Abstract
Background
Bracing can effectively treat adolescent idiopathic scoliosis (AIS), but patient outcomes have not been compared by brace type. We compared outcomes of AIS patients treated with Rigo Chêneau orthoses (RCOs) or custom-molded Boston-style thoracolumbosacral orthoses (TLSOs).
Methods
We retrospectively reviewed patient records from one scoliosis center from 1999 through 2014. Patients were studied from initial treatment until skeletal maturity or surgery. Inclusion criteria were a diagnosis of AIS, initial major curve between 25° and 40°, use of an RCO or TLSO, and no previous scoliosis treatment.
Results
The study included 108 patients (93 girls) with a mean (±standard deviation) age at brace initiation of 12.5 ± 1.3 years. Thirteen patients wore an RCO, and 95 wore a TLSO. Mean pre-bracing major curves were 32.7° ± 4.8° in the RCO group and 31.4° ± 4.4° in the TLSO group (p = 0.387). Mean brace wear time was similar between groups. Mean differences in major curve from baseline to follow-up were −0.4° ± 9.9° in the RCO group and 6.9° ± 12.1° in the TLSO group (p = 0.028). Percent changes in major curve from baseline to follow-up were 0.0% ± 30.5% for the RCO group and 21.3% ± 38.8% for the TLSO group (p = 0.030). No RCO patients and 34% of TLSO patients progressed to spinal surgery (p = 0.019). At follow-up, major curves improved by 6° or more in 31% of the RCO group and 13% of the TLSO group (p = 0.100).
Conclusions
Patients treated with RCOs compared with Boston-style TLSOs had similar baseline characteristics and brace wear time yet significantly lower rates of spinal surgery. Patients with RCOs also had lower mean and percent major curve progression versus those with TLSOs.
Similar content being viewed by others
Background
Adolescent idiopathic scoliosis (AIS) affects 2 to 3% of adolescents between the ages of 10 and 18 years [1, 2]. Brace treatment is commonly offered when the spinal curve has reached 25° [3]. Since the Bracing in Adolescent Idiopathic Scoliosis Trial study in 2013 [4], bracing has been increasingly recognized as an effective nonsurgical means of scoliosis treatment. However, the comparative effectiveness of most types of braces for AIS has not been definitively established [5].
A rigid thoracolumbosacral orthosis (TLSO) is a brace worn to minimize progression of AIS. There are various TLSO designs (e.g., Boston, Milwaukee, Wilmington) [6]. Rigo Chêneau orthoses (RCOs) were developed approximately two decades ago, with the intent to combine biomechanical forces in three dimensions, including curve derotation. They use an open pelvis design with anterior opening. However, studies of the RCO are limited, and we know little about its effectiveness, particularly in relation to other braces [5, 7, 8].
In the current study, we reviewed records of patients treated at one large academic medical center’s pediatric orthopedic scoliosis practice who were prescribed full-time bracing for AIS. Our objective was to determine if brace type, specifically the RCO compared with a Boston-style TLSO, affected outcomes. Our hypothesis was that different brace designs would lead to different patient outcomes.
Methods
Study population
We retrospectively reviewed medical records of patients treated at an academic scoliosis center from 1999 through 2014. The study population consisted of adolescents aged 10 years or older at presentation who met the following criteria: (1) diagnosis of AIS; (2) Risser stage between 0 and 2; (3) major curve between 25° and 40°; (3) no previous treatment for scoliosis; (4) if female, premenarchal or less than 1 year postmenarchal; (5) prescribed full-time brace treatment; and (6) follow-up until skeletal maturity or surgery.
Measurements
Outcome variables followed the recommendations of the Scoliosis Research Society (SRS) Committee on Bracing and Nonoperative Management and the Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) and incorporated other relevant clinical outcomes [9, 10]. Outcomes included the following: major curve exceeding 30° and major curve exceeding 50°, difference in major curve from baseline to follow-up, percent change in major curve, progression to spinal surgery, progression of curve to 45° or more after bracing, progression to spinal surgery or curve of at least 45° after bracing, major curve progression of 6° or more, major curve improvement of 6° or more, and major curve unchanged (within 5°). For the outcomes that included progression to curvature of 45° or more, we measured the patients whose major curve progressed to at least 45°.
