Abstract
Background
Microbiome restitution therapies are being developed to prevent gut pathogen colonization among patients in the intensive care unit (ICU) and in other select populations. If preventive therapies are to be effective, they must be administered prior to pathogen acquisition. The timing and risk factors for early acquisition of gut pathogen colonization (within 72 h) are currently unknown and could be helpful to guide ICU trial design.
Methods
This was a prospective cohort study. Patients in the ICU had deep rectal swabs performed within 4 h of ICU admission and exactly 72 h later. Early gut pathogen colonization was classified as the new presence (based on culture of rectal swabs) of one or more of the following organisms of interest: methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant (VRE), and Gram-negative bacteria that showed multidrug resistance (MDR) or third generation Cephalosporin resistance (Ceph-R). Clinical risk factors for early acquisition of gut pathogen colonization were captured using the Acute Physiology and Chronic Health Evaluation IV (APACHE IV) scoring system.
Findings
Among 131 patients who were swabbed at ICU admission and 72 h later, the rates of gut pathogen colonization at ICU admission were 11.4%, 10.6%, 38.6%, and 8.3% for MRSA, VRE, MDR and Ceph-R Gram-negatives respectively. Among the patients who were negative for a given pathogen at ICU admission, the rates of early acquisition of gut pathogen colonization were 7.8% for MRSA (95% CI 3.6 to 14.2%), 7.7% for VRE (95% CI 3.6 to 14.1%), 11.3% for MDR Gram-negatives (95% CI 4.4 to 18.8%), and 4.2% for Ceph-R Gram-negatives (95% CI 1.4 to 9.5%). There were no clinical risk factors which independently predicted early acquisition of gut pathogen colonization.
Interpretation
Early gut pathogen colonization was common in the ICU, but our single-center study could not identify any clinical risk factors which were significantly associated with acquisition of gut pathogens.
Similar content being viewed by others
Introduction
Healthcare-associated infections caused by pathogenic (often MDR) bacteria are a significant concern in the medical ICU with mortality rates ranging from 26% to 80% [1]. Gut colonization with pathogenic bacteria is a risk factor for subsequent all-cause and pathogen-specific systemic infections [2,3,4,5,6,7]. Therefore, understanding the prevalence and dynamics of gut pathogen colonization is crucial for developing targeted interventions to mitigate the spread of these organisms and improve patient outcomes [8, 9].
Previous studies have demonstrated that the prevalence of gut pathogen colonization is high at the time of ICU admission and that many previously uncolonized patients acquire gut pathogens during prolonged ICU stays [3, 10,11,12,13,14,15,16]. Specific estimates of gut colonization and acquisition range based on institution and organism. For example, the prevalence of gut colonization with VRE at ICU admission has been estimated at 3.6–10.6%, with acquisition rates from 3.0 to 10.2% during the ICU stay [17, 18]. Similarly, for carbapenem-resistant Enterobacteriaceae (CRE), prevalence of gut colonization at the time of ICU admission has been estimated at 2.1–28% with acquisition rates reaching up to 58.6% during prolonged ICU stays [19, 20]. Many studies show strong associations between fecal carriage of MDR organisms and subsequent systemic infections with the same organisms: e.g., 77% of patients who developed MDR Acinetobacter baumanii infections were identified as fecal carriers [21, 22].
These prior studies are valuable but leave relatively wide estimates of confidence in rates of acquisition of gut pathogen colonization. Because many studies perform sampling at the end of the study period or immediately prior to ICU discharge, they do not always describe the dynamics of acquisition of gut pathogen colonization, which is crucial for the design of future ICU trials. Among ICU patients with sepsis, improvement or lack thereof during the early ICU period—typically defined as the first 72 h after ICU admission—has been shown to be a powerful predictor of subsequent risk for death [23, 24]. An underlying hypothesis of this study was that early gut pathogen colonization would similarly have greater importance for patient outcomes compared to late gut pathogen colonization.
There are additional gaps in the existing literature. Prior studies have determined the clinical risk factors for gut colonization with pathogenic bacteria, but they have not always distinguished between prevalent colonization (colonization at the time of ICU admission) and incident colonization (acquisition of gut pathogen colonization during some predetermined time period in the ICU) [25, 26]. Last, although prior studies of gut pathogen colonization in the ICU have often utilized protocolized sample collection—e.g., weekly after ICU admission—they have not always collected samples from the same individual patients, thus leaving some uncertainty related to whether there was a within-individual change in the gut pathogen colonization status of a given patient [19].
