Abstract
Background
Whether respiratory efforts and their timing can be reliably detected during pressure support ventilation using standard ventilator waveforms is unclear. This would give the opportunity to assess and improve patient–ventilator interaction without the need of special equipment.
Methods
In 16 patients under invasive pressure support ventilation, flow and pressure waveforms were obtained from proximal sensors and analyzed by three trained physicians and one resident to assess patient’s spontaneous activity. A systematic method (the waveform method) based on explicit rules was adopted. Esophageal pressure tracings were analyzed independently and used as reference. Breaths were classified as assisted or auto-triggered, double-triggered or ineffective. For assisted breaths, trigger delay, early and late cycling (minor asynchronies) were diagnosed. The percentage of breaths with major asynchronies (asynchrony index) and total asynchrony time were computed.
Results
Out of 4426 analyzed breaths, 94.1% (70.4–99.4) were assisted, 0.0% (0.0–0.2) auto-triggered and 5.8% (0.4–29.6) ineffective. Asynchrony index was 5.9% (0.6–29.6). Total asynchrony time represented 22.4% (16.3–30.1) of recording time and was mainly due to minor asynchronies. Applying the waveform method resulted in an inter-operator agreement of 0.99 (0.98–0.99); 99.5% of efforts were detected on waveforms and agreement with the reference in detecting major asynchronies was 0.99 (0.98–0.99). Timing of respiratory efforts was accurately detected on waveforms: AUC for trigger delay, cycling delay and early cycling was 0.865 (0.853–0.876), 0.903 (0.892–0.914) and 0.983 (0.970–0.991), respectively.
Conclusions
Ventilator waveforms can be used alone to reliably assess patient’s spontaneous activity and patient–ventilator interaction provided that a systematic method is adopted.
Similar content being viewed by others
Background
During mechanical ventilation patient–ventilator asynchrony is frequent and is associated with unfavorable outcomes [1,2,3,4]. Poor patient–ventilator interaction can be a marker of disease severity or result from inappropriate settings; it may be a cause of direct damage or can indirectly affect outcome through inappropriate sedation or undue prolongation of weaning [2, 4,5,6,7,8,9]. Asynchronies have different underlying mechanisms and may have different impacts on outcome as well. Thus, phenotyping patients according to their interaction with the ventilator can be important to identify patients at risk and guide treatments.
Ventilator waveform interpretation was originally described in the 90 s’ to assess patient–ventilator interaction [5, 10] and it was proposed as a skill that intensivists should possess in the era of mechanical ventilators displaying real-time waveforms [11]. Detection of major asynchronies (i.e., ineffective efforts, auto-triggered and double-triggered breaths) was found to be highly reproducible and reliable when using waveform recordings [2]. A few years later, however, another study showed a low sensitivity in detecting the same events when waveforms displayed by the ventilator were compared to electrical activity of the diaphragm [12]. It has then been suggested that specific training focused on ventilator waveform interpretation is needed to detect major asynchronies at the bedside [13]. In addition, no data are available about waveform detection of minor asynchronies such as trigger delay, early and late cycling. These “minor” asynchronies predispose to and are more frequent than “major” asynchronies [5, 8, 14, 15], accounting for more than 75% of the total asynchrony time in patients under pressure support ventilation [16]. Prerequisite for the detection of minor asynchronies is the ability to precisely identify the start and the end of patient’s spontaneous respiratory effort.
We designed a systematic and explicit method (the waveform method), based on simple specific rules based on respiratory physiology, to detect the activity of patient’s respiratory muscles from ventilator waveforms under pressure support ventilation. The aim of this study is to test the hypothesis that the waveform method is reliable and reproducible in providing a precise assessment of the timing of the inspiratory muscles’ effort. This could have a great potential for an automated real-time analysis of ventilator waveforms, to monitor synchrony at the bedside, to directly guide the ventilator triggering and cycling functions, to prevent asynchronies and improve patient–ventilator interaction during pressure support ventilation.
Materials and methods
In this prospective observational study, we enrolled mechanically ventilated patients in pressure support ventilation (PSV) mode with an esophageal balloon already inserted for clinical purposes, either because they displayed any form of asynchrony on the ventilator screen visible at the bedside or they were considered by clinicians to be uncomfortable from a ventilation standpoint. Tachypnea, activation of accessory muscles, abdominal paradox, diaphoresis, and/or agitation were considered clinical signs of respiratory discomfort. The study was approved by the ethics committee of our institution (Fondazione IRCCS Policlinico San Matteo, n. 41223) and written informed consent to use the recordings for research purposes was obtained from all patients as soon as they were able to provide it.
