Abstract
Background
Presurgical optimisation programmes decrease the risk of postoperative complications, reduce hospital stays and speed up patient recovery. They usually involve a multidisciplinary team addressing physical, nutritional and psychosocial issues. The objective of this study was to assess the results of implementing a presurgical optimisation programme led by a liaison nurse in patients undergoing major surgery in a primary general hospital.
Methods
An observational, retrospective, descriptive, cross-sectional, comparative study based on the revision of patients’ health records undergoing major surgery between January 2019 and December 2022. Patients entering the presurgical optimisation programme (intervention group) were compared with patients receiving usual medical care (control group). The presurgical optimisation programme consisted of oral nutritional supplementation, physical exercise, strengthening of lung capacity and psychological and emotional support. Frequency (%) of surgery complications and use of healthcare resources (duration of hospitalisation, time spent in the intensive care unit (ICU), and readmission) at day 30 were recorded. Descriptive statistics were applied.
Results
Two hundred eleven patients (58.5% men, mean age: 65.76 years (SD 11.5), 75.2%. non-smokers; mean body mass index (BMI): 28.32 (SD 5.38); mean Nutritional Risk Score (NRS) 3.71 (SD 1.35; oncology diagnosis: 88.6%) were included: 135 in the intervention group, and 76 in the control group. The average duration of the presurgical optimisation programme was 20 days (SD 5). Frequency of postoperative complications was 25% (n = 33) in the intervention group and 52.6% (n = 40) in the control group (p < 0.001) [odds ratio (OR) = 3.4; 95% confidence interval (CI) (1.8; 6.2)]. 14.5% (n = 19) of patients in the intervention group and 34.2% (n = 26) in the control group had remote postoperative complications [OR = 3.1; 95% CI (1.6; 6.2)]. Patients in the intervention group spent fewer days in the hospital [mean 8.34 (SD 6.70) vs 11.63 (SD 10.63)], and there were fewer readmissions at 30 days (7.6% vs 19.7%) compared with the control group.
Conclusions
A presurgical optimisation programme led by a liaison nurse decreases the rate of immediate and late surgical complications and reduces hospital stays and readmissions in patients undergoing major surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Presurgical optimisation programmes are used before surgery to decrease the risk of postoperative complications, reduce hospital stays and speed up patient recovery (Vía 2021; Lawrence et al. 2004). Although not standardised, these multidisciplinary interventions usually include physical, nutritional, and psychosocial conditioning (Baimas-George et al. 2020) to improve the functional capacity of patients, control comorbidities, and adjust nutrition. The haemoglobin levels are also checked and optimised (in cases of anaemia), and appropriate steps are taken to reduce the anxiety and stress levels of the patient (Calleja et al. 2016; Peters et al. 2018). Such programmes are cost-effective because they can reduce postoperative complications and shorten hospitalisation, thus decreasing the use of medical care resources while improving the patient’s health (Leeds et al. 2021).
Presurgical optimisation programmes differ in length, indicated nutritional supplementation, number of visits before surgery and the participating professionals (Hijazi et al. 2017). Programmes in the United Kingdom and the Netherlands involve up to ten specialists (Davis et al. 2022). Each specialist assesses the patient and proposes the procedures to be followed before the surgery (Davis et al. 2022). Such programmes are complex and should be adapted to the needs of each individual; this implies logistical challenges. Nursing professionals usually coordinate the process and accompany the patient during the programme and the postoperative period. They do not intervene in the clinical or care-needs assessment of the patients (Dana et al. 2022).
Several studies have shown improvements in clinical outcomes and the overall health status of patients participating in presurgical optimisation programmes (Khadem et al. 2023). The reported examples include patients undergoing abdominal surgery for gastrointestinal, urological, gynaecological, hepatobiliary, or pancreatic malignancies. It has been shown that participation in these programmes can correct myopia or sarcopenia associated with poor prognosis. Moreover, surgical prehabilitation improves the tolerability of oncospecific treatments and the health-related quality of life (Martínez-Ortega et al. 2022).
Achieving good nutritional status is a fundamental component of presurgical optimisation programmes (Matthews et al. 2021) as it is one of the most important factors determining the results of surgical intervention (Ho et al. 2015). Malnutrition in surgical patients prolongs hospital stays and increases the use of resources necessary for the care and treatment of complications. It is also associated with delayed wound healing and a rise in hospital readmissions (Thomas et al. 2016; Mosquera et al. 2016). Moreover, malnutrition is a predictive factor for mortality, impaired mobility and increased long-term dependency (Helminen et al. 2017; Koren-Hakim et al. 2016). The European Society for Clinical Nutrition and Metabolism recommends that all malnourished patients or those at risk of malnutrition receive nutritional support for 7 to 14 days before the intervention and during the postoperative period (Weimann et al. 2021). Sometimes, nutritional improvement is needed within a short time, such as in cancer patients undergoing surgical resection of a solid tumour. In such cases, the diet must incorporate proteins of high biological value and certain amino acids (e.g., leucine). When combined with resistance exercise, this treatment can synergistically affect muscle tissue, enhancing protein synthesis and preventing sarcopenia (Rubio del Peral and Gracia Josa 2019).
Around 10% of patients undergoing abdominal surgery in Spain suffer from postoperative complications (Alastrué 2023) associated with increased mortality, prolonged hospital stays, and rising healthcare costs (Canet et al. 2010; Gili-Ortiz et al. 2015). The objective of the study was to assess if implementing a presurgical optimisation programme led by a liaison nurse reduces post-surgery complications and length of hospital stay in the intervention group in usual clinical practice. The evolution of anaemia and nutritional status of the participating patients were monitored at the start of the programme and 30 days after the surgery.
