Abstract
Background
The proportion of patients with breast cancer and obesity is increasing. While the therapeutic landscape of breast cancer has been expanding, we lack knowledge about the potential differential efficacy of most drugs according to the body mass index (BMI). Here, we conducted a systematic review on recent clinical drug trials to document the dosing regimen of recent drugs, the reporting of BMI and the possible exclusion of patients according to BMI, other adiposity measurements and/or diabetes (leading comorbidity of obesity). We further explored whether treatment efficacy was evaluated according to BMI.
Methods
A search of Pubmed and ClinicalTrials.gov was performed to identify phase I-IV trials investigating novel systemic breast cancer treatments. Dosing regimens and exclusion based on BMI, adiposity measurements or diabetes, documentation of BMI and subgroup analyses according to BMI were assessed.
Results
495 trials evaluating 26 different drugs were included. Most of the drugs (21/26, 81%) were given in a fixed dose independent of patient weight. BMI was an exclusion criterion in 3 out of 495 trials. Patients with diabetes, the leading comorbidity of obesity, were excluded in 67/495 trials (13.5%). Distribution of patients according to BMI was mentioned in 8% of the manuscripts, subgroup analysis was performed in 2 trials. No other measures of adiposity/body composition were mentioned in any of the trials. Retrospective analyses on the impact of BMI were performed in 6 trials.
Conclusions
Patient adiposity is hardly considered as most novel drug treatments are given in a fixed dose. BMI is generally not reported in recent trials and few secondary analyses are performed. Given the prevalence of patients with obesity and the impact obesity can have on pharmacokinetics and cancer biology, more attention should be given by investigators and study sponsors to reporting patient’s BMI and evaluating its impact on treatment efficacy and toxicity.
Similar content being viewed by others
Introduction
Over the last decade the proportion of women with overweight and obesity, reflected by an elevated body mass index (BMI equal or above 25 and 30 kg/m2, respectively), has been increasing worldwide [1]. Consequently, the proportion of women with breast cancer (BC) who are overweight or obese is increasing as well. Obesity is associated with a higher prevalence of postmenopausal breast cancer, more advanced disease burden at diagnosis and worse survival [2,3,4]. Retrospective analyses show that obesity is also associated with an increased risk of distant recurrence in patients with both estrogen receptor (ER)-negative and ER-positive disease after adjustments for standard clinicopathological parameters [5].
Different approaches are used for drug dosing related to weight and/or length parameters. Fixed dose administration minimizes the risk of mistakes and maximizes the efficacy of the drug preparation. Weight-based approaches, on the other hand, include regimens using the patient’s actual weight, body-surface area (BSA) or, in research setting, lean body weight [6, 7]. By using the actual weight to calculate drug dosing, the dosage is increased linearly with the patient’s weight [6]. The BSA resembles the two-dimensional surface area of the skin and BSA correlates with the basal metabolic rate [8]. However, different BSA formulas are rather inconsistent in obese patients [9, 10]. Lean body weight dosing, excluding the fat tissues, correlates more closely with the actual drug clearance in hydrophilic drugs, however, this is difficult to use in clinical practice [11]. These considerations are relevant since it is known that obesity can influence pharmacokinetics and -dynamics in a drug-specific manner [12]. Both fat and lean mass increase with higher body weight, but the ratio changes, resulting in a higher fat percentage and a lower lean body percentage [13]. Obesity impacts pharmacokinetics in all facets: absorption, distribution, metabolism, and clearance [12, 14, 15]. The effect of obesity on absorption and distribution is highly drug-specific and depends on the lipophilicity of the drug [14]. Greater lipophilicity enhances the drug's capacity to cross the lipid bilayer by passive diffusion; however, it concurrently augments the drug's propensity to accumulate in adipose tissue distinct from the target organ. Examples of established chemotherapeutic drugs that are lipophilic are docetaxel, paclitaxel, adriamycin, and cisplatin [17]. A retrospective analysis of the BIG 2–98 trial demonstrated that survival was worse in patients with overweight or obesity receiving a docetaxel-based regimen, as compared to lean patients receiving the same treatment, while no difference in survival was observed according to BMI in patients receiving anthracyclines and CMF (cyclophosphamide, methotrexate, fluorouracil) [18]. The impact of obesity on pharmacokinetic properties is dependent on the therapeutic window, which is generally broader for immunotherapy and targeted therapies [19,20,21].
But BMI does not only impact treatment efficacy through the pharmacokinetic properties of the drugs [22, 23]. For instance, some studies have shown a potential association between obesity and a higher rate of endocrine resistance in the adjuvant setting [23,24,25]. This could be explained through the impact of obesity on adipocytes, metabolic markers and inflammation [23]. Controversially, overweight and obesity might be associated with an increased anti-proliferative response to neoadjuvant treatment for BC with aromatase inhibitors [26]. Experimental studies and retrospective analyses from clinical trials in some cancer types suggest that obese patients might benefit more from immune checkpoint inhibitors as compared to lean patients, although results for patients with BC are limited [27]. Finally, several studies have also revealed the impact BMI has on tumor cells and the tumor microenvironment [28,29,30]. Globally, these studies have shown that in some tumor types there is an increased molecular aging with obesity, slight differences in genomic landscape, and a reorganization of the composition and interactions in the tumor microenvironment.
Altogether, this collective evidence emphasizes the need to investigate the impact of obesity on pharmacokinetics and efficacy in clinical drug trials, especially given the expansion of the BC therapeutic landscape in the last decade with the emergence of novel selective estrogen receptor degraders (SERDs), CDK4/6 inhibitors, immune checkpoint inhibitors (ICIs), antibody–drug conjugates (ADCs), PI3K and tyrosine-kinase inhibitors, PARP-inhibitors as well as other targeted therapies. For most of these therapies, it is unknown whether efficacy or associated side effects could differ according to patient adiposity. Here, we conducted a systematic review on recent clinical drug trials to document the dosing regimen of these recent drugs, the reporting of BMI (or alternative body composition measurements) and the possible exclusion of patients according to BMI (or patients with diabetes) in phase I-IV trials.
