Abstract
Background
The objective of this study was to investigate the association between ethnicity and health related quality of life (HRQoL) in patients with type 2 diabetes.
Methods
The EuroQol EQ-5D measure was administered to 1,978 patients with type 2 diabetes in the UK Asian Diabetes Study (UKADS): 1,486 of south Asian origin (Indian, Pakistani, Bangladeshi or other south Asian) and 492 of white European origin. Multivariate regression using ordinary least square (OLS), Tobit, fractional logit and Censored Least Absolutes Deviations estimators was used to estimate the impact of ethnicity on both visual analogue scale (VAS) and utility scores for the EuroQol EQ-5D.
Results
Mean EQ-5D VAS and utility scores were lower among south Asians with diabetes compared to the white European population; the unadjusted effect on the mean EQ-5D VAS score was −7.82 (Standard error [SE] = 1.06, p < 0.01) and on the EQ-5D utility score was −0.06 (SE = 0.02, p < 0.01) (OLS estimator). After controlling for socio-demographic and clinical confounders, the adjusted effect on the EQ-5D VAS score was −9.35 (SE = 2.46, p < 0.01) and on the EQ-5D utility score was 0.06 (SE = 0.04), although the latter was not statistically significant.
Conclusions
There was a large and statistically significant association between south Asian ethnicity and lower EQ-5D VAS scores. In contrast, there was no significant difference in EQ-5D utility scores between the south Asian and white European sub-groups. Further research is needed to explain the differences in effects on subjective EQ-5D VAS scores and population-weighted EQ-5D utility scores in this context.
Similar content being viewed by others
Background
Diabetes is a chronic metabolic disease estimated to have affected 285 million people globally in 2010, with the prevalence expected to increase to 438 million people by 2030 [1]. In the UK, there were approximately 2.8 million people with some form of diabetes in 2010 and, of those, 90% had type 2 diabetes[1]. Type 2 diabetes prevalence is reported to be three to four times higher in south Asian adults and the disease may occur a decade earlier than in the white European majority population in the UK [2, 3]. Type 2 diabetes is associated with micro and macro vascular complications, including increased risk of cardiovascular disease, diabetic nephropathy, retinopathy, neuropathy and lower extremity amputations [4]. Type 2 diabetes and its associated co-morbidities may impact on many areas of an individual’s life, including physical function, social interaction and mental well-being; patients may consequently experience impaired health related quality of life (HRQoL).
There is evidence to suggest that the prevalence, disease progression and treatment outcomes for people with type 2 diabetes vary significantly between ethnic groups [5–9], but very little research has been undertaken to date to directly assess the extent to which ethnicity impacts on HRQoL in adults with diabetes. In addition, in the few studies that have explored this relationship, there is inconsistency in the tools used to measure HRQoL and a lack of consensus about the optimum method of assessment. This, combined with differences in the black and minority ethnic (BME) populations studied, have resulted in both negative [5–7, 9–11] and positive [12–14] associations being reported between ethnicity and HRQoL. Although ethnicity may have an independent effect on HRQoL for people with type 2 diabetes, the size of any effect is unclear. More accurate quantification of such an effect should provide policy makers and service providers with evidence to develop initiatives that improve HRQoL for those ethnic minority populations that are most detrimentally affected. Furthermore, government agencies in many nations, such as the National Institute for Health and Care Excellence (NICE) in England and Wales, rely on cost-utility analyses, which seek to maximise Quality Adjusted Life Year (QALY) based measures of benefit that contain a HRQoL component. If there are ethnic differences in how a disease such as diabetes affects HRQoL, this should be taken into account when considering the introduction of new interventions on cost-effectiveness grounds.
The aim of the study was to investigate the association between ethnicity and HRQoL in patients with type 2 diabetes where HRQoL was measured using visual analogue scale (VAS) and utility scores for the EuroQol EQ-5D measure [15].
