Abstract
Background
Complex health interventions (CHIs) are increasingly used in public health, clinical research and education to reduce the burden of disease worldwide. Numerous theories, models and frameworks (TMFs) have been developed to support implementation of CHIs.
This systematic review aims to identify and critique theoretical frameworks concerned with three features of implementation; adaptability, scalability and sustainability (ASaS). By dismantling the constituent theories, analysing their component concepts and then exploring factors that influence each theory the review team hopes to offer an enhanced understanding of considerations when implementing CHIs.
Methods
This review searched PubMed MEDLINE, CINAHL, Web of Science, and Google Scholar for research investigating the TMFs of complex health interventions. Narrative synthesis was employed to examine factors that may influence the adaptability, scalability and sustainability of complex health interventions.
Results
A total of 9763 studies were retrieved from the five databases (PubMed, MEDLINE, CINAHL, Web of Science, and Google Scholar). Following removal of duplicates and application of the eligibility criteria, 35 papers were eligible for inclusion. Influencing factors can be grouped within outer context (socio-political context; leadership funding, inter-organisational networks), inner context; (client advocacy; organisational characteristics), intervention characteristics (supervision, monitoring and evaluation), and bridging factors (individual adopter or provider characteristics).
Conclusion
This review confirms that identified TMFS do not typically include the three components of adaptability, scalability, and sustainability. Current approaches focus on high income countries or generic “whole world” approaches with few frameworks specific to low- and middle-income countries. The review offers a starting point for further exploration of adaptability, scalability and sustainability, within a low- and middle-income context.
Trial registration
Not registered.
Similar content being viewed by others

Introduction
This systematic review examines the adaptability, scalability, and sustainability (ASaS) of complex health interventions (CHIs), which are increasingly used in public health, clinical research, and education to alleviate global disease burdens [1]. The effectiveness of CHIs depends on various factors, including health resources, education levels, and economic status [2, 3].
CHIs are interventions with multiple interacting components, posing unique evaluation challenges beyond the usual practical and methodological difficulties [4].
Adaptability, scalability, and sustainability are crucial concepts in implementing CHIs, addressed through stages of evidence efficacy, scaling-up, and long-term sustainability [5]. Initial research phases focus on adapting interventions to local contexts and needs [6]. Once effectiveness is proven, the goal shifts to broader implementation, aiming for sustainability in real-world settings [5].The definitions of the ASaS is shown in the Table 1.
Theories, models and frameworks are used extensively to advance implementation science [10,11,12,13], to guide the design and implementation of complex interventions, and to help in assessing their quality. The resultant models can also be used to elucidate causal mechanisms between influencing factors and to identify contextual factors associated with changes in outcomes [10, 11, 14]. In turn, TMFs offer a lens for the exploration of the complex fields of public health, health policy and social care [10, 13].
Generally, a theory is:
Simply put, theories, are closely related to models. Specially, theories are characterized as combining the explanatory alongside the descriptive, and models are defined as theories with a narrowly defined scope of explanation [16]. A framework is:
Compared with theories and models, frameworks do not seek to be explanatory; rather than describe the internal relationships of concepts, they simply present the concepts [16]. However, despite some diverse characteristics, the terms “theory”, “model” and “framework” (TMF) are often used interchangeably.
However, most existing frameworks and measures for determining implementation factors and outcomes have originated in high-income nations [18]. A study indicated that although the number of frameworks related to program sustainability is increasing, these frameworks are rarely applied and evaluated in low- and middle-income countries or vulnerable communities within high-income countries. The primary reason for this phenomenon is the unique challenges faced by these countries and regions in terms of community and workplace capacities [19]. Therefore, it cannot be assumed that current TMFs are suitable for resource-limited settings [20].
Consequently, the aim of this review is to conduct a systematic review of theoretical frameworks concerned with at least one of the three ASaS concepts, to deconstruct the constituent theories, and to analyze the influencing factors within these frameworks. Another aim of this study is to assess the applicability and feasibility of these TMFs in diverse settings.
Specifically, the objectives of this review are:
-
1.
To explore definitions of scalability, adaptability, and sustainability.
-
2.
To identify published theoretical studies concerned with at least one of the concepts of sustainability, scalability and adaptability of complex health intervention-related frameworks and to assemble and explore relevant models and frameworks;
-
3.
To explore inter-relationships between factors influencing scalability, adaptability, and sustainability of the complex health interventions;
-
4.
To analyse the applicability and feasibility of these TMFs;
-
5.
To appraise the methodological quality and reporting quality of the included literature.
Methods
Search strategy
Systematic review methods were employed to identify and select TMFs. Specifically, the BeHEMoTh procedure was used as a systematic approach by which to collect theoretical frameworks [10]. The BeHEMoTh procedure offers auditability and transparency when identifying published TMFs [21]. Specific features of the BeHEMoTh search process are outlined in Additional file 1. The search begins with a structured BeHEMoTh question. First, the researcher reviewed TMFs identified from a scoping review in order to construct a systematic search procedure for retrieving ASaS related TMFs via Google Scholar [Step 1a]. PubMed MEDLINE, CINAHL and Web of Science, were systematically searched using the same search strategy, in a process similar to a conventional systematic review search [step 1b]. Titles and abstracts were screened for TMFs using a spreadsheet with each additional instance being added to the list of TMFs previously identified via step 1 [step 2]. Named models retrieved from step 2, together with models found from scoping via Google Scholar, were then searched to retrieve additional related reports [step 3]. Searching of source references for these TMFs was used to reveal cited studies [step 4a and step 4b].
Search terms
Search terms across all sources were organized within five search term groups including the three ASaS concepts (See Additional file 1). By searching for the three ASaS concepts individually rather than for their intersect, the search strategy recognises that few models involve all three factors of ASaS with many involving one or two factors.
Inclusion and exclusion criteria
Identified publications were imported to Endnote 9 software and duplicates were deleted. Specific inclusion criteria for factors that influence ASaS of CHIs are shown in Table 2.
Data extraction and appraisal
The titles and abstracts were screened, and the full papers of potentially relevant studies were obtained. Two authors independently assessed 10% of all titles and abstracts with a single reviewer then selecting full text papers for eligibility. An initial data extraction form was modified and adopted after revision. A single researcher independently extracted: (1) Study identification: year of publication, authors, name of study and name of the theories, models and frameworks; (2) Methods: study design, and study context; (3) any TMFs used; (4) Purpose of the theories, models, and framework; (5) Theories, models, and frameworks: definition, conceptual model, framework; (6) factors influencing ASaS of CHIs and inter-relationships between these concepts. These tables are shown in Additional file 3.
