Abstract
Background
Despite advances in perioperative care, post-operative clinical and functional outcomes after major abdominal surgery can be suboptimal. Prehabilitation programmes attempt to optimise a patient’s preoperative condition to improve outcomes. Total body prehabilitation includes structured exercise, nutritional optimisation, psychological support and cessation of negative health behaviours. This systematic review aims to report on the current literature regarding the impact of total body prehabilitation prior to major abdominal surgery.
Methods
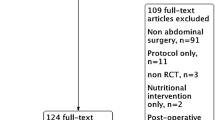
Relevant studies published between January 2000 and July 2017 were identified using MEDLINE, EMBASE, AMED, CINAHL, PsychINFO, PubMed, and the Cochrane Database. All studies published in a peer-reviewed journal, assessing post-operative clinical and functional outcomes, following a prehabilitation programme prior to major abdominal surgery were included. Studies with less than ten patients, or a prehabilitation programme lasting less than 7 days were excluded.
Results
Sixteen studies were included, incorporating 2591 patients, with 1255 undergoing a prehabilitation programme. The studies were very heterogeneous, with multiple surgical sub-specialties, prehabilitation techniques, and outcomes assessed. Post-operative complication rate was reduced in six gastrointestinal studies utilising either preoperative exercise, nutritional supplementation in malnourished patients or smoking cessation. Improved functional outcomes were observed following a multimodal prehabilitation programme. Compliance was variably measured across the studies (range 16–100%).
Conclusions
There is substantial heterogeneity in the prehabilitation programmes used prior to major abdominal surgery. A multimodal approach is likely to have better impact on functional outcomes compared to single modality; however, there is insufficient data either to identify the optimum programme, or to recommend routine clinical implementation.

Similar content being viewed by others
References
Varadhan KK, Neal KR, Dejong CHC et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–4401
Teeuwen PHE, Bliechrodt RP, Strik C et al (2010) Enhanced recovery after surgery (ERAS) versus conventional postoperative care in colorectal surgery. J Gastrointest Surg 14:88–95
Greco M, Capretti G, Beretta L et al (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38:1531–1541. https://doi.org/10.1007/s00268-013-2416-8
Smart NJ, White P, Allison AS et al (2014) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery:early prediction model. Colorectal Dis 14(10):e727–e734
Wilson RJT, Davies S, Redman J et al (2010) Impaired functional capacity is associated with all cause mortality after major elective intra-abdominal surgery. Br J Anaesth 105(3):297–303
Shukri FK, Henderson WG, DePalma RG et al (2005) Determinants of long term survical after major surgery and adverse effects of post operative complications. Ann Surg 242(3):326–343
Lawrence VA, Hazuda HP, Cornell JE et al (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 199(5):762–772
Fearon KCH, Ljungqvist O, von Meyenfeldt M et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
Carmichael JC, Keller DS, Baldini G et al (2017) Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgerons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 60(8):761–784
Topp R, Ditmyer M, King K et al (2002) The effect of bed rest and potential of prehabilitation on patients in the intensive care unit. AACN Clin Issues 13(2):263–276
Carli F, Zavorsky GS (2005) Optimizing functional exercise capacity in the elderly surgical population. Curr Opin Clin Nutr Metab Care 8(1):23–32
Lemanu DP, Singh PP, Maccormik AD et al (2013) Effect of preoperative exercise on cardiorespiratory function and recovery after surgery: a systematic review. World J Surg 37:711–720. https://doi.org/10.1007/s00268-012-1886-4
Pouwels S, Stokmans RA, Willigendael EMB et al (2014) Preoperative exercise for elective major abdominal surgery: a systematic review. Int J Surg 12:134–140
Bruns ERJ, van den Heuvel B, Buskens CJ et al (2016) The effects of physical prehabilitation in elderly patients undergoing colorectal surgery: a systematic review. Colorectal Dis 18:O267–O277
