Abstract
Background
SPG11-linked hereditary spastic paraplegia is characterized by multisystem neurodegeneration leading to a complex clinical and yet incurable phenotype of progressive spasticity and weakness. Severe cognitive symptoms are present in the majority of SPG11 patients, but a systematic and multidimensional analysis of the neuropsychological phenotype in a larger cohort is lacking. While thinning of the corpus callosum is a well-known structural hallmark observed in SPG11 patients, the neuroanatomical pattern of cortical degeneration is less understood. We here aimed to integrate neuropsychological and brain morphometric measures in SPG11.
Methods
We examined the neuropsychological profile in 16 SPG11 patients using a defined neuropsychological testing battery. Long-term follow up testing was performed in 7 patients. Cortical and subcortical degeneration was analyzed using an approved, artificial intelligence based magnetic resonance imaging brain morphometry, comparing patients to established reference values and to matched controls.
Results
In SPG11 patients, verbal fluency and memory as well as frontal-executive functions were severely impaired. Later disease stages were associated with a global pattern of impairments. Interestingly, reaction times correlated significantly with disease progression. Brain morphometry showed a significant reduction of cortical and subcortical parenchymal volume following a rostro-caudal gradient in SPG11. Whereas performance in memory tasks correlated with white matter damage, verbal fluency measures showed strong associations with frontal and parietal cortical volumes.
Conclusions
The present data will help define neuropsychological and imaging read out parameters in early as well as in advanced clinical stages for future interventional trials in SPG11.
Similar content being viewed by others
Background
Hereditary spastic paraplegias (HSP) are a heterogeneous group of rare genetic diseases characterized by progressive spasticity and weakness of the legs [1]. Biallelic pathogenic variants in SPG11 cause the most frequent form of autosomal-recessive HSP leading to a multisystem neuronal degeneration [2,3,4]. While there is a substantial phenotypic variability, an early cognitive deficit is present in the majority of patients consequently followed by progressive motor symptoms in childhood or adolescence [5]. As there is no causal treatment present at time, SPG11 HSP results in early loss of ambulation, caregiver dependence, and premature death in mid-adulthood [6, 7].
While the common motor phenotype of HSPs is well validated applying the Spastic Paraplegia Rating Scale (SPRS [8]) as primary motor outcome measure in clinical studies of HSP, there are no standardized measures of neuropsychological symptoms linked to cognitive decline and progressive brain atrophy in SPG11. In particular, cognitive impairment has long been recognized as an important symptom in SPG11 [9, 10]. Most small case series, however, employed measures of intelligence like the Wechsler Intelligence Scale (WAIS) or global cognitive tests like the Mini-Mental State Examination (MMSE [11]), Montral Cognitive Assessment (MoCA [12]) or Addenbrooke’s Cogntitive Examination (ACE [13]). However, a more detailed neuropsychological evaluation in a larger patient cohort is missing in order to comprehensively characterize the complex and multidimensional phenotype of this devastating motor neuron disease.
Likewise, the known imaging hallmarks of SPG11 are a thin corpus callosum and periventricular white matter hyperintensities [2, 3, 10, 14], but a comprehensive depiction of the atrophy pattern and its relation to the clinical and neuropsychological phenotype is scarce. Furthermore, previous MRI studies of SPG11 patients used VBM or ROI approaches being limited to provide an unbiased volumetric approach to measure distinct grey and white matter regions. Of note, a recent case series in SPG11 described a predominant subcortical degeneration using different kinds of ROI based analyses [15].
The aim of this study was to comprehensively characterize the cognitive and cerebral atrophy phenotype in a well-defined cohort of SPG11 patients in order to (1) describe the neuropsychological profile of SPG11, (2) depict the progressive impairment in specific cognitive tasks, (3) quantify atrophy of different predefined brain regions, and (4) ultimately correlate the neuropsychological with the cerebral phenotype. The determination of a distinctive pattern of cortical and subcortical degeneration in SPG11 aids the diagnosis and is essential for a specific definition of potential clinical stages in regard to disease progression and for defining important outcome measures for future interventional studies in SPG11.