Methods
This research used data collected by the UK Asian Diabetes Study (UKADS), which comprised of a community-based, cluster randomized controlled trial that evaluated the effectiveness of a culturally sensitive enhanced care package in UK general practice in improving cardiovascular risk factors in south Asian patients with type 2 diabetes, plus a parallel cohort study of cardiovascular risk factors in south Asian and white European patients with type 2 diabetes[3]. The main study, carried out in 2004–2007, recruited a total of 1486 south Asian and 492 white European patients from 25 general practices in Birmingham (16 practices) and Coventry (9 practices). All adults with type 2 diabet es were eligible for inclusion in the study; people with type 1 diabetes or impaired glucose tolerance were excluded. The research reported in this paper uses a cross-sectional study design, comparing HRQoL data for south Asian and white European patients in UKADS at the baseline assessment.
HRQoL was measured using the EuroQol EQ-5D, which is the generic, multi-attribute, preference based measure preferred by NICE for cost-effectiveness comparative purposes [16, 17]. The EQ-5D consists of two principal measurement components. The first is a descriptive system, which defines health-related quality of life in terms of five dimensions: ‘mobility’, ‘self care’, ‘usual activities’, ‘pain/discomfort’ and ‘anxiety/depression’. Responses in each dimension are divided into three ordinal levels coded: (1) no problems; (2) some or moderate problems; and (3) severe or extreme problems. A total of 243 (35) health states are generated by the EQ-5D descriptive system. For the purposes of this study, the York A1 (Dolan) tariff was applied to each set of responses to generate an EQ-5D utility score (preference weight) for each patient [16]. The York A1 tariff set was derived from a survey of the UK general population (n = 3337) which used the time trade-off valuation method to estimate utility scores for a subset of 45 EQ-5D health states, with the remainder of the EQ-5D health states subsequently valued through the estimation of a multivariate model [17]. Resulting utility scores range from scores −0.59 to 1.0, with 0 representing death and 1.0 representing full health; values below 0 indicate health states worse than death. The second measurement component of the EQ-5D consists of a 20 cm vertical visual analogue scale ranging from 100 (best imaginable health state) to 0 (worst imaginable health state), which provides an indication of the subject’s own assessment of their health status on the day of the survey.
Descriptive statistics were produced for baseline characteristics and analysed by ethnic meta-group (white European vs. south Asian) and by south Asian subgroup (Indian, Pakistani, Bangladeshi and other south Asian). Chi-squared and t-tests were employed to compare baseline variables between ethnic meta-groups and between ethnic subgroups. A descriptive analysis of levels of function within each EQ-5D dimension by ethnicity was complemented by further analysis of sub-optimal levels of function (defined as level 2 or 3) for each EQ-5D dimension. Fisher’s exact test for equality of proportions was used to compare sub-optimal levels of function within each EQ-5D dimension between ethnic meta-groups.
Four alternative methods of multivariate analysis were used to model the association between EQ-5D VAS or utility scores (dependent variables) and ethnicity: ordinary least squares (OLS), Tobit, fractional logit (Flogit) [18] and Censored Least Absolutes Deviations (CLAD) [19]. OLS regression is the most widely used of these estimators in the literature. It relies on the Gauss Markov assumptions about the data and variables used in the model, which need to be met in order to produce unbiased estimators [20]. Tobit regression was used to account for the non-trivial proportion of the study population with maximum EQ-5D VAS scores or EQ-5D utility scores [20, 21]. The main assumptions of the Tobit model are that the error term has a normal distribution and that it has constant variance. If there is heteroskedasticity present, this may lead to inconsistent estimators being produced. Alternatively, when there are specification issues with the Tobit model, Powell’s Censored Least Absolutes Deviation (CLAD) estimator can be applied. The CLAD estimator is a generalisation of the least absolute deviations estimator [19]. The fractional logit model (Flogit) [18] provides a further alternative to the OLS and Tobit estimators. The Flogit model considers the dependent variable as a count, rather than a continuous variable, by using logit transformation and binomial regression. There is