Abstract
Background
SPG4 is a subtype of hereditary spastic paraplegia (HSP), an upper motor neuron disorder characterized by axonal degeneration of the corticospinal tracts and the fasciculus gracilis. The few neuroimaging studies that have focused on the spinal cord in HSP are based mainly on the analysis of structural characteristics.
Methods
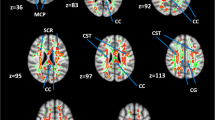
We assessed diffusion-related characteristics of the spinal cord using diffusion tensor imaging (DTI), as well as structural and shape-related properties in 12 SPG4 patients and 14 controls. We used linear mixed effects models up to T3 in order to analyze the global effects of 'group' and 'clinical data' on structural and diffusion data. For DTI, we carried out a region of interest (ROI) analysis in native space for the whole spinal cord, the anterior and lateral funiculi, and the dorsal columns. We also performed a voxelwise analysis of the spinal cord to study local diffusion-related changes.
Results
A reduced cross-sectional area was observed in the cervical region of SPG4 patients, with significant anteroposterior flattening. DTI analyses revealed significantly decreased fractional anisotropy (FA) and increased radial diffusivity at all the cervical and thoracic levels, particularly in the lateral funiculi and dorsal columns. The FA changes in SPG4 patients were significantly related to disease severity, measured as the Spastic Paraplegia Rating Scale score.
Conclusions
Our results in SPG4 indicate tract-specific axonal damage at the level of the cervical and thoracic spinal cord. This finding is correlated with the degree of motor disability.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Harding AE (1981) Hereditary “pure” spastic paraplegia: a clinical and genetic study of 22 families. J Neurol Neurosurg Psychiatry 44:871–883. https://doi.org/10.1136/jnnp.44.10.871
Solowska JM, Baas PW (2015) Hereditary spastic paraplegia SPG4: what is known and not known about the disease. Brain 138:2471–2484. https://doi.org/10.1093/brain/awv178
DeLuca GC, Ebers GC, Esiri MM (2004) The extent of axonal loss in the long tracts in hereditary spastic paraplegia. Neuropathol Appl Neurobiol 30:576–584. https://doi.org/10.1111/j.1365-2990.2004.00587.x
White KD, Ince PG, Lusher M et al (2000) Clinical and pathologic findings in hereditary spastic paraparesis with spastin mutation. Neurology 55:89–94. https://doi.org/10.1212/WNL.55.1.89
Kuru S, Sakai M, Konagaya M et al (2005) Autopsy case of hereditary spastic paraplegia with thin corpus callosum showing severe gliosis in the cerebral white matter. Neuropathology 25:346–352. https://doi.org/10.1111/j.1440-1789.2005.00620.x
Lin JZ, Zheng HH, Ma QL et al (2020) Cortical damage associated with cognitive and motor impairment in hereditary spastic paraplegia: evidence of a novel SPAST mutation. Front Neurol 11:399. https://doi.org/10.3389/fneur.2020.00399
List J, Kohl Z, Winkler J et al (2019) Ascending axonal degeneration of the corticospinal tract in pure hereditary spastic paraplegia: a cross-sectional DTI study. Brain Sci 9:268. https://doi.org/10.3390/brainsci9100268
Montanaro D, Vavla M, Frijia F et al (2020) Multimodal MRI longitudinal assessment of white and gray matter in different SPG types of hereditary spastic paraparesis. Front Neurosci 14:325. https://doi.org/10.3389/fnins.2020.00325
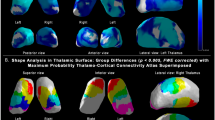
Navas-Sánchez FJ, Fernández-Pena A, Martín de Blas D et al (2021) Thalamic atrophy in patients with pure hereditary spastic paraplegia type 4. J Neurol 268:2429–2440. https://doi.org/10.1007/s00415-020-10387-4
Rezende TJR, De Albuquerque M, Lamas GM et al (2015) Multimodal MRI-based study in patients with SPG4 mutations. PLoS ONE 10:e0117666. https://doi.org/10.1371/journal.pone.0117666
Da Graça FF, De Rezende TJR, Vasconcellos LFR et al (2019) Neuroimaging in hereditary spastic paraplegias: Current use and future perspectives. Front Neurol 10:1117. https://doi.org/10.3389/fneur.2018.01117
Sperfeld AD, Baumgartner A, Kassubek J (2006) Magnetic resonance investigation of the upper spinal cord in pure and complicated hereditary spastic paraparesis. Eur Neurol 54:181–185. https://doi.org/10.1159/000090294
Hedera P, Eldevik OP, Maly P et al (2005) Spinal cord magnetic resonance imaging in autosomal dominant hereditary spastic paraplegia. Neuroradiology 47:730–734. https://doi.org/10.1007/s00234-005-1415-3
Loureiro JL, Brandão E, Ruano L et al (2013) Autosomal dominant spastic paraplegias: a review of 89 families resulting from a Portuguese survey. JAMA Neurol 70:481–487. https://doi.org/10.1001/jamaneurol.2013.1956