Materials and methods
Study design
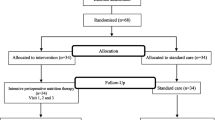
This observational, descriptive, comparative, cross-sectional study was carried out at the Infanta Cristina University Hospital in Parla (Madrid). The presurgical optimisation programme, led by a liaison nurse, was evaluated by comparing the intervention group (patients undergoing the clinical, functional, and psychological optimisation) with those who received the usual preoperative care (without clinical optimisation; control group). All patients in the study underwent major elective surgeries (Fig. 1).
Patients over 18 years old, awaiting major elective surgery and admitted to the oncology or traumatology hospital departments, were included. Medical records of eligible patients undergoing major elective surgery between January 1, 2019, and December 30, 2022, were retrospectively reviewed. Exclusions comprised patients referred elsewhere, requiring acute care surgery, or experiencing cancelled surgeries.
Recruitment was consecutive in both the intervention and control groups. However, due to the interruption in the presurgical programme caused by the COVID-19 pandemic, the intervention group included the patients who participated in the programme and had surgery during the years 2020, 2021 and 2022. The control group consisted of patients who underwent surgery in 2019 (Fig. 1).
The presurgical programme was introduced at the hospital in 2020. All patients on the surgery waiting list went through the surgical optimisation programme except those who did not meet the inclusion criteria, underwent emergency surgery, or were hospitalised in the otorhinolaryngology department.
Study variables
The following sociodemographic and clinical variables were collected: sex, age, smoking habits, body mass index (BMI), diagnosis of oncological disease (yes or no), type of oncological or non-oncological diagnosis, comorbidities, diabetes mellitus status (adequately controlled or not), immunocompromised condition (yes or no), the recommendation for neoadjuvant therapy (yes or no), and ascites (present or not). The type of surgical procedure was also recorded.
The description of clinical evolution after surgery included the need for conversion. This was defined as the change of the surgical procedure from laparoscopy to laparotomy. Other factors or events recorded (details shown in Table 3) were complications, type of postoperative infectious complications stemming from the surgery, pulmonary complications, intra-abdominal complications, paralytic ileus, suture dehiscence, wound complications, post-stress haemorrhage, whole blood transfusion requirement, number of units of red blood cells transfused, multiple organ failure, remote complications defined as complications 30 days after surgery and death.
Additionally, in the intervention group, the values for haemoglobin, ferritin, albumin, prealbumin, and C-reactive protein (CRP) levels were taken, as well as total lymphocyte count and total cholesterol. This was done to determine the nutritional and inflammatory status of the patient at the start of the presurgical optimisation programme, the day before surgery (i.e., 21 to 30 days from the admission to the programme) and 30 days after surgery.
To assess the use of resources after surgery, the following data were recorded: the duration of hospitalisation, time spent in the intensive care unit (ICU) due to emergency admission due to complications, and readmission (yes or no; 30 days after the surgery). Any reinterventions were also registered (yes or no), defined as new surgeries related to the initial intervention due to poor evolution or complications.
Intervention
The intervention group followed the protocol for the presurgical optimisation programme for 15–30 days (Fig. 2). The presurgical optimisation program initiates with the patient’s inclusion on the surgery waiting list by the attending surgeon. Cancer patients undergo evaluation by the liaison nurse within 72 h of their surgery request, with surgery scheduled within 30 days (Fig. 2). Non-cancer patients, whose surgery waiting period extends to 2 to 3 months, are assessed 21 to 30 days after listing.
Once the patient enters a presurgical optimisation programme, a comprehensive assessment is performed. This includes screening using the Nutritional Risk Score (NRS) 2002 (Kondrup et al. 2003) and the Global Leadership Initiative on Malnutrition criteria (GLIM) (Kondrup et al. 2003) to establish the nutritional status and choose the most appropriate supplement regimen for each patient. Laboratory tests are conducted to detect anaemia (haemoglobin level < 13 g/dL in a peripheral blood test). Anthropometric (weight, height, BMI, and the diameter of the rectus femoris muscle) and other (fat, muscle, and water mass) parameters are also obtained. Nutritional ultrasound analysis is performed to assess body composition. The functional status is examined using a gait test for aerobic resistance (Crapo et al. 2012) and dynamometry to determine muscle strength (Stark et al. 2011). Barthel scale is employed to define the degree of patient dependency (Mahoney and Barthel 1965). Lung capacity is estimated using incentive spirometry (Carey et al. 2014).
Moreover, a psychological evaluation is carried out to measure the self-esteem of the patient (Rosenberg scale) ( American Psychological Association 1965). The body image questionnaire (Hopwood et al. 2001) is employed to determine the perception of body image. The EQ-5D-5L survey is used to obtain health-related quality of life scores (Herdman et al. 2001). The usual pharmacological treatment and the degree of adherence are reviewed for each patient. Finally, the ability of the patient to understand the information pertaining to the objectives, implications, and the need for inclusion in the programme is assessed. Based on the obtained results, the procedures are adapted to the individual needs of each patient (Table 1).
The nutritional status was optimised if the Nutritional Risk Score (NRS) 2002 of the patient was greater than 3 points (considering the anthropometric parameters). To achieve this, two hyperproteic and hypercaloric oral supplementation, containing 20.8 g of protein (100% lactoprotein serum), leucine and vitamin D, were administered (Table S1 and Table S2). One to three bottles of 200 ml per day were recommended per patient. The diet was adjusted based on the amount of body fat, muscle and water mass of each patient and their diet during the preceding 3 days. Patients with anaemia were treated with ferric carboxymaltose.
