Abstract
Background
Limited evidence exists on the determinants of quality of life (QoL) specific to adults with type 1 diabetes (T1D). Further, it appears no study has compared the determinants of QoL between T1D and type 2 diabetes (T2D) groups. The objectives of this study were to examine: (1) determinants of QoL in adults with T1D; and, (2) differences in QoL determinants between T1D and T2D groups.
Methods
The Alberta Longitudinal Exercise and Diabetes Research Advancement (ALEXANDRA) study, a longitudinal study of adults with diabetes in Alberta, Canada. Adults (18 years and older) with T1D (N = 490) and T2D (N = 1,147) provided information on demographics (gender, marital status, education, and annual income), personality (activity trait), medical factors (diabetes duration, insulin use, number of comorbidities, and body mass index), lifestyle behaviors (smoking habits, physical activity, and diet), health-related quality of life (HRQL) and life satisfaction. Multiple regression models identified determinants of HRQL and life satisfaction in adults with T1D. These determinants were compared with determinants for T2D adults reported in a previous study from this population data set. Factors significantly associated with HRQL and life satisfaction in either T1D or T2D groups were further tested for interaction with diabetes type.
Results
In adults with T1D, higher activity trait (personality) score (β = 0.28, p < 0.01), fewer comorbidities (β = - 0.27, p < 0.01), lower body mass index (BMI)(β = - 0.12, p < 0.01), being a non-smoker (β = - 0.14, p < 0.01), and higher physical activity levels (β = 0.16, p < 0.01) were associated with higher HRQL. Having a partner (β = 0.11, p < 0.05), high annual income (β = 0.16, p < 0.01), and high activity trait (personality) score (β = 0.27, p < 0.01) were significantly associated with higher life satisfaction. There was a significant age × diabetes type interaction for HRQL. The T2D group had a stronger positive relationship between advancing age and HRQL compared to the T1D group. No interaction was significant for life satisfaction.
Conclusions
Health services should target medical and lifestyle factors and provide support for T1D adults to increase their QoL. Additional social support for socioeconomically disadvantaged individuals living with this disease may be warranted. Health practitioners should also be aware that age has different effects on QoL between T1D and T2D adults.
Similar content being viewed by others
Background
More than 180 million people worldwide have diabetes mellitus, and the number of diabetes patients is estimated to double by 2030 [1]. The increasing trend of diabetes has been reported for both type 1 diabetes (T1D) [2–4] and type 2 diabetes (T2D) populations [5, 6].
Diabetes has detrimental effects on health outcomes including quality of life (QoL) outcomes [7] and studies have shown significant negative associations for health-related quality of life (HRQL), one specific aspect of QoL, with its prognosis [8–10]. Thus, further understanding the determinants of HRQL and QoL among individuals with diabetes could guide tailored and targeted intervention strategies to improve these outcomes for this population group.
We examined personal, medical and lifestyle determinants of HRQL and life satisfaction in adults with type 2 diabetes in a previous study [11] and found older age, higher income, higher score on activity (personality) trait, not using insulin, having fewer comorbidities, lower BMI, being a non-smoker, and a higher physical activity level were significantly associated with better HRQL in adults with T2D. Age, gender, marital status, income, activity trait, insulin, comorbidities, higher BMI, smoking, and higher general diet score were significantly associated with life satisfaction.
As for T1D, although several studies have examined determinants of HRQL in adolescents and young adults with T1D [12–17], only a few studies have examined the determinants of HRQL and QoL in adults with T1D. One study that examined 397 adults with T1D, reported that female gender, lower income, longer diabetes duration, diabetes complications, experiencing more than one episode of hypoglycemia per month, and low physical activity levels were associated with poor HRQL [18]. Another study found female gender, obesity, diabetes complication and comorbidities were associated with lower HRQL, among 784 T1D adults [19]. Further Parkerson and colleagues [20] found that marital status, social relationships, and comorbidities were associated with HRQL among 170 T1D adults [20].
Despite aetiological differences between T1D and T2D [21–23], differences in levels of HRQL and QoL as well as their determinants between the two diabetes types have not been thoroughly investigated in adults with diabetes. Jacobson and colleagues [24] compared HRQL scores between 240 adults with T1D or T2D, and identified higher HRQL in T2D after adjusting for demographic factors (i.e., age, marital status and education), diabetes complications, and diabetes duration. Another study compared levels of three HRQL measures in adults (T1D, N = 236; T2D, N = 889) and found no differences in EQ-5D and QoL-DN scores between the two samples, but a higher global health profile (SF-36) score in the T2D group was reported [25]. Finally, in two studies on youth with diabetes, HRQL was lower among T2D individuals compared to those with T1D [26, 27].