Hourani R, El-Hajj T, Barada WH et al (2009) MR imaging findings in autosomal recessive hereditary spastic paraplegia. Am J Neuroradiol 30:936–940. https://doi.org/10.3174/ajnr.A1483
Masciullo M, Tessa A, Perazza S et al (2016) Hereditary spastic paraplegia: novel mutations and expansion of the phenotype variability in SPG56. Eur J Paediatr Neurol. https://doi.org/10.1016/j.ejpn.2016.02.001
Servelhere KR, Casseb RF, de Lima FD et al (2021) Spinal cord gray and white matter damage in different hereditary spastic paraplegia subtypes. Am J Neuroradiol 42:610–615. https://doi.org/10.3174/ajnr.A7017
Krabbe K, Nielsen JE, Fallentin E et al (1997) MRI of autosomal dominant pure spastic paraplegia. Neuroradiology 39:724–727. https://doi.org/10.1007/s002340050495
Branco LMT, De Albuquerque M, De Andrade HMT et al (2014) Spinal cord atrophy correlates with disease duration and severity in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Front Degener. https://doi.org/10.3109/21678421.2013.852589
Moccia M, Prados F, Filippi M et al (2019) Longitudinal spinal cord atrophy in multiple sclerosis using the generalized boundary shift integral. Ann Neurol. https://doi.org/10.1002/ana.25571
Klawiter EC, Schmidt RE, Trinkaus K et al (2011) Radial diffusivity predicts demyelination in ex vivo multiple sclerosis spinal cords. Neuroimage. https://doi.org/10.1016/j.neuroimage.2011.01.007
Patzig M, Bochmann K, Lutz J et al (2019) Measurement of structural integrity of the spinal cord in patients with amyotrophic lateral sclerosis using diffusion tensor magnetic resonance imaging. PLoS ONE. https://doi.org/10.1371/journal.pone.0224078
Wolanczyk M, Bladowska J, Koltowska A et al (2020) Diffusion tensor imaging of normal-appearing cervical spinal cords in patients with multiple sclerosis: correlations with clinical evaluation and cerebral diffusion tensor imaging changes. Preliminary experience. Adv Clin Exp Med. https://doi.org/10.17219/acem/116754
Pisharady PK, Eberly LE, Cheong I et al (2020) Tract-specific analysis improves sensitivity of spinal cord diffusion MRI to cross-sectional and longitudinal changes in amyotrophic lateral sclerosis. Commun Biol. https://doi.org/10.1038/s42003-020-1093-z
Schüle R, Holland-Letz T, Klimpe S et al (2006) The spastic paraplegia rating scale (SPRS): a reliable and valid measure of disease severity. Neurology 67:430–434. https://doi.org/10.1212/01.wnl.0000228242.53336.90
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Schmitz-Hübsch T, Du Montcel ST, Baliko L et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66:1717–1720. https://doi.org/10.1212/01.wnl.0000219042.60538.92
Veraart J, Novikov DS, Christiaens D et al (2016) Denoising of diffusion MRI using random matrix theory. Neuroimage 142:394–406. https://doi.org/10.1016/j.neuroimage.2016.08.016
Kellner E, Dhital B, Kiselev VG, Reisert M (2016) Gibbs-ringing artifact removal based on local subvoxel-shifts. Magn Reson Med 76:1574–1581. https://doi.org/10.1002/mrm.26054
Tournier JD, Smith R, Raffelt D et al (2019) MRtrix3: a fast, flexible and open software framework for medical image processing and visualisation. Neuroimage 202:551739. https://doi.org/10.1016/j.neuroimage.2019.116137
Andersson JLR, Sotiropoulos SN (2016) An integrated approach to correction for off-resonance effects and subject movement in diffusion MR imaging. Neuroimage 125:1063–1078. https://doi.org/10.1016/j.neuroimage.2015.10.019
Andersson JLR, Graham MS, Zsoldos E, Sotiropoulos SN (2016) Incorporating outlier detection and replacement into a non-parametric framework for movement and distortion correction of diffusion MR images. Neuroimage 141:556–572. https://doi.org/10.1016/j.neuroimage.2016.06.058
De Leener B, Lévy S, Dupont SM et al (2017) SCT: Spinal Cord Toolbox, an open-source software for processing spinal cord MRI data. Neuroimage. https://doi.org/10.1016/j.neuroimage.2016.10.009
De Leener B, Kadoury S, Cohen-Adad J (2014) Robust, accurate and fast automatic segmentation of the spinal cord. Neuroimage. https://doi.org/10.1016/j.neuroimage.2014.04.051
Gros C, De Leener B, Badji A et al (2019) Automatic segmentation of the spinal cord and intramedullary multiple sclerosis lesions with convolutional neural networks. Neuroimage. https://doi.org/10.1016/j.neuroimage.2018.09.081
Ullmann E, Pelletier Paquette JF, Thong WE, Cohen-Adad J (2014) Automatic labeling of vertebral levels using a robust template-based approach. Int J Biomed Imaging. https://doi.org/10.1155/2014/719520
De Leener B, Fonov VS, Collins DL et al (2018) PAM50: Unbiased multimodal template of the brainstem and spinal cord aligned with the ICBM152 space. Neuroimage. https://doi.org/10.1016/j.neuroimage.2017.10.041
