDE database while use of Albizia chinensis for treatment of DM in the same database is not found currently. Considering the biodiversity difference among countries, development of comprehensive indigenous knowledge systems for African traditional medicine requires more efforts towards documenting these knowledge at country and subsequently regional (East, North, West, and South African) levels. The unavailability of Ugandan and limited African traditional medicine databases or records may be attributed to several factors among others, difficulty associated with language translation as most countries are made of diverse population with various languages, lack of funds for establishment and maintenance, and issues of intellectual property right [111]. In fact, insufficient or lack of funding has made several indigenous knowledge systems for traditional medicine become less updated or/and inactive online. For instance, a database known as NTRAP (Website: http://www.ippc.orst.edu/ipmafrica/db/index.html) that contained traditional medicine indigenous knowledge for East Africa (Uganda inclusive) is currently inactive [111].
Ethnopharmacological activities of medicinal plants used for treating DM in Uganda based on global scientific investigations
In vitro and in vivo studies
According to the WHO Traditional Medicine Strategy objectives, experimental validation with specified doses is the only way for proper understanding of the safety and efficacy of herbal medicines despite their long traditional use [114]. With respect to DM, the typical clinical target is to reduce blood sugar [115]. Therefore, the in vivo evaluation of blood sugar lowering effect of medicinal plants is for inferring potential clinical efficacy. In vitro studies are useful in the establishment or verification of the mechanisms of action of substances with potential therapeutic effects including medicinal plants [115]. Twenty seven (59%) out of the forty six medicinal plants in this review have been evaluated for their pharmacological activities against DM in several in vitro and in vivo studies worldwide (Table 4). Indeed, these plants have shown significant pharmacological activities including anti-hyperglycemic, anti-lipidemic, and antioxidative properties.
Taken together, these ethnopharmacological activities were exerted through various mechanisms of action. The mechanisms of action included decreasing blood sugar via stimulation of pancreatic β-cells [116, 117], inhibition of α-amylase, α-glucosidase, DPP-IV, insulinase, and aldose reductase enzymes activities [118,119,120,121], increasing expression of glucose transporters [122, 123], and enhancement of the affinity as well as sensitivity of insulin receptors [124]. Additionally, the plants acted through increase of glucose utilization within several tissues and organs [125], resistance of lipid peroxidation [126,127,128], clearance of free radical [127], and correction of lipid as well as protein metabolic disorders [129,130,131]. The observed mechanisms of action are comparable to those of current drugs used in DM treatment. For example, plants such as Syzygium cumini (L.) Skeels and Kigelia africana (Lam.) Benth., with α-amylase and α-glucosidase inhibitory effects are similar in action to acarbose [132]. Stimulators of pancreatic β-cells, for instance Tithonia diversifolia (Hemsl.) A.Gray and Bidens pilosa L. function as sulfonylureas or non-sulfonylureas secretagogues classes of drugs [115]. Plants like Schkuhria pinnata (Lam.) Kuntze ex Thell. which increase glucose utilization within tissues and organs are comparable to the biguanides drugs [115]. Agonists of PPARγ, for instance, Tithonian diversifolia (Hemsl.) A.Gray are similar in action with thiazolidinediones class of hypoglycemic agents [132]. Thus, the known mechanisms of action of the antidiabetic medicinal plants provide prospective therapeutic benefits of the plants, which may be utilized in the development of DM therapy. Medicinal plants studied elsewhere such as Chiliadenus iphionoides (Boiss. & C.I.Blanche) Brullo, Prunus africana (Hook.f.) Kalkman, Aspilia africana (Pers.) C.D.Adams, Cassia fistula L., and Ocimum gratissimum L. were reported to exhibit similar mechanisms of action against DM [33, 104, 132,133,134].
Phytochemicals in these plants either singly or in combination have been implicated for their antidiabetic properties [135, 136]. In fact, antidiabetic effects of plants are attributed to several classes of compounds namely, alkaloids, phenolic acids, saponins, tannins, and terpenoids [127, 137, 138]. A case in point is Jassim et al. [139] who reported that phenol extracts of Solanum melongena L. peels decreased blood glucose, triglyceride, blood total cholesterol, and low-density lipoprotein levels alongside increased serum high density lipoprotein levels in diabetic rats. Furthermore, the extract promoted hepatic detoxification by decreasing levels of serum glutamate oxaloacetate transaminase (SGOT) and serum glutamate pyruvic transaminase (SGPT) in alloxanised diabetic albino rats [139]. Interestingly, successful isolation, characterization, and purification of some antidiabetic phytoconstituents from a few plants have been achieved [119, 125, 140,141,142] (Table 4). For example, thyrotundin and tagitinin A were isolated from Tithonian diversifolia (Hemsl.) A.Gray with confirmed effect of decreasing insulin resistance via upregulating PPARγ activity [140]. In another study, Watanabe et al. [143] reported that aculeatin isolated from Toddalia asiatica (L.) Lam. promoted the differentiation and lipolysis of 3T3-L1 adipocytes along with increased glucose uptake, which are critical for treatment of DM and associated conditions. This implies that these phytochemical compounds could be potential antidiabetic agents.
Essentially, bioactive compounds of some of the investigated plants in this study have produced antidiabetic effects by acting on specific targets (For example, agonists of PPARγ such as Citrus sinensis (L.) Osbeck) [124], while other researchers only reported antidiabetic activities without definite pharmaceutical targets [144, 145]. For successful drug development, it is pivotal to identify and select targets of therapeutic compounds. Accordingly, the bioactive principles bind selectively to the receptor on the target and trigger the desired functional response [146]. In this way, molecular interactions associated with the products are understood, enabling gain of knowledge on the mechanisms of action, a key feature in a drug discovery process. Therefore, it is crucial to establish pharmaceutical targets of these herb bioactive compounds for improved outcome and development.
Regarding medicinal plants with unspecified mechanism of action such as Solanum indicum Roxb., their mechanisms of action in the DM pathway could possibly be linked to constituent phytochemicals [146]. In this case, plants with flavonoids as major bioactive compounds decrease level of blood glucose, cholesterol, and triglycerides by increasing activity of hepatic glucokinase and enhancement of insulin release from pancreatic islets [147]. Ibrahim et al. [148] isolated luteolin (3′,4′,5,7-tetrahydroxy flavone) along with other flavonoids from Oxalis corniculata L. and this compound has been reported to possess appreciable antidiabetic potential [149, 150]. Indeed, the underlying antidiabetic mechanisms and signalling pathways of luteolin include improving the sensitivity of body cells to insulin, antioxidative effect, inhibition of enzymes like PTP1B among others [149, 150]. Luteolin exerts its antioxidant properties by scavenging ROS and inhibiting enzymes responsible for ROS generation; this protects the pancreas and promotes insulin secretion [150]. Furthermore, luteolin enhances insulin sensitivity through influencing the Akt2 kinase [151]. Accordingly, Akt2 prevents the dephosphorylation of the insulin receptor and in this way, attenuation of insulin-signaling process is prevented [151]. On the other hand, plants with alkaloids as lead compounds show inhibition of α-glucosidase and decrease glucose transport through the intestinal epithelium [146]. Based on this, antidiabetic activities of plants containing high content of alkaloids in this review for instance, Ageratum conyzoides L. [152], may possibly be via lowering blood glucose and α-glucosidase inhibition. Additionally, quinolizidine alkaloids like multiflorine and sparteine have been reported to have insulinotropic effects on isolated pancreatic islets, besides their blood glucose-lowering role [153]. In fact, Wiedenfeld and Röder [154] isolated and identified multiflorine from A. conyzoides, therefore, the plant may act in the DM pathway via mechanisms related to that of multiflorine. Antidiabetic plants with bioactive principles in the classes of saponin (For example, Solanum indicum Roxb.), polysaccharides, and ferulic acid may trigger insulin secretion by stimulating pancreatic β-cells [147]. Particularly, hypoglycemic action of saponin is realised through various pathways including improvement of insulin signalling, activation of glycogen synthesis, restoration of insulin response, gluconeogenesis inhibition, among others [153, 155]. Likewise, coumarins have hypoglycemic characteristics and inhibit aldose reductase enzyme as well as aggregation of platelet [153]. Relatedly, antidiabetic plants containing high content of dietary fibers such as Cajanus cajan (L.) Huth could act by inhibiting α-amylase and delaying glucose diffusion, which in turn cause decrease in glucose absorption rate and postprandial serum glucose [146]. However, these suggested mechanisms of action can only be validated through further scientific investigations.
Meanwhile, to the best of our knowledge, 19 (41%) of the reported medicinal plant species in this study such as Justicia betonica L., Warburgia ugandensis Sprague, and Garcinia buchananii Baker remain scientifically uninvestigated for their antidiabetic effects, yet used traditionally for DM treatment. Such plants could be potential sources of active ingredients for therapy of DM and its complications, hence need for evaluation of their antidiabetic properties.
Clinical studies
Clinical trials with medicinal plants on human subjects is a critical step in drug discovery [115]. Currently, no clinical study using standardized extracts, bioactive compounds, and preparations of medicinal plants against DM has been reported in Uganda. Globally, seven medicinal plants in this review have been subjected to clinical studies involving human subjects. These plants include Moringa oleifera Lam., Artocarpus heterophyllus Lam., Bidens pilosa L., and Indigofera arrecta Hochst. ex A. Rich. among others [25, 172, 193, 295] (Table 4). Accordingly, all the tested plants showed the desired clinical effects [25, 172, 193, 295]. These therapeutic effects justify the use of the plants traditionally to treat DM across different communities in Uganda [17, 23]. However, the clinical trials were preliminary in nature aimed at assessing therapeutic effect of these plants in human subjects with none being a randomized, controlled trial. In Uganda, the absence of clinical trials on DM with traditionally used preparations may be attributed to insufficient data generated from preclinical studies, huge financial and strict regulatory requirements associated with clinical studies [296]. This means, clinical safety and efficacy of preparations from plants traditionally used to treat DM in Uganda are yet to be unlocked. The observed therapeutic effects of the evaluated plants, indicate the need to further investigate the traditionally used preparations in DM therapy for drug discovery and development.
Other ethnomedicinal uses and toxicity of the reported antidiabetic plants
Most of the plants in this review are used to treat several other diseases apart from DM (Table 1). A classic example is Kigelia africana (Lam.) Benth. which is recorded to be used for treating various health problems such as diarrhea, malaria, and cancer across different communities [19]. As such, pharmacological efficacy of K. africana against cancer has also been reported, for instance, its seed oil suppressed human embryonic kidney (HEK-293) cell and human colon adenocarcinoma (Caco-2) cell dose dependently [297]. Several active phytochemicals of K. africana have been identified and some isolated, namely, β-sitosterol, specioside, lapachol, verminoside, 3-(2′- hydroxyethyl)-5-(2″-hydroxypropyl) dihydrofuran-2-(3H)one, kigelin minecoside, ferulic acid, and 1,3-dimethylkigelin [296]. Therefore, the diverse bioactive compounds in these plants may explain their multipurpose use in treatment of diseases [115].