Methods
SPG11 cohort, clinical characteristics and neuropsychological assessment
Patients were recruited during regular follow-up visits within the HSP outpatient center of the Center for Rare Movement Disorders at the Department of Molecular Neurology, University Hospital Erlangen between 2016 and 2020. The study was approved by the local ethics committee (No. 259_17B and 347_17B), and all participants and legal guardians (if applicable) provided a written informed consent. Inclusion criteria were a clinically and genetically confirmed diagnosis of SPG11-linked HSP and the ability to participate in a defined set of cognitive tests. Motor examination included rating by the Spastic Paraplegia Rating Scale (SPRS [8]) that ranges from 0 to 52 and increases with disease severity. The Montreal Cognitive Assessment (MoCA [12]) was performed on 14 of the 16 patients to screen the overall cognitive status. The maximum score is 30 with patients scoring below 26 being considered as cognitively impaired.
Detailed demographic and clinical characteristics of the study cohort are summarized in Table 1. Details for neuropsychological assessments are given in the Additional file 1: supplemental Methods.
Brain morphometry
High resolution MRI of the brain was performed in 12 patients using a 3.0 Tesla scanner (Magnetom Tim Trio, Siemens Healthineers, Erlangen, Germany) with a gradient field strength up to 45 mT/m (72 mT/m effective). Using the FDA-approved and CE-marked AI-Rad Companion Brain MR for Morphometry Analysis package (Siemens Healthineers), MPRAGE images underwent volumetric analysis. Segmentation quality was > 0.7 for all scans. To describe the pattern of brain atrophy in SPG11, the implemented algorithm was used first. It compares normalized morphometric values to reference values derived from a control group of the Alzheimer’s Disease Neuroimaging Initiative (ADNI [16]; http://adni.loni.usc.edu). This control group consists of 303 healthy controls (mean age 66 ± 19 years, age range 19–90 years, 51% of healthy individuals male) who underwent 3-Tesla cerebral MRI using the standardized ADNI protocol [17]. Normative ranges were calibrated on this population using a log-linear regression model taking into account the confounding effects of age and sex as covariates. Deviations from normative ranges of individual volume estimates were assessed by z-scores [18]. As clinically approved, relative values exceeding the 10th or 90th percentile were considered pathological. In order to analyze the brain atrophy pattern in a second approach, absolute morphometric volumes (in ml) were compared to a 1:1 age- and gender matched cohort of in-house controls (characteristics shown in Additional file 1: Table S1). For correlation to neuropsychological and clinical parameters, absolute values were normalized to intracranial volume.
Statistics and data availability
As most data were not normally distributed and due to small sample sizes, non-parametric tests were used. Correlation analyses were calculated by Spearman’s rho (r). Raw values of baseline and follow-up testing were compared using the Wilcoxon signed-rank test. Absolute volumetric measures were compared using the unpaired Mann–Whitney test. p values < 0.05 were considered significant. Analyses were conducted in IBM SPSS 24 and graphs were generated in GraphPad Prism 8. Anonymized raw data are available from the corresponding authors upon reasonable request.
Results
Severe neuropsychological deficits are frequent in SPG11 patients
We recruited a total of 16 patients with a clinically and genetically confirmed diagnosis of SPG11-related HSP. All patients underwent a defined neuropsychological testing battery. Due to their advanced disease stage, data for visual memory, selective attention, incompatibility and cognitive estimation are missing in 2 patients, as well as for the Tower of London task in 3 patients, respectively. Figure 1 depicts the frequency of impairment for different neuropsychological tests, as defined by a result below a percentile rank of 16 (i.e. z < − 1) according to the respective test norms. The majority of SPG11 patients showed an impairment in more than 70% of the applied tests. Phonematic verbal fluency was most frequently impaired, followed by semantic verbal fluency, digit span forward, and digit span backward. Upon the global MoCA screening test, 12 out of 14 tested patients were impaired (86%), i.e., scoring below 26.
Cognitive test performance correlates with motor deficits in SPG11
To examine whether patients at more advanced disease stages (i.e. with more severe motor impairment) exhibit more pronounced neuropsychological deficits, a sum score of tests scoring below a percentile rank of 16 was calculated for each patient. On average, patients were impaired in 9 out of 14 tests (n = 13, M = 9.77, SD = 3.37). There was a strong significant correlation between this sum score and the total SPRS score, indicating that a more severe motor phenotype of spastic paraplegia was associated with a higher number of impaired cognitive domains (r = 0.58, p = 0.038). Likewise, the global cognitive MoCA screening correlated significantly with SPRS score (r = 0.66, p = 0.01).
