Abstract
Background
The pivotal ASPECT-NP trial showed ceftolozane/tazobactam was non-inferior to meropenem for the treatment of ventilated hospital-acquired/ventilator-associated bacterial pneumonia (vHABP/VABP). Here, we evaluated treatment outcomes by degree of respiratory or cardiovascular dysfunction.
Methods
This was a subset analysis of data from ASPECT-NP, a randomized, double-blind, non-inferiority trial (ClinicalTrials.gov NCT02070757). Adults with vHABP/VABP were randomized 1:1 to 3 g ceftolozane/tazobactam or 1 g meropenem every 8 h for 8–14 days. Outcomes in participants with a baseline respiratory component of the Sequential Organ Failure Assessment (SOFA) score (R-SOFA) ≥ 2 (indicative of severe respiratory failure), cardiovascular component of the SOFA score (CV-SOFA) ≥ 2 (indicative of shock), or R-SOFA ≥ 2 plus CV-SOFA ≥ 2 were compared by treatment arm. The efficacy endpoint of primary interest was 28-day all-cause mortality. Clinical response, time to death, and microbiologic response were also evaluated.
Results
There were 726 participants in the intention-to-treat population; 633 with R-SOFA ≥ 2 (312 ceftolozane/tazobactam, 321 meropenem), 183 with CV-SOFA ≥ 2 (84 ceftolozane/tazobactam, 99 meropenem), and 160 with R-SOFA ≥ 2 plus CV-SOFA ≥ 2 (69 ceftolozane/tazobactam, 91 meropenem). Baseline characteristics, including causative pathogens, were generally similar in participants with R-SOFA ≥ 2 or CV-SOFA ≥ 2 across treatment arms. The 28-day all-cause mortality rate was 23.7% and 24.0% [difference: 0.3%, 95% confidence interval (CI) − 6.4, 6.9] for R-SOFA ≥ 2, 33.3% and 30.3% (difference: − 3.0%, 95% CI − 16.4, 10.3) for CV-SOFA ≥ 2, and 34.8% and 30.8% (difference: − 4.0%, 95% CI − 18.6, 10.3), respectively, for R-SOFA ≥ 2 plus CV-SOFA ≥ 2. Clinical cure rates were as follows: 55.8% and 54.2% (difference: 1.6%, 95% CI − 6.2, 9.3) for R-SOFA ≥ 2, 53.6% and 55.6% (difference: − 2.0%, 95% CI − 16.1, 12.2) for CV-SOFA ≥ 2, and 53.6% and 56.0% (difference: − 2.4%, 95% CI − 17.6, 12.8), respectively, for R-SOFA ≥ 2 plus CV-SOFA ≥ 2. Time to death was comparable in all SOFA groups across both treatment arms. A higher rate of microbiologic eradication/presumed eradication was observed for CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2 with ceftolozane/tazobactam compared to meropenem.
Conclusions
The presence of severe respiratory failure or shock did not affect the relative efficacy of ceftolozane/tazobactam versus meropenem; either agent may be used to treat critically ill patients with vHABP/VABP.
Trial registration: ClinicalTrials.gov NCT02070757. Registered 25 February 2014, https://clinicaltrials.gov/ct2/show/NCT02070757
Similar content being viewed by others
Background
Nosocomial pneumonia, comprising non-ventilated hospital-acquired, ventilated hospital-acquired, and ventilator-associated bacterial pneumonia (nvHABP/vHABP/VABP), is a relatively frequent infection in hospitalized patients, particularly those that are critically ill [1,2,3,4]. Mortality rates for nosocomial pneumonia range between approximately 20–50%, with the highest rates reported for vHABP and VABP [5,6,7,8,9,10]. Prompt initiation of appropriate antibacterial therapy improves survival; however, antibacterial resistance makes the selection of antibacterial agent(s) for the treatment of nosocomial pneumonia challenging [5, 9,10,11,12,13].
