Abstract
Background
Compared to developed countries, the use of antimicrobials in Egypt is less regulated and is available over the counter without the need for prescriptions. The impact of such policy on antimicrobial resistance has not been studied. This study aimed to determine the prevalence of early and late onset sepsis, and the frequency of antimicrobial resistance in a major referral neonatal intensive care unit (NICU).
Methods
The study included all neonates admitted to the NICU over a 12-month period. Prospectively collected clinical and laboratory data were retrieved, including blood cultures and endotracheal aspirate cultures if performed.
Results
A total of 953 neonates were admitted, of them 314 neonates were diagnosed with sepsis; 123 with early onset sepsis (EOS) and 191 with late onset sepsis (LOS). A total of 388 blood cultures were obtained, with 166 positive results. Total endotracheal aspirate samples were 127; of them 79 were culture-positive. The most frequently isolated organisms in blood were Klebsiella pneumoniae (42%) and Coagulase negative staphylococcus (19%) whereas in endotracheal cultures were Klebsiella pneumoniae (41%) and Pseudomonas aeruginosa (19%). Gram negative organisms were most resistant to ampicillins (100%), cephalosporins (93%–100%) and piperacillin-tazobactam (99%) with less resistance to aminoglycosides (36%–52%). Gram positive isolates were least resistant to vancomycin (18%). Multidrug resistance was detected in 92 (38%) cultures, mainly among gram negative isolates (78/92).
Conclusions
Antibiotic resistance constitutes a challenge to the management of neonatal sepsis in Egypt. Resistance was predominant in both early and late onset sepsis. This study supports the need to implement policies that prohibits the non-prescription community use of antibiotics.
Similar content being viewed by others
Background
Neonatal sepsis is a major health problem worldwide [1]. Neonates are more at risk for bacterial sepsis, with a global prevalence of 1 to 10 per 1000 live births [2]. Sepsis problem is much higher in the developing than in the developed countries, with sepsis-related mortality rate as high as 50% for untreated newborns.
Neonatal sepsis is a clinical syndrome in an infant 28 days of life or younger, manifesting with a diversity of non-specific systemic signs and symptoms and isolation of a pathogen from the bloodstream [3]. According to inception, early onset sepsis (EOS) refers to infections during the first 72 h of life that is usually related to intrapartum transmission from mothers; whereas late onset sepsis (LOS) refers to postnatal acquisition of infections after the first 3 days of life [4]. Pathogens encountered in neonatal sepsis vary worldwide; reports from developing countries more commonly show Gram negative organisms [5, 6], although Gram positive organisms have been also reported [6,7,8]. The susceptibility patterns for early neonatal sepsis typically differs from late neonatal sepsis; more resistant organisms are expected from hospital acquired late sepsis when compared to vertically transmitted, community acquired, early sepsis. However, a report from a developing country showed some resistant organisms to cause early neonatal sepsis [9]. Resistant organisms can potentially grow in the community with inappropriate use of antibiotics that is typical in some developing countries. Therefore, in this current study, investigators aimed to examine the microbiological patterns of early and late neonatal sepsis and to specify their antibiotic susceptibility.
Methods
Patients
This is a retrospective study of a prospectively collected data at the neonatal intensive care unit (NICU) of Cairo University Children’s Hospital in Egypt, conducted over a 12-month- period. The study was approved by the Ethical Committee of the hospital. Infants were included if they were diagnosed with microbiological bacteremia, and/or clinical sepsis that was accompanied by non-microbiological laboratory values suggestive of infections. Infants were considered to have sepsis if they had a score of 3 or more of the following hematologic findings: i) abnormal total leucocyte count, ii) abnormal total neutrophil (PMN) count, iii) increased immature PMN count, iv) increased immature to total PMN ratio, v) immature to mature PMN ratio ≥ 0.3, vi) platelets count ≤150,000/mm3, and vii) pronounced degenerative changes in PMNs [10]. Infants were classified into two groups according to the timing of sepsis diagnosis: EOS diagnosed ≤72 h of life and LOS diagnosed >72 h of life. Demographic, clinical, and laboratory data were retrieved for all included infants.
