Abstract
Background
Obesity remains a public health problem worldwide. The high prevalence of this condition in the population raises further concerns, considering that comorbidities are often associated with obesity. Among the comorbidities closely associated with obesity, metabolic syndrome (MS) is particularly important, which potentially increases the risk of manifestation of other disorders, such as the prothrombotic and systemic pro-inflammatory states.
Methods
A randomized, controlled clinical trial was performed involving female patients (n = 32) aged between 18 and 65 years, with a clinical diagnosis of MS, with severe obesity undergoing Roux-en-Y gastric bypass (RYGB). The study design followed the Consolidated Standards of Reporting Trials statement (CONSORT). Lipid profile, blood glucose and adipokines (adiponectin, leptin, and resistin) and (cytokines IL-1β, IL-6, IL-17, IL-23, and TNF-α) in blood plasma samples were evaluated before and six months after RYGB.
Results
Patients undergoing RYGB (BSG) showed a significant improvement from preoperative grade III obesity to postoperative grade I obesity. The results showed that while HDL levels increased, the other parameters showed a significant reduction in their postoperative values when compared not only to the values observed before surgery in the BSG group, but also to the values obtained in the control group (CG). As for systemic inflammatory markers adiponectin, leptin, resistin, IL-1β, IL-6, IL-17, IL-23 and TNF- α it was observed that the levels of resistin and IL-17 in the second evaluation increased significantly when compared to the levels observed in the first evaluation in the CG. In the BSG group, while the levels of adiponectin increased, the levels of the other markers showed significant reductions in the postoperative period, in relation to the respective preoperative levels. The analysis of Spearman’s correlation coefficient showed a significant positive correlation between IL-17 and IL-23 in the preoperative period, significant positive correlations between TNF-α and IL-6, TNF-α and IL-17, IL-6 and IL-17, and IL-17 and IL-23 were observed postoperatively.
Conclusions
According to our results, the reduction of anthropometric measurements induced by RYGB, significantly improves not only the plasma biochemical parameters (lipid profile and glycemia), but also the systemic inflammatory status of severely obese patients with MS.
Trials registration NCT02409160
Similar content being viewed by others
Background
Obesity remains a public health problem worldwide. Its prevalence has been increasing globally in recent decades, even in developing countries. According to the World Health Organization (WHO), in 2016, the global prevalence of overweight adults over the age of 18 years was approximately 1.9 billion, of which 38% were men and 40% were women, and 650 million were obese (13%). The high prevalence of this condition in the population raises further concerns, considering that comorbidities are often associated with obesity [1, 2].
Among the comorbidities closely associated with obesity, metabolic syndrome (MS) is particularly important, which potentially increases the risk of manifestation of other disorders, such as the prothrombotic and systemic pro-inflammatory states [3, 4]. In addition, the prolonged high glucose levels that are associated with MS, induce a prolonged stimulation of the pancreas to release insulins, causing insulin resistance and type 2 diabetes mellitus (DM2). Moreover, increases in the arterial blood pressure, circulating triglycerides (TG), and interleukin-6 (IL-6)—an inflammatory cytokine—have been observed, which may contribute to a pro-inflammatory state and increase the risk of cardiovascular disease [5].
It is widely accepted that both a chronic low-grade inflammation and the immune system are important factors in obesity. A significant infiltration of leukocytes, particularly macrophages, can be observed in the tissues with altered profiles, leading to a pro-inflammatory state and consequent increase in systemic inflammation [6]. In addition to the increased levels of inflammatory cytokines, such as IL-6 and tumor necrosis factor-alpha (TNF-α), the production or release of other adipose tissues, especially visceral, leads to the production of or release from other tissues by the adipocyte itself, commonly known as adipokines, which contribute to the development of insulin resistance and atherosclerosis. Obesity imposes a particular condition and the release of adiponectin, a molecule with pro-inflammatory properties, in contrast to the increased production and release of leptin and resistin, which involves the production and two reactions, by the lesser role of adipose tissue, improving and accentuating the manifestation of low-grade chronic inflammation associated with obesity and MS [7].
Consequently, certain non-invasive approaches, such as changes in pharmacological treatment, lifestyle, dietary re-education, combinations, and modifications, are used to minimize, or even reverse obesity and MS [8, 9]. With the evolution of surgical techniques and procedures, bariatric surgery has proven to be an effective and safe approach to improve the patient's overall clinical condition. Bariatric surgery is currently the most widely used therapeutic option for severe MS and among MS patients, the Roux-en-Y gastric bypass (RYGB) procedure is particularly important; a surgical procedure that is characterized by a restriction and lower absorption, owing to a small gastric pouch and a total bypass of the duodenum and proximal jejunum [10,11,12]. It is worth noting that reducing body weight using bariatric surgery is effective in decreasing the severity of chronic inflammation, and therefore, the development of comorbidities associated with obesity [13].
Therefore, to understand the benefit of bariatric surgery by RYGB in women with severe obesity and MS, whose inflammatory profile (adiponectin, resistin, leptin, TNF-α, IL-1β, IL-6, IL-17, and IL-23) is available, an improvement in the understanding and description of the changes in the group of parameters before and after the surgery in this population is extremely important for clinical practice. The main objective of this study was to verify the effects of weight loss induced by RYGB on the circulating levels of systemic inflammatory markers adiponectin, resistin, leptin, TNF-alpha, IL1-beta interleukins, IL-6, IL-8, IL-17, IL-23 and IGF-1 in women with severe obesity and MS.