Ceftolozane/tazobactam is an approved combination antibacterial agent consisting of the antipseudomonal cephalosporin ceftolozane with the established β-lactamase inhibitor tazobactam. Ceftolozane/tazobactam has broad Gram-negative activity, that includes multidrug-resistant (MDR) Pseudomonas aeruginosa and extended-spectrum β-lactamase producing (ESBL+) Enterobacterales [14,15,16]. Ceftolozane/tazobactam penetrates the lung, and a dose of 3 g every 8 h provides target epithelial lining fluid (ELF) concentrations appropriate for nosocomial pneumonia [17,18,19]. The efficacy of ceftolozane/tazobactam for the treatment of vHABP/VABP was demonstrated in the phase 3, randomized, double-blind ASPECT-NP trial, in which participants received ceftolozane/tazobactam 3 g every 8 h or meropenem 1 g every 8 h, with dose adjustments for renal function [20].
Critically ill patients have altered antibacterial pharmacokinetics (PK) and pharmacodynamics (PD) [21], which may result in the inability to achieve optimal PK/PD targets for β-lactams, negatively impacting treatment outcomes [22, 23]. For these reasons, evaluation of treatment outcomes with ceftolozane/tazobactam specifically in critically ill patients with vHABP/VABP is important to determine its clinical utility in this high-risk population. We therefore conducted a post hoc subset analysis of efficacy outcomes in ASPECT-NP using respiratory and cardiovascular Sequential Organ Failure Assessment (SOFA) component scores as markers for greater severity of illness.
Methods
Study design overview
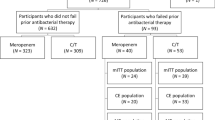
ASPECT-NP (protocol MK-7625A-008, ClinicalTrials.gov NCT02070757) was a phase 3, randomized, controlled, double-blind, multicenter, non-inferiority trial. Mechanically ventilated adults (≥ 18 years old) with nosocomial pneumonia were randomized 1:1, stratified by diagnosis (vHABP or VABP) and age (< 65 or ≥ 65 years old), to receive ceftolozane/tazobactam 3 g intravenously (IV) every 8 h or meropenem 1 g IV every 8 h, both adjusted for renal impairment. The study drugs were administered IV over 1 h for a duration of 8–14 days. Adjunctive linezolid 600 mg IV every 12 h (or a suitable alternative) was required for all participants until baseline lower respiratory tract (LRT) cultures confirmed the absence of Staphylococcus aureus. Adjunctive empirical therapy with amikacin 15 mg/kg IV daily was permitted for the first 72 h at study sites with ≥ 15% meropenem-resistant P. aeruginosa, as deemed necessary by the investigator (Fig. 1) [20].
ASPECT-NP study design [20]. h hour, ITT intent-to-treat, LRT lower respiratory tract, q8h every 8 h, TOC test-of-cure, SOFA Sequential Organ Failure Assessment, VABP ventilator-associated bacterial pneumonia, vHABP ventilated hospital-acquired bacterial pneumonia
A diagnosis of vHABP/VABP was based upon imaging showing new or progressive infiltrate, purulent tracheal secretions, and at least 1 additional clinical or laboratory criterion (fever, elevated/decreased white blood cell counts, or ≥ 15% immature neutrophils). vHABP was defined as pneumonia occurring in a mechanically ventilated participant in which at least one sign or symptom consistent with pneumonia (new/worsening cough, dyspnea, tachypnea, respiratory rate > 30 breaths per min, or hypoxemia) was present within the 24 h prior to intubation or within the 48 h after intubation in a participant who had been either hospitalized for ≥ 48 h or who had been discharged from a hospital within the prior 7 days (e.g., skilled nursing or other long-term care facility). VABP was defined as pneumonia in a participant who was mechanically ventilated for at least 48 h and had hypoxemia or required increased ventilator support. Quantitative LRT specimens were collected at baseline (within 36 h before the first dose of study drug) and post-baseline, including at the end-of-therapy (EOT) and at the test-of-cure (TOC) visit (7–14 days after the EOT visit) in participants who remained intubated or when clinically indicated. Pathogen identification and susceptibility were performed at local site microbiology laboratories and confirmed at a central microbiology laboratory, with standard broth microdilution methodology to verify minimum inhibitory concentrations (MICs) [20, 24].