no single empirical test to evaluate the performance of these alternative estimators, so we developed an a priori plan based on comparable studies. Our aim was to investigate whether one estimator provided consistently more accurate estimates. Mean absolute errors (MAEs) and root mean squared errors (RMSEs) were used to examine differences between predicted and observed EQ-5D VAS and utility scores and to also check model performance [22]. All models were tested for heteroskedasticity using the White test [20]. Once a suitable model had been chosen, bi-variate analyses were conducted to estimate the unadjusted effects of ethnicity on EQ-5D VAS and utility scores. Partially adjusted and fully adjusted multi-variate models were then estimated. In the partially adjusted multivariate models, additional independent variables included age (continuous variable), gender (male, female), marital status (single, married, divorced, widowed) and the Carstairs deprivation index (categorical variable, see Table 1 for categories). The Carstairs index is an index of deprivation, based on four census indicators: low social class, lack of car ownership, overcrowding and male unemployment. In the original UKADS data, patient post-codes were collected, which were linked to the area specific Carstairs deprivation index, with higher scores representing elevated deprivation and vice versa [23]. In the fully adjusted models, further independent variables included body mass index (BMI) (18.5-24.9, <18.5, 25.0-29.9, 30.0-34.9, 35.0-39.9, >40.0), smoking status (non-smoker, current smoker, ex-smoker), alcohol use (yes, no), duration of diabetes in years (0–1, 2–5, 6–10, 11–15, >15), treatment regime (diet, tablets, insulin, insulin and tablets), family history of diabetes (yes, no), history of cardiovascular disease (CVD) (yes, no), albumin concentration (proteinuria and microalbuminuria were defined as urinary albumin to creatinine ratio (UACR) > =30.0 mg/mmol for both males and females and UACR 2.5 – <30.0 mg/mmol for males and 3.5- < 30.0 mg/mmol for females, respectively, with values below these thresholds indicating normal albuminuria) and GP practice.
Finally to allow for potential clustering effects and confounding, the SAS PROC MIXED procedure was separately used to fit hierarchical, combined fixed and random effects models. Random effects were fitted, within a subject term for general practice, allowing for different intercepts for all individual practices (random intercepts models).
The bulk of the analyses were conducted using SPSS 19.0, STATA 11 and SAS 9.3. Differences were considered statistically significant if p-values were less than 0.05.
Results
Table 1 describes the characteristics of each ethnic group. The south Asian sample was younger than the white European group, with a mean age of 57 (standard deviation (SD) 11.9) vs. 64.8 (SD 11.6); this difference was statistically significant (p < 0.001). Duration of diabetes was significantly longer (p < 0.001) for the south Asian compared with the white European sample (Table 1). More south Asians were treated with insulin or a combination of insulin and tablets, compared with white Europeans (18.3% vs. 13.2%), while more white Europeans controlled their diabetes solely through diet (28.9% vs. 11.8%). These patterns were also observed in the study by Bellary et al.[24].
A family history of diabetes was recorded for 50% of patients, with the proportion significantly higher for south Asians compared to their white European counterparts. 18% of South Asians had some history of cardiovascular disease and approximately 28% had some indication of nephropathy (Table 1). However, the presence of chronic heart disease and microalbuminuria was higher in the white European sample, whilst proteinuria was more common amongst south Asians, in comparison to white Europeans.
Most study participants had BMI scores that were above normal (88.6%), with a high proportion of the white European sample classed as obese (54.7%). Using WHO cut-offs for Asian populations, 14% of south Asians were overweight (BMI of 23–24.9) and 80% were obese (BMI of ≥25) [25]. The majority of the sample was non-smokers; however, more white Europeans than south Asians were ex-smokers (37.8% vs. 8.6%). Current alcohol consumption was reported for 182 (12.2%) south Asians compared to 261 (53.0%) of the white Europeans. The mean Carstairs index was significantly higher (indicating residence in areas of higher deprivation) for south Asians at 6.6 (SD 4.6) compared to the white European sample, whose mean score was 1.7 (SD 3.1) (Table 1). Of the south Asian subgroups, Pakistani and Bangladeshi patients were more likely to reside in highly deprived areas.
