Abstract
Background
This study aimed to synthesize and quantitatively examine Health State Utility Values (HSUVs) for Type 2 Diabetes Mellitus (T2DM) and its complications, providing a robust meta-regression framework for selecting appropriate HSUV estimates.
Method
We conducted a systematic review to extract HSUVs for T2DM and its complications, encompassing various influencing factors. Relevant literature was sourced from a review spanning 2000-2020, supplemented by literature from PubMed, Embase, and the Web of Science (up to March 2024). Multivariate meta-regression was performed to evaluate the impact of measurement tools, tariffs, health status, and clinical and demographic variables on HSUVs.
Results
Our search yielded 118 studies, contributing 1044 HSUVs. The HSUVs for T2DM with complications varied, from 0.65 for cerebrovascular disease to 0.77 for neuropathy. The EQ-5D-3L emerged as the most frequently employed valuation method. HSUV differences across instruments were observed; 15-D had the highest (0.89), while HUI-3 had the lowest (0.70) values. Regression analysis elucidated the significant effects of instrument and tariff choice on HSUVs. Complication-related utility decrement, especially in diabetic foot, was quantified. Age <70 was linked to increased HSUVs, while longer illness duration, hypertension, overweight and obesity correlated with reduced HSUVs.
Conclusion
Accurate HSUVs are vital for the optimization of T2DM management strategies. This study provided a comprehensive data pool for HSUVs selection, and quantified the influence of various factors on HSUVs, informing analysts and policymakers in understanding the utility variations associated with T2DM and its complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health state utility values (HSUVs) quantify the degree of preference for a particular health state [1]. In the model-based economic evaluations, the acquisition of precise HSUVs for various health states is crucial. HSUVs are utilised to integrated survival time and quality of life into Quality Adjusted Life Years (QALYs), which are integral to the evidence base in pharmacoeconomic analyses [2]. These values can be gauged through direct or indirect methods, with the resulting figures needing to be aligned with a standard value tariff derived from the general population to determine the equivalent HSUVs. The choice of measurement instruments and value sets can significantly influence HSUVs. Moreover, patient demographics, the treatments, and the distinct health outcomes associated with different complications are key factors that influence HSUVs. Research indicates that 36% of the HSUVs cited in existing literature have to be adjusted due to a lack of clarity; variables such as age, sex, and side effects can markedly affect the magnitudes of HSUVs [3]. Thus, the careful selection of HSUVs is pivotal in diminishing uncertainty within economic modelling.
The prevalence of type 2 diabetes (T2DM) is extensive [4], serving as a principal catalyst for global mortality rates [5]. As T2DM progresses, it often gives rise to multiple complications that can significantly degrade quality of life and may even result in mortality [6, 7]. This widespread condition consequently incurs substantial health resource utilisation. The tension between this immense financial strain and constrained healthcare resources necessitates that health systems perform health technology appraisals, particularly economic evaluations, for therapeutic agents, including the evaluation of new medications that are continuously introduced. Such evaluations are vital for the judicious distribution of societal resources and for extending benefits to a broader patient demographic. This underscores the necessity for the judicious selection of HSUVs for T2DM patients across different health states.
The research concerning the HSUVs of diabetes is densely populated with studies. Among these, the systematic review by Redenz et al. [8] assessed HSUVs of T2DM and its complications, summarising how complications, evaluative methodologies, and national backgrounds could influence outcomes. Mok et al. [9] built a suite of reference sets specifically for T2DM complications in East and Southeast Asia, attributing independent variables in study results to nationality, assessment instruments, and value sets. Jing et al. [10] found that several factors including physical activity, glucose monitoring frequency, co-morbidities or co-existing conditions such as hypertension, duration of diabetes, dietary patterns involving red meat, and mental health factors like depression, contributed to the variability in HSUVs for individuals with T2DM. While these investigations have recognised that patient characteristics, complications, nationality, reference sets, and assessment instruments bear upon the average health utility value, they have not quantified the statistical association between these diverse factors and HSUVs, nor have they offered concrete guidance for selecting HSUVs for T2DM in various decision-making contexts. Our research will build on these studies to further clarify the association between these factors and HSUVs of T2DM and provide guidance on choosing the proper HSUVs for the future.
Based on this notion, Wang et al. [11] conducted a systematic review and meta-regression to examine the association between health state utility values (HSUVs) and factors such as age, health status, treatments received, and timing of utility measurements. Age was used as an independent variable to assess its impact on HSUV in older women diagnosed with breast cancer. The study found that the mean HSUV declines as health status worsens, with age playing a significant role in determining health utility values in this population. Specifically, the study reported a decrease in breast cancer-specific utility of -0.001 per one-year increase in age (95% CI: -0.004, 0.002). This work highlights the effectiveness of meta-regression in exploring the relationships between patient demographics, treatment variables, and HSUV, and it serves as a methodological model for our current study. The purpose of this systematic review was to consolidate and quantitatively analyse through meta-regression the HSUVs associated with T2DM and its complications. The aim was to ascertain statistical associations and devise a statistical model [11, 12] that will enable analysts to select health utility value estimates that are most pertinent to their specific policy or clinical decision-making contexts.
Method
The systematic review aimed to identify previously published studies reporting HSUVs for T2DM and its complications according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020) [13]. The protocol was PROSPERO-registered (CRD42023432948).
Inclusion and exclusion criteria
Eligibility for inclusion required articles to (1) report health state utility values (HSUVs) of T2DM; (2) use either direct or indirect methods for HSUVs assessment of the participants; (3) be published in the English language. Articles were excluded for the following reasons: (1) Inclusion of participants who were pregnant or diagnosed with gestational diabetes. (2) Lack of separate reporting for T1DM and T2DM. (3) Document participants’ health status without corresponding utility value estimations. (4) Studies that do not involve original human research, including reviews, reports, conference proceedings, and guidelines. (5) Non-English publications.
Literature search
The search for studies adhering to our inclusion criteria was conducted in two distinct phases. Initially, studies published from January 2000 to April 2020 were identified from the systematic review by Redenz et al. (2023) [8] and its related journal articles. This review comprehensively identified T2DM and its complications’ HSUVs measured using preference-based instruments (such as Standard-Gamble (SG), Time Trade-Off (TTO), the Health Utilities Index mark 3 (HUI-3), the Three-Level EuroQol Five-Dimensional Questionnaire (EQ-5D-3L) and the Five-Level EuroQol Five-Dimensional Questionnaire (EQ-5D-5L)) through three steps: (1) structured search in electronic databases including MEDLINE and Cochrane Library; (2) a free-term search in the School of Health and Related Research Health Utilities Database (ScHARRHUD); (3) a complementary search from the references of previously published systematic review and journal articles. This study shared similar inclusion and exclusion criteria as well as search strategies to those used in the review by Redenz et al. (2023) [8]. To ensure comprehensive coverage of the literature, we searched mainstream medical databases. Given the alignment in focus, the review by Redenz et al. (2023) [8] served as a valuable source for identifying studies reporting T2DM HSUV from 2000 to 2020. From this initial collection of references, we identified and retrieved studies that utilized direct or indirect instruments to measure HSUV for full-text review.
In the second stage, we conducted a comprehensive search through PubMed, Embase, and Web of Science database using a structured strategy to aggregate all relevant literature on HSUVs for T2DM and its complications from inception to March 2024. (Supplementary Materials Appendix 1 and Appendix 2).
Study selection
Two independent reviewers (YRX & HTS) initially evaluated the titles and abstracts from the electronic database search based on pre-determined inclusion criteria. The level of agreement between reviewers was quantified using intra-class correlation coefficients (ICC) [14]. According to the ICC scale, values are interpreted as follows: below 0.50 indicates poor reliability, 0.50 to 0.75 suggests moderate reliability, 0.75 to 0.90 reflects good reliability, and above 0.90 represents excellent reliability [15]. The reviewers (YRX & HTS) assessed the full texts of studies that met the eligibility requirements. Any disagreements encountered during this phase were resolved by consulting a third reviewer (YW) to confirm the final selection of studies, ensuring stringent adherence to the inclusion and exclusion criteria throughout the review process.
