Abstract
The two main societies clinically dealing with idiopathic scoliosis are the Scoliosis Research Society (SRS), founded in 1966, and the international Society on Scoliosis Orthopedic and Rehabilitation Treatment (SOSORT), started in 2004. Inside the SRS, the Non-Operative Management Committee (SRS-NOC) has the same clinical interest of SOSORT, that is the Orthopaedic and Rehabilitation (or Non-Operative, or conservative) Management of idiopathic scoliosis patients. The aim of this paper is to present the results of a Consensus among the best experts of non-operative treatment of Idiopathic Scoliosis, as represented by SOSORT and SRS, on the recommendation for research studies on treatment of Idiopathic Scoliosis. The goal of the consensus statement is to establish a framework for research with clearly delineated inclusion criteria, methodologies, and outcome measures so that future meta- analysis or comparative studies could occur. A Delphi method was used to generate a consensus to develop a set of recommendations for clinical studies on treatment of Idiopathic Scoliosis. It included the development of a reference scheme, which was judged during two Delphi Rounds; after this first phase, it was decided to develop the recommendations and 4 other Delphi Rounds followed. The process finished with a Consensus Meeting, that was held during the SOSORT Meeting in Wiesbaden, 8–10 May 2014, moderated by the Presidents of SOSORT (JP O’Brien) and SRS (SD Glassman) and by the Chairs of the involved Committees (SOSORT Consensus Committee: S Negrini; SRS Non-Operative Committee: MT Hresko). The Boards of the SRS and SOSORT formally accepted the final recommendations. The 18 Recommendations focused: Research needs (3), Clinically significant outcomes (4), Radiographic outcomes (3), Other key outcomes (Quality of Life, adherence to treatment) (2), Standardization of methods of non-operative research (6).
Similar content being viewed by others
Introduction
The two main societies clinically dealing with idiopathic scoliosis are the Scoliosis Research Society (SRS), founded in 1966, and the international Society on Scoliosis Orthopedic and Rehabilitation Treatment (SOSORT), started in 2004. Inside the SRS, the Non-Operative Management Committee (SRS-NOC) has the same clinical interest of SOSORT, that is the Orthopaedic and Rehabilitation (or Non-Operative, or conservative) Management of idiopathic scoliosis patients.
SOSORT, after verifying the gradual reduction of scientific research in the area of the so-called non-operative treatment [1,2], started producing Consensuses with the aim of reaching a minimum agreement among scientists and clinicians engaged in the field [3-11]. In this respect, in 2011 SOSORT published the Clinical Guidelines that offer a general framework of reference to clinicians treating patients with idiopathic scoliosis [12].
The SRS Non-Operative Management Committee (SRS-NOC) published in 2005 the SRS Criteria for Bracing Studies that constitute the first effort to define precise criteria for conservative treatment research [13]. After this development, a series of papers have been produced respecting these inclusion criteria [14-19]. Also a randomized clinical trial in Bracing Adolescent Scoliosis Trial (BrAIST Study) has been planned accordingly [20], although the inclusion criteria had to be enlarged to aide in recruitment [20,21]. The main strength of the SRS criteria is to focus research on the most important population of patients at risk for progression to a surgical level of treatment. Conversely, the strict inclusion criteria squelched research efforts on non-operative treatment of scoliosis in other populations of patients. Scientific journals abiding to the SRS criteria would not accept manuscript for publication on other populations limiting advancement of knowledge in those areas. In addition, clinicians restricting their treatment regimens to patients within these inclusion criteria run the risk of failing to offer treatment to some patients.
Since the 2nd SOSORT Meeting in Boston 2007, the SRS Presidents have been invited speakers by SOSORT to start collaboration between the two Societies. In the 48th SRS Meeting in Lyon 2013, the SRS-NOC and SOSORT had the first combined educational Meeting on the Non-Operative management of IS. On this occasion it was decided to create a Committee to prepare the first joint SOSORT-SRS Consensus, with the aim to guide future research in the treatment of IS.
The aim of this paper is to present the results of a Consensus among the best experts of non-operative treatment of Idiopathic Scoliosis, as represented by SOSORT and SRS, on the recommendation for research studies on treatment of IS. The goal of the consensus statement is to establish a framework for research with clearly delineated inclusion criteria, methodologies, and outcome measures so that future meta- analysis or comparative studies could occur.
