Abstract
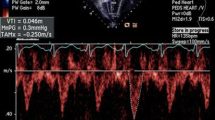
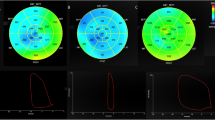
The use of untwisting rate as a novel index of LV diastolic function in clinical practice has been limited due to its tedious and time-consuming analysis. Therefore, we simplify the untwist measurement by only measuring the LV apex's recoil rate and validating and applying peak apical recoil rate (PARR) as an index of diastolic dysfunction (DD) in pediatric subjects during increased and decreased lusitropic states. We recruited 153 healthy subjects (mean age 13.8 ± 2.9 years), of whom 48 performed straight leg raising exercise and an additional 46 patients (mean 8.4 ± 5.6 years) with documented pulmonary capillary wedge pressures (PCWP) (validation cohort). In addition, we studied 16 dilated cardiomyopathy patients (mean age 9.5 ± 6.3 years) (application cohort). PARR and isovolumic relaxation time (IVRT) were compared to PCWP. Both PARR and PARR normalized by heart rate (nPARR) were excellent in detecting patients with PCWP ≥ 12 mmHg and greatly superior to IVRT in this respect (AUC: 0.98, 95% CI [0.96, 1.0] vs. AUC: 0.7 95%CI [0.54,0.86]). In DCM patients, PARR and nPARR were greatly decreased compared to controls (− 38.6 ± 18.6º/s vs − 63.1 ± 16.3º /s, p < 0.001) and (− 0.43 ± 0.20 º/ s/min vs − 0.83 ± 0.28º/s/min, p < 0.0001) but increased with straight leg raising exercise (− 59.4 ± 19.4º/s vs − 97.8 ± 39.0 º/s, p < 0.01) and − 0.85 ± 0.36 vs − 1.4 ± 0.62 º/s/min (p < 0.0001) respectively. PARR and nPARR successfully detected increased and decreased lusitropic states and superior to IVRT in correlation with PCWP. This highly reproducible parameter offers incremental value over traditional indices of DD and may potentially serve as a useful index of elevated PCWP in children.





Similar content being viewed by others
Abbreviations
- PARR:
-
Peak Apical recoil rate
- nPARR:
-
Normalized Peak Apical rate with heart rate
- PARo:
-
Peak apical rotation
- DD:
-
Diastolic Dysfunction
- IVRT:
-
Isovolumic relaxation time
- LV:
-
Left Ventricle
- PCWP:
-
Pulmonary capillary wedge pressure
References
Dragulescu A, Mertens L, Friedberg MK (2013) Interpretation of left ventricular diastolic dysfunction in children with cardiomyopathy by echocardiography problems and limitations. Circ Cardiovasc Imaging 6(2):254–261. https://doi.org/10.1161/CIRCIMAGING.112.000175
Nagueh SF, Smiseth OA, Appleton CP, Dokainish H, Edvardsen T, Flachskampf FA et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 4:277–314. https://doi.org/10.1093/ehjci/jew082
Little WC, Jae KOh (2009) Echocardiographic evaluation of diastolic function can be used to guide clinical care. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.109.869602
Burns AT, La Gerche A, Al M, Prior DL (2009) Left ventricular untwisting is an important determinant of early diastolic function. JACC Cardiovasc Imaging 2(6):709–716. https://doi.org/10.1016/j.jcmg.2009.01.015
Fukuda N, Terui T, Ishiwata S, Kurihara S (2010) Titin-based regulations of diastolic and systolic functions of mammalian cardiac muscle. J Mol Cell Cardiol 48(5):876–881. https://doi.org/10.1016/j.yjmcc.2009.11.013
Di Maria MV, Caracciolo G, Prashker S, Sengupta pp. Banerjee A, (2014) Left Ventricular Rotational Mechanics before and after exercise in Children. J Am Soc Echocardiogr 27(12):1336–1343. https://doi.org/10.1016/j.echo.2014.07.016
Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28:2539–2550. https://doi.org/10.1093/eurheartj/ehm037
Cheng CP, Igarashi Y, Little WC (1992) Mechanism of augmented rate of left ventricular filling during exercise. Circ Res 70(1):9–19. https://doi.org/10.1161/01.RES.70.1.9
Opdahl A, Helle-Valle T, Remme EW, Vartdal T, Pettersen E, Lunde K et al (2008) Apical rotation by speckle tracking echocardiography: a simplified bedside index of left ventricular twist. J Am Soc Echocardiogr 21(10):1121–1128. https://doi.org/10.1016/j.echo.2008.06.012