The patients engaged in physical exercise comprising at least 150 min of weekly aerobic activity. Lung capacity was strengthened using the incentive spirometer to raise the patient’s lung capacity to 500 ml above their baseline level before surgery. Patients with low self-esteem (Rosenberg score < 25 points) and with a low score in their assessment of the quality of life (Euro-QoL5D > 5 points) were referred to a psychologist.
Control of comorbidities was improved by adjusting pharmacological treatments, complementing the usual treatment, and increasing adherence. Carbohydrate drinks were recommended up to 2 h before surgery to reduce the preoperative fasting time and to mitigate the transient increase in insulin resistance that elective surgeries often cause (Ho et al. 2015). Health education was undertaken to improve the understanding of the presurgery optimisation programme, objectives and expected outcomes; the process was adapted to the family, social and personal background of the patient.
Role of the liaison nurse in the presurgical optimisation programme
The liaison nurse is responsible for coordinating and executing the proposed presurgical optimisation programme. The nurse conducts the assessments described in Table 2 and identifies patient needs. Based on the obtained results, the recommendations for individual optimisation are prepared, to be validated by the internist. In addition, the liaison nurse monitors the patients during the execution of the programme and performs a check-up on the day before the surgery and 30 days later (Fig. 3).
Data collection
All data were collected in a specially designed Excel sheet for this study by the researchers (N.M. and F.G.) through a review of patients’ medical records.
Ethical aspects
This study was approved by the Ethics and Research Committee of the Puerta de Hierro University Hospital (ACT 15.18).
The access to study files was password protected and restricted to the responsible researchers (N.M. and F.G.) according to current data protection regulations (BOE-A-2018, Regulation 2016).
Statistical analysis
Assuming 15% losses, a 95% confidence level, 3% precision and 5% proportion, an appropriate sample size of 211 was estimated. Convenience sampling was performed.
All study variables were examined to assess their distribution. The categorical variables were described using the percentage associated with each possible response option, and the quantitative variables using the mean, standard deviation (SD), and range. For comparisons between variables and hypothesis testing, the chi-square test was employed for categorical variables, Student’s t test or ANOVA for quantitative variables that were normally distributed, and the Mann–Whitney U test or the Kruskal–Wallis test for quantitative variables without a normal distribution. Statistical analysis was performed using the SPSS v26 software package (IBM, Armonk, New York).
Results
The average duration of the presurgical optimisation programme in the intervention group was 20 (SD 5) days.
General characteristics of the population
Two hundred eleven patients were included; 135 participated in the presurgical optimisation programme (intervention group), and 76 formed the control group.
Among the participating patients, 58.5% were men. The average age was 65.76 years (SD 11.5). Non-smokers constituted 75.2%. The average BMI was 28.32 (SD 5.38), and NRS 3.71 (SD 1.35). Most participants (88.6%) were cancer patients, and 14.4% received neoadjuvant therapy. Colorectal adenocarcinoma (54.9%) was the most prevalent surgical diagnosis, and laparoscopy was the most frequent intervention (55.3%). The most common comorbidity was cardiac disease (24.8%), followed by type 2 diabetes mellitus (DM) (21.2%) (Table 2).
Clinical characteristics of the compared groups before the surgery
The percentage of cancer patients was similar in the two groups: 88.8% in the intervention and 88.2% in the control group.
The number of patients with DM was higher in the control group than in the intervention group (27.6% and 19.3%, respectively). The percentage of patients with inadequately controlled DM was higher in the control group (16.6% compared to 5%).
The average NRS score was similar in the two groups (intervention group: 3.82 [SD 1.47]; control group: 3.29 [SD 0.52]) (Table 2).
Post-surgery clinical characteristics of the compared groups
The frequency of postoperative complications was 25% (n = 33) in the intervention group and 52.6% (n = 40) in the control group (p < 0.001) [OR = 3.4; 95% CI (1.8; 6.2)] (Table 2), while 14.5% (n = 19) of patients in the intervention group and 34.2% (n = 26) in the control group suffered from remote postoperative complications [OR = 3.1; 95% CI (1.6; 6.2)] (Table 3).
Suture dehiscence occurred in 7.5% of patients in the intervention group (n = 10) and 21.1% (n = 16) in the control group; (p = 0.005) [OR = 3.3; 95% CI (1.4, 7.7)]. Haemorrhage due to surgical stress happened in 0% in the intervention and 13.2% (n = 10) in the control group (p < 0.001) [OR = 3.1; 95% CI (2.5; 3.7)] after surgery while sepsis arose in 2.3% (n = 3) and 9.2% (n = 7); (p = 0.03) [OR = 4.5; 95% CI (1.1; 17.8)] of the intervention and control group patients. Multiple organ failure occurred in 0.8% of the subjects (n = 1) in the intervention group and 7.9% (n = 6) in the control group; (p = 0.006) [OR = 11.5; 95% CI (1.3, 97.3)]. The proportion of patients requiring blood transfusion was lower in the intervention group than among the control subjects (90.1% versus 75%, p = 0.014) [OR = 3.1 95% CI (1.4, 6.8)]. The programme participants received fewer units of packed red blood cells than the members of the control group (0.22 (0.80) vs 0.75 (2.24), p < 0.001) (Table 3).
Nutritional parameters in the intervention group at the baseline and after 30 days of the presurgical optimisation programme
The levels of albumin, prealbumin, total lymphocyte count, haemoglobin, ferritin, C-reactive protein and total cholesterol improved in the intervention group after 30 days of optimisation (Table 4).
