Abstract
Bone defects are among the most common damages in human medicine. Due to limitations and challenges in the area of bone healing, the research field has turned into a hot topic discipline with direct clinical outcomes. Among several available modalities, scaffold-free cell sheet technology has opened novel avenues to yield efficient osteogenesis. It is suggested that the intact matrix secreted from cells can provide a unique microenvironment for the acceleration of osteoangiogenesis. To the best of our knowledge, cell sheet technology (CST) has been investigated in terms of several skeletal defects with promising outcomes. Here, we highlighted some recent advances associated with the application of CST for the recovery of craniomaxillofacial (CMF) in various preclinical settings. The regenerative properties of both single-layer and multilayer CST were assessed regarding fabrication methods and applications. It has been indicated that different forms of cell sheets are available for CMF engineering like those used for other hard tissues. By tackling current challenges, CST is touted as an effective and alternative therapeutic option for CMF bone regeneration.
Similar content being viewed by others
Introduction
It has been accepted that tissue engineering (TE) is an interdisciplinary field to find appropriate biological substitutes for restoring injured tissues. For efficient reconstruction and mimicking functional and physical properties of tissues, TE uses three distinct elements as follows: heterogeneous stem cell population, suitable biomaterials, and varied growth factors [1, 2].
Among several stem cell types, mesenchymal stem cells (MSCs) are attractive cell sources for regenerative purposes because of their appropriate differentiation capacity and secretion of diverse soluble factors [3, 4]. MSCs are commonly isolated from different tissues such as adipose tissue, umbilical cord blood, bone marrow, and skeletal muscles. Adipose (AD-MSCs)- and bone marrow-derived MSCs (BM-MSCs) are two popular and most available cell sources for bone TE [5]. Although MSCs are a great stem cell source in the area of TE, a great plethora of studies has shown that MSCs isolated from different tissues possess variable degrees of regeneration capacity. For example, human ethmoid sinus mucosa-derived MSCs (hES-MSCs) display superior colonization properties and proliferation compared with maxillary sinus-derived MSCs [5]. In this regard, the selection of a suitable stem cell type can increase the possibility of osteogenesis and bone healing [6].
A comparison of different sources of MSCs [BM-MSCs, AD-MSCs, umbilical cord-derived MSCs (UC-MSCs)] indicated that AD-MSCs and BM-MSCs exhibit higher osteogenic potential in in vitro conditions related to UC-MSCs, while angiogenic capacity is more evident in AD-MSCs and UC-MSCs [7]. Data confirmed relatively similar osteogenic properties for these cells inside the body [7]. The existence of prominent osteogenic capacity in UC-MSCs and AM-MSCs is associated with a lower proliferation rate [8]. It should not be neglected that the occurrence of specific physiological and pathological conditions can affect the reparative properties of MSCs. For instance, the osteogenic capacity and proliferation of human and rodent BM-MSCs are reduced by aging [9, 10]. The application of MSCs in bone-related pathologies includes two main strategies. It is thought that MSCs can expedite the regeneration of injured bones via differentiation and secretion of several growth factors, and at the same time, properties like immunomodulatory, anti-inflammatory, and pro-angiogenesis activities can intensify the osteogenic capacity of MSCs [11].
CMF bone tissue supports numerous facial features such as pronunciation and mastication [12]. Compared to other appendicular bones, CMF basic discords include problems associated with endochondral and intramembranous ossification. Therefore, the same therapeutic strategies would not be suitable for both skull and long bones [13]. Usually, pathological injuries, even minor defects, related to maxillofacial bone are intricate in morphology compared with those that generally occurred in orthopedics [14].
Up to now, different strategies have been used for the regeneration and reconstruction of CMF bone injuries [15,16,17]. Cell-based therapies are at the center of attention for CMF bone regeneration [18]. Lendeckel et al. applied non-differentiated autologous AD-MSCs with fibrin glue to reconstruct calvaria with multi-fragment fractures in a seven-year-old girl. They also used polylactic acid (PLA)-based resorbable macro-porous mesh to fix the graft for three months [19].
Besides the efficacy of cells and different substrates in osteogenesis, introducing transplant cells in a specific structure can accelerate the healing procedure [20]. CST and other cellular sheets approaches are touted as scaffold-free methods containing natural extracellular matrix (ECM) but lack some problems related to the cell suspension seeding methods [21, 22]. Considering the importance of CMF regeneration and the high prevalence of CMF defects, we aimed to collect some experiments related to the application of CST in the regeneration of hard tissue, mainly in the CMF region.
CMF defects: current methods and challenges
Bone tissue is considered the most extensively compact tissue that is continuously remodeled during life by osteoclasts and osteoblast activities [10, 23]. To date, CMF bone defects remain not only a considerable challenge for health but also for restoring functional esthetic façades and arise from several etiologies and congenital acquired deformities, such as degenerative diseases [15, 23], congenital malformations [5, 23], traumas [1, 5, 24], tumor resection [5, 23], bone atrophy following a tooth extraction [14], inflammation [1], and wrong surgical proceedings [23]. These features may lead to non-healing bone defects that entail fast and on-time maxillofacial bone reconstruction [1, 5, 14, 23,24,25]. It should be noted that spontaneous calvarial re-ossification would be successful only in babies younger than two [26]. Besides, the activity of mastication-related muscles provides a high amount of strain, and stress tolerated by CMF bones can increase the complexity of pathological conditions [12]. Due to the proximity of mastication-related muscles, maintaining the functional integrity of craniofacial bone and appropriate reconstruction at a high vascularization degree is a critical challenge in bone TE [12].
Small bone defects left without treatment that could not heal over their life are termed critical size defects (CSD) [27]. Restoration of extensive bone defects is essential in maxillofacial, oral, plastic, orthopedic, and reconstructive surgery. Most challenges and difficulties in the treatment of bone defects are associated with the application of suitable biomaterials designed using specific devices to promote the bone healing procedure and fill the missing tissue [1].
The clinical methods used to reconstruct CMF bone tissue could be divided into three main categories: bone grafting, biomaterials, and cell-based therapies [28]. Each modality has its advantages and limitations. Insufficient capacity for bone regeneration does necessitate bone grafting. Autologous bone grafts are one available option for surgeons and are touted as a gold standard modality for the restoration of CMF structure. Because of the existence of difficulties with bone grafting, researchers have focused on the development and application of other approaches, such as cell-based therapies [14, 23, 29]. Insufficient quantity of bone stock, variable effectiveness, immune reactions, accessibility, the possibility of infections, and morbidity are the main considerable limitations related to autologous and allogenic bone grafts [1, 28, 30, 31].
TE is an alternative approach for generating bone-like transplants to reduce or eliminate the demands for bone tissue grafting from a patient's secondary site [23, 32,33,34]. In autologous bone grafting, accessibility, mobility of donors on harvesting sites, unnecessary surgery, and anesthetic times are problematic issues [5, 29]. In the TE area, both allogeneic and xenogeneic materials have been commonly used for the acceleration of bone regeneration [2]. Limitations such as inaccessibility, infection probability, stableness, immunological reaction, storage, and unexpected quantity of graft resorption remained the most problematic issues in the application of biomaterials [15, 35].
During the past decades, various substrates such as ceramics, metal alloys and meshes (titanium mesh), demineralized matrix pastes, different polymers, porous hydroxyapatite (HA) materials, and cell-based approaches have been used as artificial grafts. Lack of osteoinductive features, problems related to the prosthetic material/bone interface, immunogenic clinical response, and removal of adjacent bone is prominent current limitations in the application of artificial materials [35, 36]. Recent approaches are based on the application of decellularized ECM to mimic the native bone ECM for efficient regeneration [37]. Along with various biomaterials, numerous phytocompounds like Danshen, Ge Gan, and Cissus quadrangularis extracts have been applied to improve hard tissue regeneration [38, 39]. Biomimetic scaffolds or implants are alternative options for CMF bone reconstruction [12]. However, incomplete biodegradation rate, prominent immunological response, lack of appropriate vascularization [12], foreign body reaction, chronic sinus mucosa swelling, fragmentation, infection [40], displacement of implant, epidural hematoma, and cerebrospinal fluid leak [41] have been reported in terms of biomimetic scaffold application.
Scaffold-free CST
Several research teams have promoted the regeneration of bony tissues using the cellular sheet [42, 43]. As an innovative method, CST could recreate a biological microenvironment similar, not completely but in part, to a target site [1, 5]. In this approach, cultured cells can be picked as integrated sheets without using normal proteolytic enzymes while cell-to-cell junctions are maintained (Fig. 1) [1]. Studies have proved the deposited ECM in the basal surface of the cell sheet compartment [1, 44].
Schematic illustration of MSC sheet formation. The isolated MSCs from different sources are cultured for certain periods (please see Table 1). Cells generate single-layer or multilayer composite with intact ECM (sheet). MSC sheets can be harvested using several techniques such as electro-, thermo-, pH-, photo-responsive systems, mechanical force, and enzymatic treatment (Designed by office 2019)
Along with the disadvantages of biomimetic scaffolds inside the body, cell sheets may be a suitable regenerative approach with very low immune responses that can dictate in vivo-like phenotype for transplant cells with suitable angiogenesis [12]. Blood nourishment is a vital element for living tissues and bone remodeling procedures [45]. Compared to the cell suspension strategy, CST can notably lead to better cell retention, higher microvascular density, and juxtacrine interaction between the transplant and host cells within the interface area [37, 46]. Consequently, CST offers various considerable advantages and can circumvent several previous issues related to scaffolds. Cell sheets are routinely harvested by several methods, such as the application of thermo-responsive substrates at the bottom of cell culture dishes [44, 47], and the detachment of a single cell layer using mechanical forces (scraper) or light irradiation [14, 48]. Therefore, different responsive systems for cell sheet harvesting, such as electro-, thermo-, pH-, and photo-responsive systems, have been developed until now [49]. When cells are detached by enzymatic solutions such as trypsin or collagenase, considerable cell damage is possible, resulting in a low survival rate [50].
