Abstract
Context
Resveratrol (RV), a natural compound found in grapes, berries, and peanuts, has been extensively studied for its potential in treating Alzheimer’s disease (AD). RV has shown promise in inhibiting the formation of beta-amyloid plaques (Aβ) and neurofibrillary tangles (NFTs), protecting against neuronal damage and oxidative stress, reducing inflammation, promoting neuroprotection, and improving the function of the blood–brain barrier (BBB). However, conflicting results have been reported, necessitating a comprehensive umbrella review of systematic reviews to provide an unbiased conclusion on the therapeutic effectiveness of RV in AD.
Objective
The objective of this study was to systematically synthesize and evaluate systematic and meta-analysis reviews investigating the role of RV in AD using data from both human and animal studies.
Data sources and extraction
Of the 34 systematic and meta-analysis reviews examining the association between RV and AD that were collected, six were included in this study based on specific selection criteria. To identify pertinent studies, a comprehensive search was conducted in English-language peer-reviewed journals without any restrictions on the publication date until October 15, 2023. The search was carried out across multiple databases, including Embase, MEDLINE (PubMed), Cochrane Library, Web of Science, and Google Scholar, utilizing appropriate terms relevant to the specific research field. The AMSTAR-2 and ROBIS tools were also used to evaluate the quality and risk of bias of the included systematic reviews, respectively. Two researchers independently extracted and analyzed the data, resolving any discrepancies through consensus. Of note, the study adhered to the PRIOR checklist.
Data analysis
This umbrella review presented robust evidence supporting the positive impacts of RV in AD, irrespective of the specific mechanisms involved. It indeed indicated that all six systematic and meta-analysis reviews unanimously concluded that the consumption of RV can be effective in the treatment of AD.
Conclusion
RV exhibits promising potential for benefiting individuals with AD through various mechanisms. It has been observed to enhance cognitive function, reduce Aβ accumulation, provide neuroprotection, protect the BBB, support mitochondrial function, facilitate synaptic plasticity, stabilize tau proteins, mitigate oxidative stress, and reduce neuroinflammation commonly associated with AD.
Graphical abstract

Similar content being viewed by others
Introduction
Alzheimer’s disease (AD), the primary cause of dementia accounting for 60% to 80% of cases [1,2,3], is a progressive neurological disorder characterized by the presence of abnormal protein deposits in the brain such as beta-amyloid (Aβ) plaques and neurofibrillary tangles (NFTs) composed of tau protein [4,5,6,7]. These deposits disrupt cellular processes, impair communication between neurons, and contribute to the degeneration and death of brain cells [6, 8], resulting in memory loss, cognitive decline, and behavioral changes [9, 10].
All currently approved medications for the treatment of AD were authorized more than a decade ago. The primary drugs used as initial treatment options are acetylcholinesterase (AChE) inhibitors, namely donepezil, rivastigmine, and galantamine. These medications work by blocking the breakdown of acetylcholine, a neurotransmitter that plays a role in memory and cognitive function [12,13,14]. They are utilized to alleviate cognitive impairment and slow down the progression of dementia in AD patients [15]. Memantine, an NMDA receptor antagonist, has been approved for moderate-to-severe AD [16, 17].
Most importantly, the US FDA has approved aduhelm (aducanumab) and Leqembi (lecanemab-irmb) for treating AD patients (see https://www.fda.gov/drugs/news-events-human-drugs/fdas-decision-approve-new-treatment-alzheimers-disease and https://www.fda.gov/news-events/press-announcements/fda-converts-novel-alzheimers-disease-treatment-traditional-approval), marking them medications to target Aβ in the brain. Despite doubts about their clinical efficacy, these monoclonal antibodies have shown to decline Aβ; as a result, reducing Aβ can reduce the clinical decline of AD [6, 18].
Various substances, including nutrients, are now recognized as effective in early stages of AD, supporting brain function and slowing down AD progression [6, 12, 13, 19, 20]. Resveratrol (RV), also known as 3,4′,5-trihydroxystilbene (chemical formula: C14H12O3), is an epitome of such substances. RV, a polyphenolic phytoalexin found in grapes, berries, and certain plants, has been linked to potential health benefits like neuroprotective and anti-inflammatory properties [26, 27]. RV exists in two forms, -trans and -cis isomers, and notably, previous studies have shown that trans-RV, found in higher concentrations than cis-RV in foods like grapes and wine [29,30,31], exhibits greater antioxidant and anti-inflammatory properties [32].
The notion that RV could serve as a therapeutic agent to manage the progression of AD has been influential in recent decades, prompting numerous researchers to investigate the potential role of RV in AD [33,34,35,36]. For instance, recent research indicates that RV may play a role in anti-amyloidogenic mechanisms, suggesting that natural or synthetic analogues may have therapeutic potential in AD [36]. RV may also potentially impact AD through its antioxidant, silent information regulator-1 (SIRT1)-activating [37], and anti-inflammatory properties [33], as well as its ability to regulate Aβ and tau protein, both of which are involved in the development of AD. RV has been suggested to offer neuroprotection, promote neurogenesis, [38], and mitigate oxidative stress in the brain to control AD [37]. Nevertheless, it is important to note that not all studies have reported promising results regarding the role of RV in AD. In fact, the findings from various studies are controversial, and some studies have not specifically reported a positive impact of RV on cognitive and memory performance, which are characteristics associated with AD [39, 40].
Given the foregoing debate regarding the role of RV in AD, numerous systematic reviews have been conducted. However, no comprehensive review has yet synthesized the relevant evidence, leaving the overall benefits of RV use for AD unclear. This means that no study has undertaken as a comprehensive review that incorporates a broad spectrum of relevant studies, diverse study designs, meticulous evidence analysis, inclusion of studies conducted on diverse populations, and a thorough assessment of the impact of RV on AD. Indeed, existing systematic reviews investigating the role of RV in AD exhibit limitations stemming from diverse study designs, participant characteristics, dosage regimens, treatment durations, and outcome measures. The variability in RV dosages and formulations, influenced by factors such as food intake and metabolism, introduces the possibility of inconsistent findings across studies. Additionally, some studies fail to adequately account for potential confounding factors, including genetic predisposition, coexisting medical conditions, and medication use, which can potentially modify the effects of RV. Therefore, our objective is to evaluate the strength and credibility of the evidence derived from systematic and meta-analysis reviews on RV intake in AD by conducting an umbrella review to reach a convergent conclusion.
Umbrella reviews offer a comprehensive synthesis of evidence by integrating findings from multiple systematic and meta-analysis reviews. They assess quality, identify discrepancies, and evaluate evidence strength, providing time and resource efficiency, supporting decision-making, identifying research gaps, and optimizing resource utilization. Indeed, umbrella reviews consolidate data from multiple systematic reviews on a specific topic, providing a comprehensive overview of the research domain. They have the ability to identify patterns, contradictions, or areas that may require further investigation, which individual reviews might overlook [41, 42].
This umbrella review will synthesize and analyze the available evidence, considering the diverse study designs, participant characteristics, dosage variations, treatment durations, and outcome measures reported in existing systematic reviews. By doing so, it aims to provide a more comprehensive understanding of the relationship between RV and AD, while also accounting for potential confounding factors. This umbrella review will analyze six systematic and meta-analysis reviews that investigated the relationship between RV and AD based on predefined selection criteria.
Methods and materials
This present umbrella review was conducted in accordance with the PRIOR (Preferred Reporting Items for Overviews of Reviews) guidelines [43]. The PRIOR checklist is presented in Additional file 1: Appendix 1.
Eligibility criteria
We included systematic and meta-analysis reviews that assessed the impact of RV on AD in both human and animal studies. We have included both animal and human studies in this review because it is crucial for the evaluation of interventions [44,45,46,47]. Animal studies provide valuable insights into mechanisms, efficacy, and safety, serving as a bridge between basic research and clinical applications [48, 49]. They offer predictive value by exploring intervention effects before testing them in humans [49]. Animal studies also help identify potential harms and safety concerns [50]. By understanding the underlying biological mechanisms through animal studies, researchers can develop targeted treatments for humans. Furthermore, including animal studies respects ethical boundaries and allows exploration of interventions that may not be feasible or ethical in humans [47, 51,52,53]. Thus, integrating animal and human studies in an umbrella review provides a more robust evidence base, supporting informed decision-making in both preclinical and clinical research.
We defined systematic reviews as peer-reviewed studies that follow a specific methodology, including having a clearly reported research question, conducting a systematic search of at least two databases, and performing systematic data synthesis. Importantly, those systematic reviews that followed the PRISMA guidelines were included. These reviews aim to provide a comprehensive and unbiased summary of existing evidence on a specific topic—the role of RV in AD. Additionally, the eligibility criteria used in other overviews of systematic reviews should be replicated to ensure consistency across different reviews. Certain types of reviews were excluded from the definition of systematic reviews: Reviews with only one author were excluded because systematic reviews typically involve a team of researchers working together to minimize bias and enhance reliability; reviews that searched only one database were also excluded, as this can lead to incomplete coverage of relevant studies.