Methods
Design
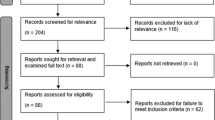
A Delphi method was used to generate a consensus to develop a set of recommendations for clinical studies on treatment of Idiopathic Scoliosis. It included the development of a reference scheme, which was judged during two Delphi Rounds; after this first phase, it was decided to develop the recommendations and 4 other Delphi Rounds followed. The process finished with a Consensus Meeting, that was held during the SOSORT Meeting in Wiesbaden, 8–10 May 2014, moderated by the Presidents of SOSORT (JP O’Brien) and SRS (SD Glassman) and by the Chairs of the involved Committees (SOSORT Consensus Committee: S Negrini; SRS Non-Operative Committee: MT Hresko). The Boards of the SRS and SOSORT formally accepted the final recommendations.
Participants
The participants were the two main scientific Societies dealing with scoliosis: SOSORT through the Executive Committee and the Advisory Board (SOSORT Boards), its members and the participants at their 2014 Annual Meeting; the SRS through the Non-Operative Management Committee, and the members who participated at the Consensus Meeting during the 2014 SOSORT Annual Meeting in Wiesbaden, 8–10 May 2014.
The Delphi consensus procedure
First reference scheme
The main idea behind the first reference scheme for research studies was to solicit authors to focus on meaningful clinical populations while writing their papers. This did not mean that that they should limit their studies to these groups of patients: while producing data with different groupings, the idea was to require them to report their data according to this specific reference scheme, to facilitate future meta-analysis and pooling of data.
Recommendations
After the first two Delphi Rounds, it was clear that it was not possible to reach any Consensus about the reference scheme. Nevertheless, according to the suggestions received, and the previous discussions inside the SOSORT and with the Chair of the SRS Non-Operative Committee, it was possible to develop a series of recommendations that were submitted to the Delphi Consensus procedure.
Delphi process
The Consensus procedure followed the Delphi principles [22]. All stages have been be coordinated by the main author (S Negrini), Chair of the SOSORT Consensus Committee, in strict collaboration with a Joint SOSORT-SRS Commission (JSSC) involving another member nominated by the SOSORT Board (JP O’Brien) and two members nominated by the SRS (T Hresko, N Price); in some phases also the SRS President (SD Glassman) has been involved.
The procedure included 8 Rounds. Documents distributed among the participants to the Delphi process were drafted by the first author (SN), and reviewed and approved by the JSSC. Table 1 reports the details of each single Delphi Round (Additional files 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 and 16). SOSORT Boards include the Executive Committee and the Advisory Board.
Agreement and importance of the recommendations
The SSJC decided to rate the recommendations according to the agreement reached at each stage and the importance defined by the participants at the Delphi procedure.
Definitions of Agreement reached for recommendations are reported in Table 2. The answers to the questions were mutually exclusive (Yes/No): if a recommendation did not reach at least 80% of Agreement it was rejected and not considered any more.
Definitions of the importance of recommendations are reported in Table 3. Importance of the Recommendation was defined using a 5 point Likert scale: 1-Very Low; 2-Low; 3-Medium; 4-High; 5-Very High.
Results
The number of responders to each Delphi Round is listed in Table 4, with their gender and profession; the rate of responders per group involved is reported in Table 5. All persons who participated at the Consensus and gave consent to be cited are listed in Table 6.
Details on the results on each single Round can be found in Attachment 16.
Recommendations for research studies on treatment of idiopathic scoliosis
Research needs
-
1.
We recommend ongoing high quality research and development focused on innovative non operative treatments for scoliosis and related spinal deformities (B2)
-
2.
We recommend that indications and contraindications for non-operative approaches are continuously researched by high quality studies (B2)
-
3.
We recommend that risks and benefits of non-operative treatments be continuously researched by high quality studies (B2)
Clinically significant outcomes
-
4.
We recommend that prognostic factors for consequences of the deformity in adulthood on primary patient-centred outcomes (such as aesthetics, deformity progression, disability, pain and quality of life) are continuously researched and better defined by high quality studies (A2)
-
5.
We recommend to systematically report in clinical studies the primary patient-centred (such as aesthetics, disability, pain and quality of life), and the secondary predictive (such as clinical, radiological and topographic data) outcomes of treatment approaches (B2)
-
6.
We recommend that non-operative clinics should focus primarily on clinical outcomes relevant to patients (such as aesthetics, disability, pain and quality of life), and secondarily on predictive outcomes (such as radiographic and topographic data). Clinical, radiological and topographic parameters must be all taken into account for clinical decisions (D2)
-
7.
We recommend to report research results in the clinically significant terms of number of patients at start and end of treatment exceeding 10°, 30° and 50° Cobb: epidemiology recognises these as risk thresholds for possible health consequences in adulthood like back pain and curve progression [3,12,20,21,23-27]. In everyday clinics, the importance of these thresholds should be defined case by case in front of single patients according to many parameters other than Cobb degrees (C2)
Radiographic outcomes
-
8.