As mentioned above, mechanical retrieval and thermo-responsive plates beyond polymers are two primary methods for collecting cell sheets [10]. Data indicated intact underlying ECM, high-rate cell viability, and tissue-like behaviors in recovered cell sheets using these approaches. Besides, maintaining cell-to-cell and cell-to-ECM interaction can provide essential signaling pathways required for proper cell bioactivity. Immunohistochemical studies have confirmed the presence of ECM components such as fibronectin, laminin, and cell junction β-catenin in the sheet cell layer, which are essential for cell attachment and functionality [51]. It is believed that cells within the sheet structure can appropriately sense mechanical signals. Compared to a 3D culture system using scaffolds, CST benefits from several advantages [52]. The distributions of growth factors are acceptable, and most cells can be stimulated in a coordinated manner [52]. The activity of surface receptors such as glucose transporter-1, Na+/K+-ATPase, sodium–glucose-linked transporter-1, neutral endopeptidase, dipeptidyl endopeptidase IV, and aquaporin-1 are normal [53]. It is believed that the integrated ECM under the cell sheets could act as a natural tissue adhesive substrate and eliminate the necessity for suture, allowing sheets to attach rapidly to the tissue's target site without invasive manipulations [50,51,52,53]. All these events can occur using the intact ECM on the basal surface cell sheets [54]. Commensurate with these descriptions, the preservation of ECM in CS helps the transplant cells to regulate homeostasis, proliferation, and migration and provides crucial clues for mechanical support during the transplantation [5, 55, 56].
In the context of bone tissue structure, cell sheets can be used as periosteum [57]. Application of MSC sheets with supportive ECM circumvents disadvantages of cell-based therapies, such as lack of appropriate migration and leaking of transplant cells after injection into the injured sites [10, 52, 57].
The addition of distinct supplements, such as ascorbic acid, promotes the synthesis and secretion of ECM components and prevents the progression of age-related changes in cells within the sheet structure [44, 58, 59]. Akahane and colleagues declared that the exposure of cells to dexamethasone (Dex) and ascorbic acid affects the expression of specific genes associated with ECM construction and sheet formation [60]. Later studies on the role of Dex and ascorbic acid on BM-MSCs indicated that both factors allow the harvesting of cultured cells in a single cell layer by improving the mechanical integrity after induction of proteoglycan and type I collagen synthesis. Preparation and/or induction of integrated substrate synthesis can increase cell number, which seems a practical approach in complex tissue reconstruction like osteonecrosis, nonunion, and union bone defects [61]. By the stimulation of type I collagen, laminin, and fibronectin synthesis, ascorbic acid promotes the osteogenic differentiation of cultured cells [61, 62]. Likewise, the expression of stemness genes such as OCT-4, Sox-2, and TERT was upregulated in MSC sheets after exposure to ascorbic acid [44]. Langenbach and Handschel previously indicated that Dex could induce BM-MSC osteogenic differentiation by the expression of MKP-1 and osteocalcin (OCN) and dephosphorylation of Runx2 [61, 62]. It seems that incubation of cells in a culture medium supplemented with the combination of Dex and ascorbic acid yields efficient sheet formation culture systems compared to that from Dex or ascorbic acid alone [61]. In addition to certain components and stimulatory factors, the application of ECM components can trigger the formation of a cell sheet. For instance, gelatin enhances cell proliferation and upregulates the expression of the bone morphogenetic protein (BMP)-7 in the differentiated sheets [63]. It is touted that the existence of a specific tripeptide motif (arginine–glycine–aspartic acid) in the backbone of gelatin improves cell adhesion properties [63, 64].
According to previous studies, the roles of cell sheets in bone engineering containing exogenous constructs can be summarized below: (i) acting as cell carriers; (ii) restricting the progression of fibrous connective tissues in the osteogenic microenvironment; and (iii) developing periosteal and endochondral osteogenesis [50, 65, 66]. Up to now, several cells such as AD-MSCs, BM-MSCs, periodontal ligament-derived cells, dental follicle cells, and gingival margin-derived cells have been applied for sheet formation, and data confirmed their restorative properties in bone, corneal epithelium, periodontal, and myocardial tissue [5, 67]. Compared to single-cell sheet treatment, multilayer MSC sheets yielded better osteochondrogenic capacities. The culture of MSCs on stacked sheets composed of methyl cellulose and poly(N-isopropyl acrylamide) [MC and PNIPAAm] increased the expression of BMP-2, alkaline phosphatase (ALP), OCN, and VEGF at tendon–bone interface (TBI) [68]. For obtaining better regenerative outcomes, Berntsen et al. used stacked tenogenic and osteogenic hAD-MSC sheets. Juxtaposed tenogenic and osteogenic hAD-MSC sheets with an integrated multilayer construct increase simultaneously several biomarkers associated with tendon, mineralized fibrocartilage, and bone tissue. Data indicated a spatial gradient of RUNX2 expression. In the osteogenic sheet, the expression of OCN and osterix were increased coinciding with the transcription of tenomodulin and scleraxis at the tenogenic cell sheet. Of note, endochondral ossification was evident in the engineered interface which is indicated by Indian Hedgehog and Type X collagen [69]. Simultaneous application of BM-MSC sheet with an acellular structure is another strategic approach to achieve triple biomimetic TBI.
However, varied cell types can affect the behavior of the final cell sheet structure. Recently, Nakao et al. have investigated differences between MSC sheets produced using various cell sources like AD-MSCs, BM-MSCs, and human umbilical cord MSCs (hUC-MSCs) [70]. Based on data, adhesion, and migration of MSCs were similar. However, some differences were found regarding cytokine secretion and proliferation capacity. On the surface of thermo-responsive cell culture dishes, BM-MSCs exhibited lower adhesion compared to AD-MSCs and UC-MSCs. Forty-eight hours after seeding, the number of AD-MSCs and UC-MSCs was higher than BM-MSCs. However, BM-MSCs showed the most potent generation rate. As a correlate, the selection of a suitable MSC source with prominent cytokine secretion capacity is integral to the successful transplantation process [70].
Akahane et al. investigated the relationship between donor age and the osteogenic potential of osteogenic matrix cell sheets (OMCS). They found a similar level of osteogenesis capacity and bone formation in both old and young donor cells, indicating the fact that OMCS can be considered an efficient method in bone healing even in aged patients [10]. Emerging data have indicated that cell sheets can improve the paracrine activity of MSCs after placing at the site of injury [71]. It was indicated that the secretion of exosomes via mouse BM-MSCs sheet promoted neural stem cell differentiation, axonal regeneration, and synaptogenesis in a mouse model of spinal cord injury [71]. These data show that cell sheets can improve the regenerative properties of MSCs via the induction of differentiation and paracrine activity.
Cell sheet in CMF defects
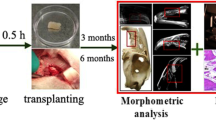
Recently, allogeneic monolayer and heterogeneous multilayer cell sheets have been developed for TE purposes. Cell sheets have been used to construct tissues such as bone, mucosa, cornea, and myocardium [50, 72,73,74]. In some studies, CST was combined with other biomaterials for bony tissue reconstruction, such as spinal cord interbody fusion [75]. Figure 2 and Table 1 show sheet-based constructs for CMF bone regeneration.
Efficacy of cell source and passage numbers
To answer whether the source of cells would be an effective regenerative outcome, Liu et al. compared the osteogenic potential of alveolar and long BM-MSC sheets in rabbits with calvarial bone defects [79]. According to the data, sheets containing alveolar BM-MSCs yielded more osteogenic outcomes with prominent mineralization and higher newly formed bone-to-total-volume ratio (BV/TV) and significant expression of osteonectin, OCN, Runx2, osteopontin (OPN), and BSP genes compared to the group received long BM-MSCs [79]. The authors suggested that the application of alveolar BM-MSC sheets would be a hopeful approach to the regeneration of CMF bone injuries in clinical settings [79]. In an experiment conducted by Xie et al., human ethmoid sinus mucosa (ES)-MSCs and rat BM-MSCs sheets in the presence of polysebacoyl diglyceride were fabricated and examined in a rat model of calvarial defects [5]. To this end, different composites [ES-MSCs‒sheet‒BM-MSCs‒polysebacoyl diglyceride, BM-MSCs–sheet–BM-MSCs‒polysebacoyl diglyceride, BM-MSCs‒polysebacoyl diglyceride, polysebacoyl diglyceride] were fabricated and transplanted into the target injury site. Based on the data, it confirmed that hES-MSCs‒sheets aligned with BM-MSC‒sebacoyl diglyceride showed maximum osteogenic properties after transplantation into the injury sites. Also, this group had higher paracrine activity to release factors such as BMP-2, BMP-4, and bFGF in in vitro conditions (Fig. 3) [5]. It should not be forgotten that the number of cell passages can affect the quality and restorative capacity of the cell sheets. Kim et al. fabricated cell sheets from hUC-MSCs at different passages (from P4 to P12) on thermo-responsive culture dishes [51]. Based on the data, the proliferation properties of MSCs were reduced upon reaching passage 9 with inadequate cell-to-cell juxtacrine interaction. It confirmed that MSCs tended to form micro-sized cell aggregates with heterogeneous morphologies by the increasing number of passages in which passage 12 MSCs lost their properties to form a confluent single cell layer.
Bright-field assessment of hESMSC sheets with different magnifications (A: a = 500 µm and b = 200 µm). The cell sheets were detached from the temperature-responsive dish at a temperature below 20 °C (B panel a) and lifted using forceps (B panel b). H & E staining revealed the existence of 4–5 cell layers with an average thickness of 100–150 µm (C; scale bar = 200 µm). The ultrastructural analysis confirmed that compact cells are embedded in dense ECM (D: panel a = 50 µm; panel b = 20 µm). Copyright with permission [5], 2015, Biomaterials
Implantation of the cell sheet
Fragmented cell sheet
Sheet pieces are eligible to initiate bone generation at different time points, with a higher peak load compared to integrated cell sheet transplantation. Related outcomes represented a considerable increment in bony junction using fragments of the BM-MSC sheet [52].