In this study, we performed protocolized collection of rectal swabs within 4 h of ICU admission (typically performed immediately when the patient was transferred into his or her ICU bed) and exactly 72 h later on the same patients. We used standard culture-based methods to define the within-individual changes in gut pathogen colonization status so that we could fully understand the acquisition rates and risk factors for gut pathogen colonization during the early period in ICU hospitalization. We focused on VRE, MRSA, and MDR Gram-negative (GN) bacteria because these organisms account for a large proportion of ICU-acquired infections and are readily cultured.
Methods
Population and rationale
The study enrolled adult patients aged 18 or more years who were newly admitted to an ICU (medical, surgical, or specialty ICU), provided informed consent for rectal swab collection (delayed patient or surrogate consent accepted) [27], and survived for a minimum of 72 h in the ICU after admission so that they could provide a follow-up rectal swab. Due to the time sensitive protocol, a “delayed consent” model was utilized, where baseline rectal swabs were obtained, and later sought permission to retain them [27]. The rationale for selecting 72 h as the sampling interval was based on prior ICU literature related to sepsis, including the APACHE studies [28, 29]. This literature suggests that ICU interventions must be deployed during the first 72 h to be most effective at altering patient outcomes. Because the focus of the study was on early acquisition of gut pathogen colonization, we excluded data from subjects who were swabbed at ICU admission and could not be swabbed again due to death or discharge. Our overall goal was to study a heterogeneous ICU population, the same population that would be targeted for future trials testing therapies to prevent acquisition of gut pathogen colonization.
Rectal swabs
Rectal swabs were performed by an ICU nurse, within 4 h of ICU admission and then again 72 h later (+/- 4 h). The swab at admission was typically taken immediately as the patient transitioned from the transport gurney to the ICU bed. Fecal soilage/staining was used to verify that swabs were adequate. With the patient in the left lateral decubitus position, flocked nylon swabs (Eswab, Copan Diagnostics, Murrieta, CA) were inserted at least 6 cm into the rectum and spun clockwise five times while moving them longitudinally.
Cultures for multi-drug resistant organisms
The organisms of interest in this study were MRSA, VRE, and MDR or Ceph-R Gram-negative bacteria. These organisms were selected because they are readily culturable and cause up to 40% of all culture-proven infections in the ICU [30]. Aliquoted rectal swab specimens were plated onto chromogenic agars for MRSA (Spectra MRSA agar, Remel, San Diego, CA)and VRE (Spectra VRE agar, Remel, San Diego, CA)), as well MacConkey agar for Gram-negative bacteria. Gram-negative colonies were selected from MacConkey based on predominant colony morphology, with identification and antimicrobial susceptibility testing performed using the Vitek 2 system with AST-N010/020 cards with confirmatory testing as needed. Current Clinical and Laboratory Standards Institute (CLSI) breakpoints were used for categorical interpretations of susceptibility. For this study, Gram-negative bacteria were classified as MDR if they were non-susceptible to three or more antimicrobial categories [31, 32]. Gram-negative bacteria were classified as Ceph-R if they showed non-susceptibility to 3rd generation cephalosporins (ceftriaxone or ceftazidime) [33]. All organisms of interest were classified as present or absent at ICU admission and again after 72 h.
Early acquisition of gut pathogen colonization
Early acquisition of gut pathogen colonization was defined categorically, in a pathogen-specific manner for each individual patient. For the organisms of interest—MRSA, VRE, and the Gram-negative bacteria—patients were defined as having acquired gut pathogen colonization if the organism was absent at the time of ICU admission but present after 72 h.
Clinical risk factors for early acquisition of gut pathogen colonization
We were interested in testing clinical variables as potential risk factors for early acquisition of gut pathogen colonization. The APACHE IV score was used to assess acute severity of illness, and was calculated at the time of ICU admission and again after 72 h. APACHE-IV is calculated by incorporating a comprehensive set of variables including age, sex, admission date to the ICU, vital signs, laboratory findings, and various clinical parameters to assess the severity of illness in critically ill patients. APACHE-IV scores were grouped into three categories: low (≤ 42), middling (43–73), and high (> 73). Besides assessing the total APACHE IV score, the component variables of the APACHE IV were also measured. We gathered the following co-variables in addition to the APACHE component variables: age (organized into tertiles), sex (biological sex at birth), ICU type (cardiac, medical, neurological, or surgical), ICU admission diagnosis, and pre-ICU hospital days. ICU admission diagnosis was determined by the primary reason for ICU admission, categorized by organ system. For all variables included in the APACHE score, we adopted the respective cutoffs specified by the APACHE criteria.