Use of healthcare resources after surgery
The intervention group members spent fewer days in the hospital after surgery (8.34 (SD 6.70) vs 11.63 (SD 10.63) days), and there were fewer readmissions within 30 days after the surgery (7.6% vs 19.7%) than in the control group. Five patients in the optimisation programme group (3.8%) had to undergo a reintervention surgery compared to 26 (34.2%) in the control group [OR = 13.5; 95% CI (4.9; 37.1)] (Table 5).
Discussion
This study describes the health outcomes for patients who underwent major elective surgery after participating in a presurgical optimisation programme led by a liaison nurse. The results were compared with those obtained for a control group receiving the usual medical care before surgery. Complications, length of hospitalisation and number of hospital readmissions in each group were recorded and compared.
Healthcare professionals working with presurgical optimisation programmes have reported that the implementation is made difficult by organisational complexity (Heil et al. 2022), insufficient time and training (Partridge et al. 2020). Programmes that involve many professionals can be inefficient due to delays in patient treatment resulting from a lack of communication and incorrect referrals (Whiteman et al. 2016). Unlike other national presurgical optimisation programmes developed by the Spanish Multimodal Rehabilitation Group (GERM) (Vía 2021), the model used here requires only two healthcare professionals. Other models employ several specialists (such as haematologists, endocrinologists, cardiologists, pulmonologists, and physiotherapists) and need an average of five visits per patient (Vía 2021). In the protocol carried out at the Infanta Cristina University Hospital of Parla (Madrid) described in this article, the assessment, management, and coordination of patient care is centrally controlled by the liaison nurse in collaboration with the hospital medical internist. Thus, the optimisation process can begin in less than 48 h after adding the patient to the surgery waiting list. In other models, the nurse takes part only in the coordination and follow-up of interventions, and patients’ assessment is carried out by medical specialists (Dana et al. 2022). It has been reported that a healthcare professional acting as a coordinator facilitates implementation (Heil et al. 2022). Empowering a nurse (with adequate training and support) to assume roles historically performed by other medical professionals expedites access to therapies and simplifies the management of complex patients (Carey et al. 2014).
The results obtained here show that presurgical optimisation significantly reduces the frequency of immediate and remote complications after surgery (p < 0.001). This is in agreement with another clinical study of patients undergoing major abdominal surgery, whose postoperative complication rate was 31% after preoperative optimisation and 62% in the control group without such a pre-surgery approach (Barberan-Garcia et al. 2018).
It has been shown that surgical patients with anaemia carry an increased risk of postoperative complications and have a higher mortality rate than those without this condition (Bolshinsky et al. 2022). Treating anaemia before surgery reduces the number of postoperative complications and blood transfusions (Blum et al. 2022)(Froessler et al. 2016) and accelerates the recuperation of mobility [s39]. These findings concur with the results of the current study, in which the handling of anaemia as a part of clinical optimisation probably contributed to improved postoperative evolution of the intervention group.
Suture dehiscence and infectious wound complications were less frequent among the preoperative optimisation programme participants than in the control group. This is in agreement with a meta-analysis published in 2021 showing that improving nutritional status and quitting smoking reduce the frequency of wound infection by 29% and 72%, respectively (Perry et al. 2021). Hyperproteic and hypercaloric oral supplementation with 100% lactoprotein serum, leucine, and vitamin D might also be associated with a decrease in the number of postoperative complications (Lawson et al. 2021). This finding concurs with the conclusions of Perry et al. (2021) in a meta-analysis of 10 clinical studies including 643 patients (Perry et al. 2021). The analysis has shown that postoperative complications decreased in the group supplemented with lactoprotein serum (22%) compared to the control group (32%) (Srinivasaraghavan et al. 2022). Leucine is the only branched-chain amino acid that stimulates the mTOR signalling pathway and, thereby, protein synthesis in the muscle (Anthony et al. 2000). Vitamin D is key in lowering the anabolic threshold for postprandial stimulation of muscle protein synthesis by leucine, which contributes to preserving or increasing muscle mass in older patients (Chanet et al. 2017). Thus, it can be argued that the combined administration of these nutritional elements in an oral nutritional supplement helps the recovery of muscle mass and muscular trophism—which is necessary for the early mobilisation of patients after surgery.
The surgical stress response involves a complex interplay of neuroendocrine, metabolic, and inflammatory-immune processes, triggering a catabolic state with the release of growth factors, energy substrates, and inflammatory mediators while suppressing anabolic hormones and causing fluid retention. Enhanced Recovery After Surgery (ERAS) protocols aim to mitigate these effects through multimodal analgesia, early mobilisation, minimally invasive techniques, and early enteral feeding, reducing surgical stress and promoting faster recovery (Choi et al. 2022; Neville et al. 2014). Additional strategies such as reducing preoperative fasting time, carbohydrate loading, and immunonutrition further decrease postoperative complications by addressing metabolic demands and immune function (Chen et al. 2022). Postoperative gastrointestinal (GI) bleeding, an unusual but serious complication of both GI and non-GI surgeries, can arise from surgery-related causes, unrelated causes, or surgical stress exacerbating a pre-existing condition. While minor postoperative bleeding is common and often uncomplicated, significant bleeding, although less common, is associated with high morbidity and mortality (Ghallab 2018). In this study, presurgical optimisation patients showed no haemorrhage compared to the control group, where its frequency was notably high. Presurgical optimisation can significantly reduce surgical stress by addressing various modifiable risk factors before the operation. Key strategies include improving nutritional status, increasing physical fitness, and managing chronic conditions. Adequate nutrition, particularly protein intake, is essential to mitigate muscle loss and support the body's response to surgical stress. Nutritional interventions such as preoperative carbohydrate loading can help reduce postoperative insulin resistance and catabolism (Surgical Optimization Center | Corewell Health n.d.; Hirsch et al. 2021). Physical conditioning through preoperative exercises enhances muscle strength and endurance, which can improve recovery and reduce complications (Sheill et al. 2020). Additionally, comprehensive patient education and mental preparation can alleviate anxiety and ensure patients are better prepared for surgery, contributing to reduced stress and improved outcomes (Surgical Optimization Center | Corewell Health n.d.). These measures collectively help decrease the length of hospital stays, reduce readmissions, and enhance overall postoperative recovery (Hirsch et al. 2021).