Quality assessment
Quality assessment criteria for assessing reports of TMFs are not common. Three papers were identified that either develop or utilize criteria for assessing theories [22,23,24] and these papers were used to compile the following quality assessment criteria:
-
1)
Is the methodology identified and justified?
-
2)
Was a theoretical lens or perspective used to guide the study, with a reference provided?
-
3)
Is the theoretical framework described?
-
4)
Is the theoretical framework easily linked with the problem?
-
5)
If a conceptual framework is used, are the concepts adequately defined?
-
6)
Are the relationships among concepts clearly identified?
-
7)
Are the influencing factors of concepts clearly identified?
-
8)
Are the relationships among influencing factors clearly described?
Quality assessments were undertaken by a single reviewer, quality assessment judgements are reported in Additional file 4.
Analysis
Given that the literature relating to TMFs derives from multiple disciplines, the researcher decided to use a narrative synthesis approach, which allows for synthesis of diverse types, designs and contexts for studies [25,26,27].
First, collected TMFs were categorized against a pre-existing classification: (1) Process models; (2) Determinant frameworks; (3) Classic theories; (4) Implementation theories; (5) Evaluation frameworks [16] (Table 3).
To effectively analyze the factors influencing the adaptability, scalability, and sustainability (ASaS) of complex health interventions (CHIs), this review integrates insights from multiple frameworks. Initially, the EPIS (Exploration, Preparation, Implementation, Sustainment) model was utilized, categorizing influencing factors into four key dimensions: Outer Context, Inner Context, Intervention Characteristics, and Bridging Factors. However, a more comprehensive understanding was needed, as the EPIS model alone did not fully capture the complexity of these factors.
To address this, features from the CFIR (Consolidated Framework for Implementation Research) and insights from the NASSS (Non-adoption, Abandonment, Scale-up, Spread, and Sustainability) framework and the Dynamic Sustainability Framework (DSF) were integrated. This meta-model enhancement involves expanding the descriptions within each EPIS dimension to cover additional critical elements found in these other frameworks.
Specifically, within the Inner Context, the organizational characteristics were elaborated to reflect deeper organizational dynamics affecting CHIs. In the Outer Context, the Sociopolitical Context was added, acknowledging its crucial influence on intervention outcomes. Further, the Intervention Characteristics were detailed more extensively to capture the nuanced nature of the interventions themselves.
This enriched model aims to provide a robust analytical framework that better reflects the complex interplay of factors influencing the ASaS of CHIs. By adopting this meta-model, the study offers a comprehensive theoretical foundation that underpins the examination of these complex interventions, paving the way for more targeted and effective implementation strategies in diverse settings.
Finally, the Theoretical Quality Tool, adapted from Hean et al. [31], was employed to rigorously assess the applicability of the collected (TMFs) in the context of Low- and Middle-Income Countries (LMICs).
Results
Characteristics of included studies
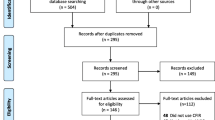
The flowchart of the search results (Fig. 1) shows that the search identified 9763 studies. Following removal of duplicates and application of eligibility criteria, 37 studies remained for inclusion in the review. 25 studies provide macroscopic TMFs for CHIs [5,6,7,8,9, 30, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49] worldwide. A further seven included TMFs [50,51,52,53,54,55,56] that were developed in high-income countries and only five studies [21, 57,58,59,60] targeted LMICs.
Types of TMF
Overall, 28 [5,6,7,8,9, 21, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46, 48,49,50, 55, 57, 58, 61] of the 37 studies describe macroscopic TMFs and nine studies [30, 47, 51,52,53,54, 56, 59, 60] describe TMFs for specific relevant interventions. Categorising these according to the five categories of Per Nilsen's schema (Table 3) reveals that 14 of the 37 TMFs are process models, 14 are determinant frameworks, one is classic theory, one is implementation theory, and seven are evaluation frameworks (See Additional file 5). One classic theory and one implementation theory are included. The Detailed classification for collected TMFs is described in Table 4.
Adaptability, scalability and sustainability definitions
All 37 included studies reported at least two out of the three concepts of ASaS, and the specific concepts involved in each study. (See Table 5). Definitions of ASaS found in the included studies are shown in the Additional file 2.
The process of implementation and relationships of adaptability, scalability and sustainability
Diverse TMFs support a strong correlation between the three ASaS concepts and the implementation process. Twenty-five of the TMFs explicitly mentioned implementation of CHIs; while the remaining ten did not [6, 8, 21, 39, 40, 44, 54,55,56, 62].
This review confirms the interconnectedness of adaptability, scalability, and sustainability in the implementation of complex health interventions (CHIs). The findings suggest that adaptability is crucial during the initial stages of CHI deployment, determining the potential for effective and cost-efficient implementation. As the intervention progresses, scalability becomes critical, ensuring that strategies effective on a smaller scale can be expanded to broader populations and regions. Ultimately, sustainability is achieved in the final stages, focusing on maintaining the benefits of the intervention over time and making necessary adjustments based on ongoing feedback and changing conditions.
In essence, the successful scaling and long-term sustainability of CHIs fundamentally depend on their initial adaptability. This streamlined approach highlights the critical progression from adaptability through scalability to sustainability, without delving into the specifics of various models and frameworks.
Influencing factors of adaptability, scalability and sustainability of complex interventions
This study collected and analyzed factors affecting the adaptability, scalability, and sustainability (ASaS) of complex health interventions (CHIs), systematically categorizing them into four distinct categories: outer context, inner context, intervention characteristics, and bridging factors. This classification helps clarify the various factors that influence the implementation of health interventions.
While all these factors impact the three concepts of ASaS, some have particularly close relationships with specific ASaS concepts. Subsequent sections will explore these factors in detail, emphasizing those closely linked to individual ASaS concepts. This approach highlights the multidimensionality of these factors and their varying impacts on the adaptability, scalability, and sustainability of CHIs. The overview of the factors influencing the ASaS is shown in the Table 6.