Infectious control management
All admitted infants received a limited sepsis work up that included complete blood count, C-reactive protein, and blood culture. Empiric parenteral antibiotics were initiated for 3 days while awaiting blood culture results. Sepsis work ups were repeated during hospital stay whenever an infant displayed clinical signs suggestive for sepsis. Infants were considered to have bloodstream infection if they had at least one blood culture positive for organisms known to cause bacteremia [11]. For other organisms that may cause true bacteremia or may represent skin contamination, infection was considered if the same organism was recorded from at least two blood cultures. Endotracheal aspirate (ETA) cultures were occasionally obtained from mechanically ventilated cases if they displayed clinical signs suggestive of ventilator associated pneumonia such as increased oxygen requirement, increased ventilator support settings, worsening radiographic findings, and changes in tracheal aspirate volume, color or consistency.
Microbiological sampling
For blood cultures, at least 1 ml of blood sample was obtained from a peripheral vein under aseptic precautions. Blood samples were incubated in blood culture incubator (BACTEC- 9050, Beckton-Dickenson, Franklin Lakes, New Jersey, USA). ETA samples were obtained by direct endotracheal suction of respiratory secretions using sterile endotracheal suction catheters into sterile suction trap.
Sample processing
Specimens were processed on arrival to the laboratory. Enriched media used included: blood, MacConkey and chocolate agar plates. These were inoculated, incubated at 37 °C, and examined for growth at 24–48 h. Isolates, if any, were identified by: Gram staining, colony characteristics, and biochemical properties including catalase, DNAse agar, mannitol salt agar, and hemolysis on blood agar plates, for Gram positive isolates, and triple sugar iron (TSI), lysine iron agar (LIA), motility indole, ornithine (MIO), citrate, urease and oxidase for Gram negative bacilli [12]. All media and biochemical reactions were systematically quality controlled according to the standards by the American Type Culture Collection. Antibiotic susceptibility tests were performed by Kerby-Bauer disc diffusion method according to the standards of Clinical and Laboratory Standards Institute (CLSI). The antibiotic discs used represented different groups of antibiotics. The inhibition zones were measured and interpreted according to the CLSI recommendations [13]. Multi drug resistant (MDR) bacteria were defined by resistance to three or more antimicrobial classes [14].
Statistical analysis
All statistical procedures were performed using the Statistical Package for Social Science (SPSS) for windows version 16.0 (SPSS Inc., Chicago, Illinois, USA). Descriptive analyses were expressed as mean ± standard deviation (SD) for quantitative variables, and percentages (%) for categorical variables. Differences in distribution for categorical variables were done using the Chi square test.
Results
Nine hundred fifty three cases were admitted during the study period; of them 314 (32.9%) neonates were diagnosed with sepsis based on clinical signs and/or microbiological laboratory. Early onset sepsis was detected in 123 cases and late onset sepsis in 191 cases. The characteristics of the study population are presented in Table 1. Seventy-seven cases were admitted solely for sepsis whereas 237 had other associated morbidities as shown in Table 2. Sepsis presented more frequently in males than females (178 vs. 136).
A total of 388 blood specimens were cultured from our 314 septic neonates, with more than one culture obtained from the same case in some occasions, with 166 microbiologically positive cultures; of them 49 cultures for cases with EOS and 117 cultures for cases with LOS. The most common organisms for EOS and LOS were gram negative bacilli (31/49 and 87/117 respectively), mainly Klebsiella pneumoniae spp. (n = 20 for EOS, and 49 for LOS). Table 3 represents the isolated organisms in the studied population.
