Abstract
Purpose
The purpose of this systematic review was to determine the effect of Parkinson’s disease (PD) on clinical outcomes and complications after total knee arthroplasty (TKA). Our systematic review was conducted to answer the following questions: (1) does TKA negatively affect clinical outcomes in patients with PD? and (2) does TKA cause more complications in patients with PD?
Methods
A rigorous and systematic approach was used, and each selected study was evaluated for methodological quality. Data on study design, total number of cases enrolled, follow-up duration, PD severity, clinical outcome, and complications after TKA were analyzed.
Results
Fourteen studies were included. Nine studies reported clinical scores. TKA significantly increased knee and functional scores in the PD group. However, compared with knee and functional scores in the non-PD group, the increase in scores in the PD group was not statistically significant, but tended to be less than that in the non-PD group. Eleven studies reported complications. In six studies, there was no difference in the complication rate between the PD and non-PD group or did not include a control group. In five studies, the PD group had higher medical complication rates and similar or higher surgical complication rates than the non-PD group.
Conclusions
Patients with PD who underwent TKA showed satisfactory functional improvement and pain reduction. However, these outcomes were not as good as those in the non-PD group. The PD group had a higher probability of occurrence of medical complications than the non-PD group. Further, the PD group had a similar or higher surgical complication rate than the non-PD group.
Similar content being viewed by others
Introduction
Total knee arthroplasty (TKA) is a common surgery for end-stage knee osteoarthritis (OA) treatment and can improve patients’ pain and function. In recent years, due to an increase in the life expectancy, many cases of TKA have been reported in elderly patients, which in turn has increased the number of patients with underlying diseases requiring TKA [1, 2]. Parkinson’s disease (PD) is a common underlying disease in elderly individuals. PD is the second most common neurodegenerative disease, with approximately 2% men and 1.3% women having a lifetime risk of PD [3]. The incidence of PD is low at a young age, but increases with age and is the highest at the age of 80 years [4].
PD is a neurodegenerative disease that exhibits characteristic clinical symptoms such as rigidity, bradykinesia, and reduced amplitude and automaticity of movement [5]. Gait impairment is a clinical manifestation of PD; its severity worsen with disease progresses [6]. Gait impairment is a problem that degrades quality of life. PD may also increase the risk of osteoporosis and falls [7]. Therefore, patients with PD and knee OA undergoing TKA may have poor outcomes.
Due to the characteristics of PD, patients undergoing TKA may have more postoperative complications and decreased functional outcomes. In addition, patients with PD have higher rates of mortality and medical comorbidity than normal patients [8]. Flexion contracture progresses as PD progresses, which adversely affects the outcome of TKA [9]. PD can also affect perioperative complications and patient satisfaction after TKA [10]. Moreover, TKA cannot prevent the progression of PD, because TKA improves only the mechanical problems of the knee. However, this does not mean that the patients are not conductive to pain reduction and functional improvement after surgery. Many studies have reported that TKA is helpful in improving the function and symptoms after the procedure.
In general, when selecting TKA as a treatment for knee OA, pain reduction, functional improvement, and complications after TKA are considered. PD can affect TKA outcomes, and several studies have reported the effect of PD on TKA. Many studies have compared and reported TKA outcomes in patients with PD, but the results are inconsistent, possibly due to the varying severity of PD and extent of complications reported in the study [11, 12]. Therefore, the purpose of this systematic review and meta-analysis was to determine the effect of PD on the clinical outcomes and complications after TKA. Our systematic review and meta-analysis was conducted to answer the following questions by analyzing studies that assessed TKA in patients with PD: (1) does TKA negatively affect clinical outcomes in patients with PD? and (2) does TKA cause more complications in patients with PD?
Materials and methods
Search strategy
To verify the research question, a rigorous and systematic approach conforming to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines was used [13]. In phase 1 of the PRISMA search process, selected databases were searched for eligible articles, including the MEDLINE, EMBASE, and Cochrane databases (30 December 2022). A Boolean strategy was used, and the field search terms included the following: (“primary total knee arthroplasty” or “total knee arthroplasty” or “primary total knee replacement” or “total knee replacement”) and (“Parkinson” or “Parkinson’s disease” or “Parkinson disease”). The citations in the included studies were screened, and unpolished articles were manually checked. The bibliographies of the relevant articles were subsequently cross-checked for articles not identified in the search. In phase 2, abstracts and titles were screened for relevance. In phase 3, the full text of the selected studies was reviewed according to the inclusion criteria, and methodological appropriateness was determined using a predetermined question. In phase 4, the studies were subjected to a systematic review process, if appropriate.