From the above, it is apparent that a limited number of studies have investigated the determinants of HRQL in adults with T1D. Further, despite the aetiological and HRQL differences between the two diabetes types, it appears limited research has specifically examined the differences in determinants of HRQL and QoL between T1D and T2D adults. The previous literature on diabetes populations has focused primarily on HRQL, while evidence on QoL (a broader concept which includes general well-being and life satisfaction dimensions) is sparse. Moreover, while the above studies have examined the differences in the relationships of demographic factors, [24, 27] medical factors (e.g., diabetes duration, complications) [24, 25, 27, 28] with HRQL between the two diabetes groups, to our knowledge, no study has tested models consisting of personality and lifestyle factors to understand the differences in the determinants of HRQL and QoL between these two diabetes groups. In particular, due to the important role that lifestyle behaviors play on the etiology of diabetes management [23] and on improved HRQL [29], it is therefore important to include lifestyle behaviors in multivariate models to examine the determinants of HRQL and QoL between the two diabetes groups.
Therefore, the objectives of this study were to use a comprehensive model [11] to examine: (1) the determinants of HRQL and QoL (life satisfaction) in adults with T1D; and, (2) the interaction effects of diabetes type (i.e., T1D/T2D) on significant determinants of HRQL and QoL in the combined T1D and T2D group. In regards to the first study objective, we hypothesized that personal factors (age, gender, personality), medical factors (duration of diabetes, number of comorbidities, BMI) and lifestyle factors (physical activity) are associated with HRQL and life satisfaction in adults with type 1 diabetes. Due to the exploratory nature of second study objective, no specific a priori hypotheses were made for the variables (personal, medical, lifestyle and the interaction effects of diabetes type) examined in the multivariate models.
Methods
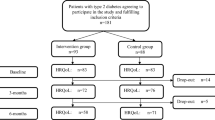
The A lberta L ongitudinal Ex ercise an d D iabetes R esearch A dvancement (ALEXANDRA) study was a population-based, longitudinal study of physical activity determinants in adults with diabetes in Alberta, Canada. The baseline data collection commenced in May 2002. The study procedures, response rates, and measures are explained elsewhere [30]. In brief, the ALEXANDRA study assessed factors related to physical activity in adults (18 years and older) with diabetes. Baseline assessments were completed by 2,319 individuals with diabetes and 1,662 (510 with T1D and 1,152 with T2D) completed the 6-month assessment. The data from the 6-month assessment were used for this study. The study protocol was reviewed by the University of Alberta Health Research Ethics Board. All participants completed written informed consent.
The determinants of HRQL and life satisfaction in the T2D group from the ALEXANDRA Study have been reported elsewhere [11]. This paper reports the determinants of HRQL and life satisfaction in the ALEXANDRA study T1D group, and compares the determinants of these outcomes between the T1D and T2D groups.
Measures
Self-report questionnaires were used to collect data on all study variables. Demographic factors (i.e., age, gender, marital status, education, and income) were assessed using identical measures from the Statistics Canada 2001 census [31]. Personality (i.e., activity trait) was measured by Saucier and Ostendorf's [32] 5-item unipolar activity trait markers (i.e., unadventurous, rambunctious, competitive, unenergetic and active), and the mean scores of the five items were used.
Medical factors
Diabetes type, duration of diabetes, insulin use, presence of comorbidities (angina, heart attack, stroke, high blood cholesterol, and high blood pressure), and BMI (kg/m2) were assessed, and the total number of comorbidities for each individual was calculated (score range from 0 to 5).
Lifestyle factors
Smoking habits were assessed by asking current smoking behavior [33]. Physical activity was measured by a modified version of the Godin Leisure-Time Exercise Questionnaire (GLTEQ) [34–36]. Total weekly minutes of moderate and vigorous physical activity were used [37]. Three diet behaviors (i.e., general and specific diet, and carbohydrate spacing) were assessed by the revised version of Diabetes Self-Care Activities measure [38].
Quality of life variables
HRQL was assessed by a single-item question: "In general, compared to other persons your age, would you say your health is poor/fair/good/very good/excellent." The response score of 1 (poor) to 5 (excellent) was calibrated into value of 0 (poor) to 100 (excellent) [39]. The use of a single item question to assess HRQL has been recommended in large population surveys [40, 41]. The 5-item Satisfaction with Life Scale was used to measure life satisfaction [42].
Data analysis
The characteristics between T1D and T2D groups were compared using t-tests and Chi-square analyses. For the T1D sample, we tested four models consisting of personal (Model 1), medical (Model 2), lifestyle factors (Model 3), and all variables (Model 4) to explain HRQL and life satisfaction [11]. Model 1 included demographics and personality. Model 2 included duration of diabetes, a number of comorbid conditions and BMI. Model 3 consisted of smoking habits, physical activity and three dietary behaviors. Model 4 included all variables of Model 1, 2 and 3. A multiple regression analysis was used to identify variables significantly associated with HRQL and life satisfaction in the T1D group and variances explained by the models.
Variables significantly associated with HRQL and life satisfaction in either the T1D or T2D groups were included and further tested for interaction effects between the two diabetes type groups. Interaction variables were created by multiplying independent variables with diabetes type. To avoid collinearity among variables, residuals of the interaction variables were used for the analysis [43]. All analyses were performed by SPSS for Windows 15.0.
