Abstract
Background
Anastomosis for gastrointestinal reconstruction has been contentious after low anterior resection of rectal cancer for the past 30 years. Despite the abundance of randomized controlled trials (RCTs) on colon J-pouch (CJP), straight colorectal anastomosis (SCA), transverse coloplast (TCP), and side-to-end anastomosis (SEA), most studies are small and lack reliable clinical evidence. We conducted a systematic review and network meta-analysis to evaluate the effects of the four anastomoses on postoperative complications, bowel function, and quality of life in rectal cancer.
Methods
We assessed the safety and efficacy of CJP, SCA, TCP, and SEA in adult patients with rectal cancer after surgery by searching the Cochrane Library, Embase, and PubMed databases to collect RCTs from the date of establishment to May 20, 2022. Anastomotic leakage and defecation frequency were the main outcome indicators. We pooled data through a random effects model in a Bayesian framework and assessed model inconsistency using the deviance information criterion (DIC) and node-splitting method and inter-study heterogeneity using the I-squared statistics (I2). The interventions were ranked according to the surface under the cumulative ranking curve (SUCRA) to compare each outcome indicator.
Results
Of the 474 studies initially evaluated, 29 were eligible RCTs comprising 2631 patients. Among the four anastomoses, the SEA group had the lowest incidence of anastomotic leakage, ranking first (SUCRASEA = 0.982), followed by the CJP group (SUCRACJP = 0.628). The defecation frequency in the SEA group was comparable to those in the CJP and TCP groups at 3, 6, 12, and 24 months postoperatively. In comparison, the defecation frequency in the SCA group 12 months after surgery all ranked fourth. No statistically significant differences were found among the four anastomoses in terms of anastomotic stricture, reoperation, postoperative mortality within 30 days, fecal urgency, incomplete defecation, use of antidiarrheal medication, or quality of life.
Conclusions
This study demonstrated that SEA had the lowest risk of complications, comparable bowel function, and quality of life compared to the CJP and TCP, but further research is required to determine its long-term consequences. Furthermore, we should be aware that SCA is associated with a high defecation frequency.
Similar content being viewed by others
Background
Colorectal cancer is the third most common cancer globally and the second largest cause of cancer fatalities, with rectal cancer accounting for at least one-third of all cancer fatalities [1]. Transabdominal low anterior resection (LAR) combined with total mesorectal excision (TME) is the standard approach for treating mid-low rectal cancer. However, anal sphincter and parasympathetic nerve damage and loss of rectal storage function result from gastrointestinal tract reconstruction after TME. Unfortunately, statistics show that approximately 50% of patients with rectal cancer experience postoperative complications, and up to 90% of patients have “low anterior resection syndrome” [2,3,4,5]. These complications and bowel dysfunction may affect a patient’s quality of life and long-term prognosis [6,7,8,9].
Conventional straight colorectal anastomosis is associated with numerous complications and is prone to severe bowel dysfunction [10,11,12]. To improve the intestinal function and quality of life of patients, Lazorthes et al. [13] and Parc et al. [14] proposed colon J-pouch (CJP) in 1986. Expanding the volume of the “new rectum” significantly improves bowel function after surgery. However, anatomical factors, including pelvic stenosis, mesenteric hypertrophy, and shortage of colon, limited CJP application; therefore, Z’Graggen et al. [15] introduced transverse coloplast (TCP) in 1999. Early research indicates that TCP was highly operational and had a similar impact on bowel function as CJP but also carried a significant risk of complications. Baker [16] first proposed the side-to-end anastomosis (SEA) technique in 1950, but its advantages were insignificant. It has reemerged in the spotlight in recent years as an alternative strategy to enhance postoperative bowel function.
Previous Cochrane systematic reviews and meta-analyses have concluded that the four anastomoses have similar complication rates. However, CJP is better than straight colorectal anastomosis (SCA) in bowel function, with no difference from SEA or TCP [17, 18]. The data they aggregated were the findings of a certain period rather than a specific point in time because of the few studies; therefore, the conclusions may be skewed. There is no consensus regarding the safest and most efficient anastomosis approach, despite an increase in the number of pertinent randomized controlled trials (RCTs) published in recent years. A network meta-analysis of postoperative complications and bowel function at 3, 6, 12, and 24 months after surgery in patients with rectal cancer will assist in summarizing the various impacts of the four anastomoses from direct and indirect comparisons by combining some of the limited trials in these systematic reviews and some recently published RCTs. This study aimed to provide more robust and comprehensive evidence for determining optimal anastomosis in clinical practice.
Methods
Protocol
The protocol for this study is registered with PROSPERO (CRD42022332911, https://www.crd.york.ac.uk/prospero/), and we have reported the results according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extended statement [19].
Search strategy
We collected RCTs from database establishment to May 20, 2022, by searching the Cochrane Library, Embase, and PubMed databases (see Supplementary Table 2, Supplementary File 1 for the detailed search strategy). Two authors (MX and YZ) screened the search results. After reading the relevant literature abstracts, we manually searched the corresponding full texts and the references of the obtained articles to avoid missing important articles.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (1) the study participants were adults with rectal cancer who underwent surgical treatment, (2) at least two of the anastomosis techniques (CJP, SCA, TCP, SEA) were included in the study, (3) at least one of the primary outcome indicators (anastomotic leakage and defecation frequency) was included, and (4) the research type was English RCTs. Exclusion criteria were as follows: (1) non-randomized controlled trials, including reviews, retrospective studies, commentaries, and meta-analyses; (2) lack of available data or outcomes; and (3) duplicate publication of content. Two authors (MX and YZ) independently reviewed the entire text in accordance with the inclusion and exclusion criteria, consulted a third author (CWL) in case of disagreement, and decided on the inclusion of eligible studies at a conference.
Data extraction and processing
Two authors (MX and YZ) independently extracted the following data: (1) anastomotic leakage, (2) defecation frequency, (3) anastomotic stricture, (4) reoperation, (5) postoperative mortality within 30 days, (6) fecal urgency, (7) incomplete defecation, (8) use of antidiarrheal medication, and (9) quality of life. We recorded the results of bowel function outcomes at 3, 6, 12, and 24 months following stoma retraction (or without stoma surgery). We considered the most common and concerning anastomotic leakage and defecation frequency as the primary outcome indicators, and the rest were secondary outcome indicators. Anastomotic leakage is defined as a significant crack at the edge of the anastomosis, leakage of bowel contents seen in the pelvis on imaging or endoscopy, or purulent discharge from the pelvic drainage tube. The defecation frequency was determined based on the patient-described average number of daily bowel movements.
Quality assessment
Two authors (YBS and ZHP) independently assessed the risk of bias for all included studies using the revised Cochrane Rob2 tool, and studies with disagreements were resolved by a third author (CWL) [20]. The following five domains were assessed separately for the included studies: randomization process, deviation from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each study’s final overall risk of bias was rated as “low,” “moderate concerns,” or “high.”
