Abstract
Background
Performing total joint arthroplasty (TJA) in Parkinson’s disease (PD) patients may encounter a higher complication rate or worse functional outcomes compared with common patients. The relationship between PD and clinical outcomes after TJA is not fully understood.
Methods
Retrospectively, we used manual charts to investigate the clinical outcomes in 41 patients including 24 total hip arthroplasty (THA) patients (28 hips) and 18 total knee arthroplasty (TKA) patients (22 knees) with a diagnosis of PD from 2009 to 2016. The stage of PD was confirmed by Hoehn and Yahr scale. Prosthesis survivorship was estimated with revision for any reason as the endpoint.
Result
All the clinical outcomes improved significantly (p < 0.05). Subgroup analysis revealed worse functional outcomes in mid- or end-stage PD patients. Sixteen short-term mild to moderate complications were noted. Two revisions were conducted for hip periprosthetic osteolysis and postoperative knee pain. The prosthesis survivorship at 60 months for TJA, total hip arthroplasty (THA), or total knee arthroplasty (TKA) was 91.6%, 94.1%, and 87.5%, respectively.
Conclusion
Patients with PD who underwent TJA would result in excellent pain relief and gain of function. However, patients at late-stage PD may suffer from functional loss. The effectiveness of TJA in patients with severe PD remains a concern. Physician should help delay the progression of PD which may optimize and stabilize the functional outcomes of TJA.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease (after Alzheimer’s disease) with a life expectancy of 7–14 years [1]. The incidence of PD in high-income countries is 14 per 100,000 and 160 per 100,000 in people aged over 65 years [2]. The motor symptoms of PD are the most prominent including bradykinesia, muscular rigidity, rest tremor, and postural and gait impairment [1]. Many PD patients demand lower limb total joint arthroplasty (TJA) for different reasons including end-stage osteoarthritis (OA), fracture, or osteonecrosis of the femoral head [3]. With the motor symptoms, the surgical outcomes may be affected.
The connection between PD and the potential requirement of TJA has been studied. Gait abnormality and instability mean a higher rate of fall of patients with PD. The study suggested that 60.5% of participants reported at least one fall, with 39% reporting recurrent falls [4]. A relevant study confirmed 4.48 times more likely of PD patients experienced hip fracture caused by severe falls [5, 6] which may sustain primary total hip arthroplasty or revision surgeries. Prior research showed that patients with PD and OA seemed suffered from akathisia, paraesthesia, and heightened pain level in comparison with OA alone [7]. Besides, previous researches have demonstrated a higher rate of complications after THA or TKA could be seen in patients with PD.
PD is a progressive disease characterized by worsening of motor features [1]. Hoehn and Yahr (H-Y) scale (Table 1) is the most commonly used form to define the stage of PD since 1967 [8]. The stage progresses with a median time range from 20 to 62 months while the motor symptoms worsen with progression [9]. At the end stage of PD (H-Y stage 5), usually with a course of 10–20 years, patients would be bed or wheelchair bounded and require home nursing [10, 11]. Therefore, the outcomes of TJA may be affected by severe functional loss.
Therefore, this study aims to demonstrate the mid-term pain and functional outcomes of PD patients who underwent THA or TKA. Further subgroup analysis would be done to demonstrate the potential relationship between the stage of PD and the outcomes of patients.
Materials and methods
Patients selection
After the approval of the Institutional Review Board of West China Hospital, this retrospective study was conducted at West China Hospital, Sichuan University, which serves as a tertiary level center and the largest medical center in the southwest China. Patients with the diagnosis of PD who underwent primary total hip or knee arthroplasty between June 2009 and June 2016 were included in our study and established TKA and THA groups afterward. The informed consent was obtained. Patients who meet the following conditions would be excluded: (1) not primary joint arthroplasty, (2) patient with other neurological diseases, and (3) patient with severe or uncontrolled comorbidities.