Clinical outcomes: death or culture-proven infection
To examine the downstream impact of gut pathogen colonization, we examined a composite outcome of death and culture-proven infection within 30 days from ICU admission, an outcome that we and others have utilized previously [2]. The rationale for this composite outcome is that death and culture-proven infection function as competing risks because a patient might die from infection before the infection can be diagnosed. Operationalization of this outcome followed previously described methods.
Statistical approach
Continuous measures were divided into tertiles. An exact binomial calculation was used to estimate the 95% confidence intervals for proportions. Chi-squared tests were used to compare co-variables based on early acquisition of gut pathogen colonization. A logistic regression model was constructed for the outcome of early acquisition of gut pathogen colonization. APACHE IV score was included in this model a priori, with additional predictor variables added stepwise and retained in the model if they had an independent association (p < 0.10) with the outcome. An additional model was examined which interrogated the component measures within APACHE IV as predictors. To examine the relationship between early acquisition of gut pathogen colonization and the composite outcome of death and culture-proven infection, we constructed a Cox proportional hazards model. This model had three exposure groups: patients who were not colonized at either ICU admission or 72 h later, patients who were colonized at ICU admission (with or without colonization at 72 h), and patients who were not colonized at admission but acquired one or more pathogens after 72 h. Last, a sample size calculation was performed to guide future ICU trials; this calculation was performed as a two-sided test of two proportions with alpha 0.05.
Results
Patient baseline characteristics
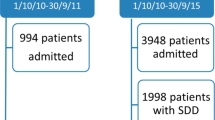
177 patients donated a rectal swab at ICU admission including 15 (8.5%) who died before 72 h had elapsed and 31 (17.5%) who remained alive but declined to provide a 72 h sample. This left 131 (74%) patients who survived 72 h and donated a second rectal swab for the analyses. Among the 131 patients, most were over 50 years old, with approximately equal numbers of females and males (Table 1). Patients were admitted to a variety of ICU types (medical, surgical, etc.) and were predominantly admitted directly to the ICU from the emergency room (74.0%). Acute severity of illness was high, with a median APACHE IV score of 52 (IQR 38 to 89).
Gut pathogen colonization
Rates of gut colonization at ICU admission were 11.4%, 10.6%, 38.6%, and 8.3% for MRSA, VRE, MDR Gram-negatives, and Ceph-R Gram-negatives respectively (Fig. 1). 48.1% of patients were colonized with one or more of these organisms at ICU admission. After 72 h in the ICU, rates of gut colonization were 14.4%, 16.7%, 34.8%, and 9.1% for the same organisms and 51.1% of patients were colonized with one or more organisms. Among 116 patients who were negative for MRSA at ICU admission, rates of early gut MRSA acquisition were 9/116 (7.8%, 95% CI 3.6 to 14.2%). Similarly, rates for early acquisition of VRE were 9/117 (7.7%, 95% CI 3.6 to 14.1%); rates for early acquisition of MDR Gram-negatives were 9/80 (11.3%, 95% CI 4.4 to 18.8%); rates for early acquisition of Ceph-R Gram-negatives were 5/120 (4.2%, 95% CI 1.4 to 9.5%). 18/131 (17.6%) of patients who tested positive for a given organism at the time of ICU admission had subsequently tested negative for the same organism at 72 h. For individual organisms, the rates were 5/131 (3.8%) for MRSA, 1/131 (0.8%) for VRE, 13/131 (9.9%) for MDR Gram-negatives, and 4/131 (3.1%) for Ceph-R organisms.
Proportion of patients with gut pathogen colonization at the time of ICU admission and 72 h later
Stacked bar graph showing the proportions of patients colonized at ICU admission and again at 72 h. The bar graph is organized by organism and to highlight the patients who acquired colonization (white bars), meaning that they were colonized at 72 h but not at ICU admission. MRSA: methicillin-resistant Staphylococcus aureus; VRE: Vancomycin-Resistant Enterococcus; MDR: Multidrug Resistance; Ceph-R: Third Generation Cephalosporin-resistant
Characteristics of colonizing Gram-negatives
The most common Gram-negative bacteria cultured from rectal swabs were E. coli, followed by K. pneumoniae and Enterobacter spp. (Table 2). There were also 3 cases of non-MDR Pseudomonas spp. The comparison of the antimicrobial resistance patterns within Gram-negative bacteria showed minimal differences comparing the overall resistance pattern at ICU admission versus 72 h later (Fig. 2). The largest increase in resistance was observed with nitrofurantoin, followed by cefoxitin and cefazolin. However, the proportion of Gram-negatives showing non-susceptibility was similar for most antibiotics over this short timeframe.