Information sources and search strategy
We conducted an extensive search across multiple databases, including Embase, MEDLINE (PubMed), Cochrane Library, Web of Science, Epistemonikos, and Google Scholar, with the aim of finding relevant research. Studies must be written in English and published in peer-reviewed journals. The search was not restricted by the publication start date and covered until October 15, 2023. We utilized specific terms such as “resveratrol,” “wine,” “SIRT1 activator,” “3,5,4′-trihydroxy-trans-stilbene,” “cis- and trans-resveratrol,” “peanuts,” and “resveratrol supplement”. These terms were combined with keywords associated with “Alzheimer's disease,” “neurodegenerative conditions,” “cognitive function,” “beta-amyloid,” “neurofibrillary tangles,” “tau protein,” “systematic review,” and “meta-analysis”.
To clarify, we conducted thorough searches in mentioned databases by combining different terms. For instance, we explored “resveratrol” combined with “Alzheimer’s disease” in each database, then “resveratrol” combined with “neurodegenerative conditions”, and so forth. We experimented with diverse search methods, using quotation marks, Boolean operators and incorporating these terms into sentences. It is important to note that our searches were not limited to specific words; instead, these words were integral components of sentences crafted for each database. Additional file 2: Appendix 2 shows details of the search strategy used in the present umbrella review.
In addition to the database search, we conducted a thorough review of the reference lists in relevant review papers and papers that met our study entry criteria. This supplementary step enabled us to discover further published research by examining the references cited within those papers.
Selection process
We sorted the included reviews based on the population and intervention comparisons (known as PICOs) while ensuring adherence to the PRISMA guidelines [54]. In cases where multiple reviews addressed the same comparison for the same population, we prioritized the review with the most recent search date and completeness of the search, as well as the highest quality. To assess overlap, the first author (A.A.) extracted this information from the reviews, and the second author (F.A.) cross-verified the data. Additionally, we evaluated the methodological quality of the included reviews using a checklist specifically designed for systematic reviews called AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews) [55]. Both authors (A.A. and F.A.) independently assessed each publication and reached a consensus on the quality through discussions. Any studies that did not meet the criteria outlined in AMSTAR-2 were excluded from the analysis. The final decision on which reviews to include was made through agreement between two of the authors (A.A. and F.A.).
Data collection process
Two of the authors involved in the overview independently extracted data from each systematic review using an electronic form that was created and tested beforehand. Any disagreements that arose were resolved through consensus among the authors. In the event that inconsistent data were identified across the systematic reviews, our plan was to extract data from all the included reviews and address the discrepancies by contacting the authors of those reviews, retrieving primary studies from the included reviews, and searching relevant trial registries. We intended to discuss any potential discrepancies in the Results section of this umbrella review; however, it is worth noting that no inconsistent data were identified during the extraction process.
Data items, synthesis methods, risk of bias assessment
Research has been conducted on the connection between RV consumption and AD in both animal and human systematic reviews. Of these six systematic reviews [56,57,58,59,60,61], four were systematic reviews involving human subjects [56, 58, 60, 61], while two involved animal subjects [57, 59]. We excluded certain studies from the analysis for various reasons. Firstly, studies that assessed AD but focused on components other than RV due to lack of sufficient data were excluded. The presence of a confounder in this situation raises the question of whether RV has influenced AD symptoms or if other components have played a role. Additionally, studies that evaluated only SIRT1 or polyphenols and nutrients without any administration of RV were also excluded. The reason for this is that SIRT1 can be influenced by various other conditions and components [62,63,64], leading to potential bias. Furthermore, studies that examined wine but did not measure RV within them were excluded as well. This is because wine contains numerous other components that have been demonstrated to have similar effects as RV can [65].
To conduct the screening process, two authors independently reviewed the titles and abstracts of relevant publications. For doing so, we used both EPPI-Reviewer (version: 6.15.0.2) and Microsoft excel 2021; This enabled us to effectively remove duplicate records and perform subsequent screening. Any discrepancies or conflicts were carefully reviewed and reanalyzed in order to reach a resolution. Publications that raised doubts about their context or eligibility were included in the list for full-text screening.
In determining the risk of bias of a systematic review with meta-analysis, we relied on the Risk of Bias in Systematic Reviews (ROBIS) tool [66]. Specifically, we considered a systematic review with meta-analysis to be of high quality if it demonstrated low risk of bias in the first three domains of the ROBIS tool. These domains encompassed the specification of study eligibility (domain 1), the methods used to identify and select studies (domain 2), and the methods used to collect data and appraise studies (domain 3). In order to assess studies that required additional scrutiny, we employed the Cochrane “Risk of Bias” tool [67]. This tool provided a framework for a comprehensive evaluation of the potential biases present in those studies.
Results
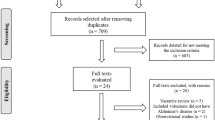
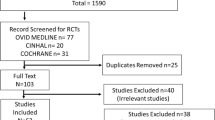
A total of 31 studies were collected through multiple databases, and three articles were found by carefully examining the reference lists of publications that had already been identified. Out of the total of 34 systematic reviews, we carefully selected only 6 for systematic evaluation. The reason for this selection was that some of the reviews failed to meet the inclusion criteria as determined by the AMSTAR-2 and ROBIS tools. Additionally, certain reviews did not adhere to the recommended PRISMA guidelines. Moreover, several reviews were found to be rife with confounding factors. For instance, these reviews examined the simultaneous administration of other components alongside RV, making it challenging to ascertain the precise impact of RV alone. Furthermore, some studies neglected to consider comorbid conditions when analyzing the effects of RV on AD patients. This introduced a potential bias, as the AD patients in question were also afflicted with other diseases or disorders such as stroke, depression, diabetes, and cardiovascular diseases, among others. Given this scenario, there are additional factors at play that can influence the impact of RV, thereby preventing us from reaching a definitive conclusion. Thus, six studies [56,57,58,59,60,61] were evaluated in this umbrella review. Figure 1 shows a flowchart of the selection of pertinent studies.
Out of these six studies [56,57,58,59,60,61], four were systematic reviews involving human subjects [56, 58, 60, 61], while two involved animal subjects’ systematic reviews [57, 59]. The methodological details of studies have been summarized in Table 1, which followed PICOS (Population, Intervention, Comparison, Outcomes, and Study) criteria.
Human systematic reviews
According to a systematic review of three randomized clinical trials, [56] RV and its metabolites have the potential to traverse the blood–brain barrier (BBB), potentially influencing cognitive function and brain metabolism. They discovered some exciting results, but there was no significant loss observed in a particular segment they were investigating. They also examined various biomarkers and found that while some of their trajectories or patterns had changed, there were no apparent treatment effects on specific factors related to AD, such as plasma plasma Aβ42, CSF Aβ42, CSF tau, CSF phosphotau 181, hippocampal volume, entorhinal cortex thickness, MMSE, CDR, ADAS-cog, NPI, glucose, or insulin metabolism The authors advise caution when interpreting the findings related to the altered biomarker trajectories, suggesting that further analysis and consideration are necessary. However, a pilot study conducted on individuals with mild cognitive decline in AD demonstrated positive outcomes in terms of cognitive function and brain metabolism. Additional studies suggest that RV may have the potential to seal a leaky BBB and contribute to cognitive and functional improvement in AD patients. In a proof-of-concept study, RV was found to reduce glycated hemoglobin (HbA1c), preserve hippocampal volume, and enhance hippocampal resting-state functional connectivity in individuals at risk for dementia [56].
Another systematic review reported that compared to the group receiving a placebo, the administration of RV demonstrated a mitigating effect on the decline of Mini-Mental State Examination (MMSE) scores, Alzheimer’s Disease Cooperative Study—Activities of Daily Living (ADCS-ADL) scores, and CSF Aβ42 levels over the course of the 52-week trial. However, there was no observed alteration in tau levels. Furthermore, RV and its primary metabolites were detectable in both plasma and CSF. The decline in CSF Aβ40 and plasma Aβ40 levels was more pronounced in the placebo group compared to the RV treatment group, resulting in a significant difference at week 52. This means that the levels of CSF Aβ40 and plasma Aβ40 in the placebo group decreased more significantly over time compared to the RV treatment group. Notably, there was a significant decrease in the mean values of the RV group when compared to the placebo group (p < 0.03) [60].