Multilayer cell sheet
It has been shown that triple-layer BM-MSC sheets could appropriately stimulate local surface bone growth [84]. Data obtained indicated that autologous pig mandibular BM-MSC sheets could increase bone growth at the mandibular symphyseal surface [84].
Cell sheet and biomaterials
The combination of CST with certain biomaterials can increase the regenerative potential of transplant cells [1, 5]. The presence of nanofibers meshes composed of poly-L-lactide (PLLA) and gelatin (PLLA/gelatin), not only improved and induced osteogenic differentiation of BM-MSCs but also remarkably enhanced new calcified bone formation [77]. Cell sheets in combination with PRF (platelet‑rich fibrin granules) and nano‑HA [1], poly(lactide-co-glycolide)/HA (PLGA/HA) scaffold [81], PLGA [53], beta-tricalcium phosphate (β-TCP) [59], and β-TCP/collagen-I [88] could be more effective in the regeneration of calvarial bone defects. It is postulated that the combination of a cell sheet with a 3D scaffold structure can yield more regenerative outcomes [53]. To this end, Du and co-workers cultured human BM-MSCs within the biodegradable β-TCP scaffolds and wrapped them simultaneously with BM-MSC sheets. This strategy reduces unwanted adipogenic and chondrogenic differentiation of cultured cells and increases osteogenic potential [89].
Cell sheet and biological agents
It has been indicated that interferon (IFN)-γ stimulates immuno-suppressive properties of MSCs by the regulation of the indoleamine 2, 3-dioxygenase (IDO) enzyme [56, 90]. Studying the effect of IFN-γ on hBM-MSC sheets showed that the upregulation of IDO leads to HLA-DR expression and T cell inhibition in grafted regions, resulting in the induction of mice calvarial bone regeneration. It is thought that IDO can diminish the host immune response, thus inducing bone tissue regeneration in the mouse model [56]. The combination of the BM-MSC sheet and PRF increased the healing of the critical size calvarial bone injury in rabbits [82]. Also, local injection of the Semaphorin 3A (Sema3A) with AD-MSC sheet and Bio-Oss® bone granules increased the osteogenic outcomes. This strategy seems to be an exciting approach for osseous healing in rats with type 2 diabetes mellitus [80]. Kaibuchi and co-workers proved the efficacy of AD-MSC sheets in the healing of mandibular wounds in beagle dogs caused by Dex and zoledronate. Following the operation, many bacterial colonies and multi-nuclear Cathepsin K-positive cells were detached from the surfaces of the jaw bone on the control side, while a complete healing process in the mucosal wounds was achieved in all dogs that received MSC sheets [11].
MSC sheet and angiogenesis
Among several important factors involved in bone healing, angiogenesis, and vascularization have critical roles [15, 91]. Efficient bone TE and regeneration require rapid neovascularization into the grafts [76]. Without tissue vascularization, the implants will not develop bone-forming units or lose their function over time [92]. Supplementation of pro-angiogenic factors, co-culture approaches, microsurgical techniques, and optimizing the scaffold structure are some ways to stimulate angiogenesis [93,94,95,96,97]. MSC secretome encompasses several angiogenic factors such as interleukin (IL)-6, FGF-2, VEGF, monocyte chemoattractant protein-1, and angiopoietin-1 [1]. It has been shown that hypoxic AD-MSCs could induce the growth of blood vessels by concurrent secretion of anti-apoptotic and angiogenic factors, like VEGF [98,99,100,101]. Thus, AD-MSCs have the potential to affect both osteogenic and angiogenesis (osteoangigoenesis) in sheet form [24, 102, 103]. The angiocrine and anti-apoptotic factors released by BM-MSC could regulate endogenous cell migration [81]. In BMP-2-mediated bone tissue regeneration, the paracrine activity of osteoprogenitors is considered a great modulator of neovascularization as well [99, 100, 104, 105].
The angiogenesis potential of MSC sheets has been highlighted in different tissues, such as the skin and heart [42]. It was suggested that MSC sheets produce significantly higher VEGF levels compared to MSC suspension after being placed at the site of injury or ischemia [57, 68, 106, 107]. The release of specific factors such as HGF and VEGF stabilizes newly formed blood vessels following the differentiation of MSCs. Of note, a fraction of MSCs within the sheets acquires a pericyte-like phenotype (Fig. 4) [86]. Therefore, one can hypothesize that the release of angiocrine by MSCs is an important factor in the acceleration healing process in the early days [51]. Based on the data, the simultaneous application of materials with engineered cell sheets (MSC sheet implants) can simultaneously increase vascularization and osteogenic abilities [108]. In this regard, Nakano and colleagues differentiated developed rat BM-MSC sheets in the presence of osteogenic medium and placed the cells within the cylindrical shaped β-TCP scaffolds [109]. It was indicated that both vascular units and bone-forming units were seen at the center of β-TCP construct two weeks after transplantation into the rats, leading to improved new bone generation [109]. Molecular investigations revealed the expression of ALP, BMP-2, OCN, and VEGF-A. It is thought that the concurrent release of VEGF with osteogenesis factors like OCN and ALP around the fracture sites after transplantation of cell sheets can help with new bone formation and remodeling [110]. Similarly, Kim et al. confirmed angiogenesis, capillary formation, and newly generated blood vessels between host tissue and hUC-MSC sheets 10 days after implantation. They showed continuous and appropriate secretion of human HGF for ten days while in the absence of hUC-MSC sheets (MSC suspension), only a few tiny blood vessels are generated (Fig. 5) [51]. Likewise, nascent vascular units have been approved around MSC sheets in different animal models. In a study, allogenic GFP-tagged rat BM-MSC sheets were transplanted into rats with osteonecrosis of the jaw [86]. Immunofluorescence staining revealed that these cells can juxtapose to the periphery of vessels and exhibit pericyte marker CD146, indicating the active participation of transplanted MSCs in the arteriogenesis process [86]. To be specific, the differentiation of MSCs toward pericytes can stabilize the structure of newly generated vascular units [111]. Multiple cell transplantation is an interesting strategy to increase the angiogenic potential of stem cells. Using an MSC, endothelial cell, and CD146 pericyte co-culture system on PIPAAm thermo-responsive surfaces, Mendes et al. improved the osteoangiogenic capacity of fabricated MSC sheets [112]. They showed that endothelial cells and CD146 pericytes migrated successfully to the MSC layer and several vascular anastomoses with the production of type I collagen and osteocalcin [112]. In some studies, cell sheets have been used along with biodegradable scaffolds to stimulate vascularization. Kang and co-workers used β-TCP-covered biomimetic periosteum cell sheets for bone tissue regeneration [113]. The biomimetic periosteum was effective in osteogenesis and vascularization due to an appropriate spatial configuration. By incorporating a vascular bed or collagen micro-channels into stacked sheets of cells, the medium could be filled into the sheets to build new capillaries inside the perfusion bioreactor [92, 114, 115]. It should be noted that it is necessary to use appropriate doses of components to avoid the development of excessive blood vessel formation that could lead to pathological diseases such as vascular malformations [116], atherosclerosis, and proliferative retinopathy [24, 116].
Possible restorative properties of MSC sheets in rats with BRONJ disease. Like MSC differentiation properties, the paracrine activity of MSCs within the sheet structure is an important factor to accelerate osteogenesis. It is believed that simultaneous activation of angiogenesis and osteogenesis by MSC sheet is critical to yield better regenerative outcomes. The release of VEGF and HGF promotes angiogenesis while RANKL secretion can orient the osteoclast precursor cells into osteoclasts and improves bone remodeling in rats with BRONJ disease (Designed by Photoshop version CS6)
Xenogeneic transplantation of human umbilical cord MSC (hUC-MSC) sheets to immuno-deficient mice (a–g). H & E staining indicates the formation of numerous vascular units in mice that received xenogeneic hUC-MSC sheets (b and c) compared to the control group (a). The transplantation area is indicated with local vascularization (d). Immunofluorescence images confirmed that hUC-MSC sheets produce HGF on days 1 and 10 after being transplanted into the target sites within the cutaneous tissue (f and g). Black arrows = transplanted hUC-MSC sheet; blue arrows = blood vessels. Scale bars in panels a and b = 100 µm; scale bars in panels c, f and g = 50 µm; scale bars in panels d and e = 0.5 cm. Copyright with permission [51] 2019, Scientific reports
Immune response and cell sheet
Undoubtedly, the infiltration of various immune cells like Th1, Th2, Th17, and macrophages into the grafts is essential for tissue regeneration or wound healing [79]. Up to now, the immune-suppressive impact of MSCs is well proved in several reports. MSCs can secrete specific bioactive molecules that could avert unpleasant immune reactions and support the healing of damaged tissues [1]. Modulatory potential and anti-inflammatory effects of MSCs occur mainly via paracrine mechanisms [5]. It is shown that MSCs can exhibit anti-inflammatory effects in many diseases via the regulation of macrophage activity [87, 117]. As reported in several animal and clinical studies, spontaneous tissue healing might lead to difficulties, such as fibrosis and inflammation. Minimizing these responses could be possible using graft materials.
In most circumstances, treatment using allogeneic MSCs is considered due to the local immuno-suppressive activities of MSCs, where using autologous cells is restricted or even impossible [1]. A limitation of allogeneic cell therapy involves immunological properties and variable efficiency in patients due to cell transfer strategies. Therefore, researchers have tried to develop novel allogeneic cell sheets using hUC-MSCs with low antigenicity. Compared to several types of MSCs, such as BM-MSC and AD-MSC sheets, the UC-MSC sheets barely express MHC II antigens related to all immune rejection (Table 2). hUC-MSC sheets could be grafted immediately within 10 min of placement into the subcutaneous tissue in immune-deficient mice. The secretion of TNF-α from hUC-MSC sheets at passage 4 was notably lower than those of sheets at passages 6, 8, 10, and 12. Together, the passage number of cells is an important factor in immunomodulatory capacities [51, 70]. It has been indicated that cytokines such as IL-6, IL-10, TGF-β1, and PGE2 are associated with the anti-inflammatory properties of MSCs [118]. TGF-β1 can down-regulate the inflammatory reactions by damping macrophage movement and release of pro-inflammatory cytokines [119]. TGF-β1 exerts pleiotropic influences on processes including cell proliferation, migration, differentiation, and death [120]. Also, this factor can eliminate T-cell activity in response to exogenous antigens [121], suggesting that the levels of TGF-β1 may influence the survival of grafted MSCs. It was found that the production of PGE2 was moderately high in UC-MSCs and BM-MSCs as compared to AD-MSCs [86]. PGE2 is involved in the anti-inflammatory response by binding to its receptors, EP1eEP4 [70, 122]. Corradetti and co-workers indicated the infiltration of neutrophils into the grafts at the beginning of 1–4 weeks accompanied by monocyte recruitment [123]. In the latter steps, this pattern was turned into anti-inflammatory cells [124].
