Abstract
Background
Centenarians are used as a model of healthy ageing and longevity. Diet is a factor known to affect mortality in middle aged adults and elderly. However, it is unknown whether diet has an impact on survival to 100 + years. The aims of this systematic review were to summarize the evidence on (i) the association between dietary patterns in late adult life and survival to 100 + years and (ii) the common characteristics across dietary patterns that are shown to be positively associated with survival to 100 + years.
Methods
We performed a systematic literature search in MEDLINE and EMBASE, and a hand search at four longevity projects homepages up to 4 June 2021. We searched for cohort and case–control studies investigating the association between dietary patterns and all-cause mortality among individuals aged ≥ 65 years at enrolment regardless of their health status and residence. Studies were excluded if follow-up was performed too soon to allow the population or a subgroup of it to have become 100 + years of age.
Results
Of 3,685 identified records 108 reports were retrieved and full text screened. No studies met our inclusion criteria, thus the review process resulted in no eligible studies found. Hence, no risk of bias assessment and no synthesis of data was performed.
Conclusions
No studies have investigated dietary patterns in late adult life in relation to survival to 100 + years of age. We have observed that as of June 2021 published cohort studies exist investigating all-cause mortality risk from different dietary patterns among the oldest old, but follow-up has been performed before the cohort could have reached 100 years of age. However, cohorts do exist where data on dietary habits in adult life has been collected decades ago and where follow-up in 2022 will allow the participants to have become 100 + years old.
Registration
The review protocol is published at University of Southern Denmark’s Research Portal (Poulsen et al. Dietary Patterns and Survival to 100 + Years: Protocol for a Systematic Review of cohort and case–control studies University of Southern Denmark's Research Portal: University of Southern Denmark, 2021) available at https://portal.findresearcher.sdu.dk/en/publications/kostm%C3%B8nstre-og-overlevelse-til-100-%C3%A5r-protokol-for-en-systematisk. We have specified aim (i) of our research question in this report compared to the protocol, by adding “late” to “adult life”.
Similar content being viewed by others
Background
Centenarians are being studied as a model for healthy ageing [1,2,3,4] aiding researchers in understanding the determinants of both exceptional health span and life span. Centenarians do not only exhibit intriguing exceptional survivorship. A large fraction of the population also seems to have lived independently into their nineties [5], and around 10–35% might continue to do so after reaching age 100 [4,5,6]. While a few centenarians might escape age-associated diseases, e.g., heart disease, diabetes, stroke, and various cancers [7], it has been suggested that the majority of centenarians do get affected by major diseases and either survive with or delay the onset of these [6, 7]. Understanding factors that has promoted this group of individuals’ longevity holds the potential for improving primary and secondary preventive efforts.
Human life span varies due to several factors. Studies of Danish twins estimate that genetic factors account for approximately 25% of the variation [8, 9]. This leaves 75% to be determined by a combination of random phenomena experienced throughout life and environmental factors, e.g., lifestyle factors [10]. Lifestyle factors including tobacco use, use of alcohol, physical activity, and diet are behaviours that are influencing life span in adult populations by affecting the risk of developing age-associated non-communicable diseases [11, 12]. Currently, these diseases are the main reasons for death at adult ages in high-income countries [13].
To assess the effects of overall dietary patters on morbidity and mortality outcomes, different approaches to measuring dietary patterns have been developed. One method is estimating adherence to predefined dietary guidelines operationalized as dietary quality indices (DQI). A plethora of DQI exists, e.g., the Mediterranean Diet Score, the Healthy Eating Index, and the Healthy Diet Indicator, and updated or adapted versions of these [14,15,16]. Through primarily epidemiologic research inverse associations with DQI and cardiovascular disease mortality, cancer mortality, as well as all-cause mortality have been documented [15, 16]. While some food components in DQI are common, e.g. vegetables and fruits, other components, such as olive oil, are not found in most of the DQI [15]. Dietary patterns have also been calculated by the means of factor or cluster analyses. These are a posterior data driven approaches, where dietary patterns are identified based on individuals sharing same dietary components, often resulting in two distinct patterns: prudent and Western [17]. Further, diet diversity scores (DDS) have been developed. Scores are derived by counting the number of different food groups or foods within groups consumed. The scores are intended to reflect how diverse the diet is and thus to which degree essential needs for nutrients are met [18]. Some DQI include this diversity or variety component, while other DQI indices reflect either intake of healthy or unhealthy dietary components, or both [15].
Embarking on the journey to elucidate the role of dietary patterns in centenarians’ health and exceptional longevity, surveys of centenarians’ diets have been conducted in different parts of the world, e.g. in Greece [19], China [20, 21], Italy [22], and Japan [23, 24]. However, attempting to establish if dietary behaviours can be regarded as one of the explanations to the exceptional survivorship of centenarians, it is essential to study adults’ dietary patterns years before they potentially become centenarians. This warrants longitudinal studies.