Methods
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed to conduct the literature search and study). Based on recent literature, 8 different categories of novel BC treatments of interest were identified [33,34,35]: CDK4/6 inhibitors, ADCs, oral SERDs, PARP inhibitors, tyrosine kinase inhibitors (TKI), ICIs, PI3K/AKT/PTEN inhibitors and other drugs under investigation such as tucidinostat and margetuximab. Two reviewers (JVC and KVB) independently searched the PubMed database and the clinicaltrials.gov database to identify phase III and IV clinical trials on these 8 novel BC drug categories by screening titles and abstracts. Additionally, a second search was conducted on phase I and II trials for those drugs within the predefined drug categories reported in phase III and IV trials (Fig. 1). Medical subject heading terms (MeSH) related to the treatments and treatment categories were used as well as names of individual drugs in the search together with the MeSH-term ‘Breast Neoplasms’ (Additional file 1: Supplementary Table 1). We included all phase I-IV trials that had a manuscript of the primary analysis accessible on the 31st of December 2023. There were no further restrictions based on date of publication. Solely manuscripts in English were included. The search terms and definitions can be found in the supplementary material (Additional file 1: Supplementary Table 1). In case of multiple records on the same trial, only the primary analyses was considered. An exception was made for basket trials investigating multiple drugs for which 1 record per study arm was allowed. Pooled analyses using results of multiple trials were excluded as well as trials that were not investigating the efficacy of drugs associated with the used search term (records off topic). Disagreements between the reviewers were resolved through discussion and consensus.
We first reported the BC drug dosing regimens in the included trials. The manuscripts were then assessed for the documentation of mean or median weight of the study population, for distribution of BMI and for potential subgroup analyses based on BMI/weight categories. BMI is defined as body mass (kg) divided by the square of the body height (m2). According to the WHO classification, BMI is categorized into underweight (≤ 18.5 kg/m2), lean (> 18.5 kg/m2 and < 25 kg/m2), overweight (≥ 25 kg/m2 and < 30 kg/m2) and obesity (≥ 30 kg/m2). We investigated whether there were exclusion criteria related to BMI or diabetes and whether other measurements of adiposity such as body composition or body measurements were reported. We investigated diabetes since it is the leading cause of BMI-related disability adjusted life years [31], 60% of patients who are diagnosed with diabetes mellitus type 2 are obese [32]. We further explored whether treatment efficacy and treatment-associated side effects were evaluated according to BMI. All supplementary material, if available, was also evaluated. Additionally, with a secondary PubMed search, we assessed the availability of additional retrospective analyses of the included clinical trials, that evaluated the impact of BMI and other adiposity measurements on pharmacokinetics or survival.
The names and classes of the drugs as well as the names of the different trials were used together with the MeSH-terms ‘Obesity’, ‘Body Mass Index’, ‘Body Weight’ or ‘Adiposity’ to see if any additional analyses had been done. In this stage, pooled analyses of the included trials were also searched to see if they reported on sub-analyses.
Results are shown in a descriptive manner.
Results
Selection of the trials investigating new breast cancer treatments
-
1.
Primary search: phase III and IV trials
We identified 26 drugs within the eight treatment categories. For the primary comprehensive search, 1273 papers were screened and a total of 95 phase III and IV trials were retained, of which 14 are in the neo-adjuvant, 11 in the adjuvant and 70 in the metastatic setting. Figure 2 depicts the PRISMA flow diagram. All original primary manuscripts were published between 12/2006 and 12/2023. All included trials are summarized in Additional file 1: Supplementary Table 2 in the Appendix.
-
2.
Secondary search: phase I and II trials
ClinicalTrials.gov and Pubmed were searched for the phase I and II trials of the 26 drugs identified during the primary search. A total of 2038 papers were screened and a total of 400 manuscripts were retained, of which 318 in metastatic, 5 in adjuvant and 74 in neoadjuvant setting. Three trials were performed in healthy participants [36]. All the included trials are summarized in Additional file 1: Supplemantary Table 3 in the Appendix (Fig. 3).
Weight-based vs fixed dose
We assessed the dosing regimen of the drugs under investigation in the clinical trials, as presented in Table 1. Notably, 21 out of 26 drugs (81%) are administered in a fixed dose during phase III/IV trials. Two drugs, atezolizumab and pembrolizumab, have been dosed in a weight-based regimen in some phase I and II trials [37,38,39,40,41], but proceeded to phase III and IV trials in a fixed dose regimen. It is noteworthy that trials employing an ICI in a weight-based regimen did not provide information regarding the weight distribution of the patients. Neither was there a direct comparison between the efficacy of the two regimens for breast cancer specifically. Out of the 26 drugs investigated, 18 were administerd in a fixed dose regimen with no documented exploration of a weight-based approach.
The dosage of sacituzumab-govitecan, trastuzumab emtansine, trastuzumab-deruxtecan, iniparib and margetuximab are based on total body weight and can be adjusted during each administration in case of weight changes over the treatment period. None of the identified drugs were administered by BSA-dosing or lean-based weight dosing.
BMI or any other adiposity measurement and diabetes as exclusion criteria
Patients were excluded based on their weight or BMI in 3/495 trials (< 1%). A phase 1 study of ribociclib on healthy subjects excluded those with a BMI > 36 kg/m2 or total body weight of > 120 kg [44]. Miller et al., a trial investigating capivaserib in a healthy subjects, also excluded patients with a body weight > 100 kg [45]. Yam et al. on the other hand only included patients with BMI ≥ 25 kg/m2 to asses the combination of everolimus and metformin [46]. In all further 492 trials (99%), BMI/weight of the patient was never considered an exclusion criterion. Diabetes mellitus type 2 on the other hand, which is the leading comorbidity of obesity [31, 47, 48], was however a criterion for exclusion to some degree in 16/95 of the phase III/IV (17%) trials and 51/400 (13%) of the phase I and II trials. Approximately 51% of the trials that excluded individuals with diabetes to some degree, were studying drugs targeting the PI3K/AKT/PTEN pathway. There is a wide variability in the severity of exclusion based on diabetes in the different trials, details can be retrieve in Additional file 1: Supplementary Table 2 and 3. Certain trials identified uncontrolled or severe diabetes mellitus as an exclusion criterion, without providing further specifics [49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67, 101,102,103,104,105,106]. Other trials have opted to exclude all individuals with diabetes mellitus [68,69,70,71,72,73,74] or patients with diabetic symptoms [75,76,77,78] or all patients receiving hypoglycemic treatments [54, 79,80,81, 106]. Some trials established strict exclusion criteria based on HbA1c and fasting glucose levels [82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100, 107,108,109, 130]. These clinical trials might not always have adequately enrolled patients with obesity and might therefore not represent the intended general patient population.