Statistical analysis
We performed a network meta-analysis using the Bayesian framework employing gemtc and rjags packages in R4.2.0 (https://www.r-project.org/). Simultaneously, the meta package was used for pairwise analysis. Network meta-analysis results provided more accurate estimates and ranked various interventions to provide clinical recommendations compared to results from traditional pairwise analyses [21, 22]. We uniformly used random effects models as conservative estimates, generating a risk ratio (RR) or mean difference (MD) with a 95% confidence interval (CI) to represent the efficacy of each intervention. We compared the consistent and inconsistent models using the deviance information criterion (DIC) [23]. A difference of the DIC less than 5 implies that the model has good goodness of fit, and there is no global inconsistency. In addition, we assessed the local inconsistency of the model using the node-splitting method [24, 25]. If the value of P > 0.05, the direct comparison was considered to be in good agreement with the indirect comparison. We also evaluated the heterogeneity between studies using the I-squared statistics (I2) [26, 27]. The range of I2 values was 0–100%, where 0–49% was low heterogeneity, 50–74% moderate heterogeneity, and 75–100% high heterogeneity. By calculating the surface under the cumulative ranking curve (SUCRA), we compared and ranked the safety and efficacy of various interventions. Higher ranking grades indicated lower perioperative complication rates or better bowel function. Due to the large variation in sample sizes of the included studies, sensitivity analyses on anastomotic leakage were performed to assess the reliability of the results, which included only studies with sample sizes greater than or equal to 20 in a single arm. To assess the publication bias of studies in the network meta-analysis, we used STATA 16.0 (Stata Corporation, College Station, TX, USA) to generate a comparison-adjusted funnel plot and thus explore the impact of publication bias or other small-sample studies [28]. In the absence of publication bias, the estimates for all comparisons were symmetrically distributed around the null hypothesis.
Results
Study characteristics
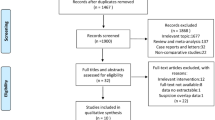
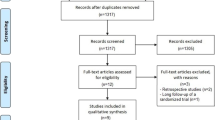
We identified 471 articles by searching the database and three articles from the reference list for a total of 474 articles (Fig. 1). After eliminating duplicates and preliminary screening of titles and abstracts, we excluded irrelevant studies, and the remaining 77 articles were potentially relevant to this study. Two authors (MX and YZ) independently reviewed the full text of the relevant literature and found that 29 studies (27 trials) met the inclusion criteria, of which Ho et al. [29, 30] and Machado et al. [31, 32] were both based on the same trial and reported two different results. These 29 studies were mainly distributed in Europe, Asia, and North America, of which six [33,34,35,36,37,38] were multicenter studies, and the remaining 23 were single-center studies. The characteristics of all the included studies are shown in Supplementary Table 3 (Supplementary File 1). In all studies, 2631 patients were included. Of these, 1166 (44%) were randomly assigned to the CJP group, 671 (25%) to the SCA group, 386 (14%) to the TCP group, and 408 (17%) to the SEA group. The studies were published from 1995 to 2019, with a maximum follow-up period of 5 years. Patients in most studies underwent ileostomies or colostomies, and only a few studies had elective or no stomas. Except for Liang et al. [39], Okkabaz et al. [40], and Parc et al. [36], all studies used open surgery.
The quality assessment of the included studies is presented in Supplementary Fig. 1 and Table 4 (Supplementary File 1). Nine (31.0%) of the total included studies [32, 34, 41,42,43,44,45,46,47] did not specifically state how the randomization sequence was assigned, and their randomization procedures were either high-risk or had some concerns. Due to the nature of the surgery, double-blinding was not feasible; however, this had less impact on the results. Clinicians must choose the final anastomosis based on the patient’s anatomical condition. This may lead to treatments that are not pre-randomized outcomes, with four (13.8%) [45, 48,49,50] studies at a high risk of deviating from the expected interventions. Of the 29 studies, one (3.4%) [42] had missing outcome data, three (10.3%) [35, 37, 50] had high-risk outcome measures, and one (3.4%) [30] was at high risk for selective reporting of results.
Results of a pairwise meta-analysis
The results of the pairwise meta-analysis of perioperative complications and bowel function are shown in Supplementary Figs. 2, 3, and 4 (Supplementary File 1). Regarding perioperative complications, compared to the CJP and SCA groups, the SEA group showed a slight decrease in the incidence of anastomotic leakage [(RR = 0.77, 95% CI 0.44–1.35) and (RR = 0.39, 95% CI 0.10–1.52)]. However, pairwise comparisons between interventions failed to show statistical differences. At 6 and 12 months postoperatively, we found that the SCA group had a substantially higher defecation frequency than the CJP group [(MD = 1.91, 95% CI 0.95–2.86) and (MD = 1.23, 95% CI 0.59–1.87)]. In terms of fecal urgency, the SCA and TCP groups had significantly more fecal urgency than the CJP group at 12 months postoperatively [(RR = 1.37, 95% CI 1.15–1.62) and (RR = 1.26, 95% CI 1.07–1.48)], respectively. Regarding the use of antidiarrheal drugs, the SCA group was significantly more frequent than the CJP group 6 months postoperatively (RR = 2.29, 95% CI 1.23–4.26). There was no discernible difference in incomplete defecation between the SCA, SEA, and CJP groups 6 and 12 months after surgery.
Results of network meta-analysis
Postoperative complications
Twenty-four studies [29, 31, 33,34,35,36,37,38,39,40,41,42,43, 45,46,47, 49,50,51,52,53,54,55,56] reported a primary safety indicator, anastomotic leakage. A network plot of the postoperative anastomotic leakage is shown in Fig. 2. The SEA group showed a considerably lower incidence of anastomotic leakage than either the SCA group or the TCP group [(RR = 0.36, 95% CI 0.14–0.81) and (RR = 0.24, 95% CI 0.06–0.74)]; however, there was no significant difference between the SEA and CJP groups. Figure 3 demonstrates that the SUCRA for the SEA group was the highest, ranking first (SUCRASEA = 0.982) and that for the CJP group was second (SUCRACJP = 0.628). These two anastomoses are the most secure. Additionally, 10 [31, 33, 34, 36, 40, 42, 43, 47, 50, 54], 13 [31, 33, 35,36,37,38, 40, 41, 43, 47, 49, 53, 55], and 14 studies [31, 33, 35, 38, 40,41,42,43, 49, 50, 52,53,54, 56] reported anastomotic stricture, reoperation, and postoperative mortality within 30 days, respectively. We found no differences among the four interventions. However, the SEA group ranked first for both reoperation and postoperative mortality within 30 days (SUCRASEA = 0.946 and 0.826), whereas the TCP group ranked fourth for both (SUCRASEA = 0.084 and 0.143).
