Abstract
Background
Continuous, reliable evaluation of left ventricular (LV) contractile function in patients with advanced heart failure requiring intensive care remains challenging. Continual monitoring of dP/dtmax from the arterial line has recently become available in hemodynamic monitoring. However, the relationship between arterial dP/dtmax and LV dP/dtmax remains unclear. This study aimed to determine the relationship between arterial dP/dtmax and LV dP/dtmax assessed using echocardiography in patients with acute heart failure.
Methods
Forty-eight patients (mean age 70.4 years [65% male]) with acute heart failure requiring intensive care and hemodynamic monitoring were recruited. Hemodynamic variables, including arterial dP/dtmax, were continually monitored using arterial line pressure waveform analysis. LV dP/dtmax was assessed using continuous-wave Doppler analysis of mitral regurgitation flow.
Results
Values from continual arterial dP/dtmax monitoring were significantly correlated with LV dP/dtmax assessed using echocardiography (r = 0.70 [95% confidence interval (CI) 0.51–0.82]; P < 0.0001). Linear regression analysis revealed that LV dP/dtmax = 1.25 × (arterial dP/dtmax) (P < 0.0001). Arterial dP/dtmax was also significantly correlated with stroke volume (SV) (r = 0.63; P < 0.0001) and cardiac output (CO) (r = 0.42; P = 0.0289). In contrast, arterial dP/dtmax was not correlated with SV variation, dynamic arterial elastance, heart rate, systemic vascular resistance (SVR), or mean arterial pressure. Markedly stronger agreement between arterial and LV dP/dtmax was observed in subgroups with higher SVR (N = 28; r = 0.91; P < 0.0001), lower CO (N = 26; r = 0.81; P < 0.0001), and lower SV (N = 25; r = 0.60; P = 0.0014). A weak correlation was observed in the subjects with lower SVR (N = 20; r = 0.61; P = 0.0004); in the subgroups with higher CO (N = 22) and higher SV (N = 23), no significant correlation was found.
Conclusion
Our results suggest that in patients with acute heart failure requiring intensive care with an arterial line, continuous calculation of arterial dP/dtmax may be used for monitoring LV contractility, especially in those with higher SVR, lower CO, and lower SV, such as in patients experiencing cardiogenic shock. On the other hand, there was only a weak or no significant correlation in the subgroups with higher CO, higher SV, and lower SVR.
Similar content being viewed by others
Background
Left ventricular (LV) contractility is one of the most important parameters determining LV performance and cardiac function and, therefore, directly influences global hemodynamic status [1]. Clinical conditions with impaired LV contractility, such as heart failure or septic cardiomyopathy, are frequent subjects of intensive and acute cardiology care [1]. There is, therefore, an apparent clinical need for bedside measurement or even monitoring of contractility. However, current options for the assessment of LV contractility are significantly limited. The reference method for the measurement of LV contractility (i.e., LV end-systolic elastance [2]) cannot be used in routine clinical practice due to invasiveness and technical issues [3, 4]. The maximum rate of LV pressure rise during ventricular contraction (LV dP/dtmax) has been adopted as a surrogate marker of LV inotropic state and contractility [5]. This parameter is determinable in clinical settings; however, it requires direct LV pressure measurement, which is impractical and too invasive for LV contractility monitoring. LV dP/dtmax can also be estimated non-invasively using echocardiographic techniques [6, 7]. However, although this measurement can be performed repeatedly, it is not feasible for continuous monitoring and is frequently limited by low-quality signal.
Recently, a new surrogate has been proposed—arterial dP/dtmax. This parameter can be calculated from the arterial pressure waveform, obtained minimally invasively from a peripheral arterial line [8,9,10] or even non-invasively [11]. Arterial dP/dtmax is, therefore, available bedside and in patients with an arterial line already used for pressure monitoring and blood gas analyses; it does not require any additional invasive access. Moreover, arterial dP/dtmax can be measured on a beat-by-beat basis and, therefore, continually monitored. On the other hand, arterial dP/dtmax is not only determined by LV contraction but is also influenced by various peripheral arterial factors and load conditions [8,9,10,11]. Recently, several experimental studies demonstrating a significant relationship between arterial dP/dtmax and LV contractility have been published [8,9,10]. To date, however, clinical studies focusing on the relationship between arterial and LV dP/dtmax in patients with acute heart failure requiring intensive care and an arterial line are lacking. The aim of our study was, therefore, to assess the relationship between arterial and LV dP/dtmax in this patient population.