Recordings
Patients were connected to a Hamilton Medical G5 ventilator (Bonaduz, Switzerland) or a GE Healthcare Engstrom (Madison (WI), USA) ventilator, both equipped with proximal pressure and flow sensors (i.e., located at the Y-piece of the respiratory circuit) and an auxiliary port for esophageal balloon catheter (NutriVent catheter; Sidam, Mirandola, Italy) connection. Airway pressure (Paw), flow and esophageal pressure (Pes) tracings were recorded at 100 Hz for approximately 10 min.
To better describe the population studied, the expiratory time constant was computed from the tracings as the slope of expiratory flow/volume relationship during passive expiration [17]. Respiratory mechanics were then defined as being restrictive, normal or obstructive according to the expiratory time constant < 0.4 s, 0.4–0.7 s, > 0.7 s, respectively.
Reference method: esophageal pressure tracings to detect patient respiratory efforts
Esophageal pressure was used as the reference in the assessment of patient inspiratory activity [18, 19]. The start of patient’s inspiratory effort (patient Ti-start) was detected as a sudden negative deflection of Pes (Figs. 1,2).
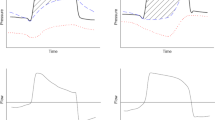
Waveform detection of patient respiratory activity and minor asynchronies. Good synchronization is shown in A while minor asynchronies are displayed in B (cycling is too early) and C (trigger is delayed and cycling is late). Airway (Paw, gray line) and esophageal (Pes, black line) pressures are displayed on the top and flow at the bottom. Gray-colored areas refer to subject’s neural inspiratory time according to Pes tracing. The start of patient’s inspiration can be detected as a negative deflection on both Paw and Pes (p1, p3 and p5) and as a positive deflection of flow (f1, f3 and f5). Normally the end of patient’s inspiration occurs at mid-relaxation of the inspiratory muscles and can be located at midpoint of the fast increase in Pes after its inspiratory nadir (p2, p4 and p6); this time point corresponds also to the start of a phase of exponential decay of flow (f2, f4 and f6). Substantial deviations from normal exponential decay of expiratory flow are associated with early cycling (B) and inspiratory trigger delay (C). Prolonged exponential decay of inspiratory flow is associated with a secondary phase of passive inflation due to cycling delay (C)
Waveform detection of patient respiratory activity and major asynchronies. Airway (Paw, gray line) and esophageal (Pes, black line) pressures are displayed on the top and flow at the bottom. Gray-colored areas refer to the subject’s neural inspiratory time according to Pes tracing. The breath in A is an autotriggered mechanical breath favored by heart noises that are evident both in airway and esophageal pressure tracings (p1). Conversely, no clear sign of patient’s inspiratory effort can be detected on flow, airway and esophageal pressure right before the mechanical breath; inspiratory flow shows exponential decay from its peak value, suggesting passive inflation (f1). In B, gray-colored area marks a patient’s inspiratory effort that is not recognized nor assisted by the ventilator. The start of patient’s inspiration can be detected as a negative deflection on Paw and Pes (p2) and a positive deflection of flow (f2) that interrupts the normal exponential decay of passive expiratory flow. The end of patient’s inspiration is located at mid-relaxation of inspiratory muscles (p3) and can be detected as the re-start of the normal exponential decay of expiratory flow (f3) and the end of a negative deflection of Paw (p4). In C, gray-colored area marks a single patient’s inspiratory effort that triggers two distinct mechanical breaths, separated by a brief expiratory phase (double trigger). The start of patient’s inspiration can be detected as a negative deflection on Paw and Pes (p5) and a positive deflection of flow (f4). The end of patient’s effort is located at mid-relaxation of inspiratory muscles (p6), occurs well after the cycling of the second mechanical breath and corresponds to the start of a normal, exponentially decaying expiratory flow (f5)
The end of inspiration was determined as follows. In normal unassisted breathing, inspiratory to expiratory flow reversal occurs before full relaxation, when the outward pressure still generated by the inspiratory muscles is exactly counterbalanced by the inward pressure generated by the elastic recoil of the respiratory system [20]. The exact time point of flow reversal depends on respiratory mechanics and breathing pattern, but can be approximated at mid-relaxation of the inspiratory muscles [21, 22]. In the absence of a universal definition [23], the end of patient’s inspiration (patient Ti-end) was pragmatically located at midpoint of the fast increase in Pes after its inspiratory nadir (Figs. 1,2).
Waveform method to detect patient’s respiratory effort
The Waveform method is based on the analysis of flow and airway pressure, according to five general physiological principles displayed in Table 1 and to the specific rules detailed below [5, 10, 11, 22].
The start of a subject’s inspiratory effort (wave Ti-start) is detected on flow, as a sudden positive deflection that interrupts a phase of exponential decay, and/or on airway pressure, as a sudden negative deflection that interrupts a phase of stable Paw (Figs. 1,2).
