Abstract
Hypoxia is a common feature of solid tumors, and develops because of the rapid growth of the tumor that outstrips the oxygen supply, and impaired blood flow due to the formation of abnormal blood vessels supplying the tumor. It has been reported that tumor hypoxia can: activate angiogenesis, thereby enhancing invasiveness and risk of metastasis; increase survival of tumor, as well as suppress anti-tumor immunity and hamper the therapeutic response. Hypoxia mediates these effects by several potential mechanisms: altering gene expression, the activation of oncogenes, inactivation of suppressor genes, reducing genomic stability and clonal selection. We have reviewed the effects of hypoxia on tumor biology and the possible strategiesto manage the hypoxic tumor microenvironment (TME), highlighting the potential use of cancer stem cells in tumor treatment.
Similar content being viewed by others
Background
Solid tumors are the most common forms of cancer, and they account for high levels of morbidity and mortality globally [1]. They consist of an abnormal mass of cells containing blood and lymphatic vessels, components of the extracellular matrix (ECM), heterogeneous cells populations including fibroblasts, cancer stem cells (CSCs) and immune cells [2]. Solid tumors are commonly affected by hypoxia. In the tumor microenvironment (TME), uncontrolled cell proliferation often exceeds the ability to satisfy the oxygen demand from the preexisting blood vessels. This usually occurs when the tumor exceeds a diameter of approximately 1 mm [3, 4]. Tumor hypoxia-induced responses, include: altered gene expression, suppressing apoptosis, or promoting autophagy [5, 6], stimulation of the epithelial-mesenchymal transition (EMT), malignant progression and distant tumor metastasis [7, 8], enhanced angiogenesis and vasculogenesis [9,10,11], and changes in anabolic phenotype to core cellular metabolism [12, 13]. Moreover, hypoxia is also implicated in genomic instability due to the increased production of reactive oxygen species (ROS) and alterations in the DNA damage repair pathways [14, 15]. Hypoxia also enhances the aggressiveness of tumors by clonal selection. The new and more invasive selected clones lead to a vicious cycle of hypoxia, that act as a barrier to conventional cancer therapy, including radiotherapy, chemotherapy and phototherapy [16]. Hypoxia also impacts on the immune system through different pathways and contributes to a reduced anti-tumor response [16, 17]. Furthermore, there is mounting evidence suggesting that CSCs that are affected by hypoxia are largely responsible for tumor resistance and recurrence after conventional therapy. In contrast, there is also data in the literature that suggest that hypoxia makes tumor cells more sensitive to chemotherapy. However, it is generally accepted that tumors that are hypoxic are associated with a poorer outcome. In this review, we describe the events in the tumor milieu that are influenced by hypoxia and lead to tumor expansion and malignant progression favoring immune escape, frustrated anti-tumor therapy, and eventually tumor relapse, highlighting the function of hypoxic CSCs. Specifically, we will pursue the following: (i) the main transcription factors in hypoxia and distribution of HIF proteins in various hypoxic zones in tumor environment, (ii) tight regulation between hypoxia and angiogenesis, (iii) the role for hypoxia associated factors in maintenance of stem-like phenotype and development of CSCs, (iv) the role of hypoxia in cancer progression, metastasis, immunosuppression, and treatment resistance, (v) therapeutic strategies for re-engineer the hypoxic tumor microenvironment, (vi) therapeutic strategies considering the roles of CSCs in tumor development, metastasis and recurrence.
Transcription factors of signaling pathways in hypoxia
The effects of hypoxia on tumor cells are mediated by the hypoxia inducible factor (HIF) family in major part [18]. The HIFs promote the expression of more than 150 genes, whose products coordinate the adaptive responses [19]. HIF-driven transcription encodes: vascular endothelial growth factor (VEGF), erythropoietin, transferrin and transferrin receptors, the enzymes required for glycolysis, anti-apoptotic factors, multiple growth factors [such as platelet-derived growth factor-B (PDGF-B), transforming growth factor beta (TGF-β), insulin-like growth factor-2 (IGF-2), epidermal growth factor (EGF)], and other proteins involved in normal homeostasis [20, 21]. Although, these factors are a part of adaptive response that allows them to compensate for reduced oxygen tension (and nutrients); hypoxic cancer cells overexpress them to increase survival, aberrant angiogenesis, extreme cell growth, and metastasis. The members of this family of transcription factors; HIF1, HIF2 and HIF3, are heterodimers that comprise α and β subunits. HIFα is a cytoplasmic protein regulated by oxygen levels, whereas HIFβ, a nuclear protein that is constitutively expressed, independent of hypoxic conditions [22]. HIF1α and HIF2α (also called EPAS-1/HRF/HLF/MOP2) in complex with HIF-1β (also known as ARNT) mediate the vast majority of HIF transcriptional activity. When oxygen supply is sufficient, HIF1α subunit is hydroxylated at proline residues through oxygen-dependent enzyme activity. By Hydroxylation of prolyl sites binding to von Hippel Lindau tumor suppressor (pVHL), HIF-1α undergoes degradation via the ubiquitin-proteasome system [23, 24]. Under hypoxic conditions, non-hydroxylated HIF-1α subunits translocated to the nucleus, where they combine with HIF-1β subunits to form heterodimers. The resultant heterodimer is the active HIF-1 factor binding to the hypoxia response elements of target genes that eventually drive the transcriptional responses [25]. HIF-1α appears to be expressed in most cell types, while the HIF-2α is mostly expressed in the endothelial cells (ECs) of the embryonic vasculature, neural crest-derived sympathetic ganglia, and of the developing pulmonary epithelial cells, kidney mesangial cells, and especially in renal cell carcinomas, in which pVHL, an E3 ligase for HIFα, is mutated. These two distinct, but highly related HIFs, have partially non-overlapping function and targeting a distinct subset of hypoxia-induced genes. An important distinction between HIF1α and HIF2α, is the specific stabilization pattern under different oxygen concentrations. Holquimvist-Mengelbier et al. [26], showed that HIF-2α, as opposed to the low HIF-1α activity, was strongly expressed and active at 5% oxygen (intermediate hypoxia), corresponding to well-vascularized tumor areas. Whereas, HIF-1α is predominantly active in 1% oxygen (severe hypoxia), under prolonged or chronic hypoxic conditions, the stabilization of HIF-1α is transient in this condition and HIF-2α is continuously accumulated in prolonged, severe hypoxia (1% O2).
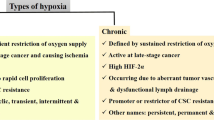
Tumor hypoxia and HIF protein expression
Hypoxic zones arise as a consequence of an imbalance between oxygen supply and consumption in solid malignant tumor, in which the oxygen pressure often reduces to a median of 0–20 mmHg (1%-2% or below). Whereas in normal healthy tissues oxygen tension is approximately 40 mmHg (~ 5%) in the liver and approximately 100 mm Hg (~ 13%) in arterial blood [4, 27]. Several mechanisms can contribute to the development of hypoxia in the tumor microenvironment. Perfusion-restricted hypoxia (also called acute, intermittent, transient, perfusion-limited or cyclic hypoxia), that can be transient, with insufficient delivery of oxygen due to aberrant blood vessels undergoing repeated cycles of closing and reopening, and consequential sluggish blood flow and fluctuations in oxygen supply. These constant fluctuations lead to cyclic periods of hypoxia and re-oxygenation that can lead to the development of a heterogeneous cell population within tumor [20, 28]. Diffusion-restricted hypoxia (also called chronic or permanent hypoxia) is the other type of tumor hypoxia and refers to the sustained restriction in oxygen diffusion by abnormal vascular network. Chronic hypoxia occurs when the tumor cells expand beyond 70 µm from the pre-existing nutritive blood vessels, which prevents an adequate delivery of oxygen [29]. At a farther distance from the blood supply (> 180 µm), the tumor cells can even become necrotic [30, 31]. Occasionally, anemic hypoxia can arise following a reduction in oxygen transport capacity by the blood. Anemic hypoxia can be either related to the presence of tumor or therapy-induced. Tumor tissue cannot fully compensate for the reduced oxygen levels, so it is more susceptible to anemic hypoxia [32].