Methods
Study population
Consecutive patients admitted between January and September 2018 to the cardiology intensive care unit due to acute heart failure requiring an arterial line for invasive blood pressure monitoring and central venous catheter were eligible for the study. Patients with moderate to severe aortic stenosis, those who required mechanical circulatory support, and those with absence of mitral regurgitation enabling measurement of LV dP/dtmax were excluded. All patients have to be at the time of measurement on stable doses of inotropes/vasopressors, on stable ventilation support, and with regular cardiac rhythm.
Hemodynamic measurement
Arterial blood pressure (mean), central venous pressure (mean), heart rate, cardiac output (CO), stroke volume (SV), dynamic arterial elastance, and systemic vascular resistance (SVR) were measured using a clinical monitoring platform (EV1000, equipped with HPI software, Edwards Lifesciences, Irvine, CA, USA) connected to the arterial and central venous lines. SVR was calculated using the formula: SVR = 80 × (MAP − CVP)/CO. The dynamic arterial elastance was defined as the ratio of pulse pressure variation and stroke volume variation. All parameters were calculated in the 20-s interval that contains few respiratory cycles. An arterial catheter was inserted into the left or right radial artery, and the left or right jugular vein was used for central venous access, with the tip of catheter in the superior vena cava.
dP/dtmax measurement
Arterial dP/dtmax was measured from the arterial pressure curve by the EV1000 system and HPI software. The system calculates dP/dtmax for each beat in a 20-s cycle, then the median value of all the dP/dtmax values in the 20-s interval is displayed; values obtained at the time of LV dP/dtmax were used in the analysis. LV dP/dtmax was measured at the end of expiration using transthoracic echocardiography (Phillips CX50, Amsterdam, The Netherlands) from the analysis of the mitral regurgitation jet by continuous-wave Doppler; calculation was based on the time interval (T) between blood flow of 1 m/s and 3 m/s using the formula: LV dP/dtmax = 32/T [6, 7]. Three measurements were performed at one time, and the mean values were used for analysis. The echocardiographic measurements were performed by an experienced physician who was blinded to the arterial dP/dtmax values.
Statistical analysis
Gaussian distribution of the measurement data was tested using the Shapiro-Wilk normality test. Correlation was tested using the Spearman test by calculating the Spearman correlation coefficient. LV and arterial dP/dtmax were compared using the Bland-Altman analysis. Linear regression was used to derive the equation representing the relationship between LV and arterial dP/dtmax. The analyses were performed using GraphPad Prism version 7 (GraphPad Software, Inc., La Jolla, CA, USA) and MedCalc (MedCalc Software, Ostend, Belgium); P < 0.05 was considered to be statistically significant.
Results
Forty-eight patients were enrolled in the study; baseline characteristics of the study population are summarized in Table 1. The mean age was 70.4 years, the majority were males (65%), and the main cause of acute heart failure was ischemic cardiomyopathy (65%). Eighty-five percent of patients were treated with intravenous inotropes, and the majority required vasopressors (73%).
The values from continual arterial dP/dtmax monitoring were significantly correlated with LV dP/dtmax assessed using echocardiography (r = 0.70 [95% confidence interval (CI) 0.51–0.82]; P < 0.0001) (Fig. 1). Linear regression revealed that LV dP/dtmax = 1.25 × (arterial dP/dtmax) (P < 0.0001). Arterial dP/dtmax was significantly correlated with SV (r = 0.63 [95% CI 0.41–0.78]; P < 0.0001) and CO (r = 0.42 [95% CI 0.14–0.63]; P = 0.003). In contrast, arterial dP/dtmax was not correlated with SV variation, dynamic arterial elastance, heart rate, SVR, or mean arterial pressure (Table 2).