Data extraction
All authors have agreed to develop a data extraction table beforehand. The data of interest should include the primary outcome and secondary outcomes. The primary outcome included the HSUVs of patients with T2DM and their complications [7, 16,17,18]. The secondary outcomes included (i) General characteristics of the patients, including gender, age, race, weight, blood pressure, and the duration since T2DM diagnosis etc. (ii) Characteristics of the study, e.g. the title, author(s), year of the study, country, country/region of respondents, research objectives, study design, sample size, sampling method, inclusion/exclusion criteria, selection and recruitment of respondents, and any other potential study issues. (iii) Health utility assessment methods, including diagnostic criteria for T2DM, instruments used for measuring HSUVs, value sets utilized, evaluation standards, statistical approaches.
Quality assessment
Given the absence of established reporting and evaluation criteria for assessing the quality of studies reporting HSUVs, it might be inappropriate to select an assessment list solely based on the design of the primary study [12, 19]. Quality assessment of HSUV studies may usefully focus on the selection and recruitment of respondents, inclusion and exclusion criteria, and the description of the background characteristics of the sample population from which value is derived [20]. To address this, we have extracted four questions (Table 1) from the 17-question evaluation tool developed by Nerich et al. [12, 21, 22] (Full appraisal tool in Appendix 3), which are tailored for assessing study quality. Zoratti et al.‘s systematic review of HSUV appraisal tools recognises these four items as being particularly suited for the critical evaluation of HSUV literature in health utility research [23].
Data synthesis
We describe the characteristics of the included subjects using descriptive statistics and present the key statistics of the HSUVs, including the mean (with standard deviation: SD or standard error: SE), median (with interquartile range: IQR), and the range of variation (or 95% confidence interval: 95% CI). The study results are presented in narrative and graphical form, with detailed categorization of the T2DM population according to different health conditions and instruments. For studies where SD were not directly given, the missing SD were estimated using the mean, sample size, SE, or 95% CI, as recommended by the Cochrane Library [24]. We attempted to integrate the acquired data using meta-analysis, but the variability of countries, measurement modalities, patient characteristics and characteristics of the disease itself made the integrated results highly heterogeneous and not directly usable; thus, the HSUVs were synthesized through a meta-regression following the methodology of Wang et al. (2022) [11] to determine the association between HSUVs and various independent variables. The large number of values identified for each state of T2DM allowed us to synthesize the data using meta-regression. We applied a linear regression model, with the average HSUV from each study serving as the dependent variable. The method was simple, pooled, ordinary least squares. Several variables that could potentially influence HSUVs were used as independent variables, and the rationale for selecting these variables is detailed below.
Factors such as complications, instruments, tariffs, nationality, and general patient characteristics, including hypertension and diabetes duration, could affect the measurement and valuation of HSUVs suggested from the reviews by MOK et al. [9], Jing et al. [10], and Redenz et al. [8]. Additionally, hyperglycaemia [25], the increase in body mass index (BMI) [26], and age [27] were considered significant risk factors for the development of T2DM. The analysis incorporated several variables that might influence HSUVs: disease health state, utility measurement instrument, valuation tariff, mean age, duration of diabetes, blood pressure, and BMI. Variables such as disease health state (e.g., T2DM or T2DM with cardiovascular disease), utility measurement instruments (e.g., EQ-5D-3L or EQ-5D-5L), and valuation tariffs (e.g., UK or US) were defined as categorical variables. Due to variations in how literature reports on mean age, diabetes duration, blood pressure, and BMI as continuous variables or intervals, the scarcity of literature on these variables was also defined as categorical variables. To avoid collinearity among categorical independent variables, other study characteristics such as the country of the study, the study design (clinical trials or observational study), and the study population were excluded from the meta-regression as independent variables. Treatment was also excluded if the treatments were not reported precisely.
Given the varying sample sizes and error magnitudes associated with each variable, the contributions of individual observations to changes in the regression model differed. To address this, we assigned more significant weight to values from studies with smaller SDs of the mean estimate than those with more significant SD. Consequently, we evaluated three regression model specifications. The first model specification used the estimated sample size of each HSUV as a weighting coefficient, recognizing that not all studies provided. The second specification employed the reciprocal of the estimated sample SD for each HSUV as the weighting coefficient, considering that studies with more minor SDs provided more reliable utility values. The third specification did not include any weighting coefficients. We used cluster-robust SEs to account for within-study correlations, given that some studies contributed multiple HSUVs to the meta-regression, which were likely to be correlated [28]. The coefficient of determination (R²) was used to assess the goodness of fit [29]. The meta-regression analysis used Stata 18.0 (Stata Corp, College Station, TX) [30].
Results
Selection of studies
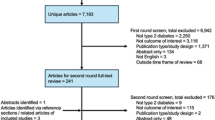
Seventy-six eligible articles were identified from the systematic review by Redenz et al. [8] and its related journal articles, and 6392 articles from the database search (Fig. 1). 118 studies met the inclusion criteria and were included in the systematic review. The inclusion process is illustrated in Fig. 1, and the reasons for exclusion are shown in Supplementary Appendix 4. The ICC value indicated good to excellent reliability between reviewers (The ICC between the two reviewers was 0.90).
Study characteristics
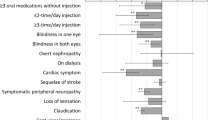
1044 HSUVs were collected from 118 manuscripts involving over 44 countries and regions (Table 2). Of 1044 HSUVs, 977 HSUVs reported mean values, of which 732 HSUVs reported mean values with SD and 245 only reported mean HSUVs without SD. 67 HSUVs reported median values with interquartile intervals. Of the 977 HSUVs that reported mean values, 25 health states were defined, including 11 complications: T2DM with cardiovascular diseases (n = 68, n means the number of the HSUVs), T2DM with cerebrovascular disease (n = 29), T2DM with diabetic foot (n = 9), T2DM with hypoglycemia (n = 22), T2DM with macrovascular disease (n = 5), T2DM with microvascular and macrovascular disease (n = 6), and T2DM with microvascular disease (n = 10), T2DM with nephropathy (n = 23), T2DM with neuropathy (n = 15), T2DM with peripheral vascular disease (n = 16), T2DM with retinopathy (n = 38). The pooled HSUVs for T2DM and each complication stratified by instrument are presented in Fig. 2. Of the 732 HSUVs reporting mean values with SD, 441 reported the HSUVs of T2DM with or without complications. The pooled HSUVs are presented in Fig. 3.
Of 977 HSUVs, nine different valuation instruments were used, with the EQ-5D-3L being the most widely used (n = 751), followed by the EQ-5D-5L (n = 122). Other instruments such as short-form 6-dimension (SF-6D) (n = 13), 15-dimension (15-D) (n = 1), SG(n = 2), the HUI mark 2 (HUI-2) (n = 9), HUI-3 (n = 50), feeling thermometer (FT) (n = 9), TTO (n = 20), etc. were applied less frequently. 31 different tariffs were applied, including EQ-5D-3L UK tariff (n = 263), EQ-5D-3L US tariff (n = 139), and EQ-5D-3L China tariff (n = 125) being the most widely used.
Among the 977 HSUVs, the T2DM without any complications (n = 14, mean:0.87; median:0.88; range: 0.78–0.95) had the highest mean HSUV. In contrast, the mean HSUV for patients with T2DM, with or without complications, was lower (n = 573, mean:0.80; median: 0.82; range: 0.39–0.95). For the subset of T2DM with complications, the mean HSUV were reported in the manuscripts (n = 22, mean: 0.65; median: 0.66; range: 0.52–0.88) [44, 65, 86, 118, 130, 139], which was lower than the estimate of the HSUV from all publications for T2DM patients with complications (n = 263, mean: 0.72; median: 0.72; range: 0.40–0.93). Of these 573 HSUVs, compared with HSUVs by EQ-5D-5L (n = 95, mean: 0.83; median: 0.83; range: 0.61–0.94) and EQ-5D-3L (n = 418, mean: 0.80; median: 0.82; range: 0.39–0.95), those measured by 15-D (n = 1, mean: 0.89; median: 0.91; SD: 0.09) had the highest value, and HUI-3(n = 17, mean: 0.70; median: 0.68; range: 0.59–0.86) had the lowest.
By complication, the highest HSUVs were T2DM with neuropathy (n = 15, mean: 0.77; median: 0.79; range: 0.62–0.85), while the lowest HSUVs were T2DM with cerebrovascular disease (n = 29, mean: 0.65; median: 0.67 range: 0.42–0.82). Of 732 HSUVs reported mean values with SD, the mean HSUVs of T2DM with complications, T2DM with cerebrovascular disease and T2DM with microvascular disease had a decrement of 0.01. In contrast, the mean HSUVs of T2DM with cardiovascular diseases had a decrement of 0.02.