To identify those tests that correlated best with motor disease stage, raw scores of individual tests were used. There were strong significant correlations between total SPRS scores and story—immediate recall (r = − 0.63, p = 0.009), verbal fluency—semantic (r = − 0.77, p = 0.001), selective attention—reaction time (r = 0.73, p = 0.003), incompatibility—reaction time (r = 0.77, p = 0.001), and Tower of London (r = − 0.60, p = 0.039). These data imply that a more severe spastic paraplegia was associated with a worse performance in these neuropsychological tasks. The subscore of language domains in the MoCA test (sum of naming and repetition tasks, ranging from 0 to 5) correlated significantly with SPRS score (r = − 0.75, p = 0.002). There was no significant correlation between total SPRS scores and all other cognitive parameters (p > 0.05).
To identify those cognitive domains that are already affected at an early stage of motor impairment, patients were split based on the median SPRS score (25 points). Three patients with missing values were excluded, thus the sample size was 13. Five out of 6 patients scoring below the median showed impairment in the tasks digit span forward, digit span backward, and verbal fluency (both phonematic and semantic). These neuropsychological results suggest that verbal fluency and verbal short-term memory are linked to an early disease stage.
Longitudinal course of motor and neuropsychological deficits
To characterize the progressive nature of SPG11, the testing battery was repeated after a mean interval of 24 months (range 12–44, n = 7). The median SPRS score of this sub-sample was 24 (IQR = 12) at the first examination and increased significantly to 29 (IQR = 17) at re-examination (z = − 2.37, p = 0.018). The global cognitive performance measured by MoCA however did not change significantly during this time period (z = − 0.83, p = 0.409, median = 16; IQR = 7 for both time points).
Concerning the course of neuropsychological impairment, the median sum score of tests scoring below a percentile rank of 16 was not significantly different between both examination time points (z = 0, p = 1).
When comparing performance in single tests, specifically reaction time in the selective attention task differed significantly between both time points (see Additional file 1: Table S2). Over time, reaction times increased by 50%, indicating a clinically relevant decrease in response speed. There was no significant correlation between reaction times and SPRS at both timepoints (baseline: r = 0.20, p = 0.670; follow-up: r = 0.27, p = 0.551) and also no correlation of the absolute changes in reaction times and SPRS values (r = 0.32, p = 0.498), indicating that the increase of reaction times may be independent from the worsened motor phenotype (Additional file 1: Fig. S1).
To sum up, while motor impairment worsened over time, there was no obvious change of overall cognitive impairment. However, we were able to detect a specific increase in reaction time in the computer-based selective attention task over time.
Rostro-caudal pattern of cortical and subcortical atrophy in SPG11
Among our cohort, 13 SPG11 patients underwent cerebral MRI at a 3.0-Tesla scanner. Most patients exhibited the prototypical signs of SPG11, i.e. thinning of the corpus callosum and cortical atrophy (Fig. 2A). The degeneration pattern of different grey and white matter areas was analyzed by a CE-marked volumetry tool recently approved for clinical use by the U.S. Food and Drug Administration. It was applied on the full brain MP-RAGE datasets. Using the implemented diagnostic algorithm, we first compared volumetric data to age- and gender-specific reference values established from the normative reference database for brain morphometry from the Alzheimer's Disease Neuroimaging Initiative (ADNI). As shown in the graphical representation of an early-stage patient and an advanced-stage patient (Fig. 2B), there was an inverse rostro-caudal gradient of brain atrophy involving both grey and white matter areas. Whereas the more rostral cerebral cortical areas showed a reduced volume in the majority of patients, parietal, cingulate and occipital cortical volumes were frequently within normal limits (Fig. 2C). Likewise, volumes of the corpus callosum and rostral white matter areas were reduced in most patients while occipital white matter volume was regular in 85% of patients (Fig. 2D). Interestingly, also subcortical grey matter areas were reduced in volume in a substantial proportion of patients, affecting the thalamus in 12/13 patients while sparing the hippocampus (Fig. 2E). On the other hand, cerebellar and brainstem volumes were decreased in few patients only (Fig. 2F).