Liu et al. reported that the immunoregulatory of alveolar BM-MSC and iliac BM-MSC sheets are similar with nonsignificant changes in the activity of Th1, M1, and M2 cells [79, 125]. Unlike this study, some authorities found that different MSC sources (BM-MSCs, AD-MSCs, and fibroblasts) within the cell sheets can exert varied anti-inflammatory properties [117]. It was indicated that AD-MSC and BM-MSC sheets stimulated the anti-inflammatory macrophage phenotype (M2) better than fibroblast sheets. Based on data, supernatants collected from AD-MSC sheets yielded higher CD206 surface markers, IL1 receptor antagonist (IL1RA), and chemokine (C–C motif) ligand 18 (CCL18) [117]. It has been shown that CD206, a mannose receptor, is upregulated in response to certain interleukins such as IL-4 and IL-13. CD206 may modulate signals induced by other receptors, such as Fc or Toll-like receptors [126]. Likewise, IL-1Ra acts as the IL-1 inhibitor by binding to the IL-1 receptor to protect tissues from inflammation-induced injuries [127].
Other possible mechanisms involved in the regenerative potential of CS
As discussed above, MSCs can commit to several cell types and promote the regeneration of tissues via different mechanisms. In addition to osteoangiogenic and immune-modulatory properties, these cells exhibit osteoinductive, neurogenic capacities via engaging paracrine mechanisms [5]. After transplantation, cell sheets not only maintain cellular function and morphology but also can help the transplanted cells to adhere to the host tissues and secret growth factors [51].
Kaibuchi et al. showed that the average number of osteoclasts was significantly higher in MSC sheets than in the control and suspended MSCs groups. Also, the secretion of receptor activator of nuclear factor ĸ-B ligand (RANKL) from MSCs could lead to the differentiation of osteoclast precursor cells to osteoclasts [86]. Xiao et al. suggested a plan to describe how ECM can regulate osteoblast differentiation [128]. They proposed that osteoblasts phenotype is acquired after the promotion of close contact between osteoblasts and collagen-bearing ECM. The reciprocal interaction between type I collagen and α2β1 integrin binds the osteoblasts to ECM components. Besides, the promotion of integrins can activate signaling pathways such as the MAPK axis. After the transduction of signals to the nucleus, specific factors such as Runx2 are activated. The concomitant expression of osteoblast marker genes such as OCN-induced osteoblast differentiation (Fig. 6) [128]. It is thought that this model could be a probable mechanism of cell sheet ECM on the host osteoblasts. In another study, it was proposed that the accumulation of extracellular signal-regulated protein kinases-p (P-ERK) occurs in the nucleus after the interaction of integrins with ECM components. Both Runx2 and P-ERK selectively bind to promoters of OCN and bone sialoprotein (BSP). Molecular investigations have revealed that two osteoblastic cis-acting elements, including OSE2a and OSE2b, exist at the proximal promoter of the OCN gene and are essential for OCN expression [129, 130]. It has been indicated that Msx2, Dlx3, and Dlx5 could positively and negatively regulate Runx2 [131]. Runx2 with Dlx3 and Dlx5 could regulate functional osteoblast HD regulatory elements including type I Collagen, OCN, OPN, and BSP [132].
Cell sheet implantation approaches and subsequent molecular responses. CS could be used as mono- or multi-cell layered form, F-CS, and Fo-CS in the site of bone injury. It is suggested that CS can be applied in combination with S, and BF. After CS transplantation, implanted cells release several factors such as RANKL with the potential to increase osteoclast precursor cells differentiation into osteoclasts. Reciprocal interaction of ECM integrin and collagen with cells leads to the activation of relevant downstream signaling pathways such as MAPK and β-catenin, resulting in OB differentiation and increased bone formation. Cell sheets: CS; fragmented form: F-CS; scaffolds: S; biological factors: BF; folded form: Fo-CS; osteoclasts: OC; osteoblasts: OB; osteocytes in lacunae: OCY; connective tissue: CT; new bone: NB; and host bone: HB (Designed by Office 2019 and Photoshop CS6)
Immunofluorescence imaging indicated that only part of the transplanted BM-MSC sheet directly differentiated into osteocytes and formed the bone matrix [133]. Labeled MSCs in the structure of cell sheets are detectable at the defect sites and in the regenerating tissues about 2 and 8 weeks after transplantation [68]. To show the probable relationship between MSC type and bone formation, Xie et al. used cellular sheets of hES-MSCs and hBM-MSCs. It was found that both MSC sheets, especially hES-MSCs, can differentiate into osteoblasts. The higher regenerative outcomes in animals that received the hES-MSC sheet are possibly due to the secretion of cytokines (Fig. 6) [5].
Limitations and potential core problems
Besides the benefits and advantages of cell sheets in bone engineering, some related limitations need further consideration [134]. For example, the period required for applied cells to form the sheet structure could be up to four weeks after cell isolation (Table 1). One strategy would be a selection of certain growth factors, appropriate initial cell density, scaffolds, and supportive matrices with specific physicochemical properties that can educate the plated MSCs to produce ECM in the least possible time. Another limiting factor is the short shelf life of cell sheet constructs. It means that at the time that sheets are formed, the patient should be in a suitable condition to receive the graft. The existence of xenobiotic materials such as serum can affect the eligibility of sheet structures in the clinical setting. Using autologous and allogeneic serum for the expansion of MSCs within the cell sheet structure can, in part, but not completely, circumvent the issues associated with the transmission of xenobiotic materials in patients. The variability of the final product is another potential problem that arises from several biological reagents during the fabrication of cell sheets, resulting in varied quality products. Developing standard GMP-grade protocols can reduce several drawbacks related to quality variation. Transporting and the distance between the laboratory and the patient hospitalization should be short. Furthermore, the final products have to be used within two or three days to avoid losing cell-to-cell connection and attachment to the wound beds [134]. For commercialization aspects, the storage, and transportation of products should be carefully addressed. Also, cell sheet manufacturing is a manual process, and the final cell sheet structurally is a very thin, skinny, and sensitive layer. Due to a lack of proper mechanical properties, cells are susceptible to damage [44, 135]. So, the cell sheet process demands an expert operator and educated surgeons to be familiar with the handling of cell sheets [134]. Cryopreservation is another issue in terms of CST. Nowadays, there are few effective methods for cell sheet cryopreservation, thawing, and administration. Regarding these obstacles, cell sheet therapy is restricted to short paths between culture facilities or demands [136].
Conclusion
Cell sheet engineering is not only limited to in vitro studies but is also used for the regeneration of several soft and hard tissues in animal models and clinical studies. Among various available techniques, the existence of a confluent cell layer, intact ECM, and secretion of several signaling biomolecules make the CST a promising therapeutic approach in CMF bone defects. The combination of CST with other modalities such as nanofibers or other substrates can yield better regenerative outcomes. Despite these descriptions, further investigations are mandatory to improve mechanical properties with a focus on vascularization potential, paracrine activity, and differentiation into the target cell types.
Availability of data and materials
Not applicable.
Abbreviations
- AD-MSCs:
-
Adipose-derived mesenchymal stem cells
- ALP:
-
Alkaline phosphatase
- β-TCP:
-
Beta-tricalcium phosphate
- BM-MSCs:
-
Bone marrow-derived mesenchymal stem cells
- BMP:
-
Bone morphogenetic protein
- BRONJ:
-
Bisphosphonate-related osteonecrosis of the jaw
- BV/TV:
-
Bone volume to total volume
- CMF:
-
Craniomaxillofacial
- CSD:
-
Critical size defect
- Dex:
-
Dexamethasone
- ECM:
-
Extracellular matrix
- FGF:
-
Fibroblast growth factor
- HA:
-
Hydroxyapatite
- hES-MSCs:
-
Human ethmoid sinus mucosa-derived MSCs
- hUC-MSCs:
-
Human umbilical cord-derived stem cells
- IDO:
-
Immuno-modulator indoleamine 2,3-dioxygenase
- IFN:
-
Interferon
- IL:
-
Interleukin
- IV:
-
Intravenous
- MSCs:
-
Mesenchymal stem cells
- OCN:
-
Osteocalcin
- OMCS:
-
Osteogenic matrix cell sheets
- TBI:
-
Tendon–bone interface
- TE:
-
Tissue engineering
- PLA:
-
Polylactic acid
- PLLA:
-
Poly-L-lactide
- PLGA:
-
Polylactide-co-glycolide
- PRF:
-
Platelet‑rich fibrin granules
- UC-MSCs:
-
Umbilical cord-derived stem cells
- VEGF:
-
Vascular endothelial growth factor
References
Wang X, Li G, Guo J, Yang L, Liu Y, Sun Q, Li R, Yu W. Hybrid composites of mesenchymal stem cell sheets, hydroxyapatite, and platelet-rich fibrin granules for bone regeneration in a rabbit calvarial critical-size defect model. Exp Ther Med. 2017;13(5):1891–9. https://doi.org/10.3892/etm.2017.4199.
Saghati S, Nasrabadi HT, Khoshfetrat AB, Moharamzadeh K, Hassani A, Mohammadi SM, Rahbarghazi R, Fathi Karkan S. Tissue engineering strategies to increase osteochondral regeneration of stem cells; a close look at different modalities. Stem Cell Rev Rep. 2021;17(4):1294–311.