Acute and chronic hypoxia are mainly mediated by HIF1α and HIF2α, respectively, and have often been reported to be associated with tumor progression and aggressive phenotype [26, 33]. However, as opposed to acute hypoxia, chronic hypoxia has also been shown to contribute to regression [34, 35]. Moreover, several studies have demonstrated that acute hypoxia increases cell survival and autophagy, selecting for cancer cells with stem cell characteristics, enhancing stem-like cell marker expression and endow resistance to radiotherapy [36,37,38,39]. Chenet al, showed that acute hypoxia, but not chronic hypoxia, induces genetic, molecular, biochemical, and cellular alterations promoting tumor cells with greater survival, heterogeneity, plasticity, tumorigenic capacity and resistance to anoikis, and thus enhanced ability for metastasis. In this study, HIF-1α expression was lost during chronic hypoxia, when HIF-2α mediated hypoxic responses may still be present [40].
Hypoxia and angiogenesis
Tumor cells adapt to reduced oxygen levels by promoting the development of new blood vessels, a process termed angiogenesis [41]. Pro-angiogenic factors and their receptors including vascular endothelial growth factor (VEGF),VEGF receptor-1,-2 (VEGFR-1,-2), basic fibroblast growth factor (bFGF), platelet derived growth factor B (PDGF), insulin-like growth factor II (IGF2), adrenomedullin, and epidermal growth factor (EGF) are targets of the HIF transcription factors, and provide a molecular mechanism by which hypoxia regulates angiogenesis [42]. Several of these angiogenesis-related gene products, including iNOS, endothelin, adrenomedullin, and heme oxygenase 1, are also implicated in the modulation of local blood flow by regulating the vascular tone [43].
New vessels develop under hypoxic conditions but display substantial abnormalities, including; (i) an unusually elongated and tortuous shape, sometimes with blind-ends causing geometric resistance, and which leads to a disruption in blood flow and intermittent stasis, (ii) increased dilations and permeability due to insufficient smooth muscle cell layer, discontinuous endothelium or absent endothelial cell lining and basement membranes, (iii) a deficiency in pharmacological/physiological receptors and contractile wall components [20, 44].
Therefore, the tissue responses to ameliorate an impaired oxygen supply still fail [45]. Furthermore, due to a more access of metastatic cells to blood vessels, angiogenesis associated with a more invasive tumor phenotype [46, 47]. Angiogenesis is also an important step in carcinogenesis and transition from hyperplasia towards neoplasia [48].
Signaling pathway for angiogenesis
Angiogenesis ismediated by the release of VEGF, the major hypoxia-inducible angiogenic stimulator, and this is driven by HIF.HIF-1 influences tumor blood flow through more complex mechanisms; HIF-1 targets different genes playing the role in vessel tone.
Information regarding the role of HIF2-α in hypoxia-related angiogenesis in tumor microenvironment is more controversial than for HIF-1α. Deletion of the HIF-1α gene in endothelial cells (EC), has been reported to reduce neovascularization and tumor growth, by disrupting the VEGF-mediated autocrine loop in EC, which is an essential component of solid tumor angiogenesis [49]. But, Skuli et al. [50], have demonstrated that HIF-2α gene deletion increased angiogenesis, albeit with more disorganized vessels resulting in poor perfusion and more hypoxic tumors in limb ischemia and autochthonous skin tumor models. They suggested that HIF-1α and HIF-2α act independently in response to local hypoxic stress, as HIF-1α promotes growth, proliferation, and morphogenesis in endothelial cells, while, HIF-2α is required for effective vessel remodeling and induction of a mature, functional vascular network. Conversely, this group of investigators had been previously reported that HIF-2α deletion resulted in reduced tumor angiogenesis, as well as increased vessel permeability and loss of integrity with a variable morphology in different adult organs [51]. These inconsistencies may be partly related to different expression patterns of HIF-2α in different tissues and its related cell type-specific signaling pathways [52]. HIF-1α and HIF-2α partially compensate for each other, however, they independently promote the modulations in the context of pathophysiological hypoxia to produce a functional vasculature [53, 54].
The effect of hypoxia on cancer stem cells
There is mounting evidence that hypoxia affects the maintenance and functions of CSCs. CSCs constitute an undifferentiated stem-like cell subpopulation within the tumor heterogeneous cell types, which contributes to cancer initiation, progression, metastasis, therapeutic resistance and cancer relapse.
In solid tumors and hematological cancers, CSCs possess common properties to their normal stem cell counterparts, including self-renewal and the capacity to give rise to various cell types [55]. Furthermore, CSCs have the capacity for sphere formation. Although there are some potential markers suggested for CSCs in hematological cancers, definitive universal markers for CSCs in solid tumors remain unknown [56, 57]. CSCs appear to ‘educate’ neighboring cells to provide nutrients, cooperate in their evasion from the immune system, and create a microenvironment favoring tumor growth. CSCs can be differentiated into various cells that may be found in the tumor, which is associated with their high plasticity [58], establishment of a quiescent state with basal activity [59], enhanced survival ability in a stressful tumor environment with reduced oxygen and nutrient levels, and increased resistance to chemo-, radio- and immuno-therapy, and therefore utilized by tumors to escape from treatment and leads to recurrence [60]. Normal stem cells, such as hematopoietic stem cells, are retained in an hypoxic zone distant from the vasculature, which aids the maintenance of their stem cell properties [61]. While increased oxygen levels lead to the loss of these properties (stem and progenitor features referred to as stemness) [62]. Likewise, CSCs tend to localize to hypoxic regions within tumors, which probably favor the preservation the stem-ness, as well as to generate highly invasive and tumorigenic cells [63]. In conformity with this, Jogi et al., have reported that hypoxic cells in neuroblastoma (NB) adopt an immature phenotype [64]. It seems that cells in hypoxic areas, within the TME, are less mature and more invasive than oxygenated cells, and display a stem cell-like phenotype. [65].
HIF signaling plays a significant role in the modulation of various signaling pathways, which are exploited by CSCs to regulate stemness during hypoxic and therapeutic stress [66,67,68]. These pathways include Notch, Hedgehog, Hippo, Wnt (wingless)/β-catenin, Janus-activated kinase/signal transducer, activator of transcription (JAK/STAT), phosphatidylinositol 3-kinase/phosphatase, tensin homolog (PI3K/PTEN), and nuclear factor-kB (NF-kB) pathways. [69,70,71].
There is a growing body of evidence that implicates the reliance of CSCs on HIFs for the maintenance of their phenotype and function [68]. HIFs induce numerous gene products, including pluripotency related transcription factors, epithelial to mesenchymal transition (EMT) programmer, glycolysis-associated molecules, drug resistance-associated molecules, miRNAs and VEGF [68, 72].
Hypoxia-mediated upregulation of pluripotency gene
HIF signaling enhances the maintenance of a CSC phenotype through the regulation of octamer-binding transcription factor 4 (Oct4), sex determining region Y box 2 (SOX2), kruppel-like factor 4 (KLF4), myelocytomatosis oncogene product (Myc), Tir nan Og (NANOG) and polycomb complex protein BMI-1 (BMI1) [72, 68].