Findings from longitudinal studies investigating the association between adherence to healthy dietary patterns and survival among primarily European and American middle aged and younger elderly have been summarized in systematic reviews. Summarized healthy dietary patterns includes adherence to the Mediterranean Diet (MD) [25], the Dietary Approaches to Stop Hypertension, and diets scoring high on the Healthy Diet Index, and the Alternative Healthy Eating Index [16, 26, 27]. Meta-analyses of data on these dietary patterns have provided consistent results showing an association between adherence to these healthy diets and survival. Pooled estimates have showed that individuals within the categories of highest adherence to healthy dietary patterns have 20–22% lower all-cause mortality-risk than adults within the lowest healthy diet-scores groups [16, 25,26,27]. Further, it has been shown that one standard deviation increment in adherence to the MD is significantly associated with an 8% reduction in all-cause mortality risk [25]. Estimates were based on data from models in primary studies with relevant adjustment for a number of potential confounders, e.g., age, sex, smoking, biometrical measures, and prevalent or family history of diseases [16, 25,26,27].
It seems intuitive to extrapolate the protective effect of adhering to a healthy diet on mortality risk during adult life to old and exceptional old ages. However, it is suggested that the effect of some risk factors change in the highest ages [28,29,30]. Although far less studied, however, some evidence exists that the association between healthy dietary habits and survival in fact could persist into old age. One study among Chinese individuals aged ≥ 80 years documented a significant association between dietary habits and mortality risk. Diet quality was assessed using a diet diversity score (DDS), which was calculated by counting one DDS unit per 1 of 9 major food groups consumed “often or almost daily”. The authors report a trend of a 9% decrease in mortality risk by one unit increase in DDS after comprehensive adjustment [31].
We intend to evaluate the progress in this research field by elucidating if dietary behaviours are a determinant of achieving exceptional survivorship. To our knowledge no systematic review exists on dietary habits in relation to survival to 100 + years.
Therefore, this systematic review was done to summarize findings from published studies to investigate (i) the association between dietary patterns in late adult life and survival to 100 + years and (ii) the common characteristics across dietary patterns that are shown to be positively associated with survival to 100 + years.
Methods
This systematic review was conducted in concordance with a pre-published study protocol [32]. It was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses updated in 2020 (PRISMA 2020) [33, 34] where applicable as documented in the PRISMA 2020 Checklist (See Additional file 1). Additionally, we integrated advise from papers discussing how to report empty reviews [35,36,37,38].
Search strategy
The search strategy was developed through four processes: (i) WP performed preliminary searches for systematic reviews on longevity, (ii) WP conducted crude searches for primary studies on dietary patterns and longevity, (iii) we received guidance from a health information specialist with experience in conducting systematic review at the library at University of Southern Denmark, and (iv) KC and CD reviewed the search strategy. On June 4th, 2021, WP conducted a systematic search in the bibliographic databases “MEDLINE(R) All” and “Embase Classic + Embase”, both through the Ovid interface, covering from 1946 and 1947, respectively, until present. We build a search strategy based on the Population-Exposure-Outcome (PEO) framework consisting of three facets based on the terms “Diet”, “Longevity”, and “Elderly”. We implemented the Ovid Expert Search Filters for focused searches on elderly in both databases [39]. No other filters or limits were used. The search histories for Medline and Embase including search terms in full detail are presented in additional tables (see Additional Tables 1 and 2, respectively).
During the development of the search strategy, we identified four longevity projects with collected dietary data that also had an accessible homepage:
-
Leiden Longevity Study at http://www.leidenlangleven.nl/en/home
-
Life and Living in Advanced Age Study at https://www.fmhs.auckland.ac.nz/en/faculty/lilacs.html
-
Chinese Longitudinal Health Longevity Study at https://www.icpsr.umich.edu/web/NACDA/series/487/publications and
-
Japan Semi-Supercentenarian Study at http://www.keio-centenarian.com/english/research/jss
By June 4, 2021, WP searched these homepages for reports including “diet” in the title by using the search functionality in the Microsoft Edge browser.
Eligibility criteria
We screened for prospective, retrospective, and multi-centre cohort and case control studies examining individuals ≥ 65 years at enrolment. This also included studies enrolling participants older than 65 years, e.g., ≥ 80 years of age. We employed no restrictions regarding health status or residence. Studies including adults ≥ 18 years were eligible if data on participants aged ≥ 65 years at enrolment was presented separately. We considered dietary patterns in concordance with the following definition: “The quantities, proportions, variety, or combination of different foods, drinks, and nutrients (when available) in diets, and the frequency with which they are habitually consumed” [40] regardless of the methodology used to assess the dietary pattern, e.g. by a priori defined DQI or through a posterior factor or cluster analysis [40, 41]. Studies reporting all-cause mortality as a single outcome or reporting this separately in studies with several outcome measures were eligible. We implemented no time-specific length of follow-up, but an age criterium. Reports were only eligible if we based on the presented methods and results could deduce that every individual in the study population or a subgroup could have reached a 100 + years of age during the follow-up period. We considered published primary studies in English, Danish, Swedish, and Norwegian without limits to year of dissemination.