Table 2 shows proportions of patients with sub-optimal levels of function within EQ-5D dimensions by ethnicity. For all dimensions except mobility a higher proportion of south Asians experienced sub-optimal function compared to their white European counterparts. Most notably, over 50% of the south Asian and white European meta-groups reported sub-optimal function for the pain/discomfort dimension, although the difference between ethnic meta-groups was not statistically significant. For the dimensions of anxiety/depression and usual activities, the proportion of south Asians reporting sub-optimal levels of function was significantly higher (p = 0.01 for usual activities, p = 0.02 for anxiety/depression) compared to their white European counterparts.
Model diagnostics comparing the different estimators for the fully adjusted multivariate models are summarised in online Additional file 1: Table S1 (EQ-5D VAS scores) and online Additional file 1: Table S2 (EQ-5D utility scores). The estimator with the smallest MAE and RMSE values shows the best fit for the data [22]. The CLAD estimator had the largest MAE and RMSE values. The results for the remaining estimators were broadly comparable across model type. The White test rejected the hypothesis of homoscedasticity in the error term (p < 0.01) for all estimators; robust standard errors (SEs) were used to correct for this. For ease of interpretation, we report the results for the OLS estimator in our main tables with comparative results across estimators found in online Additional file 1: Table S3 and S4.
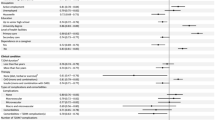
Tables 3 and 4 respectively present results for the OLS unadjusted, partially adjusted and fully adjusted models for the EQ-5D VAS and EQ-5D utility scores. For EQ-5D VAS scores, the impact of being of south Asian descent was a decrement of 7.82 compared to the white European counterparts (SE 1.06; p < 0.01) (Table 3). For EQ-5D utility scores, south Asian descent was, on average, associated with a decrement in utility score of 0.06 (SE 0.02, p < 0.01) (Table 4). After controlling for socio-economic and socio-demographic variables, a significant inverse association remained between south Asian ethnicity and EQ-5D VAS scores [−7.30 (SE 1.36, p < 0.01)]. In contrast, a non-significant association was found between south Asian ethnicity and EQ-5D utility scores. The fully adjusted analyses strengthened the effect of south Asian ethnicity on EQ-5D VAS scores [−9.35 (SE 2.46, p <0.01)] (Table 3), whilst the effect on EQ-5D utility scores remained insignificant [0.06 (SE 0.04)] (Table 4). Results of the separate mixed effects models, which included random intercepts for individual general practices, were very similar to the final OLS estimates; for EQ-5D VAS scores −9.31, p = 0.0002 and for EQ-5D utility scores −0.02, p = 0.5751.
Unadjusted, partially adjusted and fully adjusted analyses were also conducted for south Asian subgroups and can be found in online Additional file 1: Table S5 and S6. In the fully adjusted model, all south Asian ethnicities were associated with significantly lower EQ-5D VAS scores compared to the white European ethnic origin (online Additional file 1: Table S5); the most significant decrement was observed for patients of Indian origin. In contrast, when the EQ-5D utility scores were analysed by ethnic sub-group, the fully adjusted model revealed no significant decrements in scores for each of the south Asian ethnicities compared to those of white European ethnic origin (online Additional file 1: Table S6).
Discussion
In this study, the baseline disease profile of the south Asian patients mirrored that reported in the broader literature; younger people with a longer disease duration, increased severity of disease (as measured by type of treatment), and a higher incidence of family history of the disease, compared to the white European population. However, indications of CVD and albumin concentration were slightly lower in the south Asian group. This may be attributable to the population being younger and also to lifestyle factors, as south Asian patients did not smoke as much and consumed less alcohol than the white European sample. However, the percentage of current smokers in the sample (15%) was less than the current smoking population in England (21%) [26]. Similarly, the percentage of people who consumed alcohol in the entire sample (22%) was less than the comparative figure for England (63%) [27]. The south Asian population resided in areas with higher levels of deprivation than the white European sample. Mean EQ-5D VAS and utility scores were lower than for white European patients; with more of the south Asian population reporting sub-optimal levels of function across the self care, usual activities, and pain and anxiety/depression dimensions of the EQ-5 D. Mobility was the one dimension for which the White European sample reported higher sub-optimal levels of function. This could be related to the fact that the White European sample had a mean age of 64 years compared to a mean age of 57 years for the south Asians.