Though both HIFs participate in CSCs survival and stemness maintenance [73, 74], hypoxia mediated transcription of stem-ness genes is differentially regulated by HIF-1α and HIF-2α. HIF-1α triggers Nanog, whilst HIF-2α activates Oct4 and c-Myc transcription [75,76,77]. Moreover, the HIFs contribute to the induction of CSC trait in different manner, with greater involvement of HIF-1α for survival functions and more specificity of HIF-2α for stem-ness properties (i.e. self-renewal) [78]. Bae et al. showed that the role of HIFs in CSCs function is dependent on the duration of exposure to hypoxia. HIF-1α enhances the expression of stem cell marker SOX2 and acute hypoxia-mediated cell invasion, while HIF-2α elevates the chronic hypoxia-mediated SOX2 and sphere formation in prostate cancer [79]. There is some evidence for the stronger induction of CSCs by HIF-1α in hypoxic areas during tumor development, and for HIF-2α as the main HIF factor under normoxic conditions that follow after cancer therapy, leading to a reduction in tumor size [80]. Consistent with this, Johansson and colleagues show that the expression of HIF-2α is significantly enhanced under normoxic and hypoxic conditions in glioma stem cells (GSCs). Also, the intracellular domain of CD44, a stem cell marker, is released in hypoxia, and binds to HIF-2α, but not HIF-1α, and subsequently upregulates hypoxia-induced stemness genes in GSCs [81].
Hypoxia-mediated induction of EMT
There are experimental and clinical data suggesting that CSCs are strongly linked to EMT. EMT contributes to tumor aggressiveness, by promoting tumor cell invasion and migration, induction of stem cell phenotype, and subsequent therapeutic resistance leading to tumor recurrence [82,83,84,85]. Hypoxia, via HIF signaling, has been recognized to induce EMT and CSC features. During this phenomenon, tumor cells detach and acquire a mesenchymal phenotype, display the stemness properties including loss of differentiation, tumorigenesis and increased resistance to therapy [85]. Hypoxia/HIF-induced EMT and CSC phenotype mediated by similar signaling pathways consisting of NF-κB, PI3K/Akt, Wnt/β-catenin, Hedgehog and Notch [86]. A recent study also demonstrated that common genes are involved in EMT and a stemness phenotype, which contribute to tumor plasticity in response to anti-cancer therapies [87].
Hypoxia-mediated miRNAs
Recent findings have been provided evidence that support the responsiveness of a variety of miRNAs to hypoxia that play pivotal role in many aspects of tumor development and malignancy, including angiogenesis, metabolic adaptation, EMT and CSCs sustenance. Hypoxia can down regulate the expression of miR-20, miR-22, miR-101 and let-7, as well as up regulate the expression of miR-21, miR-107, miR-181b, miR-210, and miR-373 in tumor cells. Hypoxia often up regulates oncogenic miRNAs and down regulates anti-tumorigenic miRNAs and thereby are associated with a poor clinical prognosis [86, 88]. However, it has been reported to be associated with an increase in anti-tumorigenic miRNAs such as miR-107. Therefore, more investigation is required to demonstrate the role of these miRNAs in stemness regulation and tumor progression under hypoxic conditions. Hypoxia-mediated miRNAs in TME that possess the ability of stemness regulation is summarized in Table 1.
Hypoxia-mediated angiogenic factors
HIFs up regulate the expression of angiogenic factors, particularly VEGF in CSCs and promote tumor angiogenesis [151, 152]. In addition to stimulation of angiogenesis, hypoxia-induced VEGF is known to drive EMT and maintain CSC stemness, and by these mechanisms contributes to tumor invasion and metastasis [153, 154].
Hypoxia-mediated metabolic adaptation
Hypoxia-induced metabolic reprogramming can also contribute to CSC maintenance and resistance [68]. In most cases, the principal metabolic pattern in normal stem cells is glycolysis whereas differentiated cells primarily perform oxidative phosphorylation (OXPHOS). Meanwhile, CSCs do not resemble the metabolic pattern of normal stem cells. Indeed, both glycolysis and OXPHOS are metabolic engines in CSCs, and predominant metabolic pattern depends on the type of tumor and TME stimuli [155]. The hallmark of hypoxia-induced metabolic reprogramming is a shift in ATP production from OXPHOS to glycolysis. Under hypoxic conditions, HIF-1α (and HIF-2α) that is stabilized in CSCs, triggers the expression of genes involved in metabolic adaptation (e.g., GLUT1, LDH -A, PDK) [77]. Consequently, lactate increased and levels of ROS are reduced, in turn leading to CSC protection and potentially therapy failure [156]. Evidences show that high level of lactate and acidic stress in the microenvironment induce CSC phenotype [157], tumor invasiveness, and impair the immune response [158, 159]. Acidic stress is considered to be a mechanism for HIF-2α induction, in which HIF-1α can upregulate HIF-2α activation via metabolic pathways [160].
There is some evidence for a link between high levels of aldehyde dehydrogenase (ALDH), the enzyme responsible for oxidizing intracellular aldehydes, and response of CSCs to hypoxia. Shiraishi and colleagues, showed that under hypoxic conditions, the expression of ALDH1A1 is associated with the overexpression of HIF-1α, but not HIF-2α, and stemness in breast cancer stem cells (BCSCs) [161]. Kim and colleagues, however, showed that ALDH was highly associated with the HIF-2α expression of breast cancer cell lines in vitro and self-renewal ability of BCSCs in mouse model of breast cancer [162]. Regardless of HIFs, overexpression of the membrane-bound ectoenzymes carbonic anhydrases (CAIX and CAXII) and monocarboxylate transporter-4 (MCT-4) in response to hypoxia, promotes a CSC phenotype and function, by modifying acidic pH of hypoxic cancer cells with a high rate of glycolytic metabolism [163, 164].
Hypoxia-mediated quiescence
By modulation of the process of metabolic adaptation, apoptotic pathways, cell cycle and self-renewal, hypoxia, maintains the CSCs in the quiescent state. Quiescence defined as a protective response to adverse condition, enabling cells to conserve the proliferative potency and eliminate DNA damage [165]. Non-dividing quiescent CSCs that can survive after conventional therapy targeting rapidly dividing cells, are responsible for the failure of cancer therapy and tumor relapse [166]. Prati and colleagues demonstrated that under chronic hypoxic stress, breast cancer cells enter into quiescent state, characterized by cell-cycle arrest in G0/G1 and lower levels of metabolism. These dormant cells have a CSC phenotype and sphere-forming capacity [167].
One of the major regulators that contributes to the induction of cell-cycle arrest, and quiescence, during hypoxia, is HIF-1α, that acts independently of p53 and causes the up-regulation of cyclin-dependent kinase inhibitors p21 and p27, hypophosphorylation of RB and suppression of cell cycle gene CDC25A [168, 169]. However, it has been reported that the de-depression of cyclin-dependent kinase inhibitors, such as p21, is not essential for HIF-1α-induced quiescence [170]. Also, HIF-1α+ quiescent stem-like cells are associated with increased sphere-forming capacity and higher tumorigenicity in glioblastoma patients [171]. Although, HIF-1α can promote cell-cycle arrest by inhibiting c-Myc activity [172], HIF-2α has been shown to stimulate the progression of the cell-cycle and neoplastic growth of cancer cell, via functional enhancement of c-Myc [76]. The induction of quiescence by HIF-1α may appear to contradict some evidence from its role in cancer growth. However, HIF-1α may temporally maintain cancer cells in a quiescent state and conserve their survival as long as oxygen supply is available, where they become more invasive.