Results
Sample characteristics of adults with type 1 diabetes
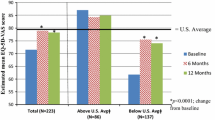
Table 1 displays the characteristics of study sample by diabetes type. The T1D group (51.5 ± 16.4 years) were younger compared with T2D group (63.7 ± 11.4 years, p < 0.0001). The percent of female was higher among T1D group (53.1%) compared to T2D group (47.3%, p = 0.03). More participants in the T2D group had a college degree and higher (43.7%) compared to T1D group (34.9%, p = 0.001). There were no differences in marital status and personality scores (activity trait) between the two diabetes groups. The mean diabetes duration was longer in T1D group (21.6 ± 12.8 years) than in T2D group (11.2 ± 12.8 years). Individuals with T2D had more comorbidities and higher BMI compared to those with T1D (p < 0.0001). There were no differences in smoking habits and physical activity levels between the two groups. T1D group had higher general diet and spacing carbohydrates scores than T2D group (p ≤ 0.01), while the specific diet scores were higher among T2D group (vs. T1D group, p = 0.05). The mean (SD) of HRQL scores were 54.8 ± 26.9 in T1D group and 54.7 ± 25.7 in T2D group. The life satisfaction scores for T1D and T2D groups were 16.2 ± 4.3 and 16.6 ± 4.3, respectively. There were no differences in HRQL and life satisfaction scores between the two diabetes groups.
Determinants of HRQL in type 1 diabetes sample
In Model 1 (personal factors), older age (β = - 0.11, p < 0.05), and higher activity trait (personality) scores (β = 0.38, p < 0.01) were significantly associated with a higher HRQL after controlling for other demographic factors. This model explained 17.4% of the variance for HRQL. In Model 2 (medical factors), a higher number of comorbidities (β = - 0.31, p < 0.01) and a higher BMI (β = - 0.16, p < 0.01) were associated with lower HRQL. This model explained 15.5% of the variance for HRQL. In Model 3, being a non-smoker (β = - 0.14, p < 0.01), higher physical activity levels (β = 0.29, p < 0.01) and more days of spacing carbohydrates (β = 0.11, p < 0.05) were positively associated with HRQL. The model explained 10.6% of the variance for HRQL. In Model 4, higher activity trait (personality) scores (β = 0.28, p < 0.01), fewer comorbidities (β = - 0.27, p < 0.01), lower BMI (β = - 0.12, p < 0.01), currently non-smoking (β = - 0.14, p < 0.01), and higher physical activity levels (β = 0.16, p < 0.01) were significantly associated with higher HRQL. This combined model explained 28.9% of the variance for HRQL. (Table 2)
Determinants of life satisfaction in type 1 diabetes sample
In Model 1 (personal factors), having a partner (β = 0.12, p < 0.01), a higher income (β = 0.16, p < 0.01), and higher activity trait scores (β = 0.30, 1 < 0.01) were significantly associated with higher life satisfaction. The model explained 13.2% of variance for life satisfaction. In Model 2, number of comorbidities (β = - 0.11, p < 0.01) was negatively associated with life satisfaction. This model explained 2.0% of the variance for life satisfaction. In model 3 (lifestyle behaviors) none of the variables were significantly associated with life satisfaction. The model explained 2.9% of variance for life satisfaction. In Model 4, marital status (β = 0.11, p < 0.05), income (β = 0.16, p < 0.01), and activity trait (β = 0.27, p < 0.01) remained significant. The combined model explained 14% of variance for life satisfaction. (Table 2)
Interaction term with diabetes type
Factors significantly associated with HRQL (i.e., age, income, activity trait (personality), number of comorbidities, BMI, current smoking status, and physical activity) and life satisfaction (i.e., age, gender, marital status, income, activity trait (personality), number of comorbidities, BMI, current smoking status, and diet (general) score) in Model 4 were examined for interaction with diabetes type. The interaction of age and diabetes type was significant for HRQL (β = 0.05, p < 0.05, ɧ2 = 0.016), Table 3). Advancing age was associated with increased HRQL in theT2D group, while age was inversely associated with HRQL in the T1D group. There were no significant interactions between the identified determinants and diabetes type in life satisfaction (Table 4).
Discussion
This study examined the differences in HRQL and life satisfaction scores between T1D and T2D groups, the determinants of HRQL and life satisfaction in adults with T1D, and interaction effects of diabetes type on identified determinants of HRQL and life satisfaction using data on a large sample of adults with diabetes. There were no differences in HRQL and life satisfaction scores between the two diabetes groups. We found that personality, numbers of comorbidities, BMI, smoking habits and physical activity were associated with HRQL, while demographic factors (marital status and income) and personality were associated with life satisfaction among adults with T1D. The only difference between the determinants of HRQL and life satisfaction between the two diabetes groups was age; the T2D group had a threshold association between advancing age and HRQL [11] compared to a negative linear relationship in the T1D group. The results of this study add to the limited literature on the determinants of HRQL and QoL in adults with T1D and on differences in determinants of HRQL and QoL between the two diabetes types.