Respiratory and cardiovascular SOFA component scores, along with total SOFA scores, were collected at baseline. A respiratory SOFA component score (R-SOFA) ≥ 2 corresponded to a PaO2/FiO2 < 300 mmHg. A cardiovascular SOFA component score (CV-SOFA) ≥ 2 corresponded to receipt of any dose of dopamine, dobutamine, epinephrine, or norepinephrine [25].
Participants were deemed clinically cured when they had a resolution of their baseline signs and symptoms, did not have any new signs or symptoms, and did not require additional antibacterial agents to treat their vHABP/VABP. Microbiologic response was categorized as eradication of all baseline pathogens [lower respiratory tract culture showing a ≥ 1-log reduction in baseline pathogenic bacterial burden, with a maximum per-pathogen count of 104 colony-forming units (CFU) per mL for endotracheal aspirate specimens, 103 CFU per mL for bronchoalveolar lavage specimens, and 102 CFU per mL for protected brush specimens] or presumed eradication in cases with clinical cure but no respiratory material to culture at the EOT or TOC visit [20].
This study was conducted in accordance with principles of Good Clinical Practice and was approved by the appropriate institutional review boards and regulatory agencies for all sites. All participants (or legally acceptable representatives) provided informed consent. Complete details of the ASPECT-NP study have been published previously by Kollef et al. [20].
Subset analysis
The population for this post hoc subset analysis consisted of all randomized participants from ASPECT-NP who had a baseline R-SOFA ≥ 2 or CV-SOFA ≥ 2, resulting in three intention-to-treat (ITT) groups: participants with R-SOFA ≥ 2, participants with CV-SOFA ≥ 2, and participants with R-SOFA ≥ 2 plus CV-SOFA ≥ 2. The microbiologic ITT (mITT) population included participants who received ≥ 1 dose of study drug and had ≥ 1 Gram-negative or streptococcal baseline LRT pathogen that was susceptible to at least one of the study drugs. Participants in the clinically evaluable (CE) population received study drug, adhered to the study protocol through the TOC visit, and had an evaluable clinical outcome at the TOC visit or clinical failure prior to the TOC visit.
Comparisons for outcomes between treatment arms in the R-SOFA ≥ 2, CV-SOFA ≥ 2, and R-SOFA ≥ 2 plus CV-SOFA ≥ 2 groups were based on a pre-specified analysis plan. Consistent with the pivotal study, the efficacy endpoint of primary interest was 28-day all-cause mortality. Clinical response, time to death, and microbiologic response were also evaluated in participants with R-SOFA ≥ 2, CV-SOFA ≥ 2, and R-SOFA ≥ 2 plus CV-SOFA ≥ 2. Additionally, to assess clinical utility in the most severely critically ill participants, outcomes between treatment arms were compared in participants with higher R- and CV-SOFA component scores (≥ 3 and 4) and SOFA > 6 versus ≤ 6.
The 28-day all-cause mortality, clinical response at the TOC visit, and microbiologic eradication/presumed eradication rates were compared using 2-sided unstratified Newcombe 95% confidence intervals (CIs) for the difference in proportions between the ceftolozane/tazobactam and meropenem arms according to R-SOFA, CV-SOFA, or SOFA [26]. Kaplan–Meier estimates were used to demonstrate time to death for each treatment arm in participants with a baseline R-SOFA ≥ 2, CV-SOFA ≥ 2, or R-SOFA ≥ 2 plus CV-SOFA ≥ 2.
Results
There were 312 participants in the ceftolozane/tazobactam arm and 321 participants in the meropenem arm who had a baseline R-SOFA ≥ 2, while there were 84 and 99 participants who had a baseline CV-SOFA ≥ 2 in each treatment arm, respectively. Sixty-nine ceftolozane/tazobactam-treated and 91 meropenem-treated participants had both R-SOFA ≥ 2 plus CV-SOFA ≥ 2 at baseline (Fig. 2).