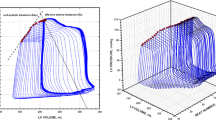
The correlation between arterial and LV dP/dtmax was calculated also in subgroups above and below the mean value of the recorded variables. Marked differences in the correlation between arterial and LV dP/dtmax were observed in the subgroups based on the mean SVR, CO, and SV; on the other hand, similar correlation was observed in the subgroups based on SV variation (r = 0.54 vs. r = 0.59), dynamic arterial elastance (r = 0.70 vs. r = 0.73), heart rate (0.68 vs. 0.72), and mean arterial pressure (r = 0.80 vs. r = 0.76).
SVR subgroups
The study population was divided into two groups according to the mean level of SVR (> or < 900 dyn·s/cm5). In the subgroup of patients with lower SVR (< 900 dyn·s/cm5 [n = 28]), a statistically significant correlation between arterial dP/dtmax and LV dP/dtmax was found (r = 0.61 [95% CI 0.31 to 0.80]; P = 0.0004). However, in the subgroup with higher SVR (> 900 dyn·s/cm5 [n = 20]), the correlation between arterial and LV dP/dtmax was markedly stronger and highly statistically significant (r = 0.91 [95% CI 0.78 to 0.97]; P < 0.0001) (Fig. 2). Linear regression analysis revealed that in subgroup with higher SVR, LV dP/dtmax could be calculated according to the equation: LV dP/dtmax = 1.08 × (arterial dP/dtmax).
Arterial and left ventricular (LV) dP/dtmax in subgroups according to systemic vascular resistance (SVR). a Subgroup with lower SVR (< 900 dyn·s/cm5, N = 20)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right). b Subgroup with higher SVR (> 900 dyn·s/cm5, N = 28)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right)
CO subgroups
In the subgroup of patients with lower CO (< 6 L/min [n = 26]), a strong and highly statistically significant correlation between arterial dP/dtmax and LV dP/dtmax was found (r = 0.81 [95% CI 0.60 to 0.91]; P < 0.0001). In contrast, in the subgroup with higher CO (> 6 L/min [n = 22]), the correlation between arterial and LV dP/dtmax was not statistically significant (r = 0.29 [95% CI − 0.16 to 0.64]; P = 0.18) (Fig. 3). Linear regression revealed that in the subgroup with lower CO, LV dP/dtmax could be calculated according to the equation: LV dP/dtmax = 1.21 × (arterial dP/dtmax).
Arterial and left ventricular (LV) dP/dtmax in subgroups according to cardiac output (CO). a Subgroup with lower CO (< 6 L/min, N = 26)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right). b Subgroup with higher CO (> 6 L/min, N = 22)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right)
SV subgroups
In the subgroup of patients with lower SV (< 65 mL [n = 25]), a statistically significant correlation between arterial dP/dtmax and LV dP/dtmax was found (r = 0.60 [95% CI 0.26 to 0.81]; P = 0.0014). In contrast, in the subgroup with higher SV (> 65 mL [n = 23]), the correlation of between arterial and LV dP/dtmax was not statistically significant (r = 0.38 [95% CI − 0.05 to 0.69]; P < 0.07) (Fig. 4). Linear regression revealed that in the subgroup with lower SV, LV dP/dtmax could be calculated according to the equation: LV dP/dtmax = 1.33 × (arterial dP/dtmax).
Arterial and left ventricular (LV) dP/dtmax in subgroups according to stroke volume (SV). a Subgroup with lower SV (< 65 mL, N = 25)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right). b Subgroup with higher SV (> 65 mL, N = 23)—correlation between arterial and LV dP/dtmax with linear regression curve (left), and the Bland-Altman plot of the agreement between arterial and LV dP/dtmax (right)
Discussion
Our results demonstrate that in adult patients with acute heart failure, the values of arterial dP/dtmax, which can be continuously monitored by analysis of the pressure waveform, were significantly correlated with LV dP/dtmax. An even better agreement between arterial dP/dtmax and LV dP/dtmax was observed in subgroups with higher SVR, lower CO, and lower SV. This observation is particularly important because monitoring LV contractility is most desirable in patients with heart failure with critical hemodynamic collapse, such as in cardiogenic shock, characterized by increased SVR and decreased CO and SV. In contrast, in the subgroups with lower SVR, higher CO, and higher SV, the correlation was weak or even absent.