Previous findings on the differences in HRQL scores between T1D and T2D groups have been mixed. In a study of 240 adults, the T2D group had higher HRQL compared to the T1D group, after adjusting for demographic factors (i.e., age, marital status and education), diabetes complications, and diabetes duration [24]. Another study (T1D N = 236, T2D N = 889) found a higher global health profile (SF-36) score in the T2D group compared to the T1D group [25]. In a survey of 1783 adults with diabetes, individuals with T1D had higher HRQL (physical functioning and social functioning) compared to those with T2D [44]. The same study reported no differences in HRQL between T1D and T2D patients treated by diet-only, but a lower HRQL score among T2D patients treated with insulin in comparison to T1D patients [44]. We did not observe significant differences in HRQL and life satisfaction scores between T1D and T2D groups; however, there were significant differences in a number of comorbidities and BMI, which were significantly associated with HRQL, in these two groups which may be explained by differences in the sample characteristics between the two diabetes groups.
The combined model, consisted of personal, medical and lifestyle factors, explained 29% and 14% of the variance respectively, for HRQL and life satisfaction, in our T1D sample which is comparable to our findings for the T2D samples (N = 1,147; 27% for HRQL and 18% for life satisfaction) [11]. Glasgow and colleagues [41] investigated HRQL and associated characteristics (demographic factors, medical factors, and self-care behaviors) in a large (N = 2,056) national sample of adults with diabetes, and found the explained variance to be 17% to 29% for three dimensions of HRQL (i.e., physical functioning, social functioning, and mental health) [44]. The study however, did not examine the factors separately for the T1D and T2D groups.
The variance explained by our model is lower compared to other studies that included psychosocial factors to explain HRQL in diabetes populations. Maddigan and associates [45] investigated factors associated with HRQL, and found that demographic, medical and psychosocial factors, (e.g., depression, stress, sense of belonging to the community, and perceived healthcare needs) were independently associated with HRQL; the model explained 36% of the variance for HRQL [45]. Another study examining coping style, diabetes-specific knowledge, doctor-patient relationship, personal characteristics, and illness on HRQL in adults with diabetes (T1D N = 224, T2D N = 401) reported an explained variance of 62% for HRQL [46]. The inclusion of psychosocial factors in a model has the potential to increase our understanding of HRQL and QoL, and may help identify relationships among psychological factors and other factors (demographics, personality, medical factors, and lifestyle behaviors).
In our study, demographic factors (i.e., marital status and income) were significantly associated with life satisfaction after controlling for other variables. This finding is consistent with previous research on non-diabetes populations [47, 48]. Most T1D cases are diagnosed during childhood [23], and researchers have identified that pediatric diseases have negative effects on adulthood demographic factors (e.g., socioeconomic level, education, marital life) [49, 50]. A review of studies on child-onset T1D identified that these individuals may have disadvantages in employment and are likely to have lower incomes in adulthood [51]. Our T1D sample demonstrated a lower annual income compared to the median income levels of the Alberta data from the 2005 Canadian Census [52]. Considering the observed significant, independent association of marital status and income with life satisfaction, support systems to improve these factors may improve QoL of T1D adults.
Personality (activity trait) was the strongest independent variable associated with HRQL and life satisfaction, which was consistent with our findings from the T2D group [11]. Although there is limited information on personality and HRQL in adults with T1D [53], the relationship between personality, HRQL and QoL is supported by the studies that identified relationships between personality and specific determinants of HRQL or QoL: glycemic control [54], diabetes complications [55, 56], diabetes self-care behaviors [57], coping [58], mood [58] and social support [58]. The observed association of personality with HRQL and QoL in our study may be mediated by these determinants.
The inverse associations of BMI and comorbidities with HRQL are consistent with a previous study [19]. In 784 adults with T1D, BMI and comorbidities such as stroke, cardiovascular disease and high blood pressure were associated with reduced HRQL (Quality of Well Being index-SA health utility score) [19]. The positive relationship between physical activity and HRQL in our study was also consistent with research on 397 adults with T1D [18]. Although we could not identify any study that examined a direct relationship between smoking and HRQL in adults with T1D, smoking was associated with poor glycemic control [59] and renal complication [60], established determinants of HRQL in diabetes population.
Medical and lifestyle factors were not associated with life satisfaction, which was consistent with other studies [61, 62]. In a general population study, BMI was significantly associated with HRQL but not with life satisfaction [61]. In a survey of 3,308 adults with/without chronic conditions, having a heart disease was associated with lower HRQL but not with rating of overall QoL, compared with healthy subjects [62].