Reporting of BMI and analysis of treatment efficacy and side-effects according to BMI
BMI or weight of the included patients was reported in 9% of the phase I/II trials (n = 37) and 3% of phase III and IV trials (n = 3), culminating in a total of 8% (n = 40) of all included trials.
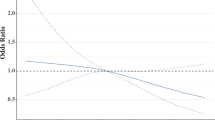
The BALLET and TBCRC 043 trials were the only trials performing a subgroup analysis in the original manuscript. The BALLET trial showed that the incidence of adverse events of everolimus was independent of BMI status [110]. In TBCRC 043 it is noted that there was a non-significant trend towards a greater benefit from atezolizumab plus carboplatin in metastatic breast cancer of obese patients (HR, 0.52; P = 0.10) [111]. Primary subgroup analyses on differences in therapy efficacy were not performed in any of the other trials. But DeCensi et al. conducted a study on the impact of patients’ weight on the pharmacokinetics of lapatinib, and the findings indicated that weight did not exert a significant impact [112].
For six trials studying CDK4/6 inhibitors, additional retrospective analyses regarding the impact of BMI on treatment efficacy and/or associated side-effects were performed. This was the case for the NEOMONARCH [113], ALTTO [114] and neo-ALTTO trial [115], the PALLAS trial [116] and a pooled analysis of MONARCH 2 and 3 trial [117]. In the NEOMONARCH BMI > 25 kg/m2 did not impact change in Ki67% or clinical/radiological response in neoadjuvant setting [113]. Di Cosimo et al. showed that the pathological complete response rate after anti-HER2 therapies in overweight and obese patients with hormone receptor (HR)-positive, HER2-positive BC included in the neo-ALTTO trial was lower compared to their lean counterparts. This was however independent of the treatment arm [115]. The secondary analysis of the ALTTO [114] trials showed that postmenopausal patients with HR-positive HER2-positive BC who were obese at diagnosis and received lapatinib, had a worse prognosis, experienced more grade 3 or 4 adverse events and had higher treatment discontinuation rate [114]. Secondary analyses of the PALLAS trial showed that palbociclib-induced neutropenia was less frequent in overweight and obese patients. A difference in iDFS was not seen [116]. A pooled analysis of Monarch-2 and 3 could not identify any difference in PFS according to BMI [117]. However, the addition of abemaciclib to endocrine therapy resulted in a greater difference in PFS in the normal weight category compared to overweight and obese [117]. Neutropenia was again less frequent in the overweight/obese population compared to normal weight population, suggesting a pharmacokinetic effect.
Discussion
Several conclusions can be drawn from this systematic review. Firstly, this study emphasizes that most recent drugs are given at fixed doses independently of patient’s weight or BSA in contrast to chemotherapy. Some recent trials question this fixed dose regimen since weight-based dosing mostly results in a lower dose and thus possibly lower cost and less toxicity [118,119,120]. Defining the maximum tolerated dose (MTD) is a frequent primary objective in phase I/II trials. However, in the case of drugs with a wider therapeutic window, as anticipated in targeted therapies and immunotherapy there is a concern that MTD could result in overdosing. Dose de-escalation might therefore lead to similar therapeutic efficacy with less toxicity [116, 121]. The Optimus Project, an FDA initiative, aims to reform dosing in drug development in early clinical trials [122]. It is hypothesized that the impact of obesity on the pharmacokinetics is less relevant in drugs with a broader therapeutic window, such as targeted therapies and immunotherapies. However, the potential impact on therapeutic efficacy through other alternative mechanisms remains uncertain due to a lack of dedicated studies on this subject.
In 2021, the American Society of Clinical Oncology (ASCO) issued guidelines on the appropriate systematic therapy dosing for obese adult patients with cancer [123]. The guidelines stated that cytotoxic therapy should be offered at full dose for obese patient and therefore dose capping should be avoided. Guidelines regarding targeted therapies and immunotherapy prescribe that these treatments should be used in all patients, regardless of obesity status. However, evidence supporting equal efficacy in obese versus lean patients is low [124]. To be able to guide our clinical practice pharmacokinetic/pharmacodynamic studies as well as dose–response analyses are needed for these drugs.
Further, obesity was in less than 1% of the trials an exclusion criterion. Since diabetes mellitus type 2 is the leading comorbidity of obesity [31], we investigated diabetes mellitus type 2 as an exclusion criterium in the context of our systematic review as a surrogate marker of obesity [125]. A note of caution should however be taken as only about 16–20% of patients with obesity develop diabetes mellitus type 2 [126, 127] and as diabetes type 2 can be diagnosed after inclusion in the study. It is noteworthy that the majority of the trials excluding patients with diabetes involve PIK3CA or mTOR inhibitors, both of which are known to cause hyperglycemia. Consequently, caution is needed when including diabetic patients in such trials. Furthermore, we acknowledge that there are more comorbidities of obesity that we did not consider in this systematic review, such as heart disease, hypertension or obstructive sleep apnea. It is important to highlight that the exclusion of obese patients indirectly contributes to a racial bias in some environments, given that obesity is more prevalent within the black or Hispanic communities in the USA [128]. Race and other socioeconomic characteristics are associated with obesity and therefore should also be considered and documented [129, 130]. Reimbursements of therapies can be based on the inclusion criteria outlined in phase III/IV trials, underscoring the importance of prioritizing inclusivity in these trials.
Thirdly, we can conclude that there is a clear gap in knowledge on the efficacy of novel anti-cancer treatments in different weight categories. Most of the clinical trials do not report individual patient data about BMI and do not perform analyses to identify potential variations in treatment efficacy according to BMI.
It is known that BMI itself is a suboptimal marker for adiposity since it does not reflect body composition and therefore underestimates adiposity in postmenopausal women [131,132,133,134,135]. BSA—based dosing is suboptimal for some obese patients and might lead to underexposure, while weight-based dosing can lead to overexposure [136]. Alternative measurements of adiposity include body composition measurements or measurements of the adipocytes in the breast tissue [137]. However, the precise relationship between these measures, BMI and their potential impact on treatment efficacy is not yet fully understood. Further research to understand these relationships is necessary before these variables can be used in clinical practice to determine treatment options.
