Abstract
Purpose
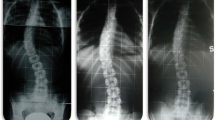
This study evaluated whether early brace treatment of curves < 25° decreased the prevalence of curve progression and surgery.
Methods
In a retrospective review, patients with idiopathic scoliosis Risser stages 0 to 2 braced at < 25° were followed until brace discontinuation, skeletal maturity, or surgery. Patients with predominantly primary thoracolumbar/lumbar curves were prescribed nighttime braces (NTB) and thoracic curves were prescribed fulltime braces (FTB). Comparisons were made for TLSO type (NTB vs. FTB) and triradiate cartilage (TRC) status (open vs. closed) at brace prescription.
Results
283 patients were included, 81% who were Risser stage 0 with curves averaging 21.8° ± 2.1° at brace prescription. The average curve change was 2.4° ± 11.2°. Curves improved ≥ 6° in 23% of patients. Patients who were not skeletally mature at brace discontinuation (n = 39) had lower Cobb angles (16.7° vs. 23.9°, p < 0.001), better curve improvement (− 4.7° vs. 2.1°, p < 0.001), and were braced for a shorter period of time (1.8 years vs. 2.3 years, p = 0.011) than those who were skeletally mature at brace discontinuation (n = 239). Only 7% of patients in NTB and 8% of patients in FTB with open TRC required surgery. The numbers needed to treat to prevent surgery in patients in FTB with open TRC was calculated to be 4.
Conclusion
Early brace treatment (Cobb < 25° and open TRC) may not only reduce curve progression and the need for surgical treatment but may also result in curve improvement, thus challenging the paradigm that the goal of bracing is merely to stop curve progression.
Level of evidence
3–retrospective cohort study.

Similar content being viewed by others
Data availability
Data can be made available in a de-identified manner upon request.
References
Zapata KA, Sucato DJ, Lee MC et al (2019) Skeletally immature patients with adolescent idiopathic scoliosis curves 15°–24° are at high risk for progression. Spine Deform 7(6):870–874. https://doi.org/10.1016/j.jspd.2019.02.012
Lonstein JE, Carlson JM (1982) The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am 66:1061e71
Richards BS, Bernstein RM, D’Amato CR et al (2005) Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS committee on bracing and nonoperative management. Spine (Phila Pa 1976) 30(18):2068–2075. https://doi.org/10.1097/01.brs.0000178819.90239.d0
Karol LA, Virostek D, Felton K et al (2016) The effect of the risser stage on bracing outcome in adolescent idiopathic scoliosis. J Bone Joint Surg Am 98:1253–1259. https://doi.org/10.2106/JBJS.15.01313
Khoshbin A, Caspi L, Law PW et al (2015) Outcomes of bracing in juvenile idiopathic scoliosis until skeletal maturity or surgery. Spine (Phila Pa 1976) 40(1):50–55. https://doi.org/10.1097/BRS.0000000000000669
Roye BD, Simhon ME, Matsumoto H et al (2020) Establishing consensus on the best practice guidelines for the use of bracing in adolescent idiopathic scoliosis. Spine Deform 8(4):597–604. https://doi.org/10.1007/s43390-020-00060-1
Weinstein SL, Dolan LA, Wright JG et al (2013) Effects of bracing in adolescents with idiopathic scoliosis. N Eng J Med 369(16):1512–1521. https://doi.org/10.1056/NEJMoa1307337
Simony A, Beuschau I, Quisth L et al (2019) Providence nighttime bracing is effective in treatment for adolescent idiopathic scoliosis even in curves larger than 35°. Eur Spine J 28(9):2020–2024. https://doi.org/10.1007/s00586-019-06077-z
Wiemann JM, Shah SA, Price CT (2014) Nighttime bracing versus observation for early adolescent idiopathic scoliosis. J Pediatr Orthop 34(6):603–606. https://doi.org/10.1097/BPO.0000000000000221
Dolan LA, Weinstein SL, Abel MF et al (2019) Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST): development and validation of a prognostic model in untreated adolescent idiopathic scoliosis using the simplified skeletal maturity system. Spine Deform 7(6):890-898.e4. https://doi.org/10.1016/j.jspd.2019.01.011
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Deviren V, Berven S, Kleinstueck F et al (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine 27(21):2346–2369. https://doi.org/10.1097/00007632-200211010-00007