Besides exerting pharmacological activity that can be utilized for therapeutic purposes, constituent phytochemicals of medicinal plants are known to interact with same or other receptors and consequently produce harmful toxic effects [298]. Toxic compounds from plants may affect vital human organs and key body functional systems such as the central nervous system resulting in altered coordination of nerve functions [299]. Most of the recapitulated plants in this review have exhibited no adverse toxic effect as per respective toxicity reports (Table 4). For instance, aqueous leaf extract of Indigofera arrecta Hochst. ex A. Rich. showed no acute (up to 10 g/kg body weight, orally administered) and subchronic toxicity (2 g/kg body weight, orally administered daily for 30 days) in mice [300]. Furthermore, the extract never altered the glutathione and hepatic cytochrome P450 (CYP) isozymes whose modulation can consequently lead to interactions of components in a multiple drug treatment [300]. In another study, oral administration of leaf aqueous extract of Indigofera arrecta did not exert nephrotoxicity in humans [295]. However, some of the plants in this review have shown potential toxicity properties. Notably, Annona muricata L. fruit and leaf extracts (106 mg/kg body weight, infused intravenously for 28 days) exhibited acute neurotoxicity in rats [243]. The degree of plant toxicity depends on several factors including route of administration, method of extraction/ preparation, plant growth stage or part, victim susceptibility, species, and dosage [298]. Some phytochemicals in these plants such as anthraquinones and annonacin in Aloe vera (L.) Burm.f. and Annona muricata, respectively have been implicated for their toxicity [228, 229, 237, 243]. In cases where toxic effects are exerted at high doses, administration of preparations should be within known safe dose ranges to minimize side effects. High-risk patients like children, the elderly, pregnant women, and people with congestive heart failure ought to be more cautious when using these herbal medicines. Many other researchers around the world have provided useful information including dosages and toxicity from preclinical and clinical studies of medicinal plants, which may be relevant for development of DM therapeutic products [31, 32, 132]. It is worth noting that there is paucity of information regarding safety/toxicity profiles of the plants in this review. Moreover, most of the reported toxicity studies tested only acute toxicity either in vitro or in vivo yet this may not reflect toxicity condition experienced when taking herbal preparation for a long time as is the case in chronic diseases like DM [301]. Therefore, there is need to conduct comprehensive (acute, sub-chronic, and chronic) safety/toxicity studies on most of these potential medicinal plants to ascertain possible toxic effects to humans [302].
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Kerner W, Brückel J (2014) Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes 122(07):384–386
DeFronzo RA, Ferrannini E, Zimmet P, Alberti G (2015) International textbook of diabetes mellitus. Wiley, Hoboken
Saeedi P, Salpea P, Karuranga S, Petersohn I, Malanda B, Gregg EW, Unwin N, Wild SH, Williams R (2020) Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract 162:108086
Alwan A (2011) Global status report on noncommunicable diseases 2010. World Health Organization, Geneva
Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, Davies J, Vollmer S (2018) Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care 41(5):963–970
Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, Bixby H, Cowan MJ, Ali MK, Taddei C (2016) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4· 4 million participants. Lancet 387(10027):1513–1530
Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, Shi B, Sun H, Ba J, Chen B (2020) Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. https://doi.org/10.1136/bmj.m997
Laakso M (2019) Biomarkers for type 2 diabetes. Mol Metab 27:S139–S146
Noubiap JJ, Nansseu JR, Nyaga UF, Nkeck JR, Endomba FT, Kaze AD, Agbor VN, Bigna JJ (2019) Global prevalence of diabetes in active tuberculosis: a systematic review and meta-analysis of data from 2· 3 million patients with tuberculosis. Lancet Glob Health 7(4):e448–e460
Chiwanga FS, Njelekela MA, Diamond MB, Bajunirwe F, Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Adebamowo C, Ajayi I, Reid TG (2016) Urban and rural prevalence of diabetes and pre-diabetes and risk factors associated with diabetes in Tanzania and Uganda. Glob Health Action 9(1):31440
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103(2):137–149
Chikezie PC, Ojiako OA, Nwufo KC (2015) Overview of anti-diabetic medicinal plants: the Nigerian research experience. J Diabetes Metab 6(6):546
Ndip RN, Tanih NF, Kuete V (2013) Antidiabetes activity of African medicinal plants. In: Kuete V (ed) Medicinal Plant Research in Africa. Elsevier, Amsterdam, pp 753–786
Saravanamuttu S, Sudarsanam D (2012) Antidiabetic plants and their active ingredients: a review. Int J Pharm Sci Res 3(10):3639
Heinrich M (2014) Ethnopharmacology: quo vadis? Challenges for the future. Rev Bras Farmacogn 24:99–102
Adia MM, Anywar G, Byamukama R, Kamatenesi-Mugisha M, Sekagya Y, Kakudidi EK, Kiremire BT (2014) Medicinal plants used in malaria treatment by Prometra herbalists in Uganda. J Ethnopharmacol 155(1):580–588
Ajayi CO, Elujoba AA, Tenywa MG, Okella H, Weisheit A, Tolo CU, Ogwang PE (2020) A review for selecting medicinal plants commonly used for malaria in Uganda. Afr J Pharm Pharmacol 14(9):347–361
Gumisiriza H, Birungi G, Olet EA, Sesaazi CD (2019) Medicinal plant species used by local communities around queen elizabeth national park, maramagambo central forest reserve and ihimbo central forest reserve, south western Uganda. J Ethnopharmacol 239:111926
Kakudidi E, Kirimuhuzya C, Anywar G, Katuura E, Kiguli J (2016) Medicinal plants used in the management of noncommunicable diseases in Uganda. In: Tsay HS, Shyur LF, Agrawal DC, Wu YC, Wang SY (eds) Medicinal plants-recent advances in research and development. Springer, Singapore, pp 397–418
Nakaziba R, Anyolitho MK, Amanya SB, Ogwal-Okeng J, Alele PE (2021) Traditional Medicinal vegetables in Northern Uganda. An ethnobotanical survey. Int J Food Sci. https://doi.org/10.1155/2021/5588196
Philip K, Elizabeth MM, Cheplogoi PK, Samuel KT (2017) Ethnobotanical survey of antimalarial medicinal plants used in Butebo County, Eastern Uganda. Eur J Med Plants. 21:1–22
Schultz F, Anywar G, Wack B, Quave CL, Garbe L-A (2020) Ethnobotanical study of selected medicinal plants traditionally used in the rural Greater Mpigi region of Uganda. J Ethnopharmacol 256:112742
Ssenyange CW, Namulindwa A, Oyik B, Ssebuliba J (2015) Plants used to manage type II diabetes mellitus in selected districts of central Uganda. Afr Health Sci 15(2):496–502
Tugume P, Kakudidi EK, Buyinza M, Namaalwa J, Kamatenesi M, Mucunguzi P, Kalema J (2016) Ethnobotanical survey of medicinal plant species used by communities around Mabira Central Forest Reserve, Uganda. J Ethnobiol 12(1):1–28
Lai BY, Chen TY, Huang SH, Kuo TF, Chang TH, Chiang CK, Yang MT, Chang CL (2015) Bidens pilosa formulation improves blood homeostasis and β-cell function in men: a pilot study. Evid Based Complement Altern Med. 2015:832314
Rutebemberwa E, Katureebe SK, Mwaka AD, Atuyambe L, Gitta SN (2013) Perceptions of diabetes in rural areas of Eastern Uganda. Curationis 36(1):1–7
Chang H, Hawley NL, Kalyesubula R, Siddharthan T, Checkley W, Knauf F, Rabin TL (2019) Challenges to hypertension and diabetes management in rural Uganda: a qualitative study with patients, village health team members, and health care professionals. Int J Equity Health 18(1):1–14
Rutebemberwa E, Lubega M, Katureebe SK, Oundo A, Kiweewa F, Mukanga D (2013) Use of traditional medicine for the treatment of diabetes in Eastern Uganda: a qualitative exploration of reasons for choice. BMC Int Health Hum Rights 13(1):1–7
Molares S, Ladio A (2012) The usefulness of edible and medicinal Fabaceae in Argentine and Chilean Patagonia: environmental availability and other sources of supply. Evid Based Complement Altern Med. 2012:1
Tugume P, Nyakoojo C (2019) Ethno-pharmacological survey of herbal remedies used in the treatment of paediatric diseases in Buhunga parish, Rukungiri District, Uganda. BMC Complement Altern 19(1):1–10
Mohammed A, Ibrahim MA, Islam MS (2014) African medicinal plants with antidiabetic potentials: a review. Planta Med 80(05):354–377
Peter EL, Nagendrappa PB, Hilonga S, Tuyiringire N, Ashuro E, Kaligirwa A, Sesaazi CD (2021) Pharmacological reflection of plants traditionally used to manage diabetes mellitus in Tanzania. J Ethnopharmacol 269:113715
Okokon JE, Obot J, Ikpatt I (2006) Antidiabetic and hypolipidemic effects of aspilia africana. Niger J Nat Prod Med 10:41
Ssegawa P, Kasenene JM (2007) Medicinal plant diversity and uses in the Sango bay area, Southern Uganda. J Ethnopharmacol 113(3):521–540