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD et al (1997) Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 30:474–480. https://doi.org/10.1016/s0735-1097(97)88335-0
Dong SJ, Hees PS, Siu CO, Weiss JL, Shapiro EP (2001) MRI assessment of LV relaxation by untwisting rate: a new isovolumic phase measure of tau. Am J Physiol Heart Circ Physiol. https://doi.org/10.1152/ajpheart.2001.281.5.H2002
Thomas JD, Flachskampf FA, Chen C, Guererro JL, Picard MH, Levine RA, Weyman AE (1992) Isovolumic relaxation time varies predictably with its time constant and aortic and left atrial pressures: implications for the noninvasive evaluation of ventricular relaxation. Am Heart J 124(5):1305–1313. https://doi.org/10.1016/0002-8703(92)90416-S
Appleton CP, Galloway JM, Gonzalez MS, Gaballa M, Basnight MA (1993) Estimation of left ventricular filling pressures using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral flow velocity at atrial contraction. J Am Coll Cardiol 22(7):1972-82. https://doi.org/10.1016/0735-1097(93)90787-2
Arsos G, Moralidis E, Karatzas N, Iakovou I, Georga S, Koliouskas D et al (2002) Heart rate is the major determinant of diastolic filling pattern during growth: a radionuclide ventriculography assessment. Pediatr Cardiol 23(4):378–387. https://doi.org/10.1007/s00246-002-1506-4
Schmitz L, Schneider MBE, Lange PE (2003) Isovolumic relaxation time corrected for heart rate has a constant value from infancy to adolescence. J Am Soc Echocardiogr 16(3):221–222. https://doi.org/10.1067/mje.2003.17
Punske BB, Taccardi B, Steadman B et al (2005) Effect of fiber orientation on propagation: electrical mapping of genetically altered mouse hearts. J Electrocardiol 38:40–44
Fuchs E, Muller MF, Oswald H, Thony H, Mohacsi P, Hess OM (2004) Cardiac rotation and relaxation in patients with chronic heart failure. Eur J Heart Fail 6:715–722
Cheng CP, Freeman GL, Santamore WP, Constantinescu MS, Little WC (1990) Effect of loading conditions, contractile state, and heart rate on early diastolic left ventricular filling in conscious dogs. Circ Res 66(3):814–823. https://doi.org/10.1161/01.RES.66.3.814
Notomi Y, Martin-Miklovic MG, Oryszak SJ, Shiota T, Deserranno D, Popovic ZB et al (2006) Enhanced ventricular untwisting during exercise: a mechanistic manifestation of elastic recoil described by Doppler tissue imaging. Circulation 113(21):2524–2533. https://doi.org/10.1161/CIRCULATIONAHA.105.596502
Cheng CP, Noda T, Nozawa T, Little WC (1993) Effect of heart failure on the mechanism of exercise-induced augmentation of mitral valve flow. Circ Res 72(4):795–806. https://doi.org/10.1161/01.RES.72.4.795
Sharifov OF, Schiros CG, Aban I, Denney TS, Gupta H (2016) Diagnostic accuracy of tissue doppler index E/e’ for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: a systematic review and meta-analysis. J Am Heart Assoc. https://doi.org/10.1161/JAHA.115.002530
Lancellotti P, Galderisi M, Edvardsen T, Donal E, Goliasch G, Cardim N et al (2017) EchoDoppler estimation of left ventricular filling pressure: results of the multicentre EACVI Euro-Filling study. Eur Heart J Cardiovasc Imaging 18(9):961–968. https://doi.org/10.1093/ehjci/jex067
Fogel MA, Sundareswaran KS, de Zelicourt D, Dasi LP, Pawlowski T, Rome J, Yoganathan AP (2012) Power loss and right ventricular efficiency in patients after tetralogy of Fallot repair with pulmonary insufficiency: clinical implications. J Thorac Cardiovasc Surg 143(6):1279–1285. https://doi.org/10.1016/j.jtcvs.2011.10.066
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest and no financial disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yubbu. P: Peak apical recoil rate as an index for diastolic dysfunction.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yubbu, P., Kauffman, H., Calderon-Anyosa, R. et al. Peak apical recoil rate is a simplified index of left ventricular untwist: validation and application for assessment of diastolic function in children. Int J Cardiovasc Imaging 38, 1505–1516 (2022). https://doi.org/10.1007/s10554-022-02587-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02587-y