We recommend that radiographic research outcomes are presented in terms of number of patients improved (6° or more), unchanged (+/−5°) and progressed (6° or more) (C2)
-
9.
We recommend the adoption of the “Risser+” staging. This is the result of the confluence between the original US Risser staging, and the so-called European version of Risser staging as modified by Stagnara [28-30]. Fusion of the tri-radiate cartilage has also been added, as it has been shown to be an important and prognostic subdivision of Risser staging 0. (D2) (NOTE: The SRS and SOSORT propose this Consensus Recommendation for further studies of repeatability of the Risser + test proposal before certifying its validity. The main authors are engaged to perform this study. As soon as this study will be performed, the SRS and SOSORT will check it for final approval of the Recommendation)

-
10.
We recommend that radiographic research outcomes are presented also split in tables according to Cobb degrees at start of treatment (group of 5° Cobb) and bone age (Risser + staging), like the following one (D2):

Other key outcomes (Quality of Life, adherence to treatment)
-
11.
We recommend that standardised and validated questionnaires are used to report Quality of Life results (B2)
-
12.
We recommend in clinical research to include data on adherence to treatment: statistical analysis should include these data. Prospective bracing studies must use objective means to monitor adherence. Exercises studies must report data on adherence to number and length of assisted sessions, and home-exercise (B2)
Standardization of methods of non-operative research
-
13.
In the introduction of a new non-operative treatment for patients during growth, for the radiographic outcome we recommend that the following research steps are followed: (B2)

-
14.
We recommend in research on non-operative treatment this table, from the Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence [31] (B2)

-
15.
In the introduction of a new brace, we recommend to focus research on the following SRS inclusion criteria [13]: above 10 years of age, Risser 0–2, curves 25-40° Cobb. (D2)
-
16.
In presenting research results on bracing, we recommend to answer to the questionnaire in Appendix of the SOSORT Guidelines for Management of braced patients [8] to understand how team managed patients. (B3)
-
17.
In presenting results on bracing, we recommend to specify results according to the dosage of bracing in terms of impact on patients’ social life. (B2)

-
18.
At this stage of research on non-operative approaches during growth other than bracing, we strongly recommend to present radiographic results (C2)
Discussion
In this section we summarize the recommendations in the light of the discussion amongst the participants to the Delphi procedure and the Consensus session.
Research needs
The first three recommendations have been grouped under the title “research needs”, since they all focus on what and how research should be performed in the near futur.. After a long period in which research on conservative treatment of IS continuously decreased [1], the situation changed in the last 10 years [2]: SOSORT was founded in 2004, and can be a cause or an effect of this change. Since the Cochrane reviews that painted the situation only a few years ago, (2009 for bracing [32,33], 2011 for exercising [34,35]), RCTs published in the literature showed the effectiveness of bracing [21,36] and also of scoliosis specific exercises [37,38]. Nevertheless, there is a strong need to continue this research, and these recommendations focus specifically on this point: they stress the need for innovations (new non-operative treatments), for searching the correct indications and contraindications. These three recommendations also stress the need for high quality studies, and not simply studies with low level of evidence.
-
1.
We recommend ongoing high quality research and development focused on innovative non operative treatments for scoliosis and related spinal deformities (B2)
-
2.
We recommend that indications and contraindications for non-operative approaches are continuously researched by high quality studies (B2)
-
3.
We recommend that risks and benefits of non-operative treatments be continuously researched by high quality studies (B2)
Clinically significant outcomes
The Cochrane Institute and modern epidemiology stress the need to focus on primary outcomes, the patient centered results, those that really change the life of patients [32,34]. In this perspective, secondary or surrogate outcomes are the biological parameters that predict the primary outcome, but are not directly and immediately connected to the life of patients. In scoliosis research, examples of primary outcomes are Quality of Life, back pain, disability, pulmonary disorders; and progression to surgical treatment. Examples of secondary outcomes are radiographic angles like the Cobb degrees or pelvis parameter, or surface measurements like the Angle of Trunk Rotation (ATR).
This set of recommendations should focus the attention of researchers on primary outcomes, since generally speaking most of the published research is focused on Cobb degrees and other secondary outcomes [3,12]. Nevertheless, since scoliosis treatment during growth is mainly prevention of primary outcomes that will happen in adulthood due to the deformity gradually developed before bone maturity, it must be recognised that secondary outcomes are crucial. In this perspective, it is also recommended to focus research on the real prognostic value of these secondary outcomes for consequences in adulthood in terms of primary outcomes.
-
4.