Achola K, Munenge R (1998) Bronchodilating and uterine activities of Ageratum conyzoides extract. Pharm Biol 36(2):93–96
Moshi MJ, Otieno DF, Mbabazi PK, Weisheit A (2009) The Ethnomedicine of the Haya people of Bugabo ward, Kagera Region, North Western Tanzania. J Ethnobiol 5(1):1–5
Moshi MJ, Otieno DF, Weisheit A (2012) Ethnomedicine of the Kagera Region, North Western Tanzania. Part 3: plants used in traditional medicine in Kikuku village, Muleba District. J Ethnobiol 8(1):1–11
Kasali F, Mahano A, Kadima N, Mpiana P, Ngbolua K, Tshibangu T (2014) Ethnopharmacological survey of medicinal plants used against malaria in Butembo City (DR Congo). J Adv Bot Zool 1(1):1–11
Kasali FM, Kadima JN, Peter EL, Mtewa AG, Ajayi CO, Tusiimire J, Tolo CU, Ogwang PE, Weisheit A, Agaba AG (2021) Antidiabetic medicinal plants used in Democratic Republic of Congo: a critical review of ethnopharmacology and bioactivity data. Front Pharmacol 12:757090
Mushagalusa Kasali F, Ahadi Irenge C, Murhula Hamuli P, Birindwa Mulashe P, Murhula Katabana D, Mangambu Mokoso JDD, Mpiana PT, Ntokamunda Kadima J (2021) Ethnopharmacological survey on treatment of hypertension by traditional healers in Bukavu City, DR Congo. Evid Based Complement Altern Med. 2021:6684855
Ochwang’i DO, Kimwele CN, Oduma JA, Gathumbi PK, Mbaria JM, Kiama SG (2014) Medicinal plants used in treatment and management of cancer in Kakamega County, Kenya. J Ethnopharmacol 151(3):1040–1055
Omara T, Kiprop AK, Kosgei VJ (2021) Albizia coriaria Welw ex Oliver: a review of its ethnobotany, phytochemistry and ethnopharmacology. Adv Trad Med. https://doi.org/10.1007/s13596-021-00600-8
Owuor B, Ochanda J, Kokwaro J, Cheruiyot A, Yeda R, Okudo C, Akala H (2012) In vitro antiplasmodial activity of selected Luo and Kuria medicinal plants. J Ethnopharmacol 144(3):779–781
Keter LK, Mutiso PC (2012) Ethnobotanical studies of medicinal plants used by Traditional Health Practitioners in the management of diabetes in Lower Eastern Province, Kenya. J Ethnopharmacol 139(1):74–80
Nguta J, Mbaria J, Gakuya D, Gathumbi P, Kiama S (2010) Antimalarial herbal remedies of Msambweni, Kenya. J Ethnopharmacol 128(2):424–432
Nyamoita M, Mokua M, Onchari N, Ondora O (2020) Nine medicinal plants used in management of HIV/AIDS in Kisii County, Kenya. J Med Plants Stud 8(5):197–203
Kacholi DS, Amir HM (2022) Ethnobotanical survey of medicinal plants used by traditional healers in managing Gonorrhoea and Syphilis in Urambo District, Tabora Region, Tanzania. J Herbs Spices Med Plants 28(2):179–192
Lunyera J, Wang D, Maro V, Karia F, Boyd D, Omolo J, Patel UD, Stanifer JW (2016) Traditional medicine practices among community members with diabetes mellitus in Northern Tanzania: an ethnomedical survey. BMC Complement Altern 16(1):1–12
Stanifer JW, Lunyera J, Boyd D, Karia F, Maro V, Omolo J, Patel UD (2015) Traditional medicine practices among community members with chronic kidney disease in northern Tanzania: an ethnomedical survey. BMC Nephrol 16:1–11
Omara T, Odero MP, Obakiro SB (2022) Medicinal plants used for treating cancer in Kenya: an ethnopharmacological overview. Bull Natl Res Cent 46(1):1–33
Nagata JM, Jew AR, Kimeu JM, Salmen CR, Bukusi EA, Cohen CR (2011) Medical pluralism on Mfangano Island: use of medicinal plants among persons living with HIV/AIDS in Suba District, Kenya. J Ethnopharmacol 135(2):501–509
Amri E, Kisangau DP (2012) Ethnomedicinal study of plants used in villages around Kimboza forest reserve in Morogoro, Tanzania. J Ethnobiol 8(1):1–9
Karar MGE, Kuhnert N (2017) Herbal drugs from Sudan: traditional uses and phytoconstituents. Pharmacogn Rev 11(22):83
Maobe MA, Gatebe E, Gitu L, Rotich H (2013) Preliminary phytochemical screening of eight selected medicinal herbs used for the treatment of diabetes, malaria and pneumonia in Kisii region, southwest Kenya. Eur J Appl Sci 5(10):01–06
de Boer HJ, Kool A, Broberg A, Mziray WR, Hedberg I, Levenfors JJ (2005) Anti-fungal and anti-bacterial activity of some herbal remedies from Tanzania. J Ethnopharmacol 96(3):461–469
Nikolajsen T, Nielsen F, Rasch V, Sørensen PH, Ismail F, Kristiansen U, Jäger AK (2011) Uterine contraction induced by Tanzanian plants used to induce abortion. J Ethnopharmacol 137(1):921–925
Boily Y, Van Puyvelde L (1986) Screening of medicinal plants of Rwanda (Central Africa) for antimicrobial activity. J Ethnopharmacol 16(1):1–13
Muthee J, Gakuya D, Mbaria J, Kareru P, Mulei CM, Njonge F (2011) Ethnobotanical study of anthelmintic and other medicinal plants traditionally used in Loitoktok district of Kenya. J Ethnopharmacol 135(1):15–21
Wambugu SN, Mathiu PM, Gakuya DW, Kanui TI, Kabasa JD, Kiama SG (2011) Medicinal plants used in the management of chronic joint pains in Machakos and Makueni counties, Kenya. J Ethnopharmacol 137(2):945–955
Tomani JCD, Gainkam LOT, Nshutiyayesu S, Mukazayire MJ, Ribeiro SO, Stevigny C, Frederich M, Muganga R, Souopgui J (2018) An ethnobotanical survey and inhibitory effects on NLRP3 inflammasomes/Caspase-1 of herbal recipes’ extracts traditionally used in Rwanda for asthma treatment. J Ethnopharmacol 227:29–40
Kaingu CK, Oduma JA, Mbaria JM, Kiama SG (2013) Medicinal plants traditionally used for the management of female reproductive health dysfunction in Tana River County, Kenya. Cell Med. 3(2):17.11
Muthaura C, Keriko J, Mutai C, Yenesew A, Gathirwa J, Irungu B, Nyangacha R, Mungai G, Derese S (2015) Antiplasmodial potential of traditional phytotherapy of some remedies used in treatment of malaria in Meru-Tharaka Nithi County of Kenya. J Ethnopharmacol 175:315–323
Nyang’au HO, Maingi J, Kebira A (2017) The efficacy of some medicinal plants used locally within Transmara west, Narok County, Kenya against selected Enterobacteria and Candida. J Pharm Biol 12:115–122
Hilonga S, Otieno JN, Ghorbani A, Pereus D, Kocyan A, de Boer H (2019) Trade of wild-harvested medicinal plant species in local markets of Tanzania and its implications for conservation. S Afr J Bot 122:214–224
wanjiku Ngari E (2010) Ethnomedicne of Ogiek of River Njoro watershed, Nakuru, Kenya. Ethnobot Res Appl 8:135–152
Ndossi BA, Chacha M (2016) Comparative antibacterial and antifungal efficacy of selected Tanzania medicinal plants. Eur J Med Plants 14:1–10
Mukazayire M-J, Minani V, Ruffo CK, Bizuru E, Stévigny C, Duez P (2011) Traditional phytotherapy remedies used in Southern Rwanda for the treatment of liver diseases. J Ethnopharmacol 138(2):415–431
Yamada T (1999) A report on the ethnobotany of the Nyindu in the eastern part of the former Zaire. Afr Study Monogr 20(1):1–72
Njoroge GN, Kibunga JW (2007) Herbal medicine acceptance, sources and utilization for diarrhoea management in a cosmopolitan urban area (Thika, Kenya). Afr J Ecol 45:65–70
Zinga C (2020) Knowledge and skill assessment of congolese traditional healers on healthy and diseased kidney. ECCMC 3:09–18
Adeka R, Lukhoba C, Odhiambo J, Maundu P (2019) Morphological traits as indicators of bitterness in traditional vegetables: the case of spider plant (Gynandropsis gynandra) in Kenya. AJB 2(3):1–15
Ngowi N (2015) Ethnobotanical study of medicinal plants in Kondoa eroded area of central Tanzania. Int J Sci Basic Appl Res 21:223–233
Chifundera K (2001) Contribution to the inventory of medicinal plants from the Bushi area, South Kivu Province, Democratic Republic of Congo. Fitoterapia 72(4):351–368
Chrian M, Erasto P, Otieno NJ (2011) Antimycobacterial activity and cytotoxicity effect of extracts of Hallea rubrostipulata and Zanthoxylum chalybeum. Spatula DD 1(3):147–152
Schlage C, Mabula C, Mahunnah R, Heinrich, M (2000) Medicinal plants of the Washambaa (Tanzania): documentation and ethnopharmacological evaluation. Plant Biol 2(1):83–92
Odongo E, Mungai N, Mutai P, Karumi E, Mwangi J, Kimondo J, Omale J, Simiyu J (2017) Antioxidant and anti-inflammatory activities of selected medicinal plants from western Kenya. AJPT 6(4):178–182
Kokwaro JO, Johns T (1998) Luo biological dictionary. East African Publishers, Kampala
Amuri B, Maseho M, Simbi L, Duez P, Byanga K (2018) Ethnobotanical survey of herbs used in the management of diabetes mellitus in Southern Katanga Area/DR Congo. Pan Afr Med J 30(1):218
Yagi SM, Yagi AI (2018) Traditional medicinal plants used for the treatment of diabetes in the Sudan: a review. Afr J Pharm Pharmacol 12(3):27–40
Kigen G, Some F, Kibosia J, Rono H, Kiprop E, Wanjohi B, Kigen P, Kipkore W (2014) Ethnomedicinal plants traditionally used by the keiyo community in Elgeyo Marakwet County, Kenya. J Biodivers Bioprospecting Dev 1(3):11
McGeoch L (2004) Plant ecology in a human context: Mondia whytei in Kakamega Forest, Kenya. Dissertation, Brown University
Koorbanally NA, Mulholland DA, Crouch NR (2000) Isolation of isovanillin from aromatic roots of the medicinal African liane, Mondia whitei. J Herbs Spices Med Plants 7(3):37–43
