Abstract
The morbidity of gestational diabetes mellitus (GDM) is increasing and is associated with adverse perinatal outcomes and long-term maternal and infant health. The exact mechanism underlying changes in plasma free fatty acid (FFA) profiles in patients with GDM is unknown. However, it is believed that changes in diet and lipid metabolism may play a role. Fatty acids contain many specific FFAs, and the type of FFA has different impacts on physiological processes; hence, determining changes in FFAs in individual plasma is essential. Alterations in FFA concentration or profile may facilitate insulin resistance. Additionally, some FFAs show potential to predict GDM in early pregnancy and are strongly associated with the growth and development of the fetus and occurrence of macrosomia. Here, we aimed to review changes in FFAs in women with GDM and discuss the relationship of FFAs with GDM incidence and adverse outcomes.
Similar content being viewed by others
Introduction
The prevalence of obesity has increased globally over the past two decades, with obesity rates exceeding 35% among women in many countries worldwide [1]. Pre-pregnancy overweight or obesity is a known risk factor for many pregnancy complications to a greater extent than gestational weight gain (GWG). The higher the pre-pregnancy maternal body mass index, the higher the risk of pregnancy complications such as pregnancy-induced hypertension (PIH) and gestational diabetes mellitus (GDM) [2, 3]. The prevalence of GDM has increased by over 35% in the last few decades and is still growing [4]. GDM pathogenesis is unclear; however, its characteristics are similar to those of type 2 diabetes mellitus, with increased insulin resistance (IR) incidence and relative insulin deficiency due to decreased β-cell function and numbers [5, 6]. Potential risk factors for GDM include pre-pregnancy overweight and obesity, age and unhealthy dietary habits [7]. Regarding dietary fat intake, higher intake of total fat saturated fatty acids (SFAs) and cholesterol in pregnant women was previously thought to be associated with an increased risk of GDM [8, 9], whereas intake of polyunsaturated fatty acids (PUFAs) and alpha-linolenic acid (ALA) was associated with a decreased risk [10]. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) and World Health Organization (WHO) recommend a 75 g, 2 h oral glucose tolerance test (OGTT) for pregnant women between 24 and 28 weeks of gestation [11, 12]. The American Diabetes Association (ADA) diagnostic criteria are a fasting blood glucose level ≥ 5.1 mmol/l at the 60th minute of the OGTT or a blood glucose concentration ≥ 10 mmol/l at the 120th minute of the OGTT or a fasting blood glucose level ≥ 8.5 mmol/l at the 120th minute of the OGTT [13]. GDM is one of the most common pregnancy complications [14]. GDM is associated with poor pregnancy outcomes, abnormal glucose tolerance, and obesity in offspring [15,16,17]. Although preventing GDM is not possible, early diagnosis is necessary [16].
Free fatty acid (FFA) is a physiologically important energy substrate released from adipose tissue through lipolysis in response to the body's energy needs. FFA is an efficient energy store in adipocytes in the form of triacylglycerides (TAGs) and phospholipids in cell membrane components [18, 19]. Fat metabolism and carbohydrates are closely related, and alterations in FFAs may be involved in pathophysiologic processes associated with IR in GDM [20]. This review aimed to summarize the correlation between altered FFA levels and GDM to provide help in early GDM prevention and find a relationship with poor outcomes.
Pathophysiologic process and risk factors of GDM
There is a progressive increase in insulin resistance during normal pregnancy due to an increase in circulating placental hormones, including adrenocorticotropic hormone, adrenocorticotropic hormone-releasing hormone, human placental lactogen, prolactin, estrogen, and progesterone [21,22,23,24,25,26]. Maternal obesity also promotes IR in early pregnancy, leading to increased lipolysis in the second trimester [27, 28], with the result that elevated FFA levels can further exacerbate IR by inhibiting maternal glucose uptake and stimulating hepatic gluconeogenesis [28, 29]. Increased maternal IR leads to elevated maternal postprandial glucose levels and growth-promoting FFAs [23, 27, 30]. In addition, insulin secretion increases during normal pregnancy to maintain maternal blood glucose levels [22]. In contrast, in pregnant women with GDM, insulin secretion fails to compensate for the progressive increase in insulin resistance during pregnancy, leading to the development of maternal hyperglycemia [31]. A high-fat and high-sugar diet leads to IR and β-cell dysfunction [32], and lipotoxicity caused by hypertriglyceridemia during pregnancy also contributes to pancreatic β-cell damage and further reduction in insulin secretion [33, 34]. In addition, excessive inflammatory activation may be associated with GDM, and preeclampsia possesses a similar pathophysiological process to GDM [35, 36], with pro-inflammatory mediators of arachidonic acid (AA) and linoleic acid (LA) derivatives playing an important role in the development of both [37]. The pathogenesis of GDM is similar to that of type 2 diabetes mellitus, which is characterized by increased insulin resistance and a decrease in β-cell function and number caused by relative insulin deficiency [5, 6]. There are many risk factors that contribute to the development of GDM, such as a history of GDM pregnancies [38], increasing maternal age [39], pre-pregnancy overweight or obesity [40], weight gain during pregnancy [41], and high dietary fat and low-carbohydrate intake [42], among other factors.
FFA sources and metabolic processes
Fatty acids (FAs) are usually found in organisms in three main esters: TAGs, phospholipids, and cholesterol esters. When FAs are not present in the plasma as esters, they are referred to as non-esterified FAs or FFAs. FAs are mainly taken up as phospholipids and TAGs. During digestion, TAGs are broken down into monoglyceride, diacylglycerol, and FFAs. Short- and medium-chain FAs (≤ 12 carbons) are directly absorbed by intestinal cells. Long-chain FAs (> 12 carbons) are absorbed and re-converted into TAGs and transported via lipoprotein particles such as high-density, low-density, very low-density lipoproteins and chymotrypsin particles [43]. Lipoprotein lipases present on the cell surface cleave TAGs to form FFAs that are taken up by the cells [44]. In the blood, FFAs are mainly carried by serum albumin. In adipose tissues, FFAs are re-esterified to form TAGs, which are stored in adipose droplets of adipocytes and later mobilized through lipolysis, i.e., the hydrolysis of TAGs [18]. In mitochondria, most FFAs undergo β-oxidation to produce acetyl-coenzyme A, and subsequently, acetyl-CoA enters the Krebs cycle to produce energy as adenosine triphosphate (ATP) [18, 45]. FFAs are also important signaling molecules [46]. In addition to dietary intake, FFAs can be synthesized endogenously, which is referred to as de novo adipogenesis, with the main source being (excess) carbohydrates [18, 44].
FFAs are hydrocarbon chains comprising methyl and carboxyl groups at each end. According to the presence or absence and number of carbon–carbon double bonds, FFAs can be categorized as saturated FAs(SFAs, no double bonds), monounsaturated FAs (MUFAs, one double bond), or polyunsaturated FAs (PUFAs, multiple double bonds), and a detailed categorization of the FFA profiles is presented in Fig. 1A. Figure 1B indicates the common sources of dietary intake. Depending on the position of the first double bond at the methyl end of the FFA molecule, PUFAs can be subdivided into n-3, n-6, and n-9 FAs. By measuring and quantifying FFAs, based on the length of the aliphatic tails, short-, medium-, and long-chain FAs have < 6, 6–12, and > 12 carbon atoms, respectively [47]. Commonly used test methods for FFA spectroscopy include gas chromatography- and liquid chromatography-mass spectrometries [48, 49]. FFAs play an important energetic role and are involved in regulating intracellular signaling, cell structure, and lipid mediator production [50]. FFAs can also be converted to sphingolipids and phospholipids, which are involved in cell membrane formation. Among them, ceramide, a type of sphingolipid, is synthesized de novo from SFA (e.g., palmitate) in a multistep enzymatic cascade reaction and is the main scaffold for most complex sphingolipids, which can be broken down into variable FFAs and sphingomyelins. It can affect glucose metabolism by blocking the activation of the anabolic enzyme Akt or protein kinase B (Akt/PKB), inhibiting insulin signaling, and inducing selective insulin resistance, which hinders glucose uptake and storage and promotes hepatic gluconeogenesis [51,52,53]. Mustaniemi Sanna et al. found that although ceramides, along with clinical risk factors and triglycerides, did not appear to significantly improve the predictive performance of GDM, unfavorable changes in ceramides could indicate the degree of metabolic disturbances in GDM [54].
