Abstract
Introduction
Hospital-acquired and ventilator-associated bacterial pneumonia (HABP and VABP) are associated with significant healthcare resource utilization (HCRU). This a priori, exploratory, secondary analysis from the ASPECT-NP clinical trial evaluated resource utilization among patients with ventilated HABP (vHABP)/VABP treated with ceftolozane/tazobactam or meropenem.
Methods
This analysis used data from the randomized, double-blind, noninferiority phase 3 ASPECT-NP trial of patients with vHABP/VABP randomized to receive ceftolozane/tazobactam 3 g (ceftolozane 2 g/tazobactam 1 g) or meropenem 1 g for 8–14 days. Day 28 outcomes included hospital length of stay (LOS), intensive care unit (ICU) LOS, and time to mechanical ventilation extubation in the microbiological intention-to-treat (mITT) population and in an HCRU population. The HCRU population, a subset of patients from the mITT population that were alive at day 28, was used to remove resource use bias influenced by mortality rates.
Results
Ceftolozane/tazobactam-treated versus meropenem-treated patients, respectively, had fewer deaths (20.1% vs. 25.5%), fewer hospital discharges (30.7% vs. 32.4%), and higher ICU discharges (60.0% vs. 58.3%) and extubations (51.9% vs. 48.2%) by day 28. In the HCRU population, adjusted LOS differences (95% confidence intervals) for ceftolozane/tazobactam compared with meropenem were 0.1 (− 1.4 to 1.6) hospitalization days, − 1.4 (− 2.9 to 0.2) ICU days, and − 0.9 (− 2.4 to 0.7) mechanical ventilation days. Patterns were similar among the VABP and Pseudomonas aeruginosa subgroups.
Conclusion
Similar 28-day resource utilization outcomes were observed between ceftolozane/tazobactam and meropenem in the mITT population of patients from ASPECT-NP with vHABP/VABP due to gram-negative pathogens. ASPECT-NP was not powered to detect differences in resource utilization outcomes between treatment groups; however, numerical differences in ICU LOS and duration of mechanical ventilation were noted. Further study is needed to assess resource utilization in the real-world practice setting, especially among patients excluded from ASPECT-NP, including those with resistant P. aeruginosa infections.
Trial Registrations
ClinicalTrials.gov: NCT02070757, registered February 25, 2014; EudraCT: 2012-002862-11.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features
This article is published with digital features to facilitate understanding of the article. To view the digital features for this article go to https://doi.org/10.6084/m9.figshare.12938396.
Key Summary Points
Why carry out this study? |
Hospital-acquired and ventilator-associated bacterial pneumonia (HABP and VABP) are associated with significant healthcare resource utilization. |
In this exploratory secondary analysis of the ASPECT-NP noninferiority registration trial, we hypothesized that participants treated with ceftolozane/tazobactam or meropenem would have similar resource utilization. |
What was learned from the study? |
Similar 28-day HCRU outcomes were observed between ceftolozane/tazobactam and meropenem in the microbiological intention-to-treat (mITT) population of participants with ventilated HABP (vHABP) or VABP due to gram-negative pathogens. |
Although ASPECT-NP was a noninferiority study and not powered to detect differences in outcomes between treatment groups, there were numerical differences in resource utilization outcomes, specifically for intensive care unit (ICU) hospital length of stay (LOS) and duration of mechanical ventilation. |
If a reduction of these costly resources (ICU days and mechanical ventilation) can be realized in a real-world setting, the use of ceftolozane/tazobactam could potentially minimize the economic burden associated with the management of patients with VABP or vHABP due to gram-negative pathogens. Further evaluations of resource utilization especially in key subpopulations are needed. |
Introduction