Methods
Study participants
We conducted a randomized, controlled, clinical trial at the Faculty of Medical Sciences of Santa Casa de São Paulo. We recruited female patients (n = 32) aged between 18 and 65 years, with a clinical diagnosis of MS and severe obesity (Body mass index (BMI) ≥ 40 kg/m2 or 35–39.9 kg/m2 associated with comorbidities) who were eligible for bariatric surgery. The exclusion criteria were clinical and/or mental instability, BMI > 55 kg/m2, unrealistic postoperative target weight and/or unrealistic expectations regarding surgical treatment, active cancer, pregnancy, lactation, or planning pregnancy within 2 years, and a diagnosis of psychiatric disorders (schizophrenia or depression).
Recruitment, randomization and sample size
The recruitment was performed at the obesity surgery outpatient clinic of Santa Casa de Misericórdia de São Paulo from January to December 2019. All the recruited volunteers signed a free and informed consent form that was previously approved by the National Ethics Committee in Research with Human Beings of Santa Casa de Misericórdia (Process number 178/2012) and registered in ClinicalTrials.gov NCT02409160. The study was conducted in accordance with the Regulatory Norms for Research Involving Human Subjects of the National Health Council of the Ministry of Health, RESOLUTION No. 466, on December 12, 2012 [14]. The study design followed the CONSORT (CONsolidated Standards of Reporting Trials) [15], as shown in Fig. 1.
The sample size was determined using G-Power software (version 3.1.2—Universitat Kiel, Germany), with an α error of 0.05 and power of 1−β error = 0.95. Based on the study of Freitas Jr. et al. [16], who studied plasma TNF-α levels in severely obese patients before and after bariatric surgery, an arbitrary moderate effect size (Cohen's d) of 0.8 was assumed, and with the calculation using a difference between two dependent means (matched pairs) t-test, the total sample size was 19 for BSG. In addition, since the CG did not show any differences in the same study assessed and that the main endpoint was evaluating the effect of bariatric surgery, we assumed that a group of 11 volunteers could be useful to perform this study [16].
All patients involved in this study were randomly allocated to the surgery and control groups. Because they were patients of the same gender and were composed of only two groups, the simple randomization procedure was adopted through a numerical sequence generated by computer in the proportion of 2:1. The consecutively generated numbers that indicated the assignment for each group were placed in sealed envelopes, later opened by the patient and stored by a research assistant. This entire process was carried out by a research assistant, avoiding the participation of researchers involved in the study. The statistician was also unaware of the composition of the data sheet.
Clinical assessment
All volunteers were initially evaluated to obtain data regarding medical and surgical history, concomitant medications, demographic data, and anthropometric measurements. Blood samples were collected for biochemical analyses and inflammatory markers. All patients involved in the study had a confirmed clinical diagnosis of metabolic syndrome due to severe obesity. Thereafter, the volunteers who did not undergo bariatric surgery were a part of the control group (CG, n = 11), and those who underwent RYGB were allocated to the bariatric surgery group (BSG, n = 21). The CG volunteers were instructed to maintain their routine, especially regarding physical activities and eating habits, and to inform the researchers of any changes in their routine. A second evaluation was performed, and blood samples were collected 6 months after the first evaluation in the CG or 6 months after the bariatric surgery in the BSG group. All assessments were performed by the same team of researchers, physicians, and physical therapists.
Bariatric surgery
All procedures related to bariatric surgery followed the previous description presented by Freitas et al. [16]. Briefly, all patients were operated on by three surgeons who alternated between being the surgeon and two assistants in each surgery. After general anesthesia, the patients were placed in the supine position with a sequential compression device for prophylaxis against deep vein thrombosis. The abdominal incision was marked, starting 2 cm below the xiphoid process and extending to 7 cm above the umbilicus. The surgery was performed by RYGB reconstruction, with a small Capella-type bag with gastrointestinal anastomosis in two sutures, one with continuous 4–0 Vicryl and the other with 3–0 seromuscular cotton sutures, with lateral anastomosis (1.5 cm in diameter). Silastic rings were not placed. The alimentary loop was 100 cm long, and the biliopancreatic loop was 70 cm long with 3–0 Vicryl, with lateral enteroanastomosis (4 cm in diameter) with continuous sutures in two layers.
Blood sampling
Venous blood samples (5 mL) were collected after 12 h of fasting, through cubital venipuncture and collected in vacuum tubes (Vacuette do Brasil Ltda, Campinas, Brazil) with ethylenediaminetetraacetic acid anticoagulant (EDTA K3) to obtain plasma after centrifugation for 10 min at 2000 rpm. The samples were collected at baseline and 6 months after the first evaluation in the CG and 6 months after the surgery in the BSG group.
Determination of lipid profile and glycemia
Plasma concentrations of total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), TG, and glucose were determined using commercial kits (Gold Análise Diagnostica Ltda, MG, Brazil) and the SpectraMax i3 system (Molecular Devices, Sunnyvale, CA, USA).
Determination of inflammatory parameters
Plasma concentrations of adipokines (adiponectin, leptin, and resistin) and cytokines (IL-1β, IL-6, IL-17, IL-23, and TNF-α) were determined using commercial enzyme-linked immune-assay kits (R&D Systems, Minneapolis, MN, USA), BioLegend (Sellex Inc., Washington, DC, USA), and Invitrogen (Thermo Fisher Scientific, Massachusetts, MA USA), according to the manufacturer's recommendations. The concentration of each parameter was calculated using an appropriate standard curve (according to the manufacturer’s instructions). The correlation coefficients of all standard curves ranged from 0.95 to 0.99, while the intra-assay coefficients of variance ranged from 3 to 5%, and the inter-assay coefficients of variance ranged from 8 to 10%.
Statistical analysis
Initially, the data obtained were evaluated for normality using the Shapiro–Wilk D'Agostino, and Pearson tests, and variance homogeneity was analyzed using the Levene’s test. The parameters that showed a normal distribution (parametric data) were presented as mean and standard deviation, and the difference between the means of these variables was evaluated using the Student’s t-test. One-way analysis of variance with Dunn’s post-test was used to compare the variables in the CG and BSG group. Pearson’s correlation test was used to analyze possible trends and product-moment correlations.