Eligibility criteria
Studies meeting the following criteria were included: (1) studies on TKA and PD, (2) articles written in English, (3) articles with full text available, and (4) articles including clinical outcomes or complications. The exclusion criteria were as follows: (1) studies not related to TKA, (2) studies published before 2000, (3) meta-analysis or systematic review articles, and (4) studies written in language other than English.
Data extraction
Each of the selected studies was evaluated for methodological quality by two independent authors. Data were extracted using the following standardized protocol: first author, publication year, publication journal, study type, number of cases, follow-up period, preoperative and postoperative clinical and functional scores, and complications. The extracted data were then cross-checked for accuracy, and any disagreements were resolved by a third author.
Quality assessment
The methodological quality of cohort studies or nonrandomized case–control studies was assessed using the Newcastle–Ottawa assessment scale [14]. This consists of three main domains (selection, comparability, and outcome), with four categories in the selection domain, one category in the comparability domain, and three categories in the outcome domain. A study was awarded a maximum of one or two stars for each item within the selection and outcome domains. A maximum of two stars was given for comparability. More stars indicated lower risk of bias.
Statistical analysis
Statistical analysis was performed for knee scores and functional scores using Stata version 14.2 static software. All the results are presented as forest plots. The 95% confidence interval (CI) was calculated for each effect size. The I2 statistic, which shows the percentage of total variation attributable to the heterogeneity among studies, was calculated, and values of < 25%, 50%, and > 75% were interpreted as small, moderate, and high levels of heterogeneity, respectively. A random effects model rather than a fixed effects model was used to calculate the effect size, as it was assumed that studies within each subgroup did not share a common effect size.
Results
Search
An initial electronic search yielded 193 articles. After excluding duplicate studies and applying the inclusion and exclusion criteria, 14 articles were included in the final analysis (Table 1). Some articles used registry data, some included retrospective cohorts, some enrolled prospective cohorts, and some were case–control studies. The PRISMA flowchart is shown in Fig. 1.
Quality
The quality assessment details are presented in Table 2. Twelve case–control studies and two cohort studies were assessed using the Newcastle–Ottawa assessment scale. Among the 12 case–control studies, six studies were awarded four stars, five studies were awarded three stars, and one study was awarded two stars of a possible four stars in the selection domain. In the comparability domain, all studies were awarded one star. In the outcome domain, five studies were awarded four stars, six studies were awarded three stars, and one study was awarded one star of a possible four stars. Both cohort studies showed a low risk of bias in all three domains. One was awarded five stars, and one was awarded three stars of a possible six stars in the selection domain. In the comparability domain, all studies were awarded one star. In the outcome domain, one study was awarded four stars and one study was awarded two stars of a possible five stars.
Clinical outcomes
Nine studies in this review reported on clinical outcomes of TKA in patients with PD (Table 3). Pooled analysis of clinical outcomes was performed for comparison before and after TKA in PD patients and before and after TKA between patients with and without PD (Figs. 2 and 3). The meta-analysis was performed using only studies that reported the mean value and standard deviation of the knee score results. TKA significantly increased knee and functional scores patients with PD (knee score 95% CI: 29.74 to 42.32, with high heterogeneity I2 = 91%, p < 0.00001, functional score 95% CI: 7.04 to 29.91, with high heterogeneity I2 = 100%, p = 0.002), However, compared with knee and functional scores in patients without PD, the increase in scores was not statistically significant in patients with PD, but improvement in patients with PD tended to be less than that in patients without PD (knee score 95% CI: −19.97 to 0.37, with high heterogeneity I2 = 84%, p = 0.06, functional score 95% CI: 33.24 to 1.62, with high heterogeneity I2 = 96%, p = 0.08).