Hospital-acquired bacterial pneumonia (HABP) and ventilator-associated bacterial pneumonia (VABP) are infections of the lower respiratory tract that occur after at least 48 h of hospitalization or mechanical ventilation, respectively [1]. Although regional variation exists, Pseudomonas aeruginosa is the leading gram-negative pathogen responsible for HABP/VABP in the USA, Europe, and Latin America, followed by Enterobacterales (mainly Escherichia coli and Klebsiella spp.) [2,3,4]. HABP and VABP are both associated with significant healthcare resource utilization (HCRU), morbidity, and mortality [5, 6]. The attributable mortality of nosocomial pneumonia is high, with rates ranging from 20% to 55% [1, 7,8,9,10]. A US national database study evaluated the economic burden, as measured by median hospitalization cost and hospital length of stay (LOS), for patients with community-acquired pneumonia, healthcare-associated pneumonia, HABP, and VABP. The highest median cost ($64,639; interquartile range [IQR], $36,979–$108,391) and longest median LOS (21 days; IQR, 13–33 days) were among patients with VABP, followed by patients with HABP at a median cost of $27,422 (IQR, $15,075–$52,469) and a median LOS of 14 days (IQR, 9–22 days). These hospital-acquired infections have a greater economic burden compared with patients with healthcare-associated pneumonia, at a median cost of $16,505 (IQR, $8706–$32,681) and a median LOS of 9 days (IQR, 6–15 days), and community-acquired pneumonia, with the lowest cost at $11,440 (IQR, $6345–$23,352) and the shortest LOS of 7 days (IQR, 5–12 days). This hierarchical economic burden remained even after adjusting for age and disease severity [11].
The burden of HABP/VABP is further complicated by the increased ubiquity of antibacterial-resistant pathogens [12]. Bacterial susceptibility to available first-line empiric treatments has diminished over time [13]. Patients with serious infections due to antibacterial-resistant pathogens have considerably worse outcomes relative to their susceptible counterparts [14]. In a US national database study, patients with multidrug-resistant P. aeruginosa respiratory infections had higher mortality, an approximately 7-day longer LOS, $20,000 excess costs, higher readmission rates, and more than $10,000 excess net loss per case for the hospital relative to those with non-multidrug-resistant P. aeruginosa infections [15]. Infections caused by antibacterial-resistant pathogens also increase the likelihood that a patient will not receive a microbiologically active antibacterial agent for several days after infection onset [16,17,18], further exacerbating the deleterious outcomes observed among patients with antibacterial-resistant infections [19].
Ceftolozane/tazobactam is a novel combination of ceftolozane, a potent antipseudomonal cephalosporin, and tazobactam, a β-lactamase inhibitor [20,21,22]. Ceftolozane/tazobactam has demonstrated in vitro activity against many pathogens that cause nosocomial pneumonia, including multidrug-resistant P. aeruginosa and extended-spectrum β-lactamase-producing Enterobacterales [23], and was recently approved by the US Food and Drug Administration and European Medicines Agency for the treatment of adult patients with HABP and VABP due to gram-negative pathogens [22]. These approvals were based on the randomized, controlled, double-blind, phase 3 noninferiority ASPECT-NP (nosocomial pneumonia) trial, conducted at 263 hospitals in 34 countries, that established the efficacy and safety of ceftolozane/tazobactam 3 g (ceftolozane 2 g/tazobactam 1 g) relative to meropenem 1 g for patients with VABP or ventilated HABP (vHABP). In ASPECT-NP, day 28 all-cause mortality (primary endpoint) and clinical response at the test-of-cure visit (key secondary efficacy endpoint) were similar between treatment groups, and noninferiority was demonstrated for both endpoints [24].
While these endpoints provide critical information on the safety and efficacy of ceftolozane/tazobactam, it is also crucial to evaluate the impact of new treatment modalities on the quality and efficiency of healthcare delivery. The emphasis on efficiency is also congruent with antibacterial stewardship efforts in the hospital setting, which seek to improve patient outcomes, reduce the development of antimicrobial resistance, and minimize unnecessary costs without negatively impacting quality of care [25]. Given the increased focus on value and efficiency of care across healthcare systems worldwide, an a priori secondary exploratory analysis was included in the ASPECT-NP protocol to evaluate the differences in hospital LOS, intensive care unit (ICU) LOS, and duration of mechanical ventilation between patients treated with ceftolozane/tazobactam or meropenem. Although this study was not powered to detect differences between treatment groups, we anticipated that patients treated with ceftolozane/tazobactam or meropenem would have similar resource utilization in this secondary exploratory analysis due to the ASPECT-NP study meeting its noninferiority endpoint.