Cancer patients who receive oral nutritional supplementation have also shown better clinical evolution, fewer complications, and need fewer health resources than those who have not received such supplementation (Fukuda et al. 2015; Hsu et al. 2021). For example, patients who received a leucine-enriched supplement to accompany a physical exercise programme showed increased grip strength compared to the control group without supplementation (Storck et al. 2020). Another study has compared the recovery of functional capacity of patients in a presurgical optimisation programme with that of a standard care group. The programme consisted of four interventions: high-intensity resistance and strength training, protein-rich nutrition and supplementation, smoking cessation and psychological support. Four weeks after surgery, the average functional capacity of patients in the intervention group (as measured by a 6-min walk test) rose above baseline, while it decreased in the control group (Weimann et al. 2017).
Likewise, the intake of carbohydrate drinks 2 h before surgery stimulates the release of insulin and ghrelin. It reduces the number of catabolic processes, mitigating the transient increase in insulin resistance that elective surgeries usually produce (Noba and Wakefield 2019). High endogenous glucose levels may increase the risk of surgical complications (Jones et al. 2011), prolonging hospitalisation (Kaška et al. 2010; Awad et al. 2013). The European Society for Clinical Nutrition and Metabolism recommends reducing preoperative fasting to 2 h (Weimann et al. 2021); this advice was followed for the intervention group in this study.
Several meta-analyses vary in their conclusions regarding the reduction of hospitalisation time of patients participating in presurgical optimisation programmes. In a meta-analysis of 9 randomised clinical trials, there were no differences between patients who participated in a presurgical optimisation programme and those who did not (Pang et al. 2022). In an umbrella review, all pooled mean differences were consistent with a reduced length of stay in the prehabilitation group, ranging from a reduction of 0.09 to 4.24 days (McIsaac et al. 2022). Lambert et al. (2021) reported a 1.78-day reduction in hospital stays among patients enrolled in presurgical optimisation programmes compared to those receiving standard care (Lambert et al. 2021). These results are similar to those obtained in the current study, where the hospitalisation in the intervention group was reduced by 3.29 days compared to the control group.
Several additional clinical factors can influence the length of hospital stay and post-operative complications. Laparotomy, surgery conversion, poorly controlled diabetes and paralytic ileus are associated with longer length of hospital stay and postoperative complications (Tevis et al. 2015; Tan et al. 2021). These factors could potentially contribute to the differences in hospital stay and complications observed between the intervention and control groups in this study. A higher rate of laparotomy and conversion in the control group may lead to an increase in the length of hospital stay. A meta-analysis showed that hospital length of stay is significantly shorter for patients who undergo laparoscopy compared to those who undergo open surgery (Cirocchi et al. 2017). In a retrospective study of rectal carcinoma patients, conversion was associated with longer postoperative hospital stays (20 days versus 14 days) (Yamamoto et al. 2009). A meta-analysis found a higher incidence of postoperative complications in patients with poorly controlled diabetes (Tan et al. 2021). On the other hand, postoperative ileus is typically associated with a significant increase in the hospital length of stay, yet it occurred less frequently in the control group compared to the intervention group in this study (Iyer and Saunders 2007).
The results of this research must be interpreted in the context of its limitations, common in retrospective-prospective observational studies of usual clinical practice. Thus, a process to randomly assign the medical records to the control group was not followed neither patients in the intervention group were randomly selected. Instead, convenience sampling was used based on the patients on the surgery waiting list, which could affect the probability of being recruited. Moreover, the degree of motivation of a patient voluntarily participating in research can differ significantly from that of other patients. In this study, the patients in the intervention group could have had different motivations to follow the medical recommendations for preoperative optimisation than those in the control group. The size of the intervention group and control group were different. Patients had different diseases requiring surgery with differing burdens. These differences may weaken the comparability of results between groups. A subgroup analysis of individuals sharing, for example, similar nutritional status or comorbidities, both of which are related to subsequent surgical recovery, was not performed. Study variables did not include any risk prediction measurements to allow for risk adjustment of outcomes and a better comparison of balance between groups, thus limiting the reliability of results.
Despite the limitations, the study presents a favourable tendency towards improving clinical outcomes by implementing a presurgical optimisation programme led by a liaison nurse, designed to reduce the number of post-surgery complications and decrease the length of hospitalisation after a major elective surgery. The findings are in accord with data reported by other studies of similar interventions. Although the design of this study has low internal validity, its external validity is relevant because it reflects the usual clinical practice and the value of the interventions that can be carried out in this context. However, the findings from this study need validation through clinical investigations employing a more rigorous design.