Quality assessment
All studies fully or partially addressed the four questions from the quality appraisal tool, with seventy-five studies (63.6%) providing detailed reports on these aspects. Specifically, 81.3%, 83%, 90.6%, and 98.3% of the studies provided thorough reporting on the four quality assessment issues. The vast majority (83%) adequately described the measurement instruments used, and almost all (98.3%) provided detailed information on the characteristics of the study population. Based on this quality assessment, these 118 studies were classified as high-quality (Table 3).
Regression analysis
Table 4 reports the results of the meta-regression analyses. The model weighted by sample size had better fit goodness (R2 is 0.6238, which is greater than the unweighted 0.4316 and SD weighted 0.4537).
In sample size weighted specification, differences in the choice of instruments significantly affected the HSUVs; SF-6D (0.083, 95%CI: 0.064, 0.101) was estimated to have the highest positive coefficient, while FT (-0.139, 95%CI: -0.195, -0.084) had the lowest negative coefficient. Meanwhile, the variables for tariff had a statistically significant (p < 0.05) association with the mean HSUV. Based on EQ-5D-3L UK tariff, the EQ-5D-3L US tariff (0.015, 95%CI: -0.008, 0.038), EQ-5D-3L Chinese tariff (0.08, 95%CI: 0.052, 0.107) and EQ-5D-3L Japanese tariff (0.061, 95%CI: -0.003,0.125) had positive effect on the mean HSUV, while EQ-5D-5L UK tariff (-0.068, 95%CI: -0.166, 0.03) had negative effect. Among these, the state of T2DM with diabetic foot (-0.17, 95%CI: -0.192, -0.147) resulted in the largest negative coefficient, while the state of T2DM without complications (0.023, 95%CI: 0.001, 0.046) resulted in the biggest positive coefficient.
The regression results for the mean age showed that the increments of HSUVs (0.029, 95%CI: -0.055, 0.112 for ages 50–60; 0.025, 95%CI: -0.058, 0.108 for ages 60–70) aligned with age increasing for the cohort of age less than 70 years, but this result was not statistically significant. While the HSUVs decremented for the duration of illness exceeding ten years (-0.006, 95%CI: -0.002, 0.008), hypertension (-0.025, 95%CI: -0.108, 0.058), overweight (-0.088, 95%CI: -0.135, -0.041) and obesity (-0.071, 95%CI: -0.103, -0.039), although the result for duration and hypertension had no statistical significance (p > 0.05).
Discussion
This study provided a valuable set of utility values for patients with T2DM to support future economic evaluations and decision-making. We synthesised 118 studies to summarise the HSUVs for patients with T2DM and its 11 complications, and the effects of different measurement instruments on HSUVs. In addition, meta-regression quantified the disutility associated with disease-related complications in patients with T2DM and estimated modifiers of HSUVs by controlling for country, selected measurement instrument, age, disease duration, blood pressure and body mass index. Overall, these estimates improved the robustness of the evidence for future quality-of-life studies and health economic assessments of patients with T2DM.
The economic evaluation of diabetes-related interventions relies heavily on HSUVs as an outcome measure of the impact of different factors on patients’ quality of life [150, 151]. It has become a consensus among health providers that having complications leads to a reduction in the health utility value of patients with T2DM [49, 121], and it is therefore important to incorporate this reduction in HSUVs in economic evaluations to improve the robustness of QALY estimates. The influence of other key associates such as country, instrument, tariff and general patient characteristics such as blood pressure, duration of illness, on HSUVs has already been assessed in existing studies (MOK et al. [9], Jing et al. [10], and Redenz et al. [8]). Our study also included these factors as control variables to quantify the associations between these variables and HSUVs. In addition, possible influences such as age and BMI were also included as variables to strengthen the model goodness-of-fit. Our meta-regression results provided new insights for future studies of T2DM-related management decisions by healthcare analysts.
Greenland et al. [152] noted that relying solely on statistical significance is inadequate for drawing inferences or making decisions about associations or effects. Meanwhile, when it comes to utilizing health economic evidence to inform healthcare decision-making, decisions are based on the incremental expected costs and health benefits of care, irrespective of statistical significance [153]. Thus, although there were no statistically significant associations between certain variables and HSUVs, our analysis quantified the incremental or decremental utility values can still be used for healthcare decision-making. First, the association between HSUVs measuring instruments and quality of life remains controversial. Our study suggested that different instruments would bring about different degrees of incremental or decremental HSUVs, which was consistent with the findings of Redenz et al. [8] and supported by the study of Glasziou et al. [154]. Lung et al. [155] noted that the utility scores obtained from the TTO method were greater than those obtained from the EQ-5D, which were greater than those obtained from the HUI2, HUI3, and SF-6D. However, our study yielded different trends and variations in the magnitude of coefficient in values. Meanwhile, it has also been shown that the utility decrements were comparable between the instruments, EQ-5D and SF-6D [9]. The validity of future research on HSUVs may require additional attention to be cast on the incremental and decremental utility values derived from specific instruments. Second, tariff differences also affected the measurement of HSUVs, the US (EQ-5D-3L), and China (EQ-5D-3L) tariff brought increments to mean HSUVs compared to the UK (EQ-5D-3L). The effect of the tariffs on HSUVs was interpreted as differences due to different socio-demographic factors in the study by Sullivan et al. [129]. Despite the observed variation in tariff application across regions such as the European countries, the United Kingdom, and the United States—which share similar ethnic compositions—it is advisable to employ tariffs that are representative of their respective jurisdictions to ensure high relevance and accuracy.
T2DM patients with complications usually have lower HSUVs than T2DM patients (with or without complications). The idea that complications have a negative impact on the quality of life of T2DM patients has been confirmed in several studies [8,9,10, 156,157,158]. Compared with other published studies, the utility reduction due to complications ranged from − 0.007 to -0.177 in Mok et al. [9] and from − 0.007 to -0.17 in our study. The lowest utility value was for end-stage renal impairment in the study by Lung et al. [155] with a utility value of 0.48 (0.25–0.71); however, in our study, the complication with the lowest HSUVs was for diabetic foot (-0.17, 95%CI: -0.192, -0.147). This difference may be attributed to differences in the countries, tariffs, assessment instruments, and the essential characteristics of the population. Our study provided the correlation between 9 instruments and 31 tariffs, in contrast to previous studies of Shao et al. [121], which only included a single instrument and tariff and Mok et al. [9], which included a limited number of countries and regions. In addition, advances in therapeutic strategies, medical treatments, and the progression of complications may also account for this difference between the size of the negative coefficients.
In the model weighted by sample size, the decremental trend of HSUVs in disease duration, blood pressure, overweight and obesity on HSUVs was consistent with previous studies [10, 149, 158]. Meanwhile, the results of the positive correlation between age <70 and HSUVs were consistent with the findings of Imayama et al. [157], which may be explained by the increased satisfaction with the quality of life associated with increasing age. Although age ≥ 70 leads to negative coefficients, there are two reasons to explain this phenomenon: firstly, older age ≥ 70 typically corresponds with lower HSUVs due to weaker physical functioning, higher complication rate and acute mortality rate [4]; secondly, the number of utility values included in the regression was only 8, so the results are not highly credible. The controversial effect of age on the HSUVs needs to be verified by further research [33].
Utility estimates naturally vary depending on factors such as study design, utility measuring instruments, health status classification, demographic characteristics and tariffs valuation [119, 127, 129, 159]. Ideal data for decision-making must take these factors into account [160]. One of the strengths of our study is that we have expanded extensively on these factors to include more comprehensive variables, we cover a wide range of HSUVs triggered by direct or indirect measurement instruments, covered 31 tariffs and across 11 complication states, and, for the first time, synthesised them using meta-regression to provide a range of reference values. Decision makers can select the most appropriate HSUVs based on their specific variables to robustly support future economic evaluations.