A total of 127 endotracheal aspirates (ETA) were obtained during the study period from 58 patients with 79 positive cultures; of them 24 cultures belonged to cases with EOS and 55 with LOS. The most prominent organisms in ETA cultures were Klebsiella pneumoniae in cases with EOS (22/24) and Pseudomonas aeruginosa (21/55) in LOS cases (Table 4). Organisms isolated from ETA cultures differed from those in blood cultures in 29% of cases.
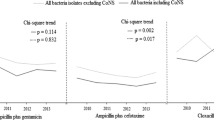
Antimicrobial sensitivity and resistance patterns were assessed for all 245 isolated bacteria; 166 blood cultures and 79 ETA cultures. Tables 5 and 6 present the susceptibility patterns of gram negative bacilli and gram positive cocci respectively. Gram negative bacilli showed highest resistance to ampicillins (ampicillin- sulbactam, 100% and amoxicillin-clavulanate, 97%), cephalosporins (cefotaxime, 93%, ceftazidime, 96%, cefoperazone, 95%, ceftriaxone, 99%, cefuroxime, 100%), and piperacillin-tazobactam, 99%. Less resistance was evident to aminoglycosides, mainly amikacin (36%) and gentamicin (52%), as well as carbapenems (imipenem, 26% and meropenem, 64%). Least resistance to quinolones (levofloxacin, 24%). Gram positive cocci showed highest resistance to ampicillins (amoxicillin-sulbactam, 100% and amoxicillin-clavulanate, 75%), cephalosporins (ceftazidime, 94%, cefoperazone, 100%, cefepime, 86%, ceftriaxone, 100%, cefuroxime, 100%, cefoxitin, 80%), carbapenems (imipenem, 84%, meropenem, 86%), piperacillin-tazobactam (100%), and erythromycin (86%). Less resistance was evident to aminoglycosides (amikacin, 49%, gentamicin, 57%), quinolones (ciprofloxacin, 77%, levofloxacin, 75%), clindamycin (53%), and rifampicin (49%). Least resistance among gram positive bacteria was found to vancomycin (18%). Multidrug resistance was detected in 67 cases; 18 with EOS and 49 with LOS, and in 92 (37.6%) cultures, mainly among gram negative isolates (78/92).
Discussion
Neonatal sepsis, a life-threatening condition, needs immediate empirical antimicrobial therapy. It is important to choose an antibiotic combination that covers the most common pathogens [15]. Blood culture remains the gold standard for diagnosis of neonatal sepsis, despite its low sensitivity which may be due to small volume of blood sample, or empirical antibiotics prior to sampling [16].
We observed the emergence of multi drug resistance among cases of EOS, which has not been frequently mentioned. A previous study from India stated that multidrug resistant organisms were leading causes of early as well as late onset sepsis [17]. Even studies from Egypt addressing this problem studied multi drug resistance either collectively [18] or in relation to late onset sepsis only [19]. The worrisome rise in levels of antimicrobial resistance among pathogens retrieved from NICUs highlight the needs for better understanding of the problem of early onset sepsis and implementing strategies to combat, especially in countries with limited resources [20].
In the current study, the overall incidence of suspected sepsis was 32.9%. These results are comparable to other studies from Egypt [21, 22], but are better than a previous report in 2001 wherein the rate of sepsis exceeded 50% [23], which may be due to better awareness and adherence to infection control measures.
In this study, the overall mortality in septic neonates was 22.3%. This value is lower than sepsis related deaths reported in other studies from Egypt [21, 23], however, several studies reviewed from different developing countries showed a wide range of infection related neonatal mortality ranging between 8 and 80% [24]. A sepsis related mortality of 19% was reported in studies from east Africa [25, 26].
In this work, the incidence of LOS was higher than that of EOS. Comparable findings were reported in other studies from Egypt and South Africa [21, 27]. The opposite was found in studies from Nepal [28] and Iran [29].