Grivas TB, Vasiliadis ES, Rodopoulos G et al (2008) The role of the intervertebral disc in correction of scoliotic curves. A theoretical model of idiopathic scoliosis pathogenesis. Stud Health Technol Inform 140:33–36
Negrini S, Donzelli S, Aulisa AG et al (2018) 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. https://doi.org/10.1186/s13013-017-0145-8
Weinstein SL (2019) The natural history of untreated adolescent idiopathic scoliosis. J Pediatr Orthop 39(6):S44–S46. https://doi.org/10.1097/BPO.0000000000001350
Ohashi M, Watanabe K, Hirano T et al (2018) Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves. Spine (Phila Pa 1976) 43(23):E1403–E1411. https://doi.org/10.1097/BRS.0000000000002716
Ohashi M, Watanabe K, Hirano T et al (2022) Impact of the flexibility of the spinal deformity on low back pain and disc degeneration in adult patients nonoperatively treated for adolescent idiopathic scoliosis with thoracolumbar or lumbar curves. Spine Deform 10(1):133–140. https://doi.org/10.1007/s43390-021-00402-7
Karol LA, Virostek D, Felton K et al (2016) Effect of compliance counseling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am 98:9–14. https://doi.org/10.2106/JBJS.O.00359
Negrini S, Di Felice F, Negrini F et al (2022) Predicting final results of brace treatment of adolescents with idiopathic scoliosis: first out-of-brace radiograph is better than in-brace radiograph—SOSORT 2020 award winner. Eur Spine J 31(12):3519–3526. https://doi.org/10.1007/s00586-022-07165-3
Negrini S, Donzelli S, Lusini M et al (2014) The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis based on SRS and SOSORT criteria: a prospective study. BMC Musculoskelet Disord 15(1):263. https://doi.org/10.1186/1471-2474-15-263
Sanders JO, Newton PO, Browne RH et al (2014) Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am 96:649–653. https://doi.org/10.2106/JBJS.M.00290
Shi B, Guo J, Mao S et al (2016) Curve progression in adolescent idiopathic scoliosis with a minimum of 2 years’ follow-up after completed brace weaning with reference to the SRS standardized criteria. Spine Deform 4(3):200–205. https://doi.org/10.1016/j.jspd.2015.12.002
Cheung PWH, Cheung JPY (2021) Sanders stage 7b: using the appearance of the ulnar physis improves decision-making for brace weaning in patients with adolescent idiopathic scoliosis. Bone Joint J 103-B(1):141–147. https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-1240.R1
Acknowledgements
The authors would like to acknowledge Rebecca Dieckmann for assisting with data collection.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
KZ: KZ made substantial contributions to the conception and design of the work and data acquisition, KZ drafted the work and revised the work, approved the version to be published, agree to be accountable for all aspects of the work. DV: DV made substantial contributions to data acquisition and interpretation, DV revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work. KD: KD made substantial contributions to data acquisition and interpretation, KD revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work. MJ: MJ made substantial contributions to data interpretation, MJ revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work. C-HJ: CJ made substantial contributions to the analysis of the data, CJ revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work. MO: MO made substantial contributions to data acquisition, MO revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work. DS: DS made substantial contributions to the study design and interpretation of the data, DS drafted and revised the work critically for important intellectual content, approved the version to be published, agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
IRB approval was received from Scottish Rite for Children and from University of Texas Southwestern.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zapata, K.A., Virostek, D., Davis, K. et al. Early brace treatment for idiopathic scoliosis may change the paradigm to improve curves. Spine Deform 11, 1381–1388 (2023). https://doi.org/10.1007/s43390-023-00726-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00726-6