Hypoxia-mediated resistance
Hypoxic CSCs also have a high expression of a number of Adenosine triphosphate–binding cassette (ABC) transporters, including multidrug resistance gene 1 (MDR1 or ABCB1) and its product permeability glycoprotein (P-glycoprotein), multidrug resistance-associated protein (MRP1), breast cancer resistance protein (BCRP or ABCG2 or MXR) and ABCB5 [78]. These membrane transporters as a feature of stem-like cells, and contribute to transporting cytotoxic materials out of cell. CSCs exploit the BCRP to offset the detrimental effect of heme or porphyrin accumulation, under hypoxic condition [173]. The ABC transporters, further, provide a high capacity efflux system, leading to chemotherapy failure and highly drug-resistant tumor formation [174]. HIFs play the role in the activation of drug transporter in CSCs upon hypoxic condition. The HIF-mediated increased expression of these transporter reduce the effect of chemotherapeutic agents, including paclitaxel, gemcitabine and Imantinib [175, 176]. Both HIF-1α and HIF-2α participate in the up-regulation of ABC transporters and chemo-resistance, but in different capacities. With a central role of HIF-1α for MDR1 activation and partial participation in BCRP and MRP1 activity, as well as more responsibility of HIF-2α for BCRP activation and less relevance to MDR1 control [177].
The role of hypoxia in cancer progression, metastasis, immunosuppression, and treatment resistance
Hypoxia can substantially affect the malignant progression and therapeutic response of solid tumors by change the transcriptome and regulating the production of proteins in tumor cells that modulate immune privilege and limit anticancer immunity [178]. Thus, hypoxic condition often linked to a poor prognosis of many cancers. Conversely, some evidences implicate the augmentation of anti-tumor response by hypoxia associated factors.
Hypoxia-induced cancer progression and metastasis
Hypoxia may facilitate the dissemination of cells from the tumor to the other region of the body, by reducing the strength of interactions between cells and their supporting extracellular matrix (Fig. 1a). Czekayet al. [179], have shown that plasminogen activator inhibitor-1 (PAI-1) has a de-adhesive activity, as well as other de-adhesion molecules that include: thrombospondins (TSPs) 1 and 2, tenascin-C, and SPARC(secreted protein, acidic and rich in cysteine) [180]. These proteins can reverse the cell adhesion process and disrupt the integrin-mediated cell attachment. Consistent with this, high levels of PAI-1 have been reported to be associated with a poor prognosis in metastatic human cancers [181, 182].
The diagram displays the responses to reduced oxygenation within the tumor microenvironment. Hypoxia promotes tumor invasion, metastasis and resistance through several ways. a Hypoxia induces detachment of tumor cells by weakening the connections between cells and their extracellular matrix supporting them, and promotes dissemination of tumor cells to the various organs of the body. Thereby hypoxia triggers the metastatic spread of tumor. b Hypoxia stimulates angiogenesis, and provides more opportunity for detached tumor cell to inter into the circulation and migrate via the newly formed vessels. Thereby hypoxia enhances invasive and metastatic spread of solid tumors to another region. c Hypoxia induces EMT, in which tumor cells detach, lose the epithelial feature, acquire a mesenchymal phenotype and display the stemness properties including loss of differentiation, tumorigenesis and aggressiveness. EMT extensively contributes to promoting of tumor cell invasion and migration. d Hypoxia up-regulates CAFs that produce the excessive altered ECM, which supports tumor growth and metastasis. e Tumor hypoxia promotes secretion of cytokines and chemokines that recruit pro-tumor immune cell and suppress anti-tumor response of various types of immune cells. f In response to hypoxia, tumor cells exploit a number of mechanisms including, extrusion of cytotoxic drug by ABC-transporters, exhibiting quiescent state, acquiring metabolic adaptations and displaying stemness features, which can contribute in chemo-, radio- therapy failure. g Hypoxia acts as a niche condition, to accumulate the CSCs enhancing tumorigenesis and resistance. EMT epithelial to mesenchymal transition, CAF cancer-associated fibroblast, ECM extracellular matrix, MDSCs myeloid-derived suppressor cells, TAM tumor-associated macrophage, TAN tumor-associated neutrophil, Treg regulatory T lymphocyte, NK cell natural killer cell, CSC cancer stem cell
Furthermore, vascularization, as an important consequences of HIF signaling, has emerged as a fundamental feature of neoplastic growth, tumor progression and distant metastasis. Excessive blood vessel formation gives the weakly attached tumor cells a greater chance to enter into the circulation and migrate (Fig. 1b) [46, 47]. Thereby, hypoxia triggers the escape of tumor cells from the hostile environment and enhances the invasiveness and metastatic spread [183, 184].
EMT is another process promoted by hypoxia. Tumor cells, which undergo EMT, are reprogramed to have greater mesenchymal features, reduced intercellular attachments and cell-to-cell contacts, increased motility, and conversion to a stem-like phenotype. Thereby, hypoxia-induced EMT increases the aggressiveness and metastatic potential of these cells (Fig. 1c) [84, 85]. Expression of lysyl oxidase (LOX) and lysyl oxidase-like 2 (LOXL2) and HIF-1 accumulation, downregulates E-cadherin and leads to EMT, which contributes to renal, breast and cervical cancer progression and metastasis [185,186,187,188]. HIF-1, also contributes to EMT induction in VHL-null renal cell carcinoma by indirect repression of E-cadherin, mediated by the expression of TCF3, ZFHX1A, and ZFHX1B [189]. Moreover, HIF1-α increases the transcriptional repressor SNA, and downregulates E-cadherin in ovarian carcinoma cells [190]. Kang and colleagues, also showed that the hypoxia-induced EMT is associated with increased CXCR4 expression via of aberrant demethylation of its promoter in lung cancer cell, in which, CXCR4 siRNA inhibits the hypoxia-induced EMT and acquisition of stemness [191].
Moreover, hypoxia has been shown to influence fibroblast reprogramming and upregulate cancer-associated fibroblasts (CAFs) in HIF-1α dependent manner with a metabolic shift towards glycolysis, and that leads to an increase in lactate production. This catabolite is produced by highly glycolytic CAFs and can be used by cancer cells and enhances cancer proliferation, which describes a negative outcome of HIF-1 accumulation in fibroblasts [192, 193]. CAFs share several characteristics with normal fibroblasts that are activated, but they possess oncogenic functions substantially due to production of altered ECM, which supports tumor growth and dissemination (Fig. 1d) [194]. The ECM produced by cancer cells and CAFs in hypoxia, differs from the normoxic ECM and continuously undergo remodeling, which facilitates angiogenesis [195], tumor cell migration and metastatic spread [196, 197].
Hypoxia-induced cancer immunosuppression
By influencing various types of immune cells, hypoxia has been associated with immunosuppression and subsequent tumor progression (Fig. 1e) [198].
