Abstract
Paclitaxel is commonly used to treat breast, ovarian, lung, esophageal, gastric, pancreatic cancer, and neck cancer cells. Cancer recurrence is observed in patients treated with paclitaxel due to paclitaxel resistance emergence. Resistant mechanisms are observed in cancer cells treated with paclitaxel, docetaxel, and cabazitaxel including changes in the target molecule β-tubulin of mitosis, molecular mechanisms that activate efflux drug out of the cells, and alterations in regulatory proteins of apoptosis. This review discusses new molecular mechanisms of taxane resistance, such as overexpression of genes like the multidrug resistance genes and EDIL3, ABCB1, MRP1, and TRAG-3/CSAG2 genes. Moreover, significant lncRNAs are detected in paclitaxel resistance, such as lncRNA H19 and cross-resistance between taxanes. This review contributed to discovering new treatment strategies for taxane resistance and increasing the responsiveness of cancer cells toward chemotherapeutic drugs.
Similar content being viewed by others
Introduction
The mortality rate is increased worldwide due to cancer and the resistance to chemotherapeutic drugs. The number of deaths in 2020 was 10 million, and it is expected to increase to 16 million by 2040 globally. The uncontrolled mortality rate is a result of the chemotherapeutic resistance of cancer cells [1]. Chemotherapeutic resistance occurs as a result of cancer cells becoming tolerant to different chemotherapies [2]. Resistance could be categorized into primary and secondary: primary is caused by tumor cells before therapy exposure, while secondary is attributed to tumor adaptation to the treatment, for instance, elevated expression of target proteins [3]. Cancer drug resistance is commonly attributed to genomic alterations. Moreover, resistance machinery types include EMT, signaling pathway bypass, drug efflux activation, and drug entry impairment [4,5,6,7]. During chemotherapeutic resistance, tumor size is not affected by chemotherapy and the occurrence rate of relapse is increased after the initial positive treatment [8]. Breast, ovarian, gastric, and uterine cancers become chemo-resistant after being treated with chemotherapy for a long time, especially paclitaxel.
Paclitaxel, a naturally occurring compound, is used as a potent cytotoxic drug against different cancer types, including bladder cancer, breast cancer, non-small-cell lung cancer, esophageal, gastric, pancreatic cancers, and head and neck cancer [9, 10]. β-tubulin is a target of the paclitaxel action which causes microtubule stabilization, resulting in cell cycle arrest and apoptosis [11]. In addition, taxane induces cancer cell death by activating the cleavage of procaspases and proapoptotic markers. Initially, cancer cells are susceptible to paclitaxel treatment, but paclitaxel resistance develops over time through several mechanisms. Paclitaxel resistance is observed in cancer cells that may be intrinsic, whereas resistance was acquired in other cancer cells after an initial positive response [12]. Cancer cells may activate paclitaxel resistance mechanisms such as DNA mutations, thereby altering the metabolic mechanisms that induce drug resistance and degradation. Furthermore, resistance to paclitaxel in cancer cells occurs through the activation of efflux drug proteins, modification of molecular pathways involved in apoptosis, and upregulation of paclitaxel resistance-associated gene-3 (TRAG-3/CSAG2) expression [13]. It is essential to discuss the strategies of paclitaxel resistance, which refers to cancer recurrence in patients treated with paclitaxel. In this review, I identified how paclitaxel resistance is developed through drug efflux, cell death inhibition, genetic modifications, and modifying the biological conditions of the epithelial-mesenchymal transition (EMT) in cancer cells. This review discusses new taxane resistance mechanisms and cross-resistance mechanisms to give a chance to find treatment strategies to overcome resistance and improve anticancer efficacy.
Different types of taxanes
Paclitaxel structure related to its action
Paclitaxel is a natural product extracted as a white powder from the bark of a Pacific yew tree called Taxus brevifolia. Paclitaxel is a tetracyclic diterpenoid belonging to the class of taxane drugs that is characterized by its mode of action [14]. Taxane drugs, including paclitaxel, inhibit cancer cell proliferation by targeting microtubules. Paclitaxel is employed as an antineoplastic agent for the treatment of many malignancies [15]. The paclitaxel formula is C47H51NO14, as shown in Fig. 1, with a molecular weight of 853.9 g/mol. Paclitaxel possesses a taxane ring structure, whereby a homochiral ester is located at the C13 position, and a four-membered oxetane side ring is present at the C4 and C5 positions [16]. The C13 location in the paclitaxel structure exhibits a very active side chain, namely, a homochiral ester side chain. This side chain shows a strong affinity for microtubules, thus impeding their depolymerization process [16]. As a result, it limits the development of cancer cells by causing a stop in the cell cycle phases, specifically at the G2/M phase [5, 7, 17]. Guenard and coworkers (1993) observed that both a taxane ring and an ester sidechain in the paclitaxel structure have cytotoxic effects against cancer cells [18].
Mechanism of paclitaxel action
Paclitaxel stabilizes the dynamics of microtubules, which contain cylindrical hollow structures with a diameter of about 25–30 nm. Microtubules are polymers of tubulin heterodimers, including α and β tubulins in dynamic balance [19, 20]. Microtubules are responsible for mitotic spindle formation throughout cell division and are needed for cell structure maintenance and motility of the cell with its intracellular cytoplasm. During the G2/M phase, the processes of tubulin biosynthesis and microtubule assembly take place continuously. There is a dynamic equilibrium between microtubules with their α and β subunits of tubulins arranged in a head-to-tail fashion. Under typical cellular equilibrium conditions, the net rate of tubulin assembly is equal to the net rate of tubulin breakdown, resulting in an unchanging microtubule length [21]. The microtubule contains a minus part that is anchored at the centrosome and ends that interact with cellular structures in the cytoplasm [22, 23]. Paclitaxel inhibits the assembly of microtubules and prevents cell division [24]. Additionally, it facilitates the formation of stable microtubules, specifically 𝛽-tubulin heterodimers, leading to the depolymerization of microtubules. This process prevents the progression of cells in the G2/M phase and eventually induces apoptosis, as shown in Fig. 2 [19, 25, 26]. N-terminal 31 amino acids of the β-tubulin subunit are the main target of paclitaxel interaction reversibly [25, 27]. Paclitaxel induces the formation of microtubules in vitro in the absence of GTP at 4 °C. Paclitaxel is observed to exert resistance mechanisms, including evading chemotherapeutic cytotoxicity that causes resistance and failure in chemotherapy [28].
Paclitaxel also activates various proapoptotic signaling pathways, such as the TLR-4 dependent pathway, c-Jun N-terminal kinase, P38 mitogen-activated protein (MAP) kinase, nuclear factor kappa B (NF-𝜅B), and Janus kinase- (JAK-) signal transducer and activator of transcription factor (STAT) pathway [29]. The activation of the P38 MAP kinase pathway by paclitaxel results in the phosphorylation of antiapoptotic markers, such as Bcl2, as well as the dephosphorylation of proapoptotic markers, including Bad and BAX [29]. Paclitaxel inhibits bcl2 (antiapoptotic marker) expression, which drives the expression of BAX (apoptotic marker) and mitochondrial efflux of cytochrome c, resulting in cleavage of procaspases into active caspases 3 and 9 and causes cell death, as shown in Fig. 2.
Mechanisms of paclitaxel mode of actions. (A) Paclitaxel targets 𝛽-tubulin heterodimers and stabilizes microtubule dynamics to prevent cell proliferation. (B) Paclitaxel causes microtubule depolymerization and arresting cells, especially in the G2/M phase and finally undergoing apoptosis. (C) Paclitaxel downregulates the expression level of bcl2 and drives the efflux of the mitochondrial cytochrome c resulting in caspase activation
Docetaxel
Docetaxel (DTX) is a 2nd generation of the taxanes family is extracted from the needles of yew trees. Previous studies have shown that docetaxel and its derivatives have a significant anti-cancer activity more than paclitaxel by 1.3- to 12-fold [30] against a wide range of cancers including lung, ovarian, gastric, breast, prostate, and head and neck cancers [31,32,33]. The structure of docetaxel is different from the paclitaxel structure in the 3’-position of the lateral chain and the 10-position on the taxane ring as shown in Fig. 3A. Paclitaxel and docetaxel have the same binding sites and are different in the strength of suppressive activity on microtubule dynamics. Docetaxel has a greater binding affinity towards β-tubulin [34, 35]. In addition, the retention time of docetaxel on cancer cells is longer than paclitaxel. So, the effect of docetaxel is potent twice more than paclitaxel [34]. During mitosis, docetaxel binds to β-tubulin causing the distribution of molecular microtubule dynamics resulting in the inhibition of cytoskeleton functions and arrest cancer cells at the G2/M phase as shown in Fig. 3B [36]. Furthermore, docetaxel triggers apoptosis through phosphorylation of BCL2 and activation of caspase [37, 38]. Also, it inhibits cancer cell proliferation by decreasing the trafficking activity of the ERK1/2 pathway [39].
(A) Chemical structure of docetaxel. (B) Mode of action of docetaxel; docetaxel binds to β-tubulin causing the distribution of microtubules resulting arrest of cancer cells at the G2/M phase. Furthermore, it triggers apoptosis by causing disturbance in mitochondrial dynamics and drives the release of cytochrome c and upregulating BAX levels. Docetaxel Raf-1 kinase phosphorylates Bcl-2 resulting in apoptosis
Cabazitaxel
Cabazitaxel (CBZ) is developed from docetaxel and its structure is different from docetaxel in its methyl groups at the 7- and 10-positions of the taxane ring as shown in Fig. 4 [40]. Cabazitaxel’s structure minimizes its affinity for drug efflux pumps including ATP-binding cassette and MDR1. Cabazitaxel is characterized by having a long intracellular retention time, which makes CBZ more potent than docetaxel in suppressing mitotic dynamics [41]. FDA approved cabazitaxel in 2010 as an anticancer drug. Cabazitaxel stabilizes microtubules by binding to the N-terminal amino acids of the β-tubulin subunit during mitosis. Therefore, cabazitaxel inhibits microtubule cell division and arrests the cancer cell cycle and its proliferation.
Paclitaxel resistance with its key molecular mechanisms
Paclitaxel resistance is a complicated mechanism of multiple genes and multiple steps that develop cancer cells into aggressive cancer cells, causing a high mortality rate with advanced ovarian cancer, gastric cancer, and esophageal cancer [42,43,44]. The resistance of cancer cells can be attributed to their rapid and uncontrolled growth, leading to the development of several new blood vessels. These vessels enhance irregular blood flow and stimulate increased demand for blood supply, resulting in the development of hypoxic regions in patients with ovarian cancer. Chronic hypoxia leads to modifications in the tumor microenvironment of cancer cells adapted to keep cancer cell functions, including proliferation and progression, and subsequently decreases its chemosensitivity [45]. Chronic hypoxia induces genomic instability changes within cancer cells, and influences the expression level of the tumor suppressor gene (p53), vascular endothelial growth factor (VEGF), and angiogenin to inhibit programmed cell death and reduce cell cycle arrest, resulting in the emergence of cancer cell resistance towards different chemotherapies [46].
In contrast, the development of resistance to paclitaxel is characterized by several modifications in mRNA and translation factors of protein, cellular oxidative stress, glycolysis, glutathione metabolism, and leukocyte transendothelial migrating pathways. Sherman-Baust and his coworkers (2011) observed that there is a total of 337 genes were extensively changed after treatment of resistant ovarian cancer cells with paclitaxel [47]. This alteration creates variations in drug effects, tumor microenvironment, mutations within microtubules, metabolism, and resistant tendencies toward chemotherapy among patients [47]. Moreover, several challenges reduce chemotherapeutic efficacy and enhance developing cancer cell resistance toward paclitaxel, including ABC transporter, P-glycoprotein, MDR-associated protein (MRP1), and breast cancer resistance protein (BCRP), as shown in Fig. 5. All these alterations inhibit cancer cell death, enhance the difficulty of treating metastasis, and avoid cancer cell targeting from chemotherapeutic drugs.
Multidrug resistance (MDR)
Chemotherapeutic resistance or multidrug resistance (MDR) is related to the relapse of cancer cell responsiveness to many anticancer drugs and their mechanisms of action [48]. Paclitaxel develops cancer cell resistance through the upregulation of the MDR gene, which enables cancer cells to overcome chemotherapeutic drugs [49]. MDR exerts an external mechanism to modify the pharmacokinetics of chemotherapeutic drugs, modifying tumor microenvironment and causing changes within cancer cells. Ingrained or intrinsic MDR develops chemotherapeutic resistance by altering the cancer cell microenvironment. Acquired MDR occurs after exposure to chemotherapeutic drugs by modifying its pharmacokinetics or causing alterations within the cancer cells. Moreover, the MDR1 gene translates ATP-binding cassette (ABC) transporters, including P-glycoprotein (P-gp), which functions as an efflux pump that enables cancer cells to deliver the needed substrates through cellular membranes [50]. Drug efflux is a crucial strategy that is responsible for paclitaxel chemoresistance. The other drug-resistant mechanisms include inhibition of drug penetration, modifications in drug targets, and alteration in the prodrug-activation mechanism.
