Abstract
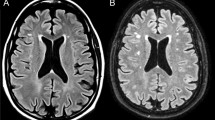
SPG4 is an autosomal dominant pure form of hereditary spastic paraplegia (HSP) caused by mutations in the SPAST gene. HSP is considered an upper motor neuron disorder characterized by progressive spasticity and weakness of the lower limbs caused by degeneration of the corticospinal tract. In other neurodegenerative motor disorders, the thalamus and basal ganglia are affected, with a considerable impact on disease progression. However, only a few works have studied these brain structures in HSP, mainly in complex forms of this disease. Our research aims to detect potential alterations in the volume and shape of the thalamus and various basal ganglia structures by comparing 12 patients with pure HSP and 18 healthy controls. We used two neuroimaging procedures: automated segmentation of the subcortical structures (thalamus, hippocampus, caudate nucleus, globus pallidus, and putamen) in native space and shape analysis of the structures. We found a significant reduction in thalamic volume bilaterally, as well as an inward deformation, mainly in the sensory-motor thalamic regions in patients with pure HSP and a mutation in SPG4. We also observed a significant negative correlation between the shape of the thalamus and clinical scores (the Spastic Paraplegia Rating Scale score and disease duration). Moreover, we found a ‘Group × Age’ interaction that was closely related to the severity of the disease. No differences in volume or in shape were found in the remaining subcortical structures studied. Our results suggest that changes in structure of the thalamus could be an imaging biomarker of disease progression in pHSP.


Similar content being viewed by others
Availability of data and material
Under request to Corresponding author.
References
Harding AE (1983) Classification of the hereditary ataxias and paraplegias. Lancet 321:1151–1155. https://doi.org/10.1016/S0140-6736(83)92879-9
Fink JK (2013) Hereditary spastic paraplegia: Clinico-pathologic features and emerging molecular mechanisms. Acta Neuropathol 126:307–328. https://doi.org/10.1007/s00401-013-1115-8
Lo Giudice T, Lombardi F, Santorelli FM et al (2014) Hereditary spastic paraplegia: Clinical-genetic characteristics and evolving molecular mechanisms. Exp Neurol 261:518–539. https://doi.org/10.1016/j.expneurol.2014.06.011
de Souza PVS, de Rezende Pinto WBV, de Rezende Batistella GN et al (2017) Hereditary spastic paraplegia: clinical and genetic hallmarks. Cerebellum 16:525–551. https://doi.org/10.1007/s12311-016-0803-z
Kadnikova VA, Ryzhkova OP, Rudenskaya GE, Polyakov AV (2019) Molecular genetic diversity and dna diagnostics of hereditary spastic paraplegia. Biol Bull Rev 9:145–156. https://doi.org/10.1134/s2079086419020063
Da Graça FF, De Rezende TJR, Vasconcellos LFR et al (2019) Neuroimaging in hereditary spastic paraplegias: Current use and future perspectives. Front Neurol 10:1117. https://doi.org/10.3389/fneur.2018.01117
Rezende TJR, De Albuquerque M, Lamas GM et al (2015) Multimodal MRI-based study in patients with SPG4 mutations. PLoS ONE 10:e0117666. https://doi.org/10.1371/journal.pone.0117666
Schieving JH, de Bot ST, van de Pol LA et al (2019) De novo SPAST mutations may cause a complex SPG4 phenotype. Brain 142:e31. https://doi.org/10.1093/brain/awz140
Solowska JM, Baas PW (2015) Hereditary spastic paraplegia SPG4: What is known and not known about the disease. Brain 138:2471–2484. https://doi.org/10.1093/brain/awv178
Hazan J, Fonknechten N, Mavel D et al (1999) Spastin, a new AAA protein, is altered in the most frequent form of autosomal dominant spastic paraplegia. Nat Genet 23:296–303. https://doi.org/10.1038/15472
