Abstract
Background
Rapid diagnostic tests (RDT) are widely used for malaria diagnosis in Madagascar, where Plasmodium falciparum is the predominant species. Molecular diagnosis is essential for malaria surveillance, but requires additional blood samples for DNA extraction. Used RDTs is an attractive alternative that can be used as a source of DNA. Plasmodium falciparum genetic diversity and multiplicity of infection, usually determined by the genotyping of polymorphic regions of merozoite surface proteins 1 and 2 genes (msp1, msp2), and the repeated region RII of the glutamate-rich protein gene (glurp) have been associated with malaria transmission levels and subsequently with the impact of the deployed control strategies.
Thus, the study aims to use RDT as DNA source to detect Plasmodium species, to characterize Plasmodium falciparum genetic diversity and determine the multiplicity of infection.
Methods
A pilot study was conducted in two sites with different epidemiological patterns: Ankazomborona (low transmission area) and Matanga (high transmission area). On May 2018, used RDT (SD BIOLINE Malaria Ag P.f/Pan, 05FK63) were collected as DNA source. Plasmodium DNA was extracted by simple elution with nuclease free water. Nested-PCR were performed to confirm Plasmodium species and to analyse P. falciparum msp1, msp2 and glurp genes polymorphisms.
Results
Amongst the 170 obtained samples (N = 74 from Ankazomborona and N = 96 from Matanga), Plasmodium positivity rate was 23.5% (40/170) [95% CI 17.5–30.8%] by nested-PCR with 92.2% (37/40) positive to P. falciparum, 5% (2/40) to Plasmodium vivax and 2.5% (1/40) to P. falciparum/P. vivax mixed infection. Results showed high polymorphisms in P. falciparum msp1, msp2 and glurp genes. Multiple infection rate was 28.6% [95% CI 12.2–52.3%]. The mean of MOI was 1.79 ± 0.74.
Conclusion
This pilot study highlighted that malaria diagnosis and molecular analysis are possible by using used malaria RDT. A large-scale study needs to be conducted to assess more comprehensively malaria parasites transmission levels and provide new data for guiding the implementation of local strategies for malaria control and elimination.
Trial registration Retrospectively registered
Similar content being viewed by others
Background
Despite the deployment of considerable efforts and various strategies to control and eliminate malaria, this disease remains one of the main cause of morbidity and mortality worldwide [1]. In 2020, 241 million cases were reported leading to 627,000 deaths [2]. Sub-Saharan Africa, including Madagascar, still remains the most affected region [2]. Among the five Plasmodium species infecting humans, Plasmodium falciparum is the most prevalent malaria species in sub-Saharan Africa and the most virulent species leading severe malaria [3].
Rapid Diagnostic Tests for malaria (RDT) are commonly used for malaria diagnosis in field by community health workers to promptly manage malaria cases. Malaria molecular diagnosis are essential for epidemiological surveillance, but requires to collect additional blood samples for DNA extraction. Used RDTs is an attractive alternative that can be used as a source of DNA [4,5,6].
Plasmodium falciparum genotyping remains an important tool for studying types and numbers of parasite clones present in an infection. Currently, this approach is mainly used to investigate the genetic diversity of parasites in human infections and subsequently estimate the malaria transmission intensity [1, 7,8,9,10]. Moreover, numerous studies have demonstrated an association between high multiplicity of infection (MOI) and malaria severity, especially in high malaria transmission areas [11]. Usually, P. falciparum genetic diversity is determined by the genotyping of the polymorphic regions of the block 2 of merozoite surface protein-1 (msp1), block 3 of merozoite surface protein-2 (msp2) and the RII repeated region of the glutamic rich protein genes (glurp) [12,13,14,15].
In Madagascar, four to eight malaria ecozones are described according to their different epidemiological profile that range from low to high transmission [16, 17]. Regular molecular and epidemiological monitoring over time and space of the genetic diversity of P. falciparum populations in association with malaria phenotypes (uncomplicated malaria, severe malaria and asymptomatic malaria cases) is crucial to evaluate the impact of malaria control interventions and to guide the deployment of local tailored strategies for elimination [1, 11, 18, 19].
Hence, this study aims to valorize blood samples collected onto RDT as DNA source for detecting Plasmodium infections, assessing the genetic diversity of P. falciparum populations and estimating the MOI in P. falciparum isolates collected from symptomatic patients seen in health centres in two sites with different epidemiological patterns: Ankazomborona, located in a low transmission area and Matanga in a high transmission area.