The ATP-binding cassette (ABC) transporters are implicated in the development of resistance to paclitaxel
The surface of resistant cancer cells is characterized by high expression of ABC transporter proteins. These transporters need energy to display their functions. ABC transporters are divided into three functional classes, including importers, exporters pump, and transporter-type proteins involved in DNA repair processes [51]. ABC importers are responsible for the uptake of biomolecules into the cell, whereas exporters are responsible for taking toxins and chemotherapeutic drugs out of the cancer cells. There are 7 ABC genes (ABCA–ABCG) that are divided and undergo their sequence homology and domain organization. ABC transporter proteins contain two domains, including the trans-membrane domain (TMD) and nucleotide-binding domain (NBD) [52]. The TMD in the ABC transporter identifies a large variability of substrates and causes conformational changes to drive passage biomolecules via the membranes in the presence of ATP. The structure and sequence of TMDs are variable, whereas the sequence structure of NBD is fixed and found in the cytoplasm where ATP-binding occurs. Ovarian and breast cancer overexpress ABCB1 and ABCC10 on their surface to pump paclitaxel out of the cancer cell and develop chemotherapeutic resistance for paclitaxel [53]. ABCB1 and ABCC10 are phosphor-glycoproteins encoded by MDR1 gene to decrease the therapeutic index of paclitaxel.
Paclitaxel resistance associated with P-glycoprotein (PGP)
P-glycoprotein (PGP) is a multidrug efflux pump that consists of 14 targeting binding sites, including 12 TMDs and two ATP-binding sites. PGP is a multidrug transporter that is translated from the ABCB1 gene [54]. In normal healthy cells, PGP regulates the rate of the uptake of biomolecules, absorption, and efflux of foreign substances. Additionally, paclitaxel, daunorubicin, vincristine, doxorubicin, and vinblastine are transported through PGP by extracting the drug from the cytoplasmic side of the lipid bilayer directly [55]. The drug transfer through phospholipids from the inner to outer regions of the bilayer in PGP is facilitated by a unidirectional lipid flippase. The glycoprotein transporter known as PGP modulates the rate of drug penetration into cancer cells. There is an apparent relationship between the levels of PGP expression and the level of the emergence of chemotherapeutic resistance [55]. Breast cancer cells induce the PGP expression that actively pumps paclitaxel out of the cell in the presence of ATP against their concentration levels. This efflux induces breast cancer resistance and decreases its efficacy.
Paclitaxel resistance associated with breast cancer resistance protein (BCRP)
The BCRP expression level is related to the presence of anticancer drugs, including paclitaxel, anthracyclines, camptothecins, and mitoxantrone, which induce the emergence of drug resistance [56]. BCRP consists of two binding domains, including the TMD and NBD [56]. The functioning homodimer of BCRP results from the bonding of two BCRP molecules with a disulfide bridge [57]. BCRP is expressed in normal cells of the gut, placenta, and bile canaliculi to eliminate toxins and xenobiotics from the cells [58]. BCRP enables normal cells to survive under hypoxia by keeping homeostasis levels of heme and folate [58]. Conversely, cancer cells upregulate the expression level of BCRP during hypoxic conditions and acquire chemotherapeutic resistance. Natarajan and coworkers (2012) observed that prostate cancer cell line 22RV1 is resistant to paclitaxel, methotrexate, and doxorubicin due to high BCRP and ABCG2 expression levels [58].
Paclitaxel-resistance-associated gene-3 (TRAG-3/CSAG2) expression
Paclitaxel resistance in ovarian cancer is associated with the overexpression of gene 3 (TRAG-3) [59]. Previous studies demonstrated that normal cells have very low expression levels of this gene compared with ovarian cancer cells. The TRAG-3 gene is located in the Xq28 region of the chromosome, specifically within a cluster associated with the MAGE (melanoma antigen) family of tumor antigens. This gene cluster comprises two coding exons [59]. TRAG-3 cDNA sequence contains an open reading frame of 333 bp that is translated as a protein product of 110 amino acids. TRAG-3 gene does not drive paclitaxel-resistant phenotype directly, but it is a significant part of the multidrug-resistant mechanism of paclitaxel. Several types of cancer cells induce high expression levels of TRAG-3, including lung, breast, and melanoma cancer cells, which are related to paclitaxel resistance. Materna and his coworkers (2007) stated that paclitaxel treatment triggers the TRAG-3 expression level in ovarian cancer [59]. Moreover, Duan and his coworkers (1999) reported that TRAG-3 overexpression is observed in breast cancer cells resistant to paclitaxel, such as the MDA 435TR cell line, prostate, and myeloid carcinoma [60]. The relationship between the TRAG-3 gene and the overexpression of the MDR1 gene in cells with paclitaxel resistance was also investigated. After isolating the TRAG-3 gene from resistant cells that overexpress the MDR1 gene, it is observed that the MDR1 gene expression is not related to paclitaxel resistance and that it does not drive paclitaxel toward resistance directly [61]. There is another gene called lipoprotein receptor-related protein (LRP), which is related to paclitaxel resistance and does not drive resistance [62]. The emergence of a drug-resistant phenotype needs coordination of the expressions of different individual genes to be sufficient to generate the phenotype. It is important to conduct several investigations to elucidate the TRAG-3 role in tumorigenesis and drug resistance. In conclusion, it is considered a significant factor in the prognosis of paclitaxel resistance in ovarian carcinoma.
Epithelial-mesenchymal transition-related EDIL3 gene and paclitaxel resistance
Cancer cells trigger metastasis, migration, and invasion by losing the protein adherent junctions between cancer cells to obtain a mesenchymal phenotype through the EMT process [63]. This process depends on integrin, TGF-β, and Wnt/β-catenin pathways. In addition, the Snail family contains SNAI1, SNAI2/Slug, and Twist members which could monitor the EMT process. The expression level of E-cadherin is inhibited by SNAI1, hence impacting the maintenance of the physical structure of cell junctions and the recruitment of cellular signaling pathways. Conversely, paclitaxel resistance is strongly related to the induction of EMT and the high expression levels of EMT-related genes, such as the EDIL3 gene in breast cancer cells [64]. EDIL3 gene encodes the extracellular matrix protein, which is a new regulator of EMT in tumor progression, adhesion, and migration [65, 66]. The expression of the EDIL3 gene is associated with an increase in the expression of EGF-like repeats and discoidin I-like domains protein 3. The protein under consideration is an extracellular matrix (ECM) developmental protein with three EGF-like domains, including the RGD motif (Arg–Gly–Asp). This motif plays a crucial role in facilitating the protein’s interaction with integrins. Several research studies observed that the EDIL3 expression level increased in different tumors characterized by poor prognosis, such as liver, bladder, pancreas, and bladder cancer [66]. The high expression level of EDIL3 induces the expression levels of ERK and TGF-β after its interaction with the integrin αVβ3. Integrin αVβ3 induces brain metastasis in breast cancer patients. According to [67, 68], paclitaxel resistance is strongly associated with high expression levels of EDIL3. Knockdown of EDIL3 by targeting the RGD motif induces the responsiveness of breast cancer and prostate cancer cells toward paclitaxel. In conclusion, EDIL3 is a significant key regulator in paclitaxel resistance and EMT via autocrine or paracrine signaling in cancer cells.
Cytochrome P450-related paclitaxel resistance
Metabolizing enzymes including Cytochrome P450 (CYP) enzymes contribute to paclitaxel metabolism such as CYP3A4 and CYP2C8 [69]. It is observed that invasive cancer cells have high levels of cytochrome P450 which induce cancer cell pathogenesis. There is a strong relationship between high expression levels of cytochrome p450 expression and the paclitaxel drug resistance. Increasing the level of paclitaxel metabolism limits the efficacy of paclitaxel by decreasing intracellular drug concentrations and developing drug resistance in cancer cells. Paclitaxel metabolism by cytochrome 450 increases its metabolites which have a low cytotoxic effect on cancer cells [70]. There are some challenges related to the activity of CYP enzymes to inhibit paclitaxel metabolism. Inhibition of the activity of CYP enzymes leads to inactivating the metabolism of other drugs which may cause critical drug–drug interactions. Cancer cells activate the cytochrome P450 and decrease paclitaxel cytotoxicity resulting in the development of paclitaxel resistance.
Modulation of p53 related to paclitaxel resistance
Paclitaxel triggers cancer cell death via programmed cell death through a group of proto-oncogenes and tumor suppressor genes. Metzinger and co-workers (2006), observed ovarian cancer cell resistance with high levels of mutant p53 after the cells treated with paclitaxel or cisplatin. Interestingly, the modification in the steps of the regulation mechanism of apoptosis leads to the emergence of chemotherapeutic resistance. One of the tumor suppressor genes of apoptosis is the p53 gene which is included in some forms of apoptosis. Loss in the activity function of the p53 gene through missense mutation, deletion, and protein stabilizing enhances the development of chemotherapeutic resistance in cancer cells. The mutated p53 gene is called the TP53 gene which encodes mutated p53 protein. In addition, mutations in TP53 occur in all coding exons essentially including exons 4–9 which illustrate the DNA binding domain. This mutation not only diminishes p53 function but also enhances the acquisition of oncogenic characteristics. The new function of mutated p53 is promoting cancer cell metastasis, migration, and invasion. In addition, mutant TP53 enhances EMT and metastasis in cancer cells. Mutant p53 enhances cancer cell motility and invasion which require fibronectin-binding a5ß1 integrin to increase metastasis in H1299 cells. Also, mutant p53 increases the expression levels of integrin’s N-glycosylation patterns which enhances the interaction between cancer cells with the extracellular matrix. As a result of N-glycosylation, increasing the number of folding of membrane proteins in the endoplasmic reticulum as well as inducing metastasis.
Modulation of metabolic enzyme expression related to paclitaxel resistance
Although paclitaxel has a significant role in the treatment of hormonal-resistant breast and prostate cancers, it loses its efficacy on cancer cells gradually and cancer cells become resistant to this chemotherapeutic drug [71]. Aoyama and co-workers (2017) declared that the cell membrane sphingolipids including sphingosine 1 phosphate (S1P), and ceramide have a significant role in the emergence of paclitaxel resistance [72]. Unbalance of the levels of ceramide and S1P induces the emergence of sphingolipid rheostat which leads to paclitaxel resistance. S1P is produced from sphingosine via sphingosine kinases (SPK1/2). Previous research studies observed that high expression levels of SPK1 and S1P trigger cancer cells tumorigenesis, survival, metastasis, migration, and invasion. In addition, overexpression of SPK1 induces chemotherapeutic resistance in leukemia and solid cancers. Not only the SPK1 enzyme but also the sphingomyelinase enzyme drives increasing the production of the levels of ceramide and apoptosis. Aoyama and co-workers (2017) observed that prostate cancer resistant to paclitaxel overexpress SPK1, and S1P as well as downregulating the expression level of ASMase [72]. Increasing the levels of SPK-1 enhances the expression levels of paclitaxel reflux out of the cell through ABC transporters and induces paclitaxel resistance. Knockdown of the expression level of SPK1 using siRNA decreases the levels of S1P in cancer cells resulting in inhibition of cancer cell proliferation and decreasing paclitaxel resistance [73]. Other inhibitors including PDMP and PPMP increase the level of ceramide in cancer cells resulting in cancer cell death and apoptosis in resistant prostate cancer [72]. In conclusion, decreasing metabolic enzyme SPK1/S1P levels can modulate the responsiveness of cancer cells towards paclitaxel.
Long noncoding RNAs (lncRNAs) related to paclitaxel resistance
lncRNA H19
Long noncoding RNAs (lncRNAs) regulate multiple resistance strategies. There are significant lncRNAs detected in paclitaxel resistance, such as lncRNA H19. High levels of lncRNA H19 drive the downregulation of the level of proapoptotic genes BIK to prevent cancer cell death and develop paclitaxel resistance [74]. High lncRNA H19 levels are observed in the triple-negative breast cancer cells resistant to paclitaxel. Han and coworkers (2018) observed that the downregulation of the lncRNA H19 expression levels increases the chemosensitivity of cancer cells and activates the Akt/phosphoAkt signaling pathway, resulting in cancer cell death [75].
MA-linc1
There is a novel regulator of lncRNA called MA-linc1, decreasing the expression level of neighboring gene Pur α. The expression level of Pur α prevents cancer cell proliferation. Knockdown of the Pur α gene inhibits the activity of MA-linc1, resulting in inducing cancer cell sensitivity toward paclitaxel. Low level of survival rates of breast cancer patients is associated with a high level of MA-linc1 [76]. Bida and his coworkers (2015) observed that low MA-linc1 levels induce the sensitivity of cancer cells toward paclitaxel and overcome paclitaxel resistance [77]. Moreover, the lncRNAs HIF1A-AS2 and AK124454 induce proliferation, invasion, and paclitaxel resistance of MDA-MB-231 and TNBC cancer [78, 79].