The parameters that deviated from the normal distribution (non-parametric data) were presented as median and interquartile range, and the difference between their values was evaluated using the Wilcoxon test. In addition, the Friedman test was used to compare the variables obtained in the CG and BSG group. The Spearman correlation test was used to analyze possible trends and product-moment correlations. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS 21.0®, Chicago, Illinois, USA). The significance level was set at 5% for all tests (p < 0.05).
Results
Table 1 presents the anthropometric characteristics of the volunteers involved in this study, who were divided into two groups, CG (n = 11) and BSG (n = 21). During the development of this clinical trial, eight patients were lost to follow-up in the control group and six in the experimental group. This loss is justified in the control group since these patients obtained surgical procedures in other hospitals. Regarding the patients in the bariatric surgery group, six patients were lost to follow-up because they refused to return to the hospital for postoperative examinations. Despite the follow-up losses, the number of patients involved in the final analysis exceeded the sample size, not affecting data analysis. The mean age of the volunteers in both the groups was similar (42 years), and all of them weighed more than 110 kg with grade III obesity. When analyzing the impact of significant weight loss and BMI reduction in the volunteers from the BSG group after surgery and comparing them to the pre-surgery values, it was shown that the difference between the BMI values in the CG and BSG group was initially 0.75 ± 0.34 (first assessment), which increased to 13.73 ± 0.6 after surgery (second assessment). Based on these observations, the volunteers in the BSG group showed a significant improvement from grade III obesity preoperatively to grade I postoperatively.
Table 2 shows the plasma levels of TC and its fractions (LDL, HDL, and TG), and blood glucose levels obtained in the first and second evaluations in the CG volunteers. These times corresponded to the pre- and post-bariatric surgery for the volunteers in the BSG group. The results showed that while HDL levels increased, the other parameters showed a significant reduction in their values in the postoperative period when compared not only to the values observed before the surgery in the BSG group, but also to the values obtained in the CG.
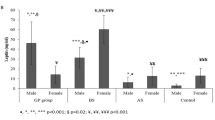
Figure 2 shows the results of the evaluation of systemic inflammatory markers adiponectin (A), leptin (B), resistin (C), IL-1β (D), IL-6 (E), IL-17 (F), IL-23 (G), and TNF-α) in the volunteers who participated in the study in the two groups, CG and BSG. The results showed that the levels of resistin (B) and IL-17 (F) in the second evaluation significantly increased when compared to the levels observed in the first evaluation in the CG. In the BSG group, while adiponectin (A) levels reduced, the levels of the other markers showed statistically significant reductions postoperatively, compared to the respective preoperative levels. Furthermore, in the inter-group analysis, it was found that IL-23 (G) levels in the BSG group preoperatively were significantly higher than those in the CG. The levels of adiponectin (A) were higher, while the levels of leptin (B), resistin (C), IL-17 (F), IL-23 (G), and TNF-α (H) were lower in the BSG group postoperatively than in the CG.
Table 3 presents the results of the Spearman correlation coefficient analysis for the groups of volunteers participating in this study. In the CG, no significant correlation was found at any of the studied time-points. With regard to the BSG group, while a significant positive correlation between IL-17 and IL-23 was observed preoperatively, significant positive correlations between TNF-α and IL-6, TNF-α and IL-17, IL-6 and IL-17, and IL-17 and IL-23 were observed postoperatively.
Discussion
Our results showed that patients with severe obesity and MS who underwent bariatric surgery using the RYGB technique had an improvement in all anthropometric, biochemical, and inflammatory parameters when compared to patients with the same conditions who did not undergo surgery. Interestingly, significant positive correlations were observed between the evaluated cytokines only after the bariatric surgery.
The accumulation of body fat is associated not only with aging, but also with the adoption of sedentary behaviors and the intake of hypercaloric foods which, over time, induce a natural reduction in metabolism and hormonal changes that can substantially contribute to the increase in the adiposity levels in the body [17].
The increase in body weight associated with the accumulation of abdominal fat in women may also be promoted by menopause. The cessation of ovarian function causes a reduction in metabolism, lean body mass, and energy expenditure in physical exercise, in addition to causing greater accumulation of fat in the adipose tissue. These conditions together contribute to a higher risk of obesity and the development of cardiovascular diseases in women [18].
Pontiroli and Morabito reported in a meta-analysis that patients undergoing bariatric surgery not only have reduced long-term mortality, but also a reduced risk of mortality from cardiovascular diseases [19] Corroborating this information, Yan et al. reiterated in their systematic review and meta-analysis that bariatric surgery using the RYGB technique promotes the reversal of DM2 in the short and medium- terms, improves the metabolic state, and reduces cardiovascular risk factors [20]. A study conducted on 47 obese women who underwent RYGB technique, demonstrated a considerable decrease in fasting blood glucose from 119.0 mg/dL to 94.6 mg/dL at 3 months and to 86.2 mg/dL at 12 months postoperatively [21]. This can be explained by the reduced length between the stomach and the intestine and increased production of incretins in anticipation of food in the terminal ileum, which regulates glucose metabolism by inhibiting insulin secretion [22]. Therefore, this corroborates with our findings of a significant reduction in circulating glucose levels in patients in the BSG group postoperatively.
Similarly, bariatric surgery with RYGB also showed a remarkable ability to reverse dyslipidemia and obesity. A systematic review and meta-analysis by Carswell et al. [23] reported that, in 7815 individuals undergoing RYGB, there was a significant reduction in plasma levels of TC, LDL, and TG (p < 0. 0.00001, p < 0.00001, and p < 0.00001, respectively) 1–3 months postoperatively. Conversely, plasma HDL levels increased after RYGB, especially after one year (p < 0.00001) [23]. Therefore, both the reduction in TC, LDL, and TG levels, and the increase in HDL levels observed in patients in the BSG group in our study corroborate with the data reported in this review.