Our primary independent variable was the type of brace. We compared an RCO with a custom Boston-style TLSO. Patients self-selected their orthotists and brace type. Follow-up orthopedist recommendations were the same for all patients: in-brace radiography and clinic visit 4 weeks after treatment initiation, then out-of-brace radiography and clinic visits every 4 months before menarche and every 6 months after menarche. We abstracted information on age, sex, race, curve location, pre-bracing initial major curve magnitude, pre-bracing Risser stage, initial in-brace major curve, time in brace, and mean patient-reported number of hours the brace was worn in Risser stages 0 and 1 and overall. We recorded information for the total course of treatment for each patient and calculated the mean brace wear time for the course of treatment.
We performed univariate and bivariate descriptive analyses, including Student t tests, Fisher exact tests, and χ 2 tests, comparing baseline characteristics and outcomes. A two-sided alpha with p < 0.05 was considered statistically significant.
Results
Baseline characteristics
Of the 108 patients (93 girls) who met the inclusion criteria, the mean age at treatment initiation was 12.5 ± 1.3 years (Table 1). Ninety-five patients were treated with a TLSO, and 13 patients were treated with an RCO. Of the study population, 72% were Caucasian and 15% were African American. Major curves were mainly thoracic (47%), lumbar (22%), or thoracic and thoracolumbar (18%). The mean pre-brace major curves were 31.6° ± 4.4° overall, 32.7° ± 4.8° in the RCO group, and 31.4° ± 4.4° in the TLSO group, corresponding to 52% of patients having an initial pre-brace major curve of more than 30°. Sixty-three percent of patients began bracing at Risser stage 0, 22% at Risser stage 1, and 15% at Risser stage 2. Demographic and clinical characteristics at baseline were similar for patients in both groups.
Treatment and outcomes
We followed all patients until skeletal maturity or progression to surgery, whichever came first. Mean initial in-brace major curves were 22.6° ± 6.4° in the RCO group and 22.6° ± 7.2° in the TLSO group (p = 0.924) (Table 2). In-brace correction of major curve from baseline of at least 35% was achieved in 42% of the RCO group and 36% of the TLSO group (p = 0.943, data not shown). Patients in the RCO group wore the brace for a mean 17.0 ± 6.1 h per day, and patients in the TLSO group wore the brace for a mean 16.1 ± 5.2 h per day (p = 0.641).
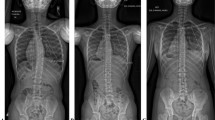
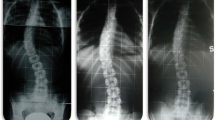
After bracing was complete, the mean final measurements for major curves were 32.3° ± 10.4° (RCO group) and 38.3° ± 13.5° (TLSO group) (p = 0.077) (Table 2). Forty-six percent of RCO patients had a major curve at follow-up of greater than 30°, compared with 67% of TLSO patients (p = 0.133). The mean difference in major curves from baseline to follow-up was −0.4° ± 9.9° for the RCO group versus 6.9° ± 12.1° for the TLSO group (p = 0.028). Figure 1 shows each patient’s change in major curve magnitude from baseline to follow-up. The percent changes in major curves from baseline to follow-up were 0.0% ± 30.5% for the RCO group and 21.3% ± 38.8% for the TLSO group (p = 0.030) (Table 2). No patients in the RCO group progressed to surgery, compared with 32 patients in the TLSO group (p = 0.019). Fifteen percent of patients in the RCO group had a final major curve of 45° or greater or progressed to spinal surgery, compared with 38% of patients in the TLSO group (p = 0.133). At follow-up, major curves improved by 6° or more in 31% of the RCO group and 13% of the TLSO group (p = 0.100).
Discussion
In this retrospective review of a large academic medical center’s patients with AIS and their experience with full-time brace treatment, we found that patients treated with RCOs were substantially less likely to progress to spinal surgery and had smaller mean change and smaller percent increase in major curves from treatment initiation through follow-up than patients treated with a TLSO, despite similar baseline characteristics and brace wear time. The outcomes of curve progression less than 45° or progression to surgery and major curve improvement of at least 6° were not statistically different; however, they appeared to favor RCOs. Although previous studies have shown the benefits of bracing [4,12,, 11–13] and the benefits of the RCO for treatment of AIS [7, 8], none has compared efficacy of the RCO with other orthoses. For this study, we incorporated guidelines from the SRS Bracing Committee and SOSORT to establish our inclusion criteria [10] and tracked patients from early Risser stages until maturity or surgery to understand the effects of brace type, specifically RCO versus TLSO, on outcomes.