A Classification of FFAs; B Common sources of dietary intake. A present the FFAs contained in SFA, PUFA (n-3/n-6), and MUFA, B reflects the common dietary categories of the above fatty acids. FFAs(free fatty acids); SFAs(saturated fatty acids); UFAs(unsaturated fatty acids); MUFAs (monounsaturated fatty acids); PUFAs (polyunsaturated fatty acids)
Association between dietary FA intake and GDM
GDM development is related to many factors, including the type and amount of FAs consumed in diets. The balance between SFA and PUFA intake is important, and women with GDM reportedly consume significantly less fatty fish representing PUFA but consume a higher proportion of saturated fat [55]. Moreover, SFA intake is positively associated with the development of GDM [56]. Most current studies tend to investigate dietary intake using questionnaires, which makes knowing the amount of each FFA consumed difficult. Humans consume nutrients as part of complex foods that contain varying amounts of nutrients, which may impact the FFA intake from specific sources.
Dietary sources of FFAs play an important role in regulating inflammation. Increased intake of MUFA may be associated with anti-inflammatory effects. One of the most abundant omega-7 MUFA is palmitoleic acid (POA; C16:1 n-7), derived from fatty fish, fish oil, macadamia nuts, sea buckthorn, and Wagyu beef. Oleic acid (OA; C18:1n9) is one of the most abundant MUFA in the human diet [57, 58]. POA activates basal lipolysis and re-esterification, increases lipoprotein lipase (Lpl) activity, regulates n3-PUFA metabolism in membrane phospholipids, and also reduces proinflammatory cytokines to alleviate chronic inflammation. OA may ameliorate inflammation by regu AA metabolism [58]. Studies have shown that dietary supplementation with palmitoleate is beneficial for improving lipid and glucose metabolism and has also been associated with favorable changes in genes that regulate inflammation [58, 59].Yang's previous research has also shown that repeated administration of palmitoleate downregulated the expression of proinflammatory genes, acted as an anti-inflammatory, and blocked glucose or SFA-induced apoptosis of β-cells and improved insulin resistance [60]. Long-chain PUFAs (LC-PUFAs) include two categories: n-3 and n-6 PUFAs. The human body needs to consume some n-3 and n-6 PUFAs from the diet. For example, ALA and LA as essential fatty acids need to be obtained from diets [61]. Typical dietary n-3 sources are oily seeds such as chia or flaxseed, fish, green vegetables, and grass-fed animal products, whereas n-6 is usually derived from vegetable oils such as corn or sunflower seeds, and non-grass-fed animal products (Fig. 1B). Generally, n-6 PUFAs are regarded as pro-inflammatory molecules, whereas n-3 PUFAs (especially eicosapentaenoic acid and docosahexaenoic acid (DHA) are regarded as anti-inflammatory molecules [62]. Maintaining a balance between n-3 and n-6 PUFAs is important for regulating inflammation and immunomodulation. Diets high in n-3 intake can cause reduced cytokine production and lower cardiovascular disease risk factors [63]. However, western diets tend to be low in fiber and rich in total fat, rich in n-6 PUFAs as well as saturated fats, including hydrogenated vegetable fat (HVF, rich in trans fat) and interesterified fat (IF), making the n-6/n-3 PUFA ratio high [64, 65]. Modern diets tend to increase n-6 intake and decrease n-3 intake owing to the increase in processed food consumption, widespread use of hydrogenated vegetable oils, and impact of industrialized agriculture. This has skewed the n-3 to n-6 ratio in favor of n-6, promoting chronic inflammatory diseases [66]. Women with GDM have increased and decreased n-6 and n-3 PUFA blood levels, respectively [67]. In pregnant women with GDM, n-3 PUFA intake is beneficial in alleviating IR and inflammation and decreasing the risk of adverse pregnancy outcomes [68, 69]. Combined supplementation with vitamin D and n-3 PUFAs for 6 weeks improves fasting glucose, very low-density lipoprotein cholesterol, serum triglycerides, and insulin levels in patients with GDM [70]. A higher dietary n-6:n-3 PUFA ratio is associated with higher GDM incidence [71]. Dietary fat-rich fish and oral n-3 supplements are more effective in increasing n-3 PUFA levels [55]. One study found no reduction in the GDM incidence in pregnant women who were supplemented with 800 mg of DHA-enriched fish oil per day [72], and the same results were found in a DHA supplementation study [73]. Thus, DHA appears to be ineffective in preventing GDM but may have a therapeutic role in women with GDM. Pregnant women with GDM may benefit from DHA supplementation, which may be considered in their treatment. MUFA consumption has benefits, and the inclusion of OA (C18:1, n9)-rich olive oil and pistachios in the Mediterranean diet [74, 75] reduces GDM incidence [76]. Olive oil intake reduces inflammatory markers in the placenta and cord blood of pregnant women with GDM [77]. In conclusion, further studies are needed to elucidate the relationship between dietary intake of different FA types and GDM. Figure 2 shows the association between dietary FFA intake and GDM occurrence and development.
Relationship between dietary intake of FFAs and GDM. Pregnant women with GDM tended to consume more SFA and n-6 PUFAs than n-3 PUFAs, and the results were similar in blood. DHA supplementation is beneficial for pregnant women with GDM. GDM (gestational diabetes mellitus); FFAs(free fatty acids); SFAs(saturated fatty acids); PUFAs (polyunsaturated fatty acids); DHA(docosahexaenoic acid); IR(insulin resistance)
Relationship between FFAs and GDM
FFAs and IR
IR is the main pathogenesis of GDM, which is mainly characterized by a decrease in sensitivity to insulin [6]. Circulating FFA is one of the most important factors promoting IR and altering insulin secretion [20, 78]. In skeletal muscle, the mechanism by which FFAs cause IR involves protein kinase C activation via diacylglycerol accumulation, leading to decreased tyrosine insulin receptor substrate-1 phosphorylation and phosphatidylinositol-3 kinase activation inhibition [79]. Acute and chronic elevation of FFA induces IR, and Chronic elevation of FFA levels may impede β-cell compensatory responses [80]. A study showed that calculating the FFA index during pregnancy can be used to measure insulin sensitivity [81]. Higher homeostatic model assessment of IR (HOMA-IR) and c-peptide levels can reflect GDM risk. Palmitic acid, stearic acid, AA, dihomo-γ-linolenic acid (DGLA), and DHA positively correlated with HOMA-IR and c-peptide [82], indicating the effect of SFAs, AAs, DGLAs, and DHAs on GDM development. There may be a relationship between inflammation and the development of IR. The saturated fatty acid palmitate promotes the production of pro-inflammatory cytokines associated with insulin resistance in adipose tissue and/or adipocytes [83]. In addition, Maternal obesity may exacerbate the development of IR. POA is a fatty acid with anti-inflammatory and insulin-sensitizing properties, and maternal obesity leads to decreased synthesis of POA by syncytiotrophoblast cells, which can lead to IR and persistent mild inflammation in the mother, placenta, or fetus [84]. Levels of 20-hydroxyeicosatetraenoic acids (20-HETEs), a metabolite of AA, are positively correlated with BMI [85]. Increased levels of cytochrome P450 (CYP) and 20-HETE, which act on AA to exert enzymatic activity, are associated with the development of IR in obese women with GDM [37]. Therefore, maternal obesity should also be of concern when considering the effect of changes in FFAs levels on IR. women with GDM who are predominantly characterized by defective insulin sensitivity have significantly higher FFA [86], also confirming the correlation between FFA and IR.