Conclusions
A presurgical optimisation programme described here was led by a liaison nurse. It included hyperproteic and hypercaloric oral nutritional supplementation (100% lactoprotein serum with leucine and vitamin D), a physical exercise program, strengthening of lung capacity and administration of carbohydrate drinks. Psychological and emotional support and health education were provided to reduce presurgical stress. These combined measures decreased the rate of complications and readmissions and reduced hospitalisation times of patients undergoing major elective surgeries. These results need to be corroborated in clinical, comparative studies with a more robust design.
Availability of data and materials
The datasets of this study are available from the corresponding author upon reasonable request.
References
Alastrué Nuñez E. Valoración y prevención de las complicaciones de la cirugía abdominal. 2023. Available from: https://revistasanitariadeinvestigacion.com/valoracion-y-prevencion-de-las-complicaciones-de-la-cirugia-abdominal/. Cited 2023 Feb 8.
American Psychological Association. Rosenberg Self-Esteem Scale - PsycNET. 1965. Available from: https://psycnet.apa.org/Landing?doi=10.1037%2Ft01038-000. Cited 2023 Feb 8.
Anthony JC, Yoshizawa F, Anthony TG, Vary TC, Jefferson LS, Kimball SR. Leucine stimulates translation initiation skeletal muscle of postabsorptive rats via a rapamycin-sensitive pathway. J Nutr. 2000;130(10):2413–9.
Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013;32(1):34–44.
Baimas-George M, Watson M, Elhage S, Parala-Metz A, Vrochides D, Davis BR. Prehabilitation in frail surgical patients: a systematic review. World J Surg. 2020;44(11):3668–78.
Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R, et al. Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg. 2018;267(1):50–6.
Blum LV, Zierentz P, Hof L, Kloka JA, Messroghli L, Zacharowski K, et al. The impact of intravenous iron supplementation in elderly patients undergoing major surgery. BMC Geriatr. 2022;22(1):1–12.
BOE-A-2018-16673 Ley Orgánica 3/2018, de 5 de diciembre, de Protección de Datos Personales y garantía de los derechos digitales. Available from: https://www.boe.es/buscar/act.php?id=BOE-A-2018-16673. Cited 2024 Apr 30.
Bolshinsky V, Ismail H, Li M, Basto J, Schier R, Hagemeier A, et al. Clinical covariates that improve surgical risk prediction and guide targeted prehabilitation: an exploratory, retrospective cohort study of major colorectal cancer surgery patients evaluated with preoperative cardiopulmonary exercise testing. Perioper Med. 2022;11(1):1–13.
Calleja JL, Delgado S, del Val A, Hervás A, Larraona JL, Terán Á, et al. Ferric carboxymaltose reduces transfusions and hospital stay in patients with colon cancer and anemia. Int J Colorectal Dis. 2016;31(3):543–51.
Canet J, Gallart L, Gomar C, Paluzié G, Vallè J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:0–1000.
Cappellini MD, Motta I. Anemia in clinical practice-definition and classification: does hemoglobin change with aging? Semin Hematol. 2015;52(4):261–9.
Carey N, Stenner K, Courtenay M. An exploration of how nurse prescribing is being used for patients with respiratory conditions across the east of England. BMC Health Serv Res. 2014;14(1):1–13.
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38(1):1–9.
Chanet A, Verlaan S, Salles J, Giraudet C, Patrac V, Pidou V, et al. Supplementing breakfast with a vitamin D and leucine-enriched whey protein medical nutrition drink enhances postprandial muscle protein synthesis and muscle mass in healthy older men. J Nutr. 2017;147(12):2262–71.
Chen T, Wei H, Yue W, Su Y, Fu X. Enhanced recovery after surgery management of perioperative period in surgical lung cancer patients: protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2022;12(2):e056068.
Choi YS, Kim TW, Chang MJ, Kang S-B, Chang CB. Enhanced recovery after surgery for major orthopedic surgery: a narrative review. Knee Surg Relat Res. 2022;34(1):8.
Cirocchi R, Cesare Campanile F, Di Saverio S, Popivanov G, Carlini L, Pironi D, et al. Laparoscopic versus open colectomy for obstructing right colon cancer: a systematic review and meta-analysis. J Visc Surg. 2017;154(6):387–99.
Crapo RO, Casaburi R, Coates AL, Enright PL, MacIntyre NR, McKay RT, et al. ATS statement: guidelines for the six-minute walk test. ATS Journals. 2012;166(1):111–7.
Dana F, Sebio-García R, Tena B, Sisó M, Vega F, Peláez A, et al. Perioperative nursing as the guiding thread of a prehabilitation program. Cancers. 2022;14(21):5376.
Davis JF, van Rooijen SJ, Grimmett C, West MA, Campbell AM, Awasthi R, et al. From theory to practice: an international approach to establishing prehabilitation programmes. Curr Anesthesiol Rep. 2022;12(1):129–37.
del Peral Rubio JA, Gracia Josa MS. Suplementos proteicos en el tratamiento y prevención de la sarcopenia en ancianos. Revisión sistemática. Gerokomos. 2019;30(1):23–7.
Froessler B, Palm P, Weber I, Hodyl NA, Singh R, Murphy EM. The important role for intravenous iron in perioperative patient blood management in major abdominal surgery. Ann Surg. 2016;264(1):41–6.
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N, et al. Prevalence of malnutrition among gastric cancer patients undergoing gastrectomy and optimal preoperative nutritional support for preventing surgical site infections. Ann Surg Oncol. 2015;22(3):778–85.
García JA, Y Olmos FC, Matheu ML, Carreño TP. Self esteem levels vs global scores on the Rosenberg self-esteem scale. Heliyon. 2019;5(3):e01378.