One limitation of this review is the search process. We searched only three databases, PubMed, Embase, and Web of Science, while identifying published manuscripts from peer-reviewed scholarly journals but potentially ignoring grey literature, unpublished work, and other data sources. Bramer et al. reported a 92.8% search rate for Medline and Embase, highlighting the robustness of these databases in identifying relevant studies [161]. Therefore, any potential omissions are unlikely to have significantly affected the overall findings of our study. The measurement of T2DM health utility values in countries around the world is carried out using a variety of standardised and validated instruments, and the diversity of the value sets is determined by differences in demographic characteristics in different countries, which inevitably leads to the high number of variables we included in the meta-regressions, resulting in small sample sizes for some variables. This is the second limitation of our study, and this under-observation prevents us from modelling even the full diversity of methods used to generate utility values, which may affect the model’s reliability. Another area of uncertainty lies in the inability to determine the impact of gender distribution in the ill population on quality of life and utility values. In addition, studies often did not adequately account for the timescales involved, either from the stage of the condition or the start of treatment. Similarly, 18.7% and 17% of the studies did not adequately explain the methods used to derive the utility values. However, our analysis found that differences in measurement methodologies significantly impacted HSUVs. To maximize the inclusion of available data, we opted not to exclude these studies, provided they addressed at least some of the four quality assessment questions. As more studies of HSUVs for people with T2DM are published, these effects could be further explored to improve the validity of meta-regression model estimates and the quality of the evidence to inform healthcare decisions.
Conclusion
Our study quantified the extent to which 11 complications, adjusted for valuation instruments and tariffs, affected patients’ quality of life, reinforcing the HSUVs evidence base and informing future decision-making processes about patients with T2DM. Analysts can use the data sources provided in this review to identify specific HSUV estimates most appropriate to their decision-making. Estimated condition-specific incremental decrements in health utility would provide more robust evidence for researchers to improve the quality of economic assessments in diabetes.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- HSUV:
-
Health Utility Value
- QALY:
-
Quality og Life Reserach
- T2DM:
-
Type 2 Diabetes Mellitus
- ICC:
-
Intra-Class Correlation Coefficients
- EQ-5D-3L:
-
Three-level EuroQol Five-Dimension
- EQ-5D-5L:
-
Five-level EuroQol Five-Dimension
- SD:
-
Standard Deviatiom
- SE:
-
Standard Error
- IQR:
-
Interquartile Range
- 95% CI:
-
95% Confidence Interval
- SF-6D:
-
Short-Form 6-Dimension
- 15-D:
-
15-Dimension
- HUI-2:
-
The Tealth Utilities Index Mark 2
- HUI-3:
-
The Tealth Utilities Index Mark 3
- FT:
-
Feeling Thermometer
- SG:
-
Stabdard Gamble
- TTO:
-
Time Trade-Off
References
Xie F, Zoratti M, Chan K, Husereau D, Krahn M, Levine O, Clifford T, Schunemann H, Guyatt G. Toward a centralized, systematic Approach to the identification, Appraisal, and Use of Health State Utility values for reimbursement decision making: introducing the Health Utility Book (HUB). MED DECIS Mak. 2019;39(4):371–9.
Rowen D, Azzabi Zouraq I, Chevrou-Severac H, van Hout B. International Regulations and Recommendations for Utility Data for Health Technology Assessment. PharmacoEconomics. 2017;35(S1):11–9.
Ara R, Brazier J, Zouraq IA. The Use of Health State Utility values in decision models. PharmacoEconomics. 2017;35(S1):77–88.
Magliano DJ, Boyko EJDA. IDF DIABETES ATLAS. Brussels: International Diabetes Federation; 2021.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan J, Mbanya JC, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. DIABETES RES CLIN PR. 2022;183:109–19.
Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of diabetes 2017. J DIABETES RES. 2018;2018:1–4.
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus. 2021;4(13):315–409.
Redenz G, Ibaceta MC, Aceituno D, Balmaceda C, Espinoza MA. Health State Utility values of type 2 diabetes Mellitus and related complications: a systematic review and Meta-analysis. VALUE HEALTH REG ISS. 2023;34:14–22.
Mok CH, Kwok HHY, Ng CS, Leung GM, Quan J. Health State Utility values for type 2 diabetes and related complications in East and Southeast Asia: a systematic review and Meta-analysis. VALUE HEALTH. 2021;24(7):1059–67.
Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, Gao F, Li C, Cui Z, Liu Y, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Volume 16. HEALTH QUAL LIFE OUT; 2018. 1.
Wang Y, Gavan SP, Steinke D, et al. The impact of age on health utility values for older women with early-stage breast cancer: a systematic review and meta-regression. Health Qual Life Outcomes. 2022;20:169.
Ara R, Brazier J, Peasgood T, Paisley S. The identification, review and synthesis of Health State Utility values from the literature. PharmacoEconomics. 2017;35(S1):43–55.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ-BRIT MED J. 2021;372:n71.
Koo TK, Li MY. A Guideline of selecting and reporting Intraclass correlation coefficients for Reliability Research. J CHIROPR MED. 2016;15(2):155–63.
Portney LG. in Foundations of Clinical Research: Applications to Evidence-Based Practice. 4th ed. New York: F. A. Davis Company; 2020.
Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, Matthews DR, Stratton IM, Holman RR. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom prospective diabetes study (UKPDS) outcomes Model (UKPDS 68). Diabetologia. 2004;47(10):1747–59.
Dadwani RS, Laiteerapong N. Economic Simulation Modeling in Type 2 Diabetes. Curr Diab Rep. 2020;20(7):24.
Yi Y, Philips Z, Bergman G, Burslem K. Economic models in type 2 diabetes. CURR MED RES OPIN. 2010;26(9):2105–18.
Muchadeyi MT, Hernandez-Villafuerte K, Schlander M. Quality appraisal for systematic literature reviews of health state utility values: a descriptive analysis. BMC MED RES METHODOL. 2022;22(1):303.
Papaioannou D, Brazier J, Paisley S. Systematic Searching and Selection of Health State Utility Values from the literature. VALUE HEALTH. 2013;16(4):686–95.
Papaioannou D, Brazier J, Paisley S, NICE DSU Technical Support Document 9. The identification, review and synthesis of Health State Utility values from the literature. London: National Institute for Health and Care Excellence (NICE); 2010.
Nerich V, Saing S, Gamper E, Holzner B, Pivot X, Viney R, Kemmler G. Critical appraisal of health-state utility values used in breast cancer-related cost–utility analyses. BREAST CANCER RES TR. 2017;164(3):527–36.
Zoratti MJ, Pickard AS, Stalmeier PFM, Ollendorf D, Lloyd A, Chan KKW, Husereau D, Brazier JE, Krahn M, Levine M, et al. Evaluating the conduct and application of health utility studies: a review of critical appraisal tools and reporting checklists. Eur J Health Econ. 2021;22(5):723–33.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions (Version 6.4). Cochrane. 2023.
Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, Zou D, Guo L, Ji Q, Chen L, Chen L, Dou J, Guo X, Kuang H, Li L, Li Q, Li X, Liu J, Ran X, Shi L, Song G, Xiao X, Yang L, Zhao Z, Chinese Diabetes Society. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev. 2019;35(6):e3158.
Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88(11):1254–64.
Adults Older. Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S139–47.
Abadie A, Athey S, Imbens GW, Wooldridge JM. When should you adjust standard errors for clustering? Q J Econ. 2023;138(1):1–35.
Draper NR, Smith H. Applied Regression Analysis. Volume 326. Wiley; 1998.
StataCorp. Stata Statistical Software: Release 18. In., College Station, TX: StataCorp LLC edn; 2023.
Adibe MO, Ukwe CV, Aguwa CN. The impact of pharmaceutical care intervention on the quality of life of Nigerian patients receiving treatment for type 2 diabetes. VALUE HEALTH REG ISS. 2013;2(2):240–7.
Al-Azayzih A, Kanaan RJ, Altawalbeh SM. Assessment of Drug-related problems and Health-Related Quality of Life Domains in Elderly patients with type 2 diabetes Mellitus. THER CLIN RISK MANAG. 2023;19:913–28.
Alshayban D, Joseph R. Health-related quality of life among patients with type 2 diabetes mellitus in Eastern Province, Saudi Arabia: a cross-sectional study. PLoS ONE. 2020;15(1):e227573.
Ananthesh L, Cutinha RM, Sahoo SS, Dsouza JD, Shetty S, Gururaj C, Kellarai A. Effect of healthcare expenditure on the health related quality of life among diabetic patients of South India: a cross- sectional study. CLIN EPIDEMIOL GLOB; 2024. p. 25.
Anirudh M, Karthikeyan K. Pharmacoeconomic Evaluation of Antidiabetic Therapy at a Tertiary Health Care Institution. Asian J Pharm Clin Res. 2021;14(6):115–20.