Methods
Study Design
This a priori, secondary, exploratory resource utilization analysis was based on data from the randomized, double-blind, noninferiority phase 3 ASPECT-NP trial of patients at least 18 years of age with VABP or vHABP. Details on inclusion and exclusion criteria of the randomized controlled trial are described elsewhere [24] and listed in the supplemental material. Patients were randomized to receive ceftolozane/tazobactam 3 g (ceftolozane 2 g and tazobactam 1 g) or meropenem 1 g via 1-h intravenous infusion every 8 h for 8–14 days. Treatment duration was at the investigator’s discretion, although a minimum of 14 days of therapy was recommended for patients with P. aeruginosa infection. Patients were stratified by the study design into VABP or vHABP groups. The VABP group required the addition of at least 48 h of mechanical ventilation and either acute changes in ventilator support to enhance oxygenation or the presence of hypoxemia before the infection. The vHABP group required hospitalization for at least 48 h (or previous discharge within the past 7 days) and had at least one of the following criteria within 24 h before intubation or within 48 h after intubation: worsening cough, tachypnea, dyspnea, respiratory rate greater than 30 breaths per minute, and/or hypoxemia [24]. The ASPECT-NP study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the appropriate institutional review boards and regulatory agencies. All patients or legally acceptable representatives provided informed consent.
Resource Utilization Outcomes
Resource utilization metrics analyzed in this study were the proportion of patients that were discharged from the hospital, discharged from the ICU, or extubated within 28 days of randomization, along with hospital/ICU LOS and duration of mechanical ventilation. Resource utilization duration was measured as the number of days between the date of randomization and either the date of resource utilization termination (i.e., hospital discharge, ICU discharge among patients in the ICU at baseline, and extubation) or the date of truncation (death or day 28, whichever came first). Although there were patients who exceeded a 28-day stay within the trial, the 28-day endpoint was chosen to align with the trial’s primary and secondary efficacy endpoints and because follow-up beyond 28 days was variable.
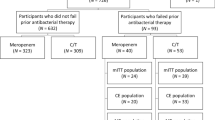
Analysis Populations
This analysis included two study populations: the microbiological intention-to-treat (mITT) population and the HCRU population. The mITT population included patients who received any amount of study drug and had at least one bacterial respiratory pathogen (excluding Staphylococcus aureus) isolated from the baseline lower respiratory tract culture that was susceptible to at least one of the study drugs. The mITT population (n = 511) was a subset of the intention-to-treat population (n = 726) and was chosen as the main analysis population to assess resource utilization because it required receipt of the study drugs and a pathogen against which the study drugs were active. The HCRU population was a subset of the mITT population and comprised patients who were alive at day 28 and achieved the outcome of interest by day 28 (i.e., hospital discharge, ICU discharge among patients in the ICU at baseline, and extubation). The HCRU population was created to mitigate the influence of death on resource utilization. The high mortality rate seen in vHABP and VABP can bias the true effect of resource utilization because patients who die tend to have a much shorter LOS relative to those who do not. Because the HCRU population is dependent on outcome of interest, the sample size varies by outcome. For example, the HCRU population for hospital discharge is less than one-third of the mITT population.