Baseline and demographic characteristics were generally well balanced between treatment arms in participants with R-SOFA ≥ 2 or CV-SOFA ≥ 2, with some minor exceptions. In the CV-SOFA ≥ 2 group, there were more participants with vHABP and APACHE II score ≥ 20 in the ceftolozane/tazobactam than in the meropenem arm. A total SOFA score > 7 was more common in the meropenem arm in the R-SOFA ≥ 2 group, while failed prior antibacterial therapy was more frequent in the ceftolozane/tazobactam arm in the R-SOFA ≥ 2 and CV-SOFA ≥ 2 groups (Table 1).
Nearly all baseline LRT pathogens across the R-SOFA ≥ 2 and the CV-SOFA ≥ 2 groups and treatment arms were Gram-negative bacteria. The most frequent causative pathogens in both groups were Enterobacterales (most often Klebsiella pneumoniae and Escherichia coli) and P. aeruginosa. Approximately a third of Enterobacterales in the R-SOFA ≥ 2 group carried ESBL genes, compared with about a quarter of Enterobacterales in the CV-SOFA ≥ 2 group (Table 2). The MIC90 for all Gram-negative pathogens in the R-SOFA ≥ 2 group was 16 mg/L for ceftolozane/tazobactam and 1 mg/L for meropenem. In the CV-SOFA ≥ 2 group, the MIC90 for all Gram-negative pathogens was 8 mg/L and 0.5 mg/L, respectively, in each treatment arm (Table 3).
Although the observed mortality in the CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2 groups was higher compared to the mortality in the R-SOFA ≥ 2 group, the 28-day all-cause mortality rates across treatment arms were comparable within each individual SOFA group in the ITT population (Fig. 3a). Clinical cure rates at TOC with ceftolozane/tazobactam and meropenem were unaffected by R-SOFA ≥ 2, CV-SOFA ≥ 2, or R-SOFA ≥ 2 plus CV-SOFA ≥ 2 in the ITT (Fig. 3b) and CE population (Additional file 1: Fig. S1). There was no observed difference between ceftolozane/tazobactam and meropenem in time to death in participants with a baseline R-SOFA ≥ 2, CV-SOFA ≥ 2, or R-SOFA ≥ 2 plus CV-SOFA ≥ 2 in the ITT population (Fig. 4a–c).
Mortality (upper panel A) and cure at TOC (bottom panel B) by SOFA component score (ITT population). Treatment differences were calculated as unstratified Newcombe 95% CIs; positive differences are in favor of ceftolozane/tazobactam, negative differences are in favor of meropenem. Participants whose 28-day mortality outcome was missing or unknown were analyzed as deceased. Participants with clinical failure at the EOT visit were counted as failures at the TOC visit. CI confidence interval, CV-SOFA cardiovascular, EOT end-of-therapy, R-SOFA respiratory SOFA component score, SOFA Sequential Organ Failure Assessment, TOC test-of-cure
Microbiologic eradication/presumed eradication rates were higher in ceftolozane/tazobactam-treated participants with CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2 than with a baseline R-SOFA ≥ 2, while the microbiologic eradication/presumed eradication rates were consistent across all three SOFA groups in meropenem-treated participants. Additionally, a higher percentage of ceftolozane/tazobactam-treated participants had microbiologic eradication/presumed eradication as compared to meropenem-treated participants in the CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2 groups in the mITT population (Fig. 5).
Microbiologic eradication/presumed eradication at TOC by SOFA component score (mITT population). Observed microbiologic eradication is represented by the lighter colored bars; presumed eradication is represented by the darker colored bars. Treatment differences were calculated as unstratified Newcombe 95% CIs; positive differences are in favor of ceftolozane/tazobactam; negative differences are in favor of meropenem. Participants with missing culture and clinical responses that were failure, indeterminate, or missing were counted as presumed failures. CI confidence interval, CV-SOFA cardiovascular SOFA component score, R-SOFA respiratory SOFA component score, SOFA Sequential Organ Failure Assessment, TOC test-of-cure
Mortality and clinical cure rates were comparable across treatment arms in the higher SOFA component score (Additional file 1: Fig. S2) and SOFA groups (Additional file 1: Fig. S3) in the ITT population, with higher mortality rates observed in the R-SOFA 4, CV-SOFA ≥ 3, CV-SOFA 4, and SOFA > 6 groups, and clinical cure rates ranging between approximately 50% to 60% in all SOFA component score and SOFA groups. Microbiologic eradication/presumed eradication rates were similar across treatment arms in the SOFA analysis in the mITT population (Additional file 1: Fig. S3).