Arifin B, Idrus LR, van Asselt ADI, Purba FD, Perwitasari DA, Thobari JA, Cao Q, Krabbe PFM, Postma MJ. Health-related quality of life in Indonesian type 2 diabetes mellitus outpatients measured with the Bahasa version of EQ-5D. Qual Life Res. 2019;28(5):1179–90.
Boye KS, Yurgin N, Dilla T, Cordero LA, Badia X, Suriñach NL, Pérez P. Health-related quality of life of patients with type 2 diabetes mellitus in primary care in Spain: self-reported and proxy assessment using the EQ-5D. J MED ECON. 2007;10(1):41–58.
Boye KS, Matza LS, Walter KN, Van Brunt K, Palsgrove AC, Tynan A. Utilities and disutilities for attributes of injectable treatments for type 2 diabetes. EUR J HEALTH ECON. 2011;12(3):219–30.
Boye KS, Sapin H, García-Pérez LE, Rosilio M, Orsini Federici M, Heitmann E, Jung H, Aigner U, Guerci B, Giorgino F, et al. The Real-World Observational Prospective Study of Health Outcomes with Dulaglutide and Liraglutide in type 2 diabetes patients (TROPHIES): baseline patient-reported outcomes. DIABETES THER. 2020;11(10):2383–99.
Boye KS, Thieu VT, Sapin H, Lee CJ, Landó LF, Brown K, Bray R, Wiese RJ, Patel H, Rodríguez Á, et al. Patient-reported outcomes in people with type 2 diabetes receiving Tirzepatide in the SURPASS Clinical Trial Programme. DIABETES THER; 2023.
Briggs AH, Bhatt DL, Scirica BM, Raz I, Johnston KM, Szabo SM, Bergenheim K, Mukherjee J, Hirshberg B, Mosenzon O. Health-related quality-of-life implications of cardiovascular events in individuals with type 2 diabetes mellitus: a subanalysis from the Saxagliptin Assessment of Vascular outcomes recorded in patients with diabetes Mellitus (SAVOR)-TIMI 53 trial. DIABETES RES CLIN PR. 2017;130:24–33.
Browna GCBM, Marvin G, Paul Dentonb D. Quality of life associated with diabetes mellitus in an adult population. 2000.
Burström K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res. 2001;10(7):621–35.
Butt M, Ali AM, Bakry MM. Health-related quality of life in poorly controlled type 2 diabetes patients- association of patients’ characteristics with EQ-5D domains, mean EQ-5D scores, and visaul analog scale score. Asian J Pharm Clin Res. 2018;11(1):93–8.
Chang K. Comorbidities, quality of life and patients’ willingness to pay for a cure for type 2 diabetes in Taiwan. Public Health. 2010;124(5):284–94.
Chen CC, Chen JH, Chen CL, Lai TJ, Ko Y. Health Utilities in patients with type 2 diabetes in Taiwan. HEALTHCARE-BASEL 2021, 9(12).
Chen S, Burstrom B, Sparring V, Qian D, Burstrom K. Differential Impact of an education-based intervention for patients with type 2 diabetes Mellitus in Rural China. INT J ENV RES PUB HE. 2019;16(15):2676.
Choi YJ, Lee MS, An SY, Kim TH, Han SJ, Kim HJ, Chung YS, Lee KW, Kim DJ. The relationship between diabetes Mellitus and Health-related quality of life in Korean adults: the Fourth Korea National Health and Nutrition Examination Survey (2007–2009). DIABETES METAB J. 2011;35(6):587–94.
Clarke P, Gray A, Holman R. Estimating Utility Values for Health States of type 2 Diabetic patients using the EQ-5D (UKPDS 62). MED DECIS Mak. 2002;22(4):340–9.
Clarke PM, Hayes AJ, Glasziou PG, Scott R, Simes J, Keech AC. Using the EQ-5D index score as a predictor of outcomes in patients with type 2 diabetes. MED CARE. 2009;47(1):61–8.
Currie CJ, McEwan P, Peters JR, Patel TC, Dixon S. The routine collation of health outcomes data from hospital treated subjects in the Health Outcomes Data Repository (HODaR): descriptive analysis from the first 20,000 subjects. VALUE HEALTH. 2005;8(5):581–90.
Currie CJ, Poole CD, Woehl A, Morgan CL, Cawley S, Rousculp MD, Covington MT, Peters JR. The health-related utility and health-related quality of life of hospital-treated subjects with type 1 or type 2 diabetes with particular reference to differing severity of peripheral neuropathy. Diabetologia. 2006;49(10):2272–80.
Currie CJ, Poole CD, Woehl A, Morgan CL, Cawley S, Rousculp MD, Covington MT, Peters JR. The financial costs of healthcare treatment for people with type 1 or type 2 diabetes in the UK with particular reference to differing severity of peripheral neuropathy. Diabet MED. 2007;24(2):187–94.
Cvetanovic G, Stojiljkovic M, Miljkovic M. Estimation of the influence of hypoglycemia and body mass index on health-related quality of life, in patients with type 2 diabetes mellitus. VOJNOSANIT PREGL. 2017;74(9):831–9.
Dominguez-Munoz FJ, Adsuar JC, Carlos-Vivas J, Villafaina S, Garcia-Gordillo MA, Hernandez-Mocholi MA, Collado-Mateo D, Gusi N. Association between TUG and Anthropometric Values, vibration perception threshold, FHSQ and 15-D in type 2 diabetes Mellitus patients. Volume 17. INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH; 2020. 6.
Dudzińska M, Tarach JS, Zwolak A, Kurowska M, Malicka J, Smoleń A, Nowakowski A. Type 2 diabetes mellitus in relation to place of residence: evaluation of selected aspects of socio-demographic status, course of diabetes and quality of life–a cross-sectional study. ANN AGR ENV MED. 2013;20(4):869–74.
Dudzinska M, Tarach JS, Zwolak A, Malicka J, Kowalczyk M, Wirska J, Daniluk J. Quality of life among patients with type 2 diabetes after insulin therapy introduction: a prospective study. Diabetologia Kliniczna. 2015;4(6):226–31.
Ekwunife OI, Ezenduka CC, Uzoma BE. Evaluating the sensitivity of EQ-5D in a sample of patients with type 2 diabetes mellitus in two tertiary health care facilities in Nigeria. BMC RES NOTES. 2016;9(1):24.
Elissen AMJ, Hertroijs DFL, Schaper NC, Bosma H, Dagnelie PC, Van Der Henry RM, Koster A, Schram MT, Stehouwer CDA et al. Differences in biopsychosocial profiles of diabetes patients by level of glycaemic control and health-related quality of life: the Maastricht Study. PLoS ONE 2017, 12(7).
Glasziou P, Alexander J, Beller E, Clarke P, Grp AC. Which health-related quality of life score ? A comparison of alternative utility measures in patients with type 2 diabetes in the ADVANCE trial. Volume 5. HEALTH QUAL LIFE OUT; 2007.
Gorter K, van Bruggen R, Stolk R, Zuithoff P, Verhoeven R, Rutten G. Overall quality of diabetes care in a defined geographic region: different sides of the same story. BRIT J GEN PRACT. 2008;58(550):339–45.
Grandy S, Fox KM. EQ-5D visual analog scale and utility index values in individuals with diabetes and at risk for diabetes: findings from the study to help improve early evaluation and management of risk factors leading to Diabetes (SHIELD). HEALTH QUAL LIFE OUT; 2008. p. 6.
Grandy S, Fox KM, Group SS. Change in health status (EQ-5D) over 5 years among individuals with and without type 2 diabetes mellitus in the SHIELD longitudinal study. HEALTH QUAL LIFE OUT. 2012;10(1):99.
Grandy S, Langkilde AM, Sugg JE, Parikh S, Sjostrom CD. Health-related quality of life (EQ-5D) among type 2 diabetes mellitus patients treated with dapagliflozin over 2 years. INT J CLIN PRACT. 2014;68(4):486–94.
Gu SY, Wang XY, Shi LZ, Sun QY, Hu XQ, Gu YX, Sun XS, Dong HJ. Health-related quality of life of type 2 diabetes patients hospitalized for a diabetes-related complication. QUAL LIFE RES. 2020;29(10):2695–704.
Hao S, Heintz E, Helgesson G, Langenskiold S, Chen J, Burstrom K. Influence of elicitation procedure and phrasing on health state valuations in experience-based time trade-off tasks among diabetes patients in China. Qual Life Res. 2020;29(1):289–301.