Statistical Analysis
We report the numbers and percentages of patient characteristics, the proportion of patients that achieved each outcome of interest (i.e., hospital discharge, ICU discharge among patients in the ICU at baseline, and extubation) by day 28 after enrollment, and the duration of resource utilization including number of patients, arithmetic mean, and standard deviation (SD). To address possible imbalances in characteristics of discharged/extubated patients in the two groups, we used the generalized linear model (GLM) to calculate adjusted differences in LOS. The GLM is a preferred statistical method for LOS analyses where skewness and truncation are often present [26,27,28]. We used the GLMs with log-link function and tested three residual distributions, namely gamma, negative binomial, and Poisson. The selection between the residual distributions was made by analyzing the scale parameter to determine the presence of overdispersion [29]. In the total 24 GLM regressions, overdispersion (i.e., scale parameter > 1.0) was detected in 20 regressions, suggesting that the negative binomial was the most appropriate distribution specification. Covariates in the GLMs included age (< 65 vs. ≥ 65 years), sex, baseline Acute Physiology and Chronic Health Evaluation II score (< 20 or ≥ 20), baseline pathogen type (P. aeruginosa vs. Enterobacterales), infection type (polymicrobial vs. monomicrobial), pneumonia type (vHABP vs. VABP), country of treatment, prior antibacterial failure, bacteremia, comorbidities (diabetes, congestive heart failure, chronic obstructive pulmonary disease, emphysema, and pleural effusion), and log-transformed pre-randomization resource utilization duration of the corresponding resource type (e.g., for ICU LOS, pre-randomization ICU stay was used). Selection of covariates was based on clinical meaningfulness and relevancy. We did not implement any variable selection procedure based on predictive power, which is often used for outcome prediction but not for effect estimation. The average LOS difference attributable to treatment was calculated as the difference in least-squares means between the two treatment groups. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA), primarily PROC GENMOD and LIFETEST functions.
Results
A total of 726 patients were enrolled and randomly assigned to ceftolozane/tazobactam (n = 362) or meropenem (n = 364). The mITT population comprised 264 patients treated with ceftolozane/tazobactam and 247 treated with meropenem. Baseline and clinical characteristics of the mITT population were comparable between both treatment groups (Table 1). However, more patients who received ceftolozane/tazobactam had prior antibacterial therapy failure (ceftolozane/tazobactam, n = 39/264 [14.8%]; meropenem, n = 24/247 [9.7%]) and bacteremia (ceftolozane/tazobactam, n = 43/264 [16.3%]; meropenem, n = 26/247 [10.5%]) at baseline. In the mITT population, the mean (SD) duration of hospitalization before randomization was 12.0 (60.4) days in the ceftolozane/tazobactam group versus 7.0 (7.0) days in the meropenem group. Mean (SD) duration of mechanical ventilation before randomization was 11.2 (26.4) days for patients treated with ceftolozane/tazobactam versus 9.8 (7.6) days for those treated with meropenem. Clinical cure was observed in 193 (73.1%) ceftolozane/tazobactam-treated patients and 168 (68.0%) meropenem-treated patients in the mITT population.
Table 2 reports 28-day mortality and hospital/ICU discharge and mechanical ventilation extubation rates among the mITT population. Mortality within 28 days occurred in 53 (20.1%) of 264 ceftolozane/tazobactam-treated patients and 63 (25.5%) of 247 meropenem-treated patients. Within 28 days, 81 (30.7%) of 264 ceftolozane/tazobactam-treated patients and 80 (32.4%) of 247 meropenem-treated patients were discharged from the hospital, 153 (60.0%) of 255 ceftolozane/tazobactam-treated patients and 140 (58.3%) of 240 meropenem-treated patients were discharged from the ICU, and 137 (51.9%) of 264 ceftolozane/tazobactam-treated patients and 119 (48.2%) of 247 meropenem-treated patients were extubated.