Outer context
Name of influencing factors, suggested definition, frequency of influencing factors of Outer context is shown in Table 7.
Sociopolitical context
This study has identified multiple studies highlighting how sociopolitical factors deeply influence the adaptability, scalability, and sustainability (ASaS) of complex health interventions (CHIs) [8, 30, 35, 37, 39, 42, 44, 47, 49,50,51,52,53,54, 58,59,60, 64]. These factors, including religion [58], ethics [39, 56], legislation [30, 35, 39, 44, 54, 58, 59, 64], norms or regulations [7, 21, 35, 38, 49, 54, 56, 58], and policies [6, 7, 9, 21, 35, 37,38,39, 44, 50, 51, 54, 56, 57, 59], play a critical role in shaping health outcomes and addressing healthcare disparities. The influence of sociocultural factors such as common traditions, habits, patterns, and beliefs was also evident across different populations [35, 37,38,39, 44, 50, 52, 54, 57, 58, 62].
Interorganizational networks
Interorganizational networks bridge full-scale relationships across organizations [65], and it was found to significantly enhance the implementation of CHIs, enabling better adaptation to local contexts and sustainability at lower costs through effective resource sharing and communication.
Funding
Also, the role of funding was another major factor discussed, highlighting its critical importance for providing necessary resources such as training, materials, and health services [66]. Nineteen of the identified models or frameworks emphasize fiscal support prioritized in implementation [6,7,8,9, 21, 30, 34,35,36, 38, 39, 44, 45, 50, 54, 55, 58, 59, 64].
Client advocacy
Three of the 37 studies identify client advocacy as an important influencing factor [9, 45, 50]. During implementation client advocacy assists healthcare workers, participants and their families in navigating the healthcare system [67].
Leadership
Finally, 16 of the 37 studies emphasize leadership [6, 21, 30, 35, 36, 40, 42,43,44,45, 50, 51, 56,57,58,59]. Specific subgroups may offer either approval or conflict. Strong leadership can promote effective use of resources while encouraging personnel to work towards a common goal.
Inner context
Name of influencing factors, suggested definition, frequency of influencing factors of Outer context is shown in the Table 8.
Organizational characteristics
Organizational characteristics influence the process of implementing complex health interventions (CHIs) through structures and processes within organizations. These characteristics encompass ten influencing factors including absorptive capacity [6, 8, 9, 21, 36, 37, 40, 44, 50,51,52, 56, 57, 59, 64], organizational readiness [8, 30, 50,51,52], structure [6, 7, 35, 38, 40, 44, 49, 51, 52, 59, 64], values or visions [35, 37, 40, 43, 44, 51, 59], working environment [6,7,8,9, 41, 45, 50, 51, 54, 56], tension for change [6, 49, 51, 53], organization culture [6, 35, 40, 43, 50, 58], leadership [6, 21, 35, 36, 40, 42,43,44,45, 50, 51, 56,57,58,59], credibility and reputation [43]. The adaptability, scalability, and sustainability (ASaS) of CHIs are significantly dependent on these organizational elements.
Structure
Organisations with strong organisational power may be likely to implement CHIs because they have stronger leadership and more frequent communication than those with weak or decentralised organisational structures [68].
Readiness for change
In addition, strong organisations are prepared and aware of possible encountered changes and can adjust their strategies and approaches of working in time to enable CHIs to be carried out well. Readiness for change is related to other factors including organisational culture, and individual attitudes [69,70,71,72].
Absorptive capacity
During the exploration and preparation phases of a CHI, an organisation's absorptive capacity (the ability to identify, assimilate, transform, and use external knowledge, research and practice [73]), readiness for change and receptive environment exert a significant impact on the adaptability of CHIs.
Individual adopter or provider characteristics
Individual adopter or provider characteristics include participants’ personal characteristics, age, race/ethnicity, education, training, foundation subjects, professional experience, adaptability, personal values and goals, and personal character creative ability.
Fourteen included studies emphasise how the CHI is accepted and scaled-up by participants and health care workers [6,7,8, 34,35,36, 41, 45, 47, 51, 53, 54, 56, 58]. In parallel to the organisational level, individual ability or capacity [6, 35, 44, 51, 53, 56, 57, 64], training or education [7, 8, 35, 36, 40, 51, 52, 56], and tenacity for change [6, 51, 53] constitute important factors. CHIs are more easily adapted and diffused when led by experienced and leaders [6, 21, 35, 36, 40, 42,43,44,45, 50, 51, 56,57,58,59] with common visions or views [6, 35, 51, 53, 56, 60, 64]. In addition, race [35, 50], spoken language [35, 50, 52] and individual culture [35, 53, 56, 59] are considered to be vital influencing factors. Specifically, when there is a high degree of fit between the norms and values of the individual, organisation and CHIs, individuals may find that they achieve higher efficacy when implementing CHIs [64].
Leadership
As mentioned above, 16 of the 37 included studies emphasize leadership [6, 21, 30, 35, 36, 40, 42,43,44,45, 48, 50, 51, 56,57,58,59].
Staffing
CHIs require sufficient, well-trained healthcare workers. Fourteen of the 37 studies list staffing as an important factor in their TMFs [7, 30, 34,35,36,37, 43,44,45, 50,51,52, 56, 64]. Job candidates may be selected so that their knowledge, skills, competencies, and attitudes [74] match the requirements of the CHI.
Supervision, monitoring and evaluation
Supervision, monitoring and evaluation refers to the collection, storage, analysis and use of data to assess whether complex interventions are achieving their intended objectives, and further influences improvement, policy development and advocacy of complex intervention [75]. Nine of the 35 studies argue for the vital role of monitoring and evaluation in providing an effective approach by which to assess the effectiveness of complex interventions [21, 30, 40, 43, 44, 50, 51, 58, 64].
Intervention characteristics
The characteristics of the intervention itself is also an important factor. Specifically, the physical and community environment, the cost of the intervention and access to resources (8 studies) [6, 21, 30, 34, 38, 51, 52, 56] and the source of funding all exert a direct impact. Project champions are committed to supporting and promoting the implementation of CHI, along with a strong belief in the value of carrying out CHIs [76]. The factors within intervention characteristics is shown in the Table 9.