FFA levels in pregnant women with GDM
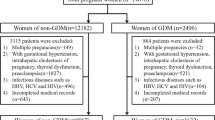
In addition to the measurement of dietary FFA intake, several studies have analyzed the association between blood FFAs and GDM. In healthy pregnancies, serum TG and NEFA levels in mid- to late-gestation, increasing with the number of gestational weeks and peaking just before delivery [87]. The period of greatest increase in FFA and maximum placental FA transport occurs in the last trimester of pregnancy [88]. A trend towards higher plasma FFA levels in patients with GDM was observed [89, 90]. In addition, in a study on the FFA profile of patients with GDM, some differences in FFA levels were found between different gestational periods [55, 91,92,93,94]. In Table 1, we present the characteristics of the population of studies and surveys on the FFA spectrum, while the corresponding results are presented in Table 2.
FFAs are altered differently during different gestational periods. Total plasma SFA, MUFA, PUFA n-6, and PUFA n-3 levels increased in pregnant women with GDM in early pregnancy [55]. At mid-pregnancy, with the elevated total FFA, elevated SFA is more pronounced [93]. In Hou et al.’s [91] study, various FFAs were elevated, including OA, ALA, and DGLA, similar to the observations in another study [94]. In early pregnancy, Ma et al. [92] and Zhang et al. [94] reported that myristic and palmitic acids were elevated in pregnant women with GDM, and Ma et al. found that palmitic acid was positively associated with GDM risk. In Zhang et al.'s study, dietary supplementation of ALA and DHA was associated with a high risk of GDM with elevated fasting glucose alone, and the levels of most FFAs, such as DGLA, myristic, palmitoleic, linolenic (γ-LA, GLA), and docosahexaenoic acids, were progressively lower from early to late pregnancy; however, the OA levels were consistently high [94]. In addition, LA levels were reversed [92, 94]. Differences in these data can be interpreted by looking at populations of different races and the controls chosen, whether they match the BMI, and whether fasting is required before blood collection. And the type of sample tested has little effect [95]. Altogether, changes in FFA levels associated with GDM during different gestational periods are complex.
Alterations in the FFA profile of patients with GDM can also affect maternal physiology by altering the levels of FFA transporters, such as increased levels of plasma FA binding protein-4 (FABP4) and other proteins in the serum [96]. Zhang et al. [97] found higher concentrations of FABP4 in GDM women in mid- to late-gestation. FABP4 is positively associated with an increased GDM risk in early and mid-gestation [98].
Treatment of pregnant women with GDM with FFAs
Currently, the treatment of GDM mainly involves lifestyle interventions and drug therapy. Among the medications are insulin injections or oral glibenclamide and metformin, among others [99]. The traditional dietary treatment for GDM is carbohydrate restriction [100]. However, this approach usually leads to higher fat intake, as protein intake is constant [101]. High-fat diets typically increase serum FFAs and promote insulin resistance [102]. Whereas an appropriate increase in the proportion of carbohydrates and a decrease in the proportion of fat in the diet can still keep blood glucose below current treatment targets and reduce postprandial FFAs [103].
In terms of pharmacological treatment, it has been suggested that increased insulin sensitivity by metformin can lead to a decrease in FFA levels [104]. There is no significant difference in FFA levels between the two modalities of glycemic control in pregnant women with GDM, namely insulin therapy or diet [105].
FFA and GDM fetal growth and development and other pregnancy outcomes
Relationship between FFA and GDM fetal growth and development
In addition to glucose, fetal growth is also closely related to lipids [106]. Fasting and 1-h postprandial triglycerides at 16 weeks of gestation are strongly associated with neonatal obesity, more so than maternal glucose [107]. TGs at delivery were independently associated with large for gestational age (LGA) [108]. Placental triglyceride levels and FFA levels in umbilical cord plasma are significantly higher in GDM pregnant women, which may be related to altered placental lipogenesis and fatty acid oxidation protein expression and increased placental transport [109, 110]. It further led to fetal overgrowth. In addition, GDM pregnant women, independently of BMI, altered the lipid profile of the placenta, with elevated levels of both palmitic and stearic acids [93]. Higher maternal FFA levels in GDM reportedly lead to increased fetal birth weights [86], and maternal FFA levels were positively associated with the prevalence of LGA newborns [108, 111]. Emilio Herrera et al. showed a positive correlation between maternal FFA and neonatal weight and adiposity in pregnant women with GDM who had good glycemic control. Maternal dyslipidemia in GDM may promote the transfer of maternal FAs to the fetus, leading to an increase in fetal adipose tissue mass, thereby increasing macrosomia risk [112]. In the study by Fan et al., FFA levels and fetal growth restriction (FGR) were higher in women with GDM than in controls in late pregnancy, and the area under curve value for GDM diagnosis and FGR was 0.84. In addition, a positive correlation was observed between serum FFA and umbilical artery systolic/diastolic ratio (S/D), pulsatility index (PI), and resistance index (RI), reflecting the resistance to blood flow in pregnant women; therefore, fetal growth in a poor intrauterine environment may contribute to FGR development. Moreover, FFA in the serum positively correlated with umbilical artery S/D, PI, and RI values, reflecting blood flow resistance in pregnant women [113]. Studies on the relationship between the FFA profile levels and fetal growth are further needed to utilize FFA concentration or profile levels to help the fetus grow within the appropriate range.
DHA and AA are essential for fetal CNS development and immune system regulation [114]. Reduced maternal-to-fetal DHA transfer in GDM may be associated with impaired placental DHA uptake [115, 116]. Reduced cord blood DHA levels in patients with GDM may lead to reduced plasma DHA levels in neonates with GDM [117, 118]. This outcome affects fetal neurodevelopment in the first 6 months of life [119]. Cord blood DHA levels positively correlate with maternal DHA levels when patients with GDM have good glycemic control [120]. Léveillé et al. also observed no reduction in DHA levels in the umbilical cord blood of pregnant women with GDM treated with diet or medication [121]. It can be seen that effective control of blood glucose levels in GDM patients is beneficial in maintaining fetal DHA levels. To some extent, it favors fetal neurodevelopment. DHA supplementation during pregnancy at 600 mg/d does not improve fetal DHA status [122].
Association between FFA and other pregnancy outcomes
N-3 and n-6 PUFAs are essential for the structural and functional growth and development of the placenta [123]. In addition to exhibiting anti-inflammatory properties, n-3 FAs have antioxidant potential and play a crucial part in stimulating placenta formation, angiogenesis, and remodeling in early pregnancy [124, 125]. Inadequate maternal LC-PUFA supply and impaired maternal–fetal transfer are associated with adverse pregnancy outcomes, such as preeclampsia, intrauterine growth retardation, and GDM [126, 127]. Neonatal hyperbilirubinemia incidence and neonatal hospitalization in pregnant women with GDM can be reduced by supplementation with n-3 PUFAs [69].
In conclusion, there have been more studies on the impact of altered FFA concentrations on pregnancy outcomes in patients with GDM, but few studies have evaluated the relevance of alterations in different FFA subclasses in patients with GDM to other adverse maternal or neonatal outcome events, and future research could be directed in this direction.