A total of 56 consecutive patients were primarily included in our study. Among them, seven patients were failed to follow-up due to the incorrect telephone numbers, four patients were excluded for incomplete chart filling, and four patients were excluded for not being primarily admitted. No demise happened during follow-up. Therefore, 41 patients including 24 THA patients (28 hips) and 18 TKA patients (22 knees) were finally enrolled in the study. One of the patients received both THA and TKA successively. The median duration of follow-up is 41.00 months (IQR 32.00–67.75) for all the candidates and, separately, 51.50 months (IQR 34.00–72.00) for THA patients and 38.00 months (IQR 29.75–50.75) for TKA patients. There were 14 males and 31 females with an average age of 67.86 years (range, 47–85). The body mass index (BMI) was 22.73 kg/m2 in average (range, 15.63–31.11). More baseline demographics could be referred to in Table 2.
Clinical data
The collection of the clinical data and evaluation was conducted by two independent observers (X-R and ZY-L). Our patients would undergo routine follow-up at postoperatively 3 weeks, 6 weeks, 12 weeks, and 6 months and annually. And manual chart interview was adopted for evaluation of the preoperative and postoperative clinical outcomes. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (pain, stiffness, and function) and The Short Form (12) Health Survey scale (SF-12) (physical component summary (PCS) and mental component summary (MCS)) were used for all the candidates. Respectively, for THA patients, Harris Hip Score (HHS) was used to evaluate the pain, function, and deformity. Moreover, for TKA patients, Knee Society Score (KSS) and Knee Society Function Score (KSFS) were used in terms of stability, pain, deformity, and function evaluation. The multiple scales provided a more comprehensive assessment which would cover pain and function, mental and physical state, daily activity, quality of life, and symptoms. Other evaluation terms including the preoperative and postoperative range of motion (ROM) and the severity of PD was assessed by Hoehn and Yahr scale [8] (Table 1).
Subgroup analysis
PD patients at H-Y stage I or II could keep balance, remain independent, and be functional free. However, at stage III, patients would develop postural instability with mild functional restriction. At stage IV or V, these symptoms deteriorate, and severe disability could be seen. Based on this phenomenon, we enrolled patients at stage I or II into the functional free group (group I). Patients at stage III to V were enrolled in the functional restriction group (group II). The clinical outcomes were compared between them.
Statistical analysis
Quantitative data were presented as means and standard deviations or as median with the interquartile ranges (IQR 25th and 75th percentiles). Qualitative data were presented with frequencies and percentages. Student’s t test was used to compare the continuous variables while Pearson chi-square test or Fisher exact test was used to analyzing the qualitative comparative variables. For the prosthesis survival analysis, Kaplan-Meier was utilized with any reason as the endpoints for revisions. Spearman correlation analysis was adopted for demonstrating the relationship between ranked data and continuous data. The significance was set at p < 0.05. We used SPSS for Windows (Version 21.0 IBM Corp, Armonk, NY, USA) to perform all the statistical analyses.
Result
Clinical outcomes
The outcomes with regard to hip or knee pain and functions were listed in Table 3. For patients who underwent THA, Harris Hip Score (HHS) demonstrated a significant improvement. The total score improved from 39.00 ± 15.74 preoperatively to 71.39 ± 19.18 postoperatively (p < 0.01). Moreover, in specific terms of pain (18.75 ± 9.92 vs. 38.83 ± 9.26, p < 0.01), function (18.08 ± 7.17 vs. 28.83 ± 13.10, p < 0.01), and deformity (2.17 ± 0.92 vs. 3.73 ± 0.44, p < 0.01), the improvement was obvious as well.
In the aspect of TKA, Knee Society Score showed the same trend of elevation from 61.22 ± 9.66 preoperatively to 91.33 ± 12.57 postoperatively (p < 0.01). Pain (21.07 ± 8.32 vs. 43.61 ± 12.10, p < 0.01) and stability (17.89 ± 2.00 vs. 24.11 ± 1.18, p < 0.01) showed a significant rise while the ROM score (22.22 ± 1.86 vs. 23.61 ± 1.61, p < 0.01) presented a slit elevation but is also statistically significant. KSFS revealed functional relief from 39.72 ± 6.52 to 58.06 ± 31.11 (p = 0.02). Further, WOMAC, SF-12, and ROM were reviewed, and all showed statistically significant improvement (Table 3).