Resource utilization durations for hospitalization, ICU stay, and mechanical ventilation are shown in Table 3. In the mITT population, the patient characteristic-adjusted LOS differences (95% confidence interval [CI]) for ceftolozane/tazobactam compared with meropenem were 1.1 (− 0.4 to 2.7) hospitalization days, − 0.6 (− 2.3 to 1.0) ICU days, and − 0.6 (− 2.1 to 0.9) mechanical ventilation days. Of note, mortality (ceftolozane/tazobactam, 20.1%; meropenem, 25.1%) had an influence on the duration of resource utilization in the mITT population, as deceased patients had, on average, a 4-day reduction in hospital LOS and a 2-day reduction in ICU LOS and time spent on mechanical ventilation. Within the HCRU population in which the influence of mortality was removed, adjusted LOS differences (95% CIs) for ceftolozane/tazobactam compared with meropenem were 0.1 (− 1.4 to 1.6) hospitalization days (n = 161), − 1.4 (− 2.9 to 0.2) ICU days (n = 284), and − 0.9 (− 2.4 to 0.7) mechanical ventilation days (n = 269).
Duration of resource utilization was further analyzed by subgroups of interest (Table 4). In general, the subgroup of patients with VABP and P. aeruginosa within the mITT population showed some numerical reductions in all three types of resource utilization for ceftolozane/tazobactam compared with meropenem. Similar results were also observed in the HCRU subgroups in which patients were alive and achieved the outcome of interest by day 28. More specifically, in the HCRU population among patients with VABP, the adjusted LOS differences (95% CIs) for ceftolozane/tazobactam compared with meropenem were − 1.1 (− 2.6 to 0.6) hospitalization days, − 1.5 (− 3.1 to 0.3) ICU days, and − 1.3 (− 3.0 to 0.8) mechanical ventilation days; the corresponding metrics for patients with infections due to P. aeruginosa were − 2.1 (− 5.1 to 1.8) days, − 3.0 (− 5.3 to − 0.2) days, and − 4.5 (− 8.1 to 0.7) days for duration of hospitalization, ICU stay, and mechanical ventilation, respectively. However, in the vHABP subgroup within the HCRU population, differences were in a reverse direction for hospitalization days (adjusted LOS difference, 5.7 [95% CI − 0.4 to 13.6] days) and mechanical ventilation (adjusted ventilation difference, 0.4 [95% CI − 1.5 to 3.1] days) but similar for ICU stay (adjusted ICU LOS, − 1.3 [95% CI − 4.8 to 3.1] days).
Discussion
Phase 3 international, multicenter, randomized, double-blind, comparative noninferiority clinical trials are the current gold standard for establishing the efficacy and safety profiles of new antibacterial agents for the treatment of HABP/VABP. Although efficacy and safety are established in such a design setting for the purposes of regulatory approval, it is challenging to infer meaningful economic or comparative effectiveness. The consideration of economic endpoints and the magnitude of these differences is key to making value judgments [30]. Given the increased focus on value and efficiency of care across healthcare systems worldwide, an a priori, secondary, exploratory analysis was included in the ASPECT-NP protocol to evaluate the differences in hospital LOS, ICU LOS, and duration of mechanical ventilation between patients treated with ceftolozane/tazobactam or meropenem. Overall, similar 28-day resource utilization outcomes were observed between ceftolozane/tazobactam and meropenem in the mITT population of patients from ASPECT-NP with vHABP/VABP due to gram-negative pathogens. Although ASPECT-NP was a noninferiority study and not powered to detect differences in outcomes between treatment groups, several numerical differences in resource utilization outcomes were noted between groups, and most favored ceftolozane/tazobactam relative to meropenem. In conjunction with the clinical efficacy and safety data shown in the randomized trial, these results support the overall value of ceftolozane/tazobactam for the treatment of patients with vHABP and VABP [24].