De Leener B, Mangeat G, Dupont S et al (2017) Topologically preserving straightening of spinal cord MRI. J Magn Reson Imaging 46:1209–1219. https://doi.org/10.1002/jmri.25622
Raffelt D, Tournier JD, Fripp J et al (2011) Symmetric diffeomorphic registration of fibre orientation distributions. Neuroimage 56:1171–1180. https://doi.org/10.1016/j.neuroimage.2011.02.014
Lévy S, Benhamou M, Naaman C et al (2015) White matter atlas of the human spinal cord with estimation of partial volume effect. Neuroimage. https://doi.org/10.1016/j.neuroimage.2015.06.040
Winkler AM, Ridgway GR, Webster MA et al (2014) Permutation inference for the general linear model. Neuroimage 92:381–397. https://doi.org/10.1016/j.neuroimage.2014.01.060
Smith SM, Nichols TE (2009) Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44:83–98. https://doi.org/10.1016/j.neuroimage.2008.03.061
Lindsey JC, Bushby KMD, Lusher ME et al (2000) Mutation analysis of the spastin gene (SPG4) in patients with hereditary spastic paraparesis. J Med Genet. https://doi.org/10.1136/jmg.37.10.759
Beaulieu C (2002) The basis of anisotropic water diffusion in the nervous system—a technical review. NMR Biomed. https://doi.org/10.1002/nbm.782
Jones DK, Knösche TR, Turner R (2013) White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage. https://doi.org/10.1016/j.neuroimage.2012.06.081
Song SK, Yoshino J, Le TQ et al (2005) Demyelination increases radial diffusivity in corpus callosum of mouse brain. Neuroimage. https://doi.org/10.1016/j.neuroimage.2005.01.028
Kronlage M, Pitarokoili K, Schwarz D et al (2017) Diffusion tensor imaging in chronic inflammatory demyelinating polyneuropathy. Invest Radiol 52:701–707. https://doi.org/10.1097/RLI.0000000000000394
Tu TW, Williams RA, Lescher JD et al (2016) Radiological-pathological correlation of diffusion tensor and magnetization transfer imaging in a closed head traumatic brain injury model. Ann Neurol 79:907–920. https://doi.org/10.1002/ana.24641
Tarrade A, Fassier C, Courageot S et al (2006) A mutation of spastin is responsible for swellings and impairment of transport in a region of axon characterized by changes in microtubule composition. Hum Mol Genet 15:3544–3558. https://doi.org/10.1093/hmg/ddl431
Wharton SB, McDermott CJ, Grierson AJ et al (2003) The cellular and molecular pathology of the motor system in hereditary spastic paraparesis due to mutation of the Spastin gene. J Neuropathol Exp Neurol 62:1166–1177. https://doi.org/10.1093/jnen/62.11.1166
Acknowledgements
All the authors wish to express our appreciation for the invaluable contribution of the late Dr. Santiago Reig to this study. We are grateful to the patients for their collaboration and the Asociación Española de Paraparesia Espástica Familiar (AEPEF) for their support with patient recruitment.
Funding
This work was supported by Ministerio de Ciencia, Innovación y Universidades and by Instituto de Salud Carlos III projects PS09/01830, PS09/01685, and PS09/00839. The ASPIDE project received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 801091. The CNIC is supported by the Instituto de Salud Carlos III (ISCIII), the Ministerio de Ciencia e Innovación (MCIN) and the Pro CNIC Foundation and is a Severo Ochoa Center of Excellence (SEV‐2015‐0505). Susanna Carmona is funded by Instituto de Salud Carlos III, Miguel Servet Type I research contract (CP16/00096).
Author information
Authors and Affiliations
Contributions
1A. Design of the work; 1B. Acquisition and analysis, 1C. Interpretation of data for the work; 2. Drafting the work or revising it critically for important intellectual content; 3. Final approval of the version to be published; 4. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved). FJNS: 1A, 1B, 1C, 2, 3, 4; LMV: 1B, 1C, 3, 4; DMdB: 1B, 2, 3, 4; AFP: 1B, 2, 3, 4; YAG: 1A, 1B 3, 4; JAGdV: 1B, 3, 4; JR: 1B, 3, 4; IC: 1B, 3, 4; LL: 1B, 3, 4; JLMB: 1B, 3, 4; AOU: 1B, 3, 4; BQ: 1B, 3, 4; MJS: 1A, 1B, 3, 4; SC: 1C, 2, 3, 4; FG: 1A, 1C, 2, 3, 4; MD: 1A, 1C, 2, 3, 4.
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors have any conflicts of interest to disclose.
Research involving human participants
The study was approved by the Ethics and Clinical Research Board of Hospital Gregorio Marañón.
Informed consent
Written informed consent was obtained from all patients before they participated in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Navas-Sánchez, F.J., Marcos-Vidal, L., de Blas, D.M. et al. Tract-specific damage at spinal cord level in pure hereditary spastic paraplegia type 4: a diffusion tensor imaging study. J Neurol 269, 3189–3203 (2022). https://doi.org/10.1007/s00415-021-10933-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10933-8