We recommend that prognostic factors for consequences of the deformity in adulthood on primary patient-centred outcomes (such as aesthetics, deformity progression, disability, pain and quality of life) are continuously researched and better defined by high quality studies (A2)
-
5.
We recommend to systematically report in clinical studies the primary patient-centred (such as aesthetics, disability, pain and quality of life), and the secondary predictive (such as clinical, radiological and topographic data) outcomes of non-operative approaches (B2)
-
6.
We recommend that non-operative clinics should focus primarily on clinical outcomes relevant to patients (such as aesthetics, disability, pain and quality of life), and secondarily on predictive outcomes (such as radiographic and topographic data). Clinical, radiological and topographic parameters must be all taken into account for clinical decisions (D2)
-
7.
We recommend to report research results in the clinically significant terms of number of patients at start and end of treatment exceeding 10°, 30° and 50° Cobb Angle as epidemiology recognises these as risk thresholds for possible health consequences in adulthood like back pain and curve progression [3,12,20,21,23-27]. In everyday clinics, the importance of these thresholds should be defined case by case based on individual patients according to many parameters other than Cobb degrees (C2)
The three thresholds reported have been quite discussed, specifically the 30° Cobb limit. In fact, concerns have been raised about focusing clinicians on this threshold, beyond the classical 50° used by surgeons [20,21,39]. Nevertheless, it must be recognised that the 30° limit has been reported as the boundary before which rarely there are health consequences in adulthood, like back pain or deformity progression. This makes this threshold particularly important for non-operative treatment that should aim at possibly maintaining patients below the limit significant for health.
Another concern about these thresholds was the fear of focusing clinicians mainly on Cobb degrees rather than on other parameters. Each patient is an individual, clinical decision must be made on a case by case basis for each patient.
Radiographic outcomes
-
8.
We recommend that radiographic research outcomes are presented in terms of number of patients improved (6° or more), unchanged (+/−5°) and progressed (6° or more) (C2)
For some years, it has been emphasized within the SOSORT community that there is the possibility to improve patients with conservative treatment [8,12,40]. For this reason, the classical SRS outcome criteria [13] were perceived as inadequate since they did not allow a description of cases where improvement was achieved. Therefore, while maintaining the classical 5° Cobb threshold to describe a clinically meaningful variation [41], it was decided to add a descriptor of improvement to stability and progression of deformity.
-
9.
We recommend the adoption of the “Risser+” staging. This is the result of the confluence between the original US Risser staging, and the so-called European version of Risser staging as modified by Stagnara [28-30]. It has been added also the tri-radiate cartilage fusion, that has been shown to be an important and prognostic subdivision of Risser staging 0. (D2) (NOTE: The SRS and SOSORT propose this Recommendation come out as a result of the Consensus for further studies of repeatability of the Risser + test proposal before certifying its validity. The main authors are engaged to perform this study. As soon as this study will be performed, the SRS and SOSORT will check it for final approval of the Recommendation)

The Risser + staging was an idea that came out during discussion when the importance of other radiographic signs like the tri-radiate cartilage was considered [30,42,43]. Many researchers in the SOSORT community use the so-called European Risser sign [28-30] that is born from a reported by Stagnara, a variation of the original Risser sign (here called US Risser sign). The consequence is that in many studies there is no clear definition of which Risser sign is considered. Unifying all these data coming from the pelvis evaluation was felt to be the first step toward a solution of these discrepancies. Obviously, the already well reported limited value of the Risser sign in describing bone growth and maturity [44-46] is recognised. But the reality remains that most of the studies, even the best ones [13], continue to use this sign since it is readily available in the same x-ray of the spine, without added exposure. The Risser + is simply defined as the convergence of the US and European Risser, adding the tri-radiate cartilage fusion: future studies should focus on this Risser + sign to check its repeatability and validity.
-
10.
We recommend that radiographic research outcomes are presented also split in tables according to Cobb degrees at start of treatment (group of 5° Cobb) and bone age (Risser + staging), like the following one (D2):

The evolution of knowledge in Medicine relies mainly on the research developments carried out by single groups, but the introduction of new statistical techniques allow today to perform so-called meta-studies: specifically, meta-analysis, permit to reach higher level of evidence joining little studies in bigger ones. In this evolution, respecting strict definitions and inclusion criteria, internationally acceptable, is very important to allow proper meta-studies to be performed. This is the reason for the reference scheme reported in the recommendation and proposed to all researchers.
Other key outcomes (Quality of Life, adherence to treatment)
-
11.
We recommend that standardised and validated questionnaires are used to report Quality of Life results (B2)
The literature on Quality of Life during scoliosis treatments is continuously increasing, as well as the questionnaires to measure it. The gold standard in surgical approaches is the SRS-22 [47,48], although there are doubts of the usefulness in non-operative care [49]. Other questionnaires have been developed and maybe useful in this specific setting if and when validated [50-53].