Methods
Study sites and sample collection
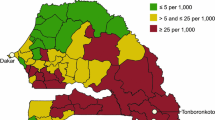
The study was conducted on May 2018 in two sites: in Ankazomborona, district region of Marovoay, located on the west coast of Madagascar (16° 07′ 00″ S and 46° 45′ 00″ E) and in Matanga, district region of Vangaindrano, located on the east coast of Madagascar (23° 31′ 00″ S and 47° 33′ 00″ E) (Fig. 1). Ankazomborona is in the tropical stratum area with a seasonal, endemic and low transmission defined as 10–50 cases per 1000 population per year. While, Matanga is in equatorial stratum area with a perennial endemic and high transmission defined as more than 100 cases per 1000 population per year [20]. Malaria prevalence by microscopy among children 6–59 months of age was 9.0 and 8.8% respectively, in the zones encompassing Ankazomborona and Matanga in 2016 [21]. Plasmodium-positive RDT (SD BIOLINE Malaria Ag P.f/Pan, 05FK63) were collected. They were obtained from children aged 6 months to 15 years suffering to uncomplicated malaria. These RDT containing blood samples were conserved at room temperature before DNA extraction.
DNA extraction
To improve the protocol aiming at extracting parasite DNA from RDT, EDTA tubes containing whole blood infected by P. falciparum and P. vivax were used. Blood smears were read to identify Plasmodium species and estimate the parasite density (parasites/µL). Blood samples were then diluted with non-infected blood to obtain aliquots containing parasitaemia ranging from 1500 to 5 parasites/µL. Four RDT were tested for each dilution. The cassettes of RDT were opened laterally and the strips were taken out and cut for DNA extraction. For each parasite densities, four different parts of the strip were used to estimate the best yield of DNA extract: (A) distal part, (B) central part, (C) proximal part and (D) all parts (Fig. 2).
Two methods of DNA extraction were applied: the Instagene Matrix© method (BioRad™), according to the manufacturer’s instructions and a simple elution method in water as previously described [4].
Plasmodium falciparum and Plasmodium vivax detection by nested-PCR
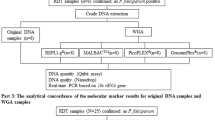
Nested-PCR [22] was performed to detect P. falciparum and P. vivax DNA and estimate which DNA extraction method and which part of RDT strip provide the more reliable results. Nested-PCR assays showed that all parts of RDT strip and simple elution method in water were the best approaches (see “Results” section). These methods were then selected for all further experiments.
Plasmodium falciparum msp1, msp2 and glurp genotyping
The polymorphic region of msp1, msp2 and glurp were genotyped using nested-PCR. Primers targeting the block 2 region of msp1, the block 3 region of msp2, and the RII repeated region of glurp were used for primary PCR (Table 1). All PCR reactions were carried out in a total volume of 25 μL, containing 200 nM dNTP mix, 2 mM MgCl2, 200 nM each of forward and reverse primers for both msp1, msp2 and glurp, 0.5 U of Taq DNA Polymerase (Bioline) and 3 μL of extracted DNA, used as template. PCR amplification of msp1, msp2 and glurp genes comprised an initial step of 94 °C for 5 min followed by 30 cycles of 94 °C for 30 s, 55 °C for 30 s, 72 °C for 1 min 30 s, and a final extension of 72 °C for 5 min.
For the nested-PCR, specific primers to allelic families of msp1 (MAD20, K1, and RO33), and msp2 (3D7 and FC27) were used. For glurp amplification, inner primers were used to amplify generated amplicons (Table 1). This secondary reaction contained the same reagents as the primary reaction except primers (Table 1) and 2 μL of the primary PCR product was used as DNA template. The cycling profile for the secondary PCR was similar to the primary PCR for glurp while for msp1 and msp2 the annealing temperature was increased from 55 to 60 °C. DNA from non-infected blood and from reference P. falciparum strains (3D7, Dd2 and 7G8) were included in each set of PCR reactions as a negative and positive controls.
Eight microlitres of nested PCR products were loaded on 2% agarose gel stained with ethidium bromide and separated by electrophoresis for an average of 60 min at 120 V. After electrophoresis, the gels were visualized under UV trans-illumination using Image Lab gel doc system and then analysed to estimate the bands sizes. PCR products size were estimated by Image Lab software using 100 bp DNA ladder marker.