Selection process
WP performed title/abstract screening of each record imported to Covidence and subsequently assessed eligibility of the retrieved reports by full text screening. CD independently assessed three full text articles of which doubts about eligibility existed. Consensus was reached through discussion.
Results
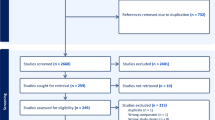
The flow of records through the review process is illustrated in Fig. 1.
Our search strategy identified a total of 3,685 records, of which 999 were duplicates and therefore removed. In total 2,682 records were title/abstract-screened and 2,574 were excluded. We retrieved 108 reports, assessed eligibility by full text screening, and excluded all reports eventually. Exclusion was mainly due to studies not having long enough follow-up time to allow the cohort participants to be 100 + years, studies investigating other exposures than dietary patterns, and publications not being primary studies but for example conference abstracts and editorials. The reason for excluding each study along with citation information is presented in an additional table (See Additional table 3). Thus, the process resulted in no eligible studies for the systematic review, and consequently, since no studies were eligible, we performed no risk of bias assessment and no data synthesis.
Discussion
This systematic review aimed to investigate the association between dietary habits in late adult life and survival to 100 + years and further to elucidate if common characteristics exist across dietary patterns associated with exceptional longevity. No studies met our inclusion criteria; hence we report an empty review, and therefore, at the current state of art, evidence remains inconclusive regarding whether dietary habits increase the probability in late life to become 100 years old.
A limited output of the systematic review process may have been expected, because studies investigating associations between diets among the oldest age groups and survival are scarce. However, it was anticipated that some of the oldest cohorts having collected dietary data, e.g., the Nurses’ Health Study [42], the Framingham Heart Study [43], and the Glostrup Population Studies [44], could have provided a first indication of whether dietary patterns continue to affect the mortality risk at high ages in the same way as observed in younger ages.
Evidence exists regarding which diets that increase our probability of surviving into old age [16, 25,26,27], but no longitudinal evidence exists on whether dietary habits continue to affect the chances of surviving from old to exceptional old age. It has been shown that some factors associated with higher mortality risk in adults and younger elderly lose their impact on survival among nonagenarians [45] and centenarians [46], e.g., socioeconomic status [45] and smoking [45, 46]. Therefore, it is still also debatable if the effect of healthy dietary habits on survival among adults and elderly might diminish among the oldest old populations.
Consensus exists that empty reviews are of value despite that no conclusions on the research question can be reached [35,36,37,38]. Lang et al. (2007) argues that new insights can be gained, as empty reviews “a) tell us who is undertaking the review and thus who is interested in the topic, b) highlight major research gaps, and c) indicate the state of research evidence at a particular point in time.” ([37], p. 596). It is suggested to summarize key messages from screened ineligible studies and to present observations compiled through the screening process of retrieved reports [35, 37], while being highly aware of the risk of bias, because cited studies are not selected based on inclusion criteria outlined prior to the review process [35, 36, 38].
Although this systematic review resulted in no eligible studies, we did some relevant observations during the screening of full text articles.