We consider our outcomes for brace treatment in relation to previous studies’ findings. In the Bracing in Adolescent Idiopathic Scoliosis Trial study, 72% of those with TLSO bracing had curve progression to less than 50° [4]. Similarly, our study showed that 68% of patients with TLSO bracing had major curve progression to less than 45° [4]. Previous studies, mostly using Milwaukee TLSO braces, have shown a large spectrum of success rates for a range of curve outcomes, likely because of dissimilarity in brace quality, patient characteristics, and decision thresholds for spinal surgery [14,15,16,17,18]. Most of these studies took place before SRS and SOSORT guidelines on reporting; thus, standards of outcome measurement and participant selection varied [10].
Little research has been published on outcomes for RCOs. Zaborowska-Sapeta et al. [8] reported on 79 patients with RCOs in Poland. In their study, 12.9% of patients progressed to a major curve greater than 50° at final follow-up, with a mean major curve increase of 9.2° for the overall study population [8]. Although we used the SRS-recommended outcome of 45°, our results are comparable to those of Zaborowska-Sapeta et al. [8]. However, our population had a lower mean change in major curve from baseline to follow-up with the RCO. Ovadia et al. [7] published the results of 93 patients in Israel treated with RCOs and found that 84% of patients’ curves progressed by less than 5°. Although we studied a smaller number of patients with RCOs than these two international reports, our study is an important addition to the research because it is one of the first to compare outcomes after RCO use versus general Boston-style TLSO bracing.
Several factors could have contributed to the favorable outcomes for RCOs compared with TLSOs in our study. First, the RCO construction with three-dimensional corrective forces may have a better effect on scoliosis curves compared with the TLSO. Second, the lighter weight of the RCO and more open design may have made it more desirable and comfortable for patients to wear, leading to increased compliance. However, we did not observe a difference in patient-reported mean wear time between brace types during the course of follow-up. Third, because this was an observational study of clinical practice, families had a choice of orthotists and orthoses. Although we did not measure how families made these decisions, we believe variation in geographical distance to orthotists and heterogeneity of insurance coverage for orthoses could have influenced the type of brace adolescents received. In addition, families who chose the RCOs could have had other factors that made their adolescents more likely to have successful bracing outcomes.
This study has limitations. Despite the large number of records encompassing 15 years of a busy, academic scoliosis clinical practice, we had a relatively small sample of patients using RCOs compared with the two international reports, and this may have limited our ability to detect statistically significant differences in some measures [7, 8]. RCO braces were principally made by one skilled orthotist in the region, which contributed to their lower frequency. Despite this, the relative comparability of our outcomes with previous TLSO and RCO studies provides face validity. In addition, this was a retrospective review of an outpatient clinical practice, and we did not have quality-of-life measures, objective monitoring of time wearing the brace, or blinded, independent outcome assessment. Although self-reports tend to overestimate brace wear time [19], it is unlikely that reported wear time would differ systematically between patients with TLSOs and RCOs in this review of a real-world clinical practice.
Another potential limitation was that although the percent initial in-brace major curve correction appeared to be better in RCOs compared with TLSOs, the difference was not statistically significant, as we may have expected given the positive RCO outcomes at the end of treatment. This could have been caused in part by the smaller number of RCOs and by the fact that if the initial correction was not clinically acceptable to the orthopedist, he would recommend the patient return for brace adjustments to achieve optimal correction. Further, in-brace radiography was generally not performed. Thus, the 1-month in-brace measurements presented here may underestimate actual in-brace correction, particularly for RCOs. In addition, the in-brace measured curve correction reflects coronal changes only, not rotational changes, which could not be studied. However, on clinical assessment such as out-of-brace examination of forward bending, the orthopedist noticed that rotational prominence often diminished in RCO-treated patients. The RCO’s influence on curve derotation may be particularly important for its effectiveness in treating scoliosis; however, future research is needed to elucidate how this mechanism contributes to bracing success [7].
There are several strengths of our report. We followed guidelines for patient inclusion and choice of clinical outcome variables [9, 10]. Our results provide a real-world comparison of patient experience with brace types in a large outpatient scoliosis practice. This use of SRS and SOSORT criteria to compare outcomes by brace type is rare in prior studies. Moreover, the similar clinical characteristics at baseline allow an assessment of differences between brace types, despite a relatively small sample size for the RCO group.