Polyclonal infection was defined by the presence of more than one allele for a given gene [23, 24]. Multiplicity of infection (MOI) was defined by the number of genotypes per infection [25].
Results
Optimization of DNA extraction
Out of 16 RDT samples (8 tested with P. falciparum infected bloods and 8 by P. vivax infected bloods), DNA extracted from all parts of RDT strip and simple elution method in water gave successful results by PCR amplification (Fig. 3).
Plasmodium falciparum and Plasmodium vivax infections by nested PCR
Out of 170 samples of used RDT (74 from Ankazomborona and 96 from Matanga) analysed, nested-PCR allowed to detect 40 positives samples (23.5%, 95% CI 17.5–30.8%) of which 37 were P. falciparum (92.5%, 95% CI 78.5–98.0%), 2 P. vivax (5%, 95% CI 0.9–18.2%) and 1 P. falciparum/P. vivax mixed infection (2.5%, 95% CI 0.1–14.7%) (Table 2).
Frequency of msp1 and msp2 allelic families
Out of all 38 P. falciparum positive samples, 21 were successfully amplified for msp1 (55.3%, 95% CI 38.5–71.0%) and 9 for msp2 (23.7%, 95% CI 12.0–40.6%). For msp1, MAD20 was the most frequent allelic family and detected in 52.4% (95% CI 30.3–73.6%) of the samples, followed by RO33 (47.6%; 95% CI 26.4–69.7%) and K1 (28.6%; 95% CI 12.2–52.3%). A total of 28.6% of the positive samples for msp1 contained polyclonal infection with MAD20/K1, MAD20/R033 and K1/R033. For msp2, all positive samples (9/9) belonged to the FC27 allelic family and were classified as monoclonal infection. None of the 3D7 allelic family was detected.
Genetic diversity, allelic frequency and multiplicity of infection
Generated alleles were classified according to their fragment sizes for msp1, msp2 and glurp. Allelic frequency for an allele was defined as being its proportion compared to the total number of all detected alleles in the whole isolates. Plasmodium falciparum isolates in both sites were highly polymorphic, since almost alleles detected were once. For msp1 gene, 14 different alleles were observed: 4 alleles for MAD20 (size range 150–250 bp), 1 allele for RO33 (size range 120–150 bp) and for 6 alleles for K1 (size range 140–300 bp) (Table 3). Only one sample from Matanga presented polyclonal infection for MAD20 allelic family (MAD20-D) (Table 3).
For msp2 gene, only the FC27 allelic family was observed but the genetic diversity was high: 6 different alleles were detected among the 9 positive samples (Table 4). For glurp gene, out of the 38 P. falciparum positive samples, 20 (52.6%; 95% CI 36.0–68.7%) were successfully amplified. As for msp1 and msp2 genes, a high proportion of different alleles (N = 8) was observed (Fig. 4A, B, Table 5).
The mean value of MOI was 1.79 ± 0.74, similar in both sites (1.79 ± 0.80 in Ankazomborona and 1.79 ± 0.70 in Matanga). No significant difference in MOI was also observed between msp1 (1.33 ± 0.48), msp2 (1.0 ± 0) and glurp (1.0 ± 0) genes.
Discussion
Used RDT as source of DNA for molecular analysis
This preliminary study, focused on Plasmodium species detection and msp1, msp2 and glurp genotyping, was performed to evaluate the feasibility of using used RDT, collected from public health facilities in Madagascar, as source of DNA for molecular analysis. Previous findings revealed that used RDTs provide a valuable source of parasite DNA, which can be used for molecular analysis [4,5,6, 26, 27]. Two DNA extraction methods, Instagene Matrix© method (BioRad™) and simple water elution method, were tested in the present study. Compared methods for DNA extraction showed that simple water elution method gave higher successful result. Thus, this method was adopted in the study. One hundred seventy used RDT samples were analysed. The proportion of Plasmodium infection was 23.5% (95% CI 17.5–30.8%) including 92.2% P. falciparum positive, 5% P. vivax positive and 2.5% P. falciparum/P. vivax mixed positive samples. Although this low proportion, this study highlighted the opportunity using used RDT for malaria diagnosis and molecular analysis [4]. Furthermore, studies confirmed that they also can be useful for molecular markers surveillance and whole genome sequencing [28, 29]. The main advantage is that no other consumable, nor reagent for blood sampling are needed and RDT are widely available in public health facilities since 2008 in Madagascar [30]. Nevertheless, the lack of DNA quality and quantity analysis constitute one of the limitations for the present study. Furthermore, the parasitaemia for each samples are not available and the laboratory analysis were carried out 8 months after the collection of used RDT that were stored two months in field. Thus, the storage of used RDT in the field conditions might have likely affected the DNA integrity. DNA extraction method may should be improved for increasing the yield of parasite DNA [5]. Yet, several parameters such as parasitaemia and the impact of storage duration and conditions of used RDT on the quality of the DNA extract should be considered. Besides, in order to increase the power of the study, conducting analysis with large samples is needed.