The included frameworks attest to how the characteristics of the CHI decide whether an intervention can be adapted, scaled-up and sustained [6, 8, 33, 36, 47, 51, 53]. Although researchers hope that CHIs can be adapted and conducted as quickly as possible, it takes time for both healthcare providers and participants to adapt to new interventions [77]. Also, when interventions change significantly within a short period of time, the lack of sufficient time to adapt to the intervention and adjust to relevant cultural factors prevent staff and participants from adopting a new CHI [78].
Bridging factors
Factors influencing the inter-relationship of outer and inner context are described as “bridging factors” in the EPIS framework. Bridging factors include community engagement and Purveyors/Intermediaries.
Twelve studies stress the importance of the community. Development of complex interventions within a community may be facilitated when they utilise existing community resources, available structures and staff, reducing dependence on external funding [21]. For example, community members were proud to participate in a project to improve malaria prevention through insecticide-treated mosquito nets and thereby contribute to disease control within their community. Consequently, the project was speedily adapted, replicated and scaled-up locally [79]. The community function is also affected by socio-political factors [80]. If the visions and beliefs of the policy are inconsistent with community objectives, the policy hinders spread and sustainability even where the community possesses powerful leadership, project champions and sufficient resources [80, 81].
Purveyors/Intermediaries take on a critical bridging role for key processes in the implementation of CHIs [45]. Purveyors, who may be individuals, groups or communities, aim to facilitate the effective and sustainable implementation of CHIs [82]. Intermediaries provide consultancy and training services to governments, organisations, etc., and also develop and implement different health-services and projects for them [82]. They also provide monitoring, support, quality improvement and evaluation services at the end of the project [82]. The factors within bridging factors is shown in the Table 10.
Applicability and feasibility of the collected TMFs
This study employs the Theoretical Quality Tool, adapted from Hean et al. [31], to rigorously assess the applicability of various Theoretical Models and Frameworks (TMFs) in the context of Low- and Middle-Income Countries (LMICs). The detailed outcomes of this assessment are presented in the Additional file 6. The summary table highlights the applicability and feasibility of TMFs in LMICs.
Of the 37 TMFs reviewed (two studies identify EPIS), seven demonstrate high applicability and feasibility, readily integrating into LMIC healthcare environments without necessitating significant overhauls. For example, models like the AIDED and NPT are readily implementable in LMICs due to their practicality and context-sensitive design. They integrate seamlessly into existing healthcare systems, offering solutions without the need for extensive system overhauls, crucial in resource-limited environments. Twenty-five TMFs require adaptations to align with the local conditions of LMICs, entailing modifications to fit cultural, economic, and healthcare infrastructure nuances. For example, the EPIS framework, CFIR framework, PRISM Model and Chronic Care Model, though broadly applicable, need customization to fit the unique cultural, economic, and healthcare infrastructures of LMICs.
For the remaining five TMFs, their inherent theoretical complexity and the fact that some were specifically designed for High-Income Countries (HICs) pose significant barriers to adoption in in Low- and Middle-Income Countries (LMICs). This finding highlights an important disconnect between their foundational assumptions and the practical realities of healthcare systems in LMICs. The evaluation outcomes of the applicability and feasibility of the collected 37 TMFs are shown in the Table 11.
Discussion
This theoretical systematic review identified common features and differences across 37 TMFs associated with ASaS.
Similarities and differences between the TMFs
All identified TMFs emphasize the importance of one or more of the three ASaS concepts. These frameworks aim to enable CHIs to adapt to new contexts and populations, scale up interventions, and ensure long-term effectiveness. The components of different TMFs share broadly similar descriptions, even if the terminology varies. For example, the EPIS framework divides the implementation process into four phases: exploration, preparation, implementation, and sustainment whereas Sarma’s framework [5] describes three domains: i: evidence – efficacy to effectiveness; ii: Scaling-up; and iii: sustainability. A further study [36] describes four stages 1. Training (dissemination); 2. adoption (planning); 3. implementation; 4. practical improvement and two key points (preparation and maintenance).
In the EPIS framework, during exploration and preparation, adaptability is considered to determine whether the complex intervention can be conducted effectively with affordable cost. Domain I of Sarma’s framework [5] includes the four vital components of intervention sources, evidence strength and quality, relative advantages, adaptability and complexity. The Framework - oral health [36] emphasizes adoption within the second stage. Hence, these three stages have the similar key components. The EPIS framework describes how a pilot study is further implemented across diverse participants and areas, which is similar to Domain ii: Scaling-up in Sarma’s framework [5] and the implementation stage in Framework - oral health [36]. Finally, the sustainment stage in EPIS framework, Domain iii: sustainability in Sarma’s framework [5] and the maintenance point in Framework - oral health [36] all convey a shared understanding of sustainability.
Similar stages may be presented in a different order within various models, reflecting the inherently multi-stage and non-linear nature of CHI implementation. Significant differences across different TMFs primarily relate to influences on ASaS. Furthermore, even when different TMFs use the same terminology to describe influencing factors, the meanings may differ due to the inherent complexity and dynamics of these factors.
The complexity of influencing factors of adaptability, scalability and sustainability
The TMFs reflect how CHIs and associated influencing factors do not operate in isolation, but are non-linear, interacting and interdependent. Some influencing factors appear across multiple studies. For example, researchers share a consensus about the importance of funding [6,7,8,9, 21, 34,35,36, 38, 39, 44, 45, 50, 54, 55, 58, 64]. Some studies emphasise adequate and sustained financial support from governments and foundations as prerequisite to the sustainability and spread [5, 44, 50, 61], while Sarma [5] recognizes the need to sustain interventions in the absence of adequate funding [21]. In addition, the sociopolitical context, leadership and organizational characteristics are repeatedly mentioned as essential components for implementation. Furthermore, all the factors mentioned in the literature are bi-directional; the same influencing factor may act differently under diverse conditions, either as a facilitator or as a hindrance.
To be specific, first, in terms of the outer context, strong leadership can facilitate effective use of resources while encouraging personnel to work towards a common goal. Also, sociopolitical factors covers ethical considerations [39, 56], legislation [35, 39, 44, 54, 58, 64], norms or regulations [7, 21, 35, 38, 54, 56, 58], policies [6, 7, 9, 21, 35, 37,38,39, 44, 50, 51, 54, 56, 57], and religion [58]. Legislation and policies not only guide, and often guarantee, complex interventions at the macro level, but also, at the empirical level, provide a basis for adapting CHIs to the local environment thereby making interventions suitable for scale up and long term sustainment [35, 39, 44, 54, 58, 64]. High quality interorganizational communication contributes to the implementation and sustainability of CHIs [83]. Additionally, weak leadership exerts a negative impact on the management of the organisation, funding applications and the recruitment of staff.