Discussion
Our subset analysis in critically ill participants with vHABP/VABP from the ASPECT-NP trial found that 28-day all-cause mortality and clinical cure rates at the TOC visit were comparable between ceftolozane/tazobactam and meropenem regardless of R-SOFA ≥ 2, CV-SOFA ≥ 2, or R-SOFA ≥ 2 plus CV-SOFA ≥ 2. The 28-day all-cause mortality rates in both treatment arms relative to the overall ITT population in the ASPECT-NP trial [24.0% (87/362) and 25.3% (92/364), respectively] [20] were, as expected, worse in participants with CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2. However, the 95% CI for the differences in mortality rates between the treatment arms included zero in all SOFA groups analyzed. Across all three SOFA groups, clinical cure rates in both treatment arms remained unchanged and aligned with the rates in ASPECT-NP [54.4% (197/362) and 53.3% (194/364), respectively] [20]. Time to death did not differ between ceftolozane/tazobactam and meropenem in participants with R-SOFA ≥ 2, CV-SOFA ≥ 2, or R-SOFA ≥ 2 plus CV-SOFA ≥ 2.
No difference was seen between ceftolozane/tazobactam and meropenem in microbiologic response rate in the mITT population with R-SOFA ≥ 2. A higher rate of microbiologic eradication/presumed eradication, driven by documented microbiologic eradication, was observed with ceftolozane/tazobactam in participants with CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2. This could be related to the optimized ceftolozane/tazobactam dose of 3 g every 8 h infused over 1 h, which has been shown to provide mean ELF penetration ratios of 0.5 and 0.6 for each component, respectively, in mechanically ventilated adults with pneumonia [17]. This may have increased the probability of reaching target ELF exposures with ceftolozane/tazobactam. Meropenem produced lower mean ELF penetration ratios in a similar population, even with higher doses and prolonged infusion times [27]. Although it has been suggested that higher doses of meropenem may be beneficial in this patient population [28], the MIC90 was 1 mg/L for P. aeruginosa and < 0.064 mg/L for Enterobacterales in the CV-SOFA ≥ 2 group. In addition, efficacy outcomes in meropenem-treated participants with augmented renal clearance at baseline were comparable to those with normal renal function in Shorr et al. [29]. Altogether this suggests the meropenem dose was adequate; however, given the complex PK in critically ill patients, we cannot confirm whether the meropenem dose or infusion time influenced the microbiologic eradication rates observed in this analysis.
A strength of this study is that the ASPECT-NP trial enrolled exclusively ventilated participants, all of whom were critically ill, with a vast majority admitted to the ICU. This is reflected by the high prevalence of severe respiratory failure or shock in this subset analysis. SOFA scores were collected prospectively from all participants in the ASPECT-NP trial. This provided a large, randomized sample of participants with vHABP/VABP and elevated SOFA component scores for our analysis. The baseline LRT pathogens identified in the participants were representative of the pathogens associated with nosocomial pneumonia. Moreover, outcomes in participants with higher SOFA component scores, which included participants with PaO2/FiO2 < 200 mmHg or vasopressor-requiring shock, aligned with those observed for R- and CV-SOFA ≥ 2. For example, the observed mortality rates with CV-SOFA ≥ 3 (ceftolozane/tazobactam 35.1%, meropenem 30.4%) were similar to the rates with CV-SOFA ≥ 2 (ceftolozane/tazobactam 33.3%, meropenem 30.3%).