As previously mentioned, RYGB promotes the reversal of dyslipidemia and obesity. Interestingly, obesity or excess fat in the adipose tissue, was identified as a metabolically active state in 2005; adipose tissue is considered a secretory organ and responsive to modulating signals such as appetite, energy balance, insulin sensitivity, reproduction, endocrine function, bone metabolism, immunity, and inflammation. [24].
The adipose tissue of obese individuals shows a marked infiltration by macrophages that promote the increased production and secretion of various pro-inflammatory mediators, thus characterizing the inflammation associated with obesity [25]. Thus, obesity is already established in the scientific literature as a low-grade inflammatory state called “Inflammome” characterized by chronic increases in the circulating levels of inflammatory markers [26]. A typical pattern of inflammation originates from the adipose tissue, which is consistent with the association between inflammatory markers and central adiposity [21, 22].
Among the various pro-inflammatory molecules associated with obesity and MS, leptin is particularly important, which is also a marker of long-term energy stores. Interestingly, both leptin and another molecule, resistin correlate with other inflammatory markers of obesity, independent of BMI [27]. Studies have also identified a close interrelationship between leptin and TNF-α, since the latter induces the production of leptin, which in turn, induces the production of TNF-α by macrophages infiltrating the adipose tissue [28, 29]. In contrast to the pro-inflammatory action of leptin, adiponectin has anti-inflammatory activities, although its interaction with TNF-α is still unclear [30].
It is widely accepted that adiponectin, which is produced and secreted preferentially by adipocytes, has remarkable anti-inflammatory and antiatherogenic properties, and is also capable of modulating glucose metabolism [31, 32]. In the context of RYGB surgery, the postoperative circulating levels of adiponectin increase in conjunction with the improved insulin sensitivity and reduced blood pressure [33,34,35]. Moreover, while adiponectin levels rise after RYGB, circulating leptin levels decrease [36].
Studies have shown significantly reduced levels of leptin in patients after RYGB surgery compared with the levels before surgery [37, 38] in individuals with normal weight [39], overweight [40], and obese individuals. [41,42,43]. Furthermore, lower leptin levels after RYGB correlate with significant reductions in body weight, body fat [44], and BMI [45, 46].
Therefore, these reports on adiponectin and leptin in patients undergoing RYGB surgery corroborate our results. Serum adiponectin levels significantly increased and leptin levels significantly reduced postoperatively when compared to the preoperative values and the values observed in the CG.
Resistin is another important molecule produced by the adipose tissue in inflammation [47, 48]. Studies have shown that, in humans, resistin has autocrine, paracrine, and endocrine actions, which affect a wide range of cell and tissue types [49, 50]. Further, the circulating level of resistin is positively associated with inflammatory biomarkers such as TNF-α, IL-1β, and IL-6, and diseases such as DM2 and atherosclerosis. [51] Studies have shown that circulating levels of resistin increase significantly with increasing BMI [52] and that obese patients have higher resistin levels than non-obese individuals [46].
Circulating levels of resistin are not generally altered after bariatric surgery [53]. However, a significant reduction in resistin levels was observed in patients with substantial weight loss [54]. For example, obese patients whose BMI reduced by approximately 50% after bariatric surgery showed significant improvement in resistin, leptin, and IL-6 levels, an increase in adiponectin, and increased insulin sensitivity [55]. Interestingly, our findings contribute to the data in the context of obesity and bariatric surgery, as they demonstrated that over time, resistin levels significantly increased in patients in the CG, which may indicate a worsening of their condition leading to adverse consequences. Conversely, patients who underwent RYGB surgery showed a significant reduction in circulating resistin levels, which may reflect a better inflammatory state in these patients. Corroborating this improvement in the inflammatory status in patients after RYGB surgery, together with the reduction in resistin levels, we also observed a decrease in the levels of pro-inflammatory molecules such as IL-1β, IL-6, IL-17, IL-23, and TNF-α.
In the context of obesity and MS, TNF-α is secreted by macrophages from the stromal vascular tissue associated with adipose tissue. TNF-α is a pro-inflammatory factor that plays a crucial role in the pathogenesis of insulin resistance. Persistently high levels of TNF-α cause phosphorylation of substrate-1 of the insulin receptor, preventing its pairing. Consequently, it prevents the signal generated by the binding of insulin to the surface receptor from activating the translocation of GLUT-4 to the membrane, especially in muscle and liver cells [56, 57].
Thus, the reduction in the circulating levels of TNF-α observed postoperatively in the BSG group after bariatric surgery with RYGB, when compared to their preoperative values and those in the CG, might have induced the normalization of blood glucose levels, thus favoring the reversal of DM2 by reducing its adverse effects on the activation of anti-Glucose transporter (GLUT-4).
Similarly, IL-17, another pro-inflammatory cytokine related to the immune profile, known as IL-17 producing T cells (Th17), is also significantly reduced after RYGB surgery [58]. Studies have reported that obese individuals, especially those with DM2, have high systemic levels of Th17 cytokines, especially IL-17.[59,60,61]. In addition to macrophages, the adipose tissue of obese individuals with insulin resistance shows a marked presence of T-cell populations that produce pro-inflammatory cytokines, such as IL-17, and this infiltration by T-cells increases with the degree of adiposity [58, 62]. Additionally, both IL-17 and IL-1β can promote insulin resistance in adipocytes and favor the development of DM2 in obese individuals [58, 63]. Owing to its prominent association with obesity and insulin resistance, IL-17 has also been the subject of studies in the context of RYGB surgery, with significant reduction postoperatively [64,65,66], further corroborating our findings.