The characteristics of the hypoxic tumor microenvironment, are frequently reported to correlate with the accumulation and augmentation of MDSCs. Hypoxic tumor cells can produce CCL26 to attract MDSCs and their homing to the primary tumor [199]. The major feature of these heterogeneous undifferentiated cells, is the exhaustion and suppression of immune cells, which in tumor context leads to evasion from immune surveillance and bypass the blockade of immune checkpoints. One of the underlying mechanism reported in 2017, in which hypoxia/HIF-1α induces ectonucleoside triphosphate diphosphohydrolase 2 (ENTPD2/CD39L1) in cancer cells result in overexpression of extracellular 5′-AMP, which maintains MDSC in undifferentiated and immunosuppressive state in the tumor stroma [200]. However, Corzo et al. [201] reported that HIF-1α mediates, the rapidly differentiation of MDSCs into macrophages with immune-suppressive features upon their arrival at tumor sites. They also described differences between MDSCs in tumor site, contrasted with MDSCs located in peripheral lymphoid organs, that acquire the ability to suppress antigen-nonspecific T cell, as a result of hypoxia induced upregulation of inducible nitric oxide synthase (iNOS) and arginase I, and associated downregulation of both nicotinamide adenine dinucleotide phosphate–oxidase 2(NOX2) and reactive oxygen species (ROS). In addition, hypoxia can enhance MDSCs activities through a HIF1α-dependent mechanism and subsequently elevates miR-210 expression. miR-210 regulates the function of MDSCs by increasing arginase activity and nitric oxide production [202]. Although it is widely accepted that MDSCs have immunosuppressive activity, some studies have found immunostimulatory properties of M1 type MDSCs, compared to the suppressive M2 phenotype [203]. SIRT1 induction and mTOR/ HIF-1α-dependent glycolytic reprogramming, has been found as an underlying mechanism in lineage differentiation of MDSCs into the tumor-suppressing M1 phenotype [204].
Under hypoxic condition, tumor cells promote the secretion of chemoattractive substances, including hypoxia-induced Semaphorin 3A (Sema3A), Endothelial-monocyte-activating polypeptide II (EMAPII), ET-1 and ET-2, which promote recruitment of macrophages [205,206,207]. As hypoxia triggers the switch to glycolysis and increases lactate and H+ production, it can also promote M2 polarization of tumor-associated macrophages [208]. Activated M2 macrophages, in contrast to their classically activate M1 counterparts, have more capacity to induce angiogenesis and tumor progression and metastasis. Besides accumulation of macrophages, hypoxia strongly augments macrophage-mediated T-cell suppression in a HIF-1α dependent manner. Nevertheless, both of HIF1-α and HIF2-α have been shown to be pivotal for macrophage infiltration and immune suppression [209, 210].
Neutrophils infiltrating into the tumor microenvironment, are known as tumor-associated neutrophils (TANs), and are a heterogeneous population including anti-(N1) and pro-tumor (N2) phenotypes [211]. Tumor hypoxia is one of the factors can influence neutrophil plasticity [212]. However, the mechanism by which hypoxia/HIFs affects the N1 and N2-polarization of TANs remains to be clarified. Reciprocally, neutrophils enhance micro-environmental hypoxia by depleting localized oxygen, resulting in upregulation of hypoxia-inducible genes [213]. Hypoxia, through HIF-dependent production of cytokines (IL-8) [214], and chemokines (CXCL1, CXCL2, and CXCL5) [215] can recruit TANs. In addition, hypoxia upregulates the expression of the cell surface adhesion molecule β2 integrin in neutrophils and enhances their function, in a HIF-1α dependent manner [216]. HIF-2α is a critical mediator of neutrophil recruitment to colon tumors and subsequent increase of colon carcinogenesis, by upregulating the potent neutrophil chemokine CXCL1 [217]. Local hypoxia have been shown to promote neutrophil extracellular traps (NETs) [218], which consist of expelled DNA and various proteins such as neutrophil elastase (NE). NETs promote angiogenesis, cancer progression and metastasis [219,220,221]. Moreover, TGF-β, as a known target of HIF-1, reported to induces a pro-tumor N2 phenotype of TANs [222]. It is appear that hypoxia causes a shift of N1 toward N2 TANs, which supports tumor progression and metastasis [212].
The metabolic competition between tumor cell and infiltrating lymphocytes, leads to a limitation of glycolysis in tumor-infiltrating T cells [223,224,225], hypoxia can suppress the anti-tumor activities of T cells through the other mechanisms mediated by HIF. Regulatory T-cell (Treg) repress the anti-tumor responses and addressed as an important limitation of cancer immunotherapy [226, 227]. Tumor cells under hypoxic conditions, upregulate the expression of chemokines and cytokines, such as CC-chemokine ligand 28 (CCL28) and VEGF, which attract Tregs (CD4 + CD25 + FoxP3 + nTreg) to suppress tumor-reactive T cells and promote angiogenesis [228,229,230,231]. Hypoxia induces FoxP3 and promotes the differentiation of Tregs (iTregs) from naive T cells through T-cell intrinsic HIF-1α pathway [232]. Indeed, hypoxia is considered to be an indicator of the inflamed microenvironment, and an increase the proportion of Tregs is an anti-inflammatory mechanisms to restrict the detrimental effects of inflammatory hypoxia [233]. In contrast, there is emerging evidence that shows that HIF-1α possesses a deleterious effect in suppressive activity and stability of Tregs by degradation of FoxP3, and implicates a role for HIF-1α in development and function of Tregs [234, 235].
Another mechanism by which hypoxia represses the anti-tumor response involves the modulation of immune checkpoints. HIF1-α, and occasionally HIF2-α, upregulates the immune inhibitory molecule programmed cell death ligand-1 (PD-L1; also termed B7-H1) in hypoxic-tumor cells, macrophages and MDSCs [236,237,238,239]. Furthermore, HIF-1α enhances the expression of inhibitory receptors including programmed cell death 1 (PDCD1; also termed PD-1), lymphocyte activating gene 3 (LAG3, also termed CD223) and CTLA-4 in CD8+ T cells [240, 241]. Hence, hypoxia promotes T cell exhaustion and tumor resistance to CTL-mediated lysis.
In contrast to what is described above, a potential adverse effect of hypoxia on tumor-reactive T cells, has been shown; in respect of the stimulatory role mediated by HIF1-α and HIF-2α in CTL proliferation and function [242]. Mohapatra et al. found that in glioblastoma (GBM) [243] there was a downregulation of immunosuppressive enzyme tryptophan-2,3-dioxygenase (TDO2) involved in tryptophan (Trp) catabolism, in a HIF1α-dependent manner, with increased T cell proliferation. While, T cell proliferation is inhibited by TDO2-expressing GBM cells under normoxia. Its assumed that tumor cells downregulate TDO2 to conserve Trp through HIF1-α in a nutrient-deficient hypoxic microenvironment. Consistent with this, Tyrakis et al. [244] were able to show an enhancement of proliferation, survival and anti-tumor capacity of CD8+ T cells by hypoxic induction of 2-hydroxyglutarate through the HIF-1α dependent fashion. Moreover, hypoxic CTLs exhibited higher intrinsic cytotoxic capacity and improved function in tumor regression compared to normoxic CTLs [245]. However, hypoxia was shown to negatively regulate the interplay between NK cells and tumor cells. In hypoxia HIF-1α upregulates the metalloproteinase ADAM10 that leads to shedding of the NK cell-activating ligand, MICA, from the surface of tumor cells, results in resistance to cytotoxic killing by NK cell. Mechanism of this NKG2DL shedding involves impaired nitric oxide (NO) signaling [246, 247]. Thereby hypoxia contributes to escape from innate immunity. In contrast, the supporting role of hypoxia in NK cell priming and activation, in synergism with IL-15, has been reported [248, 249].