In addition, Kocatürk et al. 2022 found that administering 500 mg of RV for a duration of one year resulted in reductions in CSF Aβ40 and CSF Aβ42 levels, as well as a decrease in serum Aβ40 levels in individuals with AD [58]. Likewise, Xu Lou et al., 2023 reported that RV intake, irrespective of dosage, can enhance brain volume, reduce MMSE scores, and improve AD scores in AD patients. In individuals with mild cognitive impairment, RV prevents the decline in Standard Volumes of Interest and increases Resting-state Functional Connectivity scores. Moreover, the group receiving RV exhibited notable improvements, reflected in higher rates of improvement indicated by good rate, MMSE scores, and FIM scores (p < 0.05), as well as lower clinical indicators and ADAS-cog scores (p < 0.001). Additionally, trans-RV has demonstrated a neuroprotective effect in patients with mild to moderate AD, as evidenced by change scores on ADAS-cog, MMSE, ADCS-ADL, and NPI showing less deterioration in the treatment group compared to the control group, although none of the change scores reached statistical significance [61].
In summary, the potential outcomes of taking RV from these human systematic reviews [56, 58, 60, 61] are as follows:
-
Potential to traverse the BBB, influencing cognitive function and brain metabolism.
-
Positive outcomes in cognitive function and brain metabolism in individuals with mild cognitive decline in AD.
-
Mitigating effect on the decline of MMSE and ADCS-ADL scores in AD patients.
-
Reduction in CSF Aβ40 and plasma Aβ40 levels, while a more pronounced decline observed in the placebo group.
-
Reductions in CSF Aβ40, CSF Aβ42, and serum Aβ40 levels in individuals with AD.
-
Enhancements in brain volume and resting-state functional connectivity in AD patients and individuals with mild cognitive impairment.
-
Neuroprotective effect in patients with mild to moderate AD, while showing less deterioration in change scores on ADAS-cog, MMSE, ADCS-ADL, and NPI in the treatment group compared to the control group.
Animal systematic reviews
Two systematic reviews [57, 59] reported in this regard that RV supplementation provided protective benefits against memory loss and brain pathology in AD transgenic (3xTg-AD) mice, as well as improving cognitive function in healthy nontransgenic (NoTg) mice. In addition, RV reduced anxiety levels and the accumulation of Aβ and phosphorylated tau (p-tau) aggregates specifically in the hippocampus of 3xTg-AD mice. The beneficial effects of RV were attributed to its activation of AMP-activated protein kinase (AMPK), leading to the upregulation of SIRT1 and cAMP response element-binding protein (CREB) [68]. Furthermore, the findings indicated that RV effectively reduced inflammation in both rat astrocytes and N9 microglia cell lines, suggesting that targeting the NF-κB signaling pathway could be a significant approach in the treatment of AD [69].
In addition to such findings, a long-term dietary supplementation of RV (150 mg/kg per day) significantly enhanced cognitive abilities and decreased AD markers in the brains of SAMP8 mice. These markers included reduced levels of Aβ42, decreased p-tau, increased phosphorylation of glycogen synthase kinase 3β (GSK-3β) at Ser9, and decreased expression of TNFα, IL-6, and IL-1β [70]. Further, RV effectively reduced the levels of reactive oxygen species (ROS), indicating its potential in preventing cognitive decline and neurochemical changes. Not to mentioned that RV facilitated neural repair in the mouse model of AD [71]. Of note, RV-induced mitophagy, which a process that eliminates damaged mitochondria to maintain their quality, has a protective effect against oxidative damage caused by Aβ in PC12 cells in in vitro AD model [72].
In addition to the aforementioned, an animal systematic review [57] that assessed 19 animal studies reported that RV-fed mice, irrespective of dosage, showed significant declines in Aβ counts and burden in various brain regions, including the medial cortex, striatum, and hypothalamus. Additionally, RV-induced activation of SIRT1 decreased Aβ42 and Aβ40 (p < 0.05) accumulation in SAMP8 animals. The study also revealed that RV effectively sustained the integrity of the BBB and inhibited Aβ1–42 from crossing it and accumulating in the hippocampus. More interestingly, the group of mice treated with RV showed a noteworthy reduction in Aβ42 levels compared to the control group that received the vehicle treatment (p < 0.00001) [57].
In addition to the accumulation of Aβ in the brain, abnormalities in the tau protein are also considered a major factor in the development of AD [73]. Studies show RV reduces hyperphosphorylated tau levels in AD mice by decreasing CDK5 and GSK3β activity, preventing tau phosphorylation at Ser396, and lowering p-tau levels in the cortex (p < 0.01) and hippocampus (p < 0.05). Further, RV reverses SIRT1 inactivation and tau hyperphosphorylation in both rats and mice. This suggests that active SIRT1 plays a role in attenuating tau hyperphosphorylation by reducing ERK1/2 phosphorylation (p < 0.05) and regulating neuronal PP2A activity. Noteworthy, RV treatment demonstrated cognitive improvement in rats with early AD by reducing tau activity and the activity of the Aβ–caspase3–Akt–GSK-3β-tau pathway (p < 0.05). These findings suggest that RV holds promise as a potential therapeutic approach for AD [57].
In summary, the results of RV administration from these animal systematic and meta-analysis reviews [57, 59] are as follows:
-
Protective benefits against memory loss and brain pathology in 3xTg-AD.
-
Improved cognitive function in healthy NoTg.
-
Reduction in anxiety levels and accumulation of Aβ and p-tau aggregates in the hippocampus of 3xTg-AD mice.
-
Activation of AMPK, leading to upregulation of SIRT1 and CREB.
-
Reduction of inflammation in rat astrocytes and N9 microglia cell lines.
-
Enhanced cognitive abilities and decreased AD markers in the brains of SAMP8 mice, including reduced levels of Aβ42 and p-tau.
-
Decreased expression of TNFα, IL-6, and IL-1β in the brains of SAMP8 mice.
-
Reduction of ROS.
-
Facilitation of neural repair in a mouse model of AD.
-
Significant declines in Aβ counts and burden in various brain regions in RV-fed mice.
-
Sustained integrity of the BBB and inhibition of Aβ1–42 accumulation in the hippocampus.
-
Reduction of hyperphosphorylated tau levels in AD mice.
-
Reversal of SIRT1 inactivation and tau hyperphosphorylation in rats and mice.
-
Cognitive improvement in rats with early AD.
Table 2 provides a summary of the findings derived from both human and animal studies investigating the effects of RV intake in cases of AD.
Discussion
This comprehensive overview of six systematic reviews [56,57,58,59,60,61] examining the effects of RV in AD cases, both in humans and animals, reveals significant evidence supporting RV intake as a therapeutic or protective agent for individuals with AD. However, it should be noted that further studies with reduced limitations are necessary, as a few human studies have reported no significant effects of RV intake in AD protection.
Recent research suggests that RV may hold therapeutic potential for AD [33,34,35,36]. This is due to its ability to exert anti-amyloidogenic effects [74], provide neuroprotection [75], promote neurogenesis [76], and alleviate oxidative stress [77]. However, it is important to note that not all studies consistently report positive outcomes [39, 40]. Furthermore, existing systematic reviews on RV and AD face limitations, such as variations in study designs, participant characteristics, dosage regimens, treatment durations, and outcome measures. These limitations can introduce inaccuracies and potentially overlook confounding factors. Therefore, the objective of this study was to critically evaluate the evidence while addressing these limitations.
The question that arose was whether RV can have a positive impact on AD. After evaluation included studies [56,57,58,59,60,61], despite some limitations that will be discussed at the end of this section, we found that RV can show promise in various aspects of AD treatment. Indeed, all these studies mentioned that RV has protective effects against memory loss and cognitive decline, reduces AD-related markers such as Aβ and p-tau, and improves cognitive function and brain metabolism in AD cases. The forthcoming paragraphs will discuss the potential mechanisms through which RV can exert these effects.
Most studies suggest that RV has the ability to cross the BBB [78, 79], which is a protective barrier that separates the bloodstream from the brain. By traversing the BBB, RV can directly access the brain tissue and exert its effects. The presence of RV in the brain can influence cognitive function, which refers to various mental processes such as memory, attention, and problem-solving in AD cases [80]. Additionally, RV exhibits promising health advantages by stimulating AMPK within the brain [81, 82].
Research on the activation of AMPK by resveratrol has revealed a range of mechanisms, some of which appear intricate and occasionally conflicting. One of these mechanisms involves an increase in the ratio of AMP to ATP, as indicated by certain studies [83]. Additionally, other research suggests that the activation of AMPK by resveratrol relies on upstream serine/threonine kinases, such as LKB1 [81, 84], and calcium/calmodulin-dependent protein kinase kinase β (CaMKKβ) [85, 86]. Of interesting, it has been observed that RV can trigger AMPK independently of the AMP-to-ATP ratio [81]. This activation results in elevated glucose absorption [87, 88], improved mitochondrial function, [88], and the promotion of neuroprotective effects through anti-inflammatory action, enhanced autophagy, anti-oxidant activation through the Nrf2 pathway, and restoration of energy levels [89]. Therefore, RV’s ability to traverse the BBB is significant as it allows it to directly interact with the brain, potentially influencing cognitive function and brain metabolism.