Antibiotic resistance pattern among Gram-negative bacteria cultured at the time of ICU admission and 72 h later
Mero: Meropenem; Erta: Ertapenem; Tige: Tigecycline; Ami: Amikacin; Cefep: Cefepime; Ceftaz: Ceftazidime; Pip-Tazo: Piperacillin/Tazobactam; Tobra: Tobramycin; Gent: Gentamicin; CFTX: Ceftriaxone; Azt: Aztreonam; Cefox: Cefoxitin; Nitro: Nitrofurantoin; Levo: Levofloxacin; Cefaz: Cefazolin; TMP-SMX: Trimethoprim/Sulfamethoxazole; Tetra: Tetracycline; Amp-Sul: Ampicillin/Sulbactam
Clinical risk factors for acquisition of early gut pathogen colonization
Baseline patient characteristics including acute severity of illness (APACHE IV) at ICU admission were compared between those who did versus those who did not acquire early gut pathogen colonization (Table 1). None of these clinical risk factors was associated with acquisition of early gut pathogen colonization. Neither APACHE IV score nor any other co-variables from the time of ICU admission predicted early gut pathogen colonization (odds ratio (OR) 0.86, 95% CI 0.30–2.49 for a middling vs. low APACHE IV score and OR 1.18, 95% CI 0.43–3.26 for a high vs. low APACHE IV score). In a multivariable model, there were no risk factors identified which associated with the outcome of early acquisition of pathogen colonization (Supplemental Table 1).
Death and culture-proven infection
There were 11 deaths (8.4%) and 21 (16.0%) culture-proven infections within 30 days of ICU admission; 29 (22.1%) of patients had the combined outcome of death or infection within 30 days. The most common infection sites were urine (N = 10), respiratory (N = 7), and bloodstream (N = 7) (Table 3). The most common infection-causing organisms were Klebsiella spp. (N = 5) followed by E. coli, Pseudomonas spp., and Enterobacter spp. (N = 4 each). Out of the 5 patients with Klebsiella infections, 1 was previously colonized with Klebsiella spp. (1/5, 20%), 4/4 (100%) were previously colonized with E. coli, and 0/4 (0%) were previously colonized with Enterobacter spp.
Acquisition of early gut pathogen colonization and risk for death or infection
Patient characteristics after 72 h in the ICU were examined to explore their association with subsequent occurrences of death or infection (Table 4). Longer pre-ICU hospital stays (> 2 days), receipt of dialysis, and receipt of mechanical ventilation, was associated with increased risk for the composite outcome. Elevated heart rate, respiratory rate, and creatinine levels were also associated with higher rates of death or infection, as was lower Glasgow Coma Scale scores (< 5 points) and higher APACHE IV score (Supplemental Table 2). Neither receipt of antibiotics nor receipt of PPIs was associated with the composite outcome. An additional analysis examining all-cause death showed an association between the APACHE IV score and all-cause death (OR 11.4, 95% CI 1.37–94.3); several additional APACHE IV score component variables were also associated with all cause death including creatinine, ventilation status, and Glasgow coma scale. Acquisition of early pathogen colonization was not associated with all cause death (OR 0.84, 95% CI 0.17–4.16).
Cox proportional hazards model for death or infection
Finally, we examined the relationship between new gut pathogen colonization and death or culture-proven infection using time-to-event methods (Fig. 3). Patients were divided into three groups: not colonized, colonized at admission (with or without colonization after 72 h), and new colonization. The highest rates of death or infection were among those who were newly colonized, followed by those with baseline colonization, and those without colonization had the lowest rates (Log-Rank not statistically significant, p = 0.257). Next, we constructed a Cox proportional hazards model for the outcome of death or culture-proven infection within 30 days of ICU admission. In this model, we compared three categories of patients: those who were never gut pathogen colonized, those who were colonized at ICU admission (regardless of colonization status after 72 h), and those who had early acquisition of gut pathogen colonization. Compared versus a reference group who was never colonized, the crude hazard ratio for death or infection was 1.69 (95% CI 0.70–4.09) for those who were colonized at ICU admission and was 2.19 (95% CI 0.82–5.84) for those who had early gut acquisition of colonization. APACHE IV score was a strong independent predictor for death or infection, but adjusting for APACHE score did not substantially alter the relationship between early gut colonization and death or infection.