One limitation of this study is that we used individual components of the SOFA score to define the presence of severe respiratory failure (as a baseline R-SOFA ≥ 2) and the presence of shock (as a baseline CV-SOFA ≥ 2). Although the SOFA score is a well-validated scoring system to evaluate the degree of organ dysfunction in critically ill patients [30] and individual organ system components of the score predict mortality [31], individual organ system component scores are not routinely used as unique scores to measure respiratory or cardiovascular dysfunction. The results of the SOFA analysis generally supported the outcomes of the individual SOFA component score analyses. Mortality rates were higher with SOFA > 6 (ceftolozane/tazobactam 31.6%, meropenem 29.9%) as compared to SOFA ≤ 6 and corresponded with the morality rates observed with CV-SOFA ≥ 2 (ceftolozane/tazobactam 33.3%, meropenem 30.3%). Clinical cure rates remained within the 50% to 60% range as in the SOFA component score analyses. However, no differences were identified between treatment arms for microbiologic eradication/presumed eradication based on SOFA, unlike the observations based on CV-SOFA ≥ 2 and R-SOFA ≥ 2 plus CV-SOFA ≥ 2. The results of this study cannot be applied to critically ill patients who are immunocompromised, have received an organ or stem cell transplant, have blood dyscrasias, or have cystic fibrosis, as they were excluded from the ASPECT-NP trial; yet these may be co-morbidities in patients with nosocomial pneumonia [32,33,34]. Lastly, the comparisons between outcomes were not powered for non-inferiority testing or controlled for multiplicity. Given the small sample sizes in some of the subsets, the corresponding results must be interpreted with caution.
In summary, ceftolozane/tazobactam was an effective treatment for vHABP/VABP in adults with organ failure, regardless of degree of severity of illness. Greater severity of illness did not affect the relative efficacy of ceftolozane/tazobactam versus meropenem and either agent is an appropriate option for the treatment of vHABP/VABP caused by susceptible Gram-negative pathogens.
Availability of data and materials
The data sharing policy, including restrictions, of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA (MSD) is available at http://engagezone.msd.com/ds_documentation.php. Requests for access to the study data can be submitted through the EngageZone site or via email to dataaccess@merck.com.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CE:
-
Clinically evaluable
- CFU:
-
Colony-forming units
- CI:
-
Confidence intervals
- CLCR :
-
Creatinine clearance
- CPIS:
-
Clinical pulmonary infection score
- CV-SOFA:
-
Cardiovascular SOFA component score
- ELF:
-
Epithelial lining fluid
- EOT:
-
End-of-therapy
- ESBL+:
-
Extended-spectrum β-lactamase producing
- h:
-
Hour
- ICU:
-
Intensive care unit
- ITT:
-
Intention-to-treat
- IV:
-
Intravenously
- LRT:
-
Lower respiratory tract
- MDR:
-
Multidrug-resistant
- mITT:
-
Microbiologic intention-to-treat
- MV:
-
Mechanical ventilation
- nvHABP:
-
Non-ventilated hospital-acquired pneumonia
- PD:
-
Pharmacodynamics
- PK:
-
Pharmacokinetics
- q8h:
-
Every 8 h
- R-SOFA:
-
Respiratory SOFA component score
- SOFA:
-
Sequential Organ Failure Assessment
- TOC:
-
Test-of-cure
- VABP:
-
Ventilator-associated bacterial pneumonia
- vHABP:
-
Ventilated hospital-acquired pneumonia
References
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018;23(46):1800516.
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, et al. Changes in prevalence of health care-associated infections in US hospitals. N Engl J Med. 2018;379(18):1732–44.
Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370(13):1198–208.
Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21(8):510–5.
Koulenti D, Tsigou E, Rello J. Nosocomial pneumonia in 27 ICUs in Europe: perspectives from the EU-VAP/CAP study. Eur J Clin Microbiol Infect Dis. 2017;36(11):1999–2006.
Esperatti M, Ferrer M, Theessen A, Liapikou A, Valencia M, Saucedo LM, et al. Nosocomial pneumonia in the intensive care unit acquired by mechanically ventilated versus nonventilated patients. Am J Respir Crit Care Med. 2010;182(12):1533–9.
Costa RD, Baptista JP, Freitas R, Martins PJ. Hospital-acquired pneumonia in a multipurpose intensive care unit: one-year prospective study. Acta Med Port. 2019;32(12):746–53.