Aβ peptides are a group of peptides involved in the formation of amyloid plaques in neurodegenerative diseases like AD [90]. The main types of Aβ peptides include Aβ40, Aβ42, and Aβ38, with Aβ42 being more prone to aggregation and considered more toxic [91]. Aβ43 and other variants like Aβ37, Aβ39, Aβ45, and Aβ46 also exist but are less common [92, 93]. The relative levels and aggregation properties of these peptides are believed to play a role in the development and progression of AD, though their exact mechanisms are still being studied [94].
Analyzed human systematic reviews suggest that RV can lead to a reduction in CSF Aβ40 and Aβ42 levels, as well as serum Aβ40 levels, in individuals with AD. The precise mechanisms by which RV can do so is not fully understood; yet one of which is that RV may modulate amyloid precursor protein (APP) processing and favor the non-amyloidogenic pathway, thus reducing the production of Aβ40 and Aβ42 peptides [85, 95]. APP is a protein found in cell membranes that is involved in normal brain function. However, in AD, there is a disturbance in the processing of APP, resulting in the accumulation of Aβ peptides, including Aβ40 and Aβ42, which are the hallmark of AD [96]. APP can be processed through two main pathways: The amyloidogenic pathway and the non-amyloidogenic pathway. In the amyloidogenic pathway, APP is cleaved by enzymes called β-secretases (such as β-secretase 1, or BACE1) and γ-secretases, resulting in the production of Aβ peptides [97, 98].
RV has been suggested to modulate APP processing and promote mostly the non-amyloidogenic pathway. The non-amyloidogenic pathway involves the cleavage of APP by α-secretase, which prevents the formation of Aβ peptides [99, 100]. RV has been proposed to boost the activity of α-secretase, an enzyme involved in the non-amyloidogenic cleavage of APP. When α-secretase activity is increased, it cleaves APP within the Aβ region, preventing the formation of Aβ peptides. As a result, there is a decrease in the production of Aβ40 and Aβ42, which are associated with the development of amyloid plaques in AD [101, 102]. Notably, RV can upregulate the expression of α-secretase while downregulating the expression of β-secretase. This modulation of secretase enzyme expression favors the non-amyloidogenic pathway and reduces Aβ production [103].
Of note, a study reported that RV does not affect the levels of APP holoprotein and its C-terminal proteolytic fragments, these data indicate that RV does not target an Aβ-producing activity, but rather promotes Aβ clearance [95]. Indeed, this study pointed out that RV does not hinder the production of Aβ, as it does not interfere with the enzymes responsible for generating Aβ, namely β-secretase and γ-secretase. Instead, RV facilitates the breakdown of Aβ within cells through a mechanism that involves the proteasome [95, 104]. Further research is needed to elucidate the detailed mechanisms of RV in modulating APP processing and thus reducing Aβ peptides in the context of AD.
In addition to the aforementioned, RV has been shown to upregulate SIRT1 in normal and AD cases [105, 106]. SIRT1, a sirtuin protein primarily found in neurons’ nuclei, dynamically regulates cellular processes such as aging, metabolism, and neuroprotection [107, 108]. Patients with AD and mild cognitive impairment have been found to exhibit lower levels of SIRT1 compared to healthy individuals [109], indicating that measuring serum SIRT1 levels could potentially serve as an early biomarker for AD diagnosis. In animal models of AD, the accumulation of Aβ was shown to suppress SIRT1 levels, whereas the administration of RV, a compound that activates SIRT1, significantly reduced Aβ deposition in the brain [110]. SIRT1 activation enhances the production of ADAM10, an enzyme that promotes the breakdown of APP through α-secretase activity, resulting in decreased Aβ levels in mouse brain tissue affected by AD [111]. Moreover, SIRT1 reduces the activity of ROCK1 and BACE1, leading to reduced Aβ levels [112]. For instance, in AD monkey models, interventions such as calorie restriction and SIRT1 overexpression were associated with lower brain Aβ levels, which correlated inversely with SIRT1 levels [113]. A recent study also supports the role of SIRT1 in activating α-secretase and further inhibiting Aβ production [114]. Together, these findings highlight the potential of SIRT1 as both a therapeutic target and a biomarker for AD.
In the context of AD, SIRT1 has garnered significant interest due to its involvement in pathways related to the disease’s development and progression. These pathways, along with involving Aβ metabolism, include the regulation of tau phosphorylation [115, 116], modulation of inflammation [117,118,119], mitigation of oxidative stress [120], and regulation of synaptic plasticity [121]. (For further gaining information about the role of SRIT1 in brain cells, see [106]) (Fig. 2).
Activation of SIRT1 through RV has exhibited a range of potential benefits in brain cells. These benefits encompass neuroprotection against degeneration, increased neuronal survival, improved synaptic plasticity, anti-inflammatory properties, and enhanced blood flow and neurovascular health. RV-induced SIRT1 activation aids in reducing oxidative stress, enhancing mitochondrial function, and facilitating the clearance of toxic protein aggregates like Aβ plaques and tau tangles. Furthermore, SIRT1 plays a critical role in regulating synaptic plasticity and neurogenesis for optimal learning and memory, in particular among those who suffering from AD
As per these analyzed systematic reviews, it was indicated that RV has a potential to activate SIRT1; indeed, RV can interact directly with SIRT1 and stimulate its enzymatic activity related to SIRT1 [57, 59]. Upon the whole, RV has the potential to activate SIRT1 by directly interacting with the protein and enhancing its enzymatic activity, thereby providing beneficial in preventing AD.
Another probable mechanism is that RV activates CREB [122, 123], a transcription factor involved in memory formation and neuronal plasticity, potentially enhancing cognitive function in AD cases [124, 125]. RV stimulates the activation of CREB signaling pathways by regulating levels of cAMP [122]. This activation leads to the transcription and expression of genes related to synaptic plasticity, neuronal survival, and memory formation [122, 126, 127]. Increasing the expression of genes like brain-derived neurotrophic factor (BDNF) and its receptor TrkB, RV enhances synaptic plasticity and potentially improves cognitive function in AD cases [128,129,130]. Of note, progression of AD is accompanied by reduced levels of BDNF in the brain [131], blood [132], and CSF [133] of AD patients. Conversely, higher levels of BDNF in the blood have been correlated with improved cognitive function in individuals with AD [134].
Limitations
This umbrella review on the role of RV in AD has several limitations that should be acknowledged. First, the included studies encompass a diverse range of study designs, such as randomized controlled trials, observational studies, and preclinical experiments. This variation introduces heterogeneity in the results, making it challenging to draw definitive conclusions. Differences in participant characteristics, RV dosage, treatment duration, and outcome measures across studies further contribute to the heterogeneity, limiting the ability to pool data and perform quantitative analyses.
Another limitation is the variability in RV dosages and formulations used across studies. Factors such as food intake and individual variations in metabolism can influence the absorption and bioavailability of RV [135,136,137]. This variability in RV dosages and formulations may contribute to inconsistent findings across studies and hinder the ability to determine the precise effects of RV on AD. The lack of standardized dosing protocols for RV limits the comparability and generalizability of the results.
Some studies included in this umbrella review did not fully account for potential confounding factors that could influence the effects of RV on AD. Factors such as genetic predisposition, coexisting medical conditions, and concomitant medication use may interact with RV and modify its effects [32, 138]. The heterogeneity in participant characteristics across studies may introduce confounding variables that are not adequately controlled for, thus limiting the ability to attribute observed effects solely to RV.
Notwithstanding these limitations, this umbrella review offers important insights into the current evidence regarding the involvement of RV in AD. However, it is crucial for future research to address the limitations identified in order to enhance the quality and applicability of the evidence. This will ultimately contribute to the development of RV-based interventions for the prevention and treatment of AD. As a result, researchers can improve the credibility and trustworthiness of the evidence, leading to more informed decision-making when considering the potential use of RV in managing AD.
Conclusion
Taken together, this umbrella review of systematic reviews aimed to evaluate the potential impact of RV on AD. We found that RV may hold potential as a beneficial treatment for AD, based on evidence from both human and animal studies. One key factor that contributes to its effectiveness is RV’s ability to cross the BBB, allowing it to directly impact cognitive function and brain metabolism. RV achieves this by modulating AMPK and influencing the processing of APP. Through this modulation, RV helps reduce the accumulation of Aβ peptides and tau proteins, which are characteristic of AD. Additionally, RV has been found to increase the levels of SIRT1, CREB, and BDNF, which are proteins associated with neuronal health and protection. These combined effects make RV a promising therapeutic agent for the treatment and prevention of AD.
Availability of data and materials
The search method, list of papers that were included and excluded, the data extraction process, and the quality evaluation are all accessible in the paper and upon reasonable request from the corresponding author.