To confirm that RYGB surgery has a remarkable ability to modulate the Th17 profile, we also evaluated the serum levels of IL-23, which is a promoter molecule in the Th17 profile [67]. Serum levels of IL-23 significantly reduced after surgery, which corroborates with other studies that found a decrease in IL-23 levels after bariatric surgery in patients with insulin resistance, particularly in the context of RYGB surgery [64, 67, 68]. We also found a positive correlation between the serum levels of IL-17 and IL-23 both before and after surgery in the BSG group, which reiterates the reports in literature regarding the production and concomitant action of these molecules. However, similar findings were not observed in the CG, which suggests that under certain unclear conditions, the development and presence of MS can deregulate this profile.
Increased levels of IL-1β are also related to insulin resistance and obesity [58, 69] and according to Maddur et al. IL-1β may act as the main regulator of the Th17 profile expansion in humans [70]. Contrary to our findings, recent studies that evaluated the modulation of IL-1β levels in the context of RYGB surgery showed no change in the levels of this pro-inflammatory cytokines after surgery [69, 71, 72]. Thus, our findings highlight that obese women who manifest MS may benefit from RYGB bariatric surgery, with a plausible reduction in insulin resistance.
IL-6 has pro-inflammatory properties and a significant positive correlation with abdominal adiposity. [73] It also plays an important role in the pathogenesis of atherosclerosis, insulin resistance, and DM2 [74, 75]. Therefore, lower levels of IL-6 are associated with a decrease in several metabolic parameters, such as fasting blood glucose, TG, and glycosylated hemoglobin, an increase in HDL, and consequently, an improvement in cardiovascular risk [72]. Although it has been reported that IL-6 levels did not change at 6 months after surgery [71] as in our study, some studies have however, reported significant postoperative reductions of this cytokine after RYGB surgery [44, 71, 76]. This may be related to weight loss in these patients since the significant decrease in IL-6 levels after bariatric surgery was associated with a reduction of more than 50% in BMI [55]. These data corroborate with our observations of a significant reduction in IL-6 levels in the BSG group post operatively compared to only their preoperative levels, but not the levels in the CG, since the decrease in BMI did not reach 50% after the surgery.
Finally, it is important to mention that the BSG group showed significant positive correlations between certain cytokines after RYGB, which was not observed preoperatively. This finding shows that the beneficial metabolic changes resulting from the surgery might have promoted the restoration of inflammatory responses previously altered by obesity and MS. Corroborating this suggestion, the CG showed no correlation between the evaluated cytokines, both in the first and second evaluations, suggesting that the development of obesity and the manifestation of MS results in an individual pattern of systemic inflammation; therefore, correlations between these molecules may be difficult to determine.
Study limitations
In order to generalize the clinical findings of this study to the general population, we must consider a limitation in the selection process of the patients involved. At the beginning of the study, in the enrollment phase, patients of both genders were invited to participate in this clinical trial. However, the number of male patients was much smaller when compared to the number of female patients, which could compromise the statistical analysis. In this sense, we chose to analyze data only from women with severe obesity undergoing RYBS-type bariatric surgery. Given this situation, we hope in the near future to present new clinical data from male patients with severe obesity undergoing RYBS and to compare the outcomes with female patients. Another limitation of the study was the fact that the study was blind only to the statistician who processed the data. Due to the intervention being a major surgery, the researchers could not be blinded to the results, as from an ethical point of view it would not be permissible to use a Sham group.
In contrast to this limitation, it can be highlighted as a strong point that a controlled, randomized study was conducted, where the number of patients involved in the final analysis of the data exceeded the sample calculation performed previously.
Conclusions
According to our results, the reduction of anthropometric measurements, such as body weight and BMI, induced by bariatric surgery with RYGB, significantly improves not only the plasma biochemical parameters (lipid profile and glycemia), but also the systemic inflammatory status of severely obese patients with MS.
Availability of data and materials
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MS:
-
Metabolic syndrome
- DM2:
-
Type 2 diabetes mellitus
- TG:
-
Triglycerides
- IL-6:
-
Interleukin-6
- TNF-α:
-
Tumor necrosis factor-alpha
- RYGB:
-
Roux-en-Y gastric bypass
- BMI:
-
Body mass index
- CG:
-
Control group
- BSG:
-
Bariatric surgery group
- TC:
-
Total cholesterol
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
References
WHO. Obesity: preventing and managing the global epidemic. World Health Organization, Geneva: Report of a WHO Consultation; 2016.
WHO (World Health Organization). 2018 Obesity and overweight. Key facts. Fact sheet no. 311. http://www.who.int/mediacentre/factsheets/fs311/en/index.html. Acesso em 05 Feb 2022
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). 2002 Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 106(25):3143–421. PMID: 12485966.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Robert H, Barry AE, et al. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005;112(17):2735–52.
Hayden MR, Tyagi SC. Isolated low high density lipoprotein-cholesterol (HDL-C): implications of global risk reduction. Case report and systematic scientific review. Cardiovasc Diabetol. 2005. https://doi.org/10.1186/1475-2840-4-1.
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):141–50.
Kumari R, Kumar S, Kant R. An update on metabolic syndrome: Metabolic risk markers and adipokines in the development of metabolic syndrome. Diabetes Metab Syndr. 2019;13(4):2409–17.
Zujko ME, Rożniata M, Zujko K. Individual diet modification reduces the metabolic syndrome in patients before pharmacological treatment. Nutrients. 2021;13(6):2102.
Lim S, Eckel RH. Pharmacological treatment and therapeutic perspectives of metabolic syndrome. Rev Endocr Metab Disord. 2014;15(4):329–41.