Moran J, Guinan E, McCormick P et al (2016) The ability of prehabilitation to influence post-operative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery 160(5):1189–1201
Higgens JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Wells GA, Shea B, O’Connel D, et al (2013) The Newcastle-Ottawa scale (NOS) for assessing the quailty of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed October 2017
Minnella EM, Bousquet-Dion G, Awasthi R et al (2017) Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer:a five year research experience. Acta Oncol 56(2):295–300
Dettling DS, van der Schaaf M, Blom RLGM et al (2013) Feasibility and effectiveness of pre-operative inspiratory muscle training in patients undergoing oesophagectomy: a pilot study. Physiother Res Int 18:16–26
Dronkers J, Veldman A, Hoberg E et al (2008) Prevention of pulmonary complications after upper abdominal surgery by preoperative intensive inspiratory muscle training: a randomized controlled pilot study. Clin Rehabil 22:134–142
Inoue J, Ono R, Makiura D et al (2013) Prevention of postoperative pulmonary complications through intensive preoperative respiratory rehabilitation in patients with esophageal cancer. Dis Esophagus 26:68–74
van Adrichem EJ, Meulenbroek RL, Plukker JTM et al (2014) Comparison of two preoperative programs to prevent pulmonary complications in patients undergoing esophagectomy: a randomized controlled pilot study. Ann Surg Oncol 21:2353–2360
Cho H, Yoshikawa T, Oba MS et al (2014) Matched pair analysis to examine the effects the effects of a planned preoperative exercise program in early gastric cancer patients with metabolic syndrome to reduce operative risk: the adjuvant exercise for general elective surgery (AEGES) study group. Ann Surg Oncol 21:2044–2050
Soares SM, Nucci LB, Silva M et al (2013) Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehabil 27(7):616–627
Dronkers JJ, Lamberts H, Naber RH et al (2010) Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 24:614–622
Barakat HM, Shahin Y, Khan JA et al (2016) Preoperative supervised exercise improves outcomes after elective abdominal aortic repair—a randomised controlled trial. Ann Surg 264:47–53
Barberan-Garcia A, Ubré M, Roca J et al (2017) Personalised prehabilitation in high- risk patients undergoing elective major abdominal surgery—a randomized blinded control trial. Ann Surg. https://doi.org/10.1097/sla.0000000000002293
Carli F, Charlebois P, Stein B et al (2010) Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg 97:1187–1197
Burden ST, Hill J, Shaffer JL et al (2011) An unblended randomised controlled trial of preoperative oral supplements in colorectal cancer patients. J Hum Nutr Diet 24:441–448
Gillis C, Loiselle SE, Fiore JF et al (2016) Prehabilitation with whey protein supplementation on perioperative functional exercise capacity in patients undergoing colorectal resection for cancer: a pilot double-blinded randomized placebo-controlled trial. J Acad Nutr Diet 116(5):802–812
Jie B, Jiang ZM, Nolan MT et al (2012) Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 28:1022–1027
Sorenson LT, Jorgenson LT (2003) Short-term pre-operative smoking cessation intervention does not affect postoperative complications in colorectal surgery: a randomized clinical trial. Colorectal Dis 5:347–352
Jung KH, Kim SM, Choi MG et al (2015) Preoperative smoking cessation can reduced post operative complications in gastric cancer surgery. Gastric Cancer 18(4):683–690
Li C, Carli F, Lee L et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal surgery: a pilot study. Surg Endosc 27:1072–1082
Gillis C, Li C, Lee L et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121(5):937–947
Thomsen T, Villebro N, Møller AM (2014) Interventions for preoperative smoking cessation. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD002294.pub4
Stone AA, Shiffman S, Schwartz JE et al (2003) Patient compliance with paper and electronic diaries. Control Clin Trials 24:182–199
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm they hold no conflict of interest or financial disclosures.
Rights and permissions
About this article
Cite this article
Luther, A., Gabriel, J., Watson, R.P. et al. The Impact of Total Body Prehabilitation on Post-Operative Outcomes After Major Abdominal Surgery: A Systematic Review. World J Surg 42, 2781–2791 (2018). https://doi.org/10.1007/s00268-018-4569-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4569-y