Abbreviations
- AD:
-
Alzheimer’s disease
- Aβ:
-
Beta-amyloid plaques
- NFTs:
-
Neurofibrillary tangles
- AChE:
-
Acetylcholinesterase
- RV:
-
Resveratrol
- SIRT1:
-
Silent Information Regulator-1
- MMSE:
-
Mini-Mental State Examination
- ADCS-ADL:
-
Alzheimer’s Disease Cooperative Study—Activities of Daily Living
- p-tau:
-
Phosphorylated Tau
- AMPK:
-
AMP-activated protein kinase
- CREB:
-
CAMP Response Element-Binding Protein
- GSK-3β:
-
Glycogen Synthase Kinase 3β
- ROS:
-
Reactive oxygen species
- APP:
-
Amyloid precursor protein
- BDNF:
-
Brain-derived Neurotrophic Factor
References
2021 Alzheimer’s disease facts and figures. Alzheimers Dement. 2021;17(3):327–406. https://doi.org/10.1002/alz.12328.
Sosa-Ortiz AL, Acosta-Castillo I, Prince MJ. Epidemiology of dementias and Alzheimer’s disease. Arch Med Res. 2012;43(8):600–8.
Kamboh MI. Genomics and functional genomics of Alzheimer’s disease. Neurotherapeutics. 2023;19(1):152–72.
Aa R. Risk factors for Alzheimer’s disease. Folia Neuropathol. 2019;57(2):87–105. https://doi.org/10.5114/fn.2019.85929.
Kandimalla R, Reddy PH. Therapeutics of neurotransmitters in Alzheimer’s disease. J Alzheimers Dis. 2017;57(4):1049–69. https://doi.org/10.3233/jad-161118.
Azargoonjahromi A. Dual role of nitric oxide in Alzheimer’s disease. Nitric Oxide. 2023;134–135:23–37. https://doi.org/10.1016/j.niox.2023.03.003.
Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med. 2011;1(1): a006189. https://doi.org/10.1101/cshperspect.a006189.
Zhang H, Wei W, Zhao M, Ma L, Jiang X, Pei H, et al. Interaction between Aβ and Tau in the Pathogenesis of Alzheimer’s Disease. Int J Biol Sci. 2021;17(9):2181–92. https://doi.org/10.7150/ijbs.57078.
Terry RD, Davies P. Dementia of the Alzheimer type. Annu Rev Neurosci. 1980;3(1):77–95.
DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener. 2019;14(1):32. https://doi.org/10.1186/s13024-019-0333-5.
Klein E, Daza NM, Dasgupta I, MacDuffie K, Schönau A, Flynn G, et al. Views of stakeholders at risk for dementia about deep brain stimulation for cognition. Brain Stimul. 2023;16(3):742–7.
Cummings J, Lee G, Ritter A, Sabbagh M, Zhong K. Alzheimer’s disease drug development pipeline: 2020. Alzheimer’s & Dementia: Translational Research & Clinical Interventions. 2020;6(1): e12050.
Yiannopoulou KG, Papageorgiou SG. Current and future treatments in Alzheimer disease: an update. J Cent Nerv Syst Disease. 2020;12:1179573520907397.
Marucci G, Buccioni M, Ben DD, Lambertucci C, Volpini R, Amenta F. Efficacy of acetylcholinesterase inhibitors in Alzheimer’s disease. Neuropharmacology. 2021;190: 108352. https://doi.org/10.1016/j.neuropharm.2020.108352.
Jackson S, Ham RJ, Wilkinson D. The safety and tolerability of donepezil in patients with Alzheimer’s disease. Br J Clin Pharmacol. 2004;58:1–8.
Witt A, Macdonald N, Kirkpatrick P. Memantine hydrochloride. Nat Rev Drug Discov. 2004;3(2):109–10.
Tang B-C, Wang Y-T, Ren J. Basic information about memantine and its treatment of Alzheimer’s disease and other clinical applications. Ibrain. 2023;9(3):340–8. https://doi.org/10.1002/ibra.12098.
O’Gorman J, Chiao P, Bussière T, von Rosenstiel P, Tian Y, Zhu Y, et al. Clinical Development of Aducanumab, an Anti-Aβ Human Monoclonal Antibody Being Investigated for the Treatment of Early Alzheimer’s Disease. The journal of prevention of Alzheimer’s disease. 2017;4(4):255–63.
Arora S, Santiago JA, Bernstein M, Potashkin JA. Diet and lifestyle impact the development and progression of Alzheimer’s dementia. Front Nutr. 2023. https://doi.org/10.3389/fnut.2023.1213223.
Cremonini AL, Caffa I, Cea M, Nencioni A, Odetti P, Monacelli F. Nutrients in the prevention of Alzheimer’s disease. Oxid Med Cell Longev. 2019;2019:9874159. https://doi.org/10.1155/2019/9874159.
Cole GM, Ma QL, Frautschy SA. Omega-3 fatty acids and dementia. Prostaglandins Leukot Essent Fatty Acids. 2009;81(2–3):213–21. https://doi.org/10.1016/j.plefa.2009.05.015.
Li J, Sun M, Cui X, Li C. Protective effects of flavonoids against Alzheimer’s disease: Pathological hypothesis, potential targets, and structure-activity relationship. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms231710020.
Bukhari SNA. Dietary polyphenols as therapeutic intervention for Alzheimer’s disease: A mechanistic insight. Antioxidants (Basel). 2022. https://doi.org/10.3390/antiox11030554.
Colizzi C. The protective effects of polyphenols on Alzheimer’s disease: A systematic review. Alzheimers Dement (N Y). 2019;5:184–96. https://doi.org/10.1016/j.trci.2018.09.002.
Mielech A, Puścion-Jakubik A, Markiewicz-Żukowska R, Socha K. Vitamins in Alzheimer’s disease-review of the latest reports. Nutrients. 2020. https://doi.org/10.3390/nu12113458.
Zhang L-X, Li C-X, Kakar MU, Khan MS, Wu P-F, Amir RM, et al. Resveratrol (RV): A pharmacological review and call for further research. Biomed Pharmacother. 2021;143: 112164. https://doi.org/10.1016/j.biopha.2021.112164.
Koushki M, Amiri-Dashatan N, Ahmadi N, Abbaszadeh HA, Rezaei-Tavirani M. Resveratrol: A miraculous natural compound for diseases treatment. Food Sci Nutr. 2018;6(8):2473–90. https://doi.org/10.1002/fsn3.855.
Tian B, Liu J. Resveratrol: A review of plant sources, synthesis, stability, modification and food application. J Sci Food Agric. 2020;100(4):1392–404. https://doi.org/10.1002/jsfa.10152.
Goldberg DM, Ng E, Yan J, Karumanchiri A, Soleas G, Diamandis EP. Regional differences in resveratrol isomer concentrations of wines from various cultivars. J Wine Res. 1996;7:13–24.
Ramona C, Olteanu I, Mitruț P, Cichi DD, Cichi M. Study concerning the content in trans and cis—Res veratrol at the grapes Variety. 2007.
Revel G, Hogg TA, Santos CId. Analysis of cis - and trans -resveratrol in Portuguese wines. OENO One. 1996;30:31–7.
Salehi B, Mishra AP, Nigam M, Sener B, Kilic M, Sharifi-Rad M, et al. Resveratrol: a double-edged sword in health benefits. Biomedicines. 2018. https://doi.org/10.3390/biomedicines6030091.
Sawda C, Moussa C, Turner RS. Resveratrol for Alzheimer’s disease. Ann N Y Acad Sci. 2017;1403(1):142–9.
Vingtdeux V, Dreses-Werringloer U, Zhao H, Davies P, Marambaud P. Therapeutic potential of resveratrol in Alzheimer’s disease. BMC Neurosci. 2008;9:1–5.
Anekonda TS. Resveratrol—A boon for treating Alzheimer’s disease? Brain Res Rev. 2006;52(2):316–26. https://doi.org/10.1016/j.brainresrev.2006.04.004.
Jalili C, Kiani A, Gholami M, Bahrehmand F, Fakhri S, Kakehbaraei S, Kakebaraei S. Brain targeting based nanocarriers loaded with resveratrol in Alzheimer’s disease: a review. IET Nanobiotechnol. 2023;17(3):154–70. https://doi.org/10.1049/nbt2.12127.
Gomes BAQ, Silva JPB, Romeiro CFR, Dos Santos SM, Rodrigues CA, Gonçalves PR, et al. Neuroprotective mechanisms of resveratrol in Alzheimer’s disease: role of SIRT1. Oxid Med Cell Longev. 2018;2018:8152373. https://doi.org/10.1155/2018/8152373.