Phase I and II trials are designed to study pharmacokinetics and identify the maximum tolerated dose for progression into phase III and IV trials [138]. It is noteworthy that body composition measurements are rarely reported across all phases of clinical trials. A comprehensive study of obesity throughout the entire drug development process is important as its impact extents beyond pharmacokinetics and as phase I and II trials are often conducted in a population limited in size and generally less representative of the affected population [139]. These trials often exclude patients with cardiovascular history, diabetes, hypertension or low performance score, indirectly resulting to the underrepresentation of obese patients within these cohorts [139, 140].
This systematic review has several limitations. Firstly, there is a publication bias. We have only included full manuscripts but several, more recent trials [141, 142], currently only have an abstract or poster presentation available. In addition to this, non-publication of a full manuscript is common among phase I and II trials [143]. We found 74 abstracts of results of phase I and II trials without a full manuscript. Secondly, we suspect that the patient’s weight and height are available in the electronic case report forms of most patients but not reported in publication nor analysed elsewhere.
If we would consistently report on BMI, precaution is still needed if subgroup analyses for therapeutic efficacy according to BMI are performed, as these will be most of the time unplanned analyses with possibly suboptimal statistical power. In the event that poorer survival is observed among individuals classified as obese or overweight, it will be important to distinguish the predictive versus prognostic effect. We strongly encourage investigators to study the impact of obesity on therapeutic efficacy (and the incidence and severity of treatment-related side effects) and possibly use real world data for a representative population.
To our knowledge, no previous systematic review has been conducted to point out this gap in information. Hereby we hope to emphasize the need to take BMI or alternative body composition measurements at time of treatment administration into consideration when evaluating BC therapies.
In conclusion, this systematic review emphasizes the lack of reporting BMI or other adiposity measurements in clinical trials for BC treatment. Incorporating BMI or other adiposity measurements into trial design and analysis can aid in identifying potential differences in treatment efficacy among different weight categories, ultimately resulting in more effective and tailored treatment methods for patients with BC.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
World health statistics 2022: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO.
Lohmann AE, et al. Association of obesity with breast cancer outcome in relation to cancer subtypes: a meta-analysis. J Natl Cancer Inst. 2021;113:1465–75.
Protani M, Coory M, Martin JH, Protani M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–35.
Goodwin PJ, Stambolic V. Impact of the obesity epidemic on cancer. Annu Rev Med. 2015;66:281–96.
Biganzoli E, et al. Recurrence dynamics of breast cancer according to baseline body mass index. Eur J Cancer. 2017;87:10–20.
Pai MP. Drug dosing based on weight and body surface area: mathematical assumptions and limitations in obese adults. Pharmacother J Human Pharmacol Drug Ther. 2012;32:856–68.
Hoge RHL, et al. Lean body mass and total body weight versus body surface area as a determinant of docetaxel pharmacokinetics and toxicity. Ther Drug Monit. 2022;44:755–61.
Miller AA. Body surface area in dosing anticancer agents: scratch the surface! J Natl Cancer Inst. 2002;94:1822–31.
Redlarski G, Palkowski A, Krawczuk M. Body surface area formulae: an alarming ambiguity. Sci Rep. 2016;6:1–8.
Zhang T, Krekels EHJ, Smit C, Knibbe CAJ. Drug pharmacokinetics in the obese population: challenging common assumptions on predictors of obesity-related parameter changes. Expert Opin Drug Metab Toxicol. 2022;18:657–74.
Barras M, Legg A. Drug dosing in obese adults. Aust Prescr. 2017;40:189.
Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet. 2010;49:71–87.
Cheymol G. Effects of obesity on pharmacokinetics implications for drug therapy. Clin Pharmacokinet. 2000;39:215–31.
Talevi A, Bellera CL. Drug absorption. In: ADME processes in pharmaceutical sciences: dosage, design, and pharmacotherapy success, pp 11–96 (2023). https://doi.org/10.1007/978-3-319-99593-9_2
Abernethy DR, Greenblatt DJ, Divoll M, Shader RI. Prolonged accumulation of diazepam in obesity. J Clin Pharmacol. 1983;23:369–76.
Kim YS, Nam YS, Kim DI. Evaluating the effectiveness of gluteal intramuscular injection sites: a cadaveric study. Anat Cell Biol. 2022;55:48.
Wei J, Zhang Y, Li Z, Li X, Zhao C. Docetaxel population pharmacokinetic modelling and simulation in Chinese cancer patients. Ann Transl Med. 2022;10:705–705.
Desmedt C, et al. Differential benefit of adjuvant docetaxel-based chemotherapy in patients with early breast cancer according to baseline body mass index. J Clin Oncol. 2020;38:2883–91.
Goldstein MJ, Peters M, Weber BL, Davis CB. Optimizing the therapeutic window of targeted drugs in oncology: potency-guided first-in-human studies. Clin Transl Sci. 2021;14:536.
Le Louedec F, et al. Cancer immunotherapy dosing: a pharmacokinetic/pharmacodynamic perspective. Vaccines (Basel). 2020;8:1–23.
Hendrikx JJMA, et al. Fixed dosing of monoclonal antibodies in oncology. Oncologist. 2017;22:1212–21.
Ewertz M, et al. Effect of obesity on prognosis after early-stage breast cancer. J Clin Oncol. 2011;29:25–31.
Barone I, et al. Obesity and endocrine therapy resistance in breast cancer: mechanistic insights and perspectives. Obes Rev. 2022;23:e13358.
Bougaret L, et al. Adipocyte/breast cancer cell crosstalk in obesity interferes with the anti-proliferative efficacy of tamoxifen. PLoS ONE. 2018;13:e0191571.
Sestak I, et al. Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. J Clin Oncol. 2010;28:3411–5.
Isnaldi E, et al. The association between adiposity and anti-proliferative response to neoadjuvant endocrine therapy with letrozole in post-menopausal patients with estrogen receptor positive breast cancer. NPJ Breast Cancer. 2022;8:1–10.
Yoo SK, Chowell D, Valero C, Morris LGT, Chan TA. Outcomes among patients with or without obesity and with cancer following treatment with immune checkpoint blockade. JAMA Netw Open. 2022;5:e220448–e220448.
Quail DF, Dannenberg AJ. The obese adipose tissue microenvironment in cancer development and progression. Nat Rev Endocrinol. 2018;15:139–54.
Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and cancer: local and systemic mechanisms. Annu Rev Med. 2015;66:297–309.