Leadership remains an important factor in relation to the inner context. Given that complex interventions are often run by the state, an organisation or a group, strong leadership can facilitate complex interventions. Also, the organisational culture, the vision/belief and the structure of the organisation interact with each factor and are influenced by funding, leadership and staffing.
Strong leadership needs to be accompanied by a structured organisation with a common vision in order to achieve the objectives of complex interventions. People as the carriers of culture, organisation, professional and personal attitudes, norms, interests and affiliations [84] also fulfil an important role. Individual adopter or provider characteristics are important influencing factors. When people within the organisation are aligned with the organisation's philosophy and culture, along with sufficient financial support, strong leadership and effective supervision, adaptation, scale up and long-term sustainment become possible for CHIs. Finally, intervention factors are influenced by both the outer context and the inner context, and bridging factors serve to unite the outer context, the inner context, and the intervention factors.
The dynamics of influencing factors of adaptability, scalability and sustainability
Factors that influence complex interventions are dynamic in both temporal and geographical terms. The role of these factors may change over time [85]; anticipated barriers may become facilitators [85]. For example, in the early stages of an intervention, individual adopters may exhibit skepticism and distrust, presenting a barrier to CHI delivery. However, in later stages, if the intervention proves effective, participant attitudes may shift, motivating them to cooperate and thus becoming facilitators. Similarly, in the early stages, newly recruited or local staff may be unfamiliar with the intervention, posing a hindrance. Conversely, as staff become familiar with the intervention, they are better equipped to implement it, thereby becoming facilitators.
Identical influencing factors may have different effects in various geographical and national contexts. For example, women are generally considered a vulnerable group worldwide, particularly in LMICs, where they tend to have lower income and social status compared to men, making it difficult for them to access better health care resources [86]. However, in the matrilineal community in Indonesia, women occupy similar or even higher social status than men, with a cultural tradition of controlling family finances [87]. Therefore, in this context, gender and culture may facilitate interventions, especially maternal and child health related interventions. In relation to funding, reliable sources of funding help to sustain interventions [5], and one of the challenges to sustainability is the lack of long-term available funding [21]. In summary, this systematic review offers a comprehensive understanding of factors influencing ASaS and provides a theoretical framework for effective CHIs in the future.
Have gaps in knowledge been addressed?
This is the first systematic review of ASaS related TMFs of CHIs. By focusing on the three factors of adaptability, sustainability and spread the review has been able to explore complex interactions of each with each other and with other important factors.
How have authors defined scalability, adaptability, and sustainability?
Additional file 2 consolidates definitions of scalability, adaptability and sustainability as identified across the included studies. It is noticeable that “sustainability has evolved from being considered as the endgame of a translational research process to a suggested 'adaptation phase’ that integrates and institutionalizes interventions within local organizational and cultural contexts.” [7]
This literature argues that sustainability is, in fact, a manifestation of adaptability, and that the two concepts are closely related.
Which theoretical studies explore at least one of the concepts of scalability, adaptability and sustainability of complex health intervention within a relevant model/frameworks;?
This review reveals the scarcity of theoretical models for LMICs. The review identified four main categories of theoretical models, (i) the generic TMFs (e.g. RE-AIM and CFIR), with no obvious geographical target (26/37); (ii) tailored TMFs developed by some high-income countries (e,g. [52, 53, 56]. for local needs (6/37); (iii) adapted TMFs (e.g. EPIS and Framework of Dissemination in Health Services Intervention Research), originally designed for high-income countries but now adapted to CHIs worldwide; (iv) TMFs specific to low and middle income countries (5/37) (e.g. [21, 57]). 85.7% of the included theories are either generic or specific to high-income countries, with a lack of TMFs specifically targeted at LMICs. As a result of this literature review the team have proceeded to develop a framework for Adaptability, Scalability and Sustainability that is suited for a low- and middle-income country context.
Thirty seven studies explore at least one of the concepts of sustainability, scalability and adaptability. However, no previous studies have explored all three ASaS concepts within a single TMF. Although some studies invoke the need to explore influencing factors and correlation among ASaS, no studies have actually conducted this research.
What inter-relationships have been demonstrated between factors influencing scalability, adaptability, and sustainability of the complex health interventions?
The meta-framework provides a comprehensive structure to explore the complexities of CHI implementation, emphasizing the interplay among four critical domains: outer context, inner context, intervention characteristics, and bridging factors.
In the outer context, the interplay between strong leadership, sociopolitical factors, and interorganizational networks is crucial. Strong leadership promotes resource optimization and strategic alignment toward CHI goals, essential for ASaS [35, 39, 44, 54, 58, 64]. Sociopolitical factors, including legislation, policies, and norms, provide a regulatory framework that guides the adaptation of CHIs to local settings, enhancing their feasibility and long-term integration [83]. Additionally, robust interorganizational communication facilitates effective adaptation of CHIs to local contexts, potentially lowering costs and enhancing sustainability.
Within the inner context, organizational culture, structure, and leadership significantly interact, affecting CHI outcomes. Strong, visionary leadership is crucial for fostering an organizational culture that supports CHIs and aligns with broader intervention goals [84]. The organization's structure further influences the implementation of these interventions, with well-structured organizations likely to achieve better scalability and sustainability. Additionally, the characteristics of individual providers and adopters play a critical role, impacting their ability to effectively implement and sustain CHIs.
The characteristics of the intervention itself directly impact its implementation. Factors such as the intervention's complexity, cost, resource requirements, and specific design elements determine the ASaS especially for the stages of adaptability and scalability [6, 21, 30, 34, 38, 51, 52, 56, 59]. Support from project champions and stakeholder involvement are crucial in facilitating the implementation process, ensuring that the interventions are well-supported and aligned with stakeholder expectations [8, 21, 34, 36, 37, 40, 44, 49, 50, 56, 60].