For the end of a subject’s inspiration (wave Ti-end) it is assumed that the interruption of an inspiratory effort is followed by a phase of exponential decay of flow. Therefore, the end of the patient’s inspiratory effort is pinpointed at the start of a passive exponential decay of flow, irrespective of the direction of flow (inspiratory or expiratory). Examples are provided in Figs. 1 and 2. If cycling is optimal, the peak expiratory flow is immediately followed by an exponential decay (Fig. 1A). If cycling occurs early, a delayed start of the exponential decay of expiratory flow marks the end of the inspiratory effort occurring during expiration (Fig. 1B). If cycling occurs late, an exponential decay occurs during the inspiratory flow period after a change in slope (Fig. 1C). A pure exponential decay during the whole inspiration indicates auto-triggering (Fig. 2A). In case of ineffective effort, the normal exponential decay of expiratory flow is interrupted (Fig. 2B). The end of a negative deflection of Paw can also be associated with the end of a subject’s inspiration (Fig. 1B).
Reference assessment of patient–ventilator interaction
The start of the mechanical inspiratory and expiratory phases (machine Ti-start and machine Ti-end) were detected on Paw as the start of pressurization and depressurization. According to mechanical and patients’ reference times, breaths were defined as assisted, auto-triggered, double-triggered (Fig. 2C) or ineffective. In assisted breaths, machine ΔTi-start and ΔTi-end were computed as machine Ti-start minus patient Ti-start and machine Ti-end minus patient Ti-end. The time gap between the patient and the ventilator was considered substantial when > 250 ms, corresponding to > 25% of a normal inspiratory time. Thus, trigger delay was defined as machine ΔTi-start > 250 ms; early and late cycling were defined as machine ΔTi-end < − 250 ms and > 250 ms respectively. Breaths in which machine ΔTi-start was < 250 ms, breaths in which machine ΔTi-end (absolute value) was < 250 ms, and breaths in which both machine ΔTi-start and ΔTi-end (absolute values) were < 250 ms were counted.
Asynchrony index was the percentage of breaths affected by major asynchronies and was computed as the sum of auto-triggered, ineffective and double-triggered breaths, divided by the total number of breaths. Total asynchrony time was the time (expressed as percentage of total recording time) during which the ventilator and the patient were not synchronous; it was computed as the sum of machine ΔTi-start and ΔTi-end (absolute value) in assisted breaths plus the time length of auto-triggered breaths and of ineffective efforts.
Waveform method performance
Each patient’s recording was analyzed by a “reference” operator (provided with both the standard waveforms and Pes tracing) and by another “waveform” operator (blinded to Pes), in order to assess the agreement between the reference and the waveform method. Additionally, a random selection of 30 min (approximately 120 s and 30 breaths per patient) was analyzed by three operators, in order to assess the inter-operator agreement of the waveform method (details are provided in Additional file 1: Table S1). All the operators (three senior physicians and one resident) underwent previous specific training and had experience (at least 2 years) of waveform interpretation for both clinical and research purposes. To assess the reliability of the waveform method, detected breaths (efforts detected on Pes and on waveforms), false positive breaths (efforts detected on waveforms but not on Pes) and false negative breaths (efforts detected on Pes but not on waveforms) were counted. To assess the precision in detecting the start and the end of the patient effort, wave ΔTi-start (wave Ti-start minus patient Ti-start) and wave ΔTi-end (wave Ti-end minus patient Ti-end) were computed; moreover, breaths in which wave ΔTi-start was < 250 ms, breaths in which wave ΔTi-end (absolute value) was < 250 ms, and breaths in which both wave ΔTi-start and wave ΔTi-end (absolute values) were < 250 ms were counted.
Similar to the reference analysis, wave Ti-start and wave Ti-end were used to assess patient–ventilator interaction with the waveform method and the findings compared with the reference.
Statistical analysis
The primary endpoint of the study was the percentage of spontaneous efforts detected by the waveform method. To get a confidence interval of ± 2% with a confidence level of 99%, a sample of 4160 breaths was required. Secondary endpoints included the percentage of detected efforts in which both wave ΔTi-start and wave ΔTi-end were < 250 ms (absolute values), the agreement between the waveform method and the reference in detecting major and minor asynchronies, and the inter-rater agreement when the method was applied by different physicians. Agreement of the waveform method with the reference in rating breaths as assisted, auto-triggered, double-triggered or ineffective was assessed with Cohen’s kappa. Sensitivity, specificity, area under the curve, positive and negative predictive values in detection of trigger delay, early and late cycling were computed. Asynchrony times assessed with the waveform method were compared to the reference with paired Wilcoxon test. Agreement among raters was assessed with intraclass correlation coefficient for single measures. Categorical variables are displayed as absolute number and percentage, continuous variables are displayed as mean value ± standard deviation or median value and interquartile range (IQR), as appropriate.