Liao X, Huang M, Xing W et al (2018) Resting state fMRI studies in SPG4-linked hereditary spastic paraplegia. J Neurol Sci 384:1–6. https://doi.org/10.1016/j.jns.2017.10.048
Rucco R, Liparoti M, Jacini F et al (2019) Mutations in the SPAST gene causing hereditary spastic paraplegia are related to global topological alterations in brain functional networks. Neurol Sci 40:979–984. https://doi.org/10.1007/s10072-019-3725-y
Scheuer KH, Nielsen JE, Krabbe K et al (2005) Reduced regional cerebral blood flow in SPG4-linked hereditary spastic paraplegia. J Neurol Sci 235:23–32. https://doi.org/10.1016/j.jns.2005.03.051
Duning T, Warnecke T, Schirmacher A et al (2010) Specific pattern of early white-matter changes in pure hereditary spastic paraplegia. Mov Disord 25:1986–1992. https://doi.org/10.1002/mds.23211
Lindig T, Bender B, Hauser TK et al (2015) Gray and white matter alterations in hereditary spastic paraplegia type SPG4 and clinical correlations. J Neurol 262:1961–1971. https://doi.org/10.1007/s00415-015-7791-7
Kassubek J, Juengling FD, Baumgartner A et al (2007) Different regional brain volume loss in pure and complicated hereditary spastic paraparesis: A voxel-based morphometric study. Amyotroph Lateral Scler 8:328–336. https://doi.org/10.1080/17482960701500718
Unrath A, Müller HP, Riecker A et al (2010) Whole brain-based analysis of regional white matter tract alterations in rare motor neuron diseases by diffusion tensor imaging. Hum Brain Mapp 31:1727–1740. https://doi.org/10.1002/hbm.20971
Lin JZ, Zheng HH, Ma QL et al (2020) Cortical damage associated with cognitive and motor impairment in hereditary spastic paraplegia: evidence of a novel SPAST mutation. Front Neurol 11:399. https://doi.org/10.3389/fneur.2020.00399
Agosta F, Rocca MA, Valsasina P et al (2009) A longitudinal diffusion tensor MRI study of the cervical cord and brain in amyotrophic lateral sclerosis patients. J Neurol Neurosurg Psychiatry 80:53–55. https://doi.org/10.1136/jnnp.2008.154252
Bede P, Elamin M, Byrne S et al (2013) Basal ganglia involvement in amyotrophic lateral sclerosis. Neurology 81:2107–2115. https://doi.org/10.1212/01.wnl.0000437313.80913.2c
Menke RAL, Proudfoot M, Talbot K, Turner MR (2018) The two-year progression of structural and functional cerebral MRI in amyotrophic lateral sclerosis. NeuroImage Clin 17:953–961. https://doi.org/10.1016/j.nicl.2017.12.025
Hehr U, Bauer P, Winner B et al (2007) Long-term course and mutational spectrum of spatacsin-linked spastic paraplegia. Ann Neurol 62:656–665. https://doi.org/10.1002/ana.21310
Örlén H, Melberg A, Raininko R et al (2009) SPG11 mutations cause Kjellin syndrome, a hereditary spastic paraplegia with thin corpus callosum and central retinal degeneration. Am J Med Genet Part B Neuropsychiatr Genet 150:984–992. https://doi.org/10.1002/ajmg.b.30928
Samaranch L, Riverol M, Masdeu JC et al (2008) SPG11 compound mutations in spastic paraparesis with thin corpus callosum. Neurology 71:332–336. https://doi.org/10.1212/01.wnl.0000319646.23052.d1
Ueda M, Katayama Y, Kamiya T et al (1998) Hereditary spastic paraplegia with a thin corpus callosum and thalamic involvement in Japan. Neurology 51:1751–1754. https://doi.org/10.1212/WNL.51.6.1751
Faber I, Martinez ARM, de Rezende TJR et al (2018) SPG11 mutations cause widespread white matter and basal ganglia abnormalities, but restricted cortical damage. NeuroImage Clin 19:848–857. https://doi.org/10.1016/j.nicl.2018.05.031
França MC, Yasuda CL, Pereira FRS et al (2012) White and grey matter abnormalities in patients with SPG11 mutations. J Neurol Neurosurg Psychiatry 83:828–833. https://doi.org/10.1136/jnnp-2011-300129