-
12.
We recommend in clinical research to include data on adherence to treatment: statistical analysis should include these data. Prospective bracing studies must use objective means to monitor adherence. Exercises studies must report data on adherence to number and length of assisted sessions, and home-exercise (B2)
Adherence to treatment should be distinguished from compliance [54]:”Adherence” is the result of the active choice of the patient to comply with the prescribed treatment which is necessary for brace treatment, while “compliance” is a passive behaviour. In non-operative treatment there is the need to look at adherence, since deciding to use a brace and or to perform exercises regularly is a choice to be made every day by the patient. Adherence also underlines the need (stressed in the literature) to help the patient in active participation in the treatment. In clinical research, adherence must be strictly monitored to better describe the treatment performed. A good adherence is not only a matter of feasibility of the non-operative treatment, but it is also a quality check of the entire approach. While for bracing there are now some monitors for adherence [55-60], in case of exercises, diaries are the only means at this point in time.
Standardization of methods of non-operative research
-
13.
In the introduction of a new non-operative treatment for patients during growth, for the radiographic outcome we recommend that the following research steps are followed: (B2)

One of the problems with assessing the effectiveness of non-operative treatment is the long duration in time in treatment. If the prevailing idea is to publish only final results, then research can be only rare and very sparse, thereby reducing the possibility of knowledge and improvement of treatments. On the other hand, it is not possible to consider as really relevant any research made only on the immediate in-brace results (even if in-brace results can have some predictive validity, still to be well explored) [61-63]. Even less reliable are very short term results immediately after a session, or a period of exercises, or other non-operative treatments (like manual treatments), that can change posture for a while, but without possibility to maintain this change in time like bracing [64,65]: in these cases what is researched is a training [66], and only stable results at least in the short term (12 months) can have some reliability. For this reason, knowing the timing of the results obtained is of high relevance, and very short term results are considered only for bracing.
-
14.
We recommend in research on non-operative treatment this table, from the Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence [31] (B2)

Level of Evidence is usually required by many spine journals: it was decided to adopt the table most used in the scientific literature.
-
15.
In the introduction of a new brace, we recommend to focus research on the following SRS inclusion criteria [13]: above 10 years of age, Risser 0–2, curves 25-40° Cobb. (D2)
During the Consensus it was decided to exclude the 1-year post-menarche limit for the inclusion criteria for bracing studies, since it was found poorly reliable by some studies presented during SOSORT Meetings [67].
-
16.
In presenting research results on bracing, we recommend to answer to the questionnaire in Appendix of the SOSORT Guidelines for Management of braced patients [14] to understand how team managed patients. (B3)
Adherence to treatment is recognised for a long time as a key factor of bracing: nevertheless, results published using sensors are really different among the research groups [55-60]. It has been shown that the management of patients is crucial for adherence to treatment [8,68]. While searching for Consensus on bracing, SOSORT was not able to find one, neither on the type of brace, nor on the brace’s biomechanical actions [5], although it was possible to agree on the management of patients [8]. The SOSORT criteria for Management of braced patients offer an understanding of how patients were managed, and in the Appendix a questionnaire is given, whose usage would allow researchers to better paint their clinical approach, and readers to really understand the results obtained.
-
17.
In presenting results on bracing, we recommend to specify results according to the dosage of bracing in terms of impact on patients’ social life. (B2)

This was one of the most difficult recommendations, since all clinicians use their own definitions, with different number of hours and dosages. After long discussion, it was decided to maintain this recommendation to reach some kind of agreement as a baseline to move on. This scheme was found as the most reasonable (and voted) since it is quite coherent with real-life habits of patients and not too complicated. Such a scheme is offered to the research community for further understanding.
-
18.
At this stage of research on non-operative approaches during growth other than bracing, we strongly recommend to present radiographic results (C2)
While non-operative treatments can seek results other than the deformity (such as back pain reduction, pulmonary function improvement, quality of life increase and so on) it has been decided after long discussion to give this recommendation, since we cannot ignore the deformity that could progress while treating other key health problems. This eventual progression (or contrarily, improvement) should never be ignored, and always reported, specifically for treatments whose results on the deformity are not yet known in the literature.
References
Negrini S. Approach to scoliosis changed due to causes other than evidence: patients call for conservative (rehabilitation) experts to join in team orthopedic surgeons. Disabil Rehabil. 2008;30:731–41.
Negrini S, Zaina F, O’Brien JP. Re: adolescent idiopathic scoliosis. BMJ. 2013;346:f2508.