Linc-ROR
There is another new regulator of EMT called long intergenic noncoding RNA (Linc-ROR), which drives chemoresistance via miRNA interactions and TGF- β2 signaling [79,80,81]. The high expression level of Linc-ROR downregulates the expression level of E-cadherin and develops paclitaxel resistance in MDA-MB-231 cells [82].
FTH1P3
There is another regulator of paclitaxel resistance called ferritin heavy chain 1 pseudogene 3 (FTH1P3). A high expression level of FTH1P3, which is resistant to paclitaxel, is observed in MCF-7 and MDA-MB-231 cells. The high expression level of FTH1P3 promotes the expression of drug transporter P-gp transporter, which drives the reflux of paclitaxel out of the cell and develops paclitaxel resistance. Furthermore, FTH1P3 targets miR-206, which is related to high levels of ABCB1 and develops paclitaxel resistance [83].
NONHSAT141924
NONHSAT141924 is another long noncoding RNA that pertains to paclitaxel resistance. High expression levels of NONHSAT141924 have a significant role in upregulating the expression levels of Bcl-2, which leads to paclitaxel resistance [84].
Key genes associated with taxanes resistance
Treatment of cancer cells with paclitaxel for a long time leads to paclitaxel resistance. Shen and his coworkers (2021) identified the key genes related to paclitaxel resistance through LASSO analysis in esophageal squamous cell carcinoma (ESCC) [85]. There are nine specific key genes driving paclitaxel resistance in cancer cells, including microfibril-associated protein 2 (MFAP2), membrane metalloendopeptidase (MME), inhibin subunit beta A (INHBA), claudin 1 (CLDN1), putative homeodomain transcription factor 2 (PHTF2), tetraspanin 9 (TSPAN9), MLLT11 transcription factor 7 cofactor (MLLT11), chemokine (C-C motif) ligand 26 (CCL26), and glycosyltransferases (KDELC1) gene (Fig. 6) [85].
MFAP2, MFAP5 gene
MFAP2 is one of the genes linked to paclitaxel resistance, which is located at 1p36.13 and consists of 10 exons [86]. MFAP2 is a biomarker of ECM that enhances B16 melanoma cancer cell motility and invasion in vitro and in vivo research studies [87]. [88] used clinical samples to predict the association between MFAP5 and the survival of ovarian cancer patients. The high expression level of MFAP5 (microfibrillar-associated protein 5) induces the ovarian cancer resistance of paclitaxel and cisplatin [88]. [89] observed that MFAP5 silencing in nude mice injected with luciferase labeled OVCA432 cells induces normalization of tumor vessels and improves the paclitaxel sensitivity.
MME gene
Conversely, a low expression level of MME induces cancer cell resistance in prostate cancer [90]. MME is located at 3q21-27 and consists of 24 exons [91]. MME normally binds to phosphatase and tensin homolog deleted on chromosome 10 (PTEN), resulting in suppression of oncogenesis. Cancer cell resistance of paclitaxel is characterized by low levels of both MME and PTEN, driving vascular invasion and metastasis [90].
INHBA gene
The INHBA gene is another gene observed in cancer cells resistant to paclitaxel [92]. INHBA gene is located at 2q35 and consists of two exons. Dysregulation of the INHBA gene induces metastasis and keeps mesenchymal phenotypes in cancer cells [93]. Chen and his coworkers (2019) observed that the INHBA gene induces the TGF-β signaling pathway, promoting cancer cell motility, invasion, migration, and consequently cancer cell resistance [94].
ITGA2 gene
Ma and his coworkers [95] observed that high expression levels of the ITGA2 gene, which encodes integrin subunit α2, induce proliferation, metastasis, and the emergence of taxanes resistance in vitro. High expression of the ITGA2 gene promotes the phosphorylation of forkhead box O1 (FoxO1) by facilitating the phosphorylation of AKT in taxane-resistant cells [95, 96].
CLDN1 gene
Moreover, the CLDN1 gene is another paclitaxel-resistant gene observed in cancer cells at a high level. CLDN1 gene is located at 3q28 and consists of four exons, which are expressed as membrane proteins responsible for tight junctions’ formation and monitor the transport of transendothelial, cell growth, and differentiation in normal cells [97]. Cancer cells contain dysregulated levels of CLDN-1, which trigger cancer cell invasion, aggressiveness, and resistance. Zhao and his co-workers [98] observed that high expression levels of CLDN1 induce migration, invasion, and cisplatin resistance of NSCLC. High levels of CLDN1 promote autophagy via increasing the expression levels of ULK1 phosphorylation and induce the emergence of cisplatin resistance in NSCLC [98]. CLDN-1 is also involved in Wnt and Notch signaling, which has a significant role in the tumorigenesis, and resistance of cancer cells toward chemotherapeutic drugs [99].
PHTF2 gene
Furthermore, the PHTF2 is a gene related to paclitaxel resistance in cancer cells, according to [85]. PHTF2 is a gene located at 7q11.23 with 21 exons, which is observed to have a significant role in inducing tumorigenesis of gastric cancer cells by regulating fatty acid metabolism [100].
CCL26 gene
One of the genes related to paclitaxel resistance is CCL26, which is located at 7q11.23 with five exons [85]. In addition, the CCL26 expression level is overexpressed in human osteosarcoma cells (MG63). CCL26 enhances the invasiveness, proliferation, metastasis, and resistance in MG63 [101].
CCL2 gene
Natsagdorj and his coworkers [102] observed in vitro that cabazitaxel-resistant cell lines express high levels of CCL2, which induce invasion, migration, and chemoresistance in prostate cancer cells. CCL2 induces not only the activator of transcription 3 (STAT3) but also AKT in prostate cell line. It is observed that there is a strong association between CCL2 and MDR1. Activation of STAT3 upregulates the expression level of MDR1 and induces the emergence of paclitaxel and cabazitaxel resistance in prostate cancer cells [102, 103].
TSPAN9 gene
TSPAN9 is another specific gene related to paclitaxel resistance located at 12p13.33-p13.32 with 15 exons. The TSPAN9 overexpression induces drug resistance in gastric cancer by downregulating the expression levels of PI3K proteins-related autophagy [104].
MAGE/GAGE gene
Transfection of MAGE/GAGE gene into sensitive cancer cells drive the emergence of paclitaxel resistance in ovarian cancer cell line by 4-fold increase [105]. Acquisition of paclitaxel resistance related with increased expression of a variety of proteins and both neighboring and non-neighboring cancer antigens genes.
MLLT11 gene
MLLT11 is also a specific gene-related paclitaxel resistance located at 1q21.3 with 2 exons. The MLLT11 overexpression induces tumorigenesis, development, and resistance in endometrial cancer by targeting the Akt protein and consequently inhibiting the PI3K/AKT/mTOR signaling pathway [106].
KDELC1 gene
KDELC1 is one of the paclitaxel-resistant genes, which is located at 13q33.1 with 11 exons. Overexpression of KDELC1 induces dysregulation of immune cell infiltration and driving Notch-related signaling [107]. High levels of KDELC1 trigger cancer cell motility, invasion, progression, and consequently resistance [107]. Lueong and his coworkers [108] observed that after analysis of 10 patients who have a poor response to systemic chemotherapy that they have high expression levels of KDELC1. KDELC1 activates many inflammatory pathways that are strongly associated with the pro-inflammatory microenvironment and result in the aggressiveness of PDAC tumors [108].Finally, it is important to study the genes related to taxane resistance to restore drug sensitivity and produce significant therapeutic strategies.
Molecular mechanisms related to docetaxel resistance
Alterations of microtubules
Docetaxel targets microtubule alterations including structural and functional [109]. Mutations of genes related to β- tubulin [110], high expression levels of βIII-tubulin [111], and alterations in the functional proteins associated with microtubules can modify the dynamics of microtubules and alter the capability of docetaxel binding [112]. Therefore, cancer cells become less sensitive to the toxicity of docetaxel and drive the emergence of docetaxel resistance.
Upregulation of drug efflux transporter-related docetaxel resistance
[113,114,115] observed that docetaxel upregulates the expression levels of ATP-binding cassette transporters including ABCC1, and ABCC4 in prostate cancer. ATP-binding cassette transporters efflux docetaxel out of the cancer cell and drive the emergence of docetaxel resistance. These transporters are characterized by drug specificity and included in chemoresistance causing drug failure to target cancer cells [109, 116]. Prostate cancer cells treated with docetaxel after a period express ABCB1, which is associated with TaxR genes automatically. ABCB1 knockdown induces the responsiveness of docetaxel-resistant cancer cells toward drug invitro [114]. Zhu and his co-workers [114] observed that the natural product apigenin inhibits the expression levels of ABCB1 and restores the sensitivity of docetaxel-resistant prostate cancer cells in vitro.
Antioxidant activation
The toxicity of the taxane family is associated with the production of reactive oxygen species (ROS) inside cancer cells which leads to the activation of apoptosis [117, 118]. Taxane triggers variations in the mitochondrial membrane that induce the release of cytochrome C which activates ROS production and cleavage of procaspases into caspases and cancer cell death [119]. Then, cancer cells induce an antioxidant response that drives taxane resistance [117, 120]. High expression levels of antioxidant enzymes have been associated with docetaxel resistance. Furthermore, high expression levels of BIM-1 activate antioxidant response and minimize ROS production and cancer cell death in cells treated with docetaxel [117]. Therefore, it is observed that high levels of BIM-1 are associated with poor prognosis in prostate cancer and increased docetaxel resistance [117]. Interestingly, ROS production and antioxidant response activate pro-survival mechanisms and drive the emergence of docetaxel resistance. Also, a high expression level of superoxide dismutase 2 impairs the degradation of the arrestin-1-related insulin-like growth factor-I receptor (IGF-1R) which is associated with the reduction of ROS [121]. IGF-1 signaling has an obvious role in cancer proliferation and drug resistance [122].
Cancer stem cells related to docetaxel resistance
Stemness properties of cancer cells enable cancer cells to be self-renewable and are related to drug resistance. The niche around cancer stem cells provides maintenance properties to cancer cells that enable them to resist chemotherapy [123, 124]. These maintenance properties include high survival capacity, high telomerase activity, upregulation of the expression levels of drug efflux transporters, EMT induction, and low levels of ROS production [124]. Lai and his co-workers [125] observed that resistant prostate cancer cells are characterized by the presence of CD44+ and/or CD133+ which make cells resistant to docetaxel toxicity. The high levels of CD44+ induce the HIPPO-YAP signaling pathway which induces metastasis, migration, and invasion and in turn chemotherapeutic resistance [125]. Furthermore, it is observed that prostate cancer stem cells which are resistant to docetaxel, are characterized by the presence of CD44+ and CD133+ and stemness-related genes [126]. The amount of ABCB1 transporters expressed in resistant cells depends on the activity of MDA-9, which is linked to the activity of the STAT3 and NOTCH/cMYC signaling pathways. The knockdown of STAT3 is a significant strategy to overcome docetaxel resistance in vitro [127, 128].
SLCO genes and drug influx
Another promising taxane resistance mechanism is SLCO genes, which are responsible for reducing taxane concentration inside cancer cells and emergence resistance. It is observed that patients with castrate-resistant prostate cancer (CRPC) have low sensitivity towards taxanes associated with single nucleotide polymorphisms (SNPs) and a loss of activity in the solute carrier of organic anions (SLCO) genes [129,130,131]. Slco1b2 Knockdown in mice is strongly associated with the high level of docetaxel in plasma which is not metabolized. SLCO proteins are important for transporting docetaxel into cells, and loss could lead to reduced intracellular docetaxel concentrations. [132] observed that impairment of docetaxel influx is related to the genetic variations of SLCO genes in vivo. From this point, there is no adoption to consider that the genetic polymorphism and expression levels are considered potential indicators for cellular taxane uptake or the emergence of resistance. Other studies observed that docetaxel resistance has emerged in prostate cell lines due to low expression levels of SLCO1B3 [133]. The overexpression of SLCO1B3 genes improves the sensitivity of prostate cell lines towards taxane [133]. The SLCO genes are related to the expression levels of efflux pumps on the cancer cell surface. These surface pumps drive the efflux of docetaxel out of the cell before its cytotoxic action [134]. de Morrée and his co-workers [135] observed that the influx and efflux pumps induce the emergence of docetaxel resistance in resistant patient-derived xenograft models of CRPC. It is important to focus on SLCO genes related to the influx pumps to overcome taxane resistance.