Network plot for anastomotic leakage. Circles represent interventions, and their size is proportional to the number of patients who received the corresponding intervention. Lines represent direct comparisons, and their width is proportional to the number of studies in the corresponding comparison. CJP, colon J-pouch; SCA, straight colorectal anastomosis; TCP, transverse coloplasty; SEA, side-to-end anastomosis
Bowel function
Results at 3 months
Five [39, 43, 46, 51, 54], six [39, 43, 46, 51, 54, 55], and five studies [39, 43, 51, 54, 55] reported defecation frequency, fecal urgency, and the use of antidiarrheal medication, respectively. Like previous studies, the defecation frequency in the TCP and CJP groups ranked first (SUCRATCP = 0.727) and second (SUCRACJP = 0.720), respectively, followed by the SEA and SCA groups. However, there was no statistical difference among the groups (Table 1). There were no differences among the groups regarding fecal urgency and use of antidiarrheal medication, but the CJP group still ranked better than the SEA and SCA groups.
Results at 6 months
Thirteen [30, 31, 36, 39, 40, 42, 43, 46, 50,51,52, 54, 57], eight [39, 40, 43, 46, 51, 52, 54, 55], seven [30, 31, 38, 39, 51, 52, 54], and eight studies [30, 38, 39, 43, 51, 54, 55, 57] reported defecation frequency, fecal urgency, incomplete defecation, and the use of antidiarrheal medication, respectively. The SEA, TCP, and CJP groups did not differ significantly in terms of defecation frequency, but all performed better than the SCA group (Table 1), with the second (SUCRASEA = 0.689), third (SUCRATCP = 0.556), and first (SUCRACJP = 0.722) positions, respectively. No intervention was found to be noticeably superior regarding fecal urgency, incomplete defecation, and use of antidiarrheal medication. The TCP group ranked first in fecal urgency and incomplete defecation (SUCRATCP = 0.689 and 0.603, respectively), while the CJP group ranked second in both (SUCRACJP = 0.612 and 0.548, respectively). The SEA group ranked first in the use of antidiarrheal medications (SUCRASEA = 0.718).
Results at 12 months
Twelve [29, 31, 33, 34, 36, 40, 43, 48, 49, 52, 54, 57], nine [34, 40, 41, 43, 46, 48, 52, 54, 57], six [29, 31, 48, 49, 52, 54], and six studies [29, 33, 43, 48, 49, 54] reported defecation frequency, fecal urgency, incomplete defecation, and the use of antidiarrheal medication, respectively. The SEA, TCP, and CJP groups did not differ significantly in terms of defecation frequency, but all performed better than the SCA group (Table 2), with the third (SUCRASEA = 0.587), second (SUCRATCP = 0.659), and first (SUCRACJP = 0.743) positions, respectively. In addition, no substantial advantage was discovered for any specific intervention of fecal urgency, incomplete defecation, and use of antidiarrheal medication; nevertheless, the SEA group ranked best for both fecal urgency and use of antidiarrheal medication (SUCRASEA = 0.773 and 0.679).
Results at 24 months
Four [30, 32, 34, 54] and three studies [30, 34, 54] reported defecation frequency and use of antidiarrheal medication, respectively. The four intervention groups did not differ significantly in terms of defecation frequency (Table 2); however, the SEA and CJP groups were at the first (SUCRASEA = 0.779) and second (SUCRACJP = 0.727), respectively. Similarly, there was no statistical difference in the use of antidiarrheal medication among the intervention groups, but the SEA and CJP groups were first (SUCRASEA = 0.776) and second (SUCRACJP = 0.708), respectively.
Quality of life
Nine studies assessed the quality of life of patients with different types of anastomoses. However, because the assessment scales and timing varied among the studies, we could not combine them for the analysis. We summarize all the results in the table below (Table 3).
Sensitivity analysis, inconsistency, and heterogeneity
We only performed sensitivity analyses on data from anastomotic leakage because of the few studies. The DIC difference between models was reduced from 5.47 to 0.71 after removing studies with less than 20 sample sizes in a single arm, and the results were unchanged. The other outcome indicator models fit well, with the difference in DIC between the consistent and inconsistent models being less than 5. In our study, only the comparison of SCA with SEA in the fecal urgency outcome indicator at 12 months postoperatively was inconsistent (P = 0.02); no significant inconsistency was found in the other comparisons. Furthermore, we discovered low heterogeneity among studies on anastomotic leakage but generally high heterogeneity among studies on defecation frequency. We did not analyze it because of study limitations, but we speculated that it could be related to the variety of assessment scales and lack of objective evaluation.
Publication bias
The effect estimates of anastomotic leakage, postoperative mortality within 30 days, and fecal urgency at 3 months postoperatively were found to be symmetric around the null hypothesis by looking at the comparison-adjusted funnel plots (see Supplementary Fig. 5B-21B, Supplementary File 1), while the other outcome indicators were asymmetric and had publication bias.
Two-dimensional plot of primary outcomes
The two-dimensional plot of anastomotic leakage and defecation frequency estimates revealed that SEA had the lowest probability of causing anastomotic leakage and that CJP was generally better in defecation frequency. With time, the defecation frequency of the four anastomoses tended to stabilize. The defecation frequency in the SCA group was greater at all follow-up periods; the SEA group’s frequency was the same as the CJP group’s frequency starting 6 months postoperatively, and the TCP group’s frequency fluctuated around the CJP group’s level (Fig. 4).
Two-dimensional plot of anastomotic leakage and defecation frequency. Using the CJP group as the control group, the X-axis represents the MD and 95% CI of defecation frequency, and the Y-axis represents the RR and 95% CI of anastomotic leakage. a 3 months after surgery, b 6 months after surgery, c 12 months after surgery, and d 24 months after surgery. CJP, colon J-pouch; SCA, straight colorectal anastomosis; TCP, transverse coloplasty; SEA, side-to-end anastomosis
Discussion
In our study analysis, SEA was the best anastomosis based on safety to avoid anastomotic leakage, CJP being the next best. In recent years, surgeons have favored SEA because of its low complication rate, good bowel function, and high operability. Two recent meta-analyses of SEA versus CJP found that the SEA group had a lower incidence of anastomotic leakage than the CJP group, although the difference was not statistically significant [58, 59]. This could be because SEA avoids requiring a lateral anastomosis at the distal colon and excessive bowel freeing, which ensures an abundant blood supply and lower anastomotic tension. Notably, anastomotic leakage can result in severe abdominal infections, pelvic abscesses, sepsis, etc., which can cause reoperations, prolonged hospital stays, cancer recurrence, and lower patient survival rates [60,61,62,63]. Due to the advantages of SEA in reducing the risk of anastomotic leakage, our findings also show that SEA outperforms other anastomotic techniques for reducing both reoperation and postoperative mortality within 30 days. SCA is the simplest and earliest form of anastomosis and is now widely accepted to have a high incidence of anastomotic leakage [64,65,66,67], as confirmed in our study. In addition, similar to the results of the previous studies by Pimentel et al. [43] and Stratilatovas et al. [45], we found the highest incidence of postoperative complications (anastomotic leakage, reoperation, and postoperative mortality within 30 days) in the TCP group. Because the coloplasty site is proximal to the colorectal anastomosis (4 cm), perfusion of the anterior rectal wall is easily compromised, resulting in all leaks after TCP is located in the anterior part of the colorectal anastomosis (below the coloplasty site) [49]. Despite the advantages of TCP, including fewer surgical restrictions and better functional bowel outcomes, serious postoperative complications have hampered its development. Factors, including neoadjuvant radiotherapy, anastomotic height, and tumor stage may negatively affect anastomotic leakage and bowel function [68,69,70,71]. Unfortunately, data from different studies were inconsistent, and we could not obtain detailed data for further analysis.