Nguyen HL, et al. Obesity-associated changes in molecular biology of primary breast cancer. Nat Commun. 2023;14:1–17.
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017; 377:13–27.
Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. The Lancet. 2017;389:2239–51.
Elliott MJ, Cescon DW. Development of novel agents for the treatment of early estrogen receptor positive breast cancer. Breast Off J Eur Soc Mastol. 2022;62:S34.
Nagayama A, Vidula N, Bardia A. Novel therapies for metastatic triple-negative breast cancer: spotlight on immunotherapy and antibody-drug conjugates. Oncology (Williston Park). 2021;35:249–54.
Martin M, López-Tarruella S. Emerging therapeutic options for HER2-positive breast cancer. Am Soc Clin Oncol Educ Book. 2016;35:e64–70.
Yu Y, et al. Palbociclib (PD-0332991) pharmacokinetics in subjects with impaired renal function. Cancer Chemother Pharmacol. 2020;86:701–10.
Emens LA, et al. Long-term clinical outcomes and biomarker analyses of atezolizumab therapy for patients with metastatic triple-negative breast cancer: a phase 1 study. JAMA Oncol. 2019;5:74–82.
Herbst RS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–7.
Nanda R, et al. Pembrolizumab in patients with advanced triple-negative breast cancer: phase Ib KEYNOTE-012 study. J Clin Oncol. 2016;34:2460–7.
Weiss GJ, et al. A phase Ib study of pembrolizumab plus chemotherapy in patients with advanced cancer (PembroPlus). Br J Cancer. 2017;117:33–40.
Rugo HS, et al. Safety and antitumor activity of pembrolizumab in patients with estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer. Clin Cancer Res. 2018;24:2804–11.
Mansoor A, Mahabadi N. Volume of distribution. Transl Clin Pharmacol. 2023;24:74–7.
Marra A, Curigliano G. Are all cyclin-dependent kinases 4/6 inhibitors created equal? NPJ Breast Cancer. 2019;5:27.
Samant TS, Yang S, Miller M, Ji Y. Pharmacokinetics of ribociclib in subjects with hepatic impairment. J Clin Pharmacol. 2021;61:1001–9.
Miller C, et al. Pharmacokinetics of the Akt Serine/threonine protein kinase inhibitor, capivasertib, administered to healthy volunteers in the presence and absence of the CYP3A4 inhibitor itraconazole. Clin Pharmacol Drug Dev. 2023;12:856–62.
Yam C, et al. Efficacy and safety of the combination of metformin, everolimus and exemestane in overweight and obese postmenopausal patients with metastatic, hormone receptor-positive, HER2-negative breast cancer: a phase II study. Invest New Drugs. 2019;37:345–51.
Ershow AG. Personalized medicine for diabetes: environmental influences on development of Type 2 diabetes and obesity: challenges in personalizing prevention and management. J Diabetes Sci Technol. 2009;3:727.
Barnes AS, Coulter SA. The epidemic of obesity and diabetes: trends and treatments. Tex Heart Inst J. 2011;38:142.
Waks AG, et al. Phase Ib study of pembrolizumab in combination with trastuzumab emtansine for metastatic HER2-positive breast cancer. J Immunother Cancer. 2022;10:e005119.
Yam C, et al. A phase II study of neoadjuvant atezolizumab and nab-paclitaxel in patients with anthracycline-resistant early-stage triple-negative breast cancer. Breast Cancer Res Treat. 2023;199:457–69.
Yuan Y, et al. Phase I trial of ipatasertib plus carboplatin, carboplatin/paclitaxel, or capecitabine and atezolizumab in metastatic triple-negative breast cancer. Oncologist. 2023;28:e498–507.
Gianni L, et al. Neoadjuvant treatment with trastuzumab and pertuzumab plus palbociclib and fulvestrant in HER2-positive, ER-positive breast cancer (NA-PHER2): an exploratory, open-label, phase 2 study. Lancet Oncol. 2018;19:249–56.
Yan M, et al. Dalpiciclib and pyrotinib in women with HER2-positive advanced breast cancer: a single-arm phase II trial. Nat Commun. 2023;14:6272.
Yonemori K, et al. A phase I/II trial of olaparib tablet in combination with eribulin in Japanese patients with advanced or metastatic triple-negative breast cancer previously treated with anthracyclines and taxanes. Eur J Cancer. 2019;109:84–91.
Li Q, et al. Safety, efficacy, and biomarker analysis of pyrotinib in combination with capecitabine in HER2-positive metastatic breast cancer patients: a phase I clinical trial. Clin Cancer Res. 2019;25:5212–20.
Hu ZY, et al. Pyrotinib in combination with letrozole for hormone receptor-positive, human epidermal growth factor receptor 2-positive metastatic breast cancer (PLEHERM): a multicenter, single-arm, phase II trial. BMC Med. 2023;21:226.
Cao J, et al. Pyrotinib plus capecitabine for trastuzumab-resistant, HER2-positive advanced breast cancer (PICTURE): a single-arm, multicenter phase 2 trial. BMC Med. 2023;21:1–10.
Savas P, et al. Alpelisib monotherapy for PI3K-altered, pretreated advanced breast cancer: a phase II study. Cancer Discov. 2022;12:2058–73.
Jhaveri K, et al. A phase I study of alpelisib in combination with trastuzumab and LJM716 in patients with PIK3CA-mutated HER2-positive metastatic breast cancer. Clin Cancer Res. 2021;27:3867.
McRee AJ, et al. A phase I trial of the PI3K inhibitor buparlisib combined with capecitabine in patients with metastatic breast cancer. Clin Breast Cancer. 2018;18:289.
Welt A, et al. Buparlisib in combination with tamoxifen in pretreated patients with hormone receptor-positive, HER2-negative advanced breast cancer molecularly stratified for PIK3CA mutations and loss of PTEN expression. Cancer Med. 2020;9:4527–39.
Garrido-Castro AC, et al. Phase 2 study of buparlisib (BKM120), a pan-class I PI3K inhibitor, in patients with metastatic triple-negative breast cancer. Breast Cancer Res. 2020;22:1–13.
Infante JR, et al. A phase I dose-escalation study of Selumetinib in combination with Erlotinib or Temsirolimus in patients with advanced solid tumors. Invest New Drugs. 2017;35:576.