Despite numerical differences in key outcomes, including duration of ICU and mechanical ventilation use, most results were nonsignificant, reflected in most 95% CIs including the null value. This could be related to several facets of the trial design. First and foremost, the trial was not adequately powered for these resource utilization endpoints. Further, the inclusion criteria required that patients have a susceptible infection. Since meropenem has been shown to be an effective agent for patients with susceptible HABP/VABP, the benefit of ceftolozane/tazobactam among patients with antibacterial-resistant infections, such as meropenem-resistant or multidrug-resistant P. aeruginosa, could not be assessed in this study. In addition, the average hospital LOS before infection was 12 days for ceftolozane/tazobactam-treated patients compared with 7 days for meropenem-treated patients. Previous hospitalization and the patient’s underlying condition could also influence subsequent outcomes that are not attributable to treatment or the infection. As an international study, variable local clinical practice and healthcare reimbursement policies may influence duration of ICU and hospital stay for study participants that could lead to unmeasurable bias. Lastly, like most phase 3 trials, ASPECT-NP had fixed therapy duration requirements, lacked oral stepdown therapy, and lacked predefined criteria for hospital discharge, which could also impact overall ICU and hospital stay.
Although the resource utilization measures were constrained by study design limitations, time to extubation is an important effectiveness metric for clinicians treating patients with VABP and vHABP. Mechanical ventilation is one of the primary drivers of resource utilization for patients with VABP and vHABP. There are considerable efforts, irrespective of healthcare system or country, exerted to minimize patients’ time spent on mechanical ventilation due to long-term complications and healthcare costs. Although no definitive conclusions can be drawn from these data, the observed differences in extubation between treatment groups highlight the need for additional real-world comparative effectiveness and quality assurance initiatives between ceftolozane/tazobactam and meropenem. Furthermore, the results of this study highlight the need for further resource utilization assessment in high-risk patient populations (i.e., patients with VABP, infections due to P. aeruginosa and resistant pathogens) as they represented the groups with the largest numerical differences in resource utilization treatment outcomes.
This study is not without limitations. First, this study only evaluated a portion of the patient’s experience during their hospitalization, specifically from the time of randomization to day 28. Although the 28-day window is consistent with the primary endpoints of the randomized clinical trial, some patients continued to accrue resources past 28 days. Moreover, there were differences in prior resource utilization before randomization. Resource utilization before infection may impact a patient’s future resource utilization after infection that is not necessarily attributed to the infection.
Secondly, challenges exist with resource utilization studies, particularly when there is a high underlying mortality rate. In this analysis, patients who died did not have the opportunity for discharge or extubation, which violates an assumption of future occurrence. Patients who died during this study had, on average, a 4-day reduction in hospital LOS and a 2-day reduction in ICU LOS and time spent on mechanical ventilation. As these data suggest, most patients who die consume less resources, which can underestimate the burden of mortality on resource utilization, especially for conditions that generally have high mortality levels. There are multiple methods described in the literature to account for the deleterious effects of mortality in a resource utilization study. In this study, we analyzed those patients who were alive at day 28 to minimize the impact of mortality on resource utilization [31]. Furthermore, these patients had significant underlying issues independent of the infection that could have also impacted resource utilization duration. Overall hospitalization was the most similar endpoint between the two treatment groups in this study and had the largest truncation due to the 28-day window. However, the 28-day observation period represents a reasonable time from infection to account for resource utilization associated with the acute event of the infection as opposed to other underlying reasons for hospitalization.
Conclusions
Similar 28-day resource utilization outcomes were observed between ceftolozane/tazobactam and meropenem in the mITT and HCRU populations, a subset of patients included within ASPECT-NP that had vHABP/VABP due to gram-negative pathogens. Although ASPECT-NP was a noninferiority study and not powered to detect differences in outcomes between treatment groups, several numerical differences in resource utilization outcomes were noted between treatment groups, particularly with respect to ICU LOS and duration of mechanical ventilation. If a reduction for these costly resources (ICU days and mechanical ventilation use) can be realized in a real-world setting, the use of ceftolozane/tazobactam could potentially minimize the economic burden associated with the management of patients with VABP or vHABP due to gram-negative pathogens. In addition, from both the hospital and patient perspective, decreased hospital LOS minimizes the transmission of resistant pathogens and reduces the need for additional treatment regimens. Resource utilization measures and the sequential benefits of reduced hospital exposure are important considerations in determining the overall value of novel antibacterial agents and are included in the principles of antimicrobial stewardship.
References
Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111.