Results
We analyzed 4426 breaths that were recorded (total recording time 174 min) in sixteen patients: 7 males and 9 females, 55 (IQR 43 to 63] years old, under pressure support ventilation with evidence of suboptimal interaction with the mechanical ventilator, as defined in methods. Causes of respiratory failure were ARDS (2), pneumonia (2), lung fibrosis (1), COPD decompensation (3), congestive heart failure (2), postoperative (3), sepsis (2) and pancreatitis (1). According to the expiratory time constant, 4 patients displayed a restrictive flow pattern, 5 normal and 7 obstructive. Patients’ characteristics are summarized in Additional file 1:Table S2.
Breaths and delays: machine performance
Out of 4426 total breaths, 3444 (77.8%) were detected and assisted, 976 (22.1%) were not detected by the ventilator (ineffective efforts) and 6 (0.1%) were auto-triggered; no double-triggered breaths were observed. In assisted breaths, machine ΔTi-start was 200 ± 139 ms ranging 0 to 1002 ms and machine ΔTi-end was 195 ± 361 ms ranging − 1023 to 2258 ms. Trigger delay was detected in 897 (26.0%) assisted breaths, late cycling occurred in 1231 (35.7%) and early cycling in 439 (12.7%). Machine ΔTi-start and ΔTi-end were < 250 ms in 2547 (74.0%) and 1774 (51.5%) assisted breaths respectively (Fig. 3); breaths that were properly assisted without minor asynchronies were 1321 (38.4%). Early cycling was detected only in the 4 restrictive patients, whereas late cycling was detected in all obstructive and normal patients and in 2 restrictive patients (Additional file 1:Table S3).
Performance of the mechanical ventilator versus the waveform method in detecting patient inspiratory efforts. Compared to the mechanical ventilator (blue bars), the waveform method (red bars) detected substantially more patient efforts. Among detected breaths, the proportion of those without minor asynchronies (ΔTi-start and/or ΔTi-end < 0.25 s) was larger for the waveform method. For detected, false positive and false negative breaths, % values refer to the total number of breaths (N = 4426); for breaths with ΔTi-start and/or ΔTi-end < 0.25 s, % values refer to the number of detected breaths (N = 3444 for the machine, N = 4397 for the waveform method). *p < 0.0001 mechanical ventilator versus waveform method.
The Asynchrony Index was 5.9% (IQR 0.6–29.6) ranging 0.0–45.5. The total asynchrony time represented 22.4% (16.3–30.1) of total recording time, ranging 11.3–47.3 (Additional file 1: Figure S1). Minor asynchronies lasted more than major ones (p = 0.0013): 16.5% (14.0–20.4) of total recording time, accounting for 92.1% (66.2–99.2) of total asynchrony time.
Performance of the waveform method
Among 4420 spontaneous efforts identified on the esophageal pressure tracings, 4397 (99.5%) were also detected by the expert waveform analysis using only airway pressure and flow. False negative (not detected) breaths were 23 (0.5%; p < 0.0001 vs. machine) and only 1 (0.0%) false positive breath was observed (Fig. 3). For breaths detected on waveforms, wave ΔTi-start was − 7 ± 106 ms (p < 0.0001 vs. machine ΔTi-start) and wave ΔTi-end was − 21 ± 96 ms (p < 0.0001 vs. machine ΔTi-end). Overall, breaths with wave ΔTi-start < 250 ms were 4200 (95.5%; p < 0.0001 vs. machine), breaths with wave ΔTi-end < 250 ms were 4262 (96.9%; p < 0.0001 vs. machine) and breaths with both wave ΔTi-start and ΔTi-end < 250 ms were 4071 (92.6%; p < 0.0001 vs. machine). Findings in individual patients are displayed in Additional file 1: Table S4. The global agreement between the reference and the waveform methods in defining breaths as assisted, auto-triggered, double-triggered or ineffective was excellent, as assessed by a Cohen’s Kappa of 0.98 (0.98 – 0.99). Out of 4426 total breaths (4420 patients efforts and 6 autotriggers), 17 ineffective efforts were undetected, 6 assisted breaths were erroneously considered autotriggers and 1 autotrigger was erroneously considered an assisted breath by the waveform method (Additional file 1: Table S5). The Asynchrony Index did not differ when assessed with the waveform method versus esophageal pressure.
Sensitivity, specificity, positive and negative predictive values of the waveform method in detecting asynchronies are reported in Table 2. Area under the curve (95% confidence interval; p value) for trigger delay, cycling delay and early cycling was 0.865 (0.853–0.876; p < 0.0001), 0.903 (0.892–0.914; p < 0.0001) and 0.983 (0.970–0.991; p < 0.0001) respectively (Additional file 1: Figure S2).
Total asynchrony time and asynchrony times related to ineffective efforts, auto-triggered breaths, trigger delay, early and late cycling were not different when assessed with the Waveform method compared to the reference (Additional file 1: Figure S1).