Hypoxia-induced cancer resistance
Resistance to conventional treatment is a major obstacle in clinical oncology that lead to cancer relapse. Oxygen deprivation may cause in resistance to ionizing radiation, multiple forms of chemotherapy and photodynamic therapy. Several mechanisms of hypoxia-induced resistance related to cellular adaptations to poor oxygenation and nutrition (Fig. 1f). Hypoxia promotes cell cycle arrest and a quiescence cellular state that reduces the susceptibility to external stress during radiation or chemotherapy, especially therapies targeted at rapidly dividing cells [63]. Hypoxia increases the synthesis of certain proteins in subclones, undergoing selection pressure. Consequently, during clonal selection and genome changes, tumorigenic subpopulations are formed which related to a lack of differentiation, defective senescence and apoptosis, augmented spreading and metastasis can lead to further resistance to therapy [29, 63, 250]. Moreover, hypoxia modulates mitochondrial activity [cell apoptosis and necroptosis, as well as generation of reactive oxygen species (ROS)] and induces mitophagy. Thereby, hypoxia reduces the susceptibility of tumor cell to drug- and radiation-induced apoptosis and ROS formation [251, 252]. Modulation of autophagy and p53 known as another mechanism involved in the hypoxia-induced resistance to chemotherapy, however their molecular pathways remained largely elusive [253, 254].
In addition, loss of oxygen required for the cytotoxic function of the certain chemotherapeutics, orientation of chaotic and malfunctioning blood vessels, and augmentation of metastasis [255], reduction of drug delivery and cellular uptake due to tissue acidosis, overexpression of the multidrug resistance (MDR1) gene [256] and its product P- glycoprotein (drug efflux pump) [257, 258], enhanced production of nucleophilic substances such as glutathione, which compete with the target DNA for alkylation, and upregulated enzymatic repair of DNA, are other possible mechanisms by which hypoxia reduces the responsiveness to chemotherapeutic agents [259].
Vasculogenic mimicry (VM) is a major factor in metastasizing breast cancer and resistance to anti-angiogenic drugs. Hypoxia, EMT and CSC are considered as important factors in the formation of VM. Melatonin is also a hormone derived from amino acids, with many anti-tumor effects. There are numerous antitumor effects of melatonin, but its effect on breast cancer VM formation has not yet been investigated. Therefore, we investigated the impact of melatonin in breast CSCs on VM formation via the EMT cycle under hypoxia conditions. We evaluated the impact of melatonin on the EMT markers expression. As a CSC marker in the MDA-MB-231 cell line, CD44 + CD24-phenotype was 80.8 percent whereas in the MCF-7 cell line it was 11.1 percent. The expression of HIF-1α in the VM-positive breast cancer cell line MDA-MB-231 was up-regulated and thus influenced the expression of the EMT markers E-cadherin, vimentin, snail and MMP9. Melatonin in breast CSCs had major effects on EMT and VM formations. Melatonin may hinder VM formation by influencing the key molecules taking part in VM structure and the EMT formation. In addition, our results demonstrate obviously that melatonin is a hormone with important anti-cancer activity. It may probably improve breast cancer management via overcome anti-angiogenic drug resistance [260].
Notwithstanding, these mechanisms that are principally mediated by the HIF-1, the roles of HIF-2 in resistant to anticancer therapy is recently reported, including its roles in affecting HIF-induced autophagy and hampering p53-mediated apoptosis [261, 262].
Recent evidence also suggests that resistance is largely linked to the function of CSCs [166]. As previously described, hypoxic areas within the TME provide a niche for development and accumulation of CSCs, which are poorly differentiated and more invasive, enhancing tumorigenesis and resistance to chemo-, radio- and immuno-therapy (Fig. 1g).
Strategies to re-engineer the tumor microenvironment for treatment
Hypoxia is a major feature of solid tumors and an important impediment to conventional cancer therapy. Identification of the predominant cellular and molecular mechanisms in hypoxic TME presents the first step to design of effective anti-cancer strategies in the context of solid tumors.
Targeting HIFs as a therapeutic strategy
Given that HIF proteins are the master regulators of oxygen homeostasis in hypoxia, targeting HIFs is an attractive strategy in the treatment of tumors. Several approaches for targeting hypoxia and HIF may be achieved by exploiting; (1) hypoxia-activated prodrugs (HAPs) or drug; (2) specific targeting of HIFs; (3) targeting of downstream HIF signaling pathways and important pathways in hypoxic cells (such as mTOR and UPR).
HAPs, which also known as bioreductive alkylating agents, can directly or indirectly regulate HIFs. HAPs are inactive compounds that can be activated to cytotoxic drugs in hypoxic cells or tissues, spontaneously or via one/two electron oxidoreductases [263]. Several HAPs, including PR-104, Evofosfamide (TH-302), and apaziquone (EO9), have undergone preclinical study and clinical development. However the result of clinical trials showed some disappointments and thus far there is no FDA approved HAP [264]. Fortunately, promising progress has been reported in phase II clinical trial on TH-302 in combination with gemcitabine for pancreatic cancer [265], and with adriamycin or doxorubicin for soft tissue sarcoma [266], and phase III studies are underway. Furthermore, TH-302 sensitizes prostate cancer to immunotherapy with checkpoint blockades CTLA-4 and PD-1. Combination therapy with this hypoxia-prodrug and checkpoint blockade drive a more influx of T cells into hypoxic zones and reduce MDSC and granulocytic subsets in tumor environment [267].
The other approaches for overcoming hypoxia, involve direct or indirect targeting of HIF and targeting of downstream HIF signaling pathways. The agent exploited to inhibit the HIF response to hypoxia include inhibitor of HIF-1α mRNA expression (such as antisense oligonucleotide EZN-2968), HIF-1α protein translation (including inhibitors of topoisomerase I/II, receptor tyrosine kinase, cyclin-dependent kinase, oncogenic pathways, thioredoxin reductase, activators of p53 and microtubule disrupting agents), HIF-1α protein degradation (including Hsp90 inhibitors such as 17-AAG and 17-DMAG), HIF-1α DNA binding (such as doxorubicin and daunorubicin) and HIF-1α transcriptional activity (Bortezomib (PS-341) and chetomin) [268]. These inhibitors have been described in detail in several comprehensive reviews [18, 268]. Here we will summarize the strategies targeting the main pathways involved in hypoxia in tumor environment.
Targeting angiogenesis as a therapeutic strategy
One good example of targeting gene products at downstream HIF signaling, is anti-VEGF therapeutic strategy. Anti-angiogenic approaches including monoclonal antibodies (mAb) targeting VEGF or small-molecule inhibitors targeting VEGF receptors can obviate the deleterious effects of angiogenesis in TME favoring tumor growth [269].
Bevacizumab (avastin) is a humanized anti-VEGF IgG1 mAb that has been approved for numerous recurrent and metastatic cancer. Ramucirumab is the anti-VEGFR-2 IgG1 mAb and approved for the treatment of advanced and metastatic several types of cancer, including stomach, colorectal and non-small cell lung carcinoma (NSCLC) [269]. Another anti-angiogenic approach has been achieved through targeting Angiopoietin-1 or 2 (Ang-1,2), using Trebananib. Angiopoietin displays broad expression in the remodeling vasculature of tumors and binds to its receptor, Tie-2. Trebananib is a “peptibody” madeas an antibody and peptide-Fc fusion protein that impairs the interaction between Ang-1,2and Tie-2, leading to the suppression of angiogenesis and tumor growth [270, 271].
Over the last few years, several small-molecule kinase inhibitors have been developed for treatment of different cancers. For instance, sorafenib, regorafenib, lenvatinib, nintedanib, sunitinib, cabozantinib and pazopanib that can inhibit several protein kinases including VEGF receptor (VEGFR), approved by the FDA for treatment of different cancers and as adjuvant for cancer chemotherapy. In addition, 1,2-disubstituted benzimidazoles, the newly synthesized compounds exhibits promising cytotoxic and VEGFR-2 inhibitory [272].