Jones RN. Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clin Infect Dis. 2010;51(suppl 1):S81–7.
Sader HS, Castanheira M, Flamm RK. Antimicrobial activity of ceftazidime-avibactam against gram-negative bacteria isolated from patients hospitalized with pneumonia in US medical centers, 2011 to 2015. Antimicrob Agents Chemother. 2017;61(4):e02083-16.
Weiner LM, Webb AK, Limbago B, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(11):1288–301.
Frantzeskaki F, Orfanos SE. Treating nosocomial pneumonia: what’s new. ERJ Open Res. 2018;4(2):00058–2018.
Niederman MS. Hospital-acquired pneumonia, health care-associated pneumonia, ventilator-associated pneumonia, and ventilator-associated tracheobronchitis: definitions and challenges in trial design. Clin Infect Dis. 2010;51(suppl 1):S12–7.
Ibn Saied W, Mourvillier B, Cohen Y, et al. A comparison of the mortality risk associated with ventilator-acquired bacterial pneumonia and nonventilator ICU-acquired bacterial pneumonia. Crit Care Med. 2019;47(3):345–52.
Kollef MH, Hamilton CW, Ernst FR. Economic impact of ventilator-associated pneumonia in a large matched cohort. Infect Control Hosp Epidemiol. 2012;33(3):250–6.
Micek ST, Kollef MH, Torres A, et al. Pseudomonas aeruginosa nosocomial pneumonia: impact of pneumonia classification. Infect Control Hosp Epidemiol. 2015;36(10):1190–7.
Muscedere JG, Day A, Heyland DK. Mortality, attributable mortality, and clinical events as end points for clinical trials of ventilator-associated pneumonia and hospital-acquired pneumonia. Clin Infect Dis. 2010;51(suppl 1):S120–5.
Sun D, Moorthy V, Chang S-C, et al. Economic burden of ventilator-associated, hospital-acquired, healthcare-associated and community-acquired pneumonia in the hospital setting [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):1494.
O’Neill J. Antimicrobial resistance: tackling a crisis for the health and wealth of nations. Review on Antimicrobial Resistance. 2014;20:1–16. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf. Accessed 7 Apr 2020
Infectious Diseases Society of America, Spellberg B, Blaser M, et al. Combating antimicrobial resistance: policy recommendations to save lives. Clin Infect Dis. 2011;52(suppl 5):S397–428.
Martin-Loeches I, Torres A, Rinaudo M, et al. Resistance patterns and outcomes in intensive care unit (ICU)-acquired pneumonia. Validation of European Centre for Disease Prevention and Control (ECDC) and the Centers for Disease Control and Prevention (CDC) classification of multidrug resistant organisms. J Infect. 2015;70(3):213–22.
Tabak YP, Merchant S, Ye G, et al. Incremental clinical and economic burden of suspected respiratory infections due to multi-drug-resistant Pseudomonas aeruginosa in the United States. J Hosp Infect. 2019;103(2):134–41.
Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–98.
Lodise TP, Zhao Q, Fahrbach K, Gillard PJ, Martin A. A systematic review of the association between delayed appropriate therapy and mortality among patients hospitalized with infections due to Klebsiella pneumoniae or Escherichia coli: how long is too long? BMC Infect Dis. 2018;18(1):625.
Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40(4):277–83.
Bonine NG, Berger A, Altincatal A, et al. Impact of delayed appropriate antibiotic therapy on patient outcomes by antibiotic resistance status from serious gram-negative bacterial infections. Am J Med Sci. 2019;357(2):103–10.
ZERBAXA® (ceftolozane and tazobactam) for injection, for intravenous use. Prescribing information. Whitehouse Station, NJ: Merck Sharpe & Dohme Corp. 2020.
Moya B, Zamorano L, Juan C, Ge Y, Oliver A. Affinity of the new cephalosporin CXA-101 to penicillin-binding proteins of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2010;54(9):3933–7.