Aelfers S, Janssen IMC, Arte OE, et al. Doença inflamatória intestinal não é contraindicação para cirurgia bariátrica. Obes Surg. 2018;28:1681–7.
Short S, Shahabuddin Hoseini S, Naderan M, et al. 2017 Cirurgia bariátrica em pacientes obesos mórbidos com doença inflamatória intestinal uma revisão sistemática.Surg Obes Relat Dis. 13: 652–59.
Ikramuddin S, Kendrick ML, Kellogg TA, Sarr MG. Open and laparoscopic Roux-en-Y gastric bypass: our techniques. J Gastrointest Surg. 2007;11(2):217–28.
de Sousa ART, Freitas Junior WR, Perez EA, Ilias EJ, Silva AS, Alves VLS, et al. Surgery for obesity and weight-related diseases changes the inflammatory profile in women with severe obesity: a randomized controlled clinical trial. Obes Surg. 2021;31(12):5224–36.
da Saúde M. 2012 RESOLUÇÃO Nº 466. Normas Reguladoras para Pesquisas Envolvendo Seres Humanos do Conselho Nacional de Saúde. Disponível em: https://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf. Citado 30 Jun 2022
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11:32.
Freitas WR Jr, Oliveira LVF, Perez EA, Ilias EJ, Lottenberg CP, Silva AS, et al. Systemic inflammation in severe obese patients undergoing surgery for obesity and weight-related diseases. Obes Surg. 2018;28(7):1931–42.
Yadav R, Hama S, Liu Y, Siahmansur T, Schofield J, Syed AA, et al. Effect of Roux-en-Y bariatric surgery on lipoproteins, insulin resistance, and systemic and vascular inflammation in obesity and diabetes. Front Immunol. 2017;8:1512.
França AP, Aldrighi JM, Marucci MFN. Factors associated with body and abdominal obesity in post-menopausal women. Rev Bras Saúde Matern Infant. 2008;8(1):65–73.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. a systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253(3):484–7.
Yan Y, Sha Y, Yao G, Wang S, Kong F, Liu H, et al. Roux-en-Y gastric bypass versus medical treatment for type 2 diabetes mellitus in obese patients: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95(17):e3462.
Carvalho PS, Moreira CL, Barelli MD, Oliveira FH, Guzzo MF, Miguel GP, et al. Cirurgia bariátrica cura síndrome metabólica? Arquivos Brasileiros de Endocrinologia & Metabologia. 2007;51(1):79–85.
Alves M, Neves C, Medina JL. Incretinas e Tratamento da Diabetes. Revista Portuguesa de Diabetes. 2007;2(4):22–5.
Carswell KA, Belgaumkar AP, Amiel SA, Patel AG. A Systematic review and meta-analysis of the effect of gastric bypass surgery on plasma lipid levels. Obes Surg. 2015;26(4):843–55.
Rao SR. Inflammatory markers and bariatric surgery: a meta-analysis. Inflamm Res. 2012;61(8):789–807.
Nieto-Vazquez I, Fernández-Veledo S, Krämer DK, Vila-Bedmar R, Garcia-Guerra L, Lorenzo M. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114(3):183–94.
Prevedello CF, Colpo E, Mayer ET, Copetti H. Análise do impacto da cirurgia bariátrica em uma população do centro do estado do Rio Grande do Sul utilizando o método BAROS. Arq Gastroenterol. 2009;46(3):199–203.
Finck BN, Johnson RW. Tumor necrosis factor (TNF)-alpha induces leptin production through the p55 TNF receptor. Am J Physiol Regul Integr Comp Physiol. 2000;278:R537–43.
Zhao T, Hou M, Xia M, Wang Q, Zhu H, Xiao Y, et al. Globular adiponectin decreases leptin-induced tumor necrosis factor-alpha expression by murine macrophages: involvement of cAMP-PKA and MAPK pathways. Cell Immunol. 2005;238(1):19–30.
Ouchi N, Kihara S, Funahashi T, Nakamura T, Nishida M, Kumada M, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003;107(5):671–4.
Mallipedhi A, Prior SL, Barry JD, Caplin S, Baxter JN, Stephens JW. Changes in inflammatory markers after sleeve gastrectomy in patients with impaired glucose homeostasis and type 2 diabetes. Surg Obes Relat Dis. 2014;10(6):1123–8.
Nigro E, Scudiero O, Monaco ML, Palmieri A, Mazzarella G, Costagliola C, et al. New insight into adiponectin role in obesity and obesity-related diseases. Biomed Res Int. 2014;2014:658913.
Ouchi N, Kihara S, Arita Y, Nishida M, Matsuyama A, Okamoto Y, et al. Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation. 2001;103(8):1057–63.
Swarbrick MM, Austrheim-Smith IT, Stanhope KL, Van Loan MD, Ali MR, Wolfe BM, Havel PJ. Circulating concentrations of high-molecular-weight adiponectin are increased following Roux-en-Y gastric bypass surgery. Diabetologia. 2006;49(11):2552–8.
Kopp HP, Krzyzanowska K, Möhlig M, Spranger J, Pfeiffer AF, Schernthaner G. Effects of marked weight loss on plasma levels of adiponectin, markers of chronic subclinical inflammation and insulin resistance in morbidly obese women. Int J Obes. 2005;29(7):766–71.
Sjöström CD, Lissner L, Wedel H, Sjöström L. Reduction in incidence of diabetes, hypertension and lipid disturbances after intentional weight loss induced by bariatric surgery: the SOS intervention study. Obes Res. 1999;7(5):477–84.
Ballantyne GH, Gumbs A, Modlin IM. Changes in insulin resistance following bariatric surgery and the adipoinsular axis: role of the Adipocytokines, leptin. Obes Surg. 2005;5(5):692–9.