Discussion
FFAs are derived from various sources, have a high correlation with IR, and are likely to be associated with GDM development. Regarding diet, having a balanced FFA intake is important; however, analyzing a specific FFA is difficult owing to its complexity and various dietary components. Excessive SFA intake can have harmful effects, leading to an increase in inflammation, IR [128], and cardiovascular disease [129]. Before GDM diagnosis, SFA intake was higher than that of PUFAs. When the balance of n-6 PUFAs versus n-3 PUFAs favored the former, a positive correlation was observed with GDM incidence, and preventing GDM by supplementing with n-3 PUFAs has not yet been conclusively demonstrated. Available evidence suggests that n-3 PUFA supplementationis not beneficial in reducing the incidence of maternal pregnancy outcomes such as gestational diabetes and hypertension, but is beneficial for neonatal health, such as reducing the incidence of preterm labor and low birth weight, and increasing birth weight and birth length [130]. Notably, n-3 FA supplementation in pregnant women with GDM is beneficial to reducing IR and inflammation and decreasing adverse pregnancy outcomes. In addition to dietary intake, plasma FFAs reflect FFA levels from various sources, and FFA levels in pregnant women with GDM vary considerably across gestational periods, with the majority being elevated from early to mid-pregnancy and progressively decreasing in late pregnancy. Differences were observed in the results of different studies over the same period, which may be related to factors such as the study populations and whether the relevant indicators were matched. FFAs, palmitic acid, ALA, and DHA are highly correlated with GDM development. In addition, lipocalin is a potent anti-inflammatory/anti-diabetic adipokine [131]. Saturated fatty acids and omega-3 fatty acids are associated with circulating concentrations of lipocalin in healthy humans [132]. Lipocalin is associated with the development of GDM during pregnancy [133]. More studies could be done in the future to evaluate the effects of altered lipocalin and FFAs in patients with GDM.
Lipids are associated with fetal growth and development; FFA levels are closely related to fetal weight, and mechanisms of fetal underweight or overweight require further exploration. Fetal FFA acquisition is regulated by maternal FFA levels and placental mechanisms. DHA is closely related to fetal neurological development, and the reduced DHA transfer to the fetus in patients with GDM may be related to impaired placental uptake, whereas good control of blood glucose promotes the transfer of placental FFAs to an extent, providing sufficient DHA to the fetus. Other adverse pregnancy events are less well-studied. High FFA levels in the postpartum period in women with a previous history of GDM likely contribute to type 2 diabetes mellitus [134, 135]. This may be related to reduced sensitivity to insulin via lipolytic inhibition [136]. Positive recognition of changes in FFAs facilitates a smooth pregnancy course; however, more research and standardization between clinical trials and patient sampling are needed. Finally, appropriate FA intake should be considered before and during pregnancy to optimize maternal and infant outcomes and bring new preventive and therapeutic strategies for GDM.
Availability of data and materials
Not applicable.
Abbreviations
- GDM:
-
Gestational diabetes mellitus
- FFA:
-
Free fatty acid
- GWG:
-
Gestational weight gain
- IADPSG:
-
International Association of Diabetes and Pregnancy Study Groups
- WHO:
-
World Health Organization
- ADA:
-
American Diabetes Association
- BMI:
-
Body mass index
- PIH:
-
Pregnancy-induced hypertension
- IR:
-
Insulin resistance
- SFAs:
-
Saturated fatty acids
- PUFAs:
-
Polyunsaturated fatty acids
- ALA:
-
Alpha-linolenic acid
- ADA:
-
American Diabetes Association
- OGTT:
-
Oral glucose tolerance test
- TAGs:
-
Triacylglycerides
- FAs:
-
Fatty acids
- ATP:
-
Adenosine triphosphate
- MUFAs:
-
Monounsaturated fatty acids
- UFAs:
-
Unsaturated fatty acids
- LPl:
-
Lipoprotein lipase
- OA:
-
Oleic acid
- POA:
-
Palmitoleic acid
- AA:
-
Arachidonic acid
- LC-PUFAs:
-
Long-chain polyunsaturated fatty acids
- ALA:
-
Alpha-linolenic acid
- LA:
-
Linoleic acid
- DHA:
-
Docosahexaenoic acid
- HVF:
-
Hydrogenated vegetable fat
- IF:
-
Interesterified fat
- 20-HETEs:
-
20-Hydroxyeicosatetraenoic acids
- CYP450:
-
Cytochrome P450
- EPA:
-
Eicosapentaenoic acid
- GLA:
-
γ-Linolenic acid
- DGLA:
-
Dihomo-γ-linolenic acid
- ARA:
-
Arachidonic acid
- FABP4:
-
FA binding protein-4
- LGA:
-
Large for gestational age
- FGR:
-
Fetal growth restriction
- S/D:
-
Systolic/diastolic
- PI:
-
Pulsatility index
- RI:
-
Resistance index
- HOMA-IR:
-
Homeostatic model assessment of IR
References
Neeland IJ, Poirier P, Després JP. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation. 2018;137:1391–406.
Lewandowska M, Więckowska B, Sajdak S. Pre-pregnancy obesity, excessive gestational weight gain, and the risk of pregnancy-induced hypertension and gestational diabetes mellitus. J Clin Med. 2020. https://doi.org/10.3390/jcm9061980.
Wang X, Zhang S, Yu W, Li G, Li J, Ji J, Mi Y, Luo X. Pre-pregnancy body mass index and glycated-hemoglobin with the risk of metabolic diseases in gestational diabetes: a prospective cohort study. Front Endocrinol (Lausanne). 2023;14:1238873.
Filardi T, Tavaglione F, Di Stasio M, Fazio V, Lenzi A, Morano S. Impact of risk factors for gestational diabetes (GDM) on pregnancy outcomes in women with GDM. J Endocrinol Invest. 2018;41:671–6.
Halban PA, Polonsky KS, Bowden DW, Hawkins MA, Ling C, Mather KJ, Powers AC, Rhodes CJ, Sussel L, Weir GC. β-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care. 2014;37:1751–8.
Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic β cell dedifferentiation as a mechanism of diabetic β cell failure. Cell. 2012;150:1223–34.
Nijs H, Benhalima K. Gestational diabetes mellitus and the long-term risk for glucose intolerance and overweight in the offspring: a narrative review. J Clin Med. 2020. https://doi.org/10.3390/jcm9020599.
Gao F, Cui CY. Dietary cholesterol intake and risk of gestational diabetes mellitus: a meta-analysis of observational studies. J Am Nutr Assoc. 2022;41:107–15.
Mizgier M, Jarzabek-Bielecka G, Mruczyk K. Maternal diet and gestational diabetes mellitus development. J Matern Fetal Neonatal Med. 2021;34:77–86.
Barbieiri P, Nunes JC, Torres AG, Nishimura RY, Zuccolotto DC, Crivellenti LC, Franco LJ, Sartorelli DS. Indices of dietary fat quality during midpregnancy is associated with gestational diabetes. Nutrition. 2016;32:656–61.
WHO Guidelines Approved by the Guidelines Review Committee. In Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. Geneva: World Health Organization Copyright © World Health Organization 2013; 2013.
Weinert LS. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: comment to the International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Diabetes Care. 2010;33:e97; author reply e98.
Classification and Diagnosis of Diabetes. Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45:S17-s38.
American Diabetes Association. Gestational diabetes mellitus. Diabetes Care. 2004; 27(Suppl 1):S88–90.