Two of the included studies reported the results of TKA in patients with PD without a control group [12, 15]. Both studies showed statistically significant improvement in clinical score, pain reduction, and increased range of motion (ROM) after TKA in patients with PD. In another study, postoperative results were divided into a PD patient group and a non-PD patient group, and there was no difference in the Oxford knee score (OKS), ROM after TKA, and the degree of increase in OKS and ROM compared with preoperative values [16]. The remaining five studies compared the preoperative and postoperative clinical outcomes of the PD and non-PD groups. Two of these studies reported that the preoperative and postoperative clinical outcomes did not differ between the two groups [9, 11]. Another four studies reported worse clinical outcomes in the PD group than in the non-PD group after TKA [17,18,19,20].
Differences in clinical outcomes according to disease severity after TKA were reported in two studies [11, 12]. Xiao reported that patients with mild PD (Hoehn and Yahr stages I and II) showed better clinical symptom improvement after TKA than patients with severe PD [12]. However, Ergin et al. reported that in patients with high PD severity, the preoperative function was low, but the postoperative function was similar to patients with severe PD [11].
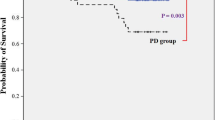
Complications
Among the studies, 11 studies reported postoperative complications (Table 4). Two studies reported only the complications that occurred in the PD group, which included gastrointestinal disorders, delirium, upper respiratory infection, confusion, and flexion contracture [12, 15]. In another two studies, complications such as infection, urinary retention, and deep vein thrombosis were reported in both groups [9, 16]. However, the number of complications was small, and comparisons were not made. In five studies, the probability of complication occurrence in the PD group was higher than in the non-PD group [1, 18, 19, 21, 22]. The remaining two studies reported no difference between the two groups [8, 23]. Newman et al. reported that delirium, mental status, pneumonia, urinary tract infection, and transfusion rates were higher in the PD group than in the non-PD groups, but there was no difference between the groups in terms of surgical complications [1]. Merchand et al. reported that medical complications, such as transfusion, anemia, cerebrovascular event, and thrombocytopenia, were 3.5 times higher and other implant-related complications, such as loosening and periprosthetic fracture, were 1.6 times higher in the PD group than in the non-PD group [21].
For detailed complications, the infection rate was reported in five studies [1, 8, 19, 21, 22]. Three registry-based studies reported no difference in infection rate [1, 8, 22]. However, one case–control study and one registry-based study reported that the infection rate was higher in the PD group than in the non-PD group [19, 21]. For aseptic loosening, there was no difference between groups in the study by Rodon, but Merchand reported higher aseptic loosening in the PD group than in the non-PD group. Mortality was reported in three studies [8, 22, 23]. Jämsen et al. reported that the mortality in the PD group was 1.94 times higher than that in the non-PD group at the 10-year follow-up, but Kleiner et al. and Cheppalli et al. reported that there was no difference in mortality between the groups.
Discussion
The purpose of this systematic review and meta-analysis was to determine the effect of PD on clinical outcomes and complications after TKA. Based on the included studies, the principal findings were as follows: (1) TKA significant improved clinical symptoms in patients with PD and (2) the probability of complications, but not fatal complications, is high in patients with PD after TKA.
Due to the increase in life expectancy, the number of patients with underlying diseases requiring TKA has increased. Moreover, PD is an increasingly common disease in elderly individuals, and it is a disease that lowers the quality of life of patients with gait disorders. It is thought that the outcome of TKA is inevitably affected by PD due to the natural progression of the disease. We believe that PD adversely affects TKA outcomes. However, if the clinical outcomes can be improved significantly, we believe that TKA can be a good treatment for OA with PD, even if the degree of improvement in clinical outcomes is less than that in patients without PD. In this study, most of the included studies showed improved clinical scores in patients with PD after TKA. In addition, four out of six studies showed that the outcomes of TKA were similar between patients with and without PD patients; therefore, the degree of improvement cannot be considered low [9, 11, 16, 18]. Further, the effects of TKA are considered to be different depending on the severity of PD. Two studies compared the clinical outcomes according to PD severity. However, one study reported that there was no difference in clinical outcome according to PD severity, [11] and another study reported that patients with high PD severity had poor outcomes [12]; therefore, this study could not conclude on the effect of PD severity on the clinical outcomes of TKA. In addition, a direct comparison between studies was not possible because the indicators that suggested PD severity in each study were different (Charlson Comorbidity index, Hoehn and Yahr stage, and Elixhauser Comorbidity index).