Discussion
This study assessed early acquisition of gut pathogen colonization by performing protocolized deep rectal swabs on patients at the time of ICU admission and exactly 72 h later. Focusing on acquisition of VRE, MRSA, or MDR/Ceph-R Gram-negative bacteria, we found that rates of early acquisition varied from 4.2 to 11.3% across the organisms of interest. Among patients who were not previously gut pathogen colonized, one in every five patients became colonized during this period of short-term follow-up. One caveat to this finding is that there was “noise” in our data, with some patients who were classified as colonized at ICU admission then testing negative three days later. This intermittent intestinal carriage has been observed in previous studies and may represent false negatives or true changes in carriage due to administration of antibiotics or natural clearance [8, 34, 35]. False negative misclassification of baseline swabs could lead to an overestimation of rates of early gut pathogen colonization.
Interestingly, the observed rates of 30-day death or infection were worse among patients who had early acquisition of gut pathogen colonization compared to those who were already colonized at the time of ICU admission, although this result was not statistically significant. Overall, our findings highlight the need for early interventions aimed at preventing acquisition of gut pathogen colonization in the ICU, particularly for patients at high risk for sepsis. The early hours of an ICU admission are a critical window during which interventions can have the most substantial impact on patient outcomes (e.g., in treatment of sepsis where in-hospital mortality can be reduced by early interventions by up to 16%) [36]. Our study demonstrates that substantial, likely clinically relevant, changes are taking place in terms of gut colonization status during this same early ICU time period.
In terms of specific organisms, our study results are similar to previous studies, although variation in the ICU population, local pathogen prevalence, and the timeframe of testing make exact comparisons challenging [3]. A prior meta-analysis estimated the acquisition rate of VRE to be 10.2% within the United States [18], which is similar to our finding of a VRE acquisition rate of 10.6% within the first 72 h. However, acquisition rates of VRE can vary greatly between studies based on frequency and type of screening [17, 37]. Our study had an MRSA acquisition rate of 7.8% during the initial 72 h of ICU admission and Thompson et al. similarly found an MRSA acquisition rate of 7.5%; however, this study and many others re-tested for colonization after one week or more instead of 72 h [38,39,40]. For Gram-negative bacteria, our study had a Ceph-R acquisition rate of 4.2% within the first 72 h of ICU admission which is similar to the 3% acquisition rate in the Americas estimated by a previous meta-analysis [3]. However, these studies screened weekly after admission [41, 42], so it is again unclear what proportion was acquired within 72 h. Given the similar rates of acquisition in our study after 72 h and other studies that screen after a greater time interval, it is likely that much pathogen acquisition takes place during the first few days after ICU admission.
Our results also can be used as the basis for sample size calculations for future trials seeking to intervene to decolonize patients or prevent colonization and emphasize that the appropriate design for future trials will depend on the hypothesized mechanism of the intervention. Pre-selection of patients based on rapid testing for colonization at the time of ICU admission is likely to enhance the efficiency of future trials design. Clinical variables, on the other hand, are less likely to be useful in pre-selecting patients for future trials; none of them—including APACHE IV score—were associated with acquisition of gut pathogens in this study. No clinical variables—including APACHE IV and its components—were associated with early gut colonization whereas APACHE score and a number of other clinical predictors were identified which associated with death or infection. Although no clinical variables were associated with early acquisition of gut pathogen colonization, we did not have access to data related to pre-ICU antibiotics exposure or to prior residence in a nursing home, two variables which might associate with colonization. Our single-center data is insufficient to conclusively determine whether clinical risk factors might be useful in pre-selecting colonized patients for trials.
This study has some strengths. The emphasis on early acquisition of gut pathogen colonization (within 72 h) is unusual. This approach provides unique insights into the rapid dynamics of gut colonization in critically ill patients, a timeframe that has been less explored in previous research. By narrowing the window of observation, the study highlights the urgency of addressing colonization during the initial stages of an ICU stay, which informs the timing of future interventions. Sample acquisition was strictly protocolized, was done in real time, and used low cost, readily accessible culture-based methods (as opposed to sequencing) that could be easily replicated across institutions. The study also has limitations. We did not have the resources to extend sample collection beyond 72 h; we have ongoing studies which will address this by taking protocolized samples on ICU days 0, 3, 7, 14, and 30. Future studies may wish to gather samples even more densely, and for longer durations. Our findings are derived from a diverse range of ICU types, but in a single institution, and the gut colonization characteristics of the background population are likely to influence ICU colonization and impact study generalizability. The decision to exclude subjects who were swabbed at ICU admission but did not undergo a second swab introduces a potential for immortal time bias. Last, the sample size was relatively small, with a consequent effect on the confidence for our estimates of acquisition of gut pathogen colonization.