Our regression analyses indicate that south Asian ethnicity has an overall negative impact on EQ-5D VAS scores in patients with type 2 diabetes. On average, EQ-5D VAS scores were 9.35 lower for south Asians compared to white European patients in the fully adjusted OLS model. Comparison of the ethnic subgroups showed that Indians experienced the largest negative decrement in EQ-5D VAS scores compared to their white European counterparts in the adjusted analyses. Lower EQ-5D utility scores in south Asians were also observed, with south Asians experiencing an adjusted utility decrement of 0.06 compared to the white European sample. However, the effects on EQ-5D utility scores were only significant in the unadjusted analyses. It should be noted that a difference of 0.05 in mean multi-attribute utility scores is deemed clinically important for evaluative purposes [28]. The results of the regression analyses for both the EQ-5D VAS and utility scores remained robust to alternative model estimators.
The study revealed a consistent negative association between south Asian ethnicity and the EQ-5D VAS scores in patients with type 2 diabetes. In the broader literature, there are few studies that used the EQ-5D measure to assess HRQoL in ethnic minority populations with diabetes. Of the studies that did use this measure, Lubetkin et al.[14] reported results similar to the present study. The authors had used the EQ-5D measure to compare HRQoL between African-Americans, Hispanics and white Americans and found that after adjusting for known determinants of HRQoL, including chronic conditions such as diabetes; Hispanics had lower EQ-5D VAS scores and slightly higher EQ-5D utility scores compared to the white American sample. However, African Americans experienced both higher EQ-5D VAS and utility scores compared to the white American population. Although these results are similar in some respects to the ones reported here, they may not be generalisable due to the fact that different ethnic minority populations were studied. Differences may also be attributable to other methodological factors; for example, Lubetkin et al.[14] controlled for income, education and six chronic conditions in their study. In the current study, no data were available for income or education although lifestyle factors, co-morbidities and area deprivation were all included. In addition, cultural differences in rating tendencies have been observed in some studies. Lubetkin et al.[14] discussed the possibility that US Asians may be averse to valuing their health at the upper end of the VAS scale and may choose values towards the middle of the scale. This could partly account for any consistently negative association between ethnic minority status and EQ-5D VAS scores. In contrast, for EQ-5D utility scores, although individuals’ describe their own health-related quality of life, the values placed on those descriptions reflect general population preferences for health states. Moreover, a different valuation technique (the time trade-off approach) is used to derive those values. In the present study, there were patients who reported low EQ-5D VAS scores, such as a score of 20, but who had EQ-5D utility scores at the upper end of the utility scale, for example 0.8. Clearly, further research is required that disentangles the effects of the valuation technique itself and the underpinning source of values when assessing ethnicity-related effects on the HRQoL of individuals with type 2 diabetes.