Bridging factors like community engagement and the role of purveyors/intermediaries are vital for linking the outer and inner contexts of CHIs. Community engagement leverages local resources and capacities, which is essential for the localized adaptation and sustainability of interventions [8, 9, 21, 30, 34, 38, 42, 44, 45, 54, 56, 58]. Purveyors and intermediaries facilitate the transfer of knowledge and best practices, enhancing the overall effectiveness and reach of CHIs [45]. These bridging roles ensure that interventions are not only well-integrated within communities but also maintain fidelity to their objectives and outcomes over time.
Lack of TMFs designed for LMICs
The lack of specifically designed TMFs for LMICs presents significant challenges in effectively implementing complex health interventions (CHIs) in these settings. Evaluating existing TMFs reveals a gap in their suitability and feasibility for application within the unique healthcare environments of LMICs.
Of the 37 TMFs assessed, many were found to require adaptations to align with the local conditions of LMICs, necessitating modifications to fit cultural, economic, and healthcare infrastructure nuances. For instance, frameworks such as EPIS, CFIR, PRISM Model, and Chronic Care Model, though broadly applicable, need customization to fit the unique contexts of LMICs.
Five of the TMFs reviewed were identified as inherently complex and primarily designed for high-income settings, posing substantial barriers to their adoption in LMICs. This highlights a critical disconnect between the foundational assumptions of these models and the practical realities of healthcare systems in LMICs, which face challenges such as limited resources, differing disease burdens, and varied healthcare delivery systems.
Despite these challenges, some models demonstrate higher applicability and feasibility. For example, the Dynamic Sustainability Framework (DSF) and the AIDED model are noted for their practicality and context-sensitive design, aligning with the continuous adaptation and learning required in LMICs. These models integrate seamlessly into existing healthcare systems, offering solutions without the need for extensive system overhauls, which is crucial in resource-limited environments.
The findings underscore the need to develop or adapt existing TMFs specifically tailored to the conditions of LMICs. This involves considering local healthcare practices, resource limitations, and cultural factors to ensure that the frameworks are both applicable and feasible in supporting the effective implementation and sustainability of CHIs in these settings.
Strengths and limitations
This systematic review retrieved relevant literature through a comprehensive search across four databases. Only studies published in English were included, potentially missing those from the grey literature. Identifying relevant implementation TMFs proved challenging due to the complex and diffuse terminologies used in this field. Exhaustive lists of synonyms would have been prohibitive, resulting in lack of specificity and numerous false positives. The authors sought an optimal balance between sensitivity and workload. Although the included studies were evaluated using a quality assessment tool, the risk of bias remains, particularly since only one author was responsible for data extraction.
Furthermore, although this review has identified how influencing factors interact, no clear theoretical model charts the specific TMFs, routes, and pathways from the influencing factors to the ASaS of CHIs. Finally, concepts such as acceptability, fidelity, and feasibility, are recognized as important features of CHIs [88] but fell outside the remit of this review.
Only one classic theory and one implementation theory are included. There are two possible reasons. Classical theories are borrowed from such disciplines as psychology, sociology and organisational development (e.g. the Diffusion of Innovation theory [89]. Similarly. the Health Belief Model was published in 1950 [90] and the Theory of Planned Behavior in the late 1980s [91]. Given that inclusion requires publication after 2000, many classic theories predate the study period. On the other hand, other theories, such as the implementation climate theory [92], may not be conceptually related to ASaS, resulting in their exclusion. The Detailed classification for collected TMFs is described in Table 4.
Conclusion
This review synthesizes 37 TMFs that document factors influencing the ASaS of CHIs. It confirms the wide variety of definitions used for adaptability, scalability, and sustainability within current TMFs, which typically do not include all three components. Current approaches focus on high-income countries or generic “whole world” approaches, with few frameworks specific to low- and middle-income countries. Numerous attempts have been made to describe and explore the interrelationships between implementation components. Of these, the EPIS and CFIR frameworks seem to possess the greatest inherent value, particularly within a model consisting of outer context, inner context, intervention characteristics, and bridging factors. This review offers a starting point for further exploration of adaptability, scalability, and sustainability, particularly within a low- and middle-income context.
Availability of data and materials
All data cited in this review derives from published papers and therefore already available.
Abbreviations
- ASaS:
-
Adaptability, scalability and sustainability
- COM-B:
-
Capability, Opportunity, Motivation and Behaviour
- CHI:
-
Complex health interventions
- EBP:
-
Evidence-based practice
- EPIS framework:
-
Exploration, Preparation, Implementation, Sustainment (EPIS) framework
- LMICs:
-
Low- and middle- income countries
- MRC:
-
Medical Research Council
- TMF:
-
Theory, model and framework
Reference List
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M et al. Developing and evaluating complex interventions: the new Medical Research Council guidance BMJ. BMJ: 2008;337:a1655. https://doi.org/10.1136/bmj.a1655.
Waters E, et al. Essential components of public health evidence reviews: capturing intervention complexity, implementation, economics and equity. J Public Health. 2011;33(3):462–5.
Wells M, et al. Intervention description is not enough: evidence from an in-depth multiple case study on the untold role and impact of context in randomised controlled trials of seven complex interventions. Trials. 2012;13(1):1–17.
Anderson R. New MRC guidance on evaluating complex interventions BMJ. BMJ: 2008;337:a1937. https://doi.org/10.1136/bmj.a1937.
Sarma H, et al. Developing a conceptual framework for implementation science to evaluate a nutrition intervention scaled-up in a real-world setting. Public Health Nutr. 2021;24(S1):s7–22.
Damschroder LJ, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):1–15.
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8(1):1–11.
Organization, W.H., Practical guidance for scaling up health service innovations. World Health Organization. World Health Organization: 2009. https://iris.who.int/bitstream/handle/10665/44180/9789241598521_eng.pdf?sequence=1.
Scheirer MA, Dearing JW. An agenda for research on the sustainability of public health programs. Am J Public Health. 2011;101(11):2059–67.
Booth A, Carroll C. Systematic searching for theory to inform systematic reviews: is it feasible? Is it desirable? Health Inform Libr J. 2015;32(3):220–35.
Noyes J, et al. Current use was established and Cochrane guidance on selection of social theories for systematic reviews of complex interventions was developed. J Clin Epidemiol. 2016;75:78–92.
Oliver SR, et al. A multidimensional conceptual framework for analysing public involvement in health services research. Health Expect. 2008;11(1):72–84.