Postoperative bowel function is an important indicator of clinical efficacy. According to this meta-analysis, there was no statistically significant difference in the defecation frequency among the groups at 3 and 24 months postoperatively, with the former possibly related to high rectal sensitivity and poor adaptation in the early postoperative period and the latter with adaptation having reached equilibrium over time. At 6 and 12 months postoperatively, there was no statistically significant difference in the defecation frequency among the CJP, TCP, and SEA groups. However, all were significantly lower than that of the SCA group, with the CJP group being first. The J-shaped pouch of the CJP and the lateral limb of the SEA, as well as coloplasty, improved fecal function to some extent after increasing the volume of the “new rectum” and decreasing peristaltic waves. In a prospective RCT by Okkabaz et al. [40], a 1-year postoperative follow-up found that the number of daytime and nighttime bowel movements was essentially the same in the CJP and SEA groups, and the difference in the fecal incontinence severity index (FISI) was not statistically significant. These results are in agreement with those of Ahmed et al. [72] and Markovic et. [73] RCTs. However, a recent RCT found that SEA and CJP were not equally effective in improving postoperative bowel function [74]. Sixty patients with rectal cancer were randomly assigned to the CJP, SCA, and SEA groups. Follow-up 6 months after surgery, revealed that 70% of patients in the CJP group had normal bowel frequency. In contrast, the number of patients with normal defecation frequency was significantly lower in the other two groups (10%, 19%, P < 0.001). However, the study had a small sample size, short follow-up time, high missed follow-up rate, and variations in the proportion of radiotherapy among the groups, which somewhat diminished the credibility of the findings.
Regarding fecal urgency, incomplete defecation, and the use of antidiarrheal medication, we did not find a consistent advantage for any of the anastomoses. Early studies found that CJP caused incomplete defecation, but after years of clinical practice, surgeons showed that a 5–6-cm J-shaped pouch has the same defecation frequency as an 8–10-cm J-shaped pouch and significantly reduces stool retention and the use of laxatives and enemas [75, 76]. Most of the studies in this trial used smaller J-shaped pouches, the volume of which did not differ significantly from a 4–6 cm SEA’s lateral limb. Although we only pooled data on incomplete defecation at 6 and 12 months after surgery, it is sufficient to show that smaller J-shaped pouches have little effect. In a large RCT in Switzerland, 112 patients were randomly assigned to each intervention group (CJP, SEA, SCA), and no differences in composite evacuation and incontinence scores were found after 24 months of follow-up [77]. Brown et al. [17] conducted a systematic review of gastrointestinal reconstruction modalities after low anterior resection for rectal cancer and found that CJP improved bowel function for up to 2 years. Hüttner et al. [18] conducted a meta-analysis of bowel function outcomes and concluded that CJP, TCP, and SEA had better functional outcomes than SCA in the first postoperative year. However, their pooled data were divided into three stages: early (8 months), intermediate (8–18 months), and late (>18 months), and their conclusions may be uncertain. As a result, we addressed this shortcoming by statistically analyzing bowel function results at 3, 6, 12, and 24 months after surgery, respectively. From the results of our network meta-analysis, bowel function in CJP, TCP, and SEA is comparable and can be improved for 1–2 years compared with that of SCA. However, it is still difficult to definitively say which CJP and SEA is superior or inferior in terms of bowel function. Bowel function outcomes may be comparable with similar anatomical structures. Whether SEA can provide the same or better bowel function outcome as CJP in patients with rectal cancer deserves further validation through high-quality studies.
One of the primary goals of evolving rectal cancer treatment is improving the patient’s quality of life. We discovered that severe postoperative complications and bowel dysfunction do not positively correlate with the quality of life. Most patients have a higher quality of life than expected from their bowel function outcomes. Table 3 shows that five of the nine studies included did not find a statistical difference among the anastomoses. This may be because most patients with rectal cancer have become accustomed to living with bowel dysfunction before surgery and are not as severely impacted as those who do not. A multicenter prospective study assessed the quality of life and bowel function in the CJP (190 patients) and SCA groups (189 patients) 24 months after surgery and found that postoperative scores on each questionnaire were lower than baseline in both groups. However, there were no significant differences in either group [78]. Another multicenter, randomized, phase III trial (SAKK 40/04) found clinically relevant short-term deterioration in the trial outcome index (primary quality of life endpoint) in the SCA and SEA groups 6 months after surgery [79]. In contrast, scores in the CJP group remained relatively stable throughout the observation period. In addition, at 12 months, there was a significant difference in colorectal cancer symptom (secondary quality of life endpoint) scores between the SCA and CJP groups (P = 0.007). The results of the available studies show that the four anastomoses have a similar impact on patient’s quality of life after surgery, with possible short-term quality of life benefits for patients with J-shaped pouches; however, CJP may result in poorer sexual function in male patients. Therefore, when selecting surgical procedures for patients, particularly male patients, clinicians should consider the patient’s specific situation and the surgeon’s preferences.
Strengths, limitations, and prospects
This systematic review integrated recent RCTs to rank postoperative complications and bowel function outcomes in rectal cancer by a network meta-analysis, giving an up-to-date basis for the anastomoses selection following rectal cancer surgery. However, some limitations limited the interpretation of our findings. First, the early trials included in this network meta-analysis were primarily single-center small-sample studies with short follow-up times and the inability to be double-blinded in clinical trials, which impacted the pooled results. Second, discrepancies in bowel dysfunction definition, measurement, and assessment scales resulted in a high level of inter-study heterogeneity in the comparison. Furthermore, some researchers have exaggerated the superiority of modified anastomosis, resulting in general publication bias in bowel function studies. Third, fecal incontinence, laxative use, enema use, anorectal pressure, overall survival, and disease-free survival, all of which are closely related to the quality of life of patients with rectal cancer, were not summarized in this network meta-analysis, and the conclusions may be limited.