Androgen receptor signaling
The androgen receptor is considered a ligand-dependent nuclear transcription factor that induces genes responsible for prostate cancer proliferation and differentiation [136, 137]. Androgen receptors are localized to the nucleus through metallothioneins [138]. Metallothioneins are proteins rich in cysteine which are responsible for mitotic spindle synthesis, metal homeostasis, and cellular protection that emerges from DNA damage and oxidative stress. In a normal cell, androgens signalling occurs after attachment to the androgen receptor, and metallothionein aid in its localization to the nucleus [139]. Taxanes stabilize metallothionein, resulting in the inhibition of androgen signalling. absence of androgen receptor localization is observed in the cells derived from docetaxel-treated CRPC patients. As a result, metallothionein is deduced to bind androgen receptors directly and the emergence of taxane resistance [140, 141]. It is observed that there is an inverse relationship between the amount of nuclear localization of the androgen receptor and the responsiveness of cells towards taxane. From this context, it is observed that the rate of sequestration of androgen receptors is related to the rate of the bundling of metallothionein which improves taxanes response [142]. Antonarakis and his co-workers [143] observed that there is a strong relationship between docetaxel resistance and androgen receptor signalling mechanisms. Once the androgen receptor is localized to the nucleus, Lysine-specific demethylase 5D (KDM5D) regulates the transcription of the androgen receptor. Knockdown of the KDM5D enzyme induces the signalling of androgen receptor and emergence of docetaxel resistance in cancer cells [144]. On the other hand, adding enzalutamide to taxane treatment decreases the effect of androgen receptor signalling on resistance. Enzalutamide as an anti-androgen inhibitor which block androgen receptor signalling. In conclusion, it is important to target androgen receptor signalling pathway as a new target to overcome taxane resistance.
Epithelial-to-mesenchymal transition phenotype
The Epithelial-to-mesenchymal transition (EMT) phenotype has a crucial role in promoting cancer cell resistance and metastasis [145, 146]. EMT develops taxane resistance in castration-resistant prostate cancer CRPC cells. The low expression level of E-cadherin (an indicator of EMT) is observed in both untreated and docetaxel prostate cancer cells [147]. In addition, high expression levels of CD44 populations, vimentin, and zinc-finger e-box binding homeobox 1 (ZEB1) are observed in docetaxel-resistant CRPC cell lines [148]. [149, 150] observed that the knockdown of ZEB1 and decreased CD44 populations can induce the responsiveness of cancer cells towards docetaxel [150]. In addition, a high expression level of macrophage inhibitory cytokine 1 (MIC-1) is associated with EMT and docetaxel resistance [151]. MIC-1 is a member of the TGFβ family which targets decreased taxane resistance in vitro and in vivo [152]. Martin and his co-workers [153] observed that the treatment using the combination of both cabazitaxel and enzalutamide reversed EMT and decreased resistance. Targeting the EMT mediators is a promising strategy to overcome taxan resistance.
PI3K/Akt Pathway
PI3K/Akt pathway is also another mechanism that induces survival in cancer cells by increasing the expression levels of activating kinases or downregulating the expression levels of the inhibitory regulators. Recent studies have observed that taxane resistance in prostate cancer is associated with irregular expression levels of PI3K/Akt [154,155,156]. [157, 158] observed that high expression levels of AKT and inhibition of phosphatase and tensin homologue deleted on chromosome 10 (PTEN) in PI3K induce chemoresistance of docetaxel in castration-resistant prostate cancer CRPC. So, it is observed that using the dietary flavonoid quercetin improves the sensitivity of resistant cells toward docetaxel by inducing apoptosis by decreasing the expression levels of phosphorylated Akt [159]. Furthermore, low PTEN expression levels are strongly associated with paclitaxel resistance. To overcome paclitaxel resistance and So, overexpression of PTEN induces the responsiveness of resistant cancer cells toward paclitaxel in vitro [158]. Docetaxel induces cancer resistance by increasing the activity of phosphorylated Akt depending on the dose of docetaxel. LY294002 is an inhibitor of PI3K/Akt signalling resulting in an improvement in the sensitivity of resistant cells to docetaxel and triggering apoptosis. Furthermore, NVP-BEZ235 targets the mammalian target of rapamycin (mTOR) results decreasing the expression levels of phosphorylated Akt, inducing cancer cell death invitro and inhibiting cancer cell proliferation in vivo [160]. As a result, NVP-BEZ235 is considered the most significant drug for inhibiting PI3K/Akt signaling and overcoming taxane resistance. In conclusion, targeting of PI3K/Akt pathway is the most significant mechanism to overcome taxane resistance.
miRNAs-related taxane resistance
MicroRNAs are considered endogenous non-coding RNAs with a short length of 19–24 nucleotides that regulate tumorigenesis [161, 162]. It binds to 3′-UTR of mRNA and reduces gene expression. In prostate cancer cells, miRNAs regulate cancer cell proliferation such as miR-1273 g-3p, miR-34a-5p, miR-148, and miR-34a as shown in Fig. 7. It is observed that overexpression of CD133 is displayed on the surface of the paclitaxel-resistant cells. CD133 induces the Akt/mTOR/c-Myc axis and the development of paclitaxel resistance [163]. MiR-1273 g-3p induces poor prognosis in prostate cancer cells by triggering cancer cell proliferation and metastasis [164]. It is observed that miR-34a has a low level in cancer cells resistant to paclitaxel. In normal cells, miR-34a targets the NOTCH signaling pathway that involves the BCL-2 family, but its downregulation induces paclitaxel resistance in cancer cells in vitro [165]. MiR-34a-5p induces cancer cell proliferation and triggers paclitaxel resistance in prostate cancer by inducing the expression levels of Human sirtuin1 (SIRT1) and suppressing TP53 expression [166]. In addition, overexpression of miR-135b induces paclitaxel resistance and aggressiveness of NSCLC by directly targeting the 3′-untranslated region (UTR) of the deubiquitinase CYLD, thereby modulating ubiquitination and activation of NF-κB signaling. Interleukin-6 (IL-6)/STAT3 could bind to the promoter of miR-135b results elevating its level of expression [167]. Also, high levels of miR-155 induce paclitaxel resistance in vitro. MiR-155 overexpression induces exosome secretion acquires epithelial-mesenchymal transition characteristics and promotes a high rate of migration and metastasis in breast cancer [168]. lncRNA CCAT1 has an oncogenic role by inhibiting the expression of miR-24–3p which minimizes the level of fascin actin-bundling protein 1 (FSCN1) that induces the paclitaxel resistance [169].
On the other hand, microRNAs could improve the sensitivity of cancer cells towards drugs. MiR-148 for example is used to improve the responsiveness of resistant cells towards paclitaxel [170, 171]. MiR-200 restores docetaxel sensitivity by increasing E-cadherin and ZEB1 expressions which induce apoptosis in prostate cancer [116, 147]. In addition, low expression level of miR-199a has a tumor suppressor role in prostate cancer. MiR-199a inhibits the expression level of YES1 (YES Proto-Oncogene 1) to overcome paclitaxel resistance [172]. In conclusion, microRNA expression levels are considered as chemotherapeutic targets to overcome paclitaxel resistance.
Molecular mechanisms related to cabazitaxel resistance
Despite cabazitaxel’s potent cytotoxicity which is more than both paclitaxel and docetaxel, there is a substantial cross-resistance remaining. Taxanes, including cabazitaxel, activate efflux transporters such as ABCB1/P-gp [173,174,175,176]. It is observed that cabazitaxel is the most active taxane drug in expressing efflux transporters, including ABCB1, but not ABCC2, ABCC10, or ABCG2. Furthermore, any alterations in microtubule dynamics and composition have been observed in taxane drugs [166, 177, 178]. It was also observed that non-ABCB1 taxane resistance is associated with high expression levels of the β-tubulin isotype (TUBB4) in leukemia [179]. The cabazitaxel-resistant ovarian and breast cancer cells express high expression levels of the content of class III (TUBB3) in the presence of a P-gp inhibitor (PSC-833). Upregulation of TUBB3 enables MCF-7/ CTAX-P to acquire mesenchymal properties which are associated with cabazitaxel resistance [180,181,182]. It was also confirmed by [183,184,185] who observed that cabazitaxel resistance is a result of high expression levels of class III β-tubulin. [186,187,188] used siRNAs to inhibit TUBB3 expression to restore taxanes sensitivity. In addition, [189] observed that the knockdown of TUBB3 restores the sensitivity of the MCF-7/CTAX-P cell line towards cabazitaxel.
Other studies reported that knockdown of BRCA1 expression is one of the significant causes of cabazitaxel resistance in breast, lung, and ovarian cancer cell lines [190,191,192]. Both BRCA1 and BRCA2 are genes that express proteins responsible for repairing damaged DNA. Furthermore, BRCA1 is observed to control microtubule dynamics and binding of cabazitaxel to microtubules, impairing its effect as a stabilizer of microtubules and inducing the emergence of cabazitaxel resistance in A549 lung cancer [193]. Silencing of the BRCA1 expression increases the cabazitaxel resistance by 4-fold in MCF-7 cells [194]. Targeting of EMT, level of BRCA1, and high level of class III β-tubulin are significant strategies to overcome cabazitaxel resistance.
Cross-resistance between taxanes
Cross-resistance is considered as acquired resistance that is defined as a reaction to chemotherapy and results in resistance to other drugs. Cross-resistance may depend on the genetic profile of the patient [195]. The risk of cross-resistance emerges after sequential treatment of two chemotherapy have the same mode of action and results that the second drug might lose its efficacy [196]. The cross-resistance may be observed between paclitaxel and docetaxel or between docetaxel and cabazitaxel.
Cross-resistance between paclitaxel and docetaxel
There are large cross-resistance is observed after using paclitaxel and docetaxel as a combination to treat metastatic gastric cancer [197]. Asić and his co-workers [3] observed among 484 patients with metastatic gastric cancer who received both paclitaxel and docetaxel as a combination therapy that the 2nd taxane achieved a response rate of 5% and an overall disease control rate of 17.9%. These results demonstrate a large degree of cross-resistance between paclitaxel and docetaxel [197]. So, after the failure of treatment by other types of taxane in gastric cancer, both paclitaxel and docetaxel should not be routinely administered for metastatic gastric cancer [197]. Also, Valero and his coworkers [198] evaluated the efficacy of docetaxel in patients who suffered from paclitaxel-resistant breast cancer (MBC). They observed that 7 patients from a total of 44 patients had partial responses and 1 patient responded completely with severe adverse effects. It is observed that docetaxel has a higher potency than paclitaxel in promoting phosphorylation of bcl-2, which results in high efficiency in inducing apoptotic cell death. Paclitaxel resistance mechanisms involving microtubule binding resistance may still be sensitive to docetaxel if the bcl-2 phosphorylation mechanism remains sensitive to docetaxel [198, 199]. If the bcl-2 phosphorylation is not sensitive to docetaxel this means microtubule binding resistance and the emergence of cross-resistance. Docetaxel induces the production of interferon-α and tumor necrosis factor-α (TNF-α) which downregulate cell death in paclitaxel-resistant cancer cells [200]. It is observed that FOXO3a in glycolysis increases the expression levels of P-glycoprotein/ABCB1 which drives docetaxel cross-resistance. Knockdown of FOXO3a expression levels impairs glycolytic shift-induced apoptosis. Targeting of FOXO3a in glycolysis restores the sensitivity of the docetaxel-cross-resistant paclitaxel-resistant cancer cell line and triggers apoptosis [200]. Lin and his co-workers [201] demonstrated that there is a partial cross-resistance between paclitaxel and docetaxel. They observed that docetaxel has a modest activity in breast cancer patients (25%) pre-treated with paclitaxel [201].
Cross-resistance between docetaxel and cabazitaxel
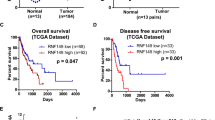
Chen and his co-workers [202] used cabazitaxel to treat docetaxel-resistant prostate cancer. It is observed that cabazitaxel has a potent cytotoxic effect on HCC cell lines by arresting the cancer cell cycle in the G2/M phase and inducing apoptosis in vitro and in vivo. Cabazitaxel also has very low cross-resistant in P-gp-overexpressed HCC cells by 1.53 resistance fold compared to paclitaxel and docetaxel [202]. Lombard and his coworkers [203] declared that the docetaxel resistance induces cross-resistance to cabazitaxel. It is observed that high expression levels of ABCB1 in docetaxel-resistant prostate cancer cells are the main cause of cross-resistance to cabazitaxel [203]. ABCB1 inhibitors involving antiandrogen can resensitize taxane-resistant cells to both docetaxel and cabazitaxel. Liu and his colleagues [204] observed that the kinesin-3 superfamily (KIF14) associated with cross-resistance between docetaxel and cabazitaxel by inhibiting microtubule depolymerization. The knockdown of the expression levels of KIF14 drives decreasing the expression levels of AKT and induces the sensitivity of resistant cells towards taxanes [204]. Wang and his coworkers [205] observed that inhibition of the nuclear receptor ROR drives downregulating the expression levels of MDR1 expression. Furthermore, its inhibition restores the sensitivity of cross-resistant cells towards DTX and CBZ. Machioka and his coworkers [206] observed that inhibition of MDR1 restores the sensitivity of cross-resistant cells to DTX/CBZ. Cross-resistance between taxanes is a significant clinical issue that needs more research studies to understand and deal with it.