Conclusions
In this large retrospective review of an academic outpatient scoliosis practice, patients treated with RCOs were substantially less likely to progress to spinal surgery than those treated with Boston-style TLSOs. Patients treated with RCOs also had smaller mean change and smaller percent increase in major curves from treatment initiation through follow-up. Future studies should examine differences in outcomes by brace type in other settings and in larger samples, and they should investigate the impact of the rotational dimension of correction with RCOs. Clinicians may consider increasing use of RCOs for AIS.
Abbreviations
- AIS:
-
Adolescent idiopathic scoliosis
- RCO:
-
Rigo Chêneau orthosis
- SOSORT:
-
Society on Scoliosis Orthopaedic and Rehabilitation Treatment
- SRS:
-
Scoliosis Research Society
- TLSO:
-
Thoracolumbosacral orthosis
References
Nachemson A, Lonstein J, Weinstein S. Report of the SRS Prevalence and Natural History Committee 1982. Presented at the Scoliosis Research Society 17th Annual Meeting, Denver, CO, September 22-25, 1982.
Weinstein SL, Dolan LA, Cheng JCY, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371(9623):1527–37.
Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect. 2005;54:529–36.
Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369(16):1512–21.
Negrini S, Aulisa AG, Aulisa L, Circo AB, de Mauroy JC, Durmala J, Grivas TB, Knott P, Kotwicki T, Maruyama T, Minozzi S, O’Brien JP, Papadopoulos D, Rigo M, Rivard CH, Romano M, Wynne JH, Villagrasa M, Weiss HR, Zaina F. 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. 2012;7(1):3.
Zaina F, De Mauroy JC, Grivas T, Hresko MT, Kotwizki T, Maruyama T, Price N, Rigo M, Stikeleather L, Wynne J, Negrini S. Bracing for scoliosis in 2014: state of the art. Eur J Phys Rehabil Med. 2014;50(1):93–110.
Ovadia D, Eylon S, Mashiah A, Wientroub S, Lebel ED. Factors associated with the success of the Rigo System Chêneau brace in treating mild to moderate adolescent idiopathic scoliosis. J Child Orthop. 2012;6(4):327–31.
Zaborowska-Sapeta K, Kowalski IM, Kotwicki T, Protasiewicz-Faldowska H, Kiebzak W. Effectiveness of Chêneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis. 2011;6(1):2.
Negrini S, Hresko TM, O’Brien JP, Price N, Boards S, Committee SRSN-O. Recommendations for research studies on treatment of idiopathic scoliosis: consensus 2014 between SOSORT and SRS non-operative management committee. Scoliosis. 2015;10:8.
Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies. SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976). 2005;30(18):2068–75.
Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92(6):1343–52.
Nachemson AL, Peterson LE, members of The Brace Study Group of the Scoliosis Research Society. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77(6):815-822.
Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am. 1997;79(5):664–74.
Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis. A follow-up mean of 16 years after maturity. Spine (Phila Pa 1976). 2007;32(20):2198–207.
Fernandez-Feliberti R, Flynn J, Ramirez N, Trautmann M, Alegria M. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop. 1995;15(2):176–81.
Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine (Phila Pa 1976). 2001;26(1):42–7.
Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76(8):1207–21.
Noonan KJ, Weinstein SL, Jacobson WC, Dolan LA. Use of the Milwaukee brace for progressive idiopathic scoliosis. J Bone Joint Surg (Br). 1996;78(4):557–67.
Morton A, Riddle R, Buchanan R, Katz D, Birch J. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2008;28(3):336–41.
Acknowledgements
Not applicable.
Funding
Not applicable. There was no funding for this study.
Availability of data and materials
The data that support the findings of this study could be available on request from the corresponding author after additional human subject research approval is obtained. The data are not publicly available because of information that could compromise research participant privacy.
Authors’ contributions
MKM designed the data abstraction, abstracted the data from the records, performed the analyses, and drafted the manuscript. KDV was a major contributor in the data abstraction design and participated in writing the manuscript. GLD contributed to the analyses, interpretation of the data, and editing the manuscript. PDS designed the study and was a major contributor to the interpretation of the data and editing the manuscript. All authors provided approval of the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The Office of Human Subjects Research institutional review boards at The Johns Hopkins University School of Medicine approved this retrospective study and waived informed consent (protocol 00070565).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Minsk, M.K., Venuti, K.D., Daumit, G.L. et al. Effectiveness of the Rigo Chêneau versus Boston-style orthoses for adolescent idiopathic scoliosis: a retrospective study. Scoliosis 12, 7 (2017). https://doi.org/10.1186/s13013-017-0117-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13013-017-0117-z