Among the three “waveform” operators, the agreement for single measures was 0.99 (0.98 – 0.99) in classifying breaths as auto-triggered, double triggered, assisted or ineffective, 0.84 (0.76 – 0.89) in measuring ΔTi-start and 0.96 (0.90 – 0.98) in measuring ΔTi-end.
Discussion
The main findings of this study are: (1) the waveform method allows a very precise assessment of the timing of patients’ spontaneous activity using only pressure and flow waveforms during PSV, (2) the method is highly reproducible and reliable in detecting both major and minor asynchronies, and (3) during PSV the majority of total asynchrony time is related to “minor” asynchronies.
In the present study we prospectively enrolled ICU patients under PSV with evidence of suboptimal interaction with the mechanical ventilator, as suggested by subject’s discomfort and/or asynchronies visible on the ventilator screen. In this selected population, experts were able to detect more than 99% of patients’ spontaneous efforts looking at standard ventilator waveforms, and in more than 90% of cases, both the start and the end of respiratory efforts were identified with good precision. Waveform detection of major asynchronies was almost in perfect agreement with the reference with very good agreement among different raters. The waveform method allowed a precise assessment of the timing of patients’ spontaneous effort. Thus waveform recognition of minor asynchronies is highly reliable and reproducible as well. Looking at the composition of total asynchrony time in individual patients, the picture was very similar whether the assessment was performed with the reference or the waveform method.
Once asynchronies are detected at the bedside, patient–ventilator interaction can be optimized with both general and specific measures [5,6,7, 10, 21, 22, 24,25,26,27]. Proper ventilator settings -including pressure support level, pressurization rate, inspiratory and expiratory trigger sensitivity- can substantially improve the interaction. Adjustments of ventilator settings must be guided by bedside assessment of asynchronies and be individualized [5, 11, 22, 24,25,26,27,28,29,30,31]. Although esophageal pressure is the reference method to assess patient’s respiratory activity and patient–ventilator interaction [18, 19], it is moderately invasive, requires special equipment and some expertise to manage technical issues, and generates additional costs as well. Because asynchronies are very frequent in mechanically ventilated patients, esophageal pressure cannot be the standard approach. Our findings suggest that the interpretation of bedside waveform, readily available, can identify patients with poor interaction with the mechanical ventilator, quantify the problem, define the specific asynchrony pattern and guide the ventilator setting.
Automatic real-time analysis of ventilator waveforms has been described to monitor and possibly improve patient–ventilator interaction [4, 32,33,34]. Triggering and cycling-off functions guided by waveforms were originally implemented on mechanical ventilators for noninvasive respiratory support to overcome the issue of large air leaks [35]. The performance of waveform method, designed for invasive ventilation setting and tested in intubated patients, should encourage further advancement. Automation of the method is particularly attractive having the potential to decrease asynchronies and being at the same time non-invasive, low-cost and easy to be integrated in a mechanical ventilator. Machine learning has been already applied in the field with promising results [36,37,38,39].
Our results are different from those of Colombo and colleagues, who observed good specificity but insufficient sensitivity in waveform detection of major asynchronies [12]. Three main aspects explain the different performances of waveform interpretation in the present study. First, we explicitly described a method based on general principles and specific rules that was adopted beforehand. All the raters of the present study were considered reasonably well trained in ventilator waveform analysis, whereas clinical experience in treating ICU mechanically ventilated patients is not invariably associated with this skill [13]. To note, one of our expert raters was a resident when she analyzed the recordings of the present study. Second, all mechanical ventilators were equipped with proximal sensors and this may have substantially improved the reliability of pressure and flow tracings. Third, as reference signal we used esophageal pressure instead of electrical activity of the diaphragm (EADi); differently from EADi, esophageal pressure is affected by the activity of other main and accessory respiratory muscles thus providing a more comprehensive information on patient’s spontaneous activity. Moreover, the use of EADi to guide positive-pressure ventilation has been associated with a significant increase in auto-triggered and double-triggered breaths, suggesting that EADi may sometimes lack specificity [40,41,42].
Total asynchrony time was computed in our patients as the sum of all the different asynchronous events. Overall, asynchronies accounted for 22% of the time on mechanical ventilation with values close to 50%. Most of this time was related to the so-called minor asynchronies, a result consistent with previous findings [5, 16]; in particular, delayed cycling is confirmed to be a major problem of PSV [43,44,45]. Minor asynchronies predispose to major ones: late cycling promotes dynamic hyperinflation finally leading to ineffective efforts [5, 46], whereas early cycling is a pre-requisite for double triggering [8, 24]. Different asynchronies have also different meanings and can impact differently on outcome. For instance, trigger delay, late cycling and ineffective efforts are often associated with over-assistance and/or over-sedation [2, 5, 28, 43], predisposing to diaphragm disuse atrophy, prolonged mechanical ventilation and ICU stay [2,3,4, 29]. Both early cycling and ineffective efforts correspond to eccentric contractions of the inspiratory muscles, a potential mechanism of muscle fiber injury [9]. Double trigger with associated breath stacking represents instead an obvious risk of lung baro- and volo-trauma [8]. For all these reasons, it might be very useful to recognize (and hopefully correct or prevent) all the different asynchronous events at the bedside.