Nassiri SM, Rahbarghazi R. Interactions of mesenchymal stem cells with endothelial cells. Stem Cells Dev. 2014;23(4):319–32.
Rahbarghazi R, Nassiri SM, Ahmadi SH, Mohammadi E, Rabbani S, Araghi A, Hosseinkhani H. Dynamic induction of pro-angiogenic milieu after transplantation of marrow-derived mesenchymal stem cells in experimental myocardial infarction. Int J Cardiol. 2014;173(3):453–66.
Xie Q, Wang Z, Huang Y, Bi X, Zhou H, Lin M, Yu Z, Wang Y, Ni N, Sun J. Characterization of human ethmoid sinus mucosa derived mesenchymal stem cells (hESMSCs) and the application of hESMSCs cell sheets in bone regeneration. Biomaterials. 2015;66:67–82. https://doi.org/10.1016/j.biomaterials.2015.07.013.
Midha S, Jain KG, Bhaskar N, Kaur A, Rawat S, Giri S, Basu B, Mohanty S. Tissue-specific mesenchymal stem cell-dependent osteogenesis in highly porous chitosan-based bone analogs. Stem Cells Transl Med. 2021;10(2):303–19. https://doi.org/10.1002/sctm.19-0385.
Kang B-J, Ryu H-H, Park SS, Koyama Y, Kikuchi M, Woo H-M, Kim WH, Kweon O-K. Comparing the osteogenic potential of canine mesenchymal stem cells derived from adipose tissues, bone marrow, umbilical cord blood, and Wharton’s jelly for treating bone defects. J Vet Sci. 2012;13(3):299–310.
Shen C, Yang C, Xu S, Zhao H. Comparison of osteogenic differentiation capacity in mesenchymal stem cells derived from human amniotic membrane (AM), umbilical cord (UC), chorionic membrane (CM), and decidua (DC). Cell Biosci. 2019;9(1):1–11.
Stolzing A, Jones E, Mcgonagle D, Scutt A. Age-related changes in human bone marrow-derived mesenchymal stem cells: consequences for cell therapies. Mech Ageing Dev. 2008;129(3):163–73.
Akahane M, Shimizu T, Inagaki Y, Kira T, Egawa T, Okuda A, Onishi T, Imamura T, Tanaka Y. Implantation of bone marrow stromal cell sheets derived from old donors supports bone tissue formation. Tissue Eng Regen Med. 2018;15(1):89–100. https://doi.org/10.1007/s13770-017-0088-4.
Kaibuchi N, Iwata T, Onizuka S, Yano K, Tsumanuma Y, Yamato M, Okano T, Ando T. Allogeneic multipotent mesenchymal stromal cell sheet transplantation promotes healthy healing of wounds caused by zoledronate and dexamethasone in canine mandibular bones. Regen Therapy. 2019;10:77–83. https://doi.org/10.1016/j.reth.2018.10.008.
Tian T, Zhang T, Lin Y, Cai X. Vascularization in craniofacial bone tissue engineering. J Dent Res. 2018;97(9):969–76. https://doi.org/10.1177/0022034518767120.
Wang D, Gilbert JR, Zhang X, Zhao B, Ker DFE, Cooper GM. Calvarial versus long bone: implications for tailoring skeletal tissue engineering. Tissue Eng Part B Rev. 2020;26(1):46–63. https://doi.org/10.1089/ten.teb.2018.0353.
Ueyama Y, Yagyuu T, Maeda M, Imada M, Akahane M, Kawate K, Tanaka Y, Kirita T. Maxillofacial bone regeneration with osteogenic matrix cell sheets: an experimental study in rats. Arch Oral Biol. 2016;72:138–45. https://doi.org/10.1016/j.archoralbio.2016.08.017.
Szpalski C, Barr J, Wetterau M, Saadeh PB, Warren SM. Cranial bone defects: current and future strategies. Neurosurg Focus. 2010;29(6):E8.
Crist TE, Mathew PJ, Plotsker EL, Sevilla AC, Thaller SR. Biomaterials in craniomaxillofacial reconstruction: past, present, and future. J Craniofacial Surg. 2021;32(2):535–40.
Lopez CD, Witek L, Torroni A, Flores RL, Demissie DB, Young S, Cronstein BN, Coelho PG. The role of 3D printing in treating craniomaxillofacial congenital anomalies. Birth Defects Res. 2018;110(13):1055–64.
Oliver JD, Madhoun W, Graham EM, Hendrycks R, Renouard M, Hu MS. Stem cells regenerating the craniofacial skeleton: current state-of-the-art and future directions. J Clin Med. 2020;9(10):3307.
Lendeckel S, Jödicke A, Christophis P, Heidinger K, Wolff J, Fraser JK, Hedrick MH, Berthold L, Howaldt H-P. Autologous stem cells (adipose) and fibrin glue used to treat widespread traumatic calvarial defects: case report. J Craniomaxillofac Surg. 2004;32(6):370–3. https://doi.org/10.1016/j.jcms.2004.06.002.
Iwata T, Washio K, Yoshida T, Ishikawa I, Ando T, Yamato M, Okano T. Cell sheet engineering and its application for periodontal regeneration. J Tissue Eng Regen Med. 2015;9(4):343–56.
Li M, Ma J, Gao Y, Yang L. Cell sheet technology: a promising strategy in regenerative medicine. Cytotherapy. 2019;21(1):3–16. https://doi.org/10.1016/j.jcyt.2018.10.013.
Iwasaki K, Washio K, Meinzer W, Tsumanuma Y, Yano K, Ishikawa I. Application of cell-sheet engineering for new formation of cementum around dental implants. Heliyon. 2019;5(6):e01991. https://doi.org/10.1016/j.heliyon.2019.e01991.
Kawecki F, Clafshenkel WP, Fortin M, Auger FA, Fradette J. Biomimetic tissue-engineered bone substitutes for maxillofacial and craniofacial repair: the potential of cell sheet technologies. Adv Healthc Mater. 2018;7(6):1700919. https://doi.org/10.1002/adhm.201700919.
Wang Z, Han L, Sun T, Wang W, Li X, Wu B. Osteogenic and angiogenic lineage differentiated adipose-derived stem cells for bone regeneration of calvarial defects in rabbits. J Biomed Mater Res A. 2021;109(4):538–50. https://doi.org/10.1002/jbm.a.37036.
Lin H, Sohn J, Shen H, Langhans MT, Tuan RS. Bone marrow mesenchymal stem cells: aging and tissue engineering applications to enhance bone healing. Biomaterials. 2019;203:96–110. https://doi.org/10.1016/j.biomaterials.2018.06.026.
Fong KD, Warren SM, Loboa EG, Henderson JH, Fang TD, Cowan CM, Carter DR, Longaker MT. Mechanical strain affects dura mater biological processes: implications for immature calvarial healing. Plast Reconstr Surg. 2003;112(5):1312–27. https://doi.org/10.1097/01.PRS.0000079860.14734.D6.
Ma D, Ren L, Chen F, Liu Y, Zhang J, Xue Z, Mao T. Reconstruction of rabbit critical-size calvarial defects using autologous bone marrow stromal cell sheets. Ann Plast Surg. 2010;65(2):259–65. https://doi.org/10.1097/SAP.0b013e3181c9c3f5.
Falguera Uceda MI, Sánchez-Casanova S, Escudero-Duch C, Vilaboa N. A narrative review of cell-based approaches for cranial bone regeneration. Pharmaceutics. 2022;14(1):132. https://doi.org/10.3390/pharmaceutics14010132.
Sándor GK, Numminen J, Wolff J, Thesleff T, Miettinen A, Tuovinen VJ, Mannerström B, Patrikoski M, Seppänen R, Miettinen S. Adipose stem cells used to reconstruct 13 cases with cranio-maxillofacial hard-tissue defects. Stem Cells Transl Med. 2014;3(4):530–40. https://doi.org/10.5966/sctm.2013-0173.
Ghaffarinovin Z, Soltaninia O, Mortazavi Y, Esmaeilzadeh A, Nadri S. Repair of rat cranial bone defect by using amniotic fluid-derived mesenchymal stem cells in polycaprolactone fibrous scaffolds and platelet-rich plasma. BioImpacts BI. 2021;11(3):209. https://doi.org/10.34172/bi.2021.28.
Rezaei H, Shahrezaee M, Monfared MJ, Karkan SF, Ghafelehbashi R. Simvastatin-loaded graphene oxide embedded in polycaprolactone-polyurethane nanofibers for bone tissue engineering applications. J Polym Eng. 2021;41(5):375–86.
Hassani A, Khoshfetrat AB, Rahbarghazi R, Sakai S. Collagen and nano-hydroxyapatite interactions in alginate-based microcapsule provide an appropriate osteogenic microenvironment for modular bone tissue formation. Carbohyd Polym. 2022;277:118807.
Hassani A, Avci ÇB, Kerdar SN, Amini H, Amini M, Ahmadi M, Sakai S, Bagca BG, Ozates NP, Rahbarghazi R. Interaction of alginate with nano-hydroxyapatite-collagen using strontium provides suitable osteogenic platform. J Nanobiotechnol. 2022;20(1):1–22.
Saghati S, Rahbarghazi R, Baradar Khoshfetrat A, Moharamzadeh K, Tayefi Nasrabadi H, Roshangar L. Phenolated alginate-collagen hydrogel induced chondrogenic capacity of human amniotic mesenchymal stem cells. J Biomater Appl. 2021;36(5):789–802.
Shi J, Sun J, Zhang W, Liang H, Shi Q, Li X, Chen Y, Zhuang Y, Dai J. Demineralized bone matrix scaffolds modified by CBD-SDF-1α promote bone regeneration via recruiting endogenous stem cells. ACS Appl Mater Interfaces. 2016;8(41):27511–22. https://doi.org/10.1021/acsami.6b08685.
Jensen SS, Broggini N, Weibrich G, Hjôrting-Hansen E, Schenk R, Buser D. Bone regeneration in standardized bone defects with autografts or bone substitutes in combination with platelet concentrate: a histologic and histomorphometric study in the mandibles of minipigs. Int J Oral Maxillofac Implants. 2005;20(5).