Despite the reported clinical benefits, anti-angiogenic therapies have been not shown to be always effective. Hypoxia induced in response to reduced perfusion during anti-VEGF treatment promotes a greater dependence on hypoxia adaptations, in particular, mediated by HIF1 and HIF2, the unfolded protein response (UPR) and ATF4 [269, 273]. For example, anti-angiogenic therapy promotes metabolic changes through HIF-1 expression, in turn increases lactic acid and carbonic acids production. Therapy against VEGF, also, can promote the inherent selection of tumor cells, which adapt to more hypoxic conditions. Furthermore, exaggerated hypoxia resulted following anti-VEGF treatment which favored a sustained CSC phenotype, and which in turn may contribute to tumor maintenance and resistance to therapies [274]. Hence, an effective anti-angiogenic therapy may be achieved in combination with inhibitors of tumor hypoxic adaptation.
Targeting hypoxia-induced metabolic changes as a therapeutic strategy
The accumulation of lactate in tumors results in reduced intracellular pH (pHi). Moreover, tumor cells in response to hypoxia, upregulate carbonic anhydrases and the production of CO2, which contributes to cellular acidification [275]. To counteract acidification, hypoxic tumor cells upregulate a number of membrane transporters, exchangers and pumps and release the lactic acid into extracellular space. Further, they upregulate extracellular carbonic anhydrases (CAs) catalyzing the hydration of CO2 to bicarbonate, which pumped in and in turn increases the pHi and acidifies the extracellular pH (pHe) [276]. The other important transporters, involved in the export of proton from cells, include the sodium hydrogen exchanger 1 (NHE1) and monocarboxylic acid transporters (MCTs) [277, 278]. Also, ion channels such as transporters, exchanger, pumps and voltage gated sodium channels, endow the tumor with the proliferative, invasive and metastatic ability [279]. These channels modulate tumor cell survival, proliferation, resistance to apoptosis, cell adhesion, motility and extracellular matrix invasion [280, 281]. Given that the hypoxic tumor is dependent on glycolysis and pHi-regulating systems, ion channels have been recently proposed as a potential target for selective therapeutics. The strategy of ion channel blockades accompanies maintaining the low intracellular pH in malignant cells, which induce acid-mediated metabolic collapse following by apoptosis or necrosis [282, 283]. For instance, targeting of NHE1 recently reported to be effective in the treatment of glioblastomas, as highly glycolytic and strongly pH-dependent malignancies [284, 285]. It has also been shown that proton pump inhibitors (PPI, V-ATPase blocker) increase the uptake and effect of cytotoxic drugs in chemo-resistant epithelial ovarian cancer [286]. Furthermore, MCTs (in particular, MCT-4, as hypoxia-inducible isoform and MCT-1) and CAs (in particular, CAIX and CAXII) have been offered the promising therapeutic targets for various cancer types, and recently, a large variety of inhibitors that target their different isoforms are being tested [277, 287]. Additionally, targeting of CAIX emerged as attractive strategy to eliminating CSCs in hypoxia [288, 289].
Targeting hypoxia-induced metabolic changes to improve the efficacy of immunotherapy
A relatively low pH is a hallmark of solid tumor environments, with pH 6.0–6.5, compared to pH 7.5 present in normal environments [290]. High acidity associated with solid tumors acts as a barrier for immune-based therapies such as checkpoint inhibitors or adoptive T-cell transfer [291]. This could, in part, be due to the adverse effect of acidity on different immune cells. Acidity leads to a reduced lifespan of CD8+ memory T cells [292], raise the activation threshold of T cells and modulate the activity of T cells by up-regulating the immune checkpoints such as CTLA-4 [293]. High extracellular lactate can induce a tolerogenic phenotype of dendritic cells, characterized by reduced IL-12 and increased IL-10 production in response to TLR stimulation, impaired migratory response to chemokines and defective metabolism [294]. Chronic long-term exposure to acidic milieu of tumor, also, impairs NK cell activation, function and survival [293]. On the other hand, tumor acidity recruits MDSCs [294]. There is also evidence suggesting that low a pH decreases T cell infiltration and their homing into the TME.
Recently, Thomas and coworkers [295], examine the effect of pH buffering and neutralizing tumor acidity by oral bicarbonate administration, on anti-tumor responses to checkpoint immunotherapyand observed the increase of anti-tumor immunity in multiple cancer modelsOf note, acidity-reversing drugs appear to be artificially raised the pH of tumor vasculature, allowing to increase T cell homing at this site. In addition, pH gradient created between intracellular and extracellular environments affects the drug absorption and metabolism, also suppresses cytoplasmic retention of cytotoxic anticancer agents [296], and thereby facilitates the acquired drug resistance.
Strategies to limit hypoxia-induced radio- and chemo-resistance
Recent studies show that a combination of supplemental oxygen therapy with cytotoxic drug or radiation therapy enhanced their effectiveness [297]. Anti-cancer drugs mostly kill cells in an oxygen-dependent manner and require oxygen for maximal activity. Platinum based chemotherapeutic agents produced free radicals in tumor cells, which killed them by capturing electrons and delivered them to oxygen [298]. Moreover, many of these drugs have a large molecular weight, which makes their distribution difficult. This can be exaggerated in abnormal vascular network in hypoxic area within the solid tumors [299]. Hence, drug availability decreases to the levels less than the lethal dose [300]. In addition to this, upregulation of hypoxia-inducible genes involves in chemo-resistance. HIF-1 target hypoxia response elements (HREs) have been found in genes encoding members of the ABC transporters such as MDR1 and BCRP, which their products actively extrude cytotoxic drug out of tumor cells [300, 301]. Hypoxia, also triggers the inhibition of DNA damage and decreased tumor cell senescence particularly in a HIF-1 dependent fashion. For instance, hypoxia inhibits etoposide-induced DNA damage [301]. Cell cycle regulation is an important determinant of tumor resistance [302]. Hypoxic tumor cells, especially being distant from blood supply, have downregulated cell cycle, which protects them against a variety of chemotherapeutic drugs targeted cellular DNA of dividing cells. Such cells also promote drug resistance by altering metabolism and create acidic conditions as previously described [303]. Furthermore, hypoxia, considered as a main driver of autophagy, which have been accompanied with anti-cancer therapeutic resistance. During autophagy, damaged cellular components degraded and tumor cell protected against apoptosis induced by chemotherapy and radiotherapy [304, 305].
Radiation therapy causes cell death by inducing DNA damage, which in the presence of oxygen leads to the generation of free radicals, failure to repair the damage and therefore becomes irreversible. While in hypoxic conditions, the ability of DNA repair increased, results in cell survival and remaining subpopulations responsible for poor outcome [306]. Evidence, also suggested that hypoxia might protect the CSCs to escape from lethal effects of radiotherapy [303]. In addition, radiation can induce transient oxygen fluctuation within the tumor, which leads to ROS generation and HIF-1 expression that in turn promote production of cytokines, VEGF and basic fibroblast growth factor (bFGF). They can eventually, prevent endothelial apoptosis, which provide an additional mechanism for radio-resistance [307]. Several strategies have been exploited to limit hypoxia-induced radio-resistance, such as increase oxygen availability through enhancement of blood flow, mimicking oxygen and targeting hypoxic tumor cells [301].