Ipona EN, Inkoto CL, Bongo GN, Mulenga CM, Ilinga BL, Shetonde O, Mbala BM, Tshilanda DD, Mvingu BK, Kayembe JS (2019) Ethno-Botanical survey and ecological study of medicinal plants traditionally used against erectile dysfunction in Democratic Republic of the Congo. J Biosci Bioeng 4(4):85–91
Kamau LN, Mbaabu PM, Mbaria JM, Gathumbi PK, Kiama SG (2016) Ethnobotanical survey and threats to medicinal plants traditionally used for the management of human diseases in Nyeri County, Kenya. Cell Med. 6(3):21.1-21.15
Omwenga E, Hensel A, Shitandi A, Goycoolea F (2015) Ethnobotanical survey of traditionally used medicinal plants for infections of skin, gastrointestinal tract, urinary tract and the oral cavity in Borabu sub-county, Nyamira county, Kenya. J Ethnopharmacol 176:508–514
Tibuhwa DD (2016) Oxalis corniculata L. in Tanzania: traditional use, cytotoxicity and antimicrobial activities. J Appl Biol 105:10055–10063
Arika W, Ogola P, Nyamai D, Mawia A, Wambua F, Kiboi NG, Wambani J, Njagi S, Rachuonyo H, Emmah K (2016) Mineral elements content of selected Kenyan antidiabetic medicinal plants. Adv Tech Biol Med 4:1
Chhabra S, Mahunnah R, Mshiu E (1990) Plants used in traditional medicine in Eastern Tanzania IV. Angiosperms (Mimosaceae to Papilionaceae). J Ethnopharmacol 29(3):295–323
Malebo H, Tanja W, Cal M, Swaleh S, Omolo M, Hassanali A, Séquin U, Hamburger M, Brun R, Ndiege I (2009) Antiplasmodial, anti-trypanosomal, anti-leishmanial and cytotoxicity activity of selected Tanzanian medicinal plants. Tanzan J Health Res. https://doi.org/10.4314/thrb.v11i4.50194
Mutwiwa C, Rotich B, Kauti M, Rithaa J (2018) Ethnobotanical survey of medicinal plants in Mwala sub-county, Machakos County, Kenya. J Dis Med Plants 4:110–119
Kareru P, Kenji G, Gachanja A, Keriko J, Mungai G (2007) Traditional medicines among the Embu and Mbeere people of Kenya. Afr J Tradit Complement Altern Med 4(1):75–86
Johns T, Faubert GM, Kokwaro JO, Mahunnah R, Kimanani EK (1995) Anti-giardial activity of gastrointestinal remedies of the Luo of East Africa. J Ethnopharmacol 46(1):17–23
Maregesi SM, Ngassapa OD, Pieters L, Vlietinck AJ (2007) Ethnopharmacological survey of the Bunda district, Tanzania: plants used to treat infectious diseases. J Ethnopharmacol 113(3):457–470
Masunda AT, Inkoto CL, Bongo GN, Wa Oloko J, Ngbolua K, Tshibangu D, Tshilanda D, Mpiana P (2019) Ethnobotanical and ecological studies of plants used in the treatment of diabetes in Kwango, Kongo central and Kinshasa in the Democratic Republic of the Congo. JDE 4(1):18–25
Pathy KK, Flavien NB, Honoré BK, Vanhove W, Van Damme P (2021) Ethnobotanical characterization of medicinal plants used in Kisantu and Mbanza-Ngungu territories, Kongo-Central Province in DR Congo. J Ethnobiol 17(1):1–15
Kareru P, Gachanja A, Keriko J, Kenji G (2008) Antimicrobial activity of some medicinal plants used by herbalists in eastern province, Kenya. Afr J Tradit Complement Altern Med 5(1):51–55
Kigen G, Maritim A, Some F, Kibosia J, Rono H, Chepkwony S, Kipkore W, Wanjoh B (2016) Ethnopharmacological survey of the medicinal plants used in Tindiret, Nandi County, Kenya. Afr J Tradit Complement Altern Med 13(3):156–168
Orwa JA, Jondiko I, Minja RJ, Bekunda M (2008) The use of Toddalia asiatica (L) Lam. (Rutaceae) in traditional medicine practice in East Africa. J Ethnopharmacol 115(2):257–262
Nderitu KW, Mwenda NS, Macharia NJ, Barasa SS, Ngugi MP (2017) Antiobesity activities of methanolic extracts of Amaranthus dubius, Cucurbita pepo, and Vigna unguiculata in progesterone-induced obese Mice. Evid Based Complement Altern Med. 2017:4317321
Peter EL, Rumisha SF, Mashoto KO, Malebo HM (2014) Ethno-medicinal knowledge and plants traditionally used to treat anemia in Tanzania: a cross sectional survey. J Ethnopharmacol 154(3):767–773
Mpiana P, Mudogo V, Ngbolua K, Tshibangu D, Atibu E, Kitwa E, Kanangila A (2009) In vitro antisickling activity of anthocyanins extracts of Vigna unguiculata (L.) Walp. In: Mpiana P (ed) Chemistry and medicinal value Houston. Studium Press LLC, Houston, pp 75–82
Maobe MA, Gitu L, Gatebe E, Rotich H, Box P (2012) Phytochemical analysis of phenol and flavonoid in eight selected medicinal herbs used for the treatment of diabetes, malaria and pneumonia in Kisii, Kenya. Acad J Cancer Res 5:31–39
Mollel NP, Otieno JN, Sitoni DK (2022) Medicinal plants traded in Arusha city, Tanzania. J Med Plants Stud 10:175–182
Skalli S, Hassikou R, Arahou M (2019) An ethnobotanical survey of medicinal plants used for diabetes treatment in Rabat, Morocco. Heliyon 5(3):e01421
del Carmen J-Vázquez M, Carranza-Álvarez C, Alonso-Castro AJ, González-Alcaraz VF, Bravo-Acevedo E, Chamarro-Tinajero FJ, Solano E (2013) Ethnobotany of medicinal plants used in Xalpatlahuac, Guerrero, México. J Ethnopharmacol 148(2):521–527
Tamene S, Addisu D, Debela E (2020) Ethno-medicinal study of plants in Boricha district: use, preparation and application by traditional healers, Southern Ethiopia. J Med Plants Res 14(7):343–353
Emre G, Dogan A, Haznedaroglu MZ, Senkardes I, Ulger M, Satiroglu A, Can Emmez B, Tugay O (2021) An ethnobotanical study of medicinal plants in Mersin (Turkey). Front Pharmacol 12:664500
Omara T, Kagoya S, Openy A, Omute T, Ssebulime S, Kiplagat KM, Bongomin O (2020) Antivenin plants used for treatment of snakebites in Uganda: ethnobotanical reports and pharmacological evidences. Trop Med Health 48(1):1–16
Owuor BO, Kisangau DP (2006) Kenyan medicinal plants used as antivenin: a comparison of plant usage. J Ethnobiol 2:1–8
Wodah D, Asase A (2012) Ethnopharmacological use of plants by Sisala traditional healers in Northwest Ghana. Pharm Biol 50(7):807–815
Mangare CF, Li JA (2018) survey on indigenous knowledge systems databases for African traditional medicines. In: Proceedings of the 2018 7th international conference on bioinformatics and biomedical science, pp 9–15
D’avigdor E, Wohlmuth H, Asfaw Z, Awas T (2014) The current status of knowledge of herbal medicine and medicinal plants in Fiche. Ethiopia J Ethnobiol 10(1):1–33
Hatherley R, Brown DK, Musyoka TM, Penkler DL, Faya N, Lobb KA, Tastan Bishop Ö (2015) SANCDB: a South African natural compound database. J Cheminformatics 7:1–9
Organization WH (2013) WHO traditional medicine strategy: 2014–2023. World Health Organization, Geneva
Ezuruike UF, Prieto JM (2014) The use of plants in the traditional management of diabetes in Nigeria: pharmacological and toxicological considerations. J Ethnopharmacol 155(2):857–924
Cerf ME (2013) Beta cell dysfunction and insulin resistance. Front Endocrinol 4:37
Chang CL-T, Kuo H-K, Chang S-L, Chiang Y-M, Lee T-H, Wu W-M, Shyur L-F, Yang W-C (2005) The distinct effects of a butanol fraction of Bidens pilosa plant extract on the development of Th1-mediated diabetes and Th2-mediated airway inflammation in mice. J Biomed Sci 12(1):79–89
Ajiboye BO, Ojo OA, Adeyonu O, Imiere O, Oyinloye BE, Ogunmodede O (2018) Ameliorative activity of ethanolic extract of Artocarpus heterophyllus stem bark on alloxan-induced diabetic rats. Adv Pharm Bull 8(1):141
Mukherjee A, Sengupta S (2013) Characterization of nimbidiol as a potent intestinal disaccharidase and glucoamylase inhibitor present in Azadirachta indica (neem) useful for the treatment of diabetes. J Enzyme Inhib Med Chem 28(5):900–910
Njateng GSS, Zaib S, Chimi LY, Feudjio C, Mouokeu RS, Gatsing D, Kuiate J-R, Adewole E, Iqbal J (2018) Antidiabetic potential of methanol extracts from leaves of Piper umbellatum L. and Persea americana Mill. Asian Pac J Trop Biomed 8(3):160
Suleiman KY (2009) The effects of a Kenyan antidiabetic plant on insulin homeostasis. Dissertation, Nelson Mandela Metropolitan University
Ong KW, Hsu A, Song L, Huang D, Tan BKH (2011) Polyphenols-rich Vernonia amygdalina shows anti-diabetic effects in streptozotocin-induced diabetic rats. J Ethnopharmacol 133(2):598–607
Sewnarain P (2021) Antidiabetic activity of Schkuhria pinnata–Biological screening, PK analysis and mode of action. Dissertation, University of Cape Town
Sathiyabama RG, Gandhi GR, Denadai M, Sridharan G, Jothi G, Sasikumar P, Quintans JdSS, Narain N, Cuevas LE, Coutinho HDM (2018) Evidence of insulin-dependent signalling mechanisms produced by Citrus sinensis (L.) Osbeck fruit peel in an insulin resistant diabetic animal model. Food Chem Toxicol 116:86–99
Li X, Huang G, Zhao G, Chen W, Li J, Sun L (2013) Two new monoterpenes from Tithonia diversifolia and their anti-hyperglycemic activity. Rec Nat Prod 7(4):351
Ajiboye BO, Ojo OA, Oyinloye BE, Okesola MA, Oluwatosin A, Boligon AA, Kappo AP (2020) Investigation of the in vitro antioxidant potential of polyphenolic-rich extract of Artocarpus heterophyllus lam stem bark and its antidiabetic activity in streptozotocin-induced diabetic rats. J Evid Based Integr Med. 25:2515690X20916123
Tania PM, Castilo BD, Serrão PC, Lobato RA, Silva RR, Oliveira PF, Ferreira SP, Távora N, de de Silva AS (2016) Antioxidant effect of plant extracts of the leaves of Tithonia diversifolia (Hemsl.) A. Gray on the free radical DPPH. J Chem Pharm Res 8(8):1182–1189