Schmid P, et al. Fulvestrant plus vistusertib vs fulvestrant plus everolimus vs fulvestrant alone for women with hormone receptor-positive metastatic breast cancer: the MANTA Phase 2 Randomized clinical trial. JAMA Oncol. 2019;5:1556.
Park IH, et al. Phase I/II clinical trial of everolimus combined with gemcitabine/cisplatin for metastatic triple-negative breast cancer. J Cancer. 2018;9:1145.
Baselga J, et al. Phase II randomized study of neoadjuvant everolimus plus letrozole compared with placebo plus letrozole in patients with estrogen receptor-positive breast cancer. J Clin Oncol. 2009;27:2630–7.
Gonzalez-Angulo AM, et al. Biologic markers in axillary node-negative breast cancer: differential expression in invasive ductal carcinoma versus invasive lobular carcinoma. Clin Breast Cancer. 2006;7:396–400.
Clark AS, et al. Combination paclitaxel and palbociclib: results of a phase I trial in advanced breast cancer. Clin Cancer Res. 2019;25:2072–9.
Curigliano G, et al. Alpelisib in combination with everolimus ± exemestane in solid tumours: phase Ib randomised, open-label, multicentre study. Eur J Cancer. 2021;151:49–62.
Bardia A, et al. Phase Ib study of combination therapy with MEK Inhibitor binimetinib and phosphatidylinositol 3-kinase inhibitor buparlisib in patients with advanced solid tumors with RAS/RAF alterations. Oncologist. 2020;25:e160–9.
Smyth LM, et al. Capivasertib, an AKT kinase inhibitor, as monotherapy or in combination with fulvestrant in patients with AKT1 E17K-mutant, ER-positive metastatic breast cancer. Clin Cancer Res. 2020;26:3947–57.
Banerji U, et al. A phase I open-label study to identify a dosing regimen of the pan-AKT inhibitor AZD5363 for evaluation in solid tumors and in PIK3CA-mutated breast and gynecologic cancers. Clin Cancer Res. 2018;24:2050–9.
Turner NC, et al. BEECH: a dose-finding run-in followed by a randomised phase II study assessing the efficacy of AKT inhibitor capivasertib (AZD5363) combined with paclitaxel in patients with estrogen receptor-positive advanced or metastatic breast cancer, and in a PIK3CA mutant sub-population. Ann Oncol. 2019;30:774–80.
Oliveira M, et al. FAIRLANE, a double-blind placebo-controlled randomized phase II trial of neoadjuvant ipatasertib plus paclitaxel for early triple-negative breast cancer. Ann Oncol. 2019;30:1289–97.
Mayer IA, et al. A phase Ib study of alpelisib (BYL719), a PI3Kα-specific inhibitor, with letrozole in ER+/HER2-negative metastatic breast cancer. Clin Cancer Res. 2017;23:26.
Pistilli B, et al. Phase II study of buparlisib (BKM120) and trastuzumab in patients with HER2+ locally advanced or metastatic breast cancer resistant to trastuzumab-based therapy. Breast Cancer Res Treat. 2018;168:357.
Bendell JC, et al. Phase I, dose-escalation study of BKM120, an oral pan-class I PI3K inhibitor, in patients with advanced solid tumors. J Clin Oncol. 2012;30:282–90.
Mayer IA, et al. Stand up to cancer phase Ib study of pan-phosphoinositide-3-kinase inhibitor buparlisib with letrozole in estrogen receptor-positive/human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2014;32:1202–9.
Rodon J, et al. A Phase Ib, open-label, dose-finding study of alpelisib in combination with paclitaxel in patients with advanced solid tumors. Oncotarget. 2018;9:31709–18.
Saura C, et al. Neoadjuvant letrozole plus taselisib versus letrozole plus placebo in postmenopausal women with oestrogen receptor-positive, HER2-negative, early-stage breast cancer (LORELEI): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2019;20:1226–38.
Ma CX, et al. A phase i trial of the IGF-1R antibody Cixutumumab in combination with temsirolimus in patients with metastatic breast cancer. Breast Cancer Res Treat. 2013;139:145–53.
Malorni L, et al. Serum thymidine kinase activity in patients with hormone receptor-positive and HER2-negative metastatic breast cancer treated with palbociclib and fulvestrant. Eur J Cancer. 2022;164:39–51.
Mayer IA, et al. A Phase II randomized study of neoadjuvant letrozole plus alpelisib for hormone receptor-positive, human epidermal growth factor receptor 2-negative breast cancer (NEO-ORB). Clin Cancer Res. 2019;25:2975–87.
Juric D, et al. Alpelisib plus fulvestrant in PIK3CA-altered and PIK3CA-wild-type estrogen receptor-positive advanced breast cancer: a phase 1b clinical trial. JAMA Oncol. 2019;5:e184475–e184475.
Juric D, et al. Phosphatidylinositol 3-Kinase α-selective inhibition with alpelisib (BYL719) in PIK3CA-altered solid tumors: results from the first-in-human study. J Clin Oncol. 2018;36:1291–9.
Sharma P, et al. Clinical and biomarker results from phase I/II study of PI3K inhibitor alpelisib plus nab-paclitaxel in HER2-negative metastatic breast cancer. Clin Cancer Res. 2021;27:3896–904.
Rugo HS, et al. Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): one cohort of a phase 2, multicentre, open-label, non-comparative study. Lancet Oncol. 2021;22:489–98.
Ma CX, et al. A phase 1 trial of BKM120 (Buparlisib) in combination with fulvestrant in postmenopausal women with estrogen receptor positive metastatic breast cancer. Clin Cancer Res. 2016;22:1583.
Schmid P, et al. Capivasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer: the PAKT trial. J Clin Oncol. 2020;38:423–33.
Howell SJ, et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive, HER2-negative breast cancer (FAKTION): overall survival, updated progression-free survival, and expanded biomarker analysis from a randomised, phase 2 trial. Lancet Oncol. 2022;23:851–64.
Jones RH, et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive breast cancer (FAKTION): a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2020;21:345–57.
Gombos A, et al. FDG positron emission tomography imaging and ctDNA detection as an early dynamic biomarker of everolimus efficacy in advanced luminal breast cancer. NPJ Breast Cancer. 2021;7:1–9.
Kornblum N, et al. Randomized phase II trial of fulvestrant plus everolimus or placebo in postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer resistant to aromatase inhibitor therapy: results of PrE0102. J Clin Oncol. 2018;36:1556–63.