Short-term complications
Six hips (28.43%) and six knees (27.27%) showed 16 mild short-term complications (Table 4). One of the hips (3.57%) experienced intraoperative femoral fracture and were cured with cerclage cable. Upper respiratory infection occurred in two hip cases (7.14%) and one knee case (4.55%) and was cured with antivirus, antibiotic, or atomization inhalation. Two knee cases (9.09%) presented nausea or sour regurgitation while one hip case (3.57%) complained of vomiting. They were controlled with gastroprokinetic agents or omeprazole. Bruise happened in two hips (7.14%) and three knees (13.64%). All of them recovered after withdrawal or reducing the dosage of anticoagulant. One knee (4.55%) presented lower limb swelling which was handled with functional training and rehabilitation. Other short-term complications include delirium (one hip 3.57% and one knee 4.55%), which was controlled with olanzapine, and mild anemia (1 hip, 3.53%) with proper iron agent treatment. No evidence of embolism, hematoma, or nerve palsy was observed.
Survivorship analysis
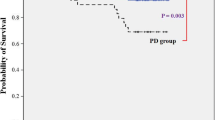
One patient suffered from knee pain after the TKA and was cured with humeral replacement at 44 months postoperatively. Another patient in the THA group presented periprosthetic osteolysis and polyethylene wear at 42 months after primary THA and was treated with revision surgery. No evidence of periprosthetic infection, dislocation, aseptic loosening, or other complications occurred during the follow-up.
Using revision for any reason as the end point, the overall survivorship rate of the lower limb arthroplasty at 60 months was 91.6% (95% CI 80.4–99.9%). Also, for the THA group and TKA group respectively, the 60 months survivorship rate was 94.1% (95% CI 82.9–99.9%) and 87.5% (95% CI 64.6–99.9%) (Fig. 1).
Subgroup analysis
The SF-12 score (PCS and MCS p < 0.01) and the WOMAC pain (p = 0.01) and function score (p < 0.01) revealed significant improvement in group II for the entire case series. Respectively, in the THA group, the HHS score (p = 0.03) and function score (p = 0.03), SF-12 score (PCS p = 0.02, MCS p < 0.01), and the WOMAC function score (p < 0.01) were statistically different between subgroups (Table 5). Of the patients in TKA group, the KSFS (p < 0.01), SF-12 (PCS P < 0.01, MCS p < 0.01), and the WOMAC pain (p = 0.03) and function score (p < 0.01) were significantly higher in group II. Furthermore, comparisons of the final clinical data with preoperative data were done in each group. Significant differences of all the data were seen in group I. However, in group II, there were no differences in HHS function score (p = 0.25) and KSFS (p = 0.50). The SF-12 (THA: PCS, p = 0.69 and MCS, p = 0.61; TKA: PCS, p = 0.10 and MCS, p = 0.26) and WOMAC function score (THA: p = 0.93; TKA: p = 0.74) were not statistically different as well.
Spearman correlation analysis was done to demonstrate the relationship between functional outcomes and the H-Y stage of the patient. For all the candidates, the SF-12 score (r = − 0.67, p < 0.01) and WOMAC function score (r = 0.64, p < 0.01) correlated with the H-Y stage. The HHS function score (r = − 0.53, p < 0.01) in the THA group and KSFS (r = − 0.82, p < 0.01) in the TKA group also demonstrate the same result. The scatter diagrams and the fitted lines are presented in Fig. 2.