Future studies should first standardize the definition of various lesions. A comprehensive, universal, and well-validated international tool should be designed to facilitate communication and dissemination of research results between different regions. Second, more long-term multicenter RCTs are required to investigate the effects of different anastomoses on patient’s quality of life and sexual and urological function.
Conclusions
Our systematic review of postoperative complications and bowel function in rectal cancer revealed that SEA has the lowest risk of complications and the best safety profile. Six months after surgery, the CJP and SEA were identical in defecation frequency, and other indicators of bowel function were similar. We also discovered that TCP is predisposed to complications, with SCA resulting in significantly more frequent postoperative bowel movements. Furthermore, the different anastomoses did not significantly impact the patient’s quality of life. However, the heterogeneity of bowel function studies undermines the credibility of the findings. In the future, more in-depth evaluations of the benefits and risks of various anastomoses in the long-term, high-quality studies are required.
Availability of data and materials
All data generated or analyzed during this study are included in this article (and its additional file).
Abbreviations
- CJP:
-
Colon J-pouch
- SCA:
-
Straight colorectal anastomosis
- TCP:
-
Transverse coloplasty
- SEA:
-
Side-to-end anastomosis
- DIC:
-
Deviance information criterion
- SUCRA:
-
Surface under the cumulative ranking curve
- LAR:
-
Low anterior resection
- TME:
-
Total mesorectal excision
- RCTs:
-
Randomized controlled trials
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RR:
-
Risk ratio
- MD:
-
Mean difference
- CI:
-
Confidence interval
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Hashimoto S, Hamada K, Sumida Y, Araki M, Wakata K, Kugiyama T, et al. Postoperative complications predict long-term outcome after curative resection for perforated colorectal cancer. In Vivo. 2021;35(1):555–61.
Nguyen TH, Chokshi RV. Low anterior resection syndrome. Curr Gastroenterol Rep. 2020;22(10):48.
Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol. 2012;13(9):e403–8.
Keane C, Wells C, O'Grady G, Bissett IP. Defining low anterior resection syndrome: a systematic review of the literature. Color Dis. 2017;19(8):713–22.
Arnarson Ö, Butt-Tuna S, Syk I. Postoperative complications following colonic resection for cancer are associated with impaired long-term survival. Color Dis. 2019;21(7):805–15.
Planellas P, Farrés R, Cornejo L, Rodríguez-Hermosa JI, Pigem A, Timoteo A, et al. Randomized clinical trial comparing side to end vs end to end techniques for colorectal anastomosis. Int J Surg. 2020;2020(83):220–9.
Zeman M, Czarnecki M, Chmielik E, Idasiak A, Skałba W, Strączyński M, et al. The assessment of risk factors for long-term survival outcome in ypN0 patients with rectal cancer after neoadjuvant therapy and radical anterior resection. World J Surg Oncol. 2021;19(1):154.
Chen TY, Wiltink LM, Nout RA, Meershoek-Klein Kranenbarg E, Laurberg S, Marijnen CA, et al. Bowel function 14 years after preoperative short-course radiotherapy and total mesorectal excision for rectal cancer: report of a multicenter randomized trial. Clin Colorectal Cancer. 2015;14(2):106–14.
Rasulov AO, Baichorov AB, Merzlykova AM, Ovchinnikova AI, Semyanikhina AV. Surgical treatment of low anterior resection syndrome. Khirurgiia. 2020;11:53–60.
Alvandipour M, Karami MY, Khodabakhsh M. Colonic J-pouch, straight colorectal and side-to-end anastomosis procedures in rectal cancer: a randomised, prospective, singleblind, parallel single centre clinical trial. Color Dis. 2020;22(Suppl 3):55–6.
Madyarov J, Rasulov A, Baichorov A. Short-term and long-term outcomes of J-pouch vs side-to-end vs end-to-end colorectal anastomoses after total mesorectal excision for rectal carcinoma: a randomized trial. Eur J Surg Oncol. 2019;45(2):e3.
Lazorthes F, Fages P, Chiotasso P, Lemozy J, Bloom E. Resection of the rectum with construction of a colonic reservoir and colo-anal anastomosis for carcinoma of the rectum. Br J Surg. 1986;73(2):136–8.
Parc R, Tiret E, Frileux P, Moszkowski E, Loygue J. Resection and colo-anal anastomosis with colonic reservoir for rectal carcinoma. Br J Surg. 1986;73(2):139–41.
Z'Graggen K, Maurer CA, Mettler D, Stoupis C, Wildi S, Büchler MW. A novel colon pouch and its comparison with a straight coloanal and colon J-pouch--anal anastomosis: preliminary results in pigs. Surgery. 1999;125(1):105–12.
Baker JW. Low end to side rectosigmoidal anastomosis; description of technic. Arch Surg (1920). 1950;61(1):143–57.
Brown CJ, Fenech D, McLeod RS. Reconstructive techniques after rectal resection for rectal cancer. Cochrane Database Syst Rev. 2008;2008(2):CD006040.
Hüttner FJ, Tenckhoff S, Jensen K, Uhlmann L, Kulu Y, Büchler MW, et al. Meta-analysis of reconstruction techniques after low anterior resection for rectal cancer. Br J Surg. 2015;102(7):735–45.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Watt J, Tricco AC, Straus S, Veroniki AA, Naglie G, Drucker AM. Research techniques made simple: network meta-analysis. J Invest Dermatol. 2019;139(1):4–12.e11.
Du H, Bradbury TN, Lavner JA, Meltzer AL, McNulty JK, Neff LA, et al. A comparison of Bayesian synthesis approaches for studies comparing two means: a tutorial. Res Synth Methods. 2020;11(1):36–65.
Spiegelhalter DJ, Best NG, Carlin BR, van der Linde A. Bayesian measures of model complexity and fit. J R Statist Soc B. 2002;64(4):583–616.
Donegan S, Dias S, Welton NJ. Assessing the consistency assumptions underlying network meta-regression using aggregate data. Res Synth Methods. 2019;10(2):207–24.
Shih MC, Tu YK. An evidence-splitting approach to evaluation of direct-indirect evidence inconsistency in network meta-analysis. Res Synth Methods. 2021;12(2):226–38.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Kiefer C, Sturtz S, Bender R. A simulation study to compare different estimation approaches for network meta-analysis and corresponding methods to evaluate the consistency assumption. BMC Med Res Methodol. 2020;20(1):36.
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One. 2013;8(10):e76654.
Ho YH, Tan M, Leong AF, Seow-Choen F. Ambulatory manometry in patients with colonic J-pouch and straight coloanal anastomoses: randomized, controlled trial. Dis Colon Rectum. 2000;43(6):793–9.
Ho YH, Seow-Choen F, Tan M. Colonic J-pouch function at six months versus straight coloanal anastomosis at two years: randomized controlled trial. World J Surg. 2001;25(7):876–81.