One caveat to this study was the absence of information on education levels in the two samples. A lower level of education has been shown to be associated with impaired HRQoL [14]. Furthermore, as diabetes is a self-managed disease, higher levels of education could relate to better self-management and control of the disease, which in its turn should promote HRQoL. A study by Thoolen et al. examined the characteristics of patients with diabetes who participate in diabetes self-management programmes [29]. The authors found that education level was the most important factor differentiating participants and non-participants/dropouts, with participation linked to higher education levels. Since the south Asian sample in our study, on average, resided in areas with higher levels of deprivation compared to the White European sample, it is possible that their educational levels were also lower than in the white Europeans. By not adjusting for this difference between the two groups in the regressions, education effects may be reflected in the error terms of our models. A second caveat to the study revolves around the estimators selected to model the association between ethnicity and EQ-5D VAS or utility scores. Our selection of OLS, Tobit, Flogit and CLAD estimators was in keeping with the modelling approaches used more broadly by health economists to estimate EQ-5D values [16, 30]. Furthermore, our statistical plan for model selection, which included the use of MAEs, RMSEs and tests for heteroskedasticity was in keeping with recommended diagnostic approaches [22]. Nevertheless, a number of methodological concerns surround the application of these estimators when modelling EQ-5D data. The OLS estimator does not capture the ceiling effect at 1.0 for utility values, whilst the Tobit and CLAD estimators may generate biased results when the true utility is conceptually bounded above at 1.0 [31, 32]. The FLogit estimator has not previously been used on an extensive basis in the modelling utility data literature; a recent application did not generate promising results [33]. Alternative estimators for modelling health state utility values, such as adjusted limited dependent variable mixture models, are currently under development [34]; their application to UKADS data remains a topic for future enquiry.
Conclusion
The study suggests that south Asian ethnicity has a negative effect on both the EQ-5D VAS and utility scores compared to white Europeans. However no statistically significant difference was observed for utility scores when socio-economic, demographic and clinical variables were included in the models. Moreover, as observed in the broader literature, the nature and magnitude of the HRQoL effects vary depending on the ethnic minority under consideration [12, 14]. Further research is needed to explain the differences in ethnicity-related effects on subjective EQ-5D VAS scores and population-weighted EQ-5D utility scores in patients with type 2 diabetes.
References
Diabetes UK: Diabetes in the UK 2010 – Key statistics on Diabetes. 2010. [http://www.diabetes.org.uk/Documents/Reports/Diabetes_in_the_UK_2010.pdf] Diabetes UK. What is diabetes? 2011. [http://www.diabetes.org.uk/Guide-to-diabetes/Introduction-to-diabetes/What_is_diabetes/]
Greenhalgh PM: Diabetes in British south Asians: nature, nurture, and culture. Diabet Med 1997, 14: 10–18. 10.1002/(SICI)1096-9136(199701)14:1<10::AID-DIA282>3.0.CO;2-B
Bellary S, O'Hare JP, Raymond NT, Gumber A, Mughal S, Szczepura A, Kumar S, Barnett AH, UKADS Study Group: Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet 2008, 371: 1769–1776. 10.1016/S0140-6736(08)60764-3
Amos AF, McCarty DJ, Zimmet P: The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med 1997, 14(Suppl 5):S1–85.
Wändell P: Foreign- and Swedish-born diabetic patients - medical situation and quality of life. Scand J Prim Health Care 1999, 17: 158–163. 10.1080/028134399750002575
Wee H, Li S, Cheung Y, Fong K, Thumboo J: The influence of ethnicity on health-related quality of life in diabetes mellitus. J Diabetes Complications 2006, 20: 170–178. 10.1016/j.jdiacomp.2005.06.010
Thommasen HV, Berkowitz J, Thommasen AT, Michalos AC: Understanding relationships between diabetes mellitus and health-related quality of life in a rural community. Rural & Remote Health 2005, 5: 1–18.
Two Feathers JT, Kieffer EC, Palmisano G, Anderson M, Sinco B, Janz N, Heisler M, Spencer M, Guzman R, Thompson J, Wisdom K, James SA: Racial and ethnic approaches to community health (reach) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health 2005, 95: 1552–1560. 10.2105/AJPH.2005.066134
Quandt SA, Graham CN, Bell RA, Snively BM, Golden SL, Stafford JM, Arcury TA: Ethnic disparities in health-related quality of life among older rural adults with diabetes. Ethn Dis 2007, 17: 471–476.