Seidel K, De Vos R, Derksen L et al (2009) Widespread thalamic and cerebellar degeneration in a patient with a complicated hereditary spastic paraplegia (HSP). Ann Anat 191:203–211. https://doi.org/10.1016/j.aanat.2008.11.003
Falco M, Scuderi C, Musumeci S et al (2004) Two novel mutations in the spastin gene (SPG4) found by DHPLC mutation analysis. Neuromuscul Disord 14:750–753. https://doi.org/10.1016/j.nmd.2004.05.017
Crippa F, Panzeri C, Martinuzzi A et al (2006) Eight novel mutations in SPG4 in a large sample of patients with hereditary spastic paraplegia. Arch Neurol 63:750–755. https://doi.org/10.1001/archneur.63.5.750
Álvarez V, Sánchez-Ferrero E, Beetz C et al (2010) Mutational spectrum of the SPG4 (SPAST) and SPG3A (ATL1) genes in Spanish patients with hereditary spastic paraplegia. BMC Neurol 10:89. https://doi.org/10.1186/1471-2377-10-89
Schickel J, Beetz C, Frömmel C et al (2006) Unexpected pathogenic mechanism of a novel mutation in the coding sequence of SPG4 (spastin). Neurology 66:421–423. https://doi.org/10.1212/01.wnl.0000196468.01815.55
Depienne C, Fedirko E, Faucheux JM et al (2007) A de novo SPAST mutation leading to somatic mosaicism is associated with a later age at onset in HSP. Neurogenetics 8:231–233. https://doi.org/10.1007/s10048-007-0090-4
Schüle R, Holland-Letz T, Klimpe S et al (2006) The spastic paraplegia rating scale (SPRS): A reliable and valid measure of disease severity. Neurology 67:430–434. https://doi.org/10.1212/01.wnl.0000228242.53336.90
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Schmitz-Hübsch T, Du Montcel ST, Baliko L et al (2006) Scale for the assessment and rating of ataxia: Development of a new clinical scale. Neurology 66:1717–1720. https://doi.org/10.1212/01.wnl.0000219042.60538.92
Smith SM, Jenkinson M, Woolrich MW et al (2004) Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 23:S208–S219. https://doi.org/10.1016/j.neuroimage.2004.07.051
Zhang Y, Brady M, Smith S (2001) Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging 20:45–57. https://doi.org/10.1109/42.906424
Patenaude B, Smith SM, Kennedy DN, Jenkinson M (2011) A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage 56:907–922. https://doi.org/10.1016/j.neuroimage.2011.02.046
Tournier JD, Smith R, Raffelt D et al (2019) MRtrix3: A fast, flexible and open software framework for medical image processing and visualisation. Neuroimage 202:551739. https://doi.org/10.1016/j.neuroimage.2019.116137
Veraart J, Fieremans E, Novikov DS (2016) Diffusion MRI noise mapping using random matrix theory. Magn Reson Med 76:1582–1593. https://doi.org/10.1002/mrm.26059
Veraart J, Novikov DS, Christiaens D et al (2016) Denoising of diffusion MRI using random matrix theory. Neuroimage 142:394–406. https://doi.org/10.1016/j.neuroimage.2016.08.016
Kellner E, Dhital B, Kiselev VG, Reisert M (2016) Gibbs-ringing artifact removal based on local subvoxel-shifts. Magn Reson Med 76:1574–1581. https://doi.org/10.1002/mrm.26054
Tustison NJ, Avants BB, Cook PA et al (2010) N4ITK: Improved N3 bias correction. IEEE Trans Med Imaging 29:1310–1320. https://doi.org/10.1109/TMI.2010.2046908
Avants BB, Tustison NJ, Song G et al (2011) A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage 54:2033–2044. https://doi.org/10.1016/j.neuroimage.2010.09.025
Andersson JLR, Sotiropoulos SN (2016) An integrated approach to correction for off-resonance effects and subject movement in diffusion MR imaging. Neuroimage 125:1063–1078. https://doi.org/10.1016/j.neuroimage.2015.10.019