Brain volumetry in SPG11 patients relative to ADNI reference values. A Classical MRI signs of thin corpus callosum and cortical atrophy shown in an early, mildly affected SPG11 patient (individual #16 in Table 1; SPRS 16) and a severely affected SPG11 patient at an advanced stage of the disease (individual #4; SPRS 36). B Representative graphical depiction of volume z-scores of different cortical and subcortical regions of both patients. C–F Bar diagrams for different brain regions representing the proportional presence of a distinct structural phenotype, i.e. < 10% of age- and gender-matched control values derived from the ADNI control cohort
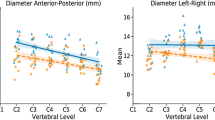
In order to cross validate these data to a locally recruited control cohort, 13 age- and gender-matched control subjects underwent brain imaging at the identical MRI scanner. Comparing absolute volumes of different cortical and subcortical areas of SPG11 patients and these controls, we confirmed the severe decrease in cortical grey matter areas in SPG11 which was more pronounced in the frontal and parietal lobe (Fig. 3A). Concerning white matter areas, the reduction of white matter volume was also most pronounced within the frontal and parietal lobe (Fig. 3B). Analysis of the corpus callosum confirmed the structural hallmark of thinning of the corpus callosum in SPG11 (Fig. 3C). In line with the reference value analysis (Fig. 2F), also subcortical grey matter areas were significantly smaller when compared to our in-house controls, i.e. thalamus, putamen, caudate and pallidum (Fig. 3D). While cerebellar and medulla oblongata volumes were unchanged in SPG11, there was a small, but significant reduction of midbrain and pontine volume in SPG11 (Fig. 3E).
Brain volumetry in SPG11 compared to 1:1 age- and gender-matched in-house controls (n = 13, demographic characteristics shown in Additional file 1: Table S1) for different cortical and subcortical regions: (A) cortical regions, (B) white matter regions, (C) corpus callosum, (D) subcortical grey matter regions, (E) infratentorial regions. Bars represent means ± SD of absolute volume values in controls (white) and SPG11 patients (black). Means were compared by unpaired Mann–Whitney test. *p < .05; **p < .01; ***p < .001; ****p < .0001; n.s. not significant
In summary, our morphometric analysis shows a specific pattern of brain degeneration in SPG11 with rostral (i.e., frontal, parietal and temporal) areas being predominantly affected, involving cortical and subcortical regions of both forebrain hemispheres.
Cortical atrophy associates with cognitive rather than motor impairment
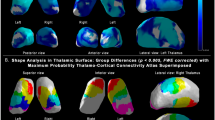
We next asked whether the degree of atrophy of specific brain regions correlates with motor functions or specific neuropsychological outcomes. As the SPRS score mostly reflects motor function, we first correlated imaging data to total SPRS scores. Interestingly, frontal and parietal grey matter and white matter regions showed no significant correlation to SPRS scores (complete set of correlations shown in Additional file 1: Table S3). There were strong inverse correlations of SPRS scores to subcortical motor region volumes (Fig. 4A), i.e. to putamen (r = − 0.742, p = 0.005), caudate (r = − 0.763, p = 0.003) and pallidum (r = − 0.873, p = 0.0002) and to the mesencephalon (r = − 0.751, p = 0.004).
Correlation of grey matter atrophy to motor and cognitive function in SPG11. A Motor function (as measured by the SPRS score) correlates to basal ganglia and mesencephalic atrophy. B Verbal fluency (as measured by the verbal fluency semantic score) correlates to fronto-parietal cortical atrophy. r Spearman’s rho correlation coefficient, SPRS spastic paraplegia rating scale, GM grey matter
Importantly, correlation analyses identified no specific brain regions that may account for neuropsychological deficits in SPG11 in general (Additional file 1: Table S3). Rather, distinct neuropsychological measures correlated with volumes of specific brain regions. For example, performance in the verbal memory test (‘Story Immediate’ and ‘Story Delayed’) correlated with parietal and temporal white matter volumes (Additional file 1: Table S3), both involved in memory processes. As an additional example, the ‘verbal fluency semantic’ score correlated significantly with those cortical grey matter areas that were also most affected on volumetry, i.e. frontal, parietal, cingulate and insular cortex (Fig. 4B).
Discussion
The aim of this study was to provide a detailed neuropsychological and MRI volumetric characterization of the progressive forebrain degeneration in SPG11-linked HSP. A detailed understanding of the natural history of this devastating disorder is an important prerequisite for the identification of robust outcome parameters in order to design interventional trials, a challenging task in rare diseases. Clearly, disease mechanisms and the phenotype of SPG11 HSP are different from pure HSPs [19]. This highlights the importance of genotype-specific studies in HSP beyond motor correlations.