First, we observed that in 15 of the 108 full text screened reports follow-up had been performed at a timepoint when the entire population or a defined subgroup was ≥ 80 years of age [31, 47,48,49,50,51,52,53,54,55,56,57,58,59,60]. Thus, it seems that enough primary research has been conducted to investigate through a meta-analysis if an association exists between healthy dietary patterns and survival among the oldest old. However, this is beyond the scope of this paper. Among the 15 reports, we noted two studies which came close to being eligible for answering our research question. In one study among 1,990 participants aged ≥ 80 years from Pennsylvania, USA, the entire study population had reached ≥ 88 years of age at follow-up [58]. This represents the highest collective follow-up age identified in our systematic search. In this study, a dietary screening tool reflecting diet quality was developed and validated for the specific population. Points were assigned for both intake of specific found groups, such as whole grain breads and fruits, as well as not consuming other specific food groups, e.g., candy or chocolate, and bacon or sausages. The authors reported that having a high diet quality, defined as scoring > 75 of 105 possible points, was associated with lower mortality risk (adjusted HR = 0.76; 95% CI = 0.59–0.97; P-trend = 0.04) compared with having a low diet quality, i.e., scoring < 60 points. The analysis included adjustment for known potential confounders including sociodemographic covariates such as sex, age, BMI, and race, as well as variables indicating disease burden, e.g., oral health problems, and diagnosed diseases. However, the adjustment did not include income or educational attainment indicating socioeconomic status. The authors performed several secondary analyses which all suggested robustness of findings [58]. However, no subgroup analyses excluding individuals aged < 100 years at follow-up were performed. Thus, the study does not formally elucidate the impact of diet on survival to 100 + years. In another report from a study among 28,790 Chinese oldest olds, the researchers performed stratified survival analyses with individuals aged 100 + years at baseline constituting a strata [31]. A diet diversity score (DDS) was calculated for each participant with a maximum of 9 obtainable points, each point representing “often or almost daily” consumption of foods within one of 9 food groups, e.g., fish and seafood, beans, and tea. The overall finding for the entire cohort aged ≥ 80 years at baseline was a significant inverse association between the DDS and survival in the comprehensively adjusted analysis after a mean follow-up time of 3.4 years. The analysis included adjustment for sociodemographic variables such as age, sex, educational background, and living patterns, as well as lifestyle related covariates including smoking, and further considered substantial potential confounders of disease and disability, e.g., number of teeth, heart disease, and disabilities in activities of daily living. Overall, one increase in DDS was associated with a reduced mortality risk (HR = 0.91; 95% CI = 0.90–0.92; P-trend < 0.001). Individuals with the most diverse diets defined as a DDS ≥ 6 points had a HR of 0.56 (95% CI = 0.53–0.58) compared to individuals with the least diverse diets reflected by a score < 2 points. The effect decreased by increasing age in three strata (octogenarians, nonagenarians, and centenarians). For individuals aged ≥ 100 years at baseline one increase in DDS was associated with HR of 0.93 (95% CI = 0.92–0.94) [31]. Although including centenarians, this study does not investigate what dietary habits these individuals had while they were in their eighties or nineties, or younger. However, if increasing diet diversity is associated with better survival among octogenarians and nonagenarians, it is likely to be associated with better chances of becoming a centenarian. In other words, the nascent evidence from these two studies indicates that diets scoring high in quality or diversity continue to impact survival for individuals in their eighties, and nineties, and for centenarians.
Second, we noticed one report that investigated change in dietary habits over time among 17,959 Chinese individuals aged ≥ 65 years. Consumption of foods within 9 different food groups, e.g., fresh fruit, fish, fresh vegetables, and beans, was collected at two time points with 2–5 years between baseline and first follow-up. A diet diversity score (DDS) was calculated assigning 1 point per food group consumed 1–4 times/week and 2 points per food group consumed ≥ 5 times/week, allowing scores ranging from 0–18 points. Subsequently the relation between changes in DDS and mortality was investigated [61]. The authors reported that regardless of how the participants’ DDS changed, e.g., from low to medium or high scores, from medium to high scores, or from high to medium or low scores, the individuals maintaining high scores (13–18 points) had a lower mortality risk. The results shows that a highly diverse diet throughout several years is associated with a lower mortality risk at ages ≥ 65 years [61]. However, this study did not have a follow-up time long enough to allow the population to be 100 + years and thus does not provide information regarding if this association persists among individuals reaching 100 years of age.
Third, we identified numerous cohorts having collected data on diet among middle aged adults and/or elderly during the 1970’ies, 1980’ies, and 1990’ies (Table 1). Given that up to five decades have already passed since the establishment of these cohorts, a hundred years have passed since the entire population within some of these cohort was born. Within a decade, the same situation will occur for additional cohorts. This might allow the conduct of original studies linking collected data on diet in adulthood with mortality data and hence elucidating the association between dietary patterns in adult life and survival to 100 + years. It will, nonetheless, require very large original sample sizes to make meaningful statistical analyses due to sample attrition.
This systematic review has limitations. First, only one author screened titles and abstracts which may have resulted in missed relevant studies [34]. However, this seems unlikely as 108 papers were retrieved and full text-screened to assure that no studies had relevant subgroup or supplementary analyses concordant with our eligibility criteria. Second, we only looked for published studies and some unpublished information might be found in the above-mentioned cohorts already. Third, we chose to search for studies with cohort and case–control designs, because we expected to find at least a few eligible studies. With the review process coming up empty, we could have included lower quality evidence such as cross-sectional studies. However, as we aimed to elucidate if dietary patterns affect the probability of surviving to 100 years, cross-sectional studies will not suffice. Fourth, the largest exclusion of studies was caused by the inclusion criteria of long enough follow-up time to allow participants to survive to 100 + years as a definition of exceptional longevity. However, exceptional longevity could be defined otherwise [9]. Another option would have been to choose a top x% oldest of a specific sex- and birth cohort where the age defined as exceptional longevity was set by the implemented percentage, e.g., the top 1% oldest American males born in 1900 [9]. Implementing a definition of exceptional survival as a top x% of survivors, eligible primary studies would have to have results at follow-up ages corresponding to the chosen percentage and of the chosen sex to be comparable. The follow-up age would then vary across cohorts because different birth cohorts in different areas of the world have been impacted by different secular trends [9, 76]. However, this method to define exceptional survival and follow-up ages has not been implemented in any of the excluded cohort studies. A third opportunity for defining exceptional longevity could be to lower the age threshold from 100 to, e.g., 90 years. This would potentially increase the probability of finding eligible studies, as a shorter follow-up period would be required. However, while there are numerous centenarian studies worldwide that search for determinants of longevity, there are few studies using 90 years as eligibility criteria. Furthermore, centenarians are a much more selected group than 90-year-olds. In the Danish 1905 cohort the probability of surviving from birth to 92 years (1 in 20) is about the same as surviving from age 93 to 100 years (again 1 in 20) [77].