Genetic diversity and multiplicity of Plasmodium falciparum infection
Out of 38 confirmed P. falciparum samples, 21 were successfully amplified for msp1 (55.3%, 95% CI 38.5–71.0%), 9 (23.7%, 95% CI 12.0–40.6%) for msp2 and 20 (52.6%, 95% CI 36.0–68.7%) for glurp genes. Compared to previous studies, this amplification rate was low [23, 31]. The small amount of blood deposited on RDT, 5 µL according manufacturer’s instructions [32, 33], might have affected extract DNA quantity. Moreover, targeting genes are in a single copy which could reduce amplification rate especially in low DNA concentration cases [34,35,36].
For msp1, the most frequent allelic family was MAD20 (52.4%), followed by RO33 (47.6%) and K1 (28.6%), similar to those found in Equatorial Guinea, Myanmar and Senegal [24, 37, 38], but in contrast to those observed in Congo DR and Yemen where the K1 allelic family predominate about 40 to 60% [39, 40].
Due to the low amplification rate and the limited samples, only the FC27 allelic family was detected for the msp2, concordant with data observed by Rakotomanjaka in the same locality (Matanga) in 2016 [41]. This is not the case in all localities in Madagascar, since several studies using DNA sequencing method, reported higher frequency of 3D7 allelic (up to 48%) such as in Andapa, Mahasolo and Saharevo [42, 43] [44]. Whereas, the study was carried out during the peak of malaria transmission [45].
Analysis based on the PCR product fragments showed 4 distinct alleles for MAD 20 allelic family (11 samples), 1 allele for RO33 (10 samples) and 6 alleles for K1 (6 samples). The K1 allelic family was found at low frequency (28.6%) compared to MAD20 and RO33, but this allelic family was more polymorphic (6 distinct alleles for 6 samples). For FC27 allelic family of msp2, out of the 9 positive samples, 6 distinct alleles were detected. Regarding to glurp gene, 8 distinct alleles were observed in the 20 positive samples. Polymorphism analysis showed high genetic diversity of P. falciparum populations in Ankazomborona and Matanga. Majority of alleles detected during in this study were single with a high polymorphism level. No significant difference of polymorphism level was detected in two study sites. Parasite genetic diversity is one of key elements to consider for strategies implementation to fight against malaria [40]. It has an impact on parasite transmission and control strategies, and it varies according to transmission in endemic areas [7,8,9,10]. According to the results, it seems, transmission intensity is similar in Ankazomborona and in Matanga. However, parasites transmission and genetic diversity could be higher during the peak of malaria transmission and may reflect the dynamics of parasites transmission [23, 25]. Hence, a study on large samples is crucial before giving final conclusion.
This study showed 28.6% multiple infection for P. falciparum msp1 gene not for msp2 and glurp. These results indicate that polyclonal infection frequency is low compared to those found in other countries [46, 47]. The MOI average value was 1.79 ± 0.74, a lower value than in other northwestern Ethiopia (2.6), in Republic of Congo (2.64), and in Equatorial Guinea (5.5) [25, 37, 40]. MOI for Ankazomborona and Matanga did not differ significantly. Thus, hypothesis concerning the link between the high level of MOI and malaria severity, particularly in areas with high transmission rate [11], is not verified during this study due to the limited number of samples. Despite this, the present study revealed that P. falciparum populations circulating in Madagascar showed a high level of genetic polymorphism. That high polymorphism reflects transmission intensity. Consequently, it would be interesting to increase samples number in order to continue genetic diversity study over time and space for carrying out a cartographic study about Plasmodium allelic families’ distribution in Madagascar.