This study has limitations. First, the study population was small, raising the question whether our findings are generalizable or not. However, our case-mix was quite representative of a general ICU population in terms of age, etiology of respiratory failure and respiratory mechanics; moreover, the number of analyzed breaths was high and exceeded the sample size requirements. Second, our experts performed an off-line analysis of ventilator waveforms recorded by proximal sensors and the results could be different if the method was applied automatically by the machine and/or proximal sensors were not available.
Conclusions
Our findings support the notion that standard ventilator waveforms can reliably be used to accurately assess patient’s spontaneous activity and patient–ventilator interaction at the bedside, provided that a systematic method is adopted after sufficient training.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- PSV:
-
Pressure support ventilation
- Paw:
-
Airway pressure
- Pes:
-
Esophageal pressure
- Patient Ti-start:
-
The start of patient’s inspiratory effort detected on esophageal pressure wave
- Patient Ti-end:
-
The end of patient’s inspiratory effort detected on esophageal pressure wave
- Wave Ti-start:
-
The start of a subject’s inspiratory effort detected on flow and/or pressure waveforms
- Wave Ti-end:
-
The end of a subject’s inspiratory effort detected on flow and/or pressure waveforms
- Machine Ti-start:
-
The start of the mechanical inspiratory phase
- Machine Ti-end:
-
The end of the mechanical expiratory phase
- Machine ΔTi-start:
-
Machine Ti-start minus patient Ti-start
- Machine ΔTi-end:
-
Machine Ti-end minus patient Ti-end
- Wave ΔTi-start:
-
Wave Ti-start minus patient Ti-start
- Wave ΔTi-end:
-
Wave Ti-end minus patient Ti-end
- IQR:
-
Interquartile range
- ARDS:
-
Acute respiratory distress syndrome
- COPD:
-
Chronic obstructive pulmonary disease
- ICU:
-
Intensive care unit
- EaDi:
-
Electrical activity of the diaphragm
References
Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M. Patient–ventilator trigger asynchrony in prolonged mechanical ventilation. Chest. 1997;112(6):1592–9.
Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient–ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515–22.
De Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37(10):2740–5.
Blanch L, Villagra A, Sales B, Montanya J, Lucangelo U, Luján M, García-Esquirol O, Chacón E, Estruga A, Oliva JC, Hernández-Abadia A, Albaiceta GM, Fernández-Mondejar E, Fernández R, Lopez-Aguilar J, Villar J, Murias G, Kacmarek RM. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015;41(4):633–41.
Fabry B, Guttmann J, Eberhard L, Bauer T, Haberthür C, Wolff G. An analysis of desynchronization between the spontaneously breathing patient and ventilator during inspiratory pressure support. Chest. 1995;107(5):1387–94.
Nava S, Bruschi C, Fracchia C, Braschi A, Rubini F. Patient–ventilator interaction and inspiratory effort during pressure support ventilation in patients with different pathologies. Eur Respir J. 1997;10(1):177–83.
de Wit M, Pedram S, Best AM, Epstein SK. Observational study of patient–ventilator asynchrony and relationship to sedation level. J Crit Care. 2009;24(1):74–80.
Pohlman MC, McCallister KE, Schweickert WD, Pohlman AS, Nigos CP, Krishnan JA, et al. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit Care Med. 2008;36(11):3019–23.
Gea J, Zhu E, Gáldiz JB, Comtois N, Salazkin I, Fiz JA, Grassino A. Functional consequences of eccentric contractions of the diaphragm. Arch Bronconeumol. 2009;45(2):68–74.
Giannouli E, Webster K, Roberts D, Younes M. Response of ventilator-dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med. 1999;159(6):1716–25.
Georgopoulos D, Prinianakis G, Kondili E. Bedside waveform interpretation as a tool to identify patient–ventilator asynchronies. Intensive Care Med. 2006;32(1):34–47.
Colombo D, Cammarota G, Alemani M, Carenzo L, Barra FL, Vaschetto R, Slutsky AS, Della Corte F, Navalesi P. Efficacy of ventilator waveforms observation in detecting patient–ventilator asynchrony. Crit Care Med. 2011;39(11):2452–7.