Lowe WL Jr, Scholtens DM, Kuang A, Linder B, Lawrence JM, Lebenthal Y, McCance D, Hamilton J, Nodzenski M, Talbot O, et al. Hyperglycemia and adverse pregnancy outcome follow-up study (HAPO FUS): maternal gestational diabetes mellitus and childhood glucose metabolism. Diabetes Care. 2019;42:372–80.
Liu B, Cai J, Xu Y, Long Y, Deng L, Lin S, Zhang J, Yang J, Zhong L, Luo Y, et al. Early diagnosed gestational diabetes mellitus is associated with adverse pregnancy outcomes: a prospective cohort study. J Clin Endocrinol Metab. 2020. https://doi.org/10.1210/clinem/dgaa633.
Chung HR, Moon JH, Lim JS, Lee YA, Shin CH, Hong JS, Kwak SH, Choi SH, Jang HC. Maternal hyperglycemia during pregnancy increases adiposity of offspring. Diabetes Metab J. 2021;45:730–8.
Large V, Peroni O, Letexier D, Ray H, Beylot M. Metabolism of lipids in human white adipocyte. Diabetes Metab. 2004;30:294–309.
Qian X, Yang Z, Mao E, Chen E. Regulation of fatty acid synthesis in immune cells. Scand J Immunol. 2018;88: e12713.
McLachlan KA, Boston R, Alford FP. Impaired non-esterified fatty acid suppression to intravenous glucose during late pregnancy persists postpartum in gestational diabetes: a dominant role for decreased insulin secretion rather than insulin resistance. Diabetologia. 2005;48:1373–9.
Alvarez JJ, Montelongo A, Iglesias A, Lasunción MA, Herrera E. Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women. J Lipid Res. 1996;37:299–308.
Ryan EA, Enns L. Role of gestational hormones in the induction of insulin resistance. J Clin Endocrinol Metab. 1988;67:341–7.
Leturque A, Hauguel S, Sutter Dub MT, Maulard P, Girard J. Effects of placental lactogen and progesterone on insulin stimulated glucose metabolism in rat muscles in vitro. Diabete Metab. 1989;15:176–81.
Kalkhoff RK, Kissebah AH, Kim HJ. Carbohydrate and lipid metabolism during normal pregnancy: relationship to gestational hormone action. Semin Perinatol. 1978;2:291–307.
Costrini NV, Kalkhoff RK. Relative effects of pregnancy, estradiol, and progesterone on plasma insulin and pancreatic islet insulin secretion. J Clin Invest. 1971;50:992–9.
Lain KY, Catalano PM. Metabolic changes in pregnancy. Clin Obstet Gynecol. 2007;50:938–48.
Barbour LA, McCurdy CE, Hernandez TL, Kirwan JP, Catalano PM, Friedman JE. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care. 2007;30(Suppl 2):S112-119.
Bomba-Opon D, Wielgos M, Szymanska M, Bablok L. Effects of free fatty acids on the course of gestational diabetes mellitus. Neuro Endocrinol Lett. 2006;27:277–80.
Boden G, Chen X, Ruiz J, White JV, Rossetti L. Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest. 1994;93:2438–46.
Kühl C. Etiology and pathogenesis of gestational diabetes. Diabetes Care. 1998;21(Suppl 2):B19-26.
Buchanan TA, Kitzmiller JL. Metabolic interactions of diabetes and pregnancy. Annu Rev Med. 1994;45:245–60.
Mishra A, Ruano SH, Saha PK, Pennington KA. A novel model of gestational diabetes: acute high fat high sugar diet results in insulin resistance and beta cell dysfunction during pregnancy in mice. PLoS ONE. 2022;17: e0279041.
Koukkou E, Watts GF, Lowy C. Serum lipid, lipoprotein and apolipoprotein changes in gestational diabetes mellitus: a cross-sectional and prospective study. J Clin Pathol. 1996;49:634–7.
Nolan CJ. Controversies in gestational diabetes. Best Pract Res Clin Obstet Gynaecol. 2011;25:37–49.
Phoswa WN, Khaliq OP. The role of oxidative stress in hypertensive disorders of pregnancy (preeclampsia, gestational hypertension) and metabolic disorder of pregnancy (gestational diabetes mellitus). Oxid Med Cell Longev. 2021;2021:5581570.
McElwain CJ, Tuboly E, McCarthy FP, McCarthy CM. Mechanisms of endothelial dysfunction in pre-eclampsia and gestational diabetes mellitus: windows into future cardiometabolic health? Front Endocrinol (Lausanne). 2020;11:655.
Szczuko M, Kikut J, Komorniak N, Bilicki J, Celewicz Z, Ziętek M. The role of arachidonic and linoleic acid derivatives in pathological pregnancies and the human reproduction process. Int J Mol Sci. 2020;21(24):9628.
Kim C, Berger DK, Chamany S. Recurrence of gestational diabetes mellitus: a systematic review. Diabetes Care. 2007;30:1314–9.
Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, Saade GR, Eddleman KA, Klugman S, Dugoff L, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105:983–90.
Yang H, Wei Y, Gao X, Xu X, Fan L, He J, Hu Y, Liu X, Chen X, Yang Z, Zhang C. Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16,286 pregnant women in China. Diabet Med. 2009;26:1099–104.
Gibson KS, Waters TP, Catalano PM. Maternal weight gain in women who develop gestational diabetes mellitus. Obstet Gynecol. 2012;119:560–5.
Morisset AS, St-Yves A, Veillette J, Weisnagel SJ, Tchernof A, Robitaille J. Prevention of gestational diabetes mellitus: a review of studies on weight management. Diabetes Metab Res Rev. 2010;26:17–25.
Ramírez M, Amate L, Gil A. Absorption and distribution of dietary fatty acids from different sources. Early Hum Dev. 2001;65(Suppl):S95-s101.
Rui L. Energy metabolism in the liver. Compr Physiol. 2014;4:177–97.
Saponaro C, Gaggini M, Carli F, Gastaldelli A. The subtle balance between lipolysis and lipogenesis: a critical point in metabolic homeostasis. Nutrients. 2015;7:9453–74.
Miyamoto J, Hasegawa S, Kasubuchi M, Ichimura A, Nakajima A, Kimura I. Nutritional signaling via free fatty acid receptors. Int J Mol Sci. 2016;17:450.
Burdge GC, Calder PC. Introduction to fatty acids and lipids. World Rev Nutr Diet. 2015;112:1–16.
Baldi S, Menicatti M, Nannini G, Niccolai E, Russo E, Ricci F, Pallecchi M, Romano F, Pedone M, Poli G, et al. Free fatty acids signature in human intestinal disorders: significant association between butyric acid and celiac disease. Nutrients. 2021. https://doi.org/10.3390/nu13030742.
Liu Y, Li Y, Shen H, Li Y, Xu Y, Zhou M, Xia X, Shi B. Association between the metabolic profile of serum fatty acids and diabetic nephropathy: a study conducted in northeastern China. Ther Adv Endocrinol Metab. 2022;13:20420188221118750.
Papackova Z, Cahova M. Fatty acid signaling: the new function of intracellular lipases. Int J Mol Sci. 2015;16:3831–55.
Chaurasia B, Summers SA. Ceramides in metabolism: key lipotoxic players. Annu Rev Physiol. 2021;83:303–30.
Brown MS, Goldstein JL. Selective versus total insulin resistance: a pathogenic paradox. Cell Metab. 2008;7:95–6.
Chaurasia B, Tippetts TS, Mayoral Monibas R, Liu J, Li Y, Wang L, Wilkerson JL, Sweeney CR, Pereira RF, Sumida DH, et al. Targeting a ceramide double bond improves insulin resistance and hepatic steatosis. Science. 2019;365:386–92.