Acute heart failure is a critical condition in which LV contractility is commonly depressed, and therapeutic strategies are frequently based on increasing inotropy [12]. Although LV contractility status can be routinely and intermittently assessed using echocardiography in patients with acute heart failure, even with the use of new techniques, the measurement can be inaccurate and interpretation difficult [13,14,15,16,17]. There are currently highly limited options for continuous LV contractility monitoring. In contrast to echocardiographic techniques, the maximal rate of arterial pressure increases during systole (arterial dP/dtmax) can be easily and continuously calculated from the pressure waveform. It has been shown in animal studies that arterial dP/dtmax may correlate with LV contractility status under various hemodynamic conditions. In a porcine model of endotoxin-induced shock and catecholamine infusion, Morimont et al. [8] observed that arterial dP/dtmax was significantly correlated with LV contractility measured by LV end-systolic elastance (Ees) or LV dP/dtmax. The authors also found a better correlation when adequate vascular filling according to the arterial pulse pressure variation was achieved. These results are consistent with our observations. We have demonstrated a strong relationship between arterial and LV dP/dtmax under higher SVR, which could be also a result of increased vascular filling. Monge Garcia et al. [10] analyzed the relationship among arterial dP/dtmax, LV dP/dtmax, and Ees in sequential changes of afterload, preload, and contractility in pigs. In this study, arterial dP/dtmax enabled the tracking of Ees changes, especially during the modification of afterload and contractility, and changes in cardiac contractility (i.e., Ees) were the main determinants of arterial dP/dtmax changes. Moreover, these observations are in good agreement with our results; Monge Garcia et al. recorded higher values of LV dP/dtmax in comparison with arterial dP/dtmax, similar to our study. A good correlation between arterial dP/dtmax and LV dP/dtmax in heart failure patients was also reported in the study by Tartiere et al. [11], in which the dP/dtmax from the radial artery was assessed non-invasively using applanation tonometry and LV dP/dtmax. Our results are also consistent with the observation by Scolletta et al. [18] who reported significant correlation between arterial dP/dtmax and LV dP/dtmax in a group of critically ill patients. Furthermore, and again similar to our results, a very close linear relationship was found between arterial dP/dtmax from the femoral artery and invasively measured LV dP/dtmax (with a catheter in the LV) in patients scheduled for coronary artery bypass surgery [9]; arterial dP/dtmax also underestimated LV dP/dtmax in this study.
In contrast, Kim et al. [19] studied the relationship between arterial dP/dtmax from the radial artery, aortic dP/dtmax, and selected echocardiographic variables such as LV ejection fraction or LV fractional shortening in children undergoing congenital heart disease surgery. They did not find a significant correlation between arterial dP/dtmax and the other variables, and these observations were explained by differences between radial artery and aortic pressure waveforms. The discrepancy with our results can be elucidated by the other measured parameters in Kim et al.’s study. While we used LV dP/dtmax as a surrogate parameter of LV contractility, Kim et al. measured LV ejection fraction and LV fractional shortening, which are not the accepted markers of LV contractility, because they are influenced by many other factors (e.g., preload, mitral regurgitation). The observations in the study by Kim et al. could be also influenced by CO or SVR (or vascular filling), which were not recorded. Recently, Vaquer et al. [20] published a study focused on femoral arterial dP/dtmax in critically ill patients, predominantly with septic shock. They observed increase in arterial dP/dtmax after administration of dobutamine and norepinephrine but not after volume expansion. The changes in arterial dP/dtmax were strongly correlated with the changes in pulse pressure and systolic arterial pressure in all interventions including volume expansion. Vaquer et al. conclude that femoral arterial dP/dtmax is, therefore, an unreliable estimate of LV systolic function [20]. Our study was not designed to evaluate the relationship between dP/dtmax and LV systolic function; we focused on the comparison of the arterial dP/dtmax and the LV dP/dtmax, as a surrogate marker of LV contractility. Although the study group characteristics are different, the observation of increase in arterial dP/dtmax after administration of agents with inotropic effect (dobutamine, norepinephrine) in the study by Vaquer et al. [20] is in a good agreement with our results showing significant correlation between arterial and LV dP/dtmax. Our observation that correlation between arterial and LV dP/dtmax depends on SVR is also consistent with the results by Vaquer et al. [20] describing that femoral dP/dtmax is influenced by LV preload and afterload.