García-Almeida JM, García-García C, Vegas-Aguilar IM, Ballesteros Pomar MD, Cornejo-Pareja IM, Fernández Medina B, et al. Nutritional ultrasound®: Conceptualisation, technical considerations and standardisation. Endocrinol Diabetes y Nutr. 2023;70(Suppl 1):74–84.
Ghallab ET. Post-operative bleeding and its management. Egypt J Hosp Med. 2018;70(9):1480–3.
Gili-Ortiz E, González-Guerrero R, Béjar-Prado L, Ramírez-Ramírez G, López-Méndez J. Postoperative dehiscence of the abdominal wound and its impact on excess mortality, hospital stay and costs. Cir Esp. 2015;93(7):444–9.
Heil TC, Driessen EJM, Argillander TE, Melis RJF, Maas HAAM, Olde Rikkert MGM, et al. Implementation of prehabilitation in colorectal cancer surgery: qualitative research on how to strengthen facilitators and overcome barriers. Support Care Cancer. 2022;30(9):7373.
Helminen H, Luukkaala T, Saarnio J, Nuotio M. Comparison of the mini-nutritional assessment short and long form and serum albumin as prognostic indicators of hip fracture outcomes. Injury. 2017;48(4):903–8.
Herdman M, Badia X, Berra S. El EuroQol-5D: una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Atención Primaria. 2001;28(6):425–30.
Hijazi Y, Gondal U, Aziz O. A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg. 2017;39:156–62.
Hirsch KR, Wolfe RR, Ferrando AA. Pre- and post-surgical nutrition for preservation of muscle mass, strength, and functionality following orthopedic surgery. Nutrients. 2021;13:1675.
Ho JWC, Wu AHW, Lee MWK, Lau SY, Lam PS, Lau WS, et al. Malnutrition risk predicts surgical outcomes in patients undergoing gastrointestinal operations: results of a prospective study. Clin Nutr. 2015;34(4):679–84.
Hopwood P, Fletcher I, Lee A, Al GS. A body image scale for use with cancer patients. Eur J Cancer. 2001;37(2):189–97.
Hsu PI, Chuah SK, Lin JT, Huang SW, Lo JC, Rau KM, et al. Taiwan nutritional consensus on the nutrition management for gastric cancer patients receiving gastrectomy. J Formos Med Assoc. 2021;120(1):25–33.
Iyer S, Saunders W. Impact of post-operative ileus (POI) on hospital length of stay in colectomy surgery patients: 874. Off J Am Coll Gastroenterol | ACG. 2007;102:S440.
Jones C, Badger SA, Hannon R. The role of carbohydrate drinks in preoperative nutrition for elective colorectal surgery. Ann R Coll Surg Engl. 2011;93(7):504.
Kaška M, Grosmanová T, Havel E, Hyšpler R, Petrová Z, Brtko M, et al. The impact and safety of preoperative oral or intravenous carbohydrate administration versus fasting in colorectal surgery-a randomized controlled trial. Wien Klin Wochenschr. 2010;122(1–2):23–30.
Khadem S, Herzberg J, Honarpisheh H, Jenner RM, Guraya SY, Strate T. Safety profile of a multimodal fail-safe model to minimize postoperative complications in oncologic colorectal resections—a cohort study. Perioper Med. 2023;12(1):1–12.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–36.
Koren-Hakim T, Weiss A, Hershkovitz A, Otzrateni I, Anbar R, Gross Nevo RF, et al. Comparing the adequacy of the MNA-SF, NRS-2002 and MUST nutritional tools in assessing malnutrition in hip fracture operated elderly patients. Clin Nutr. 2016;35(5):1053–8.
Lambert JE, Hayes LD, Keegan TJ, Subar DA, Gaffney CJ. The impact of prehabilitation on patient outcomes in hepatobiliary, colorectal, and upper gastrointestinal cancer surgery: a PRISMA-Accordant Meta-analysis. Ann Surg. 2021;274(1):70–7.
Lawrence VA, Hazuda HP, Cornell JE, Pederson T, Bradshaw PT, Mulrow CD, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199(5):762–72.
Lawson C, Ferreira V, Carli F, Chevalier S. Effects of multimodal prehabilitation on muscle size, myosteatosis, and dietary intake of surgical patients with lung cancer - a randomized feasibility study. Appl Physiol Nutr Metab. 2021;46(11):1407–16.
Leeds IL, Drabo EF, Lehmann LS, Safar B, Johnston FM. On all accounts: cost-effectiveness analysis of limited preoperative optimization efforts before colon cancer surgery. Dis Colon Rectum. 2021;64(6):744–53.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Martínez-Ortega AJ, Piñar-Gutiérrez A, Serrano-Aguayo P, González-Navarro I, Remón-Ruíz PJ, Pereira-Cunill JL, et al. Perioperative nutritional support: a review of current literature. Nutrients. 2022;14(8):1601.
Matthews LS, Wootton SA, Davies SJ, Levett DZH. Screening, assessment and management of perioperative malnutrition: a survey of UK practice. Perioper Med. 2021;10(1):1–8.
McIsaac DI, Gill M, Boland L, Hutton B, Branje K, Shaw J, et al. Prehabilitation in adult patients undergoing surgery: an umbrella review of systematic reviews. Br J Anaesth. 2022;128(2):244–57. Available from: https://www.sciencedirect.com/science/article/pii/S0007091221007303.
Mosquera C, Koutlas NJ, Edwards KC, Strickland A, Vohra NA, Zervos EE, et al. Impact of malnutrition on gastrointestinal surgical patients. J Surg Res. 2016;205(1):95–101.