Mustaniemi S, Keikkala E, Kajantie E, Nurhonen M, Jylhä A, Morin-Papunen L, Öhman H, Männistö T, Laivuori H, Eriksson JG, et al. Serum ceramides in early pregnancy as predictors of gestational diabetes. Sci Rep. 2023;13:13274.
Tryggvadottir EA, Gunnarsdottir I, Birgisdottir BE, Hrolfsdottir L, Landberg R, Hreidarsdottir IT, Hardardottir H, Halldorsson TI. Early pregnancy plasma fatty acid profiles of women later diagnosed with gestational diabetes. BMJ Open Diabetes Res Care. 2021. https://doi.org/10.1136/bmjdrc-2021-002326.
Bo S, Menato G, Lezo A, Signorile A, Bardelli C, De Michieli F, Massobrio M, Pagano G. Dietary fat and gestational hyperglycaemia. Diabetologia. 2001;44:972–8.
Miklankova D, Markova I, Hüttl M, Stankova B, Malinska H. The different insulin-sensitising and anti-inflammatory effects of palmitoleic acid and oleic acid in a prediabetes model. J Diabetes Res. 2022;2022:4587907.
Yang ZH, Pryor M, Noguchi A, Sampson M, Johnson B, Pryor M, Donkor K, Amar M, Remaley AT. Dietary palmitoleic acid attenuates atherosclerosis progression and hyperlipidemia in low-density lipoprotein receptor-deficient mice. Mol Nutr Food Res. 2019;63: e1900120.
Frigolet ME, Gutiérrez-Aguilar R. The role of the novel lipokine palmitoleic acid in health and disease. Adv Nutr. 2017;8:173s–81s.
Yang ZH, Miyahara H, Hatanaka A. Chronic administration of palmitoleic acid reduces insulin resistance and hepatic lipid accumulation in KK-Ay Mice with genetic type 2 diabetes. Lipids Health Dis. 2011;10:120.
Godhamgaonkar AA, Wadhwani NS, Joshi SR. Exploring the role of LC-PUFA metabolism in pregnancy complications. Prostaglandins Leukot Essent Fatty Acids. 2020;163: 102203.
Sears B, Perry M. The role of fatty acids in insulin resistance. Lipids Health Dis. 2015;14:121.
Van Dael P. Role of n-3 long-chain polyunsaturated fatty acids in human nutrition and health: review of recent studies and recommendations. Nutr Res Pract. 2021;15:137–59.
Plissonneau C, Sivignon A, Chassaing B, Capel F, Martin V, Etienne M, Wawrzyniak I, Chausse P, Dutheil F, Mairesse G, et al. Beneficial effects of linseed supplementation on gut mucosa-associated microbiota in a physically active mouse model of Crohn’s disease. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23115891.
Haygert P, Roversi K, Milanesi LH, Maurer LH, Camponogara C, Duarte T, Barcelos RCS, Emanuelli T, Oliveira SM, Duarte M, et al. Can the dietary fat type facilitate memory impairments in adulthood? A comparative study between Mediterranean and Western-based diet in rats. J Nutr Biochem. 2018;59:104–13.
Mariamenatu AH, Abdu EM. Overconsumption of omega-6 polyunsaturated fatty acids (PUFAs) versus deficiency of omega-3 PUFAs in modern-day diets: the disturbing factor for their “balanced antagonistic metabolic functions” in the human body. J Lipids. 2021;2021:8848161.
Ogundipe E, Samuelson S, Crawford MA. Gestational diabetes mellitus prediction? A unique fatty acid profile study. Nutr Diabetes. 2020;10:36.
Samimi M, Jamilian M, Asemi Z, Esmaillzadeh A. Effects of omega-3 fatty acid supplementation on insulin metabolism and lipid profiles in gestational diabetes: randomized, double-blind, placebo-controlled trial. Clin Nutr. 2015;34:388–93.
Jamilian M, Samimi M, Kolahdooz F, Khalaji F, Razavi M, Asemi Z. Omega-3 fatty acid supplementation affects pregnancy outcomes in gestational diabetes: a randomized, double-blind, placebo-controlled trial. J Matern Fetal Neonatal Med. 2016;29:669–75.
Jamilian M, Samimi M, Ebrahimi FA, Hashemi T, Taghizadeh M, Razavi M, Sanami M, Asemi Z. The effects of vitamin D and omega-3 fatty acid co-supplementation on glycemic control and lipid concentrations in patients with gestational diabetes. J Clin Lipidol. 2017;11:459–68.
Fu Y, Yang Y, Zhu L, Chen J, Yu N, Zhao M. Effect of dietary n-6: n-3 Poly-Unsaturated fatty acids ratio on gestational diabetes mellitus: a prospective cohort. Gynecol Endocrinol. 2022;38:583–7.
Zhou SJ, Yelland L, McPhee AJ, Quinlivan J, Gibson RA, Makrides M. Fish-oil supplementation in pregnancy does not reduce the risk of gestational diabetes or preeclampsia. Am J Clin Nutr. 2012;95:1378–84.
Garmendia ML, Casanello P, Flores M, Kusanovic JP, Uauy R. The effects of a combined intervention (docosahexaenoic acid supplementation and home-based dietary counseling) on metabolic control in obese and overweight pregnant women: the MIGHT study. Am J Obstet Gynecol. 2021;224:526.e521-526.e525.
Ojeda-Amador RM, Fregapane G, Salvador MD. Composition and properties of virgin pistachio oils and their by-products from different cultivars. Food Chem. 2018;240:123–30.
Piccinin E, Cariello M, De Santis S, Ducheix S, Sabbà C, Ntambi JM, Moschetta A. Role of oleic acid in the gut-liver axis: from diet to the regulation of its synthesis via stearoyl-CoA desaturase 1 (SCD1). Nutrients. 2019. https://doi.org/10.3390/nu11102283.
Assaf-Balut C, García de la Torre N, Durán A, Fuentes M, Bordiú E, Del Valle L, Familiar C, Ortolá A, Jiménez I, Herraiz MA, et al. A Mediterranean diet with additional extra virgin olive oil and pistachios reduces the incidence of gestational diabetes mellitus (GDM): A randomized controlled trial: The St. Carlos GDM prevention study. PLoS ONE. 2017;12: e0185873.
Gomez Ribot D, Diaz E, Fazio MV, Gómez HL, Fornes D, Macchi SB, Gresta CA, Capobianco E, Jawerbaum A. An extra virgin olive oil-enriched diet improves maternal, placental, and cord blood parameters in GDM pregnancies. Diabetes Metab Res Rev. 2020;36: e3349.
Sivan E, Homko CJ, Whittaker PG, Reece EA, Chen X, Boden G. Free fatty acids and insulin resistance during pregnancy. J Clin Endocrinol Metab. 1998;83:2338–42.
Sivan E, Boden G. Free fatty acids, insulin resistance, and pregnancy. Curr Diab Rep. 2003;3:319–22.
Carpentier A, Mittelman SD, Lamarche B, Bergman RN, Giacca A, Lewis GF. Acute enhancement of insulin secretion by FFA in humans is lost with prolonged FFA elevation. Am J Physiol. 1999;276:E1055-1066.
Wagner R, Fritsche L, Heni M, Fehlert E, Stefan N, Staiger H, Häring HU, Fritsche A. A novel insulin sensitivity index particularly suitable to measure insulin sensitivity during gestation. Acta Diabetol. 2016;53:1037–44.
Chen X, Stein TP, Steer RA, Scholl TO. Individual free fatty acids have unique associations with inflammatory biomarkers, insulin resistance and insulin secretion in healthy and gestational diabetic pregnant women. BMJ Open Diabetes Res Care. 2019;7: e000632.