Machado M, Nygren J, Goldman S, Ljungqvist O. Similar outcome after colonic pouch and side-to-end anastomosis in low anterior resection for rectal cancer: a prospective randomized trial. Ann Surg. 2003;238(2):214–20.
Machado M, Nygren J, Goldman S, Ljungqvist O. Functional and physiologic assessment of the colonic reservoir or side-to-end anastomosis after low anterior resection for rectal cancer: a two-year follow-up. Dis Colon Rectum. 2005;48(1):29–36.
Hallböök O, Påhlman L, Krog M, Wexner SD, Sjödahl R. Randomized comparison of straight and colonic J pouch anastomosis after low anterior resection. Ann Surg. 1996;224(1):58–65.
Fazio VW, Zutshi M, Remzi FH, Parc Y, Ruppert R, Fürst A, et al. A randomized multicenter trial to compare long-term functional outcome, quality of life, and complications of surgical procedures for low rectal cancers. Ann Surg. 2007;246(3):481–8.
Doeksen A, Bakx R, Vincent A, van Tets WF, Sprangers MAG, Gerhards MF, et al. J-pouch vs side-to-end coloanal anastomosis after preoperative radiotherapy and total mesorectal excision for rectal cancer: a multicentre randomized trial. Color Dis. 2012;14(6):705–13.
Parc Y, Ruppert R, Fuerst A, Golcher H, Zutshi M, Hull T, et al. Better function with a Colonic J-Pouch or a side-to-end anastomosis?: a randomized controlled trial to compare the complications, functional outcome, and quality of life in patients with low rectal cancer after a J-Pouch or a side-to-end anastomosis. Ann Surg. 2019;269(5):815–25.
Pucciarelli S, Del Bianco P, Pace U, Bianco F, Restivo A, Maretto I, et al. Multicentre randomized clinical trial of colonic J pouch or straight stapled colorectal reconstruction after low anterior resection for rectal cancer. Br J Surg. 2019;106(9):1147–55.
Biondo S, Frago R, Codina Cazador A, Farres R, Olivet F, Golda T, et al. Long-term functional results from a randomized clinical study of transverse coloplasty compared with colon J-pouch after low anterior resection for rectal cancer. Surgery. 2013;153(3):383–92.
Liang JT, Lai HS, Lee PH, Huang KC. Comparison of functional and surgical outcomes of laparoscopic-assisted colonic J-pouch versus straight reconstruction after total mesorectal excision for lower rectal cancer. Ann Surg Oncol. 2007;14(7):1972–9.
Okkabaz N, Haksal M, Atici AE, Altuntas YE, Gundogan E, Gezen FC, et al. J-pouch vs. side-to-end anastomosis after hand-assisted laparoscopic low anterior resection for rectal cancer: a prospective randomized trial on short and long term outcomes including life quality and functional results. Int J Surg. 2017;2017(47):4–12.
Ortiz H, De Miguel M, Armendáriz P, Rodriguez J, Chocarro C. Coloanal anastomosis: are functional results better with a pouch? Dis Colon Rectum. 1995;38(4):375–7.
Fürst A, Burghofer K, Hutzel L, Jauch KW. Neorectal reservoir is not the functional principle of the colonic J-pouch: the volume of a short colonic J-pouch does not differ from a straight coloanal anastomosis. Dis Colon Rectum. 2002;45(5):660–7.
Pimentel JM, Duarte A, Gregório C, Souto P, Patrício J. Transverse coloplasty pouch and colonic J-pouch for rectal cancer - A comparative study. Color Dis. 2003;5(5):465–70.
Park JG, Lee MR, Lim SB, Hong CW, Yoon SN, Kang SB, et al. Colonic J-pouch anal anastomosis after ultralow anterior resection with upper sphincter excision for low-lying rectal cancer. World J Gastroenterol. 2005;11(17):2570–3.
Stratilatovas E, Sangaila E, Sinkevičius Z, Burneckis A, Poškus E, Strupas K. A randomized multicenter trial to compare functional outcome and complications of surgical procedures for low rectal cancers. Acta Med Litu. 2011;18(1):37–42.
Tsunoda A, Kamiyama G, Suzuki N, Watanabe M, Narita K, Nakao K, et al. Side-to-end vs. colonic pouch vs. end-to-end anastomosis in low anterior resection. Showa Univ. J Med Sci. 2008;20(2):61–8.
Brisinda G, Vanella S, Cadeddu F, Civello IM, Brandara F, Nigro C, et al. End-to-end versus end-to-side stapled anastomoses after anterior resection for rectal cancer. J Surg Oncol. 2009;99(1):75–9.
Ho YH, Tan M, Seow-Choen F. Prospective randomized controlled study of clinical function and anorectal physiology after low anterior resection: comparison of straight and colonic J pouch anastomoses. Br J Surg. 1996;83(7):978–80.
Ho YH, Brown S, Heah SM, Tsang C, Seow-Choen F, Eu KW, et al. Comparison of J-pouch and coloplasty pouch for low rectal cancers: a randomized, controlled trial investigating functional results and comparative anastomotic leak rates. Ann Surg. 2002;236(1):49–55.
Parray FQ, Farouqi U, Wani ML, Chowdri NA, Shaheen FP. Colonic J pouch neo-rectum versus straight anastomosis for low rectal cancers. Indian J Cancer. 2014;51(4):560–4.
Huber FT, Herter B, Siewert JR. Colonic pouch vs. side-to-end anastomosis in low anterior resection. Dis Colon Rectum. 1999;42(7):896–902.
Oya M, Komatsu J, Takase Y, Nakamura T, Ishikawa H. Comparison of defecatory function after colonic J-pouch anastomosis and straight anastomosis for stapled low anterior resection: results of a prospective randomized trial. Surg Today. 2002;32(2):104–10.
Sailer M, Fuchs KH, Fein M, Thiede A. Randomized clinical trial comparing quality of life after straight and pouch coloanal reconstruction. Br J Surg. 2002;89(9):1108–17.
Jiang JK, Yang SH, Lin JK. Transabdominal anastomosis after low anterior resection: a prospective, randomized, controlled trial comparing long-term results between side-to-end anastomosis and colonic J-pouch. Dis Colon Rectum. 2005;48(11):2100–8 discussion 2108-2110.
Rybakov EG, Pikunov DY, Fomenko OY, Chernyshov SV, Shelygin YA. Side-to-end vs. straight stapled colorectal anastomosis after low anterior resection: results of randomized clinical trial. Int J Color Dis. 2016;31(8):1419–26.
Ulrich AB, Seiler CM, Z'Graggen K, Löffler T, Weitz J, Büchler MW. Early results from a randomized clinical trial of colon J pouch versus transverse coloplasty pouch after low anterior resection for rectal cancer. Br J Surg. 2008;95(10):1257–63.