Harris S, Mamdani M, Galbo-Jorgensen CB, Bogelund M, Gundgaard J, Groleau D. The effect of hypoglycemia on health-related quality of life: Canadian results from a multinational time trade-off survey. CAN J DIABETES. 2014;38(1):45–52.
Hayes A, Arima H, Woodward M, Chalmers J, Poulter N, Hamet P, Clarke P. Changes in quality of Life Associated with complications of Diabetes: results from the ADVANCE study. VALUE HEALTH. 2016;19(1):36–41.
Hoda F, et al. Impact of a mHealth Intervention in Type 2 Diabetes Mellitus Patients: A Randomized Clinical Trial. SN Compr Clin Med. 2023;5(1):219.
Ishii H, Nakajima H, Kamei N, Niiya T, Hiyoshi T, Hiramori Y, Ohtsu S, Noto T, Shimono D. Quality-of-life comparison of Dapagliflozin Versus Dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes Mellitus: a randomized controlled trial (J-BOND study). DIABETES THER. 2020;11(12):2959–77.
Jalkanen K, Aarnio E, Lavikainen P, Jauhonen HM, Enlund H, Martikainen J. Impact of type 2 diabetes treated with non-insulin medication and number of diabetes-coexisting diseases on EQ-5D-5 L index scores in the Finnish population. HEALTH QUAL LIFE OUT. 2019;17(1):117.
Javanbakht M, Abolhasani F, Mashayekhi A, Baradaran HR, Jahangiri Noudeh Y. Health Related Quality of Life in patients with type 2 diabetes Mellitus in Iran: A National Survey. PLoS ONE 2012, 7(8).
Jhita T, Petrou S, Gumber A, Szczepura A, Raymond NT, Bellary S. Ethnic differences in health related quality of life for patients with type 2 diabetes. HEALTH QUAL LIFE OUT. 2014;12(1):83.
Kamradt M, Krisam J, Kiel M, Qreini M, Besier W, Szecsenyi J, Ose D. Health-Related Quality of Life in Primary Care: which aspects Matter in Multimorbid patients with type 2 diabetes Mellitus in a community setting? PLoS ONE. 2017;12(1):e170883.
Kiadaliri AA, Gerdtham UG, Eliasson B, Gudbjornsdottir S, Svensson AM, Carlsson KS. Health Utilities of Type 2 Diabetes-Related Complications: A Cross-Sectional Study in Sweden. Int J Environ Res Public Health. 2014;11(5):4939–52.
Kiadaliri AA, Eliasson B, Gerdtham UG. Does the choice of EQ-5D tariff matter? A comparison of the Swedish EQ-5D-3L index score with UK, US, Germany and Denmark among type 2 diabetes patients. HEALTH QUAL LIFE OUT. 2015;13(1):145.
Koekkoek PS, Biessels GJ, Kooistra M, Janssen J, Kappelle LJ, Rutten GE, Cog IDSG. Undiagnosed cognitive impairment, health status and depressive symptoms in patients with type 2 diabetes. J DIABETES COMPLICAT. 2015;29(8):1217–22.
Konerding U, Bowen T, Elkhuizen SG, Faubel R, Forte P, Karampli E, Mahdavi M, Malmström T, Pavi E, Torkki P. The impact of travel distance, travel time and waiting time on health-related quality of life of diabetes patients: an investigation in six European countries. DIABETES RES CLIN PR. 2017;126:16–24.
Kuo S, Yang CT, Chen HY, Ou HT. Valuing health states of people with type 2 diabetes: analyses of the nationwide representative linked databases. J DIABETES INVEST. 2021;12(9):1749–58.
Landy J, Stein J, Brown MM, Brown GC, Sharma S. Patient, community and clinician perceptions of the quality of life associated with diabetes mellitus. MED SCI Monit. 2002;8(8):R543–8.
Lane S, Levy AR, Mukherjee J, Sambrook J, Tildesley H. The impact on utilities of differences in body weight among Canadian patients with type 2 diabetes. Curr Med Res Opin. 2014;30(7):1267–73.
Laxy M, Becker J, Kahm K, Holle R, Peters A, Thorand B, Schwettmann L, Karl FM. Utility Decrements Associated with Diabetes and related complications: estimates from a Population-based study in Germany. VALUE HEALTH. 2021;24(2):274–80.
Lee AJ, Morgan CL, Morrissey M, Wittrup-Jensen KU, Kennedy-Martin T, Currie CJ. Evaluation of the association between the EQ-5D(index) (health-related utility) and body mass index (obesity) in hospital-treated people with type 1 diabetes, type 2 diabetes and with no diagnosed diabetes. Diabet MED. 2005;22(11):1482–6.
Lee WJ, Song KH, Noh JH, Choi YJ, Jo MW. Health-related quality of life using the EuroQol 5D questionnaire in Korean patients with type 2 diabetes. J KOREAN MED SCI. 2012;27(3):255–60.
Lim LL, Pheng Chan ESHL, Ji S, Lim L, Sirinvaravong S, Unnikrishnan S, Cortese AGAOYL, Durocher V. A et al: Real-world evidence on health-related quality of life in patients with type 2 diabetes mellitus using sulphonylureas: an analysis of the Joint Asia Diabetes evaluation (JADE) Register. Volume 203. DIABETES RES CLIN PR; 2023. p. 110855.
Lui JNM, Lau ESH, Yang A, Wu H, Fu A, Lau V, Loo K, Yeung T, Yue R, Ma RCW et al. Temporal associations of diabetes-related complications with health-related quality of life decrements in Chinese patients with type 2 diabetes: a prospective study among 19 322 adults—joint Asia diabetes evaluation (JADE) register (2007–2018). J DIABETES 2023.
Maddigan SL, Majumdar SR, Guirguis LM, Lewanczuk RZ, Lee TK, Toth EL, Johnson JA. Improvements in patient-reported outcomes associated with an intervention to enhance quality of care for rural patients with type 2 diabetes: results of a controlled trial. Diabetes Care. 2004;27(6):1306–12.
Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA. Health Utilities Index mark 3 demonstrated construct validity in a population-based sample with type 2 diabetes. J CLIN EPIDEMIOL. 2006;59(5):472–7.
Malanda UL, Bot SD, French DP, Kostense PJ, Wade AN, Dekker JM, Nijpels G, Farmer AJ. Experience of hypoglycaemia is associated with changes in beliefs about diabetes in patients with type 2 diabetes. Diabet MED. 2011;28(11):1395–400.
Marrett E, Stargardt T, Mavros P, Alexander CM. Patient-reported outcomes in a survey of patients treated with oral antihyperglycaemic medications: associations with hypoglycaemia and weight gain. Diabetes Obes Metab. 2009;11(12):1138–44.
Matza LS, Stewart KD, Redig J, Howell TA, Morris W, Newson RS, Yasui A, Ishak J, Boye KS. Health state utilities associated with weight loss: preferences of people with type 2 diabetes and obesity in Japan. J MED ECON 2024:1–38.
Matza LS, Boye KS, Yurgin N. Validation of two generic patient-reported outcome measures in patients with type 2 diabetes. HEALTH QUAL LIFE OUT. 2007;5(1):47.
Matza LS, Stewart KD, Davies EW, Paczkowski R, Boye KS. Health State Utilities Associated with Attributes of Weekly Injection Devices for Treatment of Type 2 diabetes. VALUE HEALTH. 2017;18(7):A363.
Matza LS, Boye KS, Yurgin N, Brewster-Jordan J, Mannix S, Shorr JM, Barber BL. Utilities and disutilities for type 2 diabetes treatment-related attributes. QUAL LIFE RES. 2007;16(7):1251–65.
Mehta Z, Cull C, Stratton I, Yudkin J, Jenkinson C, Fletcher A, Battersby C, Holman R, Turner R. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). Diabetes Care. 1999;22(7):1125–36.
Mihevc M, Virtič Potočnik T, Zavrnik C, Šter MP, Klemenc-Ketiš Z, Poplas Susič A. Beyond diagnosis: investigating factors influencing health-related quality of life in older people with type 2 diabetes in Slovenia. PRIM CARE DIABETES; 2024.
Modarresnia L, Golgiri F, Madani NH, Emami Z, Tanha K. Restless legs syndrome in Iranian people with type 2 diabetes Mellitus: the Role in Quality of Life and Quality of Sleep. J CLIN SLEEP MED. 2018;14(2):223–8.