Ramirez II, Arellano DH, Adasme RS, Landeros JM, Salinas FA, Vargas AG, Vasquez FJ, Lobos IA, Oyarzun ML, Restrepo RD. Ability of ICU health-care professionals to identify patient–ventilator asynchrony using waveform analysis. Respir Care. 2017;62(2):144–9.
Beck J, Gottfried SB, Navalesi P, Skrobik Y, Comtois N, Rossini M, Sinderby C. Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med. 2001;164(3):419–24.
Mauri T, Bellani G, Grasselli G, Confalonieri A, Rona R, Patroniti N, Pesenti A. Patient–ventilator interaction in ARDS patients with extremely low compliance undergoing ECMO: a novel approach based on diaphragm electrical activity. Intensive Care Med. 2013;39(2):282–91.
Mojoli F, Bianzina S, Torriglia F, Viola L, Bianchi IM, Orlando A, Pozzi M, Braschi A. Continuous monitoring of patient–ventilator interaction in ICU patients undergoing prolonged mechanical ventilation. Intensive Care Med. 2014;40(Suppl 1):A0112.
Brunner JX, Laubscher TP, Banner MJ, Iotti G, Braschi A. Simple method to measure total expiratory time constant based on the passive expiratory flow-volume curve. Crit Care Med. 1995;23:1117–22.
Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, Mojoli F, Chiumello D, Piquilloud L, Grasso S, Jubran A, Laghi F, Magder S, Pesenti A, Loring S, Gattinoni L, Talmor D, Blanch L, Amato M, Chen L, Brochard L, Mancebo J. PLeUral Pressure Working Group: esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42(9):1360–73.
Akoumianaki E, Maggiore SM, Valenza F, Bellani G, Jubran A, Loring SH, Pelosi P, Talmor D, Grasso S, Chiumello D, Guérin C, Patroniti N, Ranieri VM, Gattinoni L, Nava S, Terragni PP, Pesenti A, Tobin M, Mancebo J, Brochard L. PLUG Working Group: the application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med. 2014;189(5):520–31.
Younes M. Proportional assist ventilation, a new approach to ventilatory support. Theory. Am Rev Respir Dis. 1992;145(1):114–20.
Yamada Y, Du HL. Analysis of the mechanisms of expiratory asynchrony in pressure support ventilation: a mathematical approach. J Appl Physiol. 2000;88(6):2143–50.
Mojoli F, Iotti GA, Arnal JM, Braschi A. Is the ventilator switching from inspiration to expiration at the right time? Look at waveforms! Intensive Care Med. 2016;42(5):914–5.
Rittayamai N, Phuangchoei P, Tscheikuna J, Praphruetkit N, Brochard L. Effects of high-flow nasal cannula and non-invasive ventilation on inspiratory effort in hypercapnic patients with chronic obstructive pulmonary disease: a preliminary study. Ann Intensive Care. 2019;9:122.
Subirà C, de Haro C, Magrans R, Fernández R, Blanch L. Minimizing asynchronies in mechanical ventilation: current and future trends. Respir Care. 2018;63(4):464–78.
Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L. Reduction of patient–ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med. 2008;34(8):1477–86.
Tassaux D, Gainnier M, Battisti A, Jolliet P. Impact of expiratory trigger setting on delayed cycling and inspiratory muscle workload. Am J Respir Crit Care Med. 2005;172(10):1283–9.
Tokioka H, Tanaka T, Ishizu T, Fukushima T, Iwaki T, Nakamura Y, Kosogabe Y. The effect of breath termination criterion on breathing patterns and the work of breathing during pressure support ventilation. Anesth Analg. 2001;92(1):161–5.
Leung P, Jubran A, Tobin MJ. Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am J Respir Crit Care Med. 1997;155(6):1940–8.
Hudson MB, Smuder AJ, Nelson WB, Bruells CS, Levine S, Powers SK. Both high level pressure support ventilation and controlled mechanical ventilation induce diaphragm dysfunction and atrophy. Crit Care Med. 2012;40(4):1254–60.
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, Rittayamai N, Lanys A, Tomlinson G, Singh JM, Bolz SS, Rubenfeld GD, Kavanagh BP, Brochard LJ, Ferguson ND. Evolution of diaphragm thickness during mechanical ventilation. Impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192(9):1080–8.
Harnisch LO, Zippel C, Herrmann P, Quintel M, Moerer O. Adjusting ventilator off-cycling in invasively ventilated COPD patients needs comprehensive adjustments. Minerva Anestesiol. 2016;82(7):743–50.
Younes M, Brochard L, Grasso S, Kun J, Mancebo J, Ranieri M, Richard JC, Younes H. A method for monitoring and improving patient: ventilator interaction. Intensive Care Med. 2007;33(8):1337–46.
Mojoli F, Orlando A, Currò I, Pozzi M, Venti A, Matrone G, Magenes G, Braschi A. Automatic detection of patient–ventilator asynchronies during pressure support ventilation. Intensive Care Med. 2010;36(Suppl 2):S111.