Thongsom M, Chunglok W, Kuanchuea R, Tangpong J (2013) Antioxidant and hypoglycemic effects of Tithonia diversifolia aqueous leaves extract in alloxan-induced diabetic mice. Adv Environ Biol 1:2116–2126
Atta A, Saad S, Atta S, Mouneir S, Nasr S, Desouky H, Shaker H (2020) Cucurbita maxima and cucurbita maxima extract attenuate diabetes-induced hepatic and pancreatic injury in a rat model. JPP 4:06
Igbakin A, Oloyede O (2009) Comparative studies on the hypoglycaemic, hypoproteinaemic, hypocholesterolaemic and hypolipidaemic properties of ethanolic and normal saline extracts of the root of Vernonia amygdalina in diabetic rats. Adv Environ Biol 3(1):33–38
Mudassir HA, Khaliq S, Azmi MB, Bano M, Naheed M, Fatima M (2020) Persea americana seeds improve glycosylation and dyslipidemia in fructose-fed streptozotocin-injected type 2 diabetic male rats. Pak J Pharm Sci 33(6):2579
Salehi B, Ata A, Anil Kumar N, Sharopov F, Ramírez-Alarcón K, Ruiz-Ortega A, Abdulmajid Ayatollahi S, Valere Tsouh Fokou P, Kobarfard F, Amiruddin Zakaria Z (2019) Antidiabetic potential of medicinal plants and their active components. Biomolecules 9(10):551
Maina J, Kareru P, Gatebe E, Rotich H, Githira P, Njonge F, Kimani D, Mutembei J (2014) Hypoglycemic effects of selected herbal drug formulations from the Kenyan market. J Na Prod Plant Resour 4:10–17
Okoli R, Aigbe O, Ohaju-Obodo J, Mensah J (2007) Medicinal herbs used for managing some common ailments among Esan people of Edo State. Nigeria Pak J Nutr 6(5):490–496
Farzaei F, Morovati MR, Farjadmand F, Farzaei MH (2017) A mechanistic review on medicinal plants used for diabetes mellitus in traditional Persian medicine. J Evid Based Complement Altern Med 22(4):944–955
Patel D, Prasad SK, Kumar R, Hemalatha S (2012) An overview on antidiabetic medicinal plants having insulin mimetic property. Asian Pac J Trop Biomed 2(4):320–330
Egunyomi A, Gbadamosi I, Animashahun M (2011) Hypoglycaemic activity of the ethanol extract of Ageratum conyzoides linn. shoots on alloxan-induced diabetic rats. J Med Plant Res. 5(22):5347–5350
Temu J, Martin HD, Sauli E (2020) Hypoglycemic effects of Cymbopogon citratus ethanol leaves’ extract and its fractions in alloxan-induced diabetic mice. Int J Trop Dis Health. 41:1–11
Jassim YH, Palani AF, Dakeel AB (2016) Effect of phenolic compounds extract of S. melongena peels on sugar levels and biochemical parameters in alloxan-induced diabetic rats. J pharmacy sci 11:202–209
Lin H-R (2012) Sesquiterpene lactones from Tithonia diversifolia act as peroxisome proliferator-activated receptor agonists. Bioorganic Med Chem Lett 22(8):2954–2958
Nguyen P-H, Nguyen T-N-A, Dao T-T, Kang H-W, Ndinteh D-T, Mbafor J-T, Oh W-K (2010) AMP-activated protein kinase (AMPK) activation by benzofurans and coumestans isolated from Erythrina abyssinica. J Nat Prod 73(4):598–602
Ponnusamy S, Haldar S, Mulani F, Zinjarde S, Thulasiram H, RaviKumar A (2015) Gedunin and azadiradione: human pancreatic alpha-amylase inhibiting limonoids from neem (Azadirachta indica) as anti-diabetic agents. PLoS ONE 10(10):e0140113
Watanabe A, Kato T, Ito Y, Yoshida I, Harada T, Mishima T, Fujita K, Watai M, Nakagawa K, Miyazawa T (2014) Aculeatin, a coumarin derived from Toddalia asiatica (L.) Lam, enhances differentiation and lipolysis of 3T3-L1 adipocytes. Biochem Biophys Res Commun 453(4):787–792
Al-Qalhati IRS, Waly M, Al-Attabi Z, Al-Subhi LK (2016) Protective effect of Pteropyrum scoparium and Oxalis corniculata against streptozotocin-induced diabetes in rats. FASEB J 30:1176–1174
Borgohain R, Pathak P, Mohan R (2016) Anti-diabetic and Reno-protective effect of the ethanolic extract of Solanum indicum in alloxan-induced diabetic rats. J Evol Med Dent Sci 5(99):7294–7298
Dey S, Das D, Chakraborty A, Roychoudhury S, Choudhury BP, Choudhury AP, Mandal SC (2021) Plant-based traditional herbal contraceptive use in india: safety and regulatory issues. In: Mandal SC, Chakraborty R, Sen S (eds) Evidence based validation of traditional medicines: a comprehensive approach. Springer, Singapore, pp 659–675
Bhushan MS, Rao C, Ojha S, Vijayakumar M, Verma A (2010) An analytical review of plants for anti diabetic activity with their phytoconstituent and mechanism of action. Int J Pharm Sci Res 1(1):29–46
Ibrahim M, Hussain I, Imran M, Hussain N, Hussain A, Mahboob T (2013) Corniculatin A, a new flavonoidal glucoside from Oxalis corniculata. Rev Bras Farmacogn 23(4):630–634
Choi JS, Islam MN, Ali MY, Kim YM, Park HJ, Sohn HS, Jung HA (2014) The effects of C-glycosylation of luteolin on its antioxidant, anti-Alzheimer’s disease, anti-diabetic, and anti-inflammatory activities. Arch Pharmacal Res 37:1354–1363
Sangeetha R (2019) Luteolin in the management of type 2 diabetes mellitus. Curr Res Nutr Food Sci 7(2):393–398
Babu PVA, Liu D, Gilbert ER (2013) Recent advances in understanding the anti-diabetic actions of dietary flavonoids. J Nutr Biochem 24(11):1777–1789
Yadav N, Ganie SA, Singh B, Chhillar AK, Yadav SS (2019) Phytochemical constituents and ethnopharmacological properties of Ageratum conyzoides L. Phytother Res 33(9):2163–2178
Bushnak R, El Hajj M, Jaber A (2021) A review on the antidiabetic potential of medicinal plants. J Med Healthc 4:172–189
Wiedenfeld H, Röder E (1991) Pyrrolizidine alkaloids from Ageratum conyzoides. Planta Med 57(06):578–579
Kwon DY, Kim YS, Ryu SY, Choi YH, Cha M-R, Yang HJ, Park S (2012) Platyconic acid, a saponin from Platycodi radix, improves glucose homeostasis by enhancing insulin sensitivity in vitro and in vivo. Eur J Nutr 51:529–540
Fauziyah Y, Sunarti S, Hanoum IF, Wahyuningsih MSH (2018) Ethanol extract of Tithonia diversifolia (hemsley) a gray standardized ameliorates hyperglycemia, polyphagia, and weight loss in diabetic rats. Molekul 13(1):72–79
Chunudom L, Thongsom M, Karim N, Rahman MA, Rana MN, Tangpong J (2020) Tithonia diversifolia aqueous fraction plays a protective role against alloxan-induced diabetic mice via modulating GLUT2 expression. S Afr J Bot 133:118–123
Chunudom L, Thongsom M, Karim N, Tangpong J (2019) Amelioration of oxidative stress and pathological alterations in alloxan-induced diabetes mice by Tithonia diversifolia leaves extract. Chiang Mai J Sci 46(6):1096–1106
Elufioye T, Alatise O, Fakoya F, Agbedahunsi J, Houghton P (2009) Toxicity studies of Tithonia diversifolia A. Gray (Asteraceae) in rats. J Ethnopharmacol 122(2):410–415
Muganga R, Angenot L, Tits M, Frederich M (2010) Antiplasmodial and cytotoxic activities of Rwandan medicinal plants used in the treatment of malaria. J Ethnopharmacol 128(1):52–57
Amuri B, Maseho M, Simbi L, Okusa P, Duez P, Byanga K (2017) Hypoglycemic and antihyperglycemic activities of nine medicinal herbs used as antidiabetic in the region of Lubumbashi (DR Congo). Phytother Res 31(7):1029–1033
Ngugi P, Murugi J, Kibiti C, Ngeranwa J, Njue W, Maina D, Gathumbi P, Njagi N (2011) Hypoglycemic activity of some Kenyan plants traditionally used to manage diabetes mellitus in Eastern province. J Diabetes Metab 2(155):2
Cui L, Lee HS, Ndinteh DT, Mbafor JT, Kim YH, Le TVT, Nguyen PH, Oh WK (2010) New prenylated flavanones from Erythrina abyssinica with protein tyrosine phosphatase 1B (PTP1B) inhibitory activity. Planta Med 76(07):713–718
Bunalema L, Kirimuhuzya C, Tabuti J, Waako P, Magadula J, Otieno N, Orodho J, Okemo P (2011) The efficacy of the crude root bark extracts of Erythrina abyssinica on rifampicin resistant Mycobacterium tuberculosis. Afr Health Sci 11(4):587–593
Maroyi A (2012) Garden plants in Zimbabwe: their ethnomedicinal uses and reported toxicity. Ethnobot Res Appl 10:045–057
Al-Malki AL, El Rabey HA (2015) The antidiabetic effect of low doses of Moringa oleifera Lam. seeds on streptozotocin induced diabetes and diabetic nephropathy in male rats. BioMed Res Int 2015:381040
Asare GA, Gyan B, Bugyei K, Adjei S, Mahama R, Addo P, Otu-Nyarko L, Wiredu EK, Nyarko A (2012) Toxicity potentials of the nutraceutical Moringa oleifera at supra-supplementation levels. J Ethnopharmacol 139(1):265–272
Yassa HD, Tohamy AF (2014) Extract of Moringa oleifera leaves ameliorates streptozotocin-induced diabetes mellitus in adult rats. Acta Histochem 116(5):844–854
Busari M, Muhammad H, Ogbadoyi E, Kabiru A, Sani S, Yusuf R (2015) In vivo evaluation of antidiabetic properties of seed oil of Moringa oleifera Lam. J Appl Life Sci Int. 2:160–174
Muzumbukilwa WT, Nlooto M, Owira PMO (2019) Hepatoprotective effects of Moringa oleifera Lam (Moringaceae) leaf extracts in streptozotocin-induced diabetes in rats. J Funct Foods 57:75–82
Jimoh TO (2018) Enzymes inhibitory and radical scavenging potentials of two selected tropical vegetable (Moringa oleifera and Telfairia occidentalis) leaves relevant to type 2 diabetes mellitus. Rev Bras Farmacogn 28:73–79
Sissoko L, Diarra N, Nientao I, Stuart B, Togola A, Diallo D, Willcox ML (2020) Moringa oleifera leaf powder for type 2 diabetes: a pilot clinical trial. Afr J Tradit Complement Altern Med 17(2):29–36