Shang F, Yu Y, Liu S, Ming L, Zhang Y, Zhou Z, Zhao J, Jin Y. Advancing application of mesenchymal stem cell-based bone tissue regeneration. Bioact Mater. 2021;6(3):666–83. https://doi.org/10.1016/j.bioactmat.2020.08.014.
Lee D-H, Kim I-K, Cho H-Y, Seo J-H, Jang J-M, Kim J. Effect of herbal extracts on bone regeneration in a rat calvaria defect model and screening system. J Korean Assoc Oral Maxillofac Surg. 2018;44(2):79–85. https://doi.org/10.5125/jkaoms.2018.44.2.79.
Kashte S, Dhumal R, Chaudhary P, Sharma R, Dighe V, Kadam S. Bone regeneration in critical-size calvarial defect using functional biocompatible osteoinductive herbal scaffolds and human umbilical cord Wharton’s Jelly-derived mesenchymal stem cells. Mater Today Commun. 2021;26:102049. https://doi.org/10.1016/j.mtcomm.2021.102049.
Pourdanesh F, Latifi N, Latifi F. Complications after craniofacial reconstruction with calcium phosphate cements: a case report and review of the literature. J Korean Assoc Oral Maxillofac Surg. 2018;44(5):207–11. https://doi.org/10.5125/jkaoms.2018.44.5.207.
Shay T, Mitchell K-A, Belzberg M, Zelko I, Mahapatra S, Qian J, Mendoza L, Huang J, Brem H, Gordon C. Translucent customized cranial implants made of clear polymethylmethacrylate: an early outcome analysis of 55 consecutive cranioplasty cases. Ann Plast Surg. 2020;85(6):e27–36. https://doi.org/10.1097/SAP.0000000000002441.
Chen M, Xu Y, Zhang T, Ma Y, Liu J, Yuan B, Chen X, Zhou P, Zhao X, Pang F. Mesenchymal stem cell sheets: a new cell-based strategy for bone repair and regeneration. Biotech Lett. 2019;41(3):305–18.
Weng Y, Wang Z, Sun J, Han L, Li X, Wu B, Dong Q. Engineering of axially vascularized bone tissue using natural coral scaffold and osteogenic bone marrow mesenchymal stem cell sheets. J Stomatol Oral Maxillofac Surg. 2021;122(4):397–404.
Shotorbani BB, André H, Barzegar A, Zarghami N, Salehi R, Alizadeh E. Cell sheet biofabrication by co-administration of mesenchymal stem cells secretome and vitamin C on thermoresponsive polymer. J Mater Sci Mater Med. 2018;29(11):1–17. https://doi.org/10.1007/s10856-018-6180-z.
Hu M, Dailamy A, Lei XY, Parekh U, McDonald D, Kumar A, Mali P. Facile engineering of long-term culturable ex vivo vascularized tissues using biologically derived matrices. Adv Healthc Mater. 2018;7(23):1800845. https://doi.org/10.1002/adhm.201800845.
Ohashi K, Yokoyama T, Yamato M, Kuge H, Kanehiro H, Tsutsumi M, Amanuma T, Iwata H, Yang J, Okano T. Engineering functional two-and three-dimensional liver systems in vivo using hepatic tissue sheets. Nat Med. 2007;13(7):880–5. https://doi.org/10.1038/nm1576.
Hamahashi K, Sato M, Yamato M, Kokubo M, Mitani G, Ito S, Nagai T, Ebihara G, Kutsuna T, Okano T. Studies of the humoral factors produced by layered chondrocyte sheets. J Tissue Eng Regen Med. 2015;9(1):24–30. https://doi.org/10.1002/term.1610.
Hong Y, Yu M, Weng W, Cheng K, Wang H, Lin J. Light-induced cell detachment for cell sheet technology. Biomaterials. 2013;34(1):11–8. https://doi.org/10.1016/j.biomaterials.2012.09.043.
Patel NG, Zhang G. Responsive systems for cell sheet detachment. Organogenesis. 2013;9(2):93–100. https://doi.org/10.4161/org.25149.
Zhang H, Zhou Y, Yu N, Ma H, Wang K, Liu J, Zhang W, Cai Z, He Y. Construction of vascularized tissue-engineered bone with polylysine-modified coral hydroxyapatite and a double cell-sheet complex to repair a large radius bone defect in rabbits. Acta Biomater. 2019;91:82–98. https://doi.org/10.1016/j.actbio.2019.04.024.
Kim K, Bou-Ghannam S, Thorp H, Grainger DW, Okano T. Human mesenchymal stem cell sheets in xeno-free media for possible allogenic applications. Sci Rep. 2019;9(1):14415. https://doi.org/10.1038/s41598-019-50430-7.
Ma D, Ren L, Yao H, Tian W, Chen F, Zhang J, Liu Y, Mao T. Locally injection of cell sheet fragments enhances new bone formation in mandibular distraction osteogenesis: a rabbit model. J Orthopaed Res. 2013;31(7):1082–8. https://doi.org/10.1002/jor.22336.
Du C, Yao C, Li N, Wang S, Feng Y, Yang X. Cell sheet-engineered bones used for the reconstruction of mandibular defects in an animal model. Exp Ther Med. 2015;10(6):2216–20.
Oka M, Miyabe Y, Sugiura N, Nitta K. Cell sheet engineering and kidney diseases. In Recent advances in the pathogenesis and treatment of kidney diseases, vol 195; 2018.
Daley WP, Yamada KM. ECM-modulated cellular dynamics as a driving force for tissue morphogenesis. Curr Opin Genet Dev. 2013;23(4):408–14.
Takeshita K, Motoike S, Kajiya M, Komatsu N, Takewaki M, Ouhara K, Iwata T, Takeda K, Mizuno N, Fujita T. Xenotransplantation of interferon-gamma-pretreated clumps of a human mesenchymal stem cell/extracellular matrix complex induces mouse calvarial bone regeneration. Stem Cell Res Ther. 2017;8(1):1–14. https://doi.org/10.1186/s13287-017-0550-1.
Yorukoglu AC, Kiter A, Akkaya S, Satiroglu-Tufan NL, Tufan AC. A concise review on the use of mesenchymal stem cells in cell sheet-based tissue engineering with special emphasis on bone tissue regeneration. Stem Cells Int. 2017. https://doi.org/10.1155/2017/2374161.
Ren L, Ma D, Liu B, Li J, Chen J, Yang D, Gao P. Preparation of three-dimensional vascularized MSC cell sheet constructs for tissue regeneration. Biomed Res Int. 2014. https://doi.org/10.1155/2014/301279.
Zhang D, Gao P, Li Q, Li J, Li X, Liu X, Kang Y, Ren L. Engineering biomimetic periosteum with β-TCP scaffolds to promote bone formation in calvarial defects of rats. Stem Cell Res Ther. 2017;8(1):134. https://doi.org/10.1186/s13287-017-0592-4.
Akahane M, Nakamura A, Ohgushi H, Shigematsu H, Dohi Y, Takakura Y. Osteogenic matrix sheet-cell transplantation using osteoblastic cell sheet resulted in bone formation without scaffold at an ectopic site-. J Tissue Eng Regen Med. 2008;2(4):196–201. https://doi.org/10.1002/term.81.
Akahane M, Shimizu T, Kira T, Onishi T, Uchihara Y, Imamura T, Tanaka Y. Culturing bone marrow cells with dexamethasone and ascorbic acid improves osteogenic cell sheet structure. Bone Joint Res. 2016;5(11):569–76. https://doi.org/10.1302/2046-3758.511.BJR-2016-0013.R1.
Langenbach F, Handschel J. Effects of dexamethasone, ascorbic acid and β-glycerophosphate on the osteogenic differentiation of stem cells in vitro. Stem Cell Res Ther. 2013;4(5):117. https://doi.org/10.1186/scrt328.
Kim AY, Kim Y, Lee SH, Yoon Y, Kim W-H, Kweon O-K. Effect of gelatin on osteogenic cell sheet formation using canine adipose-derived mesenchymal stem cells. Cell Transpl. 2017;26(1):115–23. https://doi.org/10.3727/096368916x693338.
Wu S-C, Chang W-H, Dong G-C, Chen K-Y, Chen Y-S, Yao C-H. Cell adhesion and proliferation enhancement by gelatin nanofiber scaffolds. J Bioact Compat Polym. 2011;26(6):565–77. https://doi.org/10.1177/0883911511423563.
Ma D, Yao H, Tian W, Chen F, Liu Y, Mao T, Ren L. Enhancing bone formation by transplantation of a scaffold-free tissue-engineered periosteum in a rabbit model. Clin Oral Implants Res. 2011;22(10):1193–9. https://doi.org/10.1111/j.1600-0501.2010.02091.x.
Syed-Picard FN, Shah GA, Costello BJ, Sfeir C. Regeneration of periosteum by human bone marrow stromal cell sheets. J Oral Maxillofac Surg. 2014;72(6):1078–83. https://doi.org/10.1016/j.joms.2014.02.005.
Kim Y, Lee SH, Kang B-J, Kim WH, Yun H-S, Kweon O-K. Comparison of osteogenesis between adipose-derived mesenchymal stem cells and their sheets on poly-caprolactone/-tricalcium phosphate composite scaffolds in canine bone defects. Stem Cells Int. 2016. https://doi.org/10.1155/2016/8414715.
Chen G, Fang T, Qi Y, Yin X, Di T, Feng G, Lei Z, Zhang Y, Huang Z. Combined use of mesenchymal stromal cell sheet transplantation and local injection of SDF-1 for bone repair in a rat nonunion model. Cell Transpl. 2016;25(10):1801–17.
Berntsen L, Forghani A, Hayes DJ. Mesenchymal stem cell sheets for engineering of the tendon-bone interface. Tissue Eng Part A. 2022;28(7–8):341–52.
Nakao M, Inanaga D, Nagase K, Kanazawa H. Characteristic differences of cell sheets composed of mesenchymal stem cells with different tissue origins. Regen Ther. 2019;11:34–40. https://doi.org/10.1016/j.reth.2019.01.002.