Ridde V, Pérez D, Robert E. Using implementation science theories and frameworks in global health. BMJ Global Health. 2020;5(4):e002269.
Milat AJ, Li B. Narrative review of frameworks for translating research evidence into policy and practice. Public Health Res Pract. 2017;27(1):e2711704.
Rimer, B.K. and K. Glanz, Theory at a glance: a guide for health promotion practice. US Department of Health and Human Services National Institutes of Health: 2005. https://cancercontrol.cancer.gov/sites/default/files/2020-06/theory.pdf.
Nilsen, P. Making Sense of Implementation Theories, Models, and Frameworks. In: Albers B, Shlonsky A, Mildon R. (eds) Implementation Science 3.0. Springer: Springer, Cham. 2020. https://doi.org/10.1007/978-3-030-03874-8_3.
Sabatier PA, Weible CM. eds., Theories of the policy process. Westview press: 2014. https://books.google.com.hk/books?.
Kemp CG, et al. Implementation science and stigma reduction interventions in low-and middle-income countries: a systematic review. BMC Med. 2019;17:1–18.
Hodge LM, Turner KM. Sustained implementation of evidence-based programs in disadvantaged communities: A conceptual framework of supporting factors. Am J Commun Psychol. 2016;58(1–2):192–210.
Frech S, et al. C/Can city Engagement process: an implementation framework for strengthening cancer care in cities in low-and middle-income countries. JCO Glob Oncol. 2021;7:901–16.
Iwelunmor J, et al. Toward the sustainability of health interventions implemented in sub-Saharan Africa: a systematic review and conceptual framework. Implement Sci. 2015;11(1):1–27.
Caldwell K, Henshaw L, Taylor G. Developing a framework for critiquing health research: an early evaluation. Nurse Educ Today. 2011;31(8):e1–7.
Creswell JW, Creswell JD. Research design: Qualitative, quantitative, and mixed methods approaches. Sage publications: 2017. http://www.ceil-conicet.gov.ar/wp-content/uploads/2015/10/Creswell-Cap-10.pdf.
Bergeron K, et al. Theories, models and frameworks used in capacity building interventions relevant to public health: a systematic review. BMC Public Health. 2017;17(1):1–12.
Lucas PJ, et al. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):1–7.
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9(1):1–11.
Wong G, et al. RAMESES publication standards: realist syntheses. BMC Med. 2013;11(1):1–14.
Jacobson N, Butterill D, Goering P. Development of a framework for knowledge translation: understanding user context. J Health Serv Res Pol. 2003;8(2):94–9.
Atkins L, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):1–18.
Birken SA, et al. Organizational theory for dissemination and implementation research. Implement Sci. 2017;12(1):1–15.
Hean S, et al. The contribution of theory to the design, delivery, and evaluation of interprofessional curricula: BEME Guide No 49. Med Teach. 2018;40(6):542–58.
Movsisyan A, et al. Adapting evidence-informed complex population health interventions for new contexts: a systematic review of guidance. Implement Sci. 2019;14(1):1–20.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7.
Davy C, et al. Factors influencing the implementation of chronic care models: a systematic literature review. BMC Fam Pract. 2015;16(1):1–12.
Stirman SW, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. 2019;14(1):1–10.
Simpson DD. A framework for implementing sustainable oral health promotion interventions. J Public Health Dentistry. 2011;71:S84–94.
Khalil H, Kynoch K. Implementation of sustainable complex interventions in health care services: the triple C model. BMC Health Serv Res. 2021;21(1):1–10.
Mendel P, et al. Interventions in organizational and community context: a framework for building evidence on dissemination and implementation in health services research. Admin Pol Mental Health Mental Health Serv Res. 2008;35(1–2):21–37.
Pfadenhauer LM, et al. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implement Sci. 2017;12(1):1–17.
Scott KA, Pringle J. The power of the frame: systems transformation framework for health care leaders. Nurs Adm Q. 2018;42(1):4–14.
Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Joint Commission J Qual Patient Safety. 2008;34(4):228–43.
Yamey G. Scaling up global health interventions: a proposed framework for success. Plos Med. 2011;8(6): e1001049.
Cooley L, Kohl R, Ved R. Scaling up—from vision to large-scale change: a management framework for practitioners. Washington, DC: Management Systems International; 2006.
Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Ann Rev Public Health. 2018;39:55–76.
Moullin JC, et al. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implement Sci. 2019;14(1):1–16.
De Silva MJ, et al. Theory of change: a theory-driven approach to enhance the Medical Research Council’s framework for complex interventions. Trials. 2014;15(1):1–13.
Stratil JM, Voss M, Arnold L. WICID framework version 1.0: criteria and considerations to guide evidence-informed decision-making on non-pharmacological interventions targeting COVID-19. BMJ Glob Health. 2020;5(11):e003699.
Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. 2013;103(6):e38–46.
Murray E, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8(1):1–11.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Admin Pol Mental Health Mental Health Serv Res. 2011;38(1):4–23.
McMullen H, et al. Explaining high and low performers in complex intervention trials: a new model based on diffusion of innovations theory. Trials. 2015;16(1):1–16.
Hockley J, et al. A framework for cross-cultural development and implementation of complex interventions to improve palliative care in nursing homes: the PACE steps to success programme. BMC Health Serv Res. 2019;19(1):1–11.
Artieta-Pinedo I, et al. Framework for the establishment of a feasible, tailored and effective perinatal education programme. BMC Pregn Childb. 2017;17(1):1–10.
Apostolopoulos Y, et al. Moving alcohol prevention research forward—part i: introducing a complex systems paradigm. Addiction. 2018;113(2):353–62.
Greene RA, et al. A person-focused model of care for the twenty-first century: a system-of-systems perspective. Popul Health Manage. 2014;17(3):166–71.
Beets MW, et al. Translating policies into practice: a framework to prevent childhood obesity in afterschool programs. Health Promot Pract. 2013;14(2):228–37.
Barker PM, Reid A, Schall MW. A framework for scaling up health interventions: lessons from large-scale improvement initiatives in Africa. Implement Sci. 2015;11(1):1–11.
Bradley EH, et al. A model for scale up of family health innovations in low-income and middle-income settings: a mixed methods study. BMJ Open. 2012;2(4): e000987.
Hirschhorn LR, et al. Development and application of a hybrid implementation research framework to understand success in reducing under-5 mortality in Rwanda. Gates Open Res. 2021;5:72.