Kumar P, Mandapaka R (2013) Effect of moringa oleifera on blood glucose, ldl levels in types ii diabetic obese people. Innov J Med Health Sci 3(1):23–25
Girma T, Genet S, Feyisa TOO, Tufa A (2021) Antihyperglycemic and antihyperlipidemic effect of persea americana in high fat diet and low dose streptozotocin induced T2DM male albino Wistar rats. Res Squ. https://doi.org/10.21203/rs.3.rs-198182/v1
Del Toro-Equihua M, Velasco-Rodríguez R, López-Ascencio R, Vásquez C (2016) Effect of an avocado oil-enhanced diet (Persea americana) on sucrose-induced insulin resistance in Wistar rats. J Food Drug Anal 24(2):350–357
Adienbo OM, Hart VO (2021) Antidiabetic effect of Persea americana seed extract is mediated through enhanced insulin secretion, improved beta-cell function, and reduced insulin resistance in diabetic rats. Eur J Med 9 (1)
Padilla-Camberos E, Martínez-Velázquez M, Flores-Fernández JM, Villanueva-Rodríguez S (2013) Acute toxicity and genotoxic activity of avocado seed extract (Persea americana Mill., cv Hass). Sci World J 2013:245828
Taha NA, Alkhawajah AAM, Raveesha K (2008) Acute and subacute toxicity studies of Persea americana Mill (Avocado) seed in rats. Int J Med Toxicol Leg Med 11(2):31–36
Ezejiofor AN, Okorie A, Orisakwe OE (2013) Hypoglycaemic and tissue-protective effects of the aqueous extract of Persea americana seeds on alloxan-induced albino rats. Malays J Med Sci: MJMS 20(5):31
Lima C, Vasconcelos C, Costa-Silva J, Maranhão C, Costa J, Batista T, Carneiro E, Soares L, Ferreira F, Wanderley A (2012) Anti-diabetic activity of extract from Persea americana Mill. leaf via the activation of protein kinase B (PKB/Akt) in streptozotocin-induced diabetic rats. J Ethnopharmacol 141(1):517–525
Odo Christian E, Nwodo Okwesili F, Joshua Parker E, Ugwu Okechukwu P (2014) Acute toxicity investigation and anti-diarrhoeal effect of the chloroform-methanol extract of the leaves of Persea americana. Iran J Pharm Res 13(2):651
Kouamé NGM, Koffi C, N’Zoué KS, Yao N, Doukouré B, Kamagaté M (2019) Comparative antidiabetic activity of aqueous, ethanol, and methanol leaf extracts of Persea americana and their effectiveness in type 2 diabetic rats. Evid Based Complement Altern Med. https://doi.org/10.1155/2019/5984570
Okafor SC, Gyang SS, Maiha BB, Eze ED, Yakubu MI, Chindo BA (2017) Aqueous extract of Persea americana leaves ameliorates alloxan-induced hyperglycaemia and hyperlipidaemia in rats. J Med Plant Res 11(47):755–762
Ayodele A, Adeoye AT, Adedapo AD, Omobowale TO, Adedapo AA, Oyagbemi AA (2017) Antidiabetic and antioxidant activities of the methanol leaf extract of Vernonia amygdalina in alloxan-induced diabetes in Wistar rats. JOMPED 1(1):1–12
Erukainure OL, Chukwuma CI, Sanni O, Matsabisa MG, Islam MS (2019) Histochemistry, phenolic content, antioxidant, and anti-diabetic activities of Vernonia amygdalina leaf extract. J Food Biochem 43(2):e12737
Ojiako O, Nwanjo H (2006) Is Vernonia amygdalina hepatotoxic or hepatoprotective? Response from biochemical and toxicity studies in rats. Afr J Biotechnol 5(18):1648
Zakaria Y, Azlan NZ, Nik NF, Muhammad H (2016) Phytochemicals and acute oral toxicity studies of the aqueous extract of Vernonia amygdalina from state of Malaysia. J Med Plants Stud 4(3):1–5
Atangwho IJ, Ebong PE, Egbung GE, Obi AU (2010) Extract of Vernonia amygdalina Del. (African bitter leaf) can reverse pancreatic cellular lesion after alloxan damage in the rat. Aust J Basic Appl 4(5):711–716
Atangwho IJ, Egbung GE, Ahmad M, Yam MF, Asmawi MZ (2013) Antioxidant versus anti-diabetic properties of leaves from Vernonia amygdalina Del. growing in Malaysia. Food Chem 141(4):3428–3434
Fernando M, Thabrew M (1988) Studies on the possible toxicity of Artocarpus heterophyllus. Ceylon J Med Sci 32(1):1–7
Shahin N, Alam S, Ali M (2012) Pharmacognostical standardisation and antidiabetic activity of Artocarpus heterophyllus leaves Lam. Int J Drug Dev Res 4(1):346–352
Omar HS, El-Beshbishy HA, Moussa Z, Taha KF, Singab ANB (2011) Antioxidant activity of Artocarpus heterophyllus Lam. (Jack Fruit) leaf extracts: remarkable attenuations of hyperglycemia and hyperlipidemia in streptozotocin-diabetic rats. Sci World J 11:788–800
Sd GN, Eapen J, Roopesh Kumar CB (2017) Hypoglycaemic effect of leaf decoction of panasa [artocarpus heterophyllus lam] in type ii diabetes mellitus-a clinical study. Int J Ayurveda Pharma Res 5(10):20–25
Bisht S, Sisodia S (2010) Anti-hyperglycemic and antidyslipidemic potential of Azadirachta indica leaf extract in STZ-induced diabetes mellitus. J Pharm Sci 2(10):622
Braga TM, Rocha L, Chung TY, Oliveira RF, Pinho C, Oliveira AI, Morgado J, Cruz A (2021) Azadirachta indica A. Juss. In vivo toxicity—an updated review. Molecules 26(2):252
Gandhi M, Lal R, Sankaranarayanan A, Banerjee CK, Sharma PL (1988) Acute toxicity study of the oil from Azadirachta indica seed (neem oil). J Ethnopharmacol 23(1):39–51
Khosla P, Bhanwra S, Singh J, Seth S, Srivastava R (2000) A study of hypoglycaemic effects of Azadirachta indica (Neem) in normal and alloxan diabetic rabbits. Indian J Physiol Pharmacol 44(1):69–74
Patil P, Patil S, Mane A, Verma S (2013) Antidiabetic activity of alcoholic extract of Neem (Azadirachta indica) root bark. Natl J Physiol Pharm Pharmacol 3(2):142–146
Perez-Gutierrez RM, Damian-Guzman M (2012) Meliacinolin: a potent α-glucosidase and α-amylase inhibitor isolated from Azadirachta indica leaves and in vivo antidiabetic property in streptozotocin-nicotinamide-induced type 2 diabetes in mice. Biol Pharm Bull 35(9):1516–1524
Kumari DJ (2010) Hypoglycaemic effect of Moringa oleifera and Azadirachta indica in type 2 diabetes mellitus. Bioscan 5(20):211–214
Pingali U, Ali MA, Gundagani S, Nutalapati C (2020) Evaluation of the effect of an aqueous extract of Azadirachta indica (Neem) leaves and twigs on glycemic control, endothelial dysfunction and systemic inflammation in subjects with type 2 diabetes mellitus–a randomized, double-blind, placebo-controlled clinical study. Diabetes Metab Syndr Obes 13:4401
Kochhar A, Sharma N, Sachdeva R (2009) Effect of supplementation of Tulsi (Ocimum sanctum) and Neem (Azadirachta indica) leaf powder on diabetic symptoms, anthropometric parameters and blood pressure of non insulin dependent male diabetics. Stud Ethno Med 3(1):5–9
Satyanarayana K, Sravanthi K, Shaker IA, Ponnulakshmi R (2015) Molecular approach to identify antidiabetic potential of Azadirachta indica. J Ayurveda Integr Med 6(3):165
Soman S, Rajamanickam C, Rauf AA, Indira M (2013) Beneficial effects of Psidium guajava leaf extract on diabetic myocardium. Exp Toxicol Pathol 65(1–2):91–95
Huang C-S, Yin M-C, Chiu L-C (2011) Antihyperglycemic and antioxidative potential of Psidium guajava fruit in streptozotocin-induced diabetic rats. Food Chem Toxicol 49(9):2189–2195
Jaiswal D (2009) Anti-hyperglycaemic potential of Psidium guajava raw fruit peel. Indian J Med Res 129:561–565
Mukhtar H, Ansari S, Bhat Z, Naved T, Singh P (2006) Antidiabetic activity of an ethanol extract obtained from the stem bark of Psidium guajava (Myrtaceae). Die Pharm 61(8):725–727
Basha SK, Kumari VS (2012) In vitro antidiabetic activity of Psidium guajava leaves extracts. Asian Pacific J Trop Dis 2:S98–S100
Manikandan R, Anand AV, Kumar S (2016) Phytochemical and in vitro antidiabetic activity of Psidium Guajava leaves. Pharmacogn J. 8(4):392
Zhu X, Ouyang W, Lan Y, Xiao H, Tang L, Liu G, Feng K, Zhang L, Song M, Cao Y (2020) Anti-hyperglycemic and liver protective effects of flavonoids from Psidium guajava L. (guava) leaf in diabetic mice. Food Biosci 35:100574
Kuang Q-T, Zhao J-J, Ye C-L, Wang J-R, Ye K-H, Zhang X-Q, Wang Y, Ye W-C (2012) Nephro-protective effects of total triterpenoids from Psidium guajava leaves on type 2 diabetic rats. Zhong Yao Cai 35(1):94–97
Liu C-W, Wang Y-C, Hsieh C-C, Lu H-C, Chiang W-D (2015) Guava (Psidium guajava Linn.) leaf extract promotes glucose uptake and glycogen accumulation by modulating the insulin signaling pathway in high-glucose-induced insulin-resistant mouse FL83B cells. Process Biochem 50(7):1128–1135
Mahmoodpoor A, Medghalchi M, Nazemiyeh H, Asgharian P, Shadvar K, Hamishehkar H (2018) Effect of Cucurbita maxima on control of blood glucose in diabetic critically ill patients. Adv Pharm Bull 8(2):347
Cruz R, Meurer C, Silva E, Schaefer C, Santos A, Bella Cruz A, Cechinel Filho V (2006) Toxicity evaluation of Cucurbita maxima. Seed extract in mice. Pharm Biol 44(4):301–303
Sharma A, Sharma AK, Chand T, Khardiya M, Yadav KC (2013) Antidiabetic and antihyperlipidemic activity of Cucurbita maxima Duchense (pumpkin) seeds on streptozotocin induced diabetic rats. J Pharmacogn Phytochem 1(6):108–116
Kalaivani A, Sathibabu Uddandrao V, Brahmanaidu P, Saravanan G, Nivedha P, Tamilmani P, Swapna K, Vadivukkarasi S (2018) Anti obese potential of Cucurbita maxima seeds oil: effect on lipid profile and histoarchitecture in high fat diet induced obese rats. Nat Prod Res 32(24):2950–2953