Tournier JD, Calamante F, Connelly A (2007) Robust determination of the fibre orientation distribution in diffusion MRI: Non-negativity constrained super-resolved spherical deconvolution. Neuroimage 35:1459–1472. https://doi.org/10.1016/j.neuroimage.2007.02.016
Tournier JD, Calamante F, Connelly A (2013) Determination of the appropriate b value and number of gradient directions for high-angular-resolution diffusion-weighted imaging. NMR Biomed 26:1775–1786. https://doi.org/10.1002/nbm.3017
Behrens TEJ, Johansen-Berg H, Woolrich MW et al (2003) Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat Neurosci 6:750–757. https://doi.org/10.1038/nn1075
Mayka MA, Corcos DM, Leurgans SE, Vaillancourt DE (2006) Three-dimensional locations and boundaries of motor and premotor cortices as defined by functional brain imaging: A meta-analysis. Neuroimage 31:1453–1474. https://doi.org/10.1016/j.neuroimage.2006.02.004
Calamante F, Tournier JD, Heidemann RM et al (2011) Track density imaging (TDI): Validation of super resolution property. Neuroimage 56:1259–1266. https://doi.org/10.1016/j.neuroimage.2011.02.059
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57:289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x
Winkler AM, Ridgway GR, Webster MA et al (2014) Permutation inference for the general linear model. Neuroimage 92:381–397. https://doi.org/10.1016/j.neuroimage.2014.01.060
Smith SM, Nichols TE (2009) Threshold-free cluster enhancement: Addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44:83–98. https://doi.org/10.1016/j.neuroimage.2008.03.061
Kamps S, van den Heuvel OA, van der Werf YD et al (2019) Smaller subcortical volume in Parkinson patients with rapid eye movement sleep behavior disorder. Brain Imaging Behav 13:1352–1360. https://doi.org/10.1007/s11682-018-9939-4
Schönecker S, Neuhofer C, Otto M et al (2018) Atrophy in the thalamus but not cerebellum is specific for C9orf72 FTD and ALS patients - An atlas-based volumetric MRI study. Front Aging Neurosci 10:45. https://doi.org/10.3389/fnagi.2018.00045
Zou L, Song Y, Zhou X et al (2019) Regional morphometric abnormalities and clinical relevance in Wilson’s disease. Mov Disord 34:545–554. https://doi.org/10.1002/mds.27641
Carrera E, Bogousslavsky J (2006) The thalamus and behavior: Effects of anatomically distinct strokes. Neurology 66:1817–1823. https://doi.org/10.1212/01.wnl.0000219679.95223.4c
Tucker HR, Mahoney E, Chhetri A et al (2019) Deep brain stimulation of the ventroanterior and ventrolateral thalamus improves motor function in a rat model of Parkinson’s disease. Exp Neurol 317:155–167. https://doi.org/10.1016/j.expneurol.2019.03.008
Giraldo-Chica M, Rogers BP, Damon SM et al (2018) Prefrontal-thalamic anatomical connectivity and executive cognitive function in schizophrenia. Biol Psychiatry 83:509–517. https://doi.org/10.1016/j.biopsych.2017.09.022
Schoonheim MM, Hulst HE, Brandt RB et al (2015) Thalamus structure and function determine severity of cognitive impairment in multiple sclerosis. Neurology 84:776–783. https://doi.org/10.1212/WNL.0000000000001285
Haber SN, Calzavara R (2009) The cortico-basal ganglia integrative network: The role of the thalamus. Brain Res Bull 78:69–74. https://doi.org/10.1016/j.brainresbull.2008.09.013
Ross DT, Ebner FF (1990) Thalamic retrograde degeneration following cortical injury: An excitotoxic process? Neuroscience 35:525–550. https://doi.org/10.1016/0306-4522(90)90327-Z
Sørensen JC, Dalmau I, Zimmer J, Finsen B (1996) Microglial reactions to retrograde degeneration of tracer-identified thalamic neurons after frontal sensorimotor cortex lesions in adult rats. Exp Brain Res 112:203–212. https://doi.org/10.1007/bf00227639