Zhanel GG, Chung P, Adam H, et al. Ceftolozane/tazobactam: a novel cephalosporin/β-lactamase inhibitor combination with activity against multidrug-resistant gram-negative bacilli. Drugs. 2014;74(1):31–51.
Shortridge D, Pfaller MA, Castanheira M, Flamm RK. Antimicrobial activity of ceftolozane-tazobactam tested against Enterobacteriaceae and Pseudomonas aeruginosa collected from patients with bloodstream infections isolated in United States hospitals (2013–2015) as part of the Program to Assess Ceftolozane-Tazobactam Susceptibility (PACTS) surveillance program. Diagn Microbiol Infect Dis. 2018;92(2):158–63.
Kollef MH, Nováček M, Kivistik Ü, et al. Ceftolozane–tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2019;19(12):1299–311.
Rice LB. Antimicrobial stewardship and antimicrobial resistance. Med Clin N Am. 2018;102(5):805–18.
Verburg IW, de Keizer NF, de Jonge E, Peek N. Comparison of regression methods for modeling intensive care length of stay. PLoS One. 2014;9(10):e109684.
Austin PC, Rothwell DM, Tu JV. A comparison of statistical modeling strategies for analyzing length of stay after CABG surgery. Health Serv Outcomes Res Method. 2002;3(2):107–33.
Kanzaria HK, Probst MA, Ponce NA, Hsia RY. The association between advanced diagnostic imaging and ED length of stay. Am J Emerg Med. 2014;32(10):1253–8.
Pedan A. Analysis of count data using the SAS system. In: Proceedings of the 26th Annual SAS Users Group International Conference; 2001.
Drummond M, O’Brien B. Clinical importance, statistical significance and the assessment of economic and quality-of-life outcomes. Health Econ. 1993;2(3):205–12.
Brock GN, Barnes C, Ramirez JA, Myers J. How to handle mortality when investigating length of hospital stay and time to clinical stability. BMC Med Res Methodol. 2011;11:144.
Acknowledgements
We thank the patients and their families and caregivers for participating in the ASPECT-NP trial, along with all investigators and site personnel.
Funding
Funding for this research was provided by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, New Jersey, USA (MSD). MSD provided funding for the Rapid Service Fee.
Editorial Assistance
Editorial assistance was provided by Jessica Deckman, PhD, CMPP, of The Lockwood Group, Stamford, CT, USA. This assistance was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA (MSD).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors are responsible for the work described in this paper. All authors were involved in at least one of the following: [conception, design of work or acquisition, analysis, interpretation of data] and [drafting the manuscript and/or revising/reviewing the manuscript for important intellectual content]. All authors provided final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Prior Presentation
This work was presented, in part, at the 30th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), 2020. All accepted abstracts were posted in the 2020 ECCMID abstract book.
Disclosures
Laura Puzniak, Joe Yang, and Ryan Dillon are employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA (MSD) and may own stock and/or hold stock options in Merck & Co., Inc., Kenilworth, NJ, USA. Marin Kollef reports advisory board and speaker’s bureau fees and institutional research funding from MSD. Dr Kollef is funded by the Barnes-Jewish Hospital Foundation. Thomas Lodise reports consulting and grant support from MSD.
Compliance with Ethics Guidelines
The ASPECT-NP study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the appropriate institutional review boards and regulatory agencies. All patients or legally acceptable representatives provided informed consent.
Data Availability
Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA’s data sharing policy, including restrictions, is available at http://engagezone.msd.com/ds_documentation.php. Requests for access to the clinical study data can be submitted through the EngageZone site or via email to dataaccess@merck.com.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
This article is published with digital features to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12938396.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lodise, T., Yang, J., Puzniak, L.A. et al. Healthcare Resource Utilization of Ceftolozane/Tazobactam Versus Meropenem for Ventilated Nosocomial Pneumonia from the Randomized, Controlled, Double-Blind ASPECT-NP Trial. Infect Dis Ther 9, 953–966 (2020). https://doi.org/10.1007/s40121-020-00343-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-020-00343-0