Neuropsychological profile in SPG11
An impaired cognitive performance was present to different degrees in all patients. Specifically, verbal fluency, verbal memory, and executive functions were frequently impaired, reflecting a profound frontotemporal deficit. Overall, neuropsychological impairment correlated with the severity of the motor phenotype. Particularly, reaction times showed a significant worsening on follow-up testing and may thus constitute a robust digital biomarker in natural history studies and interventional studies. Verbal fluency and verbal short-term memory affected early in the disease course may indicate the onset of the neuropsychological deficit or alternatively reflect a specific neurodevelopmental phenotype.
Impaired scores on the global scales such as MMSE and WAIS have been previously reported in SPG11, as comprehensively summarized in Additional file 1: Table S4. Extending these findings of an overall cognitive impairment in SPG11 patients, we here describe a phenotype of impaired verbal fluency and verbal memory in > 80% of SPG11 patients indicating a frontotemporal neuropsychological phenotype. Severe cognitive impairment was also described in other less frequent genetic types of complicated HSP including SPG15 and the AP4-related HSP genes [5, 20, 21], but seems to be absent or mild in most patients with pure HSP, including SPG4, SPG5, and SPG7 [22].
Concerning global cognitive performance as assessed by MoCA, the large majority of SPG11 patients (12/14, i.e. 86%) were impaired, which is in line with Faber et al. [15] reporting 84% of patients classified as demented according to the global ACE-R score. A single SPG11 patient (#11, Table 1) exhibited neuropsychological impairment in distinct subtests only, which matches the previously reported mild phenotype associated with his specific missense variant [23]. No additional genotype phenotype correlations were observed as the majority of patients carried biallelic loss of function variants.
Artificial intelligence based volumetry patterns of cortical atrophy in SPG11
For morphometric analyses, we applied the “AI-Rad Companion Brain MR for Morphometry Analysis” tool, which determines the outlines of different lobes and the separation between white and grey matter areas using artificial intelligence based algorithms. In contrast to the classical methods of voxel based morphometry (VBM) and region of interest (ROI) based volumetry, this method provides unbiased volumetric measures of different brain areas. Although volumetry analyses may be less powerful to demonstrate grey matter alterations [24], our data clearly show a grey matter phenotype in SPG11. The implemented reference values (normalized for intracranial volume) are derived from a control cohort within ADNI and importantly, its application has been approved for regular clinical use. Using a cohort of own local, gender and age matched controls, we cross validate the frontotemporal predominant grey and white matter atrophy in SPG11 and thus also provide support for the validity of the ADNI cohort as controls for volumetric studies in HSP.
Previous imaging studies on SPG11 predominantly described involvement of white matter regions and the basal ganglia. Our observation of a rostro-caudal gradient of white matter volume decrease in SPG11 matches findings of previous studies: a frontal predominant decrease of fractional anisotropy was described in a study on 5 SPG11 patients [25]. Widespread and severe white matter damage was also observed in a combined VBM/DTI study on 24 SPG11 patients, with inverse correlations of ACE-R scores and fractional anisotropy for most tracts [15, 26]. In this VBM-based analysis, cortical grey matter involvement was limited to motor regions and associative cortices whereas subcortical grey matter regions were predominantly affected. Likewise, in a study consisting of two mildly demented and three severely demented SPG11 patients, grey matter atrophy was mainly restricted to the basal ganglia and involved small areas within the precentral and postcentral gyrus only [27]. The different approach for cortical volumetry providing a higher sensitivity of artificial intelligence based lobe-wise morphometry may explain the detected widespread pattern of cortical atrophy. In fact, profound cortical degeneration was reported in a total of 3 post-mortem cases of SPG11 HSP [6, 28]. Both studies describe a severe degeneration predominantly affecting layer 5 neurons in the frontal lobe confirmed by our MRI analyses.