We identified a significant interaction between age and diabetes type; however, the effect size was small according to the Cohen's guidelines [63]. The age distributions for the two diabetes groups (51.5 ± 16.4 years for T1D and 63.7 ± 11.4 years for T2D) may have influenced the effect of age on HRQL. The risk of poor self-rated health among diabetics was smaller in the older age group (60-74 years, odds ratio = 4.11, 95% CI = 2.91-5.80) compared to the younger age group (25-39 years, odds ratio = 16.10, 95% CI = 5.97-43.43)[64], suggesting that age could have different effects on HRQL between younger and older adults. The younger age of our T1D sample compared to T2D sample may have partially accounted for the age × diabetes type interaction.
There may also be psychosocial differences which could account for the age × diabetes type interaction. Studies have indicated that social support and its impact on HRQL are influenced by age. Among adults with chronic diseases, younger adults (18-44 years) reported lower social support compared to older adults (65 years and older) [65]. In a T2D sample, age was associated with better patient-provider relationships, and that better patient-provider relationship was associated with higher HRQL [66]. Having better social support among the older group may explain the positive relationship between age and HRQL in our T2D group. In addition, studies suggest poor social support among T1D individuals. A study of T1D adults with a history of pediatric diseases reported that these adults demonstrated delays or failure to achieve social development [67]. Also, among young adults, individuals with T1D showed poorer social support compared to a non-diabetic group [68]. More than 30% of our T1D sample was diagnosed with diabetes before the age of 18, which may have affected their social development and subsequent support.
Study strengths include a large population sample of adults with T1D and T2D adults, the use of validated measures of HRQL, life satisfaction and personality assessment. Several limitations however need to be acknowledged. First, because this was a secondary study, some measures were not specifically designed to examine HRQL or QoL. Further, as prior studies in diabetes population report determinants of HRQL vary for dimensions of HRQL [24, 44], future studies are encouraged to test determinants of each specific component of HRQL. Second, the results cannot imply causality amongst the significant relationships because of cross-sectional data. To assess causality, intervention studies are needed to investigate whether intervening on the identified determinants could improve HRQL and QoL in adults with diabetes. Third, the study participants were recruited through Alberta Registry which may have resulted in more cases with T1D (30% of overall sample). Finally, our study didn't include other established determinants of HRQL and QoL (e.g., psychological factors, diabetes complications). Despite these limitations, our findings provide important information regarding the determinants of HRQL and QoL among T1D adults and the differences between the two diabetes populations.
The significant associations of medical and lifestyle factors with HRQL suggest that health practitioners should be encouraged to achieve good glycemic and cardiovascular risk factor control, and promote lifestyle interventions among T1D population. Demographic factors were significantly associated with life satisfaction in the T1D group. Previous studies have identified that diabetes, especially during earlier life, negatively affects socioeconomic status [50, 51, 69]. Our results imply that major health services targeting glycemic and cardiovascular risk factor control and lifestyle behaviors may not be sufficient to improve overall QoL of T1D adults. Additional support for socioeconomically disadvantaged individuals living with this disease may be warranted.
Conclusions
In summary, medical factors and lifestyle behaviors were independently associated with HRQL in the T1D group. Health practitioners should be encouraged to achieve good glycemic and cardiovascular risk factor control, and promote lifestyle interventions to improve HRQL and overall QoL in this population. Additional support for socioeconomically disadvantaged adults with T1D may be needed. With the exception of age, the determinants of HRQL and QoL appear to be similar between T1D and T2D adults, suggesting that both diabetes groups may benefit from achieving generic, approaches in targeting optimal control of glycemic level and comorbidities as well as promoting healthy lifestyle.
Abbreviations
- ALEXANDRA:
-
Alberta Longitudinal Exercise and Diabetes Research Advancement
- BMI:
-
body mass index
- CI:
-
confidence interval
- HRQL:
-
health-related quality of life
- QoL:
-
quality of life
- T1D:
-
type 1 diabetes
- T2D:
-
type 2 diabetes.
References
World Health Organization: Diabetes. Fact sheet N°312. [http://www.who.int/mediacentre/factsheets/fs312/en/]
Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999 Diabet Med 2006,23(8):857–866.
Patterson CC, Dahlquist GG, Gyurus E, Green A, Soltesz G: Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet 2009,373(9680):2027–2033. 10.1016/S0140-6736(09)60568-7
Harjutsalo V, Sjoberg L, Tuomilehto J: Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet 2008,371(9626):1777–1782. 10.1016/S0140-6736(08)60765-5
Gregg EW, Cheng YJ, Narayan KM, Thompson TJ, Williamson DF: The relative contributions of different levels of overweight and obesity to the increased prevalence of diabetes in the United States: 1976–2004. Prev Med 2007,45(5):348–352. 10.1016/j.ypmed.2007.07.020
Kaufman RF: Type 2 diabetes in children and young adults: A "New Epidemic.". Clinical Diabetes 2002,20(4):217–218. 10.2337/diaclin.20.4.217
Rubin RR, Peyrot M: Quality of life and diabetes. Diabetes Metab Res Rev 1999,15(3):205–218. 10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O
Landman GW, van Hateren KJ, Kleefstra N, Groenier KH, Gans RO, Bilo HJ: Health-related quality of life and mortality in a general and elderly population of patients with type 2 diabetes (ZODIAC-18). Diabetes Care 2010,33(11):2378–2382. 10.2337/dc10-0979
McEwen LN, Kim C, Haan MN, Ghosh D, Lantz PM, Thompson TJ, Herman WH: Are health-related quality-of-life and self-rated health associated with mortality? Insights from Translating Research Into Action for Diabetes (TRIAD). Prim Care Diabetes 2009,3(1):37–42. 10.1016/j.pcd.2009.01.001
Kleefstra N, Landman GW, Houweling ST, Ubink-Veltmaat LJ, Logtenberg SJ, Meyboom-de Jong B, Coyne JC, Groenier KH, Bilo HJ: Prediction of mortality in type 2 diabetes from health-related quality of life (ZODIAC-4). Diabetes Care 2008,31(5):932–933. 10.2337/dc07-2072
Imayama I, Plotnikoff RC, Courneya KS, Johnson JA: Determinants of quality of life in type 2 diabetes population: the inclusion of personality. Qual Life Res 2010.