Scatter diagram and the fitted lines of functional outcomes and H-Y stages. a Correlation between SF-12 score and H-Y stages. b Correlation between WOMAC Function score and H-Y stages. c Correlation between HHS Function score of THA patients and H-Y stages. d Correlation between KSFS of TKA patients and H-Y stages
Discussion
Total joint arthroplasty in patients with Parkinson’s disease (PD) could be a challenge in functional regaining due to the high risk of fall [4], bone fractures [5, 6], and an increased incidence of osteoporosis [12, 13]. In this study, we retrospectively investigated the clinical outcomes in patients with PD who underwent TKA or THA. We showed both pain and functional outcomes improved significantly after a median follow-up of 41.00 months (IQR 32.00–67.75). We also demonstrated the functional outcomes of PD patients were related to the severity of PD. The result suggested PD patients at advanced stages result in poor function scores compared with early stages. In addition, the functional outcomes of the late-stage patients revealed no significant difference when compared with preoperative data. To explain this phenomenon, we considered the reasons as follows. Firstly, the establishment of the subgroups was based on functional performance. The onset of functional restriction starts at stage III and deteriorate with motor symptoms. Secondly, late-stage non-motor symptoms including depression and sleep disorders worsen the mental state of the patients [14, 15]. Finally, the scales are consist of walking distance, aids usage, stairs climbing, and other daily activities that are highly affected by the motor symptoms. Moreover, the SF-12 scales include the mental health assessment which is affected by the non-motor symptoms. Previous studies presented conflict conclusions with regard to functional outcomes. One study presented improvement in SF-12 scores in PD patients who underwent TJA, but it was greater in the control cohort [16]. Certain studies confirmed poor functional improvement in PD patients after TJA [17, 18], and two studies indicate the functional results depend on the severity and progression of PD [18, 19].
We find mild to moderate complications with acceptable rate happened in this case series. There was no evidence of DVT, embolism, or nerve palsy. Two of our patients suffered from transient delirium and were controlled with olanzapine, which confirmed that orthopedic surgery could induce a cognitive decline in PD patients [20]. Recently, some database studies [21,22,23,24,25,26] showed both TKA and THA in PD patients provide a higher complication rate, longer LOS, and higher charges than the controlled cohort. One study [27] considered the higher complication rate of PD patients was associated with cardiovascular and psychiatric comorbidity. Furthermore, we found excellent prosthetic survivorship in PD patients (60 months, 91.6% (95% CI 80.4–99.9%)). However, previous studies [16, 27] suggested TJA in PD patients resulted in a higher risk of revision or hip dislocation. Recurrent posterior dislocation was also reported in PD patients [28].
Lower limb muscle weakness is common in both postoperative TJA [29, 30] and PD patients [31]. As the adoption of physical exercise and training in improving limb function after TJA, a rehabilitation program is also suitable for patients with PD. A systematic review has confirmed that progressive resistance exercise could effectively improve the quality of daily activities of PD patients [32]. Meanwhile, power-based resistance training could significantly reduce bradykinesia and increased muscle strength and power in older patients with PD [33]. Based on our findings, the stage of the PD patients and the motor symptoms are highly connected with the functional outcomes of the TJA. Future studies may focus on the rehabilitation programs in relieving motor symptoms, delaying stage progression, and thus improving the function of the PD patients.
There are certain limitations to this study. First, the outcomes of our patients were based on conventional questionnaires. It would be more objective and reliable if a quantitative gait analysis were conducted for the patients. Second, we investigated both hip and knee prosthesis in one study. However, the evaluation forms were used correspondingly and all the data were presented in separate groups.
Conclusion
Patients with PD who underwent TJA would result in excellent pain relief and gain of function. However, patients at late-stage PD may suffer from functional loss. The effectiveness of TJA in patients with severe PD remains concern. Physician should help delay the progression of PD which may optimize and stabilize the functional outcomes of TJA.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Kalia LV, Lang AE. Parkinson’s disease. Lancet (London, England). 2015;386(9996):896–912. https://doi.org/10.1016/s0140-6736(14)61393-3.
Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 2016;15(12):1257–72. https://doi.org/10.1016/s1474-4422(16)30230-7.
Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ. Osteoarthritis. Lancet (London, England). 2015;386(9991):376–87. https://doi.org/10.1016/s0140-6736(14)60802-3.
Allen NE, Schwarzel AK, Canning CG. Recurrent falls in Parkinson’s disease: a systematic review. Park Dis. 2013;2013:906274. https://doi.org/10.1155/2013/906274.
Walker RW, Chaplin A, Hancock RL, Rutherford R, Gray WK. Hip fractures in people with idiopathic Parkinson’s disease: incidence and outcomes. Mov Disord. 2013;28(3):334–40. https://doi.org/10.1002/mds.25297.