Conclusion
The present study highlighted the possibility of performing malaria diagnosis and molecular genetic diversity analysis of Plasmodium using blood samples collected on RDT as DNA source. Preliminary data from this study showed high genetic diversity of P. falciparum populations in Ankazomborona and in Matanga but multiple infection rate was low in the both study sites.
This study provides fundamental information on P. falciparum genetic diversity and allow to update available data. The results of this study can be used as a baseline information for future studies on parasite transmission dynamics and to evaluate effectiveness malaria prevention and control strategies.
Availability of data and materials
The data are available from the National Malaria Control Programme of Madagascar.
References
Some AF, Bazie T, Zongo I, Yerbanga RS, Nikiema F, Neya C, et al. Plasmodium falciparum msp1 and msp2 genetic diversity and allele frequencies in parasites isolated from symptomatic malaria patients in Bobo-Dioulasso, Burkina Faso. Parasites Vectors. 2018;11:323.
WHO. World malaria report. Geneva: World Health Organization; 2021.
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
Cnops L, Boderie M, Gillet P, Van Esbroeck M, Jacobs J. Rapid diagnostic tests as a source of DNA for Plasmodium species-specific real-time PCR. Malar J. 2011;10:67.
Morris U, Aydin-Schmidt B, Shakely D, Martensson A, Jornhagen L, Ali AS, et al. Rapid diagnostic tests for molecular surveillance of Plasmodium falciparum malaria-assessment of DNA extraction methods and field applicability. Malar J. 2013;12:106.
Veron V, Carme B. Recovery and use of Plasmodium DNA from malaria rapid diagnostic tests. Am J Trop Med Hyg. 2006;74:941–3.
Auburn S, Barry AE. Dissecting malaria biology and epidemiology using population genetics and genomics. Int J Parasitol. 2017;47:77–85.
Escalante AA, Ferreira MU, Vinetz JM, Volkman SK, Cui L, Gamboa D, et al. Malaria molecular epidemiology: lessons from the international centers of excellence for malaria research network. Am J Trop Med Hyg. 2015;93:79–86.
Nabet C, Doumbo S, Jeddi F, Konate S, Manciulli T, Fofana B, et al. Genetic diversity of Plasmodium falciparum in human malaria cases in Mali. Malar J. 2016;15:353.
Nkhoma SC, Nair S, Al-Saai S, Ashley E, McGready R, Phyo AP, et al. Population genetic correlates of declining transmission in a human pathogen. Mol Ecol. 2013;22:273–85.
Mahdi Abdel Hamid M, Elamin AF, Albsheer MM, Abdalla AA, Mahgoub NS, Mustafa SO, et al. Multiplicity of infection and genetic diversity of Plasmodium falciparum isolates from patients with uncomplicated and severe malaria in Gezira State, Sudan. Parasites Vectors. 2016;9:362.
Apinjoh TO, Tata RB, Anchang-Kimbi JK, Chi HF, Fon EM, Mugri RN, et al. Plasmodium falciparum merozoite surface protein 1 block 2 gene polymorphism in field isolates along the slope of mount Cameroon: a cross-sectional study. BMC Infect Dis. 2015;15:309.
Cook J, Hergott D, Phiri W, Rivas MR, Bradley J, Segura L, et al. Trends in parasite prevalence following 13 years of malaria interventions on Bioko island, Equatorial Guinea: 2004–2016. Malar J. 2018;17:62.
Mwingira F, Nkwengulila G, Schoepflin S, Sumari D, Beck HP, Snounou G, et al. Plasmodium falciparum msp1, msp2 and glurp allele frequency and diversity in sub-Saharan Africa. Malar J. 2011;10:79.
Snounou G, Zhu X, Siripoon N, Jarra W, Thaithong S, Brown KN, et al. Biased distribution of msp1 and msp2 allelic variants in Plasmodium falciparum populations in Thailand. Trans R Soc Trop Med Hyg. 1999;93:369–74.
Howes RE, Mioramalala SA, Ramiranirina B, Franchard T, Rakotorahalahy AJ, Bisanzio D, et al. Contemporary epidemiological overview of malaria in Madagascar: operational utility of reported routine case data for malaria control planning. Malar J. 2016;15:502.