Seow-Choen F, Goh HS. Prospective randomized trial comparing J colonic pouch-anal anastomosis and straight coloanal reconstruction. Br J Surg. 1995;82(5):608–10.
Hou S, Wang Q, Zhao S, Liu F, Guo P, Ye Y. Safety and efficacy of side-to-end anastomosis versus colonic J-pouch anastomosis in sphincter-preserving resections: an updated meta-analysis of randomized controlled trials. World J Surg Oncol. 2021;19(1):130.
Wang Z. Colonic J-pouch versus side-to-end anastomosis for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. BMC Surg. 2021;21(1):331.
Furnée EJB, Aukema TS, Oosterling SJ, Borstlap WAA, Bemelman WA, Tanis PJ. Influence of conversion and anastomotic leakage on survival in rectal cancer surgery; retrospective cross-sectional study. J Gastrointest Surg. 2019;23(10):2007–18.
Koedam TWA, Bootsma BT, Deijen CL, van de Brug T, Kazemier G, Cuesta MA, et al. Oncological outcomes after anastomotic leakage after surgery for colon or rectal cancer: increased risk of local recurrence. Ann Surg. 2022;275(2):e420–7.
Arron MNN, Greijdanus NG, Bastiaans S, Vissers PAJ, Verhoeven RHA, Ten Broek RPG, et al. Long-term oncological outcomes after colorectal anastomotic leakage: a retrospective dutch population-based study. Ann Surg. 2022;276(5):882–9.
Fang C, Nie P, Jing P, Zhang Y, Yang L, Yu Y, et al. Effects of adjuvant therapy compliance and anastomotic leakage on the oncologic outcomes of patients with rectal cancer after curative resection. Dis Colon Rectum. 2021;64(6):689–96.
Zaman S, Mohamedahmed AYY, Ayeni AA, Peterknecht E, Mawji S, Albendary M, et al. Comparison of the colonic J-pouch versus straight (end-to-end) anastomosis following low anterior resection: a systematic review and meta-analysis. Int J Color Dis. 2022;37(4):919–38.
Chen ZZ, Li YD, Huang W, Chai NH, Wei ZQ. Colonic pouch confers better bowel function and similar postoperative outcomes compared to straight anastomosis for low rectal cancer. World J Gastrointest Surg. 2021;13(3):303–14.
Kato H, Ishida T, Nitori N, Kato A, Tamura T, Imai S, et al. Efficacy of side-to-end anastomosis to prevent anastomotic leakage after anterior resection for rectal cancer. Mol Clin Oncol. 2022;16(2):44.
McKechnie T, Sharma S, Daniel R, Eskicioglu C. End-to-end versus end-to-side anastomosis for low anterior resection: a systematic review and meta-analysis of randomized controlled trials. Surgery. 2021;170(2):397–404.
Ye L, Huang M, Huang Y, Yu K, Wang X. Risk factors of postoperative low anterior resection syndrome for colorectal cancer: a meta-analysis. Asian J Surg. 2022;45(1):39–50.
Dulskas A, Kavaliauskas P, Pilipavicius L, Jodinskas M, Mikalonis M, Samalavicius NE. Long-term bowel dysfunction following low anterior resection. Sci Rep. 2020;10(1):11882.
Kauff DW, Roth YDS, Bettzieche RS, Kneist W. Fecal incontinence after total mesorectal excision for rectal cancer-impact of potential risk factors and pelvic intraoperative neuromonitoring. World J Surg Oncol. 2020;18(1):12.
Pilkington SA, Bhome R, Gilbert S, Harris S, Richardson C, Dudding TC, et al. Sequential assessment of bowel function and anorectal physiology after anterior resection for cancer: a prospective cohort study. Color Dis. 2021;23(9):2436–46.
Ahmed A, Khan R, Shaikh SF, Majeed S. Comparison of side-to-end with end-to-end Anastomosis technique for colorectal anastomosis. Pak. J Med Sci. 2021;15(12):3537–9.
Markovic V, Dimitrijevic I, Barisic G, Krivokapic Z. Comparison of functional outcome of colonic J-pouch and latero-terminal anastomosis in low anterior resection for rectal cancer. Srp Arh Celok Lek. 2015;143(3-4):158–61.
Alvandipour M, Godazandeh G, Khodabakhsh E, Karami MY, Moradi S, Borna S. Comparison of performance and clinical outcome of three methods of straight, side-to-end, and colonic j-pouch colorectal anastomosis in patients with rectal cancer. J Babol Univ Med Sci. 2021;23(1):244–51.
Hida J, Yasutomi M, Fujimoto K, Okuno K, Ieda S, Machidera N, et al. Functional outcome after low anterior resection with low anastomosis for rectal cancer using the colonic J-pouch. Prospective randomized study for determination of optimum pouch size. Dis Colon Rectum. 1996;39(9):986–91.
Toiyama Y, Kusunoki M. Changes in surgical therapies for rectal cancer over the past 100 years: a review. Ann Gastroenterol Surg. 2020;4(4):331–42.
Marti WR, Curti G, Wehrli H, Grieder F, Graf M, Gloor B, et al. Clinical outcome after rectal replacement with side-to-end, Colon-J-Pouch, or straight colorectal anastomosis following total mesorectal excision: a Swiss Prospective, Randomized, Multicenter Trial (SAKK 40/04). Ann Surg. 2019;269(5):827–35.
Gavaruzzi T, Pace U, Giandomenico F, Pucciarelli S, Bianco F, Selvaggi F, et al. Colonic J-pouch or straight colorectal reconstruction after low anterior resection for rectal cancer: Impact on quality of life and bowel function: a multicenter prospective randomized study. Dis Colon Rectum. 2020;63(11):1511–23.
Ribi K, Marti WR, Bernhard J, Grieder F, Graf M, Gloor B, et al. Quality of life after total mesorectal excision and rectal replacement: comparing side-to-end, colon J-Pouch and straight colorectal reconstruction in a randomized, Phase III Trial (SAKK 40/04). Ann Surg Oncol. 2019;26(11):3568–76.
Acknowledgements
None.
Funding
The authors have no financial support to declare.