Graue M, Wentzel-Larsen T, Bru E, Hanestad BR, Sovik O: The coping styles of adolescents with type 1 diabetes are associated with degree of metabolic control. Diabetes Care 2004,27(6):1313–1317. 10.2337/diacare.27.6.1313
Hoey H, Aanstoot HJ, Chiarelli F, Daneman D, Danne T, Dorchy H, Fitzgerald M, Garandeau P, Greene S, Holl R, et al.: Good metabolic control is associated with better quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care 2001,24(11):1923–1928. 10.2337/diacare.24.11.1923
Buresova G, Veleminsky M Jr, Veleminsky M Sr: Health related quality of life of children and adolescents with type 1 diabetes. Neuro Endocrinol Lett 2008,29(6):1045–1053.
Aman J, Skinner TC, de Beaufort CE, Swift PG, Aanstoot HJ, Cameron F: Associations between physical activity, sedentary behavior, and glycemic control in a large cohort of adolescents with type 1 diabetes: the Hvidoere Study Group on Childhood Diabetes. Pediatr Diabetes 2009,10(4):234–239. 10.1111/j.1399-5448.2008.00495.x
Wiesinger GF, Pleiner J, Quittan M, Fuchsjager-Mayrl G, Crevenna R, Nuhr MJ, Francesconi C, Seit HP, Francesconi M, Fialka-Moser V, et al.: Health related quality of life in patients with long-standing insulin dependent (type 1) diabetes mellitus: benefits of regular physical training. Wien Klin Wochenschr 2001,113(17–18):670–675.
Faulkner MS: Quality of life for adolescents with type 1 diabetes: parental and youth perspectives. Pediatr Nurs 2003,29(5):362–368.
Lloyd CE, Orchard TJ: Physical and psychological well-being in adults with Type 1 diabetes. Diabetes Res Clin Pract 1999,44(1):9–19. 10.1016/S0168-8227(99)00004-2
Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, Engelgau MM, Kaplan RM, Herman WH: Valuing health-related quality of life in diabetes. Diabetes Care 2002,25(12):2238–2243. 10.2337/diacare.25.12.2238
Parkerson GR Jr, Connis RT, Broadhead WE, Patrick DL, Taylor TR, Tse CK: Disease-specific versus generic measurement of health-related quality of life in insulin-dependent diabetic patients. Med Care 1993,31(7):629–639. 10.1097/00005650-199307000-00005
Alberti KG, Zimmet PZ: Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998,15(7):539–553. 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
Cnop M, Welsh N, Jonas JC, Jorns A, Lenzen S, Eizirik DL: Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: many differences, few similarities. Diabetes 2005,54(Suppl 2):S97–107.
Loghmani E: Diabetes mellitus: type 1 and type 2. In Guidelines for Adolescent Nutrition Services Edited by: Stang J, Story M. 2005, 167–182.
Jacobson AM, de Groot M, Samson JA: The evaluation of two measures of quality of life in patients with type I and type II diabetes. Diabetes Care 1994,17(4):267–274. 10.2337/diacare.17.4.267
Currie CJ, Poole CD, Woehl A, Morgan CL, Cawley S, Rousculp MD, Covington MT, Peters JR: The health-related utility and health-related quality of life of hospital-treated subjects with type 1 or type 2 diabetes with particular reference to differing severity of peripheral neuropathy. Diabetologia 2006,49(10):2272–2280. 10.1007/s00125-006-0380-7
Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL: The PedsQL in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and type 1 Diabetes Module. Diabetes Care 2003,26(3):631–637. 10.2337/diacare.26.3.631
Naughton MJ, Ruggiero AM, Lawrence JM, Imperatore G, Klingensmith GJ, Waitzfelder B, McKeown RE, Standiford DA, Liese AD, Loots B: Health-related quality of life of children and adolescents with type 1 or type 2 diabetes mellitus: SEARCH for Diabetes in Youth Study. Arch Pediatr Adolesc Med 2008,162(7):649–657. 10.1001/archpedi.162.7.649
Solli O, Stavem K, Kristiansen IS: Health-related quality of life in diabetes: The associations of complications with EQ-5D scores. Health Qual Life Outcomes 2010, 8: 18. 10.1186/1477-7525-8-18
Bize R, Johnson JA, Plotnikoff RC: Physical activity level and health-related quality of life in the general adult population: a systematic review. Prev Med 2007,45(6):401–415. 10.1016/j.ypmed.2007.07.017
Plotnikoff RC, Taylor LM, Wilson PM, Courneya KS, Sigal RJ, Birkett N, Raine K, Svenson LW: Factors associated with physical activity in Canadian adults with diabetes. Med Sci Sports Exerc 2006,38(8):1526–1534. 10.1249/01.mss.0000228937.86539.95
Canada S: Census 2001–2B. In Health Canada. Edited by: Canada H. Ottawa, Ontario; 2001:1–32.