Several authors reported that the arterial dP/dtmax is significantly influenced by vascular filling conditions [8, 10, 20]. We observed in our study that the correlation between arterial and LV dP/dtmax was influenced by SVR, which reflects loading conditions; however, SV variation or dynamic arterial elastance had no effect on the relationship between arterial and LV dP/dtmax. This contrast can be at least partly explained by the fact that in our study, the measurement was done in a single time point, while in the other studies, serial measurements were performed enabling evaluation of dynamic changes. In addition, we included entirely patients with acute left heart failure, where the LV preload is usually increased that may or may not be accompanied by changes in other indirect markers of vascular filling. Our study had several limitations, the first of which was possible bias caused by the small sample size. We designed only a pilot study focusing primarily on feasibility; however, a larger trial should be performed to confirm our results. We also acknowledge that arterial dP/dtmax is not only a function of LV contractility but is influenced by many other factors, at least by arterial vessel wall characteristics (e.g., arterial elasticity and stiffness), which was not assessed in the present study. We did not record pulse pressure enabling to calculate arterial elastance. It can be assumed that there can be marked individual differences in arterial system properties in heart failure patients, who often present with other diseases and various degrees of peripheral atherosclerosis. Patients with moderate to severe aortic stenosis were ineligible for this study; however, we cannot exclude the possibility that even mild aortic stenosis may have influenced the results. Moreover, in our study, we have performed only single measurements at one time point in each patient. Our study, therefore, was not designed to evaluate the trends in arterial dP/dtmax changes. In addition, while the LV dP/dtmax values were obtained at the end of expiration, the arterial dP/dtmax were calculated as a median value from 20-s interval, therefore not at the same period of respiratory cycle. Finally, LV dP/dtmax is only a surrogate marker of LV contractility and measurement of this parameter using echocardiography can be inaccurate.
Conclusions
Our results suggest that in patients with acute heart failure requiring intensive care with an arterial line, continuous calculation of arterial dP/dtmax may be used for monitoring LV contractility, especially in those with higher SVR, lower CO, and lower SV, such as in patients experiencing cardiogenic shock. On the other hand, there was only a weak or no significant correlation in the subgroups with higher CO, higher SV, and lower SVR.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CO:
-
Cardiac output
- Ees:
-
End-systolic elastance
- LV:
-
Left ventricular
- SV:
-
Stroke volume
- SVR:
-
Systemic vascular resistance
- T:
-
Time interval
References
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1795–815.
Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, De Smet BJ, Herrman JP, Adriaenssens T, Vrolix M, Heestermans AA, Vis MM, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet. 2013;381(9872):1107–15.
Suga H, Sagawa K. Instantaneous pressure-volume relationships and their ratio in the excised, supported canine left ventricle. Circ Res. 1974;35(1):117–26.
Sagawa K. The end-systolic pressure-volume relation of the ventricle: definition, modifications and clinical use. Circulation. 1981;63(6):1223–7.
Wallace AG, Skinner NS Jr, Mitchell JH. Hemodynamic determinants of the maximal rate of rise of left ventricular pressure. Am J Phys. 1963;205:30–6.
Bargiggia GS, Bertucci C, Recusani F, Raisaro A, de Servi S, Valdes-Cruz LM, Sahn DJ, Tronconi L. A new method for estimating left ventricular dP/dt by continuous wave Doppler-echocardiography. Validation studies at cardiac catheterization. Circulation. 1989;80(5):1287–92.
Chung N, Nishimura RA, Holmes DR Jr, Tajik AJ. Measurement of left ventricular dp/dt by simultaneous Doppler echocardiography and cardiac catheterization. J Am Soc Echocardiogr. 1992;5(2):147–52.
Morimont P, Lambermont B, Desaive T, Janssen N, Chase G, D'Orio V. Arterial dP/dtmax accurately reflects left ventricular contractility during shock when adequate vascular filling is achieved. BMC Cardiovasc Disord. 2012;12:13.
De Hert SG, Robert D, Cromheecke S, Michard F, Nijs J, Rodrigus IE. Evaluation of left ventricular function in anesthetized patients using femoral artery dP/dt (max). J Cardiothorac Vasc Anesth. 2006;20(3):325–30.