Suspected sepsis was confirmed by blood culture, yielding different bacterial growths in only 166/388 cultures (42.8%). This rate is in the vicinity to those of other studies from Egypt [21] and other developing African and Asian countries [25, 30]. Despite being the gold standard for diagnosing sepsis, blood cultures suffer from low sensitivity, postulated reasons include prior use of antibiotics, insufficient or wrong sampling, poor transport conditions, and slow-growing or fastidious bacteria [31]. Also, some culture negative patients might be due to non-bacterial causes as fungi, viruses and parasites [32]. ETA cultures yielded matching results to blood cultures in 38% of simultaneous cultures and grew different organisms in 29% of cases. Authors showed ETA cultures to be of no value in predicting pathogens causing septicemia in ventilated infants [33]. Higher percentages of matching cultures in this study may be explained by higher simultaneous negative cultures.
Gram negative bacilli were more frequently encountered than gram positive cocci, with Klebsiella pneumoniae being the most commonly isolated organism both in blood and ETA cultures (42% and 41% respectively),. These results were consistent in multiple reports from Egypt over two decades [22, 34, 35]. However, other reports from Egypt showed CONS as the leading cause of sepsis in 2006 [36], 2010/2011 [37], and 2011/2012 [21]. These results support the fact that the diversity of organisms causing sepsis varies from region to another and changes over time even in the same place [38].
The frequency of gram negative pathogens varied from 31% to 63% with Klebsiella pneumoniae, Pseudomonas aeruginosa and Escherichia coli being the predominant organisms in almost all countries of Latin America [39]. Several other studies in a diversity of developing countries showed that gram negative bacteria were responsible for most cases of neonatal sepsis [29, 30, 40, 41]. Although some authors state that gram-positive bacteria are the most commonly encountered in NICU patients [42, 43], yet case fatalities are highest for gram-negatives [44]. Others have indicated increasing incidence of gram-negative bacterial infections in NICUs [45].
Among gram negative organisms, Klebsiella pneumoniae is increasingly emerging as a common bacteria in hospital settings [46].
The first line of empirical treatment in this NICU is Ampicillin-sulbactam combined with cephalosporins or aminoglycosides. In the absence of clinical improvement, antibiotics are changed to carbapenems and vancomycin until the blood culture results are available. Quinolones are used in culture-proven sepsis with multidrug resistant organisms. In this study, gram negative organisms were most resistant to ampicillins, cephalosporins, and piperacillin- tazobactam. Less resistance was observed to aminoglycosides and carbapenems with least resistance to levofloxacin. Several studies showed high resistance to ampicillin and amoxicillin, aminoglycosides, and different classes of cephalosporins [41, 47]. Even within the aminoglycoside spectrum, some authors found amikacin (which was less used in their units) more sensitive than gentamicin (which was more commonly used) [47]. Two studies in sub-Saharan Africa and Asia revealed resistance of the two common pathogens Klebsiella and Staphylococcus aureus to almost all commonly used antibiotics in one study [48], and Klebsiella pneumoniae median resistance to ampicillins and cephalosporins in 94 and 84% of cases in Asia and 100 and 50% in Africa [49] in the other study. Although short courses of antimicrobials as carbapenems and cephalosporins especially third generation cover a broad spectrum of bacteria, yet their extended use caused the emergence of extended spectrum β lactamase producing gram negative bacteria. This confers resistance to penicillins and cephalosporins and often coexisting with resistance to other categories of antibiotics as quinolones and aminoglycosides [50,51,52,53]. In Egypt, gram negative bacteria were resistant to ampicillin, amoxicillin clavulanate and cephalosporins, with highest sensitivity to either or both carbapenems and quinolones [21, 35, 37].
The increasing multidrug resistant gram negative bacteria with relative deficiency of new antibiotics to combat led to the revival of other classes of drugs as polymyxins, which are active against Acinetobacter species, Pseudomonas aeruginosa, Klebsiella species, and Enterobacter species [54].