Talbot GH, Das A, Cush S, Dane A, Wible M, Echols R, et al. Evidence-based study design for hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. J Infect Dis. 2019;219:1536–44.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111.
Torres A, Niederman MS, Chastre J, Ewig S, Fernandez-Vandellos P, Hanberger H, et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociacion Latinoamericana del Torax (ALAT). Eur Respir J. 2017;50(3):1700582.
Zaragoza R, Vidal-Cortés P, Aguilar G, Borges M, Diaz E, Ferrer R, et al. Update of the treatment of nosocomial pneumonia in the ICU. Crit Care. 2020;24(1):383.
Luna CM, Aruj P, Niederman MS, Garzon J, Violi D, Prignoni A, et al. Appropriateness and delay to initiate therapy in ventilator-associated pneumonia. Eur Respir J. 2006;27(1):158–64.
American Thoracic Society & Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Juan C, Zamorano L, Perez JL, Ge Y, Oliver A, Spanish Group for the Study of Pseudomonas et al. Activity of a new antipseudomonal cephalosporin, CXA-101 (FR264205), against carbapenem-resistant and multidrug-resistant Pseudomonas aeruginosa clinical strains. Antimicrob Agents Chemother. 2010;54(2):846–51.
Estabrook M, Bussell B, Clugston SL, Bush K. In vitro activity of ceftolozane-tazobactam as determined by broth dilution and agar diffusion assays against recent US Escherichia coli isolates from 2010 to 2011 carrying CTX-M-type extended-spectrum beta-lactamases. J Clin Microbiol. 2014;52(11):4049–52.
Farrell DJ, Sader HS, Flamm RK, Jones RN. Ceftolozane/tazobactam activity tested against Gram-negative bacterial isolates from hospitalised patients with pneumonia in US and European medical centres (2012). Int J Antimicrob Agents. 2014;43(6):533–9.
Caro L, Nicolau DP, De Waele JJ, Kuti JL, Larson KB, Gadzicki E, et al. Lung penetration, bronchopulmonary pharmacokinetic/pharmacodynamic profile and safety of 3 g of ceftolozane/tazobactam administered to ventilated, critically ill patients with pneumonia. J Antimicrob Chemother. 2020;75(6):1546–53.
Chandorkar G, Huntington JA, Gotfried MH, Rodvold KA, Umeh O. Intrapulmonary penetration of ceftolozane/tazobactam and piperacillin/tazobactam in healthy adult subjects. J Antimicrob Chemother. 2012;67(10):2463–9.
Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic-derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2016;56(1):56–66.
Kollef MH, Novacek M, Kivistik U, Rea-Neto A, Shime N, Martin-Loeches I, et al. Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2019;19(12):1299–311.
Veiga RP, Paiva JA. Pharmacokinetics-pharmacodynamics issues relevant for the clinical use of beta-lactam antibiotics in critically ill patients. Crit Care. 2018;22(1):233.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, et al. DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58(8):1072–83.
McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31(4):345–51.
Clinical and Laboratory Standards Institute. M07-A10. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Tenth Edition ed. Wayne, PA: CLSI; 2015.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Yan X, Su XG. Stratified Wilson and Newcombe confidence intervals for multiple binomial proportions. Stat Biopharm Res. 2010;2(3):329–35.
Heffernan AJ, Sime FB, Lipman J, Dhanani J, Andrews K, Ellwood D, et al. Intrapulmonary pharmacokinetics of antibiotics used to treat nosocomial pneumonia caused by Gram-negative bacilli: a systematic review. Int J Antimicrob Agents. 2019;53(3):234–45.
Frippiat F, Musuamba FT, Seidel L, Albert A, Denooz R, Charlier C, et al. Modelled target attainment after meropenem infusion in patients with severe nosocomial pneumonia: the PROMESSE study. J Antimicrob Chemother. 2015;70(1):207–16.