For medical and surgical complications that may occur after TKA, the definition and inclusion of complications were different for each study, and the probability of complications was also low; therefore, the two groups could not be statistically compared. In four studies included in the analysis, only the types of complications that occurred were presented, but no comparison was made between the two groups [9, 12, 15, 16]. In a registry-based cohort study involving a large number of patients, the risk of medical complications was reported differently [1, 21]. As mentioned above, different risk is thought to be due to the difference in the exact inclusion criteria of the included complications and the difference in the included complications. The probability of pneumonia, transfusion rate, mental status change, and urinary tract infection were high in patients with PD. However, considering that there was no difference in short-term mortality after surgery between the groups, there was no difference in life-threatening medical complications [8, 23].
Regarding surgical complications, the most common concerns are infection rate, aseptic loosening, and revision rate. A small-scale study reported that the probability of infection and loosening was statistically high in patients with PD, but only occurred in < 3–9 cases. [19] In a registry-based cohort study involving a large number of patients, Newman and Merchand’s studies, different opinions were presented on infection and loosening [1, 21]. However, in a study by Merchant, while the probability of surgical complications was high, that there was no difference in the revision rate [21]. Considering this, there seems to be no difference in severe surgical complications requiring revision. This conclusion is consistent with that of a previous meta-analysis on total joint arthroplasty [24].
Our analysis evaluated the effect of PD on TKA outcomes. This study included only patients with or without PD undergoing TKA. In a previous study, total joint arthroplasty in patient with PD was evaluated [24]; however, there was no systematic review or meta-analysis about patients undergoing only TKA. This is considered a strength of this study because there may be differences in results for each arthroplasty. The limitations of this study should also be considered. First, the number of patients was not large in most studies that reported clinical results. In addition, there were differences in the follow-up period. Second, there was no detailed report on the outcome of TKA according to PD severity, and although it affects the TKA outcome, PD severity could not be analyzed. This should be analyzed in future studies. Third, no studies considered the natural progression of PD. In other words, PD itself can cause various medical diseases and reduce the quality of life, and it is necessary to consider them for accurate results. Fourth, other related diseases, rather than PD itself, may have been a confounding factor. Although many of the included studies performed propensity matching for controlling confounding factors, this study itself could not consider the confounding factor due to the nature of systematic review.
Conclusions
Patients with PD had satisfactory functional improvement and pain reduction after TKA. However, these outcomes were not as good as those in the non-PD group. The PD group had a higher occurrence rate of medical complications than the non-PD group. Further, the PD group had a similar or higher surgical complication rate than the non-PD group.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PD:
-
Parkinson’s disease
- TKA:
-
Total knee arthroplasty
- ROM:
-
Range of motion
- OKS:
-
Oxford knee score
References
Newman JM, Sodhi N, Wilhelm AB, Khlopas A, Klika AK, Naziri Q, Kryzak TJ, Higuera CA, Mont MA (2019) Parkinson’s disease increases the risk of perioperative complications after total knee arthroplasty: a nationwide database study. Knee Surg Sports Traumatol Arthrosc 27(7):2189–2195
Oni OO, Mackenney RP (1985) Total knee replacement in patients with Parkinson’s disease. J Bone Joint Surg Br 67(3):424–425
Elbaz A, Bower JH, Maraganore DM, McDonnell SK, Peterson BJ, Ahlskog JE, Schaid DJ, Rocca WA (2002) Risk tables for parkinsonism and Parkinson’s disease. J Clin Epidemiol 55(1):25–31
Taylor KS, Cook JA, Counsell CE (2007) Heterogeneity in male to female risk for Parkinson’s disease. J Neurol Neurosurg Psychiatry 78(8):905–906