Bhattacharya RK, Dubinsky RM, Lai SM, Dubinsky H. Is there an increased risk of hip fracture in Parkinson’s disease? A nationwide inpatient sample. Mov Disord. 2012;27(11):1440–3. https://doi.org/10.1002/mds.25073.
Rana AQ, Qureshi AR, Akhter S, Ingar Y, Ayub A, Abdullah I, Madhosh O, Sarfraz Z, Rana MB, Rana R. Osteoarthritis increases paresthestic and akathisic pain, anxiety case-ness, and depression severity in patients with Parkinson’s disease. Front Neurol. 2018;9:409. https://doi.org/10.3389/fneur.2018.00409.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurol. 1967;17(5):427–42.
Zhao YJ, Wee HL, Chan YH, Seah SH, Au WL, Lau PN, Pica EC, Li SC, Luo N, Tan LC. Progression of Parkinson’s disease as evaluated by Hoehn and Yahr stage transition times. Mov Disord. 2010;25(6):710–6. https://doi.org/10.1002/mds.22875.
Hely MA, Morris JG, Traficante R, Reid WG, O’Sullivan DJ, Williamson PM. The Sydney multicentre study of Parkinson’s disease: progression and mortality at 10 years. J Neurol Neurosurg Psychiatry. 1999;67(3):300–7.
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG. The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord. 2008;23(6):837–44. https://doi.org/10.1002/mds.21956.
Kao CH, Chen CC, Wang SJ, Chia LG, Yeh SH. Bone mineral density in patients with Parkinson’s disease measured by dual photon absorptiometry. Nucl Med Commun. 1994;15(3):173–7.
Abou-Raya S, Helmii M, Abou-Raya A. Bone and mineral metabolism in older adults with Parkinson’s disease. Age Ageing. 2009;38(6):675–80. https://doi.org/10.1093/ageing/afp137.
Chaudhuri KR, Healy DG, Schapira AH. Non-motor symptoms of Parkinson’s disease: diagnosis and management. Lancet Neurol. 2006;5(3):235–45. https://doi.org/10.1016/s1474-4422(06)70373-8.
Marsh L. Depression and Parkinson’s disease: current knowledge. Curr Neurol Neurosci Rep. 2013;13(12):409. https://doi.org/10.1007/s11910-013-0409-5.
Rondon AJ, Tan TL, Schlitt PK, Greenky MR, Phillips JL, Purtill JJ. Total joint arthroplasty in patients with Parkinson’s disease: survivorship, outcomes, and reasons for failure. J Arthroplast. 2018;33(4):1028–32. https://doi.org/10.1016/j.arth.2017.11.017.
Mathew PG, Sponer P, Kucera T, Grinac M, Knizek J. Total HIP arthroplasty in patients with Parkinson’s disease. Acta Med (Hradec Kralove). 2013;56(3):110–6. https://doi.org/10.14712/18059694.2014.18.
Duffy GP, Trousdale RT. Total knee arthroplasty in patients with Parkinson’s disease. J Arthroplast. 1996;11(8):899–904. https://doi.org/10.1016/s0883-5403(96)80130-6.
Weber M, Cabanela ME, Sim FH, Frassica FJ, Harmsen WS. Total hip replacement in patients with Parkinson’s disease. Int Orthop. 2002;26(2):66–8. https://doi.org/10.1007/s00264-001-0308-2.
Price CC, Levy SA, Tanner J, Garvan C, Ward J, Akbar F, Bowers D, Rice M, Okun M. Orthopedic surgery and post-operative cognitive decline in idiopathic Parkinson’s disease: considerations from a pilot study. J Park Dis. 2015;5(4):893–905. https://doi.org/10.3233/jpd-150632.
Newman JM, Sodhi N, Dalton SE, Khlopas A, Newman RP, Higuera CA, Mont MA. Does Parkinson disease increase the risk of perioperative complications after total hip arthroplasty? A Nationwide Database Study. J Arthroplast. 2018;33(7s):S162–s166. https://doi.org/10.1016/j.arth.2018.01.006.