The observed atrophy pattern of the frontal and temporal cortex correlates to the neuropsychological deficits of verbal fluency, verbal memory and executive functions. It is also in line with the frontotemporal cognitive deficit reported in the literature [29, 30]. We additionally identified an atrophy of the parietal cortex, an area that is involved in memory processes as well as visuospatial abilities. The correlation analysis of single cognitive test parameters to cortical volume parameters are partly as expected from lobe-specific functions; i.e. semantic verbal fluency correlated with frontal areas [31, 32] and verbal long-term memory with temporal areas [33, 34]. A schematic overview of volumetric measures and neuropsychological and motor impairment is summarized in Fig. 5. Due to our limited sample size, these results should be cautiously interpreted and be validated in future multicenter studies. It is also important to note the heterogeneity of the analyzed cohort with regards to age and disease duration. In fact, retrospective determination of age at onset from the patients’ history is often equivocal: most families reported insidiously progressive cognitive impairment already during childhood which may have remained unrecognized in some families.
Our data add to previous evidence of dual neurodevelopmental and -degenerative disease mechanisms in SPG11 [4, 15]. Developmental deficits may be linked to an early thinning of the corpus callosum and partly be associated with those neuropsychological measures being affected during the entire disease course, i.e. verbal fluency and digit span tests. Clearly, progressive neurodegeneration causes motor impairment and grey matter atrophy which is supported by our correlations of SPRS and subcortical grey matter volumetry. The underlying mechanism of the increased susceptibility of the more rostral areas remains unknown. However, this pattern is characteristic of frontotemporal dementias. Of note, accumulation of insoluble cytoplasmic TDP-43 (the histopathological hallmark of amyotrophic lateral sclerosis) was also described in a post mortem case of SPG11 [35], and the clinical overlap of SPG11 with amyotrophic lateral sclerosis has been described before [7].
Progression of disease-specific impairments
In SPG11, motor and cognitive functions deteriorate over time [2, 10, 36]. We also observed worsening of motor function in our cohort, as indicated by progression of the SPRS score in those patients that underwent follow up analysis. The observed decrease of reaction time in computer-based attention tasks may be caused by worsened motor function as other global cognitive functions did not change over time. However, the progression rates of SPRS and reaction time were not significantly correlated to each other, indicating that reaction time might constitute an independent, longitudinal measure of cognitive impairment. Moreover, cognitive functions were inversely associated with SPRS in the overall sample, suggesting that cognitive impairment is at least partly progressive in parallel to the motor deficit. The major impact of frontotemporal neuropsychological impairment on patients’ quality of life and social interaction underlines the relevance of the neuropsychological and related imaging parameters as meaningful outcome measures [37].
Conclusions
We report a rostro-caudal pattern of cortical and subcortical atrophy in SPG11 accompanied with severe motor impairment and neuropsychological impairment, especially of verbal fluency, verbal memory and executive functions. Our data suggest that reaction times and MRI cortical volumetric measures are important outcome measures in future interventional trials for SPG11. As the presented artificial intelligence based volumetric analysis is feasible across imaging platforms, future functional and structural studies in SPG11 are possible in a multicentric and longitudinal manner in order to validate these findings and to reduce potential bias across academic centers.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Shribman S, Reid E, Crosby AH, Houlden H, Warner TT. Hereditary spastic paraplegia: from diagnosis to emerging therapeutic approaches. Lancet Neurol. 2019;18:1136–46.
Hehr U, Bauer P, Winner B, Schule R, Olmez A, Koehler W, et al. Long-term course and mutational spectrum of spatacsin-linked spastic paraplegia. Ann Neurol. 2007;62:656–65.
Kara E, Tucci A, Manzoni C, Lynch DS, Elpidorou M, Bettencourt C, et al. Genetic and phenotypic characterization of complex hereditary spastic paraplegia. Brain. 2016;139:1904–18.
Pozner T, Regensburger M, Engelhorn T, Winkler J, Winner B. Janus-faced spatacsin (SPG11): involvement in neurodevelopment and multisystem neurodegeneration. Brain. 2020;143:2369–79.
Pensato V, Castellotti B, Gellera C, Pareyson D, Ciano C, Nanetti L, et al. Overlapping phenotypes in complex spastic paraplegias SPG11, SPG15, SPG35 and SPG48. Brain. 2014;137:1907–20.
Denora PS, Smets K, Zolfanelli F, Groote CC, Casali C, Deconinck T, et al. Motor neuron degeneration in spastic paraplegia 11 mimics amyotrophic lateral sclerosis lesions. Brain. 2016;139:1723–34.
Montecchiani C, Pedace L, Giudice TL, Casella A, Mearini M, Gaudiello F, et al. ALS5/SPG11/KIAA1840mutations cause autosomal recessive axonal Charcot–Marie–Tooth disease. Brain. 2016;139:73–85.