Li S, Liao X, He Y, Chen R, Zheng WV, Tang M, Guo X, Chen J, Hu S, Sun J. Exosomes derived from NGF-overexpressing bone marrow mesenchymal stem cell sheet promote spinal cord injury repair in a mouse model. Neurochem Int. 2022;157:105339.
Nishida K, Yamato M, Hayashida Y, Watanabe K, Yamamoto K, Adachi E, Nagai S, Kikuchi A, Maeda N, Watanabe H. Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. N Engl J Med. 2004;351(12):1187–96. https://doi.org/10.1056/NEJMoa040455.
Ahn H, Ju YM, Takahashi H, Williams DF, Yoo JJ, Lee SJ, Okano T, Atala A. Engineered small diameter vascular grafts by combining cell sheet engineering and electrospinning technology. Acta Biomater. 2015;16:14–22. https://doi.org/10.1016/j.actbio.2015.01.030.
Kelm JM, Fussenegger M. Scaffold-free cell delivery for use in regenerative medicine. Adv Drug Deliv Rev. 2010;62(7–8):753–64. https://doi.org/10.1016/j.addr.2010.02.003.
Abbah SA, Lam CX, Ramruttun KA, Goh JC, Wong H-K. Autogenous bone marrow stromal cell sheets-loaded mPCL/TCP scaffolds induced osteogenesis in a porcine model of spinal interbody fusion. Tissue Eng Part A. 2011;17(5–6):809–17. https://doi.org/10.1089/ten.tea.2010.0255.
Li G, Wang X, Cao J, Ju Z, Ma D, Liu Y, Zhang J. Coculture of peripheral blood CD34+ cell and mesenchymal stem cell sheets increase the formation of bone in calvarial critical-size defects in rabbits. Br J Oral Maxillofac Surg. 2014;52(2):134–9. https://doi.org/10.1016/j.bjoms.2013.10.004.
Ren Z, Ma S, Jin L, Liu Z, Liu D, Zhang X, Cai Q, Yang X. Repairing a bone defect with a three-dimensional cellular construct composed of a multi-layered cell sheet on electrospun mesh. Biofabrication. 2017;9(2):025036. https://doi.org/10.1088/1758-5090/aa747f.
Uchiyama H, Yamato M, Sasaki R, Sekine H, Yang J, Ogiuchi H, Ando T, Okano T. In vivo 3D analysis with micro-computed tomography of rat calvaria bone regeneration using periosteal cell sheets fabricated on temperature-responsive culture dishes. J Tissue Eng Regen Med. 2011;5(6):483–90. https://doi.org/10.1002/term.340.
Liu Y, Wang H, Dou H, Tian B, Li L, Jin L, Zhang Z, Hu L. Bone regeneration capacities of alveolar bone mesenchymal stem cells sheet in rabbit calvarial bone defect. J Tissue Eng. 2020;11:2041731420930379. https://doi.org/10.1177/2041731420930379.
Xu X, Fang K, Wang L, Liu X, Zhou Y, Song Y. Local application of semaphorin 3A combined with adipose-derived stem cell sheet and anorganic bovine bone granules enhances bone regeneration in type 2 diabetes mellitus rats. Stem Cells Int. 2019;2019:2506463. https://doi.org/10.1155/2019/2506463.
Li D, Wang W, Guo R, Qi Y, Gou Z, Gao C. Restoration of rat calvarial defects by poly (lactide-co-glycolide)/hydroxyapatite scaffolds loaded with bone mesenchymal stem cells and DNA complexes. Chin Sci Bull. 2012;57(5):435–44. https://doi.org/10.1007/s11434-011-4914-0.
Wang Z, Hu H, Li Z, Weng Y, Dai T, Zong C, Liu Y, Liu B. Sheet of osteoblastic cells combined with platelet-rich fibrin improves the formation of bone in critical-size calvarial defects in rabbits. Br J Oral Maxillofac Surg. 2016;54(3):316–21. https://doi.org/10.1016/j.bjoms.2015.12.015.
Shan X, Hu D. Bone engineering by cell sheet technology to repair mandibular defects. Exp Ther Med. 2017;14(5):5007–11. https://doi.org/10.3892/etm.2017.5118.
Shi L, Tee BC, Cotter L, Sun Z. Enhance mandibular symphyseal surface bone growth with autologous mesenchymal stem cell sheets: an animal study. Aesthetic Plast Surg. 2020;44(1):191–200. https://doi.org/10.1007/s00266-019-01494-3.
Mu S, Tee B, Emam H, Zhou Y, Sun Z. Culture-expanded mesenchymal stem cell sheets enhance extraction-site alveolar bone growth: an animal study. J Periodontal Res. 2018;53(4):514–24. https://doi.org/10.1111/jre.12541.
Kaibuchi N, Iwata T, Yamato M, Okano T, Ando T. Multipotent mesenchymal stromal cell sheet therapy for bisphosphonate-related osteonecrosis of the jaw in a rat model. Acta Biomater. 2016;42:400–10.
Topdag M, Karaoz E, Kara A, Subasi C, Duman BO, Demir N, Konuk E, Ozturk M, Iseri M. Comparative analysis of the healing effects of the transplanted cell sheets to the experimentally injured maxillary sinuses. J Craniofac Surg. 2019;30(7):2285–92. https://doi.org/10.1097/scs.0000000000005638.
Lin J, Shao J, Juan L, Yu W, Song X, Liu P, Weng W, Xu J, Mehl C. Enhancing bone regeneration by combining mesenchymal stem cell sheets with β-TCP/COL-I scaffolds. J Biomed Mater Res B Appl Biomater. 2018;106(5):2037–45. https://doi.org/10.1002/jbm.b.34003.
Damerau A, Buttgereit F, Gaber T. Optimization of a tricalcium phosphate-based bone model using cell-sheet technology to simulate bone disorders. Processes. 2022;10(3):550.
Sivanathan KN, Gronthos S, Rojas-Canales D, Thierry B, Coates PT. Interferon-gamma modification of mesenchymal stem cells: implications of autologous and allogeneic mesenchymal stem cell therapy in allotransplantation. Stem Cell Rev Rep. 2014;10(3):351–75.
Paduano F, Marrelli M, Amantea M, Rengo C, Rengo S, Goldberg M, Spagnuolo G, Tatullo M. Adipose tissue as a strategic source of mesenchymal stem cells in bone regeneration: a topical review on the most promising craniomaxillofacial applications. Int J Mol Sci. 2017;18(10):2140. https://doi.org/10.3390/ijms18102140.
Moschouris K, Firoozi N, Kang Y. The application of cell sheet engineering in the vascularization of tissue regeneration. Regen Med. 2016;11(6):559–70. https://doi.org/10.2217/rme-2016-0059.
Qi Y, Niu L, Zhao T, Shi Z, Di T, Feng G, Li J, Huang Z. Combining mesenchymal stem cell sheets with platelet-rich plasma gel/calcium phosphate particles: a novel strategy to promote bone regeneration. Stem Cell Res Ther. 2015;6(1):1–16. https://doi.org/10.1186/s13287-015-0256-1.
Li T, Peng M, Yang Z, Zhou X, Deng Y, Jiang C, Xiao M, Wang J. 3D-printed IFN-γ-loading calcium silicate-β-tricalcium phosphate scaffold sequentially activates M1 and M2 polarization of macrophages to promote vascularization of tissue engineering bone. Acta Biomater. 2018;71:96–107. https://doi.org/10.1016/j.actbio.2018.03.012.
Hu C, Ashok D, Nisbet DR, Gautam V. Bioinspired surface modification of orthopedic implants for bone tissue engineering. Biomaterials. 2019;219:119366. https://doi.org/10.1016/j.biomaterials.2019.119366.
Xie R, Zheng W, Guan L, Ai Y, Liang Q. Engineering of hydrogel materials with perfusable microchannels for building vascularized tissues. Small. 2020;16(15):1902838. https://doi.org/10.1002/smll.201902838.
Santos MI, Reis RL. Vascularization in bone tissue engineering: physiology, current strategies, major hurdles and future challenges. Macromol Biosci. 2010;10(1):12–27. https://doi.org/10.1002/mabi.200900107.
Pirraco RP, Iwata T, Yoshida T, Marques AP, Yamato M, Reis RL, Okano T. Endothelial cells enhance the in vivo bone-forming ability of osteogenic cell sheets. Lab Invest. 2014;94(6):663–73. https://doi.org/10.1038/labinvest.2014.55.
Correia CR, Pirraco RP, Cerqueira MT, Marques AP, Reis RL, Mano JF. Semipermeable capsules wrapping a multifunctional and self-regulated co-culture microenvironment for osteogenic differentiation. Sci Rep. 2016;6:21883. https://doi.org/10.1038/srep21883.
Silva AS, Santos LF, Mendes MC, Mano JF. Multi-layer pre-vascularized magnetic cell sheets for bone regeneration. Biomaterials. 2020;231:119664. https://doi.org/10.1016/j.biomaterials.2019.119664.
Rehman J, Traktuev D, Li J, Merfeld-Clauss S, Temm-Grove CJ, Bovenkerk JE, Pell CL, Johnstone BH, Considine RV, March KL. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109(10):1292–8. https://doi.org/10.1161/01.CIR.0000121425.42966.F1.
Cai X, Xie J, Yao Y, Cun X, Lin S, Tian T, Zhu B, Lin Y. Angiogenesis in a 3D model containing adipose tissue stem cells and endothelial cells is mediated by canonical Wnt signaling. Bone Res. 2017;5(1):1–13. https://doi.org/10.1038/boneres.2017.48.
Toupadakis CA, Wong A, Genetos DC, Cheung WK, Borjesson DL, Ferraro GL, Galuppo LD, Leach JK, Owens SD, Yellowley CE. Comparison of the osteogenic potential of equine mesenchymal stem cells from bone marrow, adipose tissue, umbilical cord blood, and umbilical cord tissue. Am J Vet Res. 2010;71(10):1237–45. https://doi.org/10.2460/ajvr.71.10.1237.