Van Swearingen AED, et al. LCCC 1025: a phase II study of everolimus, trastuzumab, and vinorelbine to treat progressive HER2-positive breast cancer brain metastases. Breast Cancer Res Treat. 2018;171:637–48.
Singh JC, et al. Phase 2 trial of everolimus and carboplatin combination in patients with triple negative metastatic breast cancer. Breast Cancer Res. 2014;16:R32.
Rugo HS, et al. Prevention of everolimus-related stomatitis in women with hormone receptor-positive, HER2-negative metastatic breast cancer using dexamethasone mouthwash (SWISH): a single-arm, phase 2 trial. Lancet Oncol. 2017;18:654–62.
Ballhausen A, et al. Phase I study of everolimus, letrozole, and trastuzumab in patients with hormone receptor-positive metastatic breast cancer or other solid tumors. Clin Cancer Res. 2021;27:1247–55.
Peddi PF, et al. Phase II randomized trial of a non-steroidal mouth wash for prevention and treatment of stomatitis in women with hormone receptor positive breast cancer treated with everolimus. Ther Adv Med Oncol. 2020;12:1758835920967259.
Jones VE, et al. Evaluation of miracle mouthwash plus hydrocortisone versus prednisolone mouth rinses as prophylaxis for everolimus-associated stomatitis: a randomized phase II study. Oncologist. 2019;24:1153–8.
Maass N, et al. Everolimus as treatment for breast cancer patients with bone metastases only: results of the phase II RADAR study. J Cancer Res Clin Oncol. 2013;139:2047–56.
Alsaleh K, et al. Neoadjuvant endocrine therapy with or without palbociclib in low-risk patients: a phase III randomized double-blind SAFIA trial. J Cancer Res Clin Oncol. 2023. https://doi.org/10.1007/S00432-023-04588-3.
Loibl S, et al. Palbociclib for residual high-risk invasive HR-positive and HER2-negative early breast cancer-the penelope-B trial. J Clin Oncol. 2021;39:1518–30.
Krop IE, et al. Trastuzumab emtansine plus pertuzumab versus taxane plus trastuzumab plus pertuzumab after anthracycline for high-risk human epidermal growth factor receptor 2-positive early breast cancer: the phase III KAITLIN study. J Clin Oncol. 2022;40:438–48.
André F, et al. Everolimus for women with trastuzumab-resistant, HER2-positive, advanced breast cancer (BOLERO-3): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15:580–91.
Baselga J, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379:633–40.
Untch M, et al. Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol. 2012;13:135–44.
Moore HCF, et al. A randomized trial of fulvestrant, everolimus, and anastrozole for the front-line treatment of patients with advanced hormone receptor-positive breast cancer, SWOG S1222. Clin Cancer Res. 2022;28:611–7.
Guarneri V, et al. Everolimus plus aromatase inhibitors as maintenance therapy after first-line chemotherapy: final results of the phase III randomised MAIN-A (MAINtenance Afinitor) trial. Eur J Cancer. 2021;154:21–9.
Im YH, et al. Safety and efficacy of everolimus (EVE) plus exemestane (EXE) in postmenopausal women with locally advanced or metastatic breast cancer: final results from EVEREXES. Breast Cancer Res Treat. 2021;188:77–89.
Jerusalem G, et al. Safety of everolimus plus exemestane in patients with hormone-receptor-positive, HER2-negative locally advanced or metastatic breast cancer progressing on prior non-steroidal aromatase inhibitors: primary results of a phase IIIb, open-label, single-arm, expanded-access multicenter trial (BALLET). Ann Oncol. 2016;27:1719–25.
Lehmann BD, et al. Atezolizumab in combination with carboplatin and survival outcomes in patients with metastatic triple-negative breast cancer: the TBCRC 043 phase 2 randomized clinical trial. JAMA Oncol. 2024;10:193–201.
DeCensi A, et al. Lapatinib activity in premalignant lesions and HER-2-positive cancer of the breast in a randomized, placebo-controlled presurgical trial. Cancer Prev Res. 2011;4:1181–9.
Franzoi MA, Lambertini M, Ceppi M, Bruzzone M, de Azambuja E. Implication of body mass index (BMI) on the biological and clinical effects of endocrine therapy plus abemaciclib as neoadjuvant therapy for early breast cancer patients. Breast Cancer Res Treat. 2022;192:457–62.
Martel S, et al. Body mass index and weight change in patients With HER2-positive early breast cancer: exploratory analysis of the ALTTO BIG 2–06 trial. J Natl Compr Canc Netw. 2021;19:181–9.
Di Cosimo S, et al. Effect of body mass index on response to neo-adjuvant therapy in HER2-positive breast cancer: an exploratory analysis of the NeoALTTO trial. Breast Cancer Res. 2020;22:1–7.
Pfeiler G, et al. Impact of body mass index on treatment and outcomes in patients with early hormone receptor-positive breast cancer receiving endocrine therapy with or without palbociclib in the PALLAS trial. J Clin Oncol. 2022;40(16_suppl):518–518.
Franzoi MA, et al. Clinical implications of body mass index in metastatic breast cancer patients treated with abemaciclib and endocrine therapy. J Nat Cancer Inst. 2021;113:462–70.
Weight-Based Dosing vs Fixed Dosing of Pembrolizumab: an Economic Analysis – Hematology & Oncology. https://www.hematologyandoncology.net/archives/august-2018/weight-based-dosing-vs-fixed-dosing-of-pembrolizumab-an-economic-analysis/.
Hall E, et al. Economics of alternative dosing strategies for pembrolizumab and nivolumab at a single academic cancer center. Cancer Med. 2020;9:2106–12.
Freshwater T, et al. Evaluation of dosing strategy for pembrolizumab for oncology indications. J Immunother Cancer. 2017;5:1–9.
Ji Y, Jin JY, Hyman DM, Kim G, Suri A. Challenges and opportunities in dose finding in oncology and immuno-oncology. Clin Transl Sci. 2018;11:345–51.
Murphy R, Halford S, Symeonides SN. Project optimus, an FDA initiative: considerations for cancer drug development internationally, from an academic perspective. Front Oncol. 2023;13:1144056.
Griggs JJ, et al. Appropriate systemic therapy dosing for obese adult patients with cancer: ASCO Guideline update. J Clin Oncol. 2021;39:2037–48.