Ajuwon KM, Spurlock ME. Palmitate activates the NF-kappaB transcription factor and induces IL-6 and TNFalpha expression in 3T3-L1 adipocytes. J Nutr. 2005;135:1841–6.
Ferchaud-Roucher V, Barner K, Jansson T, Powell TL. Maternal obesity results in decreased syncytiotrophoblast synthesis of palmitoleic acid, a fatty acid with anti-inflammatory and insulin-sensitizing properties. Faseb J. 2019;33:6643–54.
Issan Y, Hochhauser E, Guo A, Gotlinger KH, Kornowski R, Leshem-Lev D, Lev E, Porat E, Snir E, Thompson CI, et al. Elevated level of pro-inflammatory eicosanoids and EPC dysfunction in diabetic patients with cardiac ischemia. Prostaglandins Other Lipid Mediat. 2013;100–101:15–21.
Layton J, Powe C, Allard C, Battista MC, Doyon M, Bouchard L, Perron P, Wessel J, Hivert MF. Maternal lipid profile differs by gestational diabetes physiologic subtype. Metabolism. 2019;91:39–42.
Zhang Ming WH, Yiming Z. Zhang Yiming: Study on the changes of blood lipid indexes in middle and late normal pregnancy. J Nanjing Med Univ (Natural Sciences). 2013;33:1455–7.
Haggarty P. Effect of placental function on fatty acid requirements during pregnancy. Eur J Clin Nutr. 2004;58:1559–70.
Meyer B, Calvert D, Moses R. Free fatty acids and gestational diabetes mellitus. Aust N Z J Obstet Gynaecol. 1996;36:255–7.
Villafan-Bernal JR, Acevedo-Alba M, Reyes-Pavon R, Diaz-Parra GA, Lip-Sosa DL, Vazquez-Delfin HI, Hernandez-Muñoz M, Bravo-Aguirre DE, Figueras F, Martinez-Portilla RJ. Plasma levels of free fatty acids in women with gestational diabetes and its intrinsic and extrinsic determinants: systematic review and meta-analysis. J Diabetes Res. 2019;2019:7098470.
Hou W, Meng X, Zhao A, Zhao W, Pan J, Tang J, Huang Y, Li H, Jia W, Liu F, Jia W. Development of multimarker diagnostic models from metabolomics analysis for gestational diabetes mellitus (GDM). Mol Cell Proteomics. 2018;17:431–41.
Ma Yuru YX, Wei Z. Certain serum free fatty acids during the first trimester of pregnancy associated with gestational diabetes mellitus. J Capital Med Univ. 2023;44:265–71.
Stirm L, Kovárová M, Perschbacher S, Michlmaier R, Fritsche L, Siegel-Axel D, Schleicher E, Peter A, Pauluschke-Fröhlich J, Brucker S, et al. BMI-independent effects of gestational diabetes on human placenta. J Clin Endocrinol Metab. 2018;103:3299–309.
Zhang T, Jiang WR, Xia YY, Mansell T, Saffery R, Cannon RD, De Seymour J, Zou Z, Xu G, Han TL, et al. Complex patterns of circulating fatty acid levels in gestational diabetes mellitus subclasses across pregnancy. Clin Nutr. 2021;40:4140–8.
Buchanan CDC, Lust CAC, Burns JL, Hillyer LM, Martin SA, Wittert GA, Ma DWL. Analysis of major fatty acids from matched plasma and serum samples reveals highly comparable absolute and relative levels. Prostaglandins Leukot Essent Fatty Acids. 2021;168: 102268.
Trojnar M, Patro-Małysza J, Kimber-Trojnar Ż, Leszczyńska-Gorzelak B, Mosiewicz J. Associations between fatty acid-binding protein 4–A proinflammatory adipokine and insulin resistance, gestational and type 2 diabetes mellitus. Cells. 2019. https://doi.org/10.3390/cells8030227.
Zhang Y, Zhang HH, Lu JH, Zheng SY, Long T, Li YT, Wu WZ, Wang F. Changes in serum adipocyte fatty acid-binding protein in women with gestational diabetes mellitus and normal pregnant women during mid- and late pregnancy. J Diabetes Investig. 2016;7:797–804.
Francis EC, Li M, Hinkle SN, Cao Y, Chen J, Wu J, Zhu Y, Cao H, Kemper K, Rennert L, et al. Adipokines in early and mid-pregnancy and subsequent risk of gestational diabetes: a longitudinal study in a multiracial cohort. BMJ Open Diabetes Res Care. 2020. https://doi.org/10.1136/bmjdrc-2020-001333.
Sweeting A, Wong J, Murphy HR, Ross GP. A clinical update on gestational diabetes mellitus. Endocr Rev. 2022;43:763–93.
Jovanovic-Peterson L, Peterson CM. Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes. J Am Coll Nutr. 1990;9:320–5.
Simpson SJ, Raubenheimer D. Obesity: the protein leverage hypothesis. Obes Rev. 2005;6:133–42.
Lichtenstein AH, Schwab US. Relationship of dietary fat to glucose metabolism. Atherosclerosis. 2000;150:227–43.
Hernandez TL, Van Pelt RE, Anderson MA, Daniels LJ, West NA, Donahoo WT, Friedman JE, Barbour LA. A higher-complex carbohydrate diet in gestational diabetes mellitus achieves glucose targets and lowers postprandial lipids: a randomized crossover study. Diabetes Care. 2014;37:1254–62.
Zhang T, He J, Xu C, Zu L, Jiang H, Pu S, Guo X, Xu G. Mechanisms of metformin inhibiting lipolytic response to isoproterenol in primary rat adipocytes. J Mol Endocrinol. 2009;42:57–66.
Stangenberg M, Persson B, Lunell NO, Hanson U. Effect of treatment with insulin or diet on intermediary metabolites in pregnant women with chemical diabetes in the third trimester of pregnancy. Acta Diabetol Lat. 1984;21:55–61.
Heerwagen MJR, Gumina DL, Hernandez TL, Van Pelt RE, Kramer AW, Janssen RC, Jensen DR, Powell TL, Friedman JE, Winn VD, Barbour LA. Placental lipoprotein lipase activity is positively associated with newborn adiposity. Placenta. 2018;64:53–60.
Barbour LA, Farabi SS, Friedman JE, Hirsch NM, Reece MS, Van Pelt RE, Hernandez TL. Postprandial triglycerides predict newborn fat more strongly than glucose in women with obesity in early pregnancy. Obesity (Silver Spring). 2018;26:1347–56.
Schaefer-Graf UM, Graf K, Kulbacka I, Kjos SL, Dudenhausen J, Vetter K, Herrera E. Maternal lipids as strong determinants of fetal environment and growth in pregnancies with gestational diabetes mellitus. Diabetes Care. 2008;31:1858–63.
Schaefer-Graf UM, Meitzner K, Ortega-Senovilla H, Graf K, Vetter K, Abou-Dakn M, Herrera E. Differences in the implications of maternal lipids on fetal metabolism and growth between gestational diabetes mellitus and control pregnancies. Diabet Med. 2011;28:1053–9.
Balachandiran M, Bobby Z, Dorairajan G, Jacob SE, Gladwin V, Vinayagam V, Packirisamy RM. Placental accumulation of triacylglycerols in gestational diabetes mellitus and its association with altered fetal growth are related to the differential expressions of proteins of lipid metabolism. Exp Clin Endocrinol Diabetes. 2021;129:803–12.
Kim SY, Song YS, Kim SK, Cho YW, Kim KS. Postprandial free fatty acids at mid-pregnancy increase the risk of large-for-gestational-age newborns in women with gestational diabetes mellitus. Diabetes Metab J. 2022;46:140–8.