Riedl M, Vila G, Maier C, Handisurya A, Shakeri-Manesch S, Prager G, et al. Plasma Osteopontin increases after bariatric surgery and correlates with markers of bone turnover but not with insulin resistance. J Clin Endocrinol Metab. 2008;93(6):2307–12.
Meier CA, Bobbioni E, Gabay C, Assimacopoulos-Jeannet F, Golay A, Dayer JM. IL-1 receptor antagonist serum levels are increased in human obesity: a possible link to the resistance to leptin? J Clin Endocrinol Metab. 2002;87(3):1184–8.
Faraj M, Jones P, Sniderman AD, Cianflone K. Enhanced dietary fat clearance in postobese women. J Lipid Res. 2001;42(4):571–80.
Korner J, Inabnet W, Conwell IM, Taveras C, Daud A, Olivero-Rivera L, et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels*. Obesity. 2006;14(9):1553–61.
Goldfine AB, Mun EC, Devine E, Bernier R, Baz-Hecht M, Jones DB, Schneider BE, Holst JJ, Patti ME. Patients with neuroglycopenia after gastric bypass surgery have exaggerated incretin and insulin secretory responses to a mixed meal. J Clin Endocrinol Metab. 2007;92(12):4678–85.
Stoeckli R, Chanda R, Langer I, Keller U. Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res. 2004;12(2):346–50.
Hickey MS, Pories WJ, MacDonald KG, Cory KA, Dohm GL, Swanson MS, et al. A new paradigm for type 2 diabetes mellitus. Ann Surg. 1998;227(5):637–44.
Swarbrick MM, Stanhope KL, Austrheim-Smith IT, Van Loan MD, Ali MR, Wolfe BM, Havel PJ. Longitudinal changes in pancreatic and adipocyte hormones following Roux-en-Y gastric bypass surgery. Diabetologia. 2008;51(10):1901–11.
Molina A, Vendrell J, Gutiérrez C, Simón I, Masdevall C, Soler J, Gómez JM. Insulin resistance, Leptin and TNF-α system in morbidly obese women after gastric bypass. Obes Surg. 2003;13(4):615–21.
Vendrell J, Broch M, Vilarrasa N, Molina A, Gómez JM, Gutiérrez C, et al. Resistin, adiponectin, ghrelin, leptin, and proinflammatory cytokines: relationships in obesity. Obes Res. 2004;12(6):962–71.
Pories WJ. Why does the gastric bypass control type 2 diabetes mellitus? Obes Surg. 1992;2(4):303–13.
Tripathi D, Kant S, Pandey S, Ehtesham NZ. Resistin in metabolism, inflammation, and disease. FEBS J. 2020;287(15):3141–9.
Marccoli R, Bianchi C, Odoguardi L, Penno G, Caricato F, Giovannitti MG, et al. Prevalence of the metabolic syndrome among Italian adults according to ATP III definition. NutrMetab Cardiovasc Dis. 2005;15:250–4.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Schwartz DR, Lazar MA. Human resistin: found in translation from mouse to man. Trends Endocrinol Metab. 2011;22(7):259–65.
Degawa-Yamauchi M, Bovenkerk JE, Juliar BE, Watson W, Kerr K, Jones R, et al. Serum resistin (FIZZ3) protein is increased in obese humans. J Clin Endocrinol Metab. 2003;88(11):5452–5.
Engin A. Does bariatric surgery improve obesity associated comorbid conditions. Adv Exp Med Biol. 2017;960:545–70.
Edwards C, Hindle AK, Fu S, Brody F. Downregulation of leptin and resistin expression in blood following bariatric surgery. Surg Endosc. 2010;25(6):1962–8.
Marantos G, Daskalakis M, Karkavitsas N, Matalliotakis I, Papadakis JA, Melissas J. Changes in metabolic profile and adipoinsular axis in morbidly obese premenopausal females treated with restrictive bariatric surgery. World J Surg. 2011;35(9):2022–30.
van Dielen FM, van’t Veer C, Schols AM, Soeters PB, Buurman WA, Greve JW. Increased leptin concentrations correlate with increased concentrations of inflammatory markers in morbidly obese individuals. Int J Obes Relat Metab Disord. 2001;25(12):1759–66.
Akash MS, Rehman K, Liaqat A. Tumor necrosis factor-alpha: role in development of insulin resistance and pathogenesis of type 2 diabetes mellitus. J Cell Biochem. 2017;119(1):105–10.
Dalmas E, Venteclef N, Caer C, Poitou C, Cremer I, Aron-Wisnewsky J, et al. T Cell-derived IL-22 amplifies IL-1β–driven inflammation in human adipose tissue: relevance to obesity and type 2 diabetes. Diabetes. 2014;63(6):1966–77.
Sumarac-Dumanovic M, Stevanovic D, Ljubic A, Jorga J, Simic M, Stamenkovic-Pejkovic D, et al. Increased activity of interleukin-23/interleukin-17 proinflammatory axis in obese women. Int J Obes. 2008;33(1):151–6.
Fatima N, Faisal SM, Zubair S, Siddiqui SS, Moin S, Owais M. Emerging role of Interleukins IL-23/IL-17 axis and biochemical markers in the pathogenesis of Type 2 Diabetes: Association with age and gender in human subjects. Int J Biol Macromol. 2017;105:1279–88.
Ip B, Cilfone NA, Belkina AC, DeFuria J, Jagannathan-Bogdan M, Zhu M, et al. Th17 cytokines differentiate obesity from obesity-associated type 2 diabetes and promote TNFα production. Obesity. 2015;24(1):102–12.