Schüle R, Holland-Letz T, Klimpe S, Kassubek J, Klopstock T, Mall V, et al. The Spastic Paraplegia Rating Scale (SPRS): a reliable and valid measure of disease severity. Neurology. 2006;67:430–4.
Harding AE. Classification of the hereditary ataxias and paraplegias. The Lancet. 1983;1:1151–5.
Winner B, Uyanik G, Gross C, Lange M, Schulte-Mattler W, Schuierer G, et al. Clinical progression and genetic analysis in hereditary spastic paraplegia with thin corpus callosum in spastic gait gene 11 (SPG11). Arch Neurol. 2004;61:117–21.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Mathuranath PS, Nestor PJ, Berrios GE, Rakowicz W, Hodges JR. A brief cognitive test battery to differentiate Alzheimer’s disease and frontotemporal dementia. Neurology. 2000;55:1613–20.
Pascual B, de Bot ST, Daniels MR, França MC, Toro C, Riverol M, et al. “Ears of the Lynx” MRI sign is associated with SPG11 and SPG15 hereditary spastic paraplegia. AJNR Am J Neuroradiol. 2019;40:199–203.
Faber I, Martinez ARM, de Rezende TJR, Martins CR, Martins MP, Lourenco CM, et al. SPG11 mutations cause widespread white matter and basal ganglia abnormalities, but restricted cortical damage. NeuroImage Clin. 2018;19:848–57.
Mueller SG, Weiner MW, Thal LJ, Petersen RC, Jack C, Jagust W, et al. The Alzheimer’s Disease Neuroimaging Initiative. Neuroimag Clin N Am. 2005;15:869–77.
Jack CR, Bernstein MA, Fox NC, Thompson P, Alexander G, Harvey D, et al. The Alzheimer’s disease neuroimaging initiative (ADNI): MRI methods. J Magn Reson Imaging. 2008;27:685–91.
Schmitter D, Roche A, Maréchal B, Ribes D, Abdulkadir A, Bach-Cuadra M, et al. An evaluation of volume-based morphometry for prediction of mild cognitive impairment and Alzheimer’s disease. Neuroimage Clin. 2015;7:7–17.
Schüle R, Wiethoff S, Martus P, Karle KN, Otto S, Klebe S, et al. Hereditary spastic paraplegia: clinicogenetic lessons from 608 patients. Ann Neurol. 2016;79:646–58.
Breza M, Hirst J, Chelban V, Banneau G, Tissier L, Kol B, et al. Expanding the spectrum of AP5Z1-related hereditary spastic paraplegia (HSP-SPG48): a multicenter study on a rare disease. Mov Disord. 2021;36:1034–8.
Ebrahimi-Fakhari D, Teinert J, Behne R, Wimmer M, D’Amore A, Eberhardt K, et al. Defining the clinical, molecular and imaging spectrum of adaptor protein complex 4-associated hereditary spastic paraplegia. Brain. 2020;143:2929–44.
Jacinto-Scudeiro LA, Machado GD, Ayres A, Burguêz D, Polese-Bonato M, González-Salazar C, et al. Are cognitive changes in hereditary spastic paraplegias restricted to complicated forms? Front Neurol. 2019;10:508.
Lynch DS, Koutsis G, Tucci A, Panas M, Baklou M, Breza M, et al. Hereditary spastic paraplegia in Greece: characterisation of a previously unexplored population using next-generation sequencing. Eur J Hum Genet. 2016;24:857–63.
Voormolen EHJ, Wei C, Chow EWC, Bassett AS, Mikulis DJ, Crawley AP. Voxel-based morphometry and automated lobar volumetry: the trade-off between spatial scale and statistical correction. Neuroimage. 2010;49:587–96.
Pan M-K, Huang S-C, Lo Y-C, Yang C-C, Cheng T-W, Yang C-C, et al. Microstructural integrity of cerebral fiber tracts in hereditary spastic paraparesis with SPG11 mutation. AJNR Am J Neuroradiol. 2013;34:990-996-S1.
Servelhere KR, Rezende TJR, Lima FD, Brito MR, Nunes RFF, Casseb RF, et al. Brain damage and gene expression across hereditary spastic paraplegia subtypes. Mov Disord. 2021;36:1644–53.