Conclusion
The administration of chemotherapy, specifically paclitaxel and its derivatives, are employed as a therapeutic approach for eradicating malignant neoplastic cells. The compounds demonstrate an anticancer mechanism through its interaction with β-tubulin, resulting in the stabilization of microtubules. This stabilization subsequently leads to the arrest of the cancer cell cycle, specifically in the G2/M phase. Following an extended period of administration of paclitaxel and its derivatives, cancer cells develop a resistance to chemotherapy. This review explores the recently discovered mechanisms of taxanes resistance in cancer cells. Furthermore, it provides a comprehensive list of genes associated with resistance to taxanes. miRNAs list related to taxane resistance and cross-resistance mechanisms between taxanes.
Data availability
No datasets were generated or analysed during the current study.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Observatory:Cancer Today. Lyon Int Agency Res Cancer 2020.
Sharifi-Rad J, Quispe C, Patra JK, Singh YD, Panda MK, Das G, Adetunji CO, Michael OS, Sytar O, Polito L. Paclitaxel: application in modern oncology and nanomedicine-based cancer therapy. Oxid Med Cell Longev, 2021.
Asić K. Dominant mechanisms of primary resistance differ from dominant mechanisms of secondary resistance to targeted therapies. Crit Rev Oncol Hematol. 2016;97:178–96.
Alkafaas SS, Obeid OK, Radwan MA, Elsalahaty MI, ElKaffas SS, Hafez W, Janković N, Hessien M. Novel insight into mitochondrial dynamin-related protein-1 as a new chemo-sensitizing target in resistant cancer cells. Bioorg Chem 2024;150:107574.
Diab T, Alkafaas SS, Shalaby TI, Hessien M. Paclitaxel nanoparticles induce apoptosis and regulate txr1, cyp3a4 and cyp2c8 in breast cancer and hepatoma cells. Anti-Cancer Agents Med Chem (Formerly Curr Med Chemistry-Anti-Cancer Agents). 2020;20(13):1582–91.
Alkafaas SS, Loutfy SA, Diab T, Hessien M. Vasopressin induces apoptosis but does not enhance the antiproliferative effect of dynamin 2 or PI3K/Akt inhibition in luminal A breast cancer cells. Med Oncol. 2022;40(1):35.
Alkafaas SS, Diab T, Shalaby T, Hessien M, dexamethasone improves the responsiveness of hepatoma cells for both free and solvent containing paclitaxel in vitro. Egypt J Biochem Mol Biology 2019, 37.
Alkafaas SS, Elsalahaty MI, Ismail DF, Radwan MA, Elkafas SS, Loutfy SA, Elshazli RM, Baazaoui N, Ahmed AE, Hafez W. The emerging roles of sphingosine 1-phosphate and SphK1 in cancer resistance: a promising therapeutic target. Cancer Cell Int. 2024;24(1):89.
Hassan MS, Awasthi N, Ponna S, von Holzen U. Nab-Paclitaxel in the treatment of gastrointestinal cancers—improvements in clinical efficacy and safety. Biomedicines. 2023;11(7):2000.
Nawara HM, Afify SM, Hassan G, Zahra MH, Seno A, Seno M. Paclitaxel-based chemotherapy targeting cancer stem cells from mono-to combination therapy. Biomedicines. 2021;9(5):500.
Alqahtani FY, Aleanizy FS, El Tahir E, Alkahtani HM. AlQuadeib BT: Paclitaxel. Profiles Drug Subst Excip Relat Methodol. 2019;44:205–38.
Kutuk O, Letai A. Alteration of the mitochondrial apoptotic pathway is key to acquired paclitaxel resistance and can be reversed by ABT-737. Cancer Res. 2008;68(19):7985–94.
Alatise KL, Gardner S, Alexander-Bryant A. Mechanisms of Drug Resistance in Ovarian Cancer and Associated Gene targets. Cancers. 2022;14(24):6246.
Joshee N, Dhekney SA, Parajuli P. Medicinal plants: Springer; 2019.
Ojima I, Lichtenthal B, Lee S, Wang C, Wang X. Taxane anticancer agents: a patent perspective. Expert Opin Ther Pat. 2016;26(1):1–20.
Kampan NC, Madondo MT, McNally OM, Quinn M, Plebanski M. Paclitaxel and its evolving role in the management of ovarian cancer. BioMed research international, 2015.
Diab T, AlKafaas SS, Shalaby TI, Hessien M. Dexamethasone simulates the anticancer effect of nano-formulated paclitaxel in breast cancer cells. Bioorg Chem. 2020;99:103792.
Guenard D, Gueritte-Voegelein F, Dubois J, Potier P. Structure-activity relationships of Taxol and Taxotere analogues. J Natl Cancer Inst Monogr. 1993;15:79–82.
Rowinsky EK, Donehower RC. Paclitaxel (taxol). N Engl J Med. 1995;332(15):1004–14.
Parness J, Horwitz SB. Taxol binds to polymerized tubulin in vitro. J Cell Biol. 1981;91(2):479–87.
Ganguly A, Yang H, Cabral F. Paclitaxel-dependent cell lines reveal a novel drug activity. Mol Cancer Ther. 2010;9(11):2914–23.
Dammermann A, Desai A, Oegema K. The minus end in sight. Curr Biol. 2003;13(15):R614–24.
Wiese C, Zheng Y. Microtubule nucleation: γ-tubulin and beyond. J Cell Sci. 2006;119(20):4143–53.
Schiff PB, Fant J, Horwitz SB. Promotion of microtubule assembly in vitro by taxol. Nature. 1979;277(5698):665–7.
Zhang D, Yang R, Wang S, Dong Z. Paclitaxel: new uses for an old drug. Drug Des Devel Ther 2014:279–84.
Schiff PB, Horwitz SB. Taxol stabilizes microtubules in mouse fibroblast cells. Proceedings of the National Academy of Sciences 1980, 77(3):1561–1565.
Rao S, Orr GA, Chaudhary AG, Kingston DG, Horwitz SB. Characterization of the taxol binding site on the Microtubule: 2-(m-AZIDOBENZOYL) TAXOL PHOTOLABELS a PEPTIDE (AMINO ACIDS 217–231) of β-TUBULIN (∗). J Biol Chem. 1995;270(35):20235–8.
Lim PT, Goh BH, Lee W-L. 3 - Taxol: Mechanisms of action against cancer, an update with current research. In: Paclitaxel Edited by Swamy MK, Pullaiah T, Chen Z-S: Academic Press; 2022: 47–71.
Horwitz S. Taxol (paclitaxel): mechanisms of action. Annals Oncology: Official J Eur Soc Med Oncol. 1994;5:S3–6.
Ringel I, Horwitz SB. Studies with RP 56976 (taxotere): a semisynthetic analogue of taxol. JNCI: J Natl Cancer Inst. 1991;83(4):288–91.
Crown J, O’Leary M. The taxanes: an update. Lancet. 2000;355(9210):1176–8.
Figgitt DP, Wiseman LR. Docetaxel: an update of its use in advanced breast cancer. Drugs. 2000;59:621–51.
Kaye S, Group SGCT. The integration of docetaxel into first-line chemotherapy for ovarian cancer. Int J Gynecol Cancer. 2001;11:31–3.
Gligorov J, Lotz JP. Preclinical pharmacology of the taxanes: implications of the differences. Oncologist. 2004;9(S2):3–8.
Fromes Y, Gounon P, Veitia R, Bissery M, Fellous A. Influence of microtubule-associated proteins on the differential effects of paclitaxel and docetaxel. J Protein Chem. 1996;15:377–88.
Jordan MA, Wilson L. Microtubules as a target for anticancer drugs. Nat Rev Cancer. 2004;4(4):253–65.
Kramer G, Schwarz S, Hägg M, Havelka AM, Linder S. Docetaxel induces apoptosis in hormone refractory prostate carcinomas during multiple treatment cycles. Br J Cancer. 2006;94(11):1592–8.
Fabbri F, Amadori D, Carloni S, Brigliadori G, Tesei A, Ulivi P, Rosetti M, Vannini I, Arienti C, Zoli W. Mitotic catastrophe and apoptosis induced by docetaxel in hormone-refractory prostate cancer cells. J Cell Physiol. 2008;217(2):494–501.
Mang J, Merkle K, Heller M, Schüler J, Tolstov Y, Li J, Hohenfellner M, Duensing S. Molecular complexity of taxane-induced cytotoxicity in prostate cancer cells. Urologic oncology: seminars and original investigations: 2017. Elsevier; 2017. 32. e39-32. e16.
Bachet J-B, Chibaudel B, Bonnetain F, Validire P, Hammel P, André T, Louvet C. group G: A randomized phase II study of weekly nab-paclitaxel plus gemcitabine or simplified LV5FU2 as first-line therapy in patients with metastatic pancreatic cancer: the AFUGEM GERCOR trial. BMC cancer 2015, 15:1–11.
Azarenko O, Smiyun G, Mah J, Wilson L, Jordan MA. Antiproliferative mechanism of action of the novel taxane cabazitaxel as compared with the parent compound docetaxel in MCF7 breast cancer cells. Mol Cancer Ther. 2014;13(8):2092–103.
Wang X, Zhang H, Chen X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2019;2(2):141.
Asnaashari S, Amjad E, Sokouti B. Synergistic effects of flavonoids and paclitaxel in cancer treatment: a systematic review. Cancer Cell Int. 2023;23(1):211.
Shen Y, Yang L, Li L. Cancer stem-like cells contribute to paclitaxel resistance in esophageal squamous cell carcinoma. Int J Clin Exp Pathol. 2022;15(4):183–90.
Emami Nejad A, Najafgholian S, Rostami A, Sistani A, Shojaeifar S, Esparvarinha M, Nedaeinia R, Haghjooy Javanmard S, Taherian M, Ahmadlou M, et al. The role of hypoxia in the tumor microenvironment and development of cancer stem cell: a novel approach to developing treatment. Cancer Cell Int. 2021;21(1):62.
Tang M, Bolderson E, O’Byrne KJ, Richard DJ. Tumor Hypoxia drives genomic instability. Front Cell Dev Biol. 2021;9:626229.
Sherman-Baust CA, Becker KG, Wood Iii WH, Zhang Y, Morin PJ. Gene expression and pathway analysis of ovarian cancer cells selected for resistance to cisplatin, paclitaxel, or doxorubicin. J Ovarian Res. 2011;4(1):21.
Zhang X, Yashiro M, Qiu H, Nishii T, Matsuzaki T, Hirakawa K. Establishment and characterization of multidrug-resistant gastric cancer cell lines. Anticancer Res. 2010;30(3):915–21.
Perez EA. Impact, mechanisms, and novel chemotherapy strategies for overcoming resistance to anthracyclines and taxanes in metastatic breast cancer. Breast Cancer Res Treat. 2009;114:195–201.
Gottesman MM, Pastan IH. The role of multidrug resistance efflux pumps in cancer: revisiting a JNCI publication exploring expression of the MDR1 (P-glycoprotein) gene. J Natl Cancer Inst. 2015;107(9):djv222.
Rees DC, Johnson E, Lewinson O. ABC transporters: the power to change. Nat Rev Mol Cell Biol. 2009;10(3):218–27.
Gallo JM, Li S, Guo P, Reed K, Ma J. The effect of P-glycoprotein on paclitaxel brain and brain tumor distribution in mice. Cancer Res. 2003;63(16):5114–7.
Waghray D, Zhang Q. Inhibit or evade multidrug resistance P-glycoprotein in cancer treatment: Miniperspective. J Med Chem. 2017;61(12):5108–21.
Samodelov SL, Kullak-Ublick GA, Gai Z, Visentin M. Organic Cation Transporters in Human Physiology, Pharmacology, and Toxicology. Int J Mol Sci 2020, 21(21).
Whitlock BD, Leslie EM. Efflux transporters in anti-cancer drug resistance: Molecular and functional identification and characterization of multidrug resistance proteins (MRPs/ABCCs). Drug Efflux pumps in Cancer Resistance pathways: from Molecular Recognition and characterization to possible inhibition strategies in Chemotherapy. Elsevier; 2020. pp. 31–65.
Wind N, Holen I. Multidrug resistance in breast cancer: from in vitro models to clinical studies. International journal of breast cancer, 2011.
Ni Z, Bikadi Z, Rosenberg F, Mao M. Structure and function of the human breast cancer resistance protein (BCRP/ABCG2). Curr Drug Metab. 2010;11(7):603–17.
Natarajan K, Xie Y, Baer MR, Ross DD. Role of breast cancer resistance protein (BCRP/ABCG2) in cancer drug resistance. Biochem Pharmacol. 2012;83(8):1084–103.