Naïditch N, Hehn C, Ounajim A, Fagherazzi G, Gasch-Illescas A, Braithwaite B, Thébaut JF. PRODIAB: perspectives on the use of patient-reported outcome measures among diabetic patients. Diabetes Epidemiol Manage 2023;9.
Nauck MA, Buse JB, Mann JFE, Pocock S, Bosch-Traberg H, Frimer-Larsen H, Ye Q, Gray A, Investigators LPCF. Health-related quality of life in people with type 2 diabetes participating in the LEADER trial. DIABETES OBES METAB. 2019;21(3):525–32.
Nazir SR, Hassali MA, Saleem F, Bashir S, Aljadhey H. Does adherence to the therapeutic regimen associate with health related quality of life: findings from an observational study of type 2 diabetes mellitus patients in Pakistan. PAK J PHARM SCI. 2017;30(6):2159–65.
Neumann A, Schoffer O, Norstrom F, Norberg M, Klug SJ, Lindholm L. Health-related quality of life for pre-diabetic states and type 2 diabetes mellitus: a cross-sectional study in Vasterbotten Sweden. HEALTH QUAL LIFE OUT; 2014. p. 12.
Neuwahl SJ, Zhang P, Chen HY, Shao H, Laxy M, Anderson AM, Craven TE, Hoerger TJ, Look ARG. Patient Health Utility Equations for a type 2 diabetes model. Diabetes Care. 2021;44(2):381–9.
O’Shea MP, Teeling M, Bennett K. Comorbidity, health-related quality of life and self-care in type 2 diabetes: a cross-sectional study in an outpatient population. Ir J MED SCI. 2015;184(3):623–30.
Pagkalos E, Thanopoulou A, Sampanis C, Bousboulas S, Melidonis A, Tentolouris N, Alexandrides T, Migdalis I, Karamousouli E, Papanas N. The real-life effectiveness and care patterns of type 2 diabetes management in Greece. EXP CLIN ENDOCR DIAB. 2018;126(1):53–60.
Pan CW, Sun HP, Wang X, Ma Q, Xu Y, Luo N, Wang P. The EQ-5D-5L index score is more discriminative than the EQ-5D-3L index score in diabetes patients. QUAL LIFE RES. 2014;24(7):1767–74.
Pettersson B, Rosenqvist U, Deleskog A, Journath G, Wandell P. Self-reported experience of hypoglycemia among adults with type 2 diabetes mellitus (exhype). DIABETES RES CLIN PR. 2010;92(1):19–25.
Pham TB, Nguyen TT, Truong HT, Trinh CH, Du HNT, Ngo TT, Nguyen LH. Effects of Diabetic Complications on Health-Related Quality of Life Impairment in Vietnamese Patients with Type 2 Diabetes. J DIABETES RES. 2020;2020.
Pinchevsky Y, Raal F, Butkow N, Chirwa T, Distiller L, Rothberg A. Quality of care delivered to type 2 diabetes mellitus patients in public and private sector facilities in Johannesburg, South Africa. INT J GEN MED. 2018;11:383–90.
Pratipanawatr T, Satirapoj B, Ongphiphadhanakul B, Suwanwalaikorn S, Nitiyanant W. Impact of Hypoglycemia on Health-Related Quality of Life among Type 2 Diabetes: A Cross-Sectional Study in Thailand. J Diabetes Res. 2019;2019:5903820.
Quah JHM, Luo N, Ng WY, How CH, Tay EG. Health-related quality of life is Associated with Diabetic complications, but not with short-term Diabetic Control in Primary Care. Volume 40. Singapore: Annals of the Academy of Medicine; 2011. pp. 276–86. 6.
Raisch DW, Feeney P, Goff DC, Narayan KMV, O’Connor PJ, Zhang P, Hire DG, Sullivan MD. Baseline comparison of three health utility measures and the feeling thermometer among participants in the action to control cardiovascular risk in diabetes trial. Cardiovasc Diabetol. 2012;11:35.
Randeree H, Liebl A, Hajjaji I, Khamseh M, Zajdenverg L, Chen JW, Haddad J. Safety and effectiveness of bolus insulin aspart in people with type 2 diabetes: A1chieve sub-analysis. DIABETES THER. 2013;4(1):153–66.
Reaney M, Mathieu C, Ostenson CG, Matthaei S, Krarup T, Kiljanski J, Salaun-Martin C, Sapin H, Theodorakis M, Guerci B. Patient-reported outcomes among patients using exenatide twice daily or insulin in clinical practice in six European countries: the CHOICE prospective observational study. HEALTH QUAL LIFE OUT. 2013;11(1):217.
Redekop WK, Koopmanschap MA, Stolk RP, Rutten GEHM, Wolffenbuttel BHR, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25(3):458–63.
Riandini T, Wee HL, Khoo EYH, Tai BC, Wang W, Koh GCH, Tai ES, Tavintharan S, Chandran K, Hwang SW, et al. Functional status mediates the association between peripheral neuropathy and health-related quality of life in individuals with diabetes. ACTA DIABETOL. 2018;55(2):155–64.
Ridderstråle M, Evans LM, Jensen HH, Bøgelund M, Jensen MM, Ericsson, Jendle J. Estimating the impact of changes in HbA1c, body weight and insulin injection regimen on health related quality-of-life: a time trade off study. HEALTH QUAL LIFE OUT 2016;14(1).
Rowen D, Carlton J, Elliott J. PROM validation using paper-based or online surveys: Data Collection methods affect the Sociodemographic and Health Profile of the Sample. VALUE HEALTH. 2019;22(8):845–50.
Sakamaki H, Ikeda S, Ikegami N, Uchigata Y, Iwamoto Y, Origasa H, Otani T, Otani Y. Measurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Health. 2006;9(1):47–53.
Sakthong P, Charoenvisuthiwongs R, Shabunthom R. A comparison of EQ-5D index scores using the UK, US, and Japan preference weights in a Thai sample with type 2 diabetes. HEALTH QUAL LIFE OUT. 2008;6:71.
Salampessy BH, Veldwijk J, van den Jantine Schuit A, Neslo RE, De Ardine G, Lambooij MS. The Predictive Value of Discrete Choice Experiments in Public Health: An Exploratory Application. Patient. 2015;8(6):521–9.
Shao H, Yang S, Fonseca V, Stoecker C, Shi L. Estimating quality of Life Decrements due to diabetes complications in the United States: the Health Utility Index (HUI) Diabetes Complication equation. PharmacoEconomics. 2019;37(7):921–9.
Sheu WHH, Ji L, Nitiyanant W, Baik SH, Yin D, Mavros P, Chan S. Hypoglycemia is associated with increased worry and lower quality of life among patients with type 2 diabetes treated with oral antihyperglycemic agents in the Asia-Pacific region. DIABETES RES CLIN PR. 2012;96(2):141–8.
Shi L, Shao H, Zhao Y, Thomas NA. Is hypoglycemia fear independently associated with health-related quality of life? HEALTH QUAL LIFE OUT. 2014;12(1):167.
Shim YT, Lee J, Toh MP, Tang WE, Ko Y. Health-related quality of life and glycaemic control in patients with type 2 diabetes mellitus in Singapore. Diabet MED. 2012;29(8):e241–8.
Sit RW, Wang B, Ng WS, Abullah A, Isamail IZ, Goh LH, Wong SY. Prevalence and association of chronic musculoskeletal pain on self-management, glycemic control and quality of life among Chinese type 2 diabetes patients in primary care. PRIM CARE DIABETES. 2022;16(4):525–30.
Smits KPJ, Sidorenkov G, Kleefstra N, Hendriks SH, Bouma M, Meulepas M, Navis G, Bilo HJG, Denig P. Is guideline-adherent prescribing associated with quality of life in patients with type 2 diabetes? PLoS ONE. 2018;13(8):e202319.
Solli O, Stavem K, Kristiansen IS. Health-related quality of life in diabetes: The associations of complications with EQ-5D scores. Health Qual Life Outcomes. 2010;8:18.
Stevens GD, Shi L, Vane C, Nie X, Peters AL. Primary care medical home experience and health-related quality of life among adult medicaid patients with type 2 diabetes. J GEN INTERN MED. 2015;30(2):161–8.
Sullivan PW, Ghushchyan VH. EQ-5D scores for diabetes-related comorbidities. VALUE HEALTH. 2016;19(8):1002–8.