Shorr AF, Bruno CJ, Zhang Z, Jensen E, Gao W, Feng HP, et al. Ceftolozane/tazobactam probability of target attainment and outcomes in participants with augmented renal clearance from the randomized phase 3 ASPECT-NP trial. Crit Care. 2021;25(1):354.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
Timsit JF, Fosse JP, Troche G, De Lassence A, Alberti C, Garrouste-Orgeas M, et al. Calibration and discrimination by daily Logistic Organ Dysfunction scoring comparatively with daily Sequential Organ Failure Assessment scoring for predicting hospital mortality in critically ill patients. Crit Care Med. 2002;30(9):2003–13.
Reynolds D, Kollef M. The epidemiology and pathogenesis and treatment of Pseudomonas aeruginosa infections: an update. Drugs. 2021;81(18):2117–31.
Gudiol C, Sabe N, Carratala J. Is hospital-acquired pneumonia different in transplant recipients? Clin Microbiol Infect. 2019;25(10):1186–94.
Wong JL, Evans SE. Bacterial pneumonia in patients with cancer: novel risk factors and management. Clin Chest Med. 2017;38(2):263–77.
Acknowledgements
The authors thank the patients and their families and caregivers for participating in this study, along with all investigators and site personnel. They also thank Dorothy McCoy, PharmD, BCPS, BCIDP, for medical writing assistance, Dominik J. Wolf, MSc, for his insightful comments during the development of the manuscript, and Michele McColgan, BA, for editorial assistance; all are employees of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Funding
This work was supported by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. Employees of the funder, and several of the co-authors, were involved in the design, data collection, data analysis, data interpretation, and reporting of the research.
Author information
Authors and Affiliations
Contributions
IM-L, AFS, RGW, MHK, J-FT, BY, JAH, EJ, and CJB contributed to drafting the manuscript and critically revised it for important intellectual content. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ASPECT-NP study was conducted in accordance with the principles of Good Clinical Practice (GCP) as set forth in the International Conference on Harmonisation guidelines on GCP (ICH E6) and was approved by the institutional review boards at each participating center and regulatory agencies at each participating country. Informed consent was received from all participants (or legally acceptable representatives).
Consent for publication
Not applicable.
Competing interests
IM-L has received consulting fees and honoraria from MSD and Pfizer. AFS has received medical writing support, consulting fees, and honoraria from MSD; consulting fees from Pfizer and Shionogi; honoraria from Pfizer, Shionogi, and La Jolla. RGW is a consultant to, has received medical writing support from, and has participated in advisory committees for MSD; has received an investigator-initiated grant from Calcimedica; has participated in advisory committees for Shionogi and La Jolla; has received honoraria from BioMerieux for industry workshops at ATS, APSR, and SCCM; and has participated in the Clinical Evaluation Committee for Pfizer. MHK is supported by Barnes-Jewish Hospital Foundation and has received consulting fees and honoraria from MSD, Pfizer, and Shionogi. J-FT participated on an advisory board for MSD, Pfizer, and Shionogi on treatment of HAP/VAP; has received research grants, consulting fees, honoraria, and travel support from MSD; was past chairman of the ESCMID Study Group for Infections in Critically Ill Patients—ESGCIP; and is the principal investigator of BICCS (national research program (RCT BICCS PHRC 18-0316) on the benefit of Continuous infusion and combination therapy on the treatment of severe Gram-negative infections, including pneumonia. JAH, EJ, and CJB, and BY are current or former employees of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, who may own stock and/or hold stock options in Merck & Co., Inc., Rahway, NJ USA.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Fig. S1
: Clinical cure at TOC by SOFA component score group (CE population). Fig. S2: Mortality (upper panel A) and clinical cure at TOC (bottom panel B) by SOFA component score ≥ 3 and 4 (ITT population). Fig. S3: Outcomes by SOFA ≤ 6 and > 6.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martin-Loeches, I., Shorr, A.F., Wunderink, R.G. et al. Outcomes in participants with ventilated nosocomial pneumonia and organ failure treated with ceftolozane/tazobactam versus meropenem: a subset analysis of the phase 3, randomized, controlled ASPECT-NP trial. Ann. Intensive Care 13, 8 (2023). https://doi.org/10.1186/s13613-022-01084-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01084-8