Materna V, Surowiak P, Kaplenko I, Spaczyński M, Duan Z, Zabel M, Dietel M, Lage H. Taxol-resistance-associated gene-3 (TRAG-3/CSAG2) expression is predictive for clinical outcome in ovarian carcinoma patients. Virchows Arch. 2007;450:187–94.
Duan Z, Feller AJ, Toh HC, Makastorsis T, Seiden MV. TRAG-3, a novel gene, isolated from a taxol-resistant ovarian carcinoma cell line. Gene. 1999;229(1–2):75–81.
Yao X, Hu J-F, Li T, Yang Y, Sun Z, Ulaner GA, Vu TH, Hoffman AR. Epigenetic regulation of the taxol resistance–associated gene TRAG-3 in human tumors. Cancer Genet Cytogenet. 2004;151(1):1–13.
Scheffer GL, Wijngaard PL, Flens MJ, Izquierdo MA, Slovak ML, Pinedo HM, Meijer CJ, Clevers HC, Scheper RJ. The drug resistance-related protein LRP is the human major vault protein. Nat Med. 1995;1(6):578–82.
Wang Y, Zhou BP. Epithelial-mesenchymal transition in breast cancer progression and metastasis. Chin J cancer. 2011;30(9):603.
Casalino L, Talotta F, Matino I, Verde P. FRA-1 as a Regulator of EMT and metastasis in breast Cancer. Int J Mol Sci. 2023;24(9):8307.
Loh CY, Chai JY, Tang TF, Wong WF, Sethi G, Shanmugam MK, Chong PP, Looi CY. The E-Cadherin and N-Cadherin Switch in Epithelial-to-Mesenchymal Transition: Signaling, Therapeutic Implications, and Challenges. Cells 2019, 8(10).
Zhang L, Peng KW, Wang B, Yang XF, Zhang ZM. EDIL3 regulates gastric cancer cell migration, invasion and epithelial-mesenchymal transition via TGF-β1/XIST/miR-137 feedback loop. Transl Cancer Res. 2020;9(10):6313–30.
Xia H, Chen J, Shi M, Gao H, Sekar K, Seshachalam VP, Ooi LL, Hui KM. EDIL3 is a novel regulator of epithelial-mesenchymal transition controlling early recurrence of hepatocellular carcinoma. J Hepatol. 2015;63(4):863–73.
Gasca J, Flores ML, Jiménez-Guerrero R, Sáez ME, Barragán I, Ruíz-Borrego M, Tortolero M, Romero F, Sáez C, Japón MA. EDIL3 promotes epithelial-mesenchymal transition and paclitaxel resistance through its interaction with integrin α(V)β(3) in cancer cells. Cell Death Discov. 2020;6:86.
van Eijk M, Boosman RJ, Schinkel AH, Huitema AD, Beijnen JH. Cytochrome P450 3A4, 3A5, and 2C8 expression in breast, prostate, lung, endometrial, and ovarian tumors: relevance for resistance to taxanes. Cancer Chemother Pharmacol. 2019;84:487–99.
Kamel A, Harriman S. Inhibition of cytochrome P450 enzymes and biochemical aspects of mechanism-based inactivation (MBI). Drug Discovery Today: Technol. 2013;10(1):e177–89.
Obasaju C, Hudes GR. Paclitaxel and docetaxel in prostate cancer. Hematology/Oncology Clin. 2001;15(3):525–45.
Aoyama Y, Sobue S, Mizutani N, Inoue C, Kawamoto Y, Nishizawa Y, Ichihara M, Kyogashima M, Suzuki M, Nozawa Y. Modulation of the sphingolipid rheostat is involved in paclitaxel resistance of the human prostate cancer cell line PC3-PR. Biochem Biophys Res Commun. 2017;486(2):551–7.
Shida D, Takabe K, Kapitonov D, Milstien S, Spiegel S. Targeting SphK1 as a new strategy against cancer. Curr Drug Targets. 2008;9(8):662–73.
Zhang X, Luo M, Zhang J, Guo B, Singh S, Lin X, Xiong H, Ju S, Wang L, Zhou Y, et al. The role of lncRNA H19 in tumorigenesis and drug resistance of human cancers. Front Genet. 2022;13:1005522.
Han J, Han B, Wu X, Hao J, Dong X, Shen Q, Pang H. Knockdown of lncRNA H19 restores chemo-sensitivity in paclitaxel-resistant triple-negative breast cancer through triggering apoptosis and regulating akt signaling pathway. Toxicol Appl Pharmcol. 2018;359:55–61.
Campos-Parra AD, López-Urrutia E, Orozco Moreno LT, López-Camarillo C, Meza-Menchaca T, Figueroa González G, Bustamante Montes LP, Pérez-Plasencia C. Long non-coding RNAs as new master regulators of resistance to systemic treatments in breast cancer. Int J Mol Sci. 2018;19(9):2711.
Bida O, Gidoni M, Ideses D, Efroni S, Ginsberg D. A novel mitosis-associated lncRNA, MA-linc1, is required for cell cycle progression and sensitizes cancer cells to Paclitaxel. Oncotarget. 2015;6(29):27880.
Jiang Y-Z, Liu Y-R, Xu X-E, Jin X, Hu X, Yu K-D, Shao Z-M. Transcriptome analysis of triple-negative breast cancer reveals an integrated mRNA-lncRNA signature with predictive and prognostic value. Cancer Res. 2016;76(8):2105–14.
Huang P, Li F, Li L, You Y, Luo S, Dong Z, Gao Q, Wu S, Brünner N, Stenvang J. lncRNA profile study reveals the mRNAs and lncRNAs associated with docetaxel resistance in breast cancer cells. Sci Rep. 2018;8(1):17970.
Yousefi H, Maheronnaghsh M, Molaei F, Mashouri L, Reza Aref A, Momeny M, Alahari SK. Long noncoding RNAs and exosomal lncRNAs: classification, and mechanisms in breast cancer metastasis and drug resistance. Oncogene. 2020;39(5):953–74.
Hou P, Zhao Y, Li Z, Yao R, Ma M, Gao Y, Zhao L, Zhang Y, Huang B, Lu J. LincRNA-ROR induces epithelial-to-mesenchymal transition and contributes to breast cancer tumorigenesis and metastasis. Cell Death Dis. 2014;5(6):e1287–1287.
Chen Y-M, Liu Y, Wei H-Y, Lv K-Z, Fu P. Linc-ROR induces epithelial-mesenchymal transition and contributes to drug resistance and invasion of breast cancer cells. Tumor Biology. 2016;37:10861–70.
Wang R, Zhang T, Yang Z, Jiang C, Seng J. Long non-coding RNA FTH 1P3 activates paclitaxel resistance in breast cancer through miR‐206/ABCB 1. J Cell Mol Med. 2018;22(9):4068–75.
Gu M, Zheng W, Zhang M, Dong X, Zhao Y, Wang S, Jiang H, Zheng X. LncRNA NONHSAT141924 promotes paclitaxel chemotherapy resistance through p-CREB/Bcl-2 apoptosis signaling pathway in breast cancer. J Cancer. 2020;11(12):3645.
Shen Z, Chen M, Luo F, Xu H, Zhang P, Lin J, Kang M. Identification of key genes and pathways associated with paclitaxel resistance in esophageal squamous cell carcinoma based on bioinformatics analysis. Front Genet. 2021;12:671639.
Xu W, Wang M, Bai Y, Chen Y, Ma X, Yang Z, Zhao L, Li Y. The role of microfibrillar-associated protein 2 in cancer. Front Oncol. 2022;12:1002036.
Chen Z, Lv Y, Cao D, Li X, Li Y. Microfibril-Associated protein 2 (MFAP2) Potentiates Invasion and Migration of Melanoma by EMT and Wnt/β-Catenin pathway. Med Sci Monit. 2020;26:e923808.
Kujawa KA, Zembala-Nożynska E, Syrkis JP, Cortez AJ, Kupryjańczyk J, Lisowska KM. Microfibril associated protein 5 (MFAP5) is related to survival of ovarian cancer patients but not useful as a prognostic biomarker. Int J Mol Sci. 2022;23(24):15994.
Yeung T-L, Leung CS, Yip K-P, Sheng J, Vien L, Bover LC, Birrer MJ, Wong ST, Mok SC. Anticancer immunotherapy by MFAP5 blockade inhibits fibrosis and enhances chemosensitivity in ovarian and pancreatic cancer. Clin Cancer Res. 2019;25(21):6417–28.
Cheng C-Y, Zhou Z, Stone M, Lu B, Flesken-Nikitin A, Nanus DM, Nikitin AY. Membrane metalloendopeptidase suppresses prostate carcinogenesis by attenuating effects of gastrin-releasing peptide on stem/progenitor cells. Oncogenesis. 2020;9(3):38.
Ding J, Li C, Shu K, Chen W, Cai C, Zhang X, Zhang W. Membrane metalloendopeptidase (MME) is positively correlated with systemic lupus erythematosus and may inhibit the occurrence of breast cancer. PLoS ONE. 2023;18(8):e0289960.
Xueqin T, Jinhong M, Yuping H. Inhibin subunit beta a promotes cell proliferation and metastasis of breast cancer through Wnt/β-catenin signaling pathway. Bioengineered. 2021;12(2):11567–75.
Wamsley JJ, Kumar M, Allison DF, Clift SH, Holzknecht CM, Szymura SJ, Hoang SA, Xu X, Moskaluk CA, Jones DR. Activin upregulation by NF-κB is required to maintain mesenchymal features of Cancer stem–like cells in non–small cell lung Cancer. Cancer Res. 2015;75(2):426–35.
Chen ZL, Qin L, Peng XB, Hu Y, Liu B. INHBA gene silencing inhibits gastric cancer cell migration and invasion by impeding activation of the TGF-β signaling pathway. J Cell Physiol. 2019;234(10):18065–74.
Ma L, Sun Y, Li D, Li H, Jin X, Ren D. Overexpressed ITGA2 contributes to paclitaxel resistance by ovarian cancer cells through the activation of the AKT/FoxO1 pathway. Aging. 2020;12(6):5336.
Peng Y, Dong S, Yang Z, Song Y, Ding J, Hou D, Wang L, Zhang Z, Li N, Wang H. Identification of docetaxel-related biomarkers for prostate cancer. Andrologia. 2021;53(7):e14079.
Bhat AA, Syed N, Therachiyil L, Nisar S, Hashem S, Macha MA, Yadav SK, Krishnankutty R, Muralitharan S, Al-Naemi H. Claudin-1, a double-edged sword in cancer. Int J Mol Sci. 2020;21(2):569.
Zhao Z, Li J, Jiang Y, Xu W, Li X, Jing W. CLDN1 increases drug resistance of non-small cell lung cancer by activating autophagy via up-regulation of ULK1 phosphorylation. Med Sci Monitor: Int Med J Experimental Clin Res. 2017;23:2906.
Kumar V, Vashishta M, Kong L, Wu X, Lu JJ, Guha C, Dwarakanath B. The role of notch, hedgehog, and wnt signaling pathways in the resistance of tumors to anticancer therapies. Front cell Dev Biology. 2021;9:650772.
Chi Y, Wang H, Wang F, Ding M. PHTF2 regulates lipids metabolism in gastric cancer. Aging. 2020;12(8):6600.
Kawano M, Iwasaki T, Itonaga I, Kubota Y, Tanaka K, Tsumura H. Analysis of the signal cross talk via CCL26 in the tumor microenvironment in osteosarcoma. Sci Rep. 2021;11(1):18099.
Natsagdorj A, Izumi K, Hiratsuka K, Machioka K, Iwamoto H, Naito R, Makino T, Kadomoto S, Shigehara K, Kadono Y. CCL2 induces resistance to the antiproliferative effect of cabazitaxel in prostate cancer cells. Cancer Sci. 2019;110(1):279–88.
Xi J, Yun M, Lee D, Park M-N, Kim E-O, Sohn EJ, Kwon B-M. Cinnamaldehyde derivative (CB-PIC) sensitizes chemo-resistant cancer cells to drug-induced apoptosis via suppression of MDR1 and its upstream STAT3 and AKT signalling. Cell Physiol Biochem. 2015;35(5):1821–30.
Qi Y, Qi W, Liu S, Sun L, Ding A, Yu G, Li H, Wang Y, Qiu W, Lv J. TSPAN9 suppresses the chemosensitivity of gastric cancer to 5-fluorouracil by promoting autophagy. Cancer Cell Int. 2020;20:1–11.
Duan Z, Duan Y, Lamendola DE, Yusuf RZ, Naeem R, Penson RT, Seiden MV. Overexpression of MAGE/GAGE genes in paclitaxel/doxorubicin-resistant human cancer cell lines. Clin Cancer Res. 2003;9(7):2778–85.
Liao J, Chen H, Qi M, Wang J, Wang M. MLLT11-TRIL complex promotes the progression of endometrial cancer through PI3K/AKT/mTOR signaling pathway. Cancer Biol Ther. 2022;23(1):211–24.