Kushawaha DK, Yadav M, Chatterji S, Srivastava AK, Watal G (2017) Evidence based study of antidiabetic potential of C. maxima seeds–in vivo. J Tradit Complement Med 7(4):466–470
Al-Shaheen SJA, Kaskoos RA, Hamad KJ, Ahamad J (2013) In-vitro antioxidant and a-amylase inhibition activity of Cucurbita maxima. J pharmacogn phytochem 2(2):121
Mallick N, Khan RA (2015) Effect of Citrus paradisi and Citrus sinensis on glycemic control in rats. J Pharm Pharmacol 9(3):60–64
Muhtadi H, Azizah T, Suhendi A, Yen KH (2015) Antidiabetic and antihypercholesterolemic activities of Citrus sinensis peel: in vivo study. Natl J Physiol Pharm Pharmacol 5(5):382–385
Muhammad N, Soji-Omoniwa O, Usman L, Omoniwa B (2013) Antihyperglycemic activity of leaf essential oil of Citrus sinensis (L.) Osbeck on alloxan-induced diabetic rats. Annu Res Rev Biol. 3:825–834
Boris AKG, Imelda DN, Wilfried KT, Guy T, Ngondi JL, Oben J (2017) Phytochemical screening and anti-diabetic evaluation of Citrus sinensis stem bark extracts. Int J Biochem Res Rev. 17:1–13
Chilaka K, Ifediba E, Ogamba J (2015) Evaluation of the effects of Citrus sinensis seed oil on blood glucose, lipid profile and liver enzymes in rats injected with alloxan monohydrate. J Acute Dis 4(2):129–134
Chien SC, Young PH, Hsu YJ, Chen CH, Tien YJ, Shiu SY, Li TH, Yang CW, Marimuthu P, Tsai LF (2009) Anti-diabetic properties of three common Bidens pilosa variants in Taiwan. Phytochemistry 70(10):1246–1254
Hsu YJ, Lee TH, Chang CL, Huang YT, Yang WC (2009) Anti-hyperglycemic effects and mechanism of Bidens pilosa water extract. J Ethnopharmacol 122(2):379–383
Liang YC, Lin CJ, Yang CY, Chen YH, Yang MT, Chou FS, Yang WC, Chang CL (2020) Toxicity study of Bidens pilosa in animals. J Tradit Complement Med 10(2):150–157
Dhar M, Dhar M, Dhawan B, Mehrotra B, Ray C (1968) Screening of Indian plants for biological activity: part I. Indian J Exp Biol 6(4):232–247
Du Plessis LH, Hamman JH (2014) In vitro evaluation of the cytotoxic and apoptogenic properties of aloe whole leaf and gel materials. Drug Chem Toxicol 37(2):169–177
Guo X, Mei N (2016) Aloe vera: a review of toxicity and adverse clinical effects. J Environ Sci Health C 34(2):77–96
Okyar A, Can A, Akev N, Baktir G, Sütlüpinar N (2001) Effect of Aloe vera leaves on blood glucose level in type I and type II diabetic rat models. Phytother Res 15(2):157–161
Zhou Y, Feng Y, Wang H, Yang H (2003) 90-day subchronic toxicity study of aloe whole-leaf powder. Wei Sheng Yan Jiu. 32(6):590–593
Luka C, Tijjani H (2013) Comparative studies of the aqueous extracts of Ocimum gratissimum, Aloe vera, Brassica oleracea and Ipomoea batatas on some biochemical parameters in diabetic rats. IOSR J Pharm Biol Sci 6(3):23–29
Yongchaiyudha S, Rungpitarangsi V, Bunyapraphatsara N, Chokechaijaroenporn O (1996) Antidiabetic activity of Aloe vera L. juice. I. Clinical trial in new cases of diabetes mellitus. Phytomedicine 3(3):241–243
Can A, Akev N, Ozsoy N, Bolkent S, Arda BP, Yanardag R, Okyar A (2004) Effect of Aloe vera leaf gel and pulp extracts on the liver in type-II diabetic rat models. Biol Pharm Bull 27(5):694–698
Tanaka M, Misawa E, Ito Y, Habara N, Nomaguchi K, Yamada M, Toida T, Hayasawa H, Takase M, Inagaki M (2006) Identification of five phytosterols from Aloe vera gel as anti-diabetic compounds. Biol Pharm Bull 29(7):1418–1422
Boyom FF, Fokou PVT, Yamthe LRT, Mfopa AN, Kemgne EM, Mbacham WF, Tsamo E, Zollo PHA, Gut J, Rosenthal PJ (2011) Potent antiplasmodial extracts from Cameroonian Annonaceae. J Ethnopharmacol 134(3):717–724
Coria-Téllez AV, Montalvo-Gónzalez E, Yahia EM, Obledo-Vázquez EN (2018) Annona muricata: a comprehensive review on its traditional medicinal uses, phytochemicals, pharmacological activities, mechanisms of action and toxicity. Arab J Chem 11(5):662–691
Florence NT, Benoit MZ, Jonas K, Alexandra T, Désiré DDP, Pierre K, Théophile D (2014) Antidiabetic and antioxidant effects of Annona muricata (Annonaceae), aqueous extract on streptozotocin-induced diabetic rats. J Ethnopharmacol 151(2):784–790
Adewole S, Ojewole J (2009) Protective effects of Annona muricata Linn. (Annonaceae) leaf aqueous extract on serum lipid profiles and oxidative stress in hepatocytes of streptozotocin-treated diabetic rats. Afr J Tradit Complement Altern Med 6(1):30
Adeyemi D, Komolafe O, Adewole S, Obuotor E (2009) Anti hyperlipidemic activities of Annona muricata (Linn). Internet J Altern Med 7(1):1–9
Al Syaad K, Elsaid F, Abdraboh M, Al-Doaiss A (2019) Effect of graviola (Annona muricata l.) and ginger (Zingiber officinale roscoe) on diabetes mellitus induced in male wistar albino rats. Folia Biol 65(5/6):275–284
Agu KC, Eluehike N, Ofeimun RO, Abile D, Ideho G, Ogedengbe MO, Onose PO, Elekofehinti OO (2019) Possible anti-diabetic potentials of Annona muricata (soursop): inhibition of α-amylase and α-glucosidase activities. Clin Phytosci 5(1):1–13
Champy P, Melot A, Guérineau Eng V, Gleye C, Fall D, Höglinger GU, Ruberg M, Lannuzel A, Laprévote O, Laurens A (2005) Quantification of acetogenins in Annona muricata linked to atypical parkinsonism in Guadeloupe. Mov Disord 20(12):1629–1633
Deutschländer M, Van de Venter M, Roux S, Louw J, Lall N (2009) Hypoglycaemic activity of four plant extracts traditionally used in South Africa for diabetes. J Ethnopharmacol 124(3):619–624
Beseni BK, Matsebatlela TM, Bagla VP, Njanje I, Poopedi K, Mbazima V, Mampuru L, Mokgotho MP (2019) Potential antiglycation and hypoglycaemic effects of Toona ciliata M. Roem. and Schkuhria pinnata Lam. Thell. crude extracts in differentiated C2C12 cells. Evid-based Complement Altern Med. 2019:5406862
Lacroix D, Prado S, Kamoga D, Kasenene J, Namukobe J, Krief S, Dumontet V, Mouray E, Bodo B, Brunois F (2011) Antiplasmodial and cytotoxic activities of medicinal plants traditionally used in the village of Kiohima, Uganda. J Ethnopharmacol 133(2):850–855
Bello S, Muhammad B, Gammaniel K, Abdu-Aguye I, Ahmed H, Njoku C, Pindiga U, Salka A (2005) Preliminary evaluation of the toxicity and some pharmacological properties of the aqueous crude extract of Solanum melongena. Res J Agric Biol Sci 1(1):1–9
Kwon Y-I, Apostolidis E, Shetty K (2008) In vitro studies of eggplant (Solanum melongena) phenolics as inhibitors of key enzymes relevant for type 2 diabetes and hypertension. Bioresour Technol 99(8):2981–2988
Tandi J, Danthy R, Kuncoro H (2019) Effect of ethanol extract from purple eggplant skin (Solanum melongena L.) on blood glucose levels and pancreatic Β cells regeneration on white rats male hypercholesterolemia-diabetic. Res J Pharm Technol 12(6):2936–2942
Khazaei F, Ghanbari E, Rezvani A, Ghanbari S, Khazaei M (2020) Improvement of blood glucose, serum antioxidant status and liver enzyme changes by hydroalcoholic extract of Solanum melongena green cap in diabetic rats. Res J Pharmacogn 7(4):49–55
Irudayaraj SS, Sunil C, Duraipandiyan V, Ignacimuthu S (2012) Antidiabetic and antioxidant activities of Toddalia asiatica (L.) Lam. leaves in streptozotocin induced diabetic rats. J Ethnopharmacol 143(2):515–523
Mekap SK, Sahoo S, Satapathy KB, Mishra SK (2016) Evaluation of Toddalia asiatica (L.) Lam leaf extracts for antidiabetic activity. Pharm Biol Eval. 3(1):115–125
Ezike AC, Akah PA, Okoli CC, Okpala CB (2010) Experimental evidence for the antidiabetic activity of Cajanus cajan leaves in rats. JBCP 1(2):81
Tang R, Tian R-h, Cai J-z, Wu J-h, Shen X-l, Hu Y-j (2017) Acute and sub-chronic toxicity of Cajanus cajan leaf extracts. Pharm Biol 55(1):1740–1746
Aja P, Igwenyi I, Okechukwu P, Orji O, Alum E (2015) Evaluation of anti-diabetic effect and liver function indices of ethanol extracts of Moringa oleifera and Cajanus cajan leaves in alloxan induced diabetic albino rats. Glob Vet 14(3):439–447
Uchegbu NN, Ishiwu CN (2016) Germinated pigeon pea (Cajanus cajan): a novel diet for lowering oxidative stress and hyperglycemia. Food Sci Nutr 4(5):772–777
Ariviani S, Affandi D, Listyaningsih E, Handajani S (2018) The potential of pigeon pea (Cajanus cajan) beverage as an anti-diabetic functional drink. IOP Conf Ser Earth Environ Sci. 1:012054
Fennell C, Lindsey K, McGaw L, Sparg S, Stafford G, Elgorashi E, Grace O, Van Staden J (2004) Assessing African medicinal plants for efficacy and safety: pharmacological screening and toxicology. J Ethnopharmacol 94(2–3):205–217
Muyenga T, Muungo L, Prashar L, Bwalya A (2015) The effect of Kigelia africana fruit extract on blood glucose in diabetes induced mice. JMST 4(3):201–206
Fagbohun OF, Olawoye B, Ademakinwa AN, Jolayemi KA, Msagati TA (2020) Metabolome modulatory effects of Kigelia africana (Lam.) Benth. fruit extracts on oxidative stress, hyperlipidaemic biomarkers in STZ-induced diabetic rats and antidiabetic effects in 3T3 L1 adipocytes. J Pharm Pharmacol 72(12):1798–1811
Farah HM, El Hussein AM, Khalid HE, Osman HM (2017) Toxicity of Kigelia africana fruit in rats. Adv Res 12(6):1–9