Conclusion
This systematic review resulted in no eligible studies that met our a priori chosen inclusion criteria and hence we have reported an empty review. Consequently, no direct evidence currently exists on the association between dietary habits in late adult life and survival to 100 + years. We have identified several cohorts worldwide where data on diet has been collected during the participants’ adult lives, and where a century has passed since the participants were born. Thus, cohort studies combining already collected dietary data with updated mortality data could be conducted within these cohorts. Attention should be directed at the sizes of the original cohorts to ensure sufficient power after sample attrition.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Gurinovich A, Song Z, Zhang W, Federico A, Monti S, Andersen SL, et al. Effect of longevity genetic variants on the molecular aging rate. GeroScience. 2021;43(3):1237–51.
Engberg H, Oksuzyan A, Jeune B, Vaupel JW, Christensen K. Centenarians–a useful model for healthy aging? A 29-year follow-up of hospitalizations among 40,000 Danes born in 1905. Aging Cell. 2009;8(3):270–6.
Almeida I, Magalhães S, Nunes A. Lipids: biomarkers of healthy aging. Biogerontology. 2021;22(3):273–95.
Motta M, Bennati E, Ferlito L, Malaguarnera M, Motta L. Successful aging in centenarians: myths and reality. Arch Gerontol Geriatr. 2005;40(3):241–51.
Hitt R, Young-Xu Y, Silver M, Perls T. Centenarians: the older you get, the healthier you have been. Lancet. 1999;354(9179):652.
Andersen-Ranberg K, Schroll M, Jeune B. Healthy centenarians do not exist, but autonomous centenarians do: a population-based study of morbidity among Danish centenarians. J Am Geriatr Soc. 2001;49(7):900–8.
Evert J, Lawler E, Bogan H, Perls T. Morbidity Profiles of Centenarians: Survivors, Delayers, and Escapers. J Gerontol A Biol Sci Med Sci. 2003;58(3):M232–7.
Herskind AM, McGue M, Holm NV, Sørensen TIA, Harvald B, Vaupel JW. The heritability of human longevity: A population-based study of 2872 Danish twin pairs born 1870–1900. Hum Genet. 1996;97(3):319–23.
Skytthe A, Pedersen NL, Kaprio J, StaziMA,HjelmborgJvB, Iachine I, et al. Longevity Studies in GenomEUtwin. Twin Res. 2003;6(5):448–54.
Govindaraju D, Atzmon G, Barzilai N. Genetics, lifestyle and longevity: Lessons from centenarians. Appl Transl Genom. 2015;4:23–32.
United Nations - Department of Economics and Social Affairs: Population Division. World Mortality Report 2015: Highlights. www.un.org: United Nations, Division UN-DoEaSAP; 2017. Report No.: ST/ESA/SER.A/382.
World Health Organization. Global Health Observatory (GHO) data: Risk factors: World Health Organization. 2020. (https://www.who.int/gho/ncd/risk_factors/en/).
United Nations - Department of Economics and Social Affairs: Population Division. World Mortality 2019. www.un.org: United Nations, Division DoEaSAP; 2019. Report No.: ST/ESA/SER.A/437.
Aljuraiban GS, Gibson R, Oude Griep LM, Okuda N, Steffen LM, Van Horn L, et al. Perspective: The Application of A Priori Diet Quality Scores to Cardiovascular Disease Risk—A Critical Evaluation of Current Scoring Systems. Adv Nutr. 2020;11(1):10–24.
Wirt A, Collins CE. Diet quality–what is it and does it matter? Public Health Nutr. 2009;12(12):2473–92.
Morze J, Danielewicz A, Hoffmann G, Schwingshackl L. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Second Update of a Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet. 2020;120(12):1998-2031.e15.
Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104(4):615–35.
Ruel MT. Operationalizing Dietary Diversity: A Review of Measurement Issues and Research Priorities. J Nutr. 2003;133(11):3911S-S3926.