Xu X, Xie G, Xie M, Liu Q. A comprehensive role evaluation and mechanism exploration of POGLUT2 in pan-cancer. Front Oncol. 2022;12:962540.
Lueong S, Metzenmacher M, Trajkovic-Arsic M, Cheung PF, Reißig TM, von Neuhoff N, Gallinger S, Ramotar S, Dodd A, Knox JJ. Minimally invasive determination of PDAC subtype and therapy-induced subtype switch by means of circulating cell-free RNA. 2024.
Galletti G, Leach BI, Lam L, Tagawa ST. Mechanisms of resistance to systemic therapy in metastatic castration-resistant prostate cancer. Cancer Treat Rev. 2017;57:16–27.
Hara T, Ushio K, Nishiwaki M, Kouno J, Araki H, Hikichi Y, Hattori M, Imai Y, Yamaoka M. A mutation in β-tubulin and a sustained dependence on androgen receptor signalling in a newly established docetaxel‐resistant prostate cancer cell line. Cell Biol Int. 2010;34(2):177–84.
Ploussard G, Terry S, Maillé P, Allory Y, Sirab N, Kheuang L, Soyeux P, Nicolaiew N, Coppolani E, Paule B. Class III β-tubulin expression predicts prostate tumor aggressiveness and patient response to docetaxel-based chemotherapy. Cancer Res. 2010;70(22):9253–64.
Yang J, Yu Y, Liu W, Li Z, Wei Z, Jiang R. Microtubule-associated protein tau is associated with the resistance to docetaxel in prostate cancer cell lines. Res Rep Urol 2017:71–7.
Oprea-Lager DE, Bijnsdorp IV, Van Moorselaar RJ, Van den Eertwegh AJ, Hoekstra OS, Geldof AA. ABCC4 decreases docetaxel and not cabazitaxel efficacy in prostate cancer cells in vitro. Anticancer Res. 2013;33(2):387–91.
Zhu Y, Liu C, Nadiminty N, Lou W, Tummala R, Evans CP, Gao AC. Inhibition of ABCB1 expression overcomes acquired docetaxel resistance in prostate cancer. Mol Cancer Ther. 2013;12(9):1829–36.
Liu C, Li Z, Bi L, Li K, Zhou B, Xu C, Huang J, Xu K. NOTCH1 signaling promotes chemoresistance via regulating ABCC1 expression in prostate cancer stem cells. Mol Cell Biochem. 2014;393:265–70.
Giacinti S, Poti G, Roberto M, Macrini S, Bassanelli M, Di Pietro F, Aschelter AM, Ceribelli A, Ruggeri EM, Marchetti P. Molecular basis of drug resistance and insights for new treatment approaches in mCRPC. Anticancer Res. 2018;38(11):6029–39.
Crea F, Duhagon Serrat MA, Hurt EM, Thomas SB, Danesi R, Farrar WL. BMI1 silencing enhances docetaxel activity and impairs antioxidant response in prostate cancer. Int J Cancer. 2011;128(8):1946–54.
Rabi T, Bishayee A. d-Limonene sensitizes docetaxel-induced cytotoxicity in human prostate cancer cells: generation of reactive oxygen species and induction of apoptosis. J Carcinog 2009, 8.
Varbiro G, Veres B, Gallyas F Jr, Sumegi B. Direct effect of Taxol on free radical formation and mitochondrial permeability transition. Free Radic Biol Med. 2001;31(4):548–58.
Datta S, Choudhury D, Das A, Das Mukherjee D, Das N, Roy SS, Chakrabarti G. Paclitaxel resistance development is associated with biphasic changes in reactive oxygen species, mitochondrial membrane potential and autophagy with elevated energy production capacity in lung cancer cells: a chronological study. Tumor Biology. 2017;39(2):1010428317694314.
Zhang D, Cui Y, Niu L, Xu X, Tian K, Young CY, Lou H, Yuan H. Regulation of SOD2 and β-arrestin1 by interleukin-6 contributes to the increase of IGF-1R expression in docetaxel resistant prostate cancer cells. Eur J Cell Biol. 2014;93(7):289–98.
Tang Y, Parmakhtiar B, Simoneau AR, Xie J, Fruehauf J, Lilly M, Zi X. Lycopene enhances docetaxel’s effect in castration-resistant prostate cancer associated with insulin-like growth factor I receptor levels. Neoplasia. 2011;13(2):108–19.
Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23(10):1124–34.
Prieto-Vila M, Takahashi R-u, Usuba W, Kohama I, Ochiya T. Drug resistance driven by cancer stem cells and their niche. Int J Mol Sci. 2017;18(12):2574.
Lai C-J, Lin C-Y, Liao W-Y, Hour T-C, Wang H-D, Chuu C-P. CD44 promotes migration and invasion of docetaxel-resistant prostate cancer cells likely via induction of hippo-yap signaling. Cells. 2019;8(4):295.
Talukdar S, Das SK, Pradhan AK, Emdad L, Windle JJ, Sarkar D, Fisher PB. MDA-9/Syntenin (SDCBP) is a critical regulator of chemoresistance, survival and stemness in prostate cancer stem cells. Cancers. 2019;12(1):53.
Liu Y-q, Wang S-k, Xu Q-q, Yuan H-q, Guo Y-x, Wang Q, Kong F, Lin Z-m. Sun D-q, Wang R-m: Acetyl-11-keto-β-boswellic acid suppresses docetaxel-resistant prostate cancer cells in vitro and in vivo by blocking Akt and Stat3 signaling, thus suppressing chemoresistant stem cell-like properties. Acta Pharmacol Sin. 2019;40(5):689–98.
Canesin G, Maggio V, Palominos M, Stiehm A, Contreras HR, Castellón EA, Morote J, Paciucci R, Maitland NJ, Bjartell A. STAT3 inhibition with galiellalactone effectively targets the prostate cancer stem-like cell population. Sci Rep. 2020;10(1):13958.
Njiaju UO, Gamazon ER, Gorsic LK, Delaney SM, Wheeler HE, Im HK, Dolan ME. Whole-genome studies identify solute carrier transporters in cellular susceptibility to paclitaxel. Pharmacogenet Genomics. 2012;22(7):498–507.
Sun R, Ying Y, Tang Z, Liu T, Shi F, Li H, Guo T, Huang S, Lai R. The emerging role of the SLCO1B3 protein in cancer resistance. Protein Pept Lett. 2020;27(1):17–29.
Cho E, Montgomery RB, Mostaghel EA. Minireview: SLCO and ABC transporters: a role for steroid transport in prostate cancer progression. Endocrinology. 2014;155(11):4124–32.
Lee HH, Leake BF, Teft W, Tirona RG, Kim RB, Ho RH. Contribution of hepatic organic anion-transporting polypeptides to docetaxel uptake and clearance. Mol Cancer Ther. 2015;14(4):994–1003.
De Morrée ES, Böttcher R, Van Soest RJ, Aghai A, De Ridder CM, Gibson AA, Mathijssen RH, Burger H, Wiemer EA, Sparreboom A. Loss of SLCO1B3 drives taxane resistance in prostate cancer. Br J Cancer. 2016;115(6):674–81.
Lin L, Yee SW, Kim RB, Giacomini KM. SLC transporters as therapeutic targets: emerging opportunities. Nat Rev Drug Discovery. 2015;14(8):543–60.
de Morrée E, van Soest R, Aghai A, de Ridder C, de Bruijn P, Ghobadi Moghaddam-Helmantel I, Burger H, Mathijssen R, Wiemer E, de Wit R. Understanding taxanes in prostate cancer; importance of intratumoral drug accumulation. Prostate. 2016;76(10):927–36.
Eder IE, Culig Z, Putz T, Nessler-Menardi C, Bartsch G, Klocker H. Molecular biology of the androgen receptor: from molecular understanding to the clinic. Eur Urol. 2001;40(3):241–51.
Jiang J, Huang H. Targeting the androgen receptor by taxol in castration-resistant prostate cancer. Mol Cell Pharmacol. 2010;2(1):1.
Augello MA, Den RB, Knudsen KE. AR function in promoting metastatic prostate cancer. Cancer Metastasis Rev. 2014;33:399–411.
Si M, Lang J. The roles of metallothioneins in carcinogenesis. J Hematol Oncol. 2018;11:1–20.
Darshan MS, Loftus MS, Thadani-Mulero M, Levy BP, Escuin D, Zhou XK, Gjyrezi A, Chanel-Vos C, Shen R, Tagawa ST. Taxane-induced blockade to nuclear accumulation of the androgen receptor predicts clinical responses in metastatic prostate cancer. Cancer Res. 2011;71(18):6019–29.
Zhu M-L, Horbinski CM, Garzotto M, Qian DZ, Beer TM, Kyprianou N. Tubulin-targeting chemotherapy impairs androgen receptor activity in prostate cancer. Cancer Res. 2010;70(20):7992–8002.
Gjyrezi A, Xie F, Voznesensky O, Khanna P, Calagua C, Bai Y, Kung J, Wu J, Corey E, Montgomery B. Taxane resistance in prostate cancer is mediated by decreased drug-target engagement. J Clin Investig. 2020;130(6):3287–98.
Antonarakis ES, Tagawa ST, Galletti G, Worroll D, Ballman K, Vanhuyse M, Sonpavde G, North S, Albany C, Tsao C-K. Randomized, noncomparative, phase II trial of early switch from docetaxel to cabazitaxel or vice versa, with integrated biomarker analysis, in men with chemotherapy-naive, metastatic, castration-resistant prostate cancer. J Clin Oncol. 2017;35(28):3181.
Komura K, Jeong SH, Hinohara K, Qu F, Wang X, Hiraki M, Azuma H, Lee G-SM, Kantoff PW, Sweeney CJ. Resistance to docetaxel in prostate cancer is associated with androgen receptor activation and loss of KDM5D expression. Proceedings of the National Academy of Sciences 2016, 113(22):6259–6264.
Dicken H, Hensley PJ, Kyprianou N. Prostate tumor neuroendocrine differentiation via EMT: the road less traveled. Asian J Urol. 2019;6(1):82–90.
Jolly MK, Ware KE, Gilja S, Somarelli JA, Levine H. EMT and MET: necessary or permissive for metastasis? Mol Oncol. 2017;11(7):755–69.
Puhr M, Hoefer J, Schäfer G, Erb HH, Oh SJ, Klocker H, Heidegger I, Neuwirt H, Culig Z. Epithelial-to-mesenchymal transition leads to docetaxel resistance in prostate cancer and is mediated by reduced expression of miR-200c and miR-205. Am J Pathol. 2012;181(6):2188–201.
Roche J. The epithelial-to-mesenchymal transition in cancer. In., vol. 10: MDPI; 2018: 52.
Marín-Aguilera M, Codony-Servat J, Reig Ò, Lozano JJ, Fernández PL, Pereira MV, Jiménez N, Donovan M, Puig P, Mengual L. Epithelial-to-mesenchymal transition mediates docetaxel resistance and high risk of relapse in prostate cancer. Mol Cancer Ther. 2014;13(5):1270–84.
Hanrahan K, O’Neill A, Prencipe M, Bugler J, Murphy L, Fabre A, Puhr M, Culig Z, Murphy K, Watson RW. The role of epithelial–mesenchymal transition drivers ZEB 1 and ZEB 2 in mediating docetaxel-resistant prostate cancer. Mol Oncol. 2017;11(3):251–65.
Mimeault M, Johansson SL, Batra SK. Marked improvement of cytotoxic effects induced by docetaxel on highly metastatic and androgen-independent prostate cancer cells by downregulating macrophage inhibitory cytokine-1. Br J Cancer. 2013;108(5):1079–91.
Paller C, Pu H, Begemann DE, Wade CA, Hensley PJ, Kyprianou N. TGF-β receptor I inhibitor enhances response to enzalutamide in a pre‐clinical model of advanced prostate cancer. Prostate. 2019;79(1):31–43.
Martin SK, Pu H, Penticuff JC, Cao Z, Horbinski C, Kyprianou N. Multinucleation and mesenchymal-to-epithelial transition alleviate resistance to combined cabazitaxel and antiandrogen therapy in advanced prostate cancer. Cancer Res. 2016;76(4):912–26.
Taylor BS, Schultz N, Hieronymus H, Gopalan A, Xiao Y, Carver BS, Arora VK, Kaushik P, Cerami E, Reva B. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010;18(1):11–22.
Lu X, Yang F, Chen D, Zhao Q, Chen D, Ping H, Xing N. Quercetin reverses docetaxel resistance in prostate cancer via androgen receptor and PI3K/Akt signaling pathways. Int J Biol Sci. 2020;16(7):1121.
Bitting RL, Armstrong AJ. Targeting the PI3K/Akt/mTOR pathway in castration-resistant prostate cancer. Endocrine-related Cancer. 2013;20(3):R83–99.