Kodali M, Parihar VK, Hattiangady B, Mishra V, Shuai B, Shetty AK. Resveratrol prevents age-related memory and mood dysfunction with increased hippocampal neurogenesis and microvasculature and reduced glial activation. Sci Rep. 2015;5(1):8075. https://doi.org/10.1038/srep08075.
Farzaei MH, Rahimi R, Nikfar S, Abdollahi M. Effect of resveratrol on cognitive and memory performance and mood: a meta-analysis of 225 patients. Pharmacol Res. 2018;128:338–44.
Khorshidi F, Poljak A, Liu Y, Lo JW, Crawford JD, Sachdev PS. Resveratrol: A “miracle” drug in neuropsychiatry or a cognitive enhancer for mice only? A systematic review and meta-analysis. Ageing Res Rev. 2021;65: 101199.
Choi GJ, Kang H. Introduction to umbrella reviews as a useful evidence-based practice. J Lipid Atheroscler. 2023;12(1):3–11. https://doi.org/10.12997/jla.2023.12.1.3.
Papatheodorou S, Evangelou E. Umbrella Reviews: What They Are and Why We Need Them. 2022. p. 135–46.
Michelle G, Allison G, Dawid P, Ricardo MF, Andrea CT, David M, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378: e070849. https://doi.org/10.1136/bmj-2022-070849.
Pound P, Ritskes-Hoitinga M. Can prospective systematic reviews of animal studies improve clinical translation? J Transl Med. 2020;18(1):15. https://doi.org/10.1186/s12967-019-02205-x.
Ritskes-Hoitinga M, Leenaars M, Avey M, Rovers M, Scholten R. Systematic reviews of preclinical animal studies can make significant contributions to health care and more transparent translational medicine. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.ED000078.
Perel P, Roberts I, Sena E, Wheble P, Briscoe C, Sandercock P, et al. Comparison of treatment effects between animal experiments and clinical trials: systematic review. BMJ. 2007;334(7586):197. https://doi.org/10.1136/bmj.39048.407928.BE.
Bahadoran Z, Mirmiran P, Kashfi K, Ghasemi A. Importance of systematic reviews and meta-analyses of animal studies: challenges for animal-to-human translation. J Am Assoc Lab Anim Sci. 2020. https://doi.org/10.30802/AALAS-JAALAS-19-000139.
Domínguez-Oliva A, Hernández-Ávalos I, Martínez-Burnes J, Olmos-Hernández A, Verduzco-Mendoza A, Mota-Rojas D. The importance of animal models in biomedical research: current insights and applications. Animals (Basel). 2023. https://doi.org/10.3390/ani13071223.
Regenberg A, Mathews DJ, Blass DM, Bok H, Coyle JT, Duggan P, et al. The role of animal models in evaluating reasonable safety and efficacy for human trials of cell-based interventions for neurologic conditions. J Cereb Blood Flow Metab. 2009;29(1):1–9. https://doi.org/10.1038/jcbfm.2008.98.
Spielmann H. Animal use in the safety evaluation of chemicals: harmonization and emerging needs. ILAR J. 2002;43(Suppl_1):S11–7. https://doi.org/10.1093/ilar.43.Suppl_1.S11.
Kiani AK, Pheby D, Henehan G, Brown R, Sieving P, Sykora P, et al. Ethical considerations regarding animal experimentation. J Prev Med Hyg. 2022;63(2 Suppl 3):E255–66. https://doi.org/10.15167/2421-4248/jpmh2022.63.2S3.2768.
López-Cepero J. Current status of animal-assisted interventions in scientific literature: a critical comment on their internal validity. Animals (Basel). 2020. https://doi.org/10.3390/ani10060985.
Hamilton-Bruce m, Hazel S, Krawczyk V, Milton A, Koblar S. Exploration of ethological issues in Animal Assisted Interventions (AAI) for stroke sufferers: Recommendations for action. 2014.
Matthew JP, Joanne EM, Patrick MB, Isabelle B, Tammy CH, Cynthia DM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Beverley JS, Barnaby CR, George W, Micere T, Candyce H, Julian M, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358: j4008. https://doi.org/10.1136/bmj.j4008.
Buglio DS, Marton LT, Laurindo LF, Guiguer EL, Araújo AC, Buchaim RL, et al. The role of resveratrol in mild cognitive impairment and Alzheimer’s disease: a systematic review. J Med Food. 2022;25(8):797–806. https://doi.org/10.1089/jmf.2021.0084.
Chen J-Y, Zhu Q, Zhang S, OuYang D, Lu J-H. Resveratrol in experimental Alzheimer’s disease models: a systematic review of preclinical studies. Pharmacol Res. 2019;150: 104476. https://doi.org/10.1016/j.phrs.2019.104476.
Kocatürk RR, Temizyürek A, Özcan ÖÖ, Ergüzel TT, Karahan M, Konuk M, Tarhan N. Effect of nutritional supports on malnutrition, cognition, function and biomarkers of Alzheimer’s disease: a systematic review. Int J Neurosci. 2022. https://doi.org/10.1080/00207454.2022.2079506.
Komorowska J, Wątroba M, Szukiewicz D. Review of beneficial effects of resveratrol in neurodegenerative diseases such as Alzheimer’s disease. Adv Med Sci. 2020;65(2):415–23. https://doi.org/10.1016/j.advms.2020.08.002.
Tosatti JAG, Fontes AFdS, Caramelli P, Gomes KB. Effects of resveratrol supplementation on the cognitive function of patients with Alzheimer's disease: a systematic review of randomized controlled trials. Drugs Aging. 2022;39(4):285–95. https://doi.org/10.1007/s40266-022-00923-4.
Xu Lou I, Ali K, Chen Q. Effect of nutrition in Alzheimer’s disease: a systematic review. Front Neurosci. 2023. https://doi.org/10.3389/fnins.2023.1147177.
Zendedel E, Butler AE, Atkin SL, Sahebkar A. Impact of curcumin on sirtuins: a review. J Cell Biochem. 2018;119(12):10291–300. https://doi.org/10.1002/jcb.27371.
García-Martínez JM, Chocarro-Calvo A, Martínez-Useros J, Fernández-Aceñero MJ, Fiuza MC, Cáceres-Rentero J, et al. Vitamin D induces SIRT1 activation through K610 deacetylation in colon cancer. Elife. 2023. https://doi.org/10.7554/eLife.86913.
Yang Y, Liu Y, Wang Y, Chao Y, Zhang J, Jia Y, et al. Regulation of SIRT1 and its roles in inflammation. Front Immunol. 2022;13: 831168. https://doi.org/10.3389/fimmu.2022.831168.
Buljeta I, Pichler A, Šimunović J, Kopjar M. Beneficial effects of red wine polyphenols on human health: comprehensive review. Curr Issues Mol Biol. 2023;45(2):782–98. https://doi.org/10.3390/cimb45020052.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34. https://doi.org/10.1016/j.jclinepi.2015.06.005.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
Corpas R, Griñán-Ferré C, Rodríguez-Farré E, Pallàs M, Sanfeliu C. Resveratrol induces brain resilience against Alzheimer neurodegeneration through proteostasis enhancement. Mol Neurobiol. 2019;56(2):1502–16. https://doi.org/10.1007/s12035-018-1157-y.
Zhao H, Wang Q, Cheng X, Li X, Li N, Liu T, et al. Inhibitive effect of resveratrol on the inflammation in cultured astrocytes and microglia induced by Aβ1–42. Neuroscience. 2018;379:390–404. https://doi.org/10.1016/j.neuroscience.2018.03.047.
Chen ZJ, Yang YF, Zhang YT, Yang DH. Dietary total prenylflavonoids from the fruits of Psoralea corylifolia L. prevents age-related cognitive deficits and down-regulates Alzheimer’s markers in SAMP8 mice. Molecules. 2018. https://doi.org/10.3390/molecules23010196.
Wang X, Ma S, Yang B, Huang T, Meng N, Xu L, et al. Resveratrol promotes hUC-MSCs engraftment and neural repair in a mouse model of Alzheimer’s disease. Behav Brain Res. 2018;339:297–304. https://doi.org/10.1016/j.bbr.2017.10.032.
Wang H, Jiang T, Li W, Gao N, Zhang T. Resveratrol attenuates oxidative damage through activating mitophagy in an in vitro model of Alzheimer’s disease. Toxicol Lett. 2018;282:100–8. https://doi.org/10.1016/j.toxlet.2017.10.021.
Medeiros R, Baglietto-Vargas D, LaFerla FM. The role of tau in Alzheimer’s disease and related disorders. CNS Neurosci Ther. 2011;17(5):514–24. https://doi.org/10.1111/j.1755-5949.2010.00177.x.
Vingtdeux V, Dreses-Werringloer U, Zhao H, Davies P, Marambaud P. Therapeutic potential of resveratrol in Alzheimer’s disease. BMC Neurosci. 2008;9(2):S6. https://doi.org/10.1186/1471-2202-9-S2-S6.