In this work, gram positive organisms were most resistant to ampicillins (mainly ampicillin-sulbactam), a wide variety of cephalosporins (ceftazidime, cefoperazone, cefepime, ceftriaxone, cefoxitime, cefuroxime), carbapenems, piperacillin-tazobactam, and erythromycin. They were less resistant to aminoglycosides, quinolones, clindamycin, and rifampicin and least resistant to vancomycin.
In one study in India, rifampicin was effective against Staphylococcus aureus [55]. Other drugs as erythromycin show rising resistance among streptococci species (mainly group B streptococci, group A streptococci, Streptococcus pyogenes, and Streptococcus pneumoniae) and Staphylococcus aureus [56]. Similarly, in current work, erythromycin resistance was highest against Streptococcus pneumoniae, group B streptococci. There is an increasing incidence of multi drug resistant gram positive organisms [57], as well as increasing vancomycin resistant isolates [58], however; vancomycin still is an important first-line antimicrobial for treatment of serious infections as Methicillin-Resistant Staphylococcus aureus [59]. In our study, we found high resistance to fluoroquinolones among gram positive organisms. This resistance is emerging due to their extensive and increasing use in medical practice and was stated in the literature to be greatest in Staphylococcus aureus isolates especially methicillin resistant strains [60].
Conclusion
This study demonstrated a high prevalence of gram negative bacilli sepsis and tracheal colonization. Both gram negative bacilli and gram positive cocci were highly resistant to multiple broad-spectrum antimicrobials. Resistance was the highest against antibiotics used frequently in the NICU as the first line or the second line empirical treatment. It is worrisome to discover that pan drug resistance was not restricted to LOS; infants admitted from the community with early onset sepsis had a high resistance index to the multiple antibiotics. Of note, antibiotics in Egypt are available over the counter and do not require a physician’s prescription. This study calls for global regulations to restrict the use of antimicrobials in the community as well as in the hospital setting.
Abbreviations
- CLSI:
-
Clinical and Laboratory Standards Institute
- EOS:
-
Early onset sepsis
- ETA:
-
Endotracheal aspirate
- LIA:
-
Lysine iron agar
- LOS:
-
Late onset sepsis
- MDR:
-
Multi drug resistance
- MIO:
-
Motility indole ornithine
- NICU:
-
Neonatal ntensive Care Unit
- PMN:
-
Polymorph nuclear leucocytes
- spp.:
-
Species
- SPSS:
-
Statistical Package for Social Science
- TSI:
-
Triple sugar iron
References
Afroza S. Neonatal sepsis- a global problem: an overview. Mymensingh Med J. 2006;15(1):108–14.
Goldstein B, Giroir B, Randolph A. International consensus conference on pediatric sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8.
Edwards MS, Baker CJ. Sepsis in the newborn. In: Gershon AA, Hotez PJ, Katz SL, editors. Krugman’s infectious diseases of children. Philadelphia: Mosby; 2004. p. 545.
Bizzarro MJ, Dembry LM, Baltimore RS, Gallagher PG. Changing patterns in neonatal Escherichia coli sepsis and ampicillin resistance in the era of intrapartum antibiotic prophylaxis. Pediatrics. 2008;121(4):689–96.
Tallur SS, Kasturi AV, Nadgir SD, Krishna BV. Clinico-bacteriological study of neonatal septicemia in Hubli. Indian J Pediatr. 2000;67(3):169–74.
Karunasekera KA, Pathirana D. A preliminary study on neonatal septicaemia in a tertiary referral hospital paediatric unit. Ceylon Med J. 1999;44(2):81–6.
Karthikeyan G, Premkumar K. Neonatal sepsis: Staphylococcus aureus as the predominant pathogen. Indian J Pediatr. 2001;68(8):715–7.
Malik AS, Pennie RA. Early onset neonatal septicaemia in a level II nursery. Med J Malaysia. 1994;49(1):17–23.