Herrera E, Ortega-Senovilla H. Implications of lipids in neonatal body weight and fat mass in gestational diabetic mothers and non-diabetic controls. Curr Diab Rep. 2018;18:7.
Fan Limin ZX, Peilin L. Application of ultrasonic parameters of fetal umbilical artery, serum FFA and PL in the diagnosis of FGR in GDM pregnant women in late pregnancy. Imaging Sci Photochem. 2022;40:986–90.
Ogundipe E, Johnson MR, Wang Y, Crawford MA. Peri-conception maternal lipid profiles predict pregnancy outcomes. Prostaglandins Leukot Essent Fatty Acids. 2016;114:35–43.
Pagán A, Prieto-Sánchez MT, Blanco-Carnero JE, Gil-Sánchez A, Parrilla JJ, Demmelmair H, Koletzko B, Larqué E. Materno-fetal transfer of docosahexaenoic acid is impaired by gestational diabetes mellitus. Am J Physiol Endocrinol Metab. 2013;305:E826-833.
Araújo JR, Correia-Branco A, Ramalho C, Keating E, Martel F. Gestational diabetes mellitus decreases placental uptake of long-chain polyunsaturated fatty acids: involvement of long-chain acyl-CoA synthetase. J Nutr Biochem. 2013;24:1741–50.
Thomas BA, Ghebremeskel K, Lowy C, Offley-Shore B, Crawford MA. Plasma fatty acids of neonates born to mothers with and without gestational diabetes. Prostaglandins Leukot Essent Fatty Acids. 2005;72:335–41.
Ortega-Senovilla H, Alvino G, Taricco E, Cetin I, Herrera E. Gestational diabetes mellitus upsets the proportion of fatty acids in umbilical arterial but not venous plasma. Diabetes Care. 2009;32:120–2.
Zornoza-Moreno M, Fuentes-Hernández S, Carrión V, Alcántara-López MV, Madrid JA, López-Soler C, Sánchez-Solís M, Larqué E. Is low docosahexaenoic acid associated with disturbed rhythms and neurodevelopment in offsprings of diabetic mothers? Eur J Clin Nutr. 2014;68:931–7.
Ortega-Senovilla H, Schaefer-Graf U, Herrera E. Pregnant women with gestational diabetes and with well controlled glucose levels have decreased concentrations of individual fatty acids in maternal and cord serum. Diabetologia. 2020;63:864–74.
Léveillé P, Ardilouze JL, Pasquier JC, Deacon C, Whittingstall K, Plourde M. Fatty acid profile in cord blood of neonates born to optimally controlled gestational diabetes mellitus. Prostaglandins Leukot Essent Fatty Acids. 2016;115:48–52.
Min Y, Djahanbakhch O, Hutchinson J, Eram S, Bhullar AS, Namugere I, Ghebremeskel K. Efficacy of docosahexaenoic acid-enriched formula to enhance maternal and fetal blood docosahexaenoic acid levels: Randomized double-blinded placebo-controlled trial of pregnant women with gestational diabetes mellitus. Clin Nutr. 2016;35:608–14.
Basak S, Duttaroy AK. Effects of fatty acids on angiogenic activity in the placental extravillious trophoblast cells. Prostaglandins Leukot Essent Fatty Acids. 2013;88:155–62.
Johnsen GM, Basak S, Weedon-Fekjær MS, Staff AC, Duttaroy AK. Docosahexaenoic acid stimulates tube formation in first trimester trophoblast cells, HTR8/SVneo. Placenta. 2011;32:626–32.
Leghi GE, Muhlhausler BS. The effect of n-3 LCPUFA supplementation on oxidative stress and inflammation in the placenta and maternal plasma during pregnancy. Prostaglandins Leukot Essent Fatty Acids. 2016;113:33–9.
Gauster M, Hiden U, Blaschitz A, Frank S, Lang U, Alvino G, Cetin I, Desoye G, Wadsack C. Dysregulation of placental endothelial lipase and lipoprotein lipase in intrauterine growth-restricted pregnancies. J Clin Endocrinol Metab. 2007;92:2256–63.
Wadhwani N, Patil V, Joshi S. Maternal long chain polyunsaturated fatty acid status and pregnancy complications. Prostaglandins Leukot Essent Fatty Acids. 2018;136:143–52.
Kennedy A, Martinez K, Chuang CC, LaPoint K, McIntosh M. Saturated fatty acid-mediated inflammation and insulin resistance in adipose tissue: mechanisms of action and implications. J Nutr. 2009;139:1–4.
Perna M, Hewlings S. Saturated fatty acid chain length and risk of cardiovascular disease: a systematic review. Nutrients. 2022. https://doi.org/10.3390/nu15010030.
Hao Y, Sun X, Wen N, Song D, Li H. Effects of n-3 polyunsaturated fatty acid supplementation on pregnancy outcomes: a systematic review and meta-analysis. Arch Med Sci. 2022;18:890–9.
Banerjee A, Sharma D, Trivedi R, Singh J. Treatment of insulin resistance in obesity-associated type 2 diabetes mellitus through adiponectin gene therapy. Int J Pharm. 2020;583: 119357.
Fernández-Real JM, Vendrell J, Ricart W. Circulating adiponectin and plasma fatty acid profile. Clin Chem. 2005;51:603–9.
Ye Y, Wu P, Wang Y, Yang X, Ye Y, Yuan J, Liu Y, Song X, Yan S, Wen Y, et al. Adiponectin, leptin, and leptin/adiponectin ratio with risk of gestational diabetes mellitus: a prospective nested case-control study among Chinese women. Diabetes Res Clin Pract. 2022;191: 110039.
Liu L, Li Y, Guan C, Li K, Wang C, Feng R, Sun C. Free fatty acid metabolic profile and biomarkers of isolated post-challenge diabetes and type 2 diabetes mellitus based on GC-MS and multivariate statistical analysis. J Chromatogr B Analyt Technol Biomed Life Sci. 2010;878:2817–25.
Fugmann M, Uhl O, Hellmuth C, Hetterich H, Kammer NN, Ferrari U, Parhofer KG, Koletzko B, Seissler J, Lechner A. Differences in the serum nonesterified fatty acid profile of young women associated with a recent history of gestational diabetes and overweight/obesity. PLoS ONE. 2015;10: e0128001.
Tura A, Pacini G, Winhofer Y, Bozkurt L, Di Benedetto G, Morbiducci U, Roden M, Kautzky-Willer A. Non-esterified fatty acid dynamics during oral glucose tolerance test in women with former gestational diabetes. Diabet Med. 2012;29:351–8.
Acknowledgements
In the process of writing this review, we gratefully acknowledge Na Wu for providing intellectual support and technical assistance. She provided a lot of help with the structure and writing standards of the article.
Funding
This research was funded by the National Natural Science Foundation of China, grant number 81700706; the Virtual Simulation Experiment Teaching Project of China Medical University, grant number 2020–47; the 345 Talent Project of Shengjing Hospital; the Natural Science Foundation of Liaoning Province, grant number 2021-MS-182; the Science Foundation of Liaoning Education Department, grant number LK201603; and the Clinical Research Project of Liaoning Diabetes Medical Nutrition Prevention Society, grant number LNSTNBYXYYFZXH-RS01B.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by HD, DL, NW and MLM; literature investigation and manuscript draft were performed by HD and DL; English polishing was done by MLM; and NW carefully revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Du, H., Li, D., Molive, L.M. et al. Advances in free fatty acid profiles in gestational diabetes mellitus. J Transl Med 22, 180 (2024). https://doi.org/10.1186/s12967-024-04922-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-04922-4