Monge Garcia MI, Jian Z, Settels JJ, Hunley C, Cecconi M, Hatib F, Pinsky MR. Performance comparison of ventricular and arterial dP/dtmax for assessing left ventricular systolic function during different experimental loading and contractile conditions. Crit Care. 2018;22(1):325.
Tartiere JM, Logeart D, Beauvais F, Chavelas C, Kesri L, Tabet JY, Cohen-Solal A. Non-invasive radial pulse wave assessment for the evaluation of left ventricular systolic performance in heart failure. Eur J Heart Fail. 2007;9(5):477–83.
Mebazaa A, Tolppanen H, Mueller C, Lassus J, DiSomma S, Baksyte G, Cecconi M, Choi DJ, Cohen Solal A, Christ M, et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med. 2016;42(2):147–63.
Robotham JL, Takata M, Berman M, Harasawa Y. Ejection fraction revisited. Anesthesiology. 1991;74(1):172–83.
Boissier F, Razazi K, Seemann A, Bedet A, Thille AW, de Prost N, Lim P, Brun-Buisson C, Mekontso Dessap A. Left ventricular systolic dysfunction during septic shock: the role of loading conditions. Intensive Care Med. 2017;43(5):633–42.
Cikes M, Solomon SD. Beyond ejection fraction: an integrative approach for assessment of cardiac structure and function in heart failure. Eur Heart J. 2016;37(21):1642–50.
Burns AT, La Gerche A, D'Hooge J, MacIsaac AI, Prior DL. Left ventricular strain and strain rate: characterization of the effect of load in human subjects. Eur J Echocardiogr. 2010;11(3):283–9.
Nafati C, Gardette M, Leone M, Reydellet L, Blasco V, Lannelongue A, Sayagh F, Wiramus S, Antonini F, Albanese J, et al. Use of speckle-tracking strain in preload-dependent patients, need for cautious interpretation! Ann Intensive Care. 2018;8(1):29.
Scolletta S, Bodson L, Donadello K, Taccone FS, Devigili A, Vincent JL, De Backer D. Assessment of left ventricular function by pulse wave analysis in critically ill patients. Intensive Care Med. 2013;39(6):1025–33.
Kim JW, Bang JY, Park CS, Gwak M, Shin WJ, Hwang GS. Usefulness of the maximum rate of pressure rise in the central and peripheral arteries after weaning from cardiopulmonary bypass in pediatric congenital heart surgery: a retrospective analysis. Medicine (Baltimore). 2016;95(49):e5405.
Vaquer S, Chemla D, Teboul JL, Ahmad U, Cipriani F, Oliva JC, Ochagavia A, Artigas A, Baigorri F, Monnet X. Influence of changes in ventricular systolic function and loading conditions on pulse contour analysis-derived femoral dP/dtmax. Ann Intensive Care. 2019;9(1):61.
Funding
The study was supported by an institutional grant MH CZ-DRO (Nemocnice Na Homolce-NNH, 00023884), IG150501.
Author information
Authors and Affiliations
Contributions
PO and DV conceived and designed the study. DV, AK, MJ, and JN contributed to the recruitment of trial participants and were responsible for the acquisition of data and their integrity. PO, MJ, and JN did the statistical analysis and prepared the figures and tables. All authors participated in the interpretation of the results. PO wrote the first draft of the manuscript. DV, AK, MJ, and JN critically reviewed and revised the manuscript for important intellectual content. All authors approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was performed in accordance with the principles of the Declaration of Helsinki, and the study protocol was approved by the Institutional Ethics Committee of the Na Homolce Hospital (Prague, Czech Republic). Informed consent was obtained from conscious patients before measurements. In unconscious subjects at the time of measurement, informed consent was obtained retrospectively. In two deceased patients, informed consent was obtained from next of kin.
Consent for publication
Not applicable
Competing interests
PO received speaker’s fee from Edwards Lifesciences. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ostadal, P., Vondrakova, D., Krüger, A. et al. Continual measurement of arterial dP/dtmax enables minimally invasive monitoring of left ventricular contractility in patients with acute heart failure. Crit Care 23, 364 (2019). https://doi.org/10.1186/s13054-019-2654-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-019-2654-8