Negrini S, Grivas TB, Kotwicki T, Maruyama T, Rigo M, Weiss HR. Members of the Scientific society On Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT): why do we treat adolescent idiopathic scoliosis? What we want to obtain and to avoid for our patients: SOSORT 2005 consensus paper. Scoliosis. 2006;1:4.
Weiss H-R, Negrini S, Hawes MC, Rigo M, Kotwicki T, Grivas TB, et al. Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment – SOSORT consensus paper 2005. Scoliosis. 2006;1:6.
Rigo M, Negrini S, Weiss HR, Grivas TB, Maruyama T, Kotwicki T. SOSORT: “SOSORT consensus paper on brace action: TLSO biomechanics of correction (investigating the rationale for force vector selection)”. Scoliosis. 2006;1:11.
Grivas TB, Wade MH, Negrini S, O’Brien JP, Maruyama T, Hawes MC, et al. SOSORT consensus paper: school screening for scoliosis: where are we today? Scoliosis. 2007;2:17.
Kotwicki T, Durmała J, Czaprowski D, Głowacki M, Kołban M, Snela S, et al. SOSORT: conservative management of idiopathic scoliosis--guidelines based on SOSORT 2006 consensus. Ortop Traumatol Rehabil. 2006;2009(11):379–95.
Negrini S, Grivas TB, Kotwicki T, Rigo M, Zaina F, international Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT). Guidelines on “Standards of management of idiopathic scoliosis with corrective braces in everyday clinics and in clinical research”: SOSORT Consensus 2008. Scoliosis. 2009;4:2.
De Mauroy J, Weiss H, Aulisa A, Aulisa L, Brox J, Durmala J, et al. 7th SOSORT consensus paper: conservative treatment of idiopathic & Scheuermann’s kyphosis. Scoliosis. 2010;5:9.
Grivas TB, de Mauroy JC, Négrini S, Kotwicki T, Zaina F, Wynne JH, et al. SOSORT members: terminology - glossary including acronyms and quotations in use for the conservative spinal deformities treatment: 8th SOSORT consensus paper. Scoliosis. 2010;5:23.
Knott P, Pappo E, Cameron M, Demauroy J, Rivard C, Kotwicki T, et al. SOSORT 2012 consensus paper: reducing x-ray exposure in pediatric patients with scoliosis. Scoliosis. 2014;9:4.
Negrini S, Aulisa AG, Aulisa L, Circo AB, de Mauroy JC, Durmala J, et al. 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis. 2012;7:3.
Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30:2068–75. discussion 2076–2077.
Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27:369–74.
Coillard C, Vachon V, Circo AB, Beauséjour M, Rivard CH. Effectiveness of the SpineCor brace based on the new standardized criteria proposed by the scoliosis research society for adolescent idiopathic scoliosis. J Pediatr Orthop. 2007;27:375–9.
Aulisa AG, Guzzanti V, Galli M, Perisano C, Falciglia F, Aulisa L. Treatment of thoraco-lumbar curves in adolescent females affected by idiopathic scoliosis with a progressive action short brace (PASB): assessment of results according to the SRS committee on bracing and nonoperative management standardization criteria. Scoliosis. 2009;4:21.
Guo J, Lam TP, Wong MS, Ng BKW, Lee KM, Liu KL, et al. A prospective randomized controlled study on the treatment outcome of SpineCor brace versus rigid brace for adolescent idiopathic scoliosis with follow-up according to the SRS standardized criteria. Eur Spine J. 2014;12:2650–7.
Aulisa AG, Guzzanti V, Marzetti E, Giordano M, Falciglia F, Aulisa L. Brace treatment in juvenile idiopathic scoliosis: a prospective study in accordance with the SRS criteria for bracing studies - SOSORT award 2013 winner. Scoliosis. 2014;9:3.
Negrini S, Donzelli S, Lusini M, Minnella S, Zaina F. The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis based on SRS and SOSORT criteria: a prospective study. BMC Musculoskelet Disord. 2014;15:263.
Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine. 2013;38:1832–41.
Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369:1512–21.
Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–80.
Hresko MT. Clinical practice: idiopathic scoliosis in adolescents. N Engl J Med. 2013;368:834–41.
Mayo NE, Goldberg MS, Poitras B, Scott S, Hanley J. The Ste-Justine adolescent idiopathic scoliosis cohort study. Part III: Back pain. Spine. 1994;19:1573–81.
Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559–67.
Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:447–55.
Weinstein SL, Dolan LA, Cheng JCY, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527–37.
Stagnara P. Les Deformations Du Rachis. Paris: Masson; 1985.