In sum, this prospective cohort study found that over one in five ICU patients acquired gut pathogen colonization within 72 h of ICU admission (MRSA, VRE, or MDR/Ceph-R GN bacteria). By describing the dynamics of early gut pathogen colonization in the ICU, these results may guide future trials seeking to test ICU interventions to reduce or prevent gut pathogen colonization.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive Care Unit
- MRSA:
-
Methicillin-Resistant Staphylococcus Aureus
- VRE:
-
Vancomycin-Resistant Enterococcus
- MDR:
-
Multidrug Resistance
- Ceph-R:
-
Third Generation Cephalosporin-resistant
- APACHE IV:
-
Acute Physiology and Chronic Health Evaluation IV
- CRE:
-
Carbapenem-Resistant Enterobacteriaceae
- GN:
-
Gram-negative
- CLSI:
-
Clinical and Laboratory Standards Institute
References
Morris S, Cerceo E. Trends, Epidemiology, and management of Multi-drug Resistant Gram-negative bacterial infections in the hospitalized setting. Antibiot (Basel). 2020;9(4).
Freedberg DE, Zhou MJ, Cohen ME, Annavajhala MK, Khan S, Moscoso DI, et al. Pathogen colonization of the gastrointestinal microbiome at intensive care unit admission and risk for subsequent death or infection. Intensive Care Med. 2018;44(8):1203–11.
Detsis M, Karanika S, Mylonakis EICU, Acquisition Rate. Risk factors, and clinical significance of Digestive Tract colonization with extended-spectrum beta-lactamase–producing Enterobacteriaceae. Crit Care Med. 2017;45(4):705–14.
Massart N, Camus C, Benezit F, Moriconi M, Fillatre P, Le Tulzo Y. Incidence and risk factors for acquired colonization and infection due to extended-spectrum beta-lactamase-producing Gram-negative bacilli: a retrospective analysis in three ICUs with low multidrug resistance rate. Eur J Clin Microbiol Infect Dis. 2020;39(5):889–95.
Prado V, Hernández-Tejero M, Mücke MM, Marco F, Gu W, Amoros A, et al. Rectal colonization by resistant bacteria increases the risk of infection by the colonizing strain in critically ill patients with cirrhosis graphical abstract rectal colonization by multidrug-resistant organism predominant colonizing strain. J Hepatol. 2022;76:1079–89.
Falcone M, Tiseo G, Galfo V, Giordano C, Leonildi A, Marciano E, et al. Bloodstream infections in patients with rectal colonization by Klebsiella pneumoniae producing different type of carbapenemases: a prospective, cohort study (CHIMERA study). Clin Microbiol Infect. 2022;28(2):298.e1-.e7
Oostdijk EAN, De Smet AMGA, Kesecioglu J, Bonten MJM, editors. The role of intestinal colonization with Gram-negative bacteria as a source for intensive care unit-acquired bacteremia. Critical Care Medicine; 2011: Lippincott Williams and Wilkins.
Grohs P, Podglajen I, Guerot E, Bellenfant F, Caumont-Prim A, Kac G, et al. Assessment of five screening strategies for optimal detection of carriers of third-generation cephalosporin-resistant Enterobacteriaceae in intensive care units using daily sampling. Clin Microbiol Infect. 2014;20(11):O879–86.
Sharma K, Lakshmi Nag VTV, Kumar Bhatia P. N.Kothari. An observational study on carbapenem-resistant Enterobacterales (CRE) colonisation and subsequent risk of infection in an adult intensive care unit (ICU) at a tertiary care hospital in India. Infect Prev Pract. 2023;5(4).
Maamar E, Ferjani S, Jendoubi A, Hammami S, Hamzaoui Z, Mayonnove-Coulange L, et al. High prevalence of Gut Microbiota colonization with broad-spectrum cephalosporin resistant Enterobacteriaceae in a Tunisian Intensive Care Unit. Front Microbiol. 2016;7:1859.