Mitchell BD, Stern MP, Haffner SM, Hazuda HP, Patterson JK: Functional impairment in Mexican Americans and non-Hispanic whites with diabetes. J Clin Epidemiol 1990, 43: 319–327. 10.1016/0895-4356(90)90118-9
Hill-Briggs F, Gary T, Hill M, Bone L, Brancati F: Health-related quality of life in urban African Americans with type 2 diabetes. J Gen Intern Med 2002, 17: 412–419. 10.1046/j.1525-1497.2002.11002.x
Caldwell EM, Baxter J, Mitchell CM, Shetterly SM, Hamman RF: The association of non-insulin-dependent diabetes mellitus with perceived quality of life in a biethnic population: the San Luis Valley diabetes study. Am J Public Health 1998, 88: 1225–1229. 10.2105/AJPH.88.8.1225
Sedgwick J, Pearce AJ, Gulliford MC: Evaluation of equity in diabetes health care in relation to African and Caribbean ethnicity. Ethn Health 2003, 8: 121–133. 10.1080/13557850303560
Lubetkin E, Jia H, Franks P, Gold M: Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: examining the EQ-5D in the U.S. general population. Qual Life Res 2005, 14: 2187–2196. 10.1007/s11136-005-8028-5
Brooks R: EuroQoL: the current state of play. Health Policy 1996, 37: 53–72. 10.1016/0168-8510(96)00822-6
Dolan P, Gudex C, Kind P, Williams A: A social tariff for EuroQol: Results from a UK general population survey. University of York: York, Centre for Health Economics; 1995:1–19.
NICE: Guide to the methods of technology Appraisal, 2008, section 5.4.1 -5.4.4. 2008. [http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf]
Papke LE, Wooldridge JM: Econometric methods for fractional response variables with an application to 401 (K) plan participation rates. J Appl Econ 1996, 11: 619–632. 10.1002/(SICI)1099-1255(199611)11:6<619::AID-JAE418>3.0.CO;2-1
Powell JL: Least absolute deviations estimation for the censored regression model. J Econom 1984, 25(3):303–325. 10.1016/0304-4076(84)90004-6
Wooldridge JM: Introductory Econometrics: A Modern Approach. 4th edition. Canada: South-Western Cengage Learning; 2009:68–105. 444–471
Clarke P, Gray A, Holman R: Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making 2002, 22: 340–349. 10.1177/027298902400448902
Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A: Measuring and Valuing Health Benefits for Economic Evaluation. Oxford, UK: Oxford University Press; 2007.
Carstairs V, Morris R: Deprivation and health in Scotland. Health Bull (Edinb) 1990, 48: 162–175.
Bellary S, O’Hare P, Raymond NT, Mughal S, Hanif WM, Jones A, Kumar S, Barnett AH: Premature cardiovascular events and mortality in south Asians with type 2 diabetes in the United Kingdom Asian diabetes study – effect of ethnicity on risk. Curr Med Res Opin 2010, 26: 1873–1879. 10.1185/03007995.2010.490468
WHO: Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363: 157–163.
NHS: Statistics on Smoking. England; 2010. [http://www.hscic.gov.uk/catalogue/PUB00684/smok-eng-2010-rep.pdf]
NHS: 2010. Statistics on Alcohol. England; 2010. [http://www.hscic.gov.uk/catalogue/PUB00135/alco-eng-2010-rep.pdf]
Dolan P, Gudex C, Kind P, Williams A: The time trade-off method: results from a general population study. Health Econ 1996, 5: 141–154. 10.1002/(SICI)1099-1050(199603)5:2<141::AID-HEC189>3.0.CO;2-N
Thoolen B, Ridder DD, Bensing J, Gorter K, Rutten G: Who participates in diabetes self-management interventions?: issues of recruitment and retainment. Diabetes Educ 2007, 33: 465–474. 10.1177/0145721707301491
Dakin H: Review of studies mapping from quality of life or clinical measures to EQ-5D: an online database. Health Qual Life Outcomes 2013, 11: 151. 10.1186/1477-7525-11-151
Pullenayegum EM, Tarride JE, Xie F, Goeree R, Gerstein HC, O'Reilly D: Analysis of health utility data when some subjects attain the upper bound of 1: are Tobit and CLAD models appropriate? Value Health 2010, 13(4):487–494. 10.1111/j.1524-4733.2010.00695.x