Saucier G, Ostendorf F: Hierarchical subcomponents of the Big Five personality factors: a cross-language replication. J Pers Soc Psychol 1999,76(4):613–627.
Plotnikoff RC, Hugo K, Cousineau N: Heart disease risk factor prevalence and profiles in a randomized community sample of Canadian women. Can J Public Health 2001,92(2):121–126.
Godin G, Shephard RJ: A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985,10(3):141–146.
Jacobs DR Jr, Ainsworth BE, Hartman TJ, Leon AS: A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc 1993,25(1):81–91. 10.1249/00005768-199301000-00012
Miller DJ, Freedson PS, Kline GM: Comparison of activity levels using the Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc 1994,26(3):376–382.
Plotnikoff RC, Lippke S, Karunamuni N, Eves N, Courneya KS, Sigal R, Birkett NJ: Co-morbidity, functionality and time since diagnosis as predictors of physical activity in individuals with type 1 or type 2 diabetes. Diabetes Res Clin Pract 2007,78(1):115–122. 10.1016/j.diabres.2007.02.016
Toobert DJ, Hampson SE, Glasgow RE: The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000,23(7):943–950. 10.2337/diacare.23.7.943
Hays RD, Sherbourne CD, Mazel RM: The RAND 36-Item Health Survey 1.0. Health Econ 1993,2(3):217–227. 10.1002/hec.4730020305
Quesnel-Vallee A: Self-rated health: caught in the crossfire of the quest for 'true' health? Int J Epidemiol 2007,36(6):1161–1164. 10.1093/ije/dym236
Cunny KA, Perri M: Single-item vs multiple-item measures of health-related quality of life. Psychol Rep 1991,69(1):127–130. 10.2466/pr0.1991.69.1.127
Diener E, Emmons RA, Larsen RJ, Griffin S: The Satisfaction With Life Scale. J Pers Assess 1985,49(1):71–75. 10.1207/s15327752jpa4901_13
Burrill DF: Modeling and Interpreting Interactions in Multiple Regression. Education 1989, 27: 1–12.
Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L: Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care 1997,20(4):562–567. 10.2337/diacare.20.4.562
Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA: Understanding the determinants of health for people with type 2 diabetes. Am J Public Health 2006,96(9):1649–1655. 10.2105/AJPH.2005.067728
Rose M, Fliege H, Hildebrandt M, Schirop T, Klapp BF: The network of psychological variables in patients with diabetes and their importance for quality of life and metabolic control. Diabetes Care 2002,25(1):35–42. 10.2337/diacare.25.1.35
Mookherjee HN: A comparative assessment of life satisfaction in the United States: 1978–1988. J Soc Psychol 1992,132(3):407–409. 10.1080/00224545.1992.9924717
Melin R, Fugl-Meyer KS, Fugl-Meyer AR: Life satisfaction in 18- to 64-year-old Swedes: in relation to education, employment situation, health and physical activity. J Rehabil Med 2003,35(2):84–90. 10.1080/16501970306119
Boman KK, Bodegard G: Life after cancer in childhood: social adjustment and educational and vocational status of young-adult survivors. J Pediatr Hematol Oncol 2004,26(6):354–362. 10.1097/00043426-200406000-00005
Ahlfield JE, Soler NG, Marcus SD: The young adult with diabetes: impact of the disease on marriage and having children. Diabetes Care 1985,8(1):52–56. 10.2337/diacare.8.1.52
Milton B, Holland P, Whitehead M: The social and economic consequences of childhood-onset Type 1 diabetes mellitus across the lifecourse: a systematic review. Diabet Med 2006,23(8):821–829. 10.1111/j.1464-5491.2006.01796.x
Canada Statistics: 2006 Community Profiles. 2009.