Lampiao F, Kafukiza S, Msowoya D, Phiri T, Wyson L, Alfazema L (2018) Evaluation of the hypoglycaemic potential of Kigelia africana fruit powder being sold in Malawian retail pharmacies. Afr J Tradit Complement Altern Med 15(3):27–30
Swarnalatha K, Babu CVK, Babu BH (2019) Phytochemical screening, anti-diabetic and anti-oxidant activities of Kigelia africana (LAM.) and Sterculia foetida L. Rasayan J Chem 12:907–914
Emmanuel U (2019) Oxidative and biochemical parameters analysis of alloxan-induced diabetic rats administered methanol leaf and fruit extracts of Kiglia africana. LJRS 19(3):1
Ufodike E, Omoregie E (1994) Acute toxicity of water extracts of barks of Balanites aegyptiaca and Kigelia africana to Oreochromis niloticus (L.). Aquacult Res. 25(9):873–879
Garba HA, Mohammed A, Ibrahim MA, Shuaibu MN (2020) Effect of lemongrass (Cymbopogon citratus Stapf) tea in a type 2 diabetes rat model. Clin Phytoscience 6(1):1–10
Bharti S, Kumar A, Prakash O, Krishnan S, Gupta A (2013) Essential oil of Cymbopogon citratus against diabetes: validation by vivo experiments and computational studies. J Bioanal Biomed 5(5):194–203
Fandohan P, Gnonlonfin B, Laleye A, Gbenou J, Darboux R, Moudachirou M (2008) Toxicity and gastric tolerance of essential oils from Cymbopogon citratus, Ocimum gratissimum and Ocimum basilicum in Wistar rats. Food Chem Toxicol 46(7):2493–2497
Lulekal E, Tesfaye S, Gebrechristos S, Dires K, Zenebe T, Zegeye N, Feleke G, Kassahun A, Shiferaw Y, Mekonnen A (2019) Phytochemical analysis and evaluation of skin irritation, acute and sub-acute toxicity of Cymbopogon citratus essential oil in mice and rabbits. Toxicol Rep 6:1289–1294
Ademuyiwa AJ, Elliot SO, Olamide OY, Omoyemi AA, Funmi OS (2015) The effects of Cymbopogon citratus (lemon grass) on the blood sugar level, lipid profiles and hormonal profiles of Wistar albino rats. Am J Pharmacol Toxicol 1(1):8–18
Trilochana Y, Babu DJM, Rao PR (2017) The study of anti-diabetic activity of aqueous extract of root of Gynandropsis gynandra in diabetic rats. IJRPB 5(1):13
Nagesh AHA, Pilli Y, Bhanubee P (2012) Phytochemical and hypoglycemic evaluation of Gynandropsis gynandra root extract. J Biol Act Prod Nat 2(1):38–45
Bharathi MN, Srinivas K, Bangaruthalli J, Pradesh A (2020) Phytochemical screeing and invitro antidiabetic activity of Cleome gynandra. Pak J Nutr. https://doi.org/10.3923/pjn.2020.153.159
Singh A, Marar T (2011) Inhibitory effect of extracts of Syzygium cumini and Psidium guajava on glycosidases. JCTR 11(1):2535
Bandiola T, Ignacio GB, Yunson E, Bandiola P (2017) Syzygium cumini (L.) Skeels: a review of its phytochemical constituents, toxicity studies, and traditional and pharmacological uses. Int J Appl Pharm Biol Res. 2(6):15–23
Sari AN, Januardi J, Diningrat DS (2020) Effect of ethanol extract of Jamblang Aceh (Syzygium cumini) in diabetic mice (Mus musculus) and its potential as anti-diabetic agent. Elkawnie. 6(1):37–47
Silva SdN, Abreu IC, Silva GFC, Ribeiro RM, Lopes AdS, Cartágenes MdSdS, Freire SMdF, Borges ACR, Borges MOdR (2012) The toxicity evaluation of Syzygium cumini leaves in rodents. Rev Bras Farmacogn 22(1):102–108
Bhuyan ZA, Rokeya B, Masum N, Hossain S, Mahmud I (2010) Antidiabetic effect of Syzygium cumini L. seed on type 2 diabetic rats. Dhaka Univ J Biol Sci. 19(2):157–164
Swami U, Rishi P, Soni SK (2017) Anti-diabetic, hypolipidemic and hepato-renal protective effect of a novel fermented beverage from Syzygium cumini stem. Int J Pharm Sci Res 8(3):1336
Pandhare RB, Sangameswaran B, Mohite PB, Khanage SG (2011) Antidiabetic activity of aqueous leaves extract of Sesbania sesban (L.) Merr. in streptozotocin induced diabetic rats. Avicenna J Med Biotechnol. 3(1):37
Aggarwal N, Gupta P (2012) Effect of petroleum ether extract of Sesbania sesban (Merr.) roots in streptozotocin (STZ) induced diabetes in mice. Asian Pac J Trop Biomed 2(3):S1254–S1260
Agunbiade O, Ojezele O, Ojezele J, Ajayi A (2012) Hypoglycaemic activity of Commelina africana and Ageratum conyzoides in relation to their mineral composition. Afr Health Sci 12(2):198–203
Atawodi SE, Adepoju OA, Nzelibe HC (2017) Antihyperglycaemic and hypolipidemic effect of methanol extracts of Ageratum conyzoides L. (Asteraceae) in normal and diabetic rats. Trop J Pharm Res 16(5):989–996
Diallo A, Eklu-Gadegkeku K, Agbono A, Aklikokou K, Creppy EE, Gbeassor M (2010) Acute and sub-chronic (28-day) oral toxicity studies of hydroalcohol leaf extract of Ageratum conyzoides L. (Asteraceae). Trop J Pharm Res 9(5):463
Moura A, Silva E, Fraga M, Wanderley A, Afiatpour P, Maia M (2005) Antiinflammatory and chronic toxicity study of the leaves of Ageratum conyzoides L. in rats. Phytomedicine 12(1–2):138–142
Agbafor KN, Engwa G, Ude C, Obiudu I, Festus B (2015) The effect of aqueous leaf extract of Ageratum conyzoides on blood glucose, creatinine and calcium ion levels in albino rats. J pharm chem biol sci 3(3):408–415
Nyunaı N, Abdennebi E, Bickii J (2015) Subacute antidiabetic properties of Ageratum conyzoides leaves in diabetic rat. Int J Pharm Sci Res 6(4):1378–1387
Moloto MR, Phan ADT, Shai JL, Sultanbawa Y, Sivakumar D (2020) Comparison of phenolic compounds, carotenoids, amino acid composition, in vitro antioxidant and anti-diabetic activities in the leaves of seven cowpea (Vigna unguiculata) cultivars. Foods 9(9):1285
Barnes MJ, Uruakpa F, Udenigwe C (2015) Influence of cowpea (Vigna unguiculata) peptides on insulin resistance. J Nutr Health Food Sci. https://doi.org/10.15226/jnhfs.2015.00144
Ashraduzzaman M, Alam M, Khatun S, Banu S, Absar N (2011) Vigna unguiculata linn. Walp. Seed oil exhibiting antidiabetic effects in alloxan induced diabetic rats. Malays J Pharm Sci. 9(1):13–23
Kanetro B (2015) Hypocholesterolemic properties of protein isolate from cowpeas (Vigna unguiculata) sprout in normal and diabetic rats. Proced Food Sci 3:112–118
Tazin TQ, Rumi JF, Rahman S, Al-Nahain A, Jahan R, Rahmatullah M (2014) Oral glucose tolerance and antinociceptive activity evaluation of methanolic extract of Vigna unguiculata ssp. unguiculata beans. World J Pharm Pharmaceut Sci. 3(8):28–37
Nyarko A, Sittie A, Addy M (1993) The basis for the antihyperglycemic activity of Indigofera arrecta in the rat. Phytother Res 7(1):1–4
Addy ME, Addo P, Nyarko A (1992) Indigofera arrecta prevents the development of hyperglycaemia in the db/db mouse. Phytother Res 6(1):25–28
Addy ME, Nyarko AK (1988) Diabetic patients’ response to oral administration of aqueous extract of Indigofera arrecta. Phytother Res 2(4):192–195
Omara T, Kiprop AK, Ramkat RC, Cherutoi J, Kagoya S, Moraa Nyangena D, Azeze Tebo T, Nteziyaremye P, Nyambura Karanja L, Jepchirchir A (2020) Medicinal plants used in traditional management of cancer in Uganda: a review of ethnobotanical surveys, phytochemistry, and anticancer studies. Evid Based Complement Altern Med. 2020:1
Chivandi E, Cave E, Davidson BC, Erlwanger KH, Moyo D, Madziva MT (2012) Suppression of Caco-2 and HEK-293 cell proliferation by Kigelia africana, Mimusops zeyheri and Ximenia caffra seed oils. In Vivo 26(1):99–105
Obakiro SB, Kiprop A, Kigondu E, K’Owino I, Odero MP, Manyim S, Omara T, Namukobe J, Owor RO, Gavamukulya Y (2021) Traditional medicinal uses, phytoconstituents, bioactivities, and toxicities of Erythrina abyssinica Lam. ex DC (fabaceae): a systematic review. Evid Based Complement Altern Med. 2021:1
Ndhlala AR, Ncube B, Okem A, Mulaudzi RB, Van Staden J (2013) Toxicology of some important medicinal plants in southern Africa. Food Chem Toxicol 62:609–621
Nyarko AK, Ankrah NA, Ofosuhene M, Sittie AA (1999) Acute and subchronic evaluation of Indigofera arrecta: absence of both toxicity and modulation of selected cytochrome P450 isozymes in ddY mice. Phytother Res 13(8):686–688
Obakiro SB, Kiprop A, Kowino I, Kigondu E, Odero MP, Omara T, Bunalema L (2020) Ethnobotany, ethnopharmacology, and phytochemistry of traditional medicinal plants used in the management of symptoms of tuberculosis in East Africa: a systematic review. Trop Med Health 48(1):1–21
Ekor M (2014) The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol 4:177
Acknowledgements
Not applicable.
Funding
Development of Sustainable Application funded this research for Standard Herbal Resources [grant number, KSN2021320], Korea Institute of Oriental Medicine through the Ministry of Science and ICT, Republic of Korea.
Author information
Authors and Affiliations
Contributions
RG conceptualized the review article, performed all the literature search based on the methodology, conducted data analysis, and wrote the original draft of the article. MM reviewed and edited the manuscript after due conceptualization of the review. DO reviewed and edited the manuscript. YK supervised the whole research work, reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gang, R., Matsabisa, M., Okello, D. et al. Ethnomedicine and ethnopharmacology of medicinal plants used in the treatment of diabetes mellitus in Uganda. Appl Biol Chem 66, 39 (2023). https://doi.org/10.1186/s13765-023-00797-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13765-023-00797-z