Sundaram M, Kavookjian J, Patrick JH. Health-related quality of life and quality of life in type 2 diabetes: relationships in a cross-sectional study. PATIENT. 2009;2(2):121–33.
Tan MHP, Ong SC, Vasan Thakumar A, Mustafa N. Quantifying health-related quality of life in Malaysian type 2 diabetes: focusing on complication types and severity. Qual Life Res. 2023;32(7):1925–41.
Tang Z, Jiang X, Hong L, Feng Z, He Q, Yuan J, Xiang X. Validation of the simplified Chinese version of the brief diabetes quality of life (dqol) questionnaire based on a cross-sectional study. Int J Environ Res Public Health. 2020;17(23):1–10.
Thiel DM, Al Sayah F, Vallance JK, Johnson ST, Johnson JA. Association between Physical Activity and Health-Related Quality of Life in adults with type 2 diabetes. CAN J DIABETES. 2017;41(1):58–63.
Torre C, Guerreiro J, Longo P, Raposo JF, Leufkens H, Martins AP. Health-related quality of life in adults with type 2 diabetes mellitus starting with new glucose lowering drugs: an inception cohort study. PRIM CARE DIABETES. 2019;13(3):221–32.
Tung TH, Chen SJ, Lee FL, Liu JH, Lin CH, Chou P. A community-based study for the utility values associated with diabetic retinopathy among type 2 diabetics in Kinmen, Taiwan. DIABETES RES CLIN PR. 2005;68(3):265–73.
Veldwijk J, Lambooij MS, de Bekker-Grob EW, Smit HA, de Wit GA. The effect of including an opt-out option in discrete choice experiments. PLoS One. 2014;9(11):e111805.
Vexiau P, Mavros P, Krishnarajah G, Lyu R, Yin D. Hypoglycaemia in patients with type 2 diabetes treated with a combination of metformin and sulphonylurea therapy in France. Diabetes Obes Metabolism. 2008;10(s1):16–24.
Wan EY, Fung CS, Choi EP, Wong CK, Chan AK, Chan KH, Lam CL. Main predictors in health-related quality of life in Chinese patients with type 2 diabetes mellitus. QUAL LIFE RES. 2016;25(11):2957–65.
Wang P, Luo N, Tai ES, Thumboo J. The EQ-5D-5L is more discriminative than the EQ-5D-3L in patients with diabetes in Singapore. VALUE HEALTH REG ISS. 2016;9:57–62.
Wang Y, Tan NC, Tay EG, Thumboo J, Luo N. Cross-cultural measurement equivalence of the 5-level EQ-5D (EQ-5D-5L) in patients with type 2 diabetes mellitus in Singapore. HEALTH QUAL LIFE OUT. 2015;13(1):103.
Wasem J, Bramlage P, Gitt AK, Binz C, Krekler M, Deeg E, Tschöpe D. Co-morbidity but not dysglycaemia reduces quality of life in patients with type-2 diabetes treated with oral mono- or dual combination therapy - an analysis of the DiaRegis registry. CARDIOVASC DIABETOL 2013, 12(1).
Wexler DJ, Grant RW, Wittenberg E, Bosch JL, Cagliero E, Delahanty L, Blais MA, Meigs JB. Correlates of health-related quality of life in type 2 diabetes. Diabetologia. 2006;49(7):1489–97.
Yang W, Zhuang X, Li Y, Wang Q, Bian R, Shen J, Hammerby E, Yang L. Improvements in quality of life associated with biphasic insulin aspart 30 in type 2 diabetes patients in China: results from the A1chieve(R) observational study. HEALTH QUAL LIFE OUT. 2014;12(1):137.
Yu M, Brunt KV, Milicevic Z, Varnado O, Boye KS. Patient-reported outcomes in patients with type 2 diabetes treated with Dulaglutide added to titrated insulin glargine (AWARD-9). CLIN THER. 2017;39(11):2284–95.
Zare F, Ameri H, Madadizadeh F, Reza Aghaei M. Health-related quality of life and its associated factors in patients with type 2 diabetes mellitus. SAGE OPEN MED; 2020. p. 8.
Zhang P, Brown MB, Bilik D, Ackermann RT, Li R, Herman WH. Health Utility scores for people with type 2 diabetes in U.S. Managed Care Health plans results from translating Research Into Action for Diabetes (TRIAD). Diabetes Care. 2012;35(11):2250–6.
Zhang P, Hire D, Espeland MA, Knowler WC, Thomas S, Tsai AG, Glick HA. Impact of intensive lifestyle intervention on preference-based quality of life in type 2 diabetes: results from the look AHEAD trial. OBESITY. 2016;24(4):856–64.
Zhang YC, Wu J, Chen YY, Shi LZ. EQ-5D-3L decrements by diabetes complications and comorbidities in China. DIABETES THER. 2020;11(4):939–50.
Al Hayek AA, Robert AA, Al Saeed A, Alzaid AA, Al Sabaan FS. Factors Associated with Health-related quality of life among Saudi patients with type 2 diabetes Mellitus: a cross-sectional survey. DIABETES METAB J. 2014;38(3):220.
DeWalt DA, Rothrock N, Yount S, Stone AA. Evaluation of item candidates: the PROMIS qualitative item review. MED CARE. 2007;45(5 Suppl 1):S12–21.
Ara R, Brazier J. Estimating Health State Utility Values for Comorbidities. Pharmacoeconomics. 2017;35(Suppl 1):89–94.
Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, Altman DG. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. EUR J EPIDEMIOL. 2016;31(4):337–50.
Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J HEALTH ECON. 1999;18(3):341–64.
Glasziou P, Alexander J, Beller E, Clarke P, ADVANCE Collaborative Group. Which health-related quality of life score? A comparison of alternative utility measures in patients with Type 2 diabetes in the ADVANCE trial. Health Qual Life Outcomes. 2007;5:21.
Lung TW, Hayes AJ, Hayen A, Farmer A, Clarke PM. A meta-analysis of health state valuations for people with diabetes: explaining the variation across methods and implications for economic evaluation. QUAL LIFE RES. 2011;20(10):1669–78.
Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, Engelgau MM, Kaplan RM, Herman WH. Valuing health-related quality of life in diabetes. Diabetes Care. 2002;25(12):2238–43.
Imayama I, Plotnikoff RC, Courneya KS, Johnson JA. Determinants of quality of life in adults with type 1 and type 2 diabetes. HEALTH QUAL LIFE OUT. 2011;9(1):115.
Beaudet A, Clegg J, Thuresson P, Lloyd A, McEwan P. Review of Utility Values for Economic Modeling in type 2 diabetes. VALUE HEALTH. 2014;17(4):462–70.
Karlsson JA, Nilsson, Nilsson J, Neovius M, Kristensen LE, Gülfe A, Saxne T, Geborek P. National EQ-5D tariffs and quality-adjusted life-year estimation: comparison of UK, US and Danish utilities in south Swedish rheumatoid arthritis patients. ANN RHEUM DIS. 2011;70(12):2163–6.
Cooper JT, Lloyd A, Sanchez JJG, Sörstadius E, Briggs A, McFarlane P. Health related quality of life utility weights for economic evaluation through different stages of chronic kidney disease: a systematic literature review. HEALTH QUAL LIFE OUT 2020, 18(1).
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. SYST REV-LONDON. 2017;6(1):245.
Acknowledgements
Not applicable.
Funding
This study is part of the research of the Post-Marketing Clinical Research Special Project for Innovative Drugs Programme (Grant Number: WKZ2023CX210008), funded by the Development Centre for Medical Science & Technology, National Health Commission of the People’s Republic of China.
Author information
Authors and Affiliations
Contributions
Y.W. : Conceptualization, Methodology, Validation, Data Curation, Writing - Review & Editing, Visualization, Supervision, Project administration. Y. X. : Conceptualization, Methodology, Software, Formal analysis, Investigation, Writing - Original Draft, Visualization; H.S. : Formal analysis, Investigation, Writing – Review; H. P. : Investigation; J. C. : Resources, Supervision, Writing – Review, Project administration; J. Y. : Resources, Supervision, Writing – Review, Project administration; Y.W. and Y. X. shared the first author; J. Y. and J. C. shared the corresponding author;
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Y., Xu, Y., Shan, H. et al. Health state utility values of type 2 diabetes mellitus and related complications: a systematic review and meta-regression. Health Qual Life Outcomes 22, 74 (2024). https://doi.org/10.1186/s12955-024-02288-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02288-1