Samii A, Nutt JG, Ransom BR (2004) Parkinson’s disease. Lancet 363(9423):1783–1793
Mirelman A, Bonato P, Camicioli R, Ellis TD, Giladi N, Hamilton JL, Hass CJ, Hausdorff JM, Pelosin E, Almeida QJ (2019) Gait impairments in Parkinson’s disease. Lancet Neurol 18(7):697–708
Lethbridge L, Johnston GM, Turnbull G (2013) Co-morbidities of persons dying of Parkinson’s disease. Prog Palliat Care 21(3):140–145
Jämsen E, Puolakka T, Peltola M, Eskelinen A, Lehto MU (2014) Surgical outcomes of primary hip and knee replacements in patients with Parkinson’s disease: a nationwide registry-based case-controlled study. Bone Joint J 96(4):486–491
Tinning CG, Cochrane LA, Singer BR (2013) Primary total knee arthroplasty in patients with Parkinson’s disease: analysis of outcomes. Acta Orthop Belg 79(3):301–306
Marchand KB, Vakharia R, Sodhi N, Anis H, Salem HS, Scuderi GR, Mont MA, Roche MW (2022) Impact of Parkinson’s disease on complications, readmission rates, and costs of care following primary total knee arthroplasty. J Knee Surg 35(1):21–25
Ergin ÖN, Karademir G, Şahin K, Meriç E, Akgül T, Öztürk İ (2020) Functional outcomes of total knee arthroplasty in patients with Parkinson’s disease: A case control study. J Orthop Sci 25(3):487–491
Rong X, Dahal S, Luo ZY, Zhou K, Yao SY, Zhou ZK (2019) Functional outcomes after total joint arthroplasty are related to the severity of Parkinson’s disease: a mid-term follow-up. J Orthop Surg Res 14(1):396
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Montiel Terrón V, Vitoria M (2020) Do we really improve life quality after total knee arthroplasty in patients with Parkinson’s disease? Arch Orthop Trauma Surg 56:78
Wong EH, Oh LJ, Parker DA (2018) Outcomes of primary total knee arthroplasty in patients with Parkinson’s disease. J Arthroplasty 33(6):1745–1748
Baek JH, Nam CH, Lee SC, Ahn HS, Ha YC (2021) Poor outcomes of primary total knee arthroplasty in patients with Parkinson’s disease. Int Orthop 56:34
Goh GS, Zeng GJ, Tay DK, Lo NN, Yeo SJ, Liow MHL (2020) Patients With Parkinson’s disease have poorer function and more flexion contractures after total knee arthroplasty. J Arthroplasty 5:34
Rondon AJ, Tan TL, Schlitt PK, Greenky MR, Phillips JL, Purtill JJ (2018) Total joint arthroplasty in patients with Parkinson’s disease: survivorship, outcomes, and reasons for failure. J Arthroplasty 33(4):1028–1032
Zong Y, Hao C, Zhang Y, Wu S (2022) Quality of life assessment after total knee arthroplasty in patients with Parkinson’s disease. BMC Musculoskelet Disord 23(1):230
Marchand KB, Vakharia R, Sodhi N, Anis H, Salem HS, Scuderi GR, Mont MA, Roche MW (2020) Impact of Parkinson’s disease on complications, readmission rates, and costs of care following primary total knee arthroplasty. J Knee Surg 35:21
Cheppalli NS, Senthil T, Sakthivelnathan V, Menedal A, Mounasamy V, Sambandam S (2022) Complications during the hospital stay, length of stay, and cost of care in Parkinson patients undergoing total knee arthroplasty: a propensity matched database study. J Am Acad Orthop Surg Glob Res Rev 6:7
Kleiner JE, Gil JA, Eltorai AEM, Rubin LE, Daniels AH (2019) Matched cohort analysis of peri-operative outcomes following total knee arthroplasty in patients with and without Parkinson’s disease. Knee 26(4):876–880
Min H, Lin H, Chen G (2019) Effect of Parkinson’s disease on primary total joint arthroplasty outcomes: a meta-analysis of matched control studies. Int J Surg 71:124–131
Acknowledgements
Not applicable.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
S.H.L. and J.R.Y. designed this paper and performed critical revision of the manuscript. S.H.L. coordinated the clinical study and T.H.Y. initiated and performed the study, analyzed the data, and wrote the manuscript. S.H.L. and J.R.Y. helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. This is a review article and Institutional review board approval was waived.
Consent for publication
All presented cases in this report had written consents for publication.
Competing interests
The authors declare that we have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yoon, JR., Yoon, TH. & Lee, S.H. The effect of Parkinson’s disease on total knee arthroplasty: a systematic review and meta-analysis. Knee Surg & Relat Res 35, 6 (2023). https://doi.org/10.1186/s43019-023-00179-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-023-00179-1