Stathakos D, Pratsinis H, Zachos I, Vlahaki I, Gianakopoulou A, Zianni D, et al. Greek centenarians: assessment of functional health status and life-style characteristics. Exp Gerontol. 2005;40(6):512–8.
Chen C. A survey of the dietary nutritional composition of centenarians. Chin Med J. 2001;114(10):1095–7.
Yang S, Wang S, Wang L, Liu G, Tai P, Kou F, et al. Dietary behaviors and patterns of centenarians in Hainan: A cross-sectional study. Nutrition. 2021;89:111228.
Vasto S, Scapagnini G, Rizzo C, Monastero R, Marchese A, Caruso C. Mediterranean diet and longevity in Sicily: survey in a Sicani Mountains population. Rejuvenation Res. 2012;15(2):184–8.
Akisaka M, Asato L, Chan YC, Suzuki M, Uezato T, Yamamoto S. Energy and nutrient intakes of Okinawan centenarians. J Nutr Sci Vitaminol (Tokyo). 1996;42(3):241–8.
Chan YC, Suzuki M, Yamamoto S. Dietary, anthropometric, hematological and biochemical assessment of the nutritional status of centenarians and elderly people in Okinawa, Japan. J Am Coll Nutr. 1997;16(3):229–35.
Eleftheriou D, Benetou V, Trichopoulou A, La Vecchia C, Bamia C. Mediterranean diet and its components in relation to all-cause mortality: meta-analysis. Br J Nutr. 2018;120(10):1081–97.
Schwingshackl L, Bogensberger B, Hoffmann G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet. 2018;118(1):74-100.e11.
Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780-800.e5.
Forette B. Are Common Risk Factors Relevant in the Eldest Old? In: Robine J-M, Forette B, Franceschi C, Allard M, SpringerLink, editors. The Paradoxes of Longevity. 1. 1st ed. Berlin: Springer Berlin Heidelberg; 1999. p. 73–9.
Ben-Ezra M, Shmotkin D. Predictors of mortality in the old-old in Israel: the Cross-sectional and Longitudinal Aging Study. J Am Geriatr Soc. 2006;54(6):906–11.
Nybo H, Petersen HC, Gaist D, Jeune B, Andersen K, McGue M, et al. Predictors of mortality in 2,249 nonagenarians–the Danish 1905-Cohort Survey. J Am Geriatr Soc. 2003;51(10):1365–73.
Lv Y, Kraus VB, Gao X, Yin Z, Zhou J, Mao C, et al. Higher dietary diversity scores and protein-rich food consumption were associated with lower risk of all-cause mortality in the oldest old. Clin Nutr. 2020;39(7):2246–54.
Poulsen W, Christensen K, Dalgård C. Dietary Patterns and Survival to 100+ Years: Protocol for a Systematic Review of cohort and case-control studies University of Southern Denmark’s Research Portal: University of Southern Denmark. 2021. (https://portal.findresearcher.sdu.dk/en/publications/kostm%C3%B8nstre-og-overlevelse-til-100-%C3%A5r-protokol-for-en-systematisk).
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Cochrane Effectie Practice and Organisation of Care (EPOC). Reporting empty review and results from excluded studies. 2017. (https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/reporting_empty_reviews_and_results_from_excluded_studies.pdf).
Schlosser RW, Sigafoos J. ‘Empty’ reviews and evidence-based practice. Evid Based Commun Assess Interv. 2009;3(1):1–3.
Lang A, Edwards N, Fleiszer A. Empty systematic reviews: hidden perils and lessons learned. J Clin Epidemiol. 2007;60(6):595–7.
Green S, Higgins JPT, Schünemann HJ, Becker L. Response to paper by Lang A, Edwards N, and Fleiszer A. J Clin Epidemiol. 2007;60(6):598–9.
Wolters Kluver Health. Ovid Tools and Resources Portal - Expert Searches. 2021. (https://tools.ovid.com/ovidtools/expertsearches.html#embase).
United States Department of Agriculture - Nutrition Evidence Systematic Review. A Series of Systematic Reviews on the Relationship Between Dietary Patterns and Health Outcomes. https://nesr.usda.gov/: Center for Nutrition Policy and Promotion; 2014 March 2014.
Wirfält E, Drake I, Wallström P. What do review papers conclude about food and dietary patterns? Food Nutr Res. 2013;57:20523.
Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, et al. Origin, Methods, and Evolution of the Three Nurses’ Health Studies. Am J Public Health. 2016;106(9):1573–81.
Dawber TR, Meadors GF, Moore FE Jr. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951;41(3):279–81.
Hagerup L, Eriksen M, Schroll M, Hollnagel H, Agner E, Larsen S. The Glostrup Population Studies Collection of epidemiologic tables: Reference values for use in cardiovascular population studies. Scand J Soc Med Suppl. 1981;20:1–112.