Kotwicki T. Improved accuracy in Risser sign grading with lateral spinal radiography. Eur Spine J. 2008;17:1676–85.
Nault M-L, Parent S, Phan P, Roy-Beaudry M, Labelle H, Rivard M. A modified Risser grading system predicts the curve acceleration phase of female adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92:1073–81.
The Oxford 2011 Levels of Evidence [http://www.cebm.net/ocebm-levels-of-evidence/]
Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev 2010:CD006850.
Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, et al. Braces for idiopathic scoliosis in adolescents. Spine. 2010;35:1285–93.
Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, et al. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2012;8:CD007837.
Romano M, Minozzi S, Zaina F, Saltikov JB, Chockalingam N, Kotwicki T, et al. Exercises for adolescent idiopathic scoliosis: a cochrane systematic review. Spine. 2013;38:E883–93.
Coillard C, Circo AB, Rivard CH. A prospective randomized controlled trial of the natural history of idiopathic scoliosis versus treatment with the SpineCor brace: sosort Award 2011 winner. Eur J Phys Rehabil Med. 2014;50:479–87.
Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: results of a randomised controlled trial. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2014;23:1204–14.
Negrini S, Bettany-Saltikov J, De Mauroy JC, Durmala J, Grivas TB, Knott P et al: Letter to the Editor concerning: “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial” by Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S: Eur Spine J 2014. DOI:10.1007/s00586-014-3241-y. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 2014.
Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine. 2007;32(19 Suppl):S91–100.
Negrini S, Atanasio S, Fusco C, Zaina F. Effectiveness of complete conservative treatment for adolescent idiopathic scoliosis (bracing and exercises) based on SOSORT management criteria: results according to the SRS criteria for bracing studies - SOSORT Award 2009 Winner. Scoliosis. 2009;4:19.
Morrissy RT, Goldsmith GS, Hall EC, Kehl D, Cowie GH. Measurement of the Cobb angle on radiographs of patients who have scoliosis: evaluation of intrinsic error. J Bone Joint Surg Am. 1990;72:320–7.
Sponseller PD, Betz R, Newton PO, Lenke LG, Lowe T, Crawford A, et al. Differences in curve behavior after fusion in adolescent idiopathic scoliosis patients with open triradiate cartilages. Spine. 2009;34:827–31.
Ryan PM, Puttler EG, Stotler WM, Ferguson RL. Role of the triradiate cartilage in predicting curve progression in adolescent idiopathic scoliosis. J Pediatr Orthop. 2007;27:671–6.
Dhar S, Dangerfield PH, Dorgan JC, Klenerman L. Correlation between bone age and Risser’s sign in adolescent idiopathic scoliosis. Spine. 1993;18:14–9.
Shuren N, Kasser JR, Emans JB, Rand F. Reevaluation of the use of the Risser sign in idiopathic scoliosis. Spine. 1992;17:359–61.
Wang WWJ, Xia CW, Zhu F, Zhu ZZ, Wang B, Wang SF, et al. Correlation of Risser sign, radiographs of hand and wrist with the histological grade of iliac crest apophysis in girls with adolescent idiopathic scoliosis. Spine. 2009;34:1849–54.
Bagó J, Pérez-Grueso FJS, Les E, Hernández P, Pellisé F. Minimal important differences of the SRS-22 patient questionnaire following surgical treatment of idiopathic scoliosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2009;18:1898–904.
Asher M, Min Lai S, Burton D, Manna B. Scoliosis research society-22 patient questionnaire: responsiveness to change associated with surgical treatment. Spine. 2003;28:70–3.
Negrini S, Donzelli S, Dulio M, Zaina F. Is the SRS-22 able to detect Quality of Life (QoL) changes during conservative treatments ? Stud Health Technol Inform. 2012;176:433–6.
Vasiliadis E, Grivas TB, Gkoltsiou K. Development and preliminary validation of Brace Questionnaire (BrQ): a new instrument for measuring quality of life of brace treated scoliotics. Scoliosis. 2006;1:7.
Botens-Helmus C, Klein R, Stephan C. The reliability of the Bad Sobernheim Stress Questionnaire (BSSQbrace) in adolescents with scoliosis during brace treatment. Scoliosis. 2006;1:22.
Aulisa AG, Guzzanti V, Perisano C, Marzetti E, Specchia A, Galli M, et al. Determination of quality of life in adolescents with idiopathic scoliosis subjected to conservative treatment. Scoliosis. 2010;5:21.
Caronni A, Zaina F, Negrini S. Improving the measurement of health-related quality of life in adolescent with idiopathic scoliosis: the SRS-7, a Rasch-developed short form of the SRS-22 questionnaire. Res Dev Disabil. 2014;35:784–99.