Mulqueeny Q, Ceriana P, Carlucci A, Fanfulla F, Delmastro M, Nava S. Automatic detection of ineffective triggering and double triggering during mechanical ventilation. Intensive Care Med. 2007;33(11):2014–8.
Prinianakis G, Kondili E, Georgopoulos D. Effects of the flow waveform method of triggering and cycling on patient–ventilator interaction during pressure support. Intensive Care Med. 2003;29(11):1950–9.
Gholami B, Phan TS, Haddad WM, Cason A, Mullis J, Price L, Bailey JM. Replicating human expertise of mechanical ventilation waveform analysis in detecting patient–ventilator cycling asynchrony using machine learning. Comput Biol Med. 2018;1(97):137–44.
Bakkes THGF, Montree RJH, Mischi M, Mojoli F, Turco S. A machine learning method for automatic detection and classification of patient–ventilator asynchrony. Annu Int Conf IEEE Eng Med Biol Soc. 2020;2020:150–3.
Casagrande A, Quintavalle F, Fernandez R, Blanch L, Ferluga M, Lena E, Fabris F, Lucangelo U. An effective pressure-flow characterization of respiratory asynchronies in mechanical ventilation. J Clin Monit Comput. 2021;35(2):289–96.
Pham T, Montanya J, Telias I, Piraino T, Magrans R, Coudroy R, Damiani LF, Mellado Artigas R, Madorno M, Blanch L, Brochard L. Automated detection and quantification of reverse triggering effort under mechanical ventilation. BEARDS study investigators. Crit Care. 2021;25(1):60.
Demoule A, Clavel M, Rolland-Debord C, Perbet S, Terzi N, Kouatchet A, Wallet F, Roze H, Vargas F, Guerin C, Dellamonica J, Jaber S, Brochard L, Similowski T. Neurally adjusted ventilatory assist as an alternative to pressure support ventilation in adults: a French multicentre randomized trial. Intensive Care Med. 2016;42(11):1723–32.
Piquilloud L, Vignaux L, Bialais E, Roeseler J, Sottiaux T, Laterre PF, Jolliet P, Tassaux D. Neurally adjusted ventilatory assist improves patient–ventilator interaction. Intensive Care Med. 2011;37(2):263–71.
Schmidt M, Kindler F, Cecchini J, Poitou T, Morawiec E, Persichini R, Similowski T, Demoule A. Neurally adjusted ventilatory assist and proportional assist ventilation both improve patient–ventilator interaction. Crit Care. 2015;19:56.
Spahija J, de Marchie M, Albert M, Bellemare P, Delisle S, Beck J, Sinderby C. Patient–ventilator interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit Care Med. 2010;38(2):518–26.
Costa R, Spinazzola G, Cipriani F, Ferrone G, Festa O, Arcangeli A, Antonelli M, Proietti R, Conti G. A physiologic comparison of proportional assist ventilation with load-adjustable gain factors (PAV+) versus pressure support ventilation (PSV). Intensive Care Med. 2011;37(9):1494–500.
Mojoli F, Braschi A. Effectiveness of cycling-off during pressure support ventilation. Intensive Care Med. 2004;30(5):1000.
Younes M, Kun J, Webster K, Roberts D. Response of ventilator-dependent patients to delayed opening of exhalation valve. Am J Respir Crit Care Med. 2002;166(1):21–30.
Acknowledgements
Not applicable.
Funding
No fundings were received for the present study.
Author information
Authors and Affiliations
Contributions
FM designed the study, analyzed the data and wrote the manuscript, FM, AO, MP, IMB and EA analysed the patients’ offline registrations, LB, GAI and AB revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Fondazione IRCCS Policlinico San Matteo (reference number 41223) and written informed consent to participation was obtained from all patients.
Consent for publication
Written informed consent for publication was obtained from all patients.
Competing interests
FM received fee for lectures from Hamilton Medical, GE healthcare and Seda Spa; a consultancy agreement is active between University of Pavia and Hamilton Medical; LB's laboratory received research grants from Medtronic and Draeger, equipment from Fisher Paykel, Sentec, Philips, Air Liquide, lecture's fees from Fisher Paykel; AO received a fee from Hamilton Medical for manuscript preparation; MP received fees for lectures from Hamilton Medical; GAI is a Medical Consultant for Hamilton Medical and received fees for lectures from Eurosets, Burke&Burke and Intersurgical; all the other authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Patients' characteristics and waveform method performance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mojoli, F., Pozzi, M., Orlando, A. et al. Timing of inspiratory muscle activity detected from airway pressure and flow during pressure support ventilation: the waveform method. Crit Care 26, 32 (2022). https://doi.org/10.1186/s13054-022-03895-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-03895-4