Pullenayegum EM, Tarride JE, Xie F, O’Reilly D: Calculating utility decrements associated with an adverse event: marginal Tobit and CLAD coefficients should be used with caution. Med Decis Making 2011, 31(6):790–799. 10.1177/0272989X10393284
Dakin H, Gray A, Murray D: Mapping analyses to estimate EQ-5D utilities and responses based on Oxford Knee Score. Qual Life Res 2013, 22(3):683–694. 10.1007/s11136-012-0189-4
Hernández AM, Wailoo AJ, Ara R: Tails from the peak district: adjusted limited dependent variable mixture models of EQ-5D questionnaire health state utility values. Value Health 2012, 15: 550–561. 10.1016/j.jval.2011.12.014
Acknowledgements
We would like to thank the patients who participated in UKADS. We would also like to thank Dr. David Owen of the University of Warwick’s School of Health and Social Studies for his help in linking and converting post code data into Carstairs Index scores. The original UKAD Study received grants from Pfizer, Sanofi -Aventis, Servier Laboratories UK, Merck Sharp & Dohme/Schering-Plough, Takeda UK, Roche, Merck Pharma, Daiichi-Sankyo UK, Boehringer Ingelheim, Eli Lilly, NovoNordisk, Bristol-Myers Squibb, Solvay Health Care, and Assurance Medical Society, UK. There are no relevant conflicts of interest to disclose. UKADS Study Group: The full list of members of the UKADS study group are as follows: Warwickshire Institute for Diabetes, Endocrinology and Metabolism (WISDEM),Medical School, Warwick University and University Hospital Coventry and Warwickshire, Coventry, UK: JP O’Hare, NT Raymond, S Kumar, A Szczepura, K. Johal, A Gumber, IC Agarwal, DK Mistry, FF Lyall, MR Dhadhania, KL Kakad, U Jetty, JF Sihota, S Mall, K Webb, S Khatoon, R Parker, P Claire, G Turner and University of Birmingham, University of Aston and Heart of England NHS Trust, Birmingham, UK: S. Bellary, AH Barnett, A Jones, S Mughal, S Begum, T Kauser, N Mirza, AN Dixon,WM Hanif, A Rahim, W Malik, RA Bhatti, MM Alvi, A Akthar, RAS Sangra, NH Bangash, MD Sheik, AG Hakeem, BG Najak, SA Latif, JS Sanghera, AU Shah, T Sen-Gupta, G O’Gara, PS Moonga, SH Khattak, P Machin, F Hartland, H Kaur, N Janood, J Dhalival, T Fatima, J Taylor, D Fitzpatrick, J Lucas, S Hemming.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TJ was responsible for the day to day conduct of the study, including additional data collection over and above the original data collection within UKADS, analysis and writing. SP and AS had the original idea for the study; together with AG they also provided oversight for the study. AG, NR and SB contributed to the research design, interpretation of results and writing. All authors read and approved the final manuscript.
Electronic supplementary material
12955_2013_1329_MOESM1_ESM.docx
Additional file 1: Table S1: Estimated predicted scores compared to observed EQ-5D VAS scores (fully adjusted model for all south Asians). Table S2. Estimated predicted scores compared to observe EQ-5D utility scores (fully adjusted model for all south Asians). Table S3. Marginal effects for EQ-5D VAS scores for all south Asians† by estimator and model. Table S4. Marginal effects for EQ-5D utility scores for all south Asians† by estimator and model. Table S5. OLS marginal effects of sub-group south Asian ethnicity on EQ-5D VAS scores†±. Table S6. OLS marginal effects of sub-group south Asian ethnicity on EQ-5D utility scores†±. (DOCX 20 KB)
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited.
About this article
Cite this article
Jhita, T., Petrou, S., Gumber, A. et al. Ethnic differences in health related quality of life for patients with type 2 diabetes. Health Qual Life Outcomes 12, 83 (2014). https://doi.org/10.1186/1477-7525-12-83
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-12-83