Bertola A, Ciucci T, Rousseau D, Bourlier V, Duffaut C, Bonnafous S, Blin-Wakkach C, Anty R, Iannelli A, Gugenheim J, Tran A, Bouloumie A, Gual P, Wakkach A. Identification of adipose tissue dendritic cells correlated with obesity-associated insulin-resistance and inducing Th17 responses in mice and patients. Diabetes. 2012;61(9):2238–47.
Fabbrini E, Cella M, Mccartney SA, Fuchs A, Abumrad NA, Pietka TA, et al. Association between specific adipose tissue CD4+ T-cell populations and insulin resistance in obese individuals. Gastroenterology. 2013;145(2):366–74.
Subramaniam R, Aliakbarian H, Bhutta HY, Harris DA, Tavakkoli A, Sheu EG. Sleeve Gastrectomy and Roux-en-Y gastric bypass attenuate pro-inflammatory small intestinal cytokine signatures. Obes Surg. 2019;29(12):3824–32.
Zhan J, Huang L, Ma H, Chen H, Yang Y, Tan S, et al. Reduced inflammatory responses of follicular helper T cell promote the development of regulatory B cells after Roux-en-Y gastric bypass. Clin Exp Pharmacol Physiol. 2017;44(5):556–65.
Dai X, Zhao W, Zhan J, Zeng S, Ran D, Zhang H, et al. B cells present skewed profile and lose the function of supporting T cell inflammation after Roux-en-Y gastric bypass. Int Immunopharmacol. 2017;43:16–22.
Villarreal-Calderon JR, Cuellar-Tamez R, Castillo EC, Luna-Ceron E, García-Rivas G, Elizondo-Montemayor L. Metabolic shift precedes the resolution of inflammation in a cohort of patients undergoing bariatric and metabolic surgery. Sci Rep. 2021. https://doi.org/10.1038/s41598-021-91393-y.
de Sousa ART, Freitas Junior WR, Perez EA, Ilias EJ, Silva AS, Alves VLS, et al. Surgery for obesity and weight-related diseases changes the: a randomized controlled clinical trial. Obes Surg. 2021;31(12):5224–36.
Hepprich M, Wiedemann SJ, Schelker BL, Trinh B, Stärkle A, Geigges M, Löliger J, Böni-Schnetzler M, Rudofsky G, Donath MY. Postprandial hypoglycemia in patients after gastric bypass surgery is mediated by glucose-induced IL-1β. Cell Metab. 2020;31(4):699–709.
Maddur MS, Miossec P, Kaveri SV, Bayry J. Th17 Cells. Am J Pathol. 2012;181(1):8–18.
Chiappe EL, Martin M, Iglesias Molli A, Millan A, Tetzlaff W, Botta E, et al. Effect of Roux-en-Y gastric bypass on lipoprotein metabolism and markers of HDL functionality in morbid obese patients. Obes Surg. 2021;31(3):1092–8.
Lopes KG, Romagna EC, Silva DS, et al. metabolic and inflammatory profiles of post-bariatric patients with weight recidivism. Obes Surg. 2022;32(6):1849–55.
Thorand B, Baumert J, Döring A, Herder C, Kolb H, Rathmann W, et al. Sex differences in the relation of body composition to markers of inflammation. Atherosclerosis. 2006;184(1):216–24.
IL6R Genetics Consortium Emerging Risk Factors Collaboration, Sarwar N, Butterworth AS, Freitag DF, Gregson J, Willeit P, et al. Interleukin-6 receptor pathways in coronary heart disease a collaborative meta-analysis of 82 studies. Lancet. 2012;379(9822):1205–13.
Pradhan AD. C-reactive protein, Interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286(3):327.
Kelly AS, Ryder JR, Marlatt KL, Rudser KD, Jenkins T, Inge TH. Changes in inflammation, oxidative stress and adipokines following bariatric surgery among adolescents with severe obesity. Int J Obes. 2015;40(2):275–80.
Acknowledgements
The authors would like to thank the all of the patients who completed the study protocol.
Funding
LAF, and SMBPM receives grants of Coordenaçao de Apoio ao Pessoal de Nível Superior (CAPES/PROSUP); JPRA, and MCO receives grants of Fundação de Amparo a Pesquisa (FAPEG), Goiás (GO), Brazil; LVFO receive grants Research Productivity, modality PQ1D; process no. 312731/2018-3 of Conselho Nacional de Desenvolvimento Cientifico e Tecnologico (local acronym CNPq), Brazil. RPV receive grants Research Productivity, modality PQII; process no. 313299/2018-8 of Conselho Nacional de Desenvolvimento Cientifico e Tecnologico (local acronym CNPq), Brazil. GI is a senior researcher at the Institute for Biomedical Research and Innovation, National Research Council—CNR, Palermo (SI), Italy.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: LVFO, WRFJ, SV, GI, CAM, and EIJ; contributed to the acquisition of the data: LAF, SMBPM, MCO, JPRA, and MEML; participated in its design, coordination, and statistical analysis: ALLB, VP, RPV, and WRFJ; performed the extra analyses; ALLB,, and drafted the manuscript: LVFO, CHMS, GI, and CAM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the recruited volunteers signed a free and informed consent form that was previously approved by the National Ethics Committee in Research with Human Beings of Santa Casa de Misericordia (Process number 178/2012) and registered in ClinicalTrials.gov NCT02409160. The study was conducted in accordance with the Regulatory Norms for Research Involving Human Subjects of the National Health Council of the Ministry of Health, RESOLUTION No. 466, on December 12, 2012 [14].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Felipe, L.A., Bachi, A.L.L., Oliveira, M.C. et al. Effects of Roux-en-Y gastric bypass on the metabolic profile and systemic inflammatory status of women with metabolic syndrome: randomized controlled clinical trial. Diabetol Metab Syndr 15, 19 (2023). https://doi.org/10.1186/s13098-023-00986-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-00986-2