Kleiner JE, Gil JA, Eltorai AEM, Rubin LE, Daniels AH. Matched cohort analysis of peri-operative outcomes following total knee arthroplasty in patients with and without Parkinson’s disease. Knee. 2019;26(4):876–80. https://doi.org/10.1016/j.knee.2019.05.003.
Kleiner JE, Eltorai AEM, Rubin LE, Daniels AH. Matched cohort analysis of total hip arthroplasty in patients with and without Parkinson’s disease: complications, mortality, length of stay, and hospital charges. J Arthroplast. 2019;34(7s):S228–s231. https://doi.org/10.1016/j.arth.2019.03.023.
Newman JM, Sodhi N, Wilhelm AB, Khlopas A, Klika AK, Naziri Q, Kryzak TJ, Higuera CA, Mont MA. Parkinson’s disease increases the risk of perioperative complications after total knee arthroplasty: a nationwide database study. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2189–95. https://doi.org/10.1007/s00167-018-4970-y.
Shah NV, Solow M, Lavian JD, Bloom LR, Grieco PW, Stroud SG, Abraham R, Naziri Q, Paulino CB, Maheshwari AV, Diebo BG. Total hip arthroplasty in Parkinson’s disease patients: a propensity score-matched analysis with minimum 2-year surveillance. Hip Int, 1120700019862247. 2019. https://doi.org/10.1177/1120700019862247.
Wojtowicz AL, Mohaddes M, Odin D, Bulow E, Nemes S, Cnudde P. Is Parkinson’s disease associated with increased mortality, poorer outcomes scores, and revision risk after THA? Findings from the Swedish Hip Arthroplasty Register. Clin Orthop Relat Res. 2019;477(6):1347–55. https://doi.org/10.1097/corr.0000000000000679.
Jamsen E, Puolakka T, Peltola M, Eskelinen A, Lehto MU. Surgical outcomes of primary hip and knee replacements in patients with Parkinson’s disease: a nationwide registry-based case-controlled study. Bone Joint J. 2014;96-b(4):486–91. https://doi.org/10.1302/0301-620x.96b4.33422.
Erceg M, Maricevic A. Recurrent posterior dislocation following primary posterior-stabilized total knee arthroplasty. Croat Med J. 2000;41(2):207–9.
Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35(7):424–36. https://doi.org/10.2519/jospt.2005.35.7.424.
Meier W, Mizner RL, Marcus RL, Dibble LE, Peters C, Lastayo PC. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther. 2008;38(5):246–56. https://doi.org/10.2519/jospt.2008.2715.
Stevens-Lapsley J, Kluger BM, Schenkman M. Quadriceps muscle weakness, activation deficits, and fatigue with Parkinson disease. Neurorehabil Neural Repair. 2012;26(5):533–41. https://doi.org/10.1177/1545968311425925.
Lima LO, Scianni A, Rodrigues-de-Paula F. Progressive resistance exercise improves strength and physical performance in people with mild to moderate Parkinson’s disease: a systematic review. J Phys. 2013;59(1):7–13. https://doi.org/10.1016/s1836-9553(13)70141-3.
Ni M, Signorile JF, Balachandran A, Potiaumpai M. Power training induced change in bradykinesia and muscle power in Parkinson’s disease. Parkinsonism Relat Disord. 2016;23:37–44. https://doi.org/10.1016/j.parkreldis.2015.11.028.
Acknowledgements
We are thankful for the support of the nursing staffs from the Department of Orthopedic Surgery, West China Hospital, and the patients enrolled in this study.
Funding
This research was funded by the Science & Technology Department of Sichuan Province Program (2018SZ0135 and 2018SZ0255).
Author information
Authors and Affiliations
Contributions
ZY-L provided the ideas of this study. SD collected the data. XR analyzed the patient data. KZ and XY-Y helped with the interpretation of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rong, X., Dahal, S., Luo, Zy. et al. Functional outcomes after total joint arthroplasty are related to the severity of Parkinson’s disease: a mid-term follow-up. J Orthop Surg Res 14, 396 (2019). https://doi.org/10.1186/s13018-019-1447-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-019-1447-8