Mouchet J, Blanchy S. Particularities and stratification of malaria in Madagascar. Sante. 1995;5:386–8 (in French).
Adjah J, Fiadzoe B, Ayanful-Torgby R, Amoah LE. Seasonal variations in Plasmodium falciparum genetic diversity and multiplicity of infection in asymptomatic children living in southern Ghana. BMC Infect Dis. 2018;18:432.
Zhong D, Lo E, Wang X, Yewhalaw D, Zhou G, Atieli HE, et al. Multiplicity and molecular epidemiology of Plasmodium vivax and Plasmodium falciparum infections in East Africa. Malar J. 2018;17:185.
Programme National de lutte contre le Paludisme—PNLP/Madagascar. Plan stratégique national de lutte contre le paludisme, Madagascar, 2018–2022. Antananarivo: Ministère de la Santé Publique, Secretariat General; 2017.
Institut National de la Statistique—INSTAT/Madagascar, Programme National de lutte contre le Paludisme—PNLP/Madagascar, Institut Pasteur de Madagascar—IPM/Madagascar, ICF International: Enquête sur les Indicateurs du Paludisme. Calverton, MD, USA: INSTAT, PNLP, IPM and ICF International; 2016.
Snounou G, Viriyakosol S, Zhu XP, Jarra W, Pinheiro L, do Rosario VE, et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993;61:315–20.
Duah NO, Matrevi SA, Quashie NB, Abuaku B, Koram KA. Genetic diversity of Plasmodium falciparum isolates from uncomplicated malaria cases in Ghana over a decade. Parasites Vectors. 2016;9:416.
Soe TN, Wu Y, Tun MW, Xu X, Hu Y, Ruan Y, et al. Genetic diversity of Plasmodium falciparum populations in southeast and western Myanmar. Parasites Vectors. 2017;10:322.
Mohammed H, Kassa M, Mekete K, Assefa A, Taye G, Commons RJ. Genetic diversity of the msp-1, msp-2, and glurp genes of Plasmodium falciparum isolates in Northwest Ethiopia. Malar J. 2018;17:386.
Ishengoma DS, Lwitiho S, Madebe RA, Nyagonde N, Persson O, Vestergaard LS, et al. Using rapid diagnostic tests as source of malaria parasite DNA for molecular analyses in the era of declining malaria prevalence. Malar J. 2011;10:6.
Nabet C, Doumbo S, Jeddi F, Sagara I, Manciulli T, Tapily A, et al. Analyzing deoxyribose nucleic acid from malaria rapid diagnostic tests to study Plasmodium falciparum genetic diversity in Mali. Am J Trop Med Hyg. 2016;94:1259–65.
Nag S, Ursing J, Rodrigues A, Crespo M, Krogsgaard C, Lund O, et al. Proof of concept: used malaria rapid diagnostic tests applied for parallel sequencing for surveillance of molecular markers of anti-malarial resistance in Bissau, Guinea-Bissau during 2014–2017. Malar J. 2019;18:252.
Srisutham S, Suwannasin K, Mathema VB, Sriprawat K, Smithuis FM, Nosten F, et al. Utility of Plasmodium falciparum DNA from rapid diagnostic test kits for molecular analysis and whole genome amplification. Malar J. 2020;19:193.
PNLP. Plan stratégique national de lutte contre le paludisme à Madagascar (2013–2017). Programme National de Lutte contre le Paludisme; 2013.
Mohammed H, Assefa A, Chernet M, Wuletaw Y, Commons RJ. Genetic polymorphisms of Plasmodium falciparum isolates from Melka-Werer, North East Ethiopia based on the merozoite surface protein-2 (msp-2) gene as a molecular marker. Malar J. 2021;20:85.
WHO. Prequalification of in vitro diagnostics programme. Amended public report. Product: Bioline malaria Ag P.f/Pan. version 10.0. Geneva: World Health Organization; 2020.
SD Bioline. SD Malaria Ag P.f/Pan (05FK63). One step malaria HRP-II (P.f) and pLDH (Pan) antigen rapid test.
Hofmann N, Mwingira F, Shekalaghe S, Robinson LJ, Mueller I, Felger I. Ultra-sensitive detection of Plasmodium falciparum by amplification of multi-copy subtelomeric targets. PLoS Med. 2015;12: e1001788.