Mahmood A, Karamat KA, Butt T. Neonatal sepsis: high antibiotic resistance of the bacterial pathogens in a neonatal intensive care unit in Karachi. J Pak Med Assoc. 2002;52(8):348–50.
Rodwell RL, Leslie AL, Tudehope DI. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988;112(5):761–7.
Villari P, Sarnataro C, Lacuzio L. Molecular epidemiology of Staphylococcus epidermidis in a neonatal intensive care unit over a three year period. J Clin Microbiol. 2000;38(5):1740–6.
Miller M, Holmes HT, Krisher K. Susceptibility test methods: dilution and disc diffusion methods. In: Murray PR, Pfaller MA, Jorgensen JH, Yolken RH, editors. Manual of clinical microbiology, vol. 118. 8th ed; 2003. p. 1526–43.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty- fifth informational supplement (M100-S25). Wayne: Clinical and Laboratory Standards Institute; 2015.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multi drug-resistant, extensively drug-resistant and pan drug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81.
Taheri PA, Eslamieh H, Salamati P. Is ceftizoxime an appropriate surrogate for amikacin in neonatal sepsis treatment? A randomized clinical trial. Acta Med Iran. 2011;49(8):499–503.
Kalathia MB, Shingala PA, Parmar PN, Parikh YN, Kalathia IM. Study of umbilical cord blood culture in diagnosis of early-onset sepsis among newborns with high-risk factors. J Clin Neonatol. 2013;2(4):169–72.
Viswanathan R, Singh AK, Basu S, Chatterjee S, Sardar S, Isaacs D. Multi-drug resistant gram negative bacilli causing early neonatal sepsis in India. Arch Dis Child Fetal Neonatal Ed. 2012;97(3):F182–7.
Awad HA, Mohamed MH, Badran NF, Mohsen M, Abd-Elrhman AS. Multidrug-resistant organisms in neonatal sepsis in two tertiary neonatal ICUs, Egypt. J Egypt Public Health Assoc. 2016;91(1):31–8.
Aamir MM, Abu El Wafa WM, Ali AE, Hamouda HM, Mourad FE. Prevalence of multidrug resistant bacteria causing late-onset neonatal sepsis. Int J Curr Microbiol App Sci. 2015;4(5):172–90.
Chaurasia S, Sankar MJ, Agarwal R, Yadav CP, Arya S, Investigators of the Delhi Neonatal Infection Study (DeNIS) collaboration. Characterization and antimicrobial resistance of sepsis pathogens in neonates born in tertiary care centres in Delhi, India: a cohort study. Lancet Glob Health. 2016;4:e752–60.
Moore KL, Kainer MA, Badrawi N, Afifi S, Wasfy M, Bashir M, et al. Neonatal sepsis in Egypt associated with bacterial contamination of glucose-containing intravenous fluids. Pediatr Infect Dis J. 2005;24(7):590–4.
Shehab El-Din ER, El-Sokkary MA, Bassiouny MR, Hassan R. Epidemiology of neonatal sepsis and implicated pathogens: a study from Egypt. Biomed Res Int. 2015; doi:10.1155/2015/509484.
Mohammed D, El Seifi OS. Bacterial nosocomial infections in neonatal intensive care unit, Zagazig university hospital, Egypt. Egyptian Pediatric Association Gazette. 2014;62:72–9.
Thaver D, Zaidi AK. Burden of neonatal infections in developing countries: a review of evidence from community-based studies. Pediatr Infect Dis J. 2009;28(1):3–9.
Mugalu J, Nakakeeto MK, Kiguli S, Kaddu-Mulindwa DH. Aetiology, risk factors and immediate outcome of bacteriologically confirmed neonatal septicaemia in Mulago hospital, Uganda. Afr Health Sci. 2006;6(2):120–6.