Rahman MH, Akter R, Bhattacharya T, Abdel-Daim MM, Alkahtani S, Arafah MW, et al. Resveratrol and neuroprotection: impact and Its therapeutic potential in Alzheimer’s disease. Front Pharmacol. 2020;11: 619024. https://doi.org/10.3389/fphar.2020.619024.
Wang R, Wu Z, Bai L, Liu R, Ba Y, Zhang H, et al. Resveratrol improved hippocampal neurogenesis following lead exposure in rats through activation of SIRT1 signaling. Environ Toxicol. 2021;36(8):1664–73. https://doi.org/10.1002/tox.23162.
Sarubbo F, Tejada S, Esteban S, Jimenez-García M, Moranta D. Chapter 33 - Resveratrol, SIRT1, oxidative stress, and brain aging. In: Preedy VR, Patel VB, editors. Aging (Second Edition). Academic Press; 2020. p. 319–26.
Lin Y-L, Chang H-C, Chen T-L, Chang J-H, Chiu W-T, Lin J-W, Chen R-M. Resveratrol protects against oxidized LDL-induced breakage of the blood-brain barrier by lessening disruption of tight junctions and apoptotic insults to mouse cerebrovascular endothelial cells. J Nutr. 2010;140(12):2187–92.
Wang Q, Xu J, Rottinghaus GE, Simonyi A, Lubahn D, Sun GY, Sun AY. Resveratrol protects against global cerebral ischemic injury in gerbils. Brain Res. 2002;958(2):439–47. https://doi.org/10.1016/S0006-8993(02)03543-6.
Bastianetto S, Ménard C, Quirion R. Neuroprotective action of resveratrol. Biochimica et Biophysica Acta (BBA) Molecular Basis of Disease. 2015;1852(6):1195–201. https://doi.org/10.1016/j.bbadis.2014.09.011.
Dasgupta B, Milbrandt J. Resveratrol stimulates AMP kinase activity in neurons. Proc Natl Acad Sci. 2007;104(17):7217–22. https://doi.org/10.1073/pnas.0610068104.
Pineda-Ramírez N, Alquisiras-Burgos I, Ortiz-Plata A, Ruiz-Tachiquín ME, Espinoza-Rojo M, Aguilera P. Resveratrol activates neuronal autophagy through AMPK in the ischemic brain. Mol Neurobiol. 2020;57(2):1055–69. https://doi.org/10.1007/s12035-019-01803-6.
Hawley SA, Ross FA, Chevtzoff C, Green KA, Evans A, Fogarty S, et al. Use of cells expressing gamma subunit variants to identify diverse mechanisms of AMPK activation. Cell Metab. 2010;11(6):554–65. https://doi.org/10.1016/j.cmet.2010.04.001.
Biasutto L, Mattarei A, Zoratti M. Resveratrol and health: the starting point. ChemBioChem. 2012;13(9):1256–9. https://doi.org/10.1002/cbic.201200193.
Vingtdeux V, Giliberto L, Zhao H, Chandakkar P, Wu Q, Simon JE, et al. AMP-activated protein kinase signaling activation by resveratrol modulates amyloid-beta peptide metabolism. J Biol Chem. 2010;285(12):9100–13. https://doi.org/10.1074/jbc.M109.060061.
Park SJ, Ahmad F, Philp A, Baar K, Williams T, Luo H, et al. Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting cAMP phosphodiesterases. Cell. 2012;148(3):421–33. https://doi.org/10.1016/j.cell.2012.01.017.
Ronnett GV, Ramamurthy S, Kleman AM, Landree LE, Aja S. AMPK in the brain: its roles in energy balance and neuroprotection. J Neurochem. 2009;109(Suppl 1):17–23. https://doi.org/10.1111/j.1471-4159.2009.05916.x.
Muraleedharan R, Dasgupta B. AMPK in the brain: its roles in glucose and neural metabolism. Febs j. 2022;289(8):2247–62. https://doi.org/10.1111/febs.16151.
Saito M, Saito M, Das BC. Involvement of AMP-activated protein kinase in neuroinflammation and neurodegeneration in the adult and developing brain. Int J Dev Neurosci. 2019;77:48–59. https://doi.org/10.1016/j.ijdevneu.2019.01.007.
Sun X, Chen W-D, Wang Y-D. β-amyloid: the key peptide in the pathogenesis of Alzheimer’s disease. Front Pharmacol. 2015. https://doi.org/10.3389/fphar.2015.00221.
Mawuenyega KG, Kasten T, Sigurdson W, Bateman RJ. Amyloid-beta isoform metabolism quantitation by stable isotope-labeled kinetics. Anal Biochem. 2013;440(1):56–62. https://doi.org/10.1016/j.ab.2013.04.031.
Reinert J, Richard B, Klafki H, Friedrich B, Bayer T, Wiltfang J, et al. Deposition of C-terminally truncated Aβ species Aβ37 and Aβ39 in Alzheimer’s disease and transgenic mouse models. Acta Neuropathologica Commun. 2016. https://doi.org/10.1186/s40478-016-0294-7.
Crump CJ, Johnson DS, Li YM. Development and mechanism of γ-secretase modulators for Alzheimer’s disease. Biochemistry. 2013;52(19):3197–216. https://doi.org/10.1021/bi400377p.
Murphy MP, LeVine H 3rd. Alzheimer’s disease and the amyloid-beta peptide. J Alzheimers Dis. 2010;19(1):311–23. https://doi.org/10.3233/jad-2010-1221.
Marambaud P, Zhao H, Davies P. Resveratrol promotes clearance of Alzheimer’s disease amyloid-β peptides*. J Biol Chem. 2005;280(45):37377–82. https://doi.org/10.1074/jbc.M508246200.
Tcw J, Goate AM. Genetics of β-amyloid precursor protein in Alzheimer’s disease. Cold Spring Harb Perspect Med. 2017. https://doi.org/10.1101/cshperspect.a024539.
de Paula VJR, Guimarães FM, Diniz BS, Forlenza OV. Neurobiological pathways to Alzheimer’s disease: amyloid-beta, TAU protein or both? Dement Neuropsychol. 2009;3(3):188–94. https://doi.org/10.1590/s1980-57642009dn30300003.
Zhang X, Song W. The role of APP and BACE1 trafficking in APP processing and amyloid-β generation. Alzheimer’s Res Therapy. 2013;5(5):46. https://doi.org/10.1186/alzrt211.
Sathya M, Moorthi P, Premkumar P, Kandasamy M, Jayachandran KS, Anusuyadevi M. Resveratrol intervenes cholesterol-and isoprenoid-mediated amyloidogenic processing of AβPP in familial Alzheimer’s disease. J Alzheimers Dis. 2017;60(s1):S3–23.
Li F, Gong Q, Dong H, Shi J. Resveratrol, a neuroprotective supplement for Alzheimer’s disease. Curr Pharm Des. 2012;18(1):27–33.
Turner RS, Ronald GT, Suzanne C, Christopher HvD, Jacobo M, Brigid AR, et al. A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology. 2015;85(16):1383. https://doi.org/10.1212/WNL.0000000000002035.
Jia Y, Wang N, Liu X. Resveratrol and amyloid-beta: mechanistic insights. Nutrients. 2017. https://doi.org/10.3390/nu9101122.
Wiciński M, Domanowska A, Wódkiewicz E, Malinowski B. Neuroprotective properties of resveratrol and its derivatives-influence on potential mechanisms leading to the development of Alzheimer’s disease. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21082749.
Krasinski CA, Ivancic VA, Zheng Q, Spratt DE, Lazo ND. Resveratrol sustains insulin-degrading enzyme activity toward Aβ42. ACS Omega. 2018;3(10):13275–82. https://doi.org/10.1021/acsomega.8b01913.
Yun JM, Chien A, Jialal I, Devaraj S. Resveratrol up-regulates SIRT1 and inhibits cellular oxidative stress in the diabetic milieu: mechanistic insights. J Nutr Biochem. 2012;23(7):699–705. https://doi.org/10.1016/j.jnutbio.2011.03.012.
Zhang M, Tang Z. Therapeutic potential of natural molecules against Alzheimer’s disease via SIRT1 modulation. Biomed Pharmacother. 2023;161: 114474. https://doi.org/10.1016/j.biopha.2023.114474.
Bononi G, Citi V, Lapillo M, Martelli A, Poli G, Tuccinardi T, et al. Sirtuin 1-activating compounds: discovery of a class of thiazole-based derivatives. Molecules. 2022;27(19):6535.
Xu J, Jackson CW, Khoury N, Escobar I, Perez-Pinzon MA. Brain SIRT1 mediates metabolic homeostasis and neuroprotection. Front Endocrinol. 2018;9:702.