França MC, Yasuda CL, Pereira FRS, D’Abreu A, Lopes-Ramos CM, Rosa MV, et al. White and grey matter abnormalities in patients with SPG11 mutations. J Neurol Neurosurg Psychiatry. 2012;83:828–33.
Sjaastad O, Blau N, Rydning SL, Peters V, Rødningen O, Stray-Pedersen A, et al. Homocarnosinosis: a historical update and findings in the SPG11 gene. Acta Neurol Scand. 2018;138:245–50.
Siri L, Battaglia FM, Tessa A, Rossi A, Rocco MD, Facchinetti S, et al. Cognitive profile in spastic paraplegia with thin corpus callosum and mutations in SPG11. Neuropediatrics. 2010;41:35–8.
Faber I, Martinez ARM, Martins CR, Maia ML, Souza JP, Lourenço CM, et al. SPG11-related parkinsonism: clinical profile, molecular imaging and l-dopa response. Mov Disord. 2018;33:1650–6.
Frith CD, Friston KJ, Liddle PF, Frackowiak RSJ. A PET study of word finding. Neuropsychologia. 1991;29:1137–48.
Costafreda SG, Fu CHY, Lee L, Everitt B, Brammer MJ, David AS. A systematic review and quantitative appraisal of fMRI studies of verbal fluency: role of the left inferior frontal gyrus. Hum Brain Mapp. 2006;27:799–810.
Schacter DL, Wagner AD. Medial temporal lobe activations in fMRI and PET studies of episodic encoding and retrieval. Hippocampus. 1999;9:7–24.
Squire LR, Stark CEL, Clark RE. THE MEDIAL TEMPORAL LOBE*. Annu Rev Neurosci. 2004;27:279–306.
Mori S, Honda H, Hamasaki H, Sasagasako N, Suzuki SO, Furuya H, et al. Transactivation response DNA-binding protein of 43 kDa proteinopathy and lysosomal abnormalities in spastic paraplegia type 11. Neuropathology. 2021;41:253–65.
de Bot ST, Burggraaff RC, Herkert JC, Schelhaas HJ, Post B, Diekstra A, et al. Rapidly deteriorating course in Dutch hereditary spastic paraplegia type 11 patients. Eur J Hum Genet. 2013;21:1312–5.
Riedijk SR, Vugt MED, Duivenvoorden HJ, Niermeijer MF, van Swieten JC, Verhey FRJ, et al. Caregiver burden, health-related quality of life and coping in dementia caregivers: a comparison of frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn. 2006;22:405–12.
Acknowledgements
The authors would like to thank all patients for their participation in this study. Figure 5 was compiled with BioRender.com.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation; 270949263/GRK2162 to JW and MR), by the German Bundesministerium für Bildung und Forschung (BMBF) through the treatHSP consortium (01GM1905B to JW and MR), by the “Förderverein für HSP-Forschung”, and by the “Forschungsstiftung Medizin” at the University Hospital Erlangen. MR is a fellow of the Clinician Scientist Programme (IZKF, University Hospital Erlangen).
Author information
Authors and Affiliations
Contributions
KSU conceptualized the study, performed neuropsychological assessments, analyzed data, and prepared the original manuscript draft. ZK conceptualized the study and critically revised the manuscript. DCM analyzed MRI data and revised the manuscript. AD performed MRI acquisitions and revised the manuscript. JW conceptualized the study, recruited patients and critically revised the manuscript. MS conceptualized the study, analyzed MRI data, prepared figures and critically revised the manuscript. MR conceptualized the study, recruited patients, analyzed data and prepared the original manuscript draft and figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) under protocols no. 259_17B and 347_17B. All participants and legal guardians (if applicable) provided a written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Figure S1:
Individual progression of both Reaction Time and SPRS in SPG11. Table S1: Demographic characteristics of SPG11 and in-house control imaging cohorts. Table S2: Longitudinal results of cognitive parameters (n = 7 patients, mean interval of 24 months). Table S3: Correlation coefficient (r) matrix of imaging data with neuropsychological and motor measures. Table S4: Overview of previous studies applying neuropsychological testing in SPG11 HSP. Supplemental Methods. Supplemental References.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Utz, K.S., Kohl, Z., Marterstock, D.C. et al. Neuropsychology and MRI correlates of neurodegeneration in SPG11 hereditary spastic paraplegia. Orphanet J Rare Dis 17, 301 (2022). https://doi.org/10.1186/s13023-022-02451-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-022-02451-1