Singh NS, et al. A tale of ‘politics and stars aligning’: analysing the sustainability of scaled up digital tools for front-line health workers in India. BMJ Glob Health. 2021;6(Suppl 5):e005041.
Greenhalgh T, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Int Res. 2017;19(11): e367.
James HM, et al. Spread, scale-up, and sustainability of video consulting in health care: systematic review and synthesis guided by the NASSS framework. J Med Int Res. 2021;23(1):e23775.
Kristensen FB, et al. European network for Health Technology Assessment, EUnetHTA: Planning, development, and implementation of a sustainable European network for Health Technology Assessment. Int J Technol Asses Health Care. 2009;25(S2):107–16.
Greenhalgh T, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quart. 2004;82(4):581–629.
Raab J. Interorganizational Networks. In: Alhajj R, Rokne J. (eds) Encyclopedia of Social Network Analysis and Mining. Springer: New York; 2018. https://doi.org/10.1007/978-1-4939-7131-2_369.
Simpson DD. A conceptual framework for transferring research to practice. J Subst Abuse Treat. 2002;22(4):171–82.
University; T. Why Healthcare Advocacy Is Important. 2021. https://publichealth.tulane.edu/blog/healthcare-advocacy/.
Yano EM. The role of organizational research in implementing evidence-based practice: QUERI Series. Implement Sci. 2008;3(1):1–15.
Aarons GA. Transformational and transactional leadership: Association with attitudes toward evidence-based practice. Psychiatric Services. 2006;57(8):1162–9.
Aarons GA, et al. Expanding the domains of attitudes towards evidence-based practice: the evidence based practice attitude scale-50. Admin Pol Mental Health Mental Health Serv Res. 2012;39(5):331–40.
Armenakis AA, et al. Organizational change recipients’ beliefs scale: development of an assessment instrument. J Appl Behav Sci. 2007;43(4):481–505.
Glisson C, et al. Assessing the organizational social context (OSC) of mental health services: Implications for research and practice. Admin Pol Mental Health Mental Health Serv Res. 2008;35(1–2):98.
Cohen, Levinthal. "Absorptive capacity: A new perspective on learning and innovation", Administrative Science Quarterly. 1990;35(1):128–52.
Patterson F, Ferguson E, Thomas S. Using job analysis to identify core and specific competencies: implications for selection and recruitment. Med Educ. 2008;42(12):1195–204.
Prennushi G, Rubio G, Subbarao K. Monitoring and evaluation. A sourcebook for poverty reduction strategies. 2002;107–30.
Maidique MA. Entrepreneurs, champions, and technological innovation. Sloan Manage Rev. 1980;21(2):59–76.
Sunaert P, et al. Implementation of a program for type 2 diabetes based on the chronic care model in a hospital-centered health care system:" the Belgian experience". BMC Health Serv Res. 2009;9(1):1–14.
Hroscikoski MC, et al. Challenges of change: a qualitative study of chronic care model implementation. Ann Fam Med. 2006;4(4):317–26.
Rashed S, et al. Sustaining malaria prevention in Benin: local production of bednets. Health Pol Plann. 1997;12(1):67–76.
Osawa E, Kodama T, Kundishora E. Motivation and sustainability of care facilitators engaged in a community home-based HIV/AIDS program in Masvingo Province Zimbabwe. AIDS Care. 2010;22(7):895–902.
Humphries D, Gomez L, Hartwig K. Sustainability of NGO capacity building in southern Africa: successes and opportunities. Int J Health Plann Manage. 2011;26(2):e85–101.
Proctor E, et al. Intermediary/purveyor organizations for evidence-based interventions in the US child mental health: characteristics and implementation strategies. Implement Sci. 2019;14(1):1–14.
Simpson DD, Dansereau DF. Assessing organizational functioning as a step toward innovation. Sci Pract Perspect. 2007;3(2):20.
Shi J, Jiang C, Tan D, Yu D, Lu Y, Sun P, et al. Advancing Implementation of Evidence‐Based Public Health in China: An Assessment of the Current Situation and Suggestions for Developing Regions. BioMed Research International. 2016(1):2694030.
Lau WKR. Implementation of Complex Interventions in UK General Practice (Doctoral dissertation, UCL (University College London). UCL (University College London): 2018. https://discovery.ucl.ac.uk/id/eprint/10047560/1/Lau_10047560_thesis_volume%201_revised.pdf.
Mariani G, et al. Improving women’s health in low-income and middle-income countries. Part I: challenges and priorities. Nuclear Med Commun. 2017;38(12):1019.
Bhanbhro S, et al. Factors affecting maternal nutrition and health: a qualitative study in a matrilineal community in Indonesia. Plos one. 2020;15(6):e0234545.
Klaic M, et al. Implementability of healthcare interventions: an overview of reviews and development of a conceptual framework. Implement Sci. 2022;17(1):1–20.
Rogers EM, Singhal A, Quinlan MM. Diffusion of innovations. In An integrated approach to communication theory and research. Routledge: 2014;432–48.https://www.taylorfrancis.com/chapters/edit/10.4324/9780203887011-36/diffusion-innovations-everett-rogers-arvind-singhal-margaret-quinlan.
Sheeran P, Abraham C. The health belief model. Predict Health Behav. 1996;2:29–80.
Ajzen I. From intentions to actions: A theory of planned behavior. In: Action control. Springer; 1985. p. 11–39.
Weiner BJ, et al. The meaning and measurement of implementation climate. Implement Sci. 2011;6(1):1–12.
Acknowledgments
We gratefully acknowledge Prof. Andrew Booth and Dr. Katie Sworn their review of the manuscript and guidance on the systematic review process.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Funding
There was no funding source for this work.
Author information
Authors and Affiliations
Contributions
LS conceived the research questions and prepared the research protocol in conjunction with AB and KS. LS designed the study, conducted the literature searches, and analyses. AB and KS refined the research question, contributed to the study design, participated in the literature review, helped prepare the first draft and revisions. All authors read and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
I declare that i have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, L., Booth, A. & Sworn, K. Adaptability, Scalability and Sustainability (ASaS) of complex health interventions: a systematic review of theories, models and frameworks. Implementation Sci 19, 52 (2024). https://doi.org/10.1186/s13012-024-01375-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-024-01375-7