Barati D, Shariati SRP, Moeinzadeh S, Melero-Martin JM, Khademhosseini A, Jabbari E. Spatiotemporal release of BMP-2 and VEGF enhances osteogenic and vasculogenic differentiation of human mesenchymal stem cells and endothelial colony-forming cells co-encapsulated in a patterned hydrogel. J Control Release. 2016;223:126–36. https://doi.org/10.1016/j.jconrel.2015.12.031.
Hope B, Pearson DEM, Kegelman CD, Zhao L, Dawahare JH, Kacena MA, Boerckel JD. Effects of bone morphogenetic protein-2 on neovascularization during large bone defect regeneration. Tissue Eng Part A. 2019;25(23–24):1623–34. https://doi.org/10.1089/ten.tea.2018.0326.
Ishii M, Shibata R, Numaguchi Y, Kito T, Suzuki H, Shimizu K, Ito A, Honda H, Murohara T. Enhanced angiogenesis by transplantation of mesenchymal stem cell sheet created by a novel magnetic tissue engineering method. Arterioscler Thromb Vasc Biol. 2011;31(10):2210–5. https://doi.org/10.1161/atvbaha.111.231100.
McLaughlin MM, Marra KG. The use of adipose-derived stem cells as sheets for wound healing. Organogenesis. 2013;9(2):79–81. https://doi.org/10.4161/org.24946.
Chen G, Qi Y, Niu L, Di T, Zhong J, Fang T, Yan W. Application of the cell sheet technique in tissue engineering. Biomed Rep. 2015;3(6):749–57. https://doi.org/10.3892/br.2015.522.
Nakano K, Murata K, Omokawa S, Akahane M, Shimizu T, Kawamura K, Kawate K, Tanaka Y. Promotion of osteogenesis and angiogenesis in vascularized tissue-engineered bone using osteogenic matrix cell sheets. Plast Reconstr Surg. 2016;137(5):1476–84. https://doi.org/10.1097/prs.0000000000002079.
Nakamura A, Akahane M, Shigematsu H, Tadokoro M, Morita Y, Ohgushi H, Dohi Y, Imamura T, Tanaka Y. Cell sheet transplantation of cultured mesenchymal stem cells enhances bone formation in a rat nonunion model. Bone. 2010;46(2):418–24.
Sorrell JM, Baber MA, Caplan AI. Influence of adult mesenchymal stem cells on in vitro vascular formation. Tissue Eng Part A. 2009;15(7):1751–61.
Mendes LF, Pirraco RP, Szymczyk W, Frias AM, Santos TC, Reis RL, Marques AP. Perivascular-like cells contribute to the stability of the vascular network of osteogenic tissue formed from cell sheet-based constructs. PLOS ONE. 2012;7(7):e41051. https://doi.org/10.1371/journal.pone.0041051.
Kang Y, Ren L, Yang Y. Engineering vascularized bone grafts by integrating a biomimetic periosteum and β-TCP scaffold. ACS Appl Mater Interfaces. 2014;6(12):9622–33.
Sekine H, Shimizu T, Sakaguchi K, Dobashi I, Wada M, Yamato M, Kobayashi E, Umezu M, Okano T. In vitro fabrication of functional three-dimensional tissues with perfusable blood vessels. Nat Commun. 2013;4:1399. https://doi.org/10.1038/ncomms2406.
Sakaguchi K, Shimizu T, Horaguchi S, Sekine H, Yamato M, Umezu M, Okano T. In vitro engineering of vascularized tissue surrogates. Sci Rep. 2013;3:1316. https://doi.org/10.1038/srep01316.
Tian L, George SC. Biomaterials to prevascularize engineered tissues. Cardiovasc Transl Res. 2011;4(5):685–98. https://doi.org/10.1007/s12265-011-9301-3.
Sukho P, Hesselink JW, Kops N, Kirpensteijn J, Verseijden F, Bastiaansen-Jenniskens YM. Human mesenchymal stromal cell sheets induce macrophages predominantly to an anti-inflammatory phenotype. Stem cells and development. 2018;27(13):922–34.
Madrigal M, Rao KS, Riordan NH. A review of therapeutic effects of mesenchymal stem cell secretions and induction of secretory modification by different culture methods. J Transl Med. 2014;12:260. https://doi.org/10.1186/s12967-014-0260-8.
Wahl SM, Orenstein JM, Chen W. TGF-β influences the life and death decisions of T lymphocytes. Cytokine Growth Factor Rev. 2000;11(1–2):71–9. https://doi.org/10.1016/s1359-6101(99)00030-1.
Oshimori N, Fuchs E. The harmonies played by TGF-β in stem cell biology. Cell Stem Cell. 2012;11(6):751–64. https://doi.org/10.1016/j.stem.2012.11.001.
Niu J, Yue W, Le-Le Z, Bin L, Hu X. Mesenchymal stem cells inhibit T cell activation by releasing TGF-β1 from TGF-β1/GARP complex. Oncotarget. 2017;8(59):99784–800. https://doi.org/10.18632/oncotarget.21549.
Gomez I, Foudi N, Longrois D, Norel X. The role of prostaglandin E2 in human vascular inflammation. Prostaglandins Leukot Essent Fatty Acids. 2013;89(2–3):55–63. https://doi.org/10.1016/j.plefa.2013.04.004.
Corradetti B, Taraballi F, Minardi S, Van Eps J, Cabrera F, Francis LW, Gazze SA, Ferrari M, Weiner BK, Tasciotti E. Chondroitin sulfate immobilized on a biomimetic scaffold modulates inflammation while driving chondrogenesis. Stem Cells Transl Med. 2016;5(5):670–82. https://doi.org/10.5966/sctm.2015-0233.
Wynn TA, Vannella KM. Macrophages in tissue repair, regeneration, and fibrosis. Immunity. 2016;44(3):450–62. https://doi.org/10.1016/j.immuni.2016.02.015.
Cao C, Tarlé S, Kaigler D. Characterization of the immunomodulatory properties of alveolar bone-derived mesenchymal stem cells. Stem Cell Res Ther. 2020;11(1):1–13. https://doi.org/10.1186/s13287-020-01605-x.
Nielsen MC, Hvidbjerg Gantzel R, Clària J, Trebicka J, Møller HJ, Grønbæk H. Macrophage activation markers, CD163 and CD206, in acute-on-chronic liver failure. Cells. 2020;9(5):1175.
Volarevic V, Al-Qahtani A, Arsenijevic N, Pajovic S, Lukic ML. Interleukin-1 receptor antagonist (IL-1Ra) and IL-1Ra producing mesenchymal stem cells as modulators of diabetogenesis. Autoimmunity. 2010;43(4):255–63.
Xiao G, Gopalakrishnan R, Jiang D, Reith E, Benson MD, Franceschi RT. Bone morphogenetic proteins, extracellular matrix, and mitogen-activated protein kinase signaling pathways are required for osteoblast-specific gene expression and differentiation in MC3T3-E1 cells. J Bone Miner Res. 2002;17(1):101–10.
Li Y, Ge C, Franceschi RT. Differentiation-dependent association of phosphorylated extracellular signal-regulated kinase with the chromatin of osteoblast-related genes. J Bone Miner Res. 2010;25(1):154–63.
Frendo J-L, Xiao G, Fuchs S, Franceschi RT, Karsenty G, Ducy P. Functional hierarchy between two OSE2 elements in the control of osteocalcin gene expression in vivo. J Biol Chem. 1998;273(46):30509–16.
Bialek P, Kern B, Yang X, Schrock M, Sosic D, Hong N, Wu H, Yu K, Ornitz DM, Olson EN. A twist code determines the onset of osteoblast differentiation. Dev Cell. 2004;6(3):423–35.
Hassan MQ, Javed A, Morasso MI, Karlin J, Montecino M, Van Wijnen AJ, Stein GS, Stein JL, Lian JB. Dlx3 transcriptional regulation of osteoblast differentiation: temporal recruitment of Msx2, Dlx3, and Dlx5 homeodomain proteins to chromatin of the osteocalcin gene. Mol Cell Biol. 2004;24(20):9248–61.
Zhang W, Xue D, Yin H, Wang S, Li C, Chen E, Hu D, Tao Y, Yu J, Zheng Q. Overexpression of HSPA1A enhances the osteogenic differentiation of bone marrow mesenchymal stem cells via activation of the Wnt/β-catenin signaling pathway. Sci Rep. 2016;6(1):1–11.
Kirby GT, Michelmore A, Smith LE, Whittle JD, Short RD. Cell sheets in cell therapies. Cytotherapy. 2018;20(2):169–80. https://doi.org/10.1016/j.jcyt.2017.11.004.
Lu Y, Zhang W, Wang J, Yang G, Yin S, Tang T, Yu C, Jiang X. Recent advances in cell sheet technology for bone and cartilage regeneration: from preparation to application. Int J Oral Sci. 2019;11(2):1–13. https://doi.org/10.1038/s41368-019-0050-5.
Nozaki T, Yamato M, Inuma T, Nishida K, Okano T. Transportation of transplantable cell sheets fabricated with temperature-responsive culture surfaces for regenerative medicine. J Regen Med Tissue Eng. 2008;2(4):190–5. https://doi.org/10.1002/term.80.
Acknowledgements
The authors wish to thank the personnel of the Department of Tissue Engineering for their help and guidance.
Funding
This is a report of the database from a Ph.D. thesis registered in Tabriz University of Medical Sciences with the Number 64739 (Ethical code: IR.TBZMED.VCR.REC.1399.055).
Author information
Authors and Affiliations
Contributions
BBS and SFK prepared the draft and wrote the manuscript; BBS and SS were responsible for reviewing; AM and SJ were involved in study consultation; and RR and HS took part in supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Banimohamad-Shotorbani, B., Karkan, S.F., Rahbarghazi, R. et al. Application of mesenchymal stem cell sheet for regeneration of craniomaxillofacial bone defects. Stem Cell Res Ther 14, 68 (2023). https://doi.org/10.1186/s13287-023-03309-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03309-4