Yan L, Guo M-S, Zhang Y, Yu L, Wu J-M, Tang Y, et al. Dietary plant polyphenols as the potential drugs in neurodegenerative diseases: current evidence, advances, and opportunities. Oxid Med Cell Longevity. 2022;2022.
Zhu L, Lu F, Zhang X, Liu S, Mu P. SIRT1 is involved in the neuroprotection of pterostilbene against amyloid β 25–35-induced cognitive deficits in mice. Front Pharmacol. 2022;13: 877098.
Ibi D, Kondo S, Ohmi A, Kojima Y, Nakasai G, Takaba R, Hiramatsu M. Preventive effect of betaine against cognitive impairments in amyloid β peptide-injected mice through sirtuin1 in hippocampus. Neurochem Res. 2022;47(8):2333–44.
Islam F, Nafady MH, Islam MR, Saha S, Rashid S, Akter A, et al. Resveratrol and neuroprotection: an insight into prospective therapeutic approaches against Alzheimer’s disease from bench to bedside. Mol Neurobiol. 2022;59(7):4384–404.
Qin W, Chachich M, Lane M, Roth G, Bryant M, de Cabo R, et al. Calorie restriction attenuates Alzheimer’s disease type brain amyloidosis in Squirrel monkeys (Saimiri sciureus). J Alzheimers Dis. 2006;10(4):417–22.
Wang R, Wu Y, Liu R, Liu M, Li Q, Ba Y, Huang H. Deciphering therapeutic options for neurodegenerative diseases: insights from SIRT1. J Mol Med. 2022;100(4):537–53.
Cohen TJ, Guo JL, Hurtado DE, Kwong LK, Mills IP, Trojanowski JQ, Lee VM. The acetylation of tau inhibits its function and promotes pathological tau aggregation. Nat Commun. 2011;2(1):252.
Watroba M, Szukiewicz D. Sirtuins promote brain homeostasis, preventing Alzheimer’s disease through targeting neuroinflammation. Front Physiol. 2022;13: 962769.
Ye J, Liu Z, Wei J, Lu L, Huang Y, Luo L, Xie H. Protective effect of SIRT1 on toxicity of microglial-derived factors induced by LPS to PC12 cells via the p53-caspase-3-dependent apoptotic pathway. Neurosci Lett. 2013;553:72–7.
Zhang H, Cao Y, Chen L, Wang J, Tian Q, Wang N, et al. A polysaccharide from Polygonatum sibiricum attenuates amyloid-β-induced neurotoxicity in PC12 cells. Carbohyd Polym. 2015;117:879–86.
De Mingo Á, De Gregorio E, Moles A, Tarrats N, Tutusaus A, Colell A, et al. Cysteine cathepsins control hepatic NF-κB-dependent inflammation via sirtuin-1 regulation. Cell Death Disease. 2016;7(11):e2464-e.
Palomera-Avalos V, Griñán-Ferré C, Izquierdo V, Camins A, Sanfeliu C, Pallàs M. Metabolic stress induces cognitive disturbances and inflammation in aged mice: protective role of resveratrol. Rejuvenation Res. 2017;20(3):202–17.
Shen J, Xu L, Qu C, Sun H, Zhang J. Resveratrol prevents cognitive deficits induced by chronic unpredictable mild stress: Sirt1/miR-134 signalling pathway regulates CREB/BDNF expression in hippocampus in vivo and in vitro. Behav Brain Res. 2018;349:1–7.
Thiel G, Rössler OG. Resveratrol stimulates cyclic AMP response element mediated gene transcription. Mol Nutr Food Res. 2016;60(2):256–65. https://doi.org/10.1002/mnfr.201500607.
Zhao Y-N, Li W-F, Li F, Zhang Z, Dai Y-D, Xu A-L, et al. Resveratrol improves learning and memory in normally aged mice through microRNA-CREB pathway. Biochem Biophys Res Commun. 2013;435(4):597–602.
Saura CA, Valero J. The role of CREB signaling in Alzheimer’s disease and other cognitive disorders. 2011.
Amidfar M, de Oliveira J, Kucharska E, Budni J, Kim Y-K. The role of CREB and BDNF in neurobiology and treatment of Alzheimer’s disease. Life Sci. 2020;257: 118020.
Das S, Tosaki A, Bagchi D, Maulik N, Das DK. Resveratrol-mediated activation of cAMP response element-binding protein through adenosine A3 receptor by Akt-dependent and -independent pathways. J Pharmacol Exp Ther. 2005;314(2):762–9. https://doi.org/10.1124/jpet.105.084285.
Silva AJ, Kogan JH, Frankland PW, Kida S. CREB and memory. Annu Rev Neurosci. 1998;21:127–48. https://doi.org/10.1146/annurev.neuro.21.1.127.
Wiciński M, Malinowski B, Węclewicz MM, Grześk E, Grześk G. Resveratrol increases serum BDNF concentrations and reduces vascular smooth muscle cells contractility via a NOS-3-independent mechanism. Biomed Res Int. 2017;2017:9202954. https://doi.org/10.1155/2017/9202954.
Zhang F, Wang Y-Y, Liu H, Lu Y-F, Wu Q, Liu J, Shi J-S. Resveratrol produces neurotrophic effects on cultured dopaminergic neurons through prompting astroglial BDNF and GDNF release. Evid-Based Comp Altern Med: eCAM. 2012;2012: 937605. https://doi.org/10.1155/2012/937605.
Gao L, Zhang Y, Sterling K, Song W. Brain-derived neurotrophic factor in Alzheimer’s disease and its pharmaceutical potential. Transl Neurodegener. 2022;11(1):4. https://doi.org/10.1186/s40035-022-00279-0.
Peng S, Wuu J, Mufson EJ, Fahnestock M. Precursor form of brain-derived neurotrophic factor and mature brain-derived neurotrophic factor are decreased in the pre-clinical stages of Alzheimer’s disease. J Neurochem. 2005;93(6):1412–21.
Ng TKS, Ho CSH, Tam WWS, Kua EH, Ho RC-M. Decreased serum brain-derived neurotrophic factor (BDNF) levels in patients with Alzheimer’s disease (AD): a systematic review and meta-analysis. Int J Mol Sci. 2019;20(2):257.
Forlenza OV, Diniz BS, Teixeira AL, Radanovic M, Talib LL, Rocha NP, Gattaz WF. Lower cerebrospinal fluid concentration of brain-derived neurotrophic factor predicts progression from mild cognitive impairment to Alzheimer’s disease. NeuroMol Med. 2015;17:326–32.
Weinstein G, Beiser AS, Choi SH, Preis SR, Chen TC, Vorgas D, et al. Serum brain-derived neurotrophic factor and the risk for dementia: the Framingham Heart Study. JAMA Neurol. 2014;71(1):55–61.
la Porte C, Voduc N, Zhang G, Seguin I, Tardiff D, Singhal N, Cameron DW. Steady-state pharmacokinetics and tolerability of trans-resveratrol 2000mg twice daily with food, quercetin and alcohol (ethanol) in healthy human subjects. Clin Pharmacokinet. 2010;49:449–54.
Ye JH, Thomas E, Sanguansri L, Liang YR, Augustin MA. Interaction between whole buttermilk and resveratrol. J Agric Food Chem. 2013;61(29):7096–101. https://doi.org/10.1021/jf401784z.
Skroza D, Šimat V, Smole Možina S, Katalinić V, Boban N, Generalić MI. Interactions of resveratrol with other phenolics and activity against food-borne pathogens. Food Sci Nutr. 2019;7(7):2312–8.
Ghafouri-Fard S, Bahroudi Z, Shoorei H, Hussen BM, Talebi SF, Baig SG, et al. Disease-associated regulation of gene expression by resveratrol: Special focus on the PI3K/AKT signaling pathway. Cancer Cell Int. 2022;22(1):298. https://doi.org/10.1186/s12935-022-02719-3.
Acknowledgements
Irrespective of the specific subject, we would like to express our profound gratitude to the diligent scientists who have undertaken earlier research to pave the way for gaining knowledge.
Funding
No specific grants from funding institutions in the public, commercial, or nonprofit sectors were given to this study.
Author information
Authors and Affiliations
Contributions
AA conceived the idea; AA and FA independently drafted this manuscript, selected and retrieved relevant papers, and assessed each study. Any discrepancies were reviewed and reanalyzed by both authors to resolve conflicts. AA rechecked the data curation, reanalyzed, and rewrote this manuscript appropriately to minimize bias and fit it with standard a systematic review. AA is the guarantor of the total content. All authors have revised and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
There was no need for this research because it was a review and no participants participated in it.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Appendix.
Additional file 2
. PRIOR checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Azargoonjahromi, A., Abutalebian, F. Unraveling the therapeutic efficacy of resveratrol in Alzheimer’s disease: an umbrella review of systematic evidence. Nutr Metab (Lond) 21, 15 (2024). https://doi.org/10.1186/s12986-024-00792-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-024-00792-1