Razazi K, Derde LPG, Verachten M, Legrand P, Lesprit P, Brun-Buisson C. Clinical impact and risk factors for colonization with extended-spectrum β-lactamase-producing bacteria in the intensive care unit. Intensive Care Med. 2012;38(11):1769–78.
Warren DK, Kollef MH, Seiler SM, Fridkin SK, Fraser VJ. The epidemiology of Vancomycin-resistant Enterococcus colonization in a medical intensive care unit colonization in a medical intensive care unit. Infect Control Hosp Epidemiol. 2003;24(4):257–63.
Alves M, Lemire A, Decré D, Margetis D, Bigé N, Pichereau C, et al. Extended-spectrum beta-lactamase–producing enterobacteriaceae in the intensive care unit: acquisition does not mean cross-transmission. BMC Infect Dis. 2016;16:147.
Boutrot M, Azougagh K, Guinard J, Boulain T. Antibiotics with activity against intestinal anaerobes and the hazard of acquired colonization with ceftriaxone-resistant Gram-negative pathogens in ICU patients: a propensity score-based analysis. J Antimicrob Chemother. 2019;74(10):3095–103.
Kluytmans-van den Bergh MFQ, van Mens SP, Haverkate MR, Bootsma MCJ, Kluytmans J, Bonten MJM, et al. Quantifying hospital-acquired carriage of extended-spectrum beta-lactamase-producing Enterobacteriaceae among patients in Dutch hospitals. Infect Control Hosp Epidemiol. 2018;39(1):32–9.
Papadimitriou-Olivgeris M, Drougka E, Fligou F, Kolonitsiou F, Liakopoulos A, Dodou V, et al. Risk factors for enterococcal infection and colonization by Vancomycin-resistant enterococci in critically ill patients. Infection. 2014;42(6):1013–22.
Kampmeier S, Kossow A, Clausen LM, Knaack D, Ertmer C, Gottschalk A, et al. Hospital acquired Vancomycin resistant enterococci in surgical intensive care patients - a prospective longitudinal study. Antimicrob Resist Infect Control. 2018;7:103.
Ziakas PD, Thapa R, Rice LB, Mylonakis E. Trends and significance of VRE colonization in the ICU: a Meta-analysis of published studies. PLoS ONE. 2013;8(9):e75658–e.
Armand-Lefevre L, Angebault C, Barbier F, Hamelet E, Defrance G, Ruppe E, et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013;57(3):1488–95.
McConville TH, Sullivan SB, Gomez-Simmonds A, Whittier S, Uhlemann AC. Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS ONE. 2017;12(10):e0186195.
Corbella X, Pujol M, Ayats J, Sendra M, Ardanuy C, Dominguez MA, et al. Relevance of digestive tract colonization in the epidemiology of nosocomial infections due to multiresistant Acinetobacter baumannii. Clin Infect Dis. 1996;23(2):329–34.
Munck C, Sheth RU, Cuaresma E, Weidler J, Stump SL, Zachariah P, et al. The effect of short-course antibiotics on the resistance profile of colonizing gut bacteria in the ICU: a prospective cohort study. Crit Care. 2020;24(1):404.
Jee W, Jo S, Lee JB, Jin Y, Jeong T, Yoon JC, et al. Mortality difference between early-identified sepsis and late-identified sepsis. Clin Exp Emerg Med. 2020;7(3):150–60.
Oami T, Imaeda T, Nakada TA, Abe T, Takahashi N, Yamao Y, et al. Mortality analysis among sepsis patients in and out of intensive care units using the Japanese nationwide medical claims database: a study by the Japan Sepsis Alliance study group. J Intensive Care. 2023;11(1):2.
Ochotorena E, Hernandez Morante JJ, Canavate R, Villegas RA, Viedma I. Methicillin-Resistant Staphylococcus aureus and other Multidrug-Resistant Colonizations/Infections in an intensive care unit: predictive factors. Biol Res Nurs. 2019;21(2):190–7.
Fouda R, Soliman MS, ElAnany MG, Abadeer M, Soliman G. Prevalence and risk factors of MRSA, ESBL and MDR bacterial colonization upon admission to an Egyptian medical ICU. J Infect Dev Ctries. 2016;10(4):329–36.
Terry MA, Freedberg DE, Morris MC. An alternative consent process for minimal risk research in the ICU. Crit Care Med. 2017;45(9):1450–6.