Author information
Authors and Affiliations
Contributions
HL drafted the manuscript and performed the statistical analysis; MX and YZ searched articles and collected the data; YS and ZP interpreted the data, assessed the risk of the study, and CL designed, revised, and guided this study. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Checklist of the PRISMA extension for network meta-analysis. Supplementary Table 2. Number of citations by each database searched. Supplementary Table 3. Characteristics of the 29 studies included in the network Meta-analysis. Supplementary Fig. 1. Risk-of-bias summary of the randomized controlled trials. Supplementary Table 4. Quality assessment of included randomized controlled trials. Supplementary Table 5. Results of global heterogeneity and local heterogeneity. Supplementary Table 6. Node-splitting analysis of inconsistency. Supplementary Table 7. Comparisons of the fitness of consistency and inconsistency models using deviance information criteria. Supplementary Fig. 2. Results of pairwise meta-analysis for postoperative complications. Supplementary Fig. 3. Results of pairwise meta-analysis for defecation frequency. Supplementary Fig. 4. Results of pairwise meta-analysis for bowel function. Supplementary Table 8A. Relative effects table for postoperative anastomotic leakage. Supplementary Table 8B. Rank probabilities for postoperative anastomotic leakage. Supplementary Fig. 5B. Comparison-adjusted funnel plot for postoperative anastomotic leakage. Supplementary Fig. 6A. Network plot for postoperative anastomotic stricture. Supplementary Table 9A. Relative effects table for postoperative anastomotic stricture. Supplementary Table 9B. Rank probabilities for postoperative anastomotic stricture. Supplementary Fig. 6B. Comparison-adjusted funnel plot for postoperative anastomotic stricture. Supplementary Fig. 7A. Network plot postoperative reoperation. Supplementary Table 10A. Relative effects table for postoperative reoperation. Supplementary Table 10B. Rank probabilities for postoperative reoperation. Supplementary Fig. 7B. Comparison-adjusted funnel plot for postoperative reoperation. Supplementary Fig. 8A. Network plot for postoperative mortality within 30 days. Supplementary Table 11A. Relative effects table for postoperative mortality within 30 days. Supplementary Table 11B. Rank probabilities for postoperative mortality within 30 days. Supplementary Fig. 8B. Comparison-adjusted funnel plot for postoperative mortality within 30 days. Supplementary Fig. 9A. Network plot for defecation frequency at 3 months postoperatively. Supplementary Table 12B. Rank probabilities for defecation frequency at 3 months postoperatively. Supplementary Fig. 9B. Comparison-adjusted funnel plot for defecation frequency at 3 months postoperatively. Supplementary Fig. 10A. Network plot for fecal urgency at 3 months postoperatively. Supplementary Table 13A. Relative effects table for fecal urgency at 3 months postoperatively. Supplementary Table 13B. Rank probabilities for fecal urgency at 3 months postoperatively. Supplementary Fig. 10B. Comparison-adjusted funnel plot for fecal urgency at 3 months postoperatively. Supplementary Fig. 11A. Network plot for use of antidiarrheal medication at 3 months postoperatively. Supplementary Table 14A. Relative effects table for use of antidiarrheal medication at 3 months postoperatively. Supplementary Table 14B. Rank probabilities for use of antidiarrheal medication at 3 months postoperatively. Supplementary Fig. 11B. Comparison-adjusted funnel plot for use of antidiarrheal medication at 3 months postoperatively. Supplementary Fig. 12A. Network plot for defecation frequency at 6 months postoperatively. Supplementary Table 15B. Rank probabilities for defecation frequency at 6 months postoperatively. Supplementary Fig .12B. Comparison-adjusted funnel plot for defecation frequency at 6 months postoperatively. Supplementary Fig. 13A. Network plot for fecal urgency at 6 months postoperatively. Supplementary Table 16A. Relative effects table for fecal urgency at 6 months postoperatively. Supplementary Table 16B. Rank probabilities for fecal urgency at 6 months postoperatively. Supplementary Fig. 13B. Comparison-adjusted funnel plot for fecal urgency at 6 months postoperatively. Supplementary Fig. 14A. Network plot for incomplete defecation at 6 months postoperatively. Supplementary Table 17A. Relative effects table for incomplete defecation at 6 months postoperatively. Supplementary Table 17B. Rank probabilities for incomplete defecation at 6 months postoperatively. Supplementary Fig. 14B. Comparison-adjusted funnel plot for incomplete defecation at 6 months postoperatively. Supplementary Fig. 15A. Network plot for use of antidiarrheal medication at 6 months postoperatively. Supplementary Table 18A. Relative effects table for use of antidiarrheal medication at 6 months postoperatively. Supplementary Table 18B. Rank probabilities for use of antidiarrheal medication at 6 months postoperatively. Supplementary Fig. 15B. Comparison-adjusted funnel plot for use of antidiarrheal medication at 6 months postoperatively. Supplementary Fig. 16A. Network plot for defecation frequency at 12 months postoperatively. Supplementary Table 19B. Rank probabilities for defecation frequency at 12 months postoperatively. Supplementary Fig. 16B. Comparison-adjusted funnel plot for defecation frequency at 12 months postoperatively. Supplementary Fig. 17A. Network plot for fecal urgency at 12 months postoperatively. Supplementary Table 20A. Relative effects table for fecal urgency at 12 months postoperatively. Supplementary Table 20B. Rank probabilities for fecal urgency at 12 months postoperatively. Supplementary Fig. 17B. Comparison-adjusted funnel plot for fecal urgency at 12 months postoperatively. Supplementary Fig. 18A. Network plot for incomplete defecation at 12 months postoperatively. Supplementary Table 21A. Relative effects table for incomplete defecation at 12 months postoperatively. Supplementary Table 21B. Rank probabilities for incomplete defecation at 12 months postoperatively. Supplementary Fig. 18B. Comparison-adjusted funnel plot for incomplete defecation at 12 months postoperatively. Supplementary Fig. 19A. Network plot for use of antidiarrheal medication at 12 months postoperatively. Supplementary Table 22A. Relative effects table for use of antidiarrheal medication at 12 months postoperatively. Supplementary Table 22B. Rank probabilities for use of antidiarrheal medication at 12 months postoperatively. Supplementary Fig. 19B. Comparison-adjusted funnel plot for use of antidiarrheal medication at 12 months postoperatively. Supplementary Fig. 20A. Network plot for defecation frequency at 24 months postoperatively. Supplementary Table 23B. Rank probabilities for defecation frequency at 24 months postoperatively. Supplementary Fig. 20B. Comparison-adjusted funnel plot for defecation frequency at 24 months postoperatively. Supplementary Fig. 21A. Network plot for use of antidiarrheal medication at 24 months postoperatively. Supplementary Table 24A. Relative effects table for use of antidiarrheal medication at 24 months postoperatively. Supplementary Table 24B. Rank probabilities for use of antidiarrheal medication at 24 months postoperatively. Supplementary Fig. 21B. Comparison-adjusted funnel plot for use of antidiarrheal medication at 24 months postoperatively. Supplementary Table 25A. Relative effects table for postoperative anastomotic leakage in the sensitivity analysis. Supplementary Table 25B. Rank probabilities for postoperative anastomotic leakage in the sensitivity analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, H., Xiong, M., Zeng, Y. et al. Comparison of complications and bowel function among different reconstruction techniques after low anterior resection for rectal cancer: a systematic review and network meta-analysis. World J Surg Onc 21, 87 (2023). https://doi.org/10.1186/s12957-023-02977-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-02977-z