WHO. Adherence to Long-Term Therapies. Evidence for Action. Sabaté E: World Health Organization; 2003.
Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92:1343–52.
Takemitsu M, Bowen JR, Rahman T, Glutting JJ, Scott CB. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine. 2004;29:2070–4. discussion 2074.
Hunter LN, Sison-Williamson M, Mendoza MM, McDonald CM, Molitor F, Mulcahey MJ, et al. The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine. 2008;33:1554–61.
Rahman T, Borkhuu B, Littleton AG, Sample W, Moran E, Campbell S, et al. Electronic monitoring of scoliosis brace wear compliance. J Child Orthop. 2010;4:343–7.
Miller DJ, Franzone JM, Matsumoto H, Gomez JA, Avendaño J, Hyman JE, et al. Electronic monitoring improves brace-wearing compliance in patients with adolescent idiopathic scoliosis: a randomized clinical trial. Spine. 2012;37:717–21.
Donzelli S, Zaina F, Negrini S. In defense of adolescents: they really do use braces for the hours prescribed, if good help is provided. Results from a prospective everyday clinic cohort using thermobrace. Scoliosis. 2012;7:12.
Clin J, Aubin C-É, Sangole A, Labelle H, Parent S. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine. 2010;35:1706–13.
Chan SL, Cheung KM, Luk KD, Wong KW, Wong MS. A correlation study between in-brace correction, compliance to spinal orthosis and health-related quality of life of patients with Adolescent Idiopathic Scoliosis. Scoliosis. 2014;9:1.
Zaina F, Donzelli S, Lusini M, Negrini S. Correlation between in-brace radiographic correction and short time brace results. Stud Health Technol Inform. 2012;176:342–5.
Negrini A, Parzini S, Negrini MG, Romano M, Atanasio S, Zaina F, et al. Adult scoliosis can be reduced through specific SEAS exercises: a case report. Scoliosis. 2008;3:20.
Duval-Beaupère G, Lespargot A, Grossiord A. Flexibility of scoliosis: what does it mean? Is this terminology appropriate? Spine. 1985;10:428–32.
Smania N, Picelli A, Romano M, Negrini S. Neurophysiological basis of rehabilitation of adolescent idiopathic scoliosis. Disabil Rehabil. 2008;30:763–71.
Minnella S, Donzelli S, Zaina F, Negrini S. Risser stages, menarche and their correlations with other growth parameters in a cohort of 3,553 Italian adolescent idiopathic scoliosis patients. Scoliosis. 2013;8 Suppl 1:O13.
Tavernaro M, Pellegrini A, Tessadri F, Zaina F, Zonta A, Negrini S. Team care to cure adolescents with braces (avoiding low quality of life, pain and bad compliance): a case–control retrospective study: 2011 SOSORT Award winner. Scoliosis. 2012;7:17.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
SN drafted the manuscript, the various versions of the recommendations; lead the Delphi Exercise and the final Consensus Conference. MTH, JPOB and NP corrected and gave the main inputs to the manuscript and recommendations at all stages. All authors read and approved the final manuscript.
Authors’ information
* Members of SOSORT Executive Committee and Advisory Board in 2013–14: J Bettany-Saltikov, JC De Mauroy, J Durmala, TB Grivas, P Knott, T Kotwicki, T Maruyama, S Negrini, JP O'Brien, M Rigo, M Romano, L Stikeleather, F Zaina.
# Members of SRS Non-Operative Management Committee in 2013–14: TB Grivas, P Knott, JP O'Brien, L Stikeleather, M Ain, J Burgos Flores, C Tassone, D Fabris-Monterumici, M Halsey, MT Hresko, V Talwalkar, C Tello, A Ugras, J Verska.
Additional files
Additional file 1:
First reference scheme.
Additional file 2:
Consensus Methods version 1.
Additional file 3:
Consensus Methods version 2.
Additional file 4:
Discussions version 1.
Additional file 5:
Questionnaire 1.
Additional file 6:
Discussions version 2.
Additional file 7:
Recommendations version 1.
Additional file 8:
Consensus Methods version 3.
Additional file 9:
Recommendations version 2.
Additional file 10:
Discussion version 2.
Additional file 11:
Questionnaire 2.
Additional file 12:
Questionnaire 3.
Additional file 13:
Questionnaire 4.
Additional file 14:
Discussion version 4.
Additional file 15:
Questionnaire 5.
Additional file 16:
Final results.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Negrini, S., Hresko, T.M., O’Brien, J.P. et al. Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non–operative management committee. Scoliosis 10, 8 (2015). https://doi.org/10.1186/s13013-014-0025-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13013-014-0025-4