Avan A, Narayan R, Giovannetti E, Peters GJ. Role of akt signaling in resistance to DNA-targeted therapy. World J Clin Oncol. 2016;7(5):352.
Gan Y, Chen Q, Lei Y. Regulation of paclitaxel sensitivity in prostate cancer cells by PTEN/maspin signaling. Oncol Lett. 2017;14(4):4977–82.
Ward AB, Mir H, Kapur N, Gales DN, Carriere PP, Singh S. Quercetin inhibits prostate cancer by attenuating cell survival and inhibiting anti-apoptotic pathways. World J Surg Oncol. 2018;16:1–12.
Yasumizu Y, Miyajima A, Kosaka T, Miyazaki Y, Kikuchi E, Oya M. Dual PI3K/mTOR inhibitor NVP-BEZ235 sensitizes docetaxel in castration resistant prostate cancer. J Urol. 2014;191(1):227–34.
Engels FK, Ten Tije AJ, Baker SD, Lee CK, Loos WJ, Vulto AG, Verweij J, Sparreboom A. Effect of cytochrome P450 3A4 inhibition on the pharmacokinetics of docetaxel. Clin Pharmacol Ther. 2004;75(5):448–54.
Zhang B, Zhao R, He Y, Fu X, Fu L, Zhu Z, Fu L, Dong J-T. Micro RNA 100 sensitizes luminal a breast cancer cells to paclitaxel treatment in part by targeting mTOR. Oncotarget. 2016;7(5):5702.
Aghajani M, Mokhtarzadeh A, Aghebati-Maleki L, Mansoori B, Mohammadi A, Safaei S, Asadzadeh Z, Hajiasgharzadeh K, Khaze Shahgoli V, Baradaran B. CD133 suppression increases the sensitivity of prostate cancer cells to paclitaxel. Mol Biol Rep. 2020;47:3691–703.
Lobert S, Jefferson B, Morris K. Regulation of β-tubulin isotypes by micro‐RNA 100 in MCF7 breast cancer cells. Cytoskeleton. 2011;68(6):355–62.
Liu X, Luo X, Wu Y, Xia D, Chen W, Fang Z, Deng J, Hao Y, Yang X, Zhang T. MicroRNA-34a attenuates paclitaxel resistance in prostate cancer cells via direct suppression of JAG1/Notch1 axis. Cell Physiol Biochem. 2018;50(1):261–76.
Orr GA, Verdier-Pinard P, McDaid H, Horwitz SB. Mechanisms of taxol resistance related to microtubules. Oncogene. 2003;22(47):7280–95.
Zhao J, Wang X, Mi Z, Jiang X, Sun L, Zheng B, Wang J, Meng M, Zhang L, Wang Z. STAT3/miR-135b/NF-κB axis confers aggressiveness and unfavorable prognosis in non-small-cell lung cancer. Cell Death Dis. 2021;12(5):493.
Santos JC, Lima NS, Sarian LO, Matheu A, Ribeiro ML, Derchain SFM. Exosome-mediated breast cancer chemoresistance via miR-155 transfer. Sci Rep. 2018;8(1):829.
Li X, Han X, Wei P, Yang J, Sun J. Knockdown of lncRNA CCAT1 enhances sensitivity of paclitaxel in prostate cancer via regulating mir-24-3p and FSCN1. Cancer Biol Ther. 2020;21(5):452–62.
Kopczyńska E. Role of microRNAs in the resistance of prostate cancer to docetaxel and paclitaxel. Contemp Oncology/Współczesna Onkologia. 2015;19(6):423–7.
Lo U-G, Yang D, Hsieh J-T. The role of microRNAs in prostate cancer progression. Translational Androl Urol. 2013;2(3):228.
Chen L, Cao H, Feng Y. MiR-199a suppresses prostate cancer paclitaxel resistance by targeting YES1. World J Urol. 2018;36:357–65.
Horwitz SB, Cohen D, Rao S, Ringel I, Shen H, Yang C. Taxol: mechanisms of action and resistance. J Natl Cancer Inst Monogr 1993(15):55–61.
Wang YC, Juric D, Francisco B, Yu RX, Duran GE, Chen KG, Chen X, Sikic BI. Regional activation of chromosomal arm 7q with and without gene amplification in taxane-selected human ovarian cancer cell lines. Genes Chromosom Cancer. 2006;45(4):365–74.
Boyerinas B, Park SM, Murmann AE, Gwin K, Montag AG, Zillhardt M, Hua YJ, Lengyel E, Peter ME. Let-7 modulates acquired resistance of ovarian cancer to Taxanes via IMP‐1‐mediated stabilization of multidrug resistance 1. Int J Cancer. 2012;130(8):1787–97.
Malofeeva EV, Domanitskaya N, Gudima M, Hopper-Borge EA. Modulation of the ATPase and transport activities of broad-acting multidrug resistance factor ABCC10 (MRP7). Cancer Res. 2012;72(24):6457–67.
Kavallaris M, Kuo D, Burkhart CA, Regl DL, Norris MD, Haber M, Horwitz SB. Taxol-resistant epithelial ovarian tumors are associated with altered expression of specific beta-tubulin isotypes. J Clin Investig. 1997;100(5):1282–93.
Goncalves A, Braguer D, Kamath K, Martello L, Briand C, Horwitz S, Wilson L, Jordan M. Resistance to Taxol in lung cancer cells associated with increased microtubule dynamics. Proceedings of the National Academy of Sciences 2001, 98(20):11737–11742.
Jaffrezou J-P, Dumontet C, Derry WB, Duran G, Chen K, Tsuchiya E, Wilson L, Jordan MA, Sikic BI. Novel mechanism of resistance to paclitaxel (taxol) in human K562 leukemia cells by combined selection with PSC 833. Oncol Res. 1995;7(10–11):517–27.
Kajiyama H, Shibata K, Terauchi M, Yamashita M, Ino K, Nawa A, Kikkawa F. Chemoresistance to paclitaxel induces epithelial-mesenchymal transition and enhances metastatic potential for epithelial ovarian carcinoma cells. Int J Oncol. 2007;31(2):277–83.
Işeri ÖD, Kars MD, Arpaci F, Atalay C, Pak I, Gündüz U. Drug resistant MCF-7 cells exhibit epithelial-mesenchymal transition gene expression pattern. Biomed Pharmacother. 2011;65(1):40–5.
Yang Q, Huang J, Wu Q, Cai Y, Zhu L, Lu X, Chen S, Chen C, Wang Z. Acquisition of epithelial–mesenchymal transition is associated with Skp2 expression in paclitaxel-resistant breast cancer cells. Br J Cancer. 2014;110(8):1958–67.
Ganguly A, Yang H, Cabral F. Class III β-tubulin counteracts the ability of paclitaxel to inhibit cell migration. Oncotarget. 2011;2(5):368.
Hari M, Yang H, Zeng C, Canizales M, Cabral F. Expression of class III β-tubulin reduces microtubule assembly and confers resistance to paclitaxel. Cell Motil Cytoskeleton. 2003;56(1):45–56.
Ferlini C, Raspaglio G, Mozzetti S, Cicchillitti L, Filippetti F, Gallo D, Fattorusso C, Campiani G, Scambia G. The seco-taxane IDN5390 is able to target class III β-tubulin and to overcome paclitaxel resistance. Cancer Res. 2005;65(6):2397–405.
Kavallaris M, Burkhart C, Horwitz S. Antisense oligonucleotides to class III β-tubulin sensitize drug-resistant cells to Taxol. Br J Cancer. 1999;80(7):1020–5.
Gan PP, Pasquier E, Kavallaris M. Class III β-tubulin mediates sensitivity to chemotherapeutic drugs in non–small cell lung cancer. Cancer Res. 2007;67(19):9356–63.
Don S, Verrills NM, Liaw TY, Liu ML, Norris MD, Haber M, Kavallaris M. Neuronal-associated microtubule proteins class III β-tubulin and MAP2c in neuroblastoma: role in resistance to microtubule-targeted drugs. Mol Cancer Ther. 2004;3(9):1137–46.
Duran GE, Wang YC, Francisco EB, Rose JC, Martinez FJ, Coller J, Brassard D, Vrignaud P, Sikic BI. Mechanisms of resistance to cabazitaxel. Mol Cancer Ther. 2015;14(1):193–201.
Quinn JE, Kennedy RD, Mullan PB, Gilmore PM, Carty M, Johnston PG, Harkin DP. BRCA1 functions as a differential modulator of chemotherapy-induced apoptosis. Cancer Res. 2003;63(19):6221–8.
Chabalier C, Lamare C, Racca C, Privat M, Valette A, Larminat F. BRCA1 downregulation leads to premature inactivation of spindle checkpoint and confers paclitaxel resistance. Cell Cycle. 2006;5(9):1001–7.
Lafarge S, Sylvain V, Ferrara M, Bignon Y-J. Inhibition of BRCA1 leads to increased chemoresistance to microtubule-interfering agents, an effect that involves the JNK pathway. Oncogene. 2001;20(45):6597–606.
Sung M, Giannakakou P. BRCA1 regulates microtubule dynamics and taxane-induced apoptotic cell signaling. Oncogene. 2014;33(11):1418–28.
Kurebayashi J, Yamamoto Y, Kurosumi M, Okubo S, Nomura T, Tanaka K, Sonoo H. Loss of BRCA1 expression may predict shorter time-to-progression in metastatic breast cancer patients treated with taxanes. Anticancer Res. 2006;26(1B):695–701.
Holohan C, Van Schaeybroeck S, Longley DB, Johnston PG. Cancer drug resistance: an evolving paradigm. Nat Rev Cancer. 2013;13(10):714–26.
Buck SA, Koolen SL, Mathijssen RH, de Wit R, van Soest RJ. Cross-resistance and drug sequence in prostate cancer. Drug Resist Updates. 2021;56:100761.
Shimura T, Kitagawa M, Yamada T, Yoshida M, Ebi M, Hirata Y, Mizushima T, Mizoshita T, Tanida S, Kataoka H. The impact of cross-resistance between paclitaxel and docetaxel for metastatic gastric cancer. Oncol Res Treat. 2012;35(4):176–83.
Valero V, Jones SE, Von Hoff DD, Booser DJ, Mennel RG, Ravdin PM, Holmes FA, Rahman Z, Schottstaedt MW, Erban JK. A phase II study of docetaxel in patients with paclitaxel-resistant metastatic breast cancer. J Clin Oncol. 1998;16(10):3362–8.
Haldar S, Basu A, Croce CM. Bcl2 is the guardian of microtubule integrity. Cancer Res. 1997;57(2):229–33.
Aldonza MBD, Hong J-Y, Lee SK. Paclitaxel-resistant cancer cell-derived secretomes elicit ABCB1-associated docetaxel cross-resistance and escape from apoptosis through FOXO3a-driven glycolytic regulation. Exp Mol Med. 2017;49(1):e286–286.
Lin Y-C, Chang H-K, Wang C-H, Chen J-S, Liaw C-C. Single-agent docetaxel in metastatic breast cancer patients pre-treated with anthracyclines and paclitaxel: partial cross-resistance between paclitaxel and docetaxel. Anticancer Drugs. 2000;11(8):617–21.
Chen R, Cheng Q, Owusu-Ansah KG, Chen J, Song G, Xie H, Zhou L, Xu X, Jiang D, Zheng S. Cabazitaxel, a novel chemotherapeutic alternative for drug-resistant hepatocellular carcinoma. Am J Cancer Res. 2018;8(7):1297.
Lombard AP, Liu C, Armstrong CM, Cucchiara V, Gu X, Lou W, Evans CP, Gao AC. ABCB1 mediates cabazitaxel–docetaxel cross-resistance in advanced prostate cancer. Mol Cancer Ther. 2017;16(10):2257–66.
Liu L, Li M, Zhang J, Xu D, Guo Y, Zhang H, Cang S. KIF14 mediates cabazitaxel-docetaxel cross-resistance in advanced prostate cancer by promoting AKT phosphorylation. Arch Biochem Biophys. 2023;737:109551.
Wang Y, Huang Z, Chen CZ, Liu C, Evans CP, Gao AC, Zhou F, Chen H-W. Therapeutic targeting of MDR1 expression by RORγ antagonists resensitizes cross-resistant CRPC to taxane via coordinated induction of cell death programs. Mol Cancer Ther. 2020;19(2):364–74.
Machioka K, Izumi K, Kadono Y, Iwamoto H, Naito R, Makino T, Kadomoto S, Natsagdorj A, Keller ET, Zhang J. Establishment and characterization of two cabazitaxel-resistant prostate cancer cell lines. Oncotarget. 2018;9(22):16185.
Funding
No funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
A I. A: wrote the main manuscript text.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alalawy, A.I. Key genes and molecular mechanisms related to Paclitaxel Resistance. Cancer Cell Int 24, 244 (2024). https://doi.org/10.1186/s12935-024-03415-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-024-03415-0