Taylor MD, Frier BM, Gold AE, Deary IJ: Psychosocial factors and diabetes-related outcomes following diagnosis of Type 1 diabetes in adults: the Edinburgh Prospective Diabetes Study. Diabet Med 2003,20(2):135–146. 10.1046/j.1464-5491.2003.00887.x
Vollrath ME, Landolt MA, Gnehm HE, Laimbacher J, Sennhauser FH: Child and parental personality are associated with glycaemic control in Type 1 diabetes. Diabet Med 2007,24(9):1028–1033. 10.1111/j.1464-5491.2007.02215.x
Robinson N, Stevens LK, Bush LJ, Fuller JH: Personality characteristics in diabetic patients. Practical Diabetes International 1989,6(5):224–227. 10.1002/pdi.1960060510
Brickman AL, Yount SE, Blaney NT, Rothberg ST, De-Nour AK: Personality traits and long-term health status. The influence of neuroticism and conscientiousness on renal deterioration in type-1 diabetes. Psychosomatics 1996,37(5):459–468. 10.1016/S0033-3182(96)71534-7
Skinner TC, Hampson SE, Fife-Schaw C: Personality, personal model beliefs, and self-care in adolescents and young adults with Type 1 diabetes. Health Psychol 2002,21(1):61–70.
Rose M, Burkert U, Scholler G, Schirop T, Danzer G, Klapp BF: Determinants of the quality of life of patients with diabetes under intensified insulin therapy. Diabetes Care 1998,21(11):1876–1885. 10.2337/diacare.21.11.1876
Hofer SE, Rosenbauer J, Grulich-Henn J, Naeke A, Frohlich-Reiterer E, Holl RW: Smoking and metabolic control in adolescents with type 1 diabetes. J Pediatr 2009,154(1):20–23 e21. 10.1016/j.jpeds.2008.07.052
Scott LJ, Warram JH, Hanna LS, Laffel LM, Ryan L, Krolewski AS: A nonlinear effect of hyperglycemia and current cigarette smoking are major determinants of the onset of microalbuminuria in type 1 diabetes. Diabetes 2001,50(12):2842–2849. 10.2337/diabetes.50.12.2842
Grigg A, Thommasen HV, Tildesley H, Michalos A: Comparing self-rated health, satisfaction and quality of life scores between diabetics and others living in the Bella Coola Valley. Soc Indic Res 2006,76(2):263–281. 10.1007/s11205-004-6609-2
Arnold R, Ranchor AV, Sanderman R, Kempen GI, Ormel J, Suurmeijer TP: The relative contribution of domains of quality of life to overall quality of life for different chronic diseases. Qual Life Res 2004,13(5):883–896.
Cohen J (Ed): Statistical Power Analysis for the Behavioral Sciences 2nd edition. Hillsdale, New Jersey: Lawrence Erlbaum Associates, Inc.; 1988.
Ho SY, Mak KK, Thomas GN, Schooling M, Fielding R, Janus ED, Lam TH: The relation of chronic cardiovascular diseases and diabetes mellitus to perceived health, and the moderating effects of sex and age. Soc Sci Med 2007,65(7):1386–1396. 10.1016/j.socscimed.2007.05.032
Sherbourne CD, Meredith LS, Rogers W, Ware JE Jr: Social support and stressful life events: age differences in their effects on health-related quality of life among the chronically ill. Qual Life Res 1992,1(4):235–246. 10.1007/BF00435632
Maddigan SL, Majumdar SR, Johnson JA: Understanding the complex associations between patient-provider relationships, self-care behaviours, and health-related quality of life in type 2 diabetes: a structural equation modeling approach. Qual Life Res 2005,14(6):1489–1500. 10.1007/s11136-005-0586-z
Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA: Young adult patients with a history of pediatric disease: impact on course of life and transition into adulthood. J Adolesc Health 2006,39(1):4–13. 10.1016/j.jadohealth.2005.03.011
Lloyd CE, Robinson N, Andrews B, Elston MA, Fuller JH: Are the social relationships of young insulin-dependent diabetic patients affected by their condition? Diabet Med 1993,10(5):481–485. 10.1111/j.1464-5491.1993.tb00103.x
Ng YC, Jacobs P, Johnson JA: Productivity losses associated with diabetes in the US. Diabetes Care 2001,24(2):257–261. 10.2337/diacare.24.2.257
Acknowledgements
This study was funded by the Alberta Heritage Foundation for Medical Research. II was supported from the Nakajima Foundation, Tokyo, Japan. RCP was supported from a Salary Award from the Canadian Institutes of Health Research (Applied Public Health Chair Program). KSC holds a Canada Research Chair. JAJ holds a Canada Research Chair and is a Senior Scholar with Alberta Heritage Foundation for Medical Research. We are grateful to the statistical and editorial assistance from Nandini Karunamuni.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
II performed data analysis, interpreted the data, and drafted the manuscript. RCP, KSC and JAJ were involved in study concept and design, acquisition of the data, data interpretation, manuscript drafting and revision of the manuscript. All authors approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Imayama, I., Plotnikoff, R.C., Courneya, K.S. et al. Determinants of quality of life in adults with type 1 and type 2 diabetes. Health Qual Life Outcomes 9, 115 (2011). https://doi.org/10.1186/1477-7525-9-115
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-9-115