Thinggaard M, McGue M, Jeune B, Osler M, Vaupel JW, Christensen K. Survival Prognosis in Very Old Adults. J Am Geriatr Soc. 2016;64(1):81–8.
Alvarez JA, Medford A, Strozza C, Thinggaard M, Christensen K. Stratification in health and survival after age 100: evidence from Danish centenarians. BMC Geriatr. 2021;21(1):406.
Anderson AL, Harris TB, Tylavsky FA, Perry SE, Houston DK, Hue TF, et al. Dietary Patterns and Survival of Older Adults. J Am Diet Assoc. 2011;111(1):84–91.
Bonaccio M, Di Castelnuovo A, Costanzo S, Gialluisi A, Persichillo M, Cerletti C, et al. Mediterranean diet and mortality in the elderly: a prospective cohort study and a meta-analysis. Br J Nutr. 2018;120(8):841–54.
Brown JC, Harhay MO, Harhay MN. Physical Activity, Diet Quality, and Mortality among Community-Dwelling Prefrail and Frail Older Adults. J Nutr Gerontol Geriatr. 2016;35(4):253–66.
Brown JC, Harhay MO, Harhay MN. Physical activity, diet quality, and mortality among sarcopenic older adults. Aging Clin Exp Res. 2017;29(2):257–63.
Ding D, Rogers K, van der Ploeg H, Stamatakis E, Bauman AE. Traditional and Emerging Lifestyle Risk Behaviors and All-Cause Mortality in Middle-Aged and Older Adults: Evidence from a Large Population-Based Australian Cohort. PLoS Med. 2015;12(12):e1001917.
Greenlee H, Lovasi GS, Richardson J, Fried LP, Strizich G, Kaplan RC, et al. Concordance with Prevention Guidelines and Subsequent Cancer, Cardiovascular Disease, and Mortality: A Longitudinal Study of Older Adults. Am J Epidemiol. 2017;186(10):1168–79.
Mao Z, Prizment AE, Lazovich D, Bostick RM. Associations of dietary and lifestyle oxidative balance scores with mortality risk among older women: the Iowa Women’s Health Study. Eur J Nutr. 2021;60(7):3873–86.
Mitchell DC, Hartman TJ, Coffman DL, Craig Wood G, Still C, Hsiao PY, et al. Dietary patterns and relationship to obesity-related health outcomes and mortality in adults 75 years of age or greater. J Nutr Health Aging. 2013;17(6):566–72.
Sasakabe T, Wakai K, Ukawa S, Ando M, Kawamura T, Okabayashi S, et al. Food group intakes and all-cause mortality among a young older Japanese population of the same age: the New Integrated Suburban Seniority Investigation Project. Nagoya J Med Sci. 2021;83(1):169–82.
Stanaway FF, Ribeiro RV, Khalatbari-Soltani S, Cvejic E, Blyth FM, Naganathan V, et al. Diet quality in an ethnically diverse population of older men in Australia. Eur J Clin Nutr. 2021;75(12):1792–800.
Cao Z, Cheng Y, Li S, Sun L, Wang Y, Wang R, et al. Adherence to a healthy lifestyle counteracts the negative effects of risk factors on all-cause mortality in the oldest-old. Aging (Albany NY). 2019;11(18):7605–19.
Liu Y-H, Gao X, Mitchell DC, Wood GC, Still CD, Jensen GL. Diet Quality Is Associated With Mortality in Adults Aged 80 Years and Older: A Prospective Study. J Am Geriatr Soc. 2019;67(10):2180–5.
Knoops KTB, de Groot LC, van Staveren WA, Fidanza F, Alberti-Fidanza A, Kromhout D. Comparison of three different dietary scores in relation to 10-year mortality in elderly European subjects: The HALE project. Eur J Clin Nutr. 2006;60(6):746–55.
Knoops KTB, de Groot LCPGM, Kromhout D, Perrin A-E, Moreiras-Varela O, Menotti A, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292(12):1433–9.
Liu D, Zhang X-R, Li Z-H, Zhang Y-J, Wang Z-H, Shen D, et al. Association of dietary diversity changes and mortality among older people: A prospective cohort study. Clin Nutr. 2021;40(5):2620–9.
Fleming DJ, Tucker KL, Jacques PF, Dallal GE, Wilson PWF, Wood RJ. Dietary factors associated with the risk of high iron stores in the elderly Framingham Heart Study cohort. Am J Clin Nutr. 2002;76(6):1375–84.
Tognon G, Rothenberg E, Eiben G, Sundh V, Winkvist A, Lissner L. Does the Mediterranean diet predict longevity in the elderly? A Swedish perspective. Age (Dordr). 2011;33(3):439–50.
Lo C-H, Khalili H, Song M, Lochhead P, Burke KE, Richter JM, et al. Healthy Lifestyle Is Associated With Reduced Mortality in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2021;19(1):87-95.e4.