Singh SA, Dutta S, Narang A. Predictive clinical scores for diagnosis of late onset neonatal septicemia. J Trop Pediatr. 2003;49(4):235–9.
Motara F, Ballot DE, Perovic O. Epidemiology of neonatal sepsis at Johannesburg hospital. S Afr J Epidemiol Infect. 2005;20(3):90–3.
Jain NK, Jain VM, Maheshwari S. Clinical profile of neonatal sepsis. Kathmandu Univ Med J. 2003;1(2):117–20.
Movahedian AH, Moniri R, Mosayebi Z. Bacterial culture of neonatal sepsis. Iranian J Public Health. 2006;35(4):84–9.
Ahmed AS, Chowdhury MA, Hoque M, Darmstadt GL. Clinical and bacteriological profile of neonatal septicemia in a tertiary level pediatric hospital in Bangladesh. Indian Pediatr. 2002;39(11):1034–9.
Lever A, Mackenzie I. Sepsis: definition, epidemiology, and diagnosis. BMJ. 2007;335(7625):879–83.
Blanco J, Muriel-Bombin A, Sagredo V, Taboada F, Gandia F, Tamayo L, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care. 2008;12(6):R158.
Slagle TA, Bifano EM, Wolf JW, Gross SJ. Routine endotracheal cultures for the prediction of sepsis in ventilated babies. Arch Dis Child. 1989;64(1 Spec No):34–8.
El Badawy A, El Sebaie D, Khairat S, Fouad S. A study of microbiological pattern of neonatal sepsis. Alexandria J Pediatr. 2005;19(2):357–67.
Fahmey SS. Early-onset sepsis in a neonatal intensive care unit in Beni Suef, Egypt: bacterial isolates and antibiotic resistance pattern. Korean J Pediatr. 2013;56(8):332–7.
Abd el Haleim MM, Nawar NN, Abd el Rahman EM, Abo Hussein HH, Kamel NR. Epidemiologic and microbacteriologic study of neonatal septicaemia in Cairo University neonatal intensive care units. Res J Med Med Sci. 2009;4(1):67–77.
El Feky EA. Abd el Rahman Z, Mansi YA. Retrospective analysis of neonatal bacteremia and antimicrobial resistance pattern in neonatal intensive care unit. Res J Med Med Sci. 2011;6(2):62–8.
Shrestha S, Adhikari N, Rai BK, Shreepaili A. Antibiotic resistance pattern of bacterial isolates in neonatal care unit. J Nepal Med Assoc. 2010;50(180):277–81.
Berezin EN. Solorzano F; Latin America working group on bacterial resistance. Gram negative infections in pediatric and neonatal intensive care units in Latin America. J Infect Dev Ctries. 2014;8(8):942–53.
Aftab R, Iqbal I. Bacteriological agents of neonatal sepsis in NICU at Nishtar Hospital Multan. J Coll Physicians Surg Pak. 2006;16(3):216–9.
Rahman S, Hameed A, Roghani MT, Ullah Z. Multidrug resistant neonatal sepsis in Peshawar, Pakistan. Arch Dis Child Fetal Neonatal Ed. 2002;87(1):F52–4.
Anwer SK, Mustafa S, Pariyani S, Ashraf S, Taufiq KM. Neonatal sepsis: an etiologic study. J Pak Med Assoc. 2000;50(3):91–4.
Robillard PY, Nabeth P, Hulsey TC, Sergent MP, Perianin J, Janky E. Neonatal bacterial septicemia in a tropical area. Four-year experience in Guadeloupe (French West Indies). Acta Paediatr. 1993;82(8):687–9.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2Pt1):285–91.
Nambiar S, Singh N. Change in epidemiology of health care associated infections in a neonatal intensive care unit. Pediatr Infect Dis J. 2002;21(9):839–42.
Mannan MA, Shahidullah M, Noor MK, Dey AC, Nasrin N, Marma U. Nosocomial infections in a newborn intensive care unit of a tertiary care health. Bangladesh J Child Health. 2008;32:92–6.