Ferrer I, Olive M, Rivera R et al (1995) Hereditary spastic paraparesis with dementia, amyotrophy and peripheral neuropathy. A neuropathological study Neuropathol Appl Neurobiol 21:255–261. https://doi.org/10.1111/j.1365-2990.1995.tb01057.x
Dihné M, Grommes C, Lutzenburg M et al (2002) Different mechanisms of secondary neuronal damage in thalamic nuclei after focal cerebral ischemia in rats. Stroke 33:3006–3011. https://doi.org/10.1161/01.STR.0000039406.64644.CB
Haque ME, Gabr RE, Hasan KM et al (2019) Ongoing secondary degeneration of the limbic system in patients with ischemic stroke: a longitudinal MRI study. Front Neurol. https://doi.org/10.3389/fneur.2019.00154
Kersbergen KJ, De Vries LS, Groenendaal F et al (2015) Corticospinal tract injury precedes thalamic volume reduction in preterm infants with cystic periventricular leukomalacia. J Pediatr 167:260-268.e3. https://doi.org/10.1016/j.jpeds.2015.05.013
Ruano L, Melo C, Silva MC, Coutinho P (2014) The global epidemiology of hereditary ataxia and spastic paraplegia: A systematic review of prevalence studies. Neuroepidemiology 42:174–183
Babalola KO, Patenaude B, Aljabar P et al (2009) An evaluation of four automatic methods of segmenting the subcortical structures in the brain. Neuroimage 47:1435–1447. https://doi.org/10.1016/j.neuroimage.2009.05.029
Acknowledgements
All the authors wish to express our appreciation for the invaluable contribution of the late Dr. Santiago Reig to this study. We are grateful to the patients for their collaboration and to the Asociación Española de Paraparesia Espástica Familiar (AEPEF) for support with patient recruitment.
Funding
This work was supported by Ministerio de Ciencia, Innovación y Universidades and by Instituto de Salud Carlos III projects PS09/01830; PS09/01685; PS09/00839. The ASPIDE project received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 801091. The CNIC is supported by the Instituto de Salud Carlos III (ISCIII), the Ministerio de Ciencia e Innovación (MCIN) and the Pro CNIC Foundation, and is a Severo Ochoa Center of Excellence (SEV‐2015‐0505). S. Carmona, funded by Ministerio de Ciencia, Innovación y Universidades, Instituto de Salud Carlos III, co‐ funded by European Social Fund “Investing in your future” (CP16/00096).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors have any conflict of interest to disclose.
Research involving human participants
The study was approved by the Ethics and Clinical Research Board of Hospital Gregorio Marañón. Written informed consent was obtained from all patients before their participation in the study.
Author roles in the manuscript
(1. Research project: A. Conception, B. Organization, C. Execution; 2. Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript Preparation: A. Writing of the first draft, B. Review and Critique.): Francisco J. Navas-Sánchez: 1B, 1C, 2A, 2B, 3A, 3B; Alberto Fernández-Pena: 1C, 2C, 3B; Daniel Martín de Blas: 2C, 3B; Yasser Alemán-Gómez: 1B, 2C, 3B; Luís Marcos-Vidal: 2C, 3B; Juan A. Guzmán-de-Villoria: 1C, 3B; Pilar Fernández-García: 1C, 3B; Julia Romero: 1C, 3B; Irene Catalina: 1C, 3B; Laura Lillo: 1C, 3B; José L. Muñoz-Blanco: 1C, 3B; Andrés Ordoñez-Ugalde: 1C, 3B; Beatriz Quintáns: 1C, 3B; Julio Pardo: 1C, 3B; María-Jesús Sobrido: 1C, 3B; Susanna Carmona: 1C, 3B; Francisco Grandas: 1A, 1B, 1C, 2C, 3B; Manuel Desco: 1A, 1B, 2C, 3B;
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Navas-Sánchez, F.J., Fernández-Pena, A., Martín de Blas, D. et al. Thalamic atrophy in patients with pure hereditary spastic paraplegia type 4. J Neurol 268, 2429–2440 (2021). https://doi.org/10.1007/s00415-020-10387-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10387-4