Inoue-Choi M, Robien K, Lazovich D. Adherence to the WCRF/AICR guidelines for cancer prevention is associated with lower mortality among older female cancer survivors. Cancer Epidemiol Biomarkers Prev. 2013;22(5):792–802.
Jankovic N, Geelen A, Streppel MT, de Groot LCPGM, Orfanos P, van den Hooven EH, et al. Adherence to a healthy diet according to the World Health Organization guidelines and all-cause mortality in elderly adults from Europe and the United States. Am J Epidemiol. 2014;180(10):978–88.
Diehr P, Beresford SAA. The relation of dietary patterns to future survival, health, and cardiovascular events in older adults. J Clin Epidemiol. 2003;56(12):1224–35.
Riboli E, Kaaks R. The EPIC Project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. INT J Epidemiol. 1997;26(suppl_1):S6.
Hofman A, Grobbee DE, de Jong PT, van den Ouweland FA. Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol. 1991;7(4):403–22.
Russell J, Flood V, Rochtchina E, Gopinath B, Mitchell P, Allman-Farinelli M, et al. Adherence to dietary guidelines and 15-year risk of all-cause mortality. Br J Nutr. 2013;109(3):547–55.
Limongi F, Noale M, Crepaldi G, Maggi S, Gesmundo A. Adherence to the Mediterranean Diet and all-cause mortality risk in an elderly Italian population: Data from the ILSA study. J Nutri Health Aging. 2017;21(5):505–13.
Hamer M, McNaughton SA, Bates CJ, Mishra GD. Dietary patterns, assessed from a weighed food record, and survival among elderly participants from the United Kingdom. Eur J Clin Nutr. 2010;64(8):853–61.
Reedy J, Krebs-Smith SM, Subar AF, Park Y, Miller PE, Liese AD, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6):881–9.
Shi Z, Zhang T, Byles J, Martin S, Avery JC, Taylor AW. Food Habits, Lifestyle Factors and Mortality among Oldest Old Chinese: The Chinese Longitudinal Healthy Longevity Survey (CLHLS). Nutrients. 2015;7(9):7562–79.
Molino-Lova R, Sofi F, Pasquini G, Gori A, Vannetti F, Abbate R, et al. The Mugello Study, a survey of nonagenarians living in Tuscany: Design, methods and participants’ general characteristics. Eur J Intern Med. 2013;24(8):745–9.
Guillot M. Period versus cohort life expectancy. In: Rogers RG, Crimmins EM, editors. International handbook of adult mortality. Dordrecht: Springer Netherlands; 2011. p. 533–49.
Christensen K, Thinggaard M, Oksuzyan A, Steenstrup T, Andersen-Ranberg K, Jeune B, et al. Physical and cognitive functioning of people older than 90 years: a comparison of two Danish cohorts born 10 years apart. Lancet. 2013;382(9903):1507–13.
Acknowledgements
We thank research librarian at the University Library of Southern Denmark, Sebrina Maj-Britt Hansen, for her specialist knowledge and guidance in building the search strategy.
Funding
The work on the review by WP was supported by a grant from the National Institute on Aging at National Institutes of Health, NIH/NIA U19-AG063893. The NIH/NIA had no role in the development of the scope or design of the review, the literature search, in preparation of the manuscript or in decisions regarding publishing.
Author information
Authors and Affiliations
Contributions
WP contributed substantially to the design of the review, made substantial contributions to the literature search, and drafted the manuscript. KC is the originator of the research questions, contributed substantially to the design of the review and in revising the draft. CD contributed substantially to the design of the review, the literature screening process, and in revising the draft. All authors have approved the submitted version of the manuscript.
Authors’ information
KC is head of the Danish Aging Research Center at the University of Southern Denmark.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Documentation of conformity to the PRISMA 2020 in reporting the systematic review of cohort and case-control studies on dietary patterns and survival to 100+ years.
Additional file 2: Additional Table 1.
Search history of Ovid MEDLINE(R) All 1946 to 4 June 2021 in the systematic review of cohort and case-c`ontrol studies on dietary patterns and survival to 100+ years.
Additional file 3: Additional Table 2.
Search history of Ovid Embase Classic+Embase 1947 to 4 June 2021 in the systematic review of cohort and case-control studies on dietary patterns and survival to 100+ years.
Additional file 4: Additional Table 3.
Distribution of 108 records assessed by full-text review across unfulfilled eligibility criteria in the systematic review of cohort and case-control studies on dietary patterns and survival to 100+ years.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Poulsen, W., Christensen, K. & Dalgård, C. Dietary patterns and survival to 100 + years: an empty systematic review of cohort and case–control studies. Arch Public Health 80, 161 (2022). https://doi.org/10.1186/s13690-022-00914-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-022-00914-2