Muhammad Z, Ahmed A, Hayat U, Wazir MS, Rafiyatullah, Waqas H. Neonatal sepsis: causative bacteria and their resistance to antibiotics. J Ayub Med Coll Abbottabad. 2010;22(4):33–6.
Sivanandan S, Soraisham AS, Swarnam K. Choice and duration of antimicrobial therapy for neonatal sepsis and meningitis. Int J Pediatr. 2011; doi:10.1155/2011/712150.
Le Doare K, Bielicki J, Heath PT, Sharland M. Systematic review of antibiotic resistance rates among gram negative bacteria in children with sepsis in resource limited countries. J Ped Infect Dis. 2014;4(1):11–20.
Patel SJ, Saiman L. Antibiotic resistance in neonatal intensive care unit pathogens: mechanisms, clinical impact, and prevention including antibiotic stewardship. Clin Perinatol. 2010;37(3):547–63.
Polin RA, Denson S. Brady MT; Committee on Fetus and Newborn; Committee on Infectious Diseases. Strategies for prevention of health care associated infections in the NICU. Pediatrics. 2012;129(4):e1085–93.
Gray JW, Ubhi H, Milner P. Antimicrobial treatment of serious gram negative infections in newborns. Curr Infect Dis Rep. 2014;16(2):400.
Isaacs D. Unnatural selection: reducing antibiotic resistance in neonatal units. Arch Dis Child Fetal Neonatal Ed. 2006;91(1):F72–4.
Falagas ME, Kasiakou SK. Colistin: the revival of Polymyxins for the management of multidrug resistant gram negative bacterial infections. Clin Infect Dis. 2005;40(9):1333–41.
Goswami NN, Trivedi HR, Goswami AP, Patel TK, Tripathi CB. Antibiotic sensitivity profile of bacterial pathogens in postoperative wound infections at a tertiary care hospital in Gujarat, India. J Pharmacol Pharmacother. 2011;2(3):158–64.
Desjardins M, Delgaty KL, Ramotar K, Seetaram K, Toye B. Prevalence and mechanisms of erythromycin resistance in group a and group B streptococcus: implications for reporting susceptibility results. J Clin Microbiol. 2004;42(12):5620–3.
Rice LB. Antimicrobial resistance in gram-positive bacteria. Am J Med. 2006;119(6 Suppl 1):S11–9.
Courvalin P. Vancomycin resistance in gram positive cocci. Clin Infect Dis. 2006;42(Suppl 1):S25–34.
Chua K, Howden BP. Treating gram-positive infections: vancomycin update and the whys, wherefores and evidence base for continuous infusion of anti-gram-positive antibiotics. Curr Opin Infect Dis. 2009;22(6):525–34.
Hooper DC. Fluoroquinolone resistance among Gram positive cocci. Lancet Infect Dis. 2002;2(9):530–8.
Funding
This work did not receive any funding from any source.
Availability of data and materials
The raw data can be made available to interested researchers by the authors of this article if requested.
Authors’ contributions
LM designed the study and reviewed the manuscript for important intellectual content. NR analyzed the data and wrote the manuscript. DS took part in data analysis and reviewed the manuscript. MMA performed experimental works. DA and NS were responsible for collecting the data. HA critically revised the manuscript and participated in writing. All authors read and approved the final manuscript.
Competing interests
The authors declare they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Due to the retrospective nature of the current study, no informed concent was taken from the caregivers of neonates included, however, consent for sample withdrawal was not required as they are part of routine management. This work has been approved by the Ethical Committee of Cairo University Children Hospital.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mohsen, L., Ramy, N., Saied, D. et al. Emerging antimicrobial resistance in early and late-onset neonatal sepsis. Antimicrob Resist Infect Control 6, 63 (2017). https://doi.org/10.1186/s13756-017-0225-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-017-0225-9