Silvestris N, et al. Antineoplastic dosing in overweight and obese cancer patients: an Associazione Italiana Oncologia Medica (AIOM)/Associazione Medici Diabetologi (AMD)/Società Italiana Endocrinologia (SIE)/Società Italiana Farmacologia (SIF) multidisciplinary consensus position paper. ESMO Open. 2021;6:100153.
Daousi C, et al. Prevalence of obesity in type 2 diabetes in secondary care: association with cardiovascular risk factors. Postgrad Med J. 2006;82:280.
Mandal A. Study of prevalence of type 2 diabetes mellitus and hypertension in overweight and obese people. J Family Med Prim Care. 2014;3:25.
Regmi D, Al-Shamsi S, Govender RD, Al Kaabi J. Incidence and risk factors of type 2 diabetes mellitus in an overweight and obese population: a long-term retrospective cohort study from a Gulf state. BMJ Open. 2020;10:e035813.
Wang Y, Beydoun MA. The obesity epidemic in the United States–gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28.
Anekwe CV, et al. Socioeconomics of obesity. Curr Obes Rep. 2020;9:272.
Bandera EV, Maskarinec G, Romieu I, John EM. Racial and ethnic disparities in the impact of obesity on breast cancer risk and survival: a global perspective. Adv Nutr. 2015;6:803.
Pasco JA, Nicholson GC, Brennan SL, Kotowicz MA. Prevalence of obesity and the relationship between the body mass index and body fat: cross-sectional, population-based data. PLoS ONE. 2012;7:e29580.
Ho-Pham LT, Lai TQ, Nguyen MTT, Nguyen TV. Relationship between body mass index and percent body fat in vietnamese: implications for the diagnosis of obesity. PLoS One. 2015;10:e0127198.
Shachar SS, Williams GR. The obesity paradox in cancer-moving beyond BMI. Cancer Epidemiol Biomarkers Prev. 2017;26:13–6.
Tafeit E, et al. Using body mass index ignores the intensive training of elite special force personnel. Exp Biol Med. 2019;244:873.
Banack HR, Wactawski-Wende J, Hovey KM, Stokes A. Is BMI a valid measure of obesity in post-menopausal women? Menopause. 2018;25:307.
Silvestris N, et al. Antineoplastic dosing in overweight and obese cancer patients: an Associazione Italiana Oncologia Medica (AIOM)/Associazione Medici Diabetologi (AMD)/Società Italiana Endocrinologia (SIE)/Società Italiana Farmacologia (SIF) multidisciplinary consensus position paper. ESMO Open. 2021;6:100153.
Isnaldi E, et al. Digital analysis of distant and cancer-associated mammary adipocytes. Breast Off J Eur Soc Mastol. 2020;54:179.
Umscheid CA, Margolis DJ, Grossman CE. Key concepts of clinical trials: a narrative review. Postgrad Med. 2011;123:194.
Malik L, Lu D. Eligibility criteria for phase I clinical trials: tight vs loose? Cancer Chemother Pharmacol. 2019;83:999–1002.
He J, Morales DR, Guthrie B. Exclusion rates in randomized controlled trials of treatments for physical conditions: a systematic review. Trials. 2020;21:1–11.
Lynce F, et al. Abstract CT142: TALAVE: Induction talazoparib (tala) followed by combined tala and avelumab in patients (pts) with advanced breast cancer (ABC). Cancer Res. 2023;83:CT142.
Hong R, et al. Palbociclib, trastuzumab, pyrotinib and fulvestrant in patients with brain metastasis from ER/PR positive, HER-2 positive breast cancer: Report from an interim analysis of a multicenter, prospective study in China, 2023;41: e13032–e13032. https://doi.org/10.1200/JCO.2023.41.16_suppl.e13032
Van Den Bogert CA, et al. Non-publication is common among phase 1, single-center, not prospectively registered, or early terminated clinical drug trials. PLoS ONE. 2016;11:e0167709.
Acknowledgements
Not applicable.
Funding
There was no funding specifically for this systematic review. However, J.V.C. and K.V.B. are funded by the KU Leuven Fund Nadine de Beauffort. In addition, K.V.B. is also supported by the Conquer Cancer – Lobular Breast Cancer Alliance Young Investigator Award. Any opinions, findings, and conclusions expressed in this material are those of the author(s) and do not necessarily reflect those of the American Society of Clinical Oncology® or Conquer Cancer®, or Lobular Breast Cancer Alliance. Research on breast cancer and obesity in the Laboratory for Translational Breast Cancer Research is funded by the European Research Council (ERC, FAT-BC 101003153).
Author information
Authors and Affiliations
Contributions
J.V.C, K.V.B. and C.D. developed the conceptualization and the methodology of the systematic review. The manuscript was written by J.V.C. and K.V.B. It was substantively revised and approved by M.M., T.G., H.L.N., I.N., A.S., A.D., P.N., S.K., H.W., K.P. and C.D.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
There are no conflicts of interest to declare for J.V.C., K.V.B., M.M., T.G., H.L.N., I.N., A.S., A.D., P.N., S.K. and C.D. KP: research grants paid to institution: MSD and Sanofi, speaker fees and honoraria for consultancy and advisory board functions: Astra Zeneca, Eli Lilly, Exact Sciences, Focus Patient, Gilead, MSD, Novartis, Pfizer, Roche, Seagen, speaker fees and honoraria for consultancy and advisory board functions paid to institution: Astra Zeneca, Eli Lilly, Exact Sciences, Gilead, MSD, Novartis, Pfizer, Roche, Seagen, stock options: Need Inc, travel grants: Astra Zeneca, Novartis, Pfizer, PharmaMar, Roche. HW: his institution received financial compensation on his behalf for advisory boards, lecture fees and/or consultancy fees from Immutep Pty, MSD, Astrazenca, Daiichi, AbbVie, Lilly, Roche, EISAI, Pfizer, Sirtex, Gilead. He received travel support from Pfizer and Roche.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Appendix: Supplementary Table 1:
Search terms clinical drug trials • Supplementary Table 2: Acquired data per included clinical drug trial, phase III and IV • Supplementary Table 3: Acquired data per included clinical drug trial, phase I and II.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Cauwenberge, J., Van Baelen, K., Maetens, M. et al. Reporting on patient’s body mass index (BMI) in recent clinical trials for patients with breast cancer: a systematic review. Breast Cancer Res 26, 81 (2024). https://doi.org/10.1186/s13058-024-01832-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-024-01832-7