Nguyen TT, Nzigou Mombo B, Lalremruata A, Koehne E, Zoleko Manego R, Dimessa Mbadinga LB, et al. DNA recovery from archived RDTs for genetic characterization of Plasmodium falciparum in a routine setting in Lambarene. Gabon Malar J. 2019;18:336.
Oyedeji SI, Awobode HO, Monday GC, Kendjo E, Kremsner PG, Kun JF. Comparison of PCR-based detection of Plasmodium falciparum infections based on single and multicopy genes. Malar J. 2007;6:112.
Chen JT, Li J, Zha GC, Huang G, Huang ZX, Xie DD, et al. Genetic diversity and allele frequencies of Plasmodium falciparum msp1 and msp2 in parasite isolates from Bioko Island, Equatorial Guinea. Malar J. 2018;17:458.
Niang M, Thiam LG, Loucoubar C, Sow A, Sadio BD, Diallo M, et al. Spatio-temporal analysis of the genetic diversity and complexity of Plasmodium falciparum infections in Kedougou, southeastern Senegal. Parasites Vectors. 2017;10:33.
Al-abd NM, Mahdy MA, Al-Mekhlafi AM, Snounou G, Abdul-Majid NB, Al-Mekhlafi HM, et al. The suitability of P. falciparum merozoite surface proteins 1 and 2 as genetic markers for in vivo drug trials in Yemen. PLoS ONE. 2013;8: e67853.
Singana BP, Mayengue PI, Niama RF, Ndounga M. Genetic diversity of Plasmodium falciparum infection among children with uncomplicated malaria living in Pointe-Noire, Republic of Congo. Pan Afr Med J. 2019;32:183.
Rakotomanjaka T. Evaluation de l’efficacité de la combination thérapeutique à base d’artesimine ACT: cas de commune Matanga (district de Vangaindrano). Master. Université d’Antananarivo, Biochimie, Biodiversité et Santé, Faculté des Sciences; 2016.
Randimby Rajaonarisaonina F. Identification des espèces plasmodiales chez les anophèles des marges de haute terre centrale de Madagascar. Thèse. Université d’Antananarivo, Biologie, Ecologie et conservation Animale, Faculté des Sciences; 2012.
Razafiarimanga Z. Etude de polymorphisme du gène Msp2 et de microsatellites du génome de Plasmodium falciparum à Saharevo et à Andapa. Thèse. Université d’Antananarivo, Biochimie Appliquée aux Sciences Médicales, Faculté des Sciences; 2005.
Durand R, Ariey F, Cojean S, Fontanet A, Ranaivo L, Ranarivelo LA, et al. Analysis of circulating populations of Plasmodium falciparum in mild and severe malaria in two different epidemiological patterns in Madagascar. Trop Med Int Health. 2008;13:1392–9.
Nguyen M, Howes RE, Lucas TCD, Battle KE, Cameron E, Gibson HS, et al. Mapping malaria seasonality in Madagascar using health facility data. BMC Med. 2020;18:26.
Raj DK, Das BR, Dash AP, Supakar PC. Genetic diversity in the merozoite surface protein 1 gene of Plasmodium falciparum in different malaria-endemic localities. Am J Trop Med Hyg. 2004;71:285–9.
Ranjit MR, Sharma YD. Genetic polymorphism of falciparum malaria vaccine candidate antigen genes among field isolates in India. Am J Trop Med Hyg. 1999;61:103–8.
Acknowledgements
We are thankful to the technicians and medical team, from National Malaria Control Program, for their technical support. We are grateful to Didier Menard, University of Strasbourg for his precious help and advice.
Funding
This work was supported by The Global Fund.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to preparing the final version of the manuscript. VA and ER were in charge of analysis and parasite genotyping. AR is guarantor of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was part of malaria surveillance approved by the Ethics Committee of the Ministry of Health of Madagascar (No. 083/MSANP/CE/11-2012).
Consent for publication
All the authors have agreed to the submission of this manuscript for publication.
Competing interests
The authors declare that they have no other conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andrianaranjaka, V.H.I., Ravaoarisoa, E., Rakotomanga, T.A. et al. DNA recovery from used malaria RDT to detect Plasmodium species and to assess Plasmodium falciparum genetic diversity: a pilot study in Madagascar. Malar J 21, 227 (2022). https://doi.org/10.1186/s12936-022-04246-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04246-y