Barie PS, Hydo LJ, Fischer E. Comparison of APACHE II and III scoring systems for mortality prediction in critical surgical illness. Arch Surg. 1995;130(1):77–82.
Kruse JA, Thill-Baharozian MC, Carlson RW. Comparison of clinical Assessment with APACHE II for Predicting Mortality risk in patients admitted to a medical Intensive Care Unit. JAMA. 1988;260(12):1739–42.
Tosi M, Roat E, De Biasi S, Munari E, Venturelli S, Coloretti I et al. Multidrug resistant bacteria in critically ill patients: a step further antibiotic therapy. J Emerg Crit Care Med. 2018;2.
Pop-Vicas A, Strom J, Stanley K, D’Agata EM. Multidrug-resistant gram-negative bacteria among patients who require chronic hemodialysis. Clin J Am Soc Nephrol. 2008;3(3):752–8.
Macesic N, Gomez-Simmonds A, Sullivan SB, Giddins MJ, Ferguson SA, Korakavi G, et al. Genomic Surveillance Reveals Diversity of Multidrug-Resistant Organism Colonization and infection: a prospective cohort study in liver transplant recipients. Clin Infect Dis. 2018;67(6):905–12.
Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18(4):657–86.
Bar-Yoseph H, Hussein K, Braun E, Paul M. Natural history and decolonization strategies for ESBL/carbapenem-resistant Enterobacteriaceae carriage: Systematic review and meta-analysis. Journal of Antimicrobial Chemotherapy: Oxford University Press; 2016. p. 2729-39.
Haverkate MR, Derde LPG, Brun-Buisson C, Bonten MJM, Bootsma MCJ. Duration of colonization with antimicrobial-resistant bacteria after ICU discharge. Intensive Care Med. 2014;40(4):564–71.
Jones AE, Brown MD, Trzeciak S, Shapiro NI, Garrett JS, Heffner AC, et al. The effect of a quantitative resuscitation strategy on mortality in patients with sepsis: a meta-analysis. Crit Care Med. 2008;36(10):2734–9.
Zhou MJ, Li J, Salmasian H, Zachariah P, Yang YX, Freedberg DE. The local hospital milieu and healthcare-associated Vancomycin-resistant enterococcus acquisition. J Hosp Infect. 2019;101(1):69–75.
Thompson DS. Methicillin-resistant Staphylococcus aureus in a general intensive care unit. J R Soc Med. 2004;97(11):521–6.
Jolivet S, Lolom I, Bailly S, Bouadma L, Lortat-Jacob B, Montravers P, et al. Impact of colonization pressure on acquisition of extended-spectrum β-lactamase-producing enterobacterales and meticillin-resistant Staphylococcus aureus in two intensive care units: a 19-year retrospective surveillance. J Hosp Infect. 2020;105(1):10–6.
Bloemendaal ALA, Fluit AC, Jansen WMT, Vriens MR, Ferry T, Argaud L, et al. Acquisition and Cross-transmission of Staphylococcus aureus in European Intensive Care Units. Infect Control Hosp Epidemiol. 2009;30(2):117–24.
Harris AD, Kotetishvili M, Shurland S, Johnson JA, Morris JG, Nemoy LL, et al. How important is patient-to-patient transmission in extended-spectrum β-lactamase Escherichia coli acquisition. Am J Infect Control. 2007;35(2):97–101.
Ajao AO, Johnson JK, Harris AD, Zhan M, McGregor JC, Thom KA, et al. Risk of acquiring extended-spectrum β-lactamase-producing Klebsiella species and Escherichia coli from prior room occupants in the intensive care unit. Infect Control Hosp Epidemiol. 2013;34(5):453–8.
Acknowledgements
Not applicable.
Funding
Dr. Freedberg was funded in part by the Department of Defense (PR181960) and by NIAID R01 AI132.
Author information
Authors and Affiliations
Contributions
LS: Formal analysis, interpretation of patient data regarding gut colonization and clinical outcomes, major contributor in writing the manuscript, prepared tables and figures.MH: review and editing. EL: data collection. DAG: review and editing. AGS: Review and editing. DF: conceptualization, methodology, review and editing, supervision, and funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Columbia University Institutional Review Board (IRB #AAAS2583).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shamalov, L., Heath, M., Lynch, E. et al. Timing and clinical risk factors for early acquisition of gut pathogen colonization with multidrug resistant organisms in the intensive care unit. Gut Pathog 16, 10 (2024). https://doi.org/10.1186/s13099-024-00605-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-024-00605-z