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM, et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg. 2014;101(3):159–70.
Noba L, Wakefield A. Are carbohydrate drinks more effective than preoperative fasting: a systematic review of randomised controlled trials. J Clin Nurs. 2019;28(17–18):3096–116.
Pang NQ, Tan YX, Samuel M, Tan KK, Bonney GK, Yi H, et al. Multimodal prehabilitation in older adults before major abdominal surgery: a systematic review and meta-analysis. Langenbeck’s Arch Surg. 2022;407(6):2193–204.
Partridge JSL, Rogerson A, Joughin AL, Walker D, Simon J, Swart M, et al. The emerging specialty of perioperative medicine: a UK survey of the attitudes and behaviours of anaesthetists. Perioper Med (Lond). 2020;9(1):1.
Perry R, Herbert G, Atkinson C, England C, Northstone K, Baos S, et al. Pre-admission interventions (prehabilitation) to improve outcome after major elective surgery: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e050806. Available from: http://bmjopen.bmj.com/content/11/9/e050806.abstract.
Peters F, Ellermann I, Steinbicker AU. Intravenous iron for treatment of Anemia in the 3 perisurgical phases: a review and analysis of the current literature. Anesth Analg. 2018;126(4):1268–82.
Regulation - 2016/679. Available from: https://eur-lex.europa.eu/eli/reg/2016/679/oj. Cited 2024 Apr 29.
Sheill G, Guinan E, O’Neill L, Normand C, Doyle SL, Moore S, et al. Preoperative exercise to improve fitness in patients undergoing complex surgery for cancer of the lung or oesophagus (PRE-HIIT): protocol for a randomized controlled trial. BMC Cancer. 2020;20(1):321.
Srinivasaraghavan N, Das N, Balakrishnan K, Rajaram S. Effect of whey protein supplementation on perioperative outcomes in patients with cancer-a systematic review and meta-analysis (PROSPERO 2020: CRD42020188666). Nutr Cancer. 2022;74(7):2351–64.
Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472–9.
Storck LJ, Ruehlin M, Gaeumann S, Gisi D, Schmocker M, Meffert PJ, et al. Effect of a leucine-rich supplement in combination with nutrition and physical exercise in advanced cancer patients: a randomized controlled intervention trial. Clin Nutr. 2020;39(12):3637–44.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5):547–58.
Surgical Optimization Center | Corewell Health. Available from: https://www.spectrumhealth.org/services/surgical-optimization-center. Cited 2024 May 17.
Tan DJH, Yaow CYL, Mok HT, Ng CH, Tai CH, Tham HY, et al. The influence of diabetes on postoperative complications following colorectal surgery. Tech Coloproctol. 2021;25(3):267–78.
Tevis SE, Carchman EH, Foley EF, Harms BA, Heise CP, Kennedy GD. Postoperative ileus—more than just prolonged length of stay? J Gastrointest Surg. 2015;19(9):1684–90. Available from: https://www.sciencedirect.com/science/article/pii/S1091255X23039902.
Thomas MN, Kufeldt J, Kisser U, Hornung HM, Hoffmann J, Andraschko M, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. 2016;32(2):249–54.
Thoresen L, Frykholm G, Lydersen S, Ulveland H, Baracos V, Prado CMM, et al. Nutritional status, cachexia and survival in patients with advanced colorectal carcinoma. Different assessment criteria for nutritional status provide unequal results. Clin Nutr. 2013;32(1):65–72.
Vía RICA 2021 | Grupo Español de Rehabilitación Multimodal. Available from: https://grupogerm.es/rica/. Cited 2023 Jan 19.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017;36(3):623–50.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN practical guideline: clinical nutrition in surgery. Clin Nutr. 2021;40(7):4745–61.
Whiteman AR, Dhesi JK, Walker D. The high-risk surgical patient: a role for a multi-disciplinary team approach? Br J Anaesth. 2016;116(3):311–4.
World Health Organization. Obesity and overweight. 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Cited 2024 Apr 29.
Yamamoto S, Fukunaga M, Miyajima N, Okuda J, Konishi F, Watanabe M. Impact of conversion on surgical outcomes after laparoscopic operation for rectal carcinoma: a retrospective study of 1,073 patients. J Am Coll Surg. 2009;208(3):383–9.
Acknowledgements
The authors wish to thank all the patients who participated in the study and DANONE NUTRICIA for supporting the translation and publication of this manuscript.
The authors also thank Lena Huck, Ewa Gubb and Silvia Paz at SmartWorking4U who gave writing and editorial support during the development of the manuscript.
Funding
DANONE NUTRICIA financed the writing and editorial support of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception: N.M. and F.G; design: N.M. and F.G; validation: N.M. and F.G; data acquisition: N.M. and F.G; analysis: N.M. and F.G; data interpretation: N.M. and F.G; drafting of the manuscript: N.M. and F.G; review of the manuscript: N.M. and F.G. All authors read and approved the submission and publication of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics and Research Committee of the Puerta de Hierro University Hospital (ACT 15.18).
Consent for publication
All authors approved the version of the manuscript to be published.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
13741_2024_430_MOESM1_ESM.docx
Additional file 1: Supplementary Table S1. Oral nutritional supplementation composition, 100 ml. Supplementary Table S2. Oral nutritional supplementation composition for diabetic patients, 100 ml.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
García Sánchez, F., Mudarra García, N. Evaluation of postoperative results after a presurgical optimisation programme. Perioper Med 13, 73 (2024). https://doi.org/10.1186/s13741-024-00430-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-024-00430-7