Modifying the exosome content in hypoxic tumor microenvironment
Hypoxia triggers exosomes secretion by tumor cells, however, increased exosomes secretion under hypoxic conditions is not a particular feature of tumor microenvironment. Exosomes can change the phenotype of adjacent normal cells and other cells in the tumor microenvironment as well as distant cells through systemic circulation promoting the formation of distant premetastatic niches [308]. Several studies have shown increased amount of special exosome secretion in lung, glioblastoma, prostate cancer, ovarian cancer and breast cancer cell lines through HIF-1α in hypoxic tumor environment [309]. Moreover, it has been shown that hypoxia changed the size of exosomes in pancreatic cancer cell lines [310]. The capability of exosomes to facilitate intercellular communication and their ability to transport various exogenous cargo results in tumor survival, aggressiveness angiogenesis and metastasis. Modifying the content and biogenesis of exosomes in hypoxic tumor microenvironment may be an effective therapeutic intervention approach. Biological feature of exosomes, including their stability, small size, lack of toxicity, communication with other cells, slow clearance from circulation and cargo loading capacity make them an attractive tool for the delivery of therapeutic molecules [309]. An important therapeutic intervention strategy may be to alter the content and biogenesis of exosomes in a hypoxic tumor microenvironnement. The biological characteristics of exosomes such as their stability, tiny size, non-toxicity, interaction with other cells, slow removal of cargo loading capability and circulation, make them an excellent factor for the providing therapeutic molecules [309].
Treatments of cancer emphasize microenvironment hypoxia in cancer stem cells
CSCs endowed with stemness and tumorigenic properties allow tumor development, metastasis and recurrence. Conventional anticancer approaches mainly target the bulk population of the tumor, whilst sparing CSCs. Moreover, surgery-generated hypoxia is also reported to result in dedifferentiation of tumor cells into tumor-initiating stem-like cells [311]. Therefore, a number of therapeutic approaches in order to kill CSCs have been developed based on altering the microenvironment (niches) protecting them.
In this regard, disruption of vasculature, targeting metabolism and special pH environment represent as alluring landscapes, which can be affected by hypoxia. The strategies directed to target VEGF can lead to interrupt the CSC niche. Several studies showed that bevacizumab significantly reduces the GCSCs in glioblastoma models [312, 313]. A combination of a VEGFR2 antibody with chemotherapy reported by Folkins and coworkers, to be more effective against glioma than chemotherapy alone [314].
Inhibiting the enzymatic pathways and lactic acid generation, as the main part of reprogrammed metabolic network, also presents promising approaches to CSCs elimination. Cui et al. [315], indicated that chronic stress via β2-adrenergic receptor upregulated the LDH-A, leading to a switch to lactate formation, in turn promoted stem cell phenotype through USP28/MYC/SLUG axis in breast cancer. And that vitamin C reversed the induction of stem-like phenotype by inhibition of stress-induced LDH-A, and suppressing the lactic acid generation and the USP28/MYC/SLUG pathway in BCSCs. Further, combining of vitamin C, as inhibitor of glycolysis, with the FDA-approved antibiotic doxycycline that reduces cellular respiration, reported to be effective for eradicating CSCs [316].
Mesenchymal CSCs are highly resistant and aggressive subpopulation of GCSCs, which can be resisted and even upregulated after radiation treatment. This subtype of CSCs overexpress ALDH1A3, thus inhibition of ALDH-mediated pathways could be effective in eradication of them [317]. Zhou et al. [318], showed that combining of chemotherapy, together with inhibition of glycolysis by 3-bromopyruvate, effectively eradicates GCSCs in their hypoxic niches, where they exhibit resistant to mono-therapy by chemotherapeutic agents, and tend to reside in hypoxia and perform glycolysis for ATP generation in order to maintain their stemness and highly tumor forming capacity. In addition, in several cancer models, inhibition of PDKII by dichloroacetate has been demonstrated to reverse the metabolic shift from glycolysis to OXPHOS, increase ROS and promote apoptosis in CSCs and tumor cells [319, 320].
Elimination of the stemness characteristics, such as overexpressed drug transporters, considered as the major purpose to improve efficacy of chemotherapy. The combination therapy consists of inhibitors of HIFα or HIF target gene (such as ABC transporters) suggested using concomitantly with chemotherapeutic agents. For instance, anti-MDR1 siRNA (siMDR1) successfully improved the chemo-sensitivity of human colon CSCs [321]. Several tyrosine kinase inhibitors such as imatinib, erlotinib, nilotinib and lapatinib have been applied to inhibit ABC transporters [322]. In addition, various strategies based on suppression of transporter function, including nanoparticle-mediated delivery of inhibitors, competitive and allosteric modulators, regulator of transcriptional and signaling pathways involving ABC transporters have been tested to overcome chemo-resistance in CSCs [323], however, none of them has been approved yet.
In hypoxiamediated CSC resistance, several signaling pathways recognized to be involved. Therefore, these pathways draw much attention as potential targets to eliminate CSCs, particularly in hypoxic TME. Hypoxia promotes Notch and Wnt/β-catenin signaling to CSC formation and maintenance, mainly in a HIF-1α-dependent manner [324]. Targeting Notch4 could decrease the number and activity of BCSC in vivo, as well as in vitro [325]. Zhou and coworkers [326], recently showed that Notch4 promotes EMT and quiescence in mesenchymal BCSC via activation of SLUG and GAS1, suggesting Notch4-SLUG-GAS1 serves as a candidate for tumor treatment by elimination of mesenchymal BCSC stemness and overcoming the lethal form of chemo-resistant and metastatic triple-negative breast cancer. Seo and colleagues [327], further showed that hypoxia-induced Notch signaling increases self-renewal, drug resistance, sphere formation and expression of genes relating to CSC features, such as SOX2, ALDH, and ABC transporters in ovarian CSCs (OCSCs). In fact, Notch signaling mediates the hypoxia-induced expression of Sox2 in a HIF-1 dependent manner, and Sox2 in turn upregulates the ABCB1 and ABCG2, thereby promoting drug resistance, as well as triggering sphere formation and CSCs features. They also showed that the inhibition of Sox2 in a HIF-1 abrogates hypoxia-induced CSC features. Their finding proposed the hypoxia- Notch1-SOX2 circuit as a potential target to eradicate OCSCs in hypoxic condition. Moreover, suppression of MMP-2, 9 and VEGF abrogates Notch signaling in hepatocellular carcinoma cells and decreases tumor invasiveness [328]. Hypoxia triggers phenotypic plasticity of CSCs by activation of Wnt signaling. Yan et al. [329], also indicated that HIF-1α expression increased during acute hypoxia (6–12 h), whereas, HIF-2α overexpression continuously occurred in chronic hypoxia (48 h) and activated Wnt and Notch signaling and expression of stem cell markers Nanog, c-Myc, and Oct4. Thereby, HIF-2α promoted stem phenotype conversion, augmented tumorigenesis and induced resistance to chemotherapeutic drug paclitaxel. Hypoxia, also, upregulates β-catenin transcription, downstream of Wnt, via stabilization of HIF-1α in leukemia CSCs, and promotes their survival [330]. Different drugs aimed at inhibiting the Wnt signaling pathway have been used to impede this pathway in CSCs [328, 331]. Evodiamine (Evo), an inhibitor of the Wnt signaling, demonstrated that downregulated the expression of Sox2, KLF4, Bmi1 and Oct4 in GCCs, thus promoted apoptosis and decreased proliferation, sphere formation capacity and resistance to oxaliplatin. Evo, also, downregulated the expression of Slug, Twist, Zeb1 and vimentin, and thereby acquired the inhibitory effect on EMT. Further, Evo reduced cMyc, cyclin D1, as well as βcatenin expression in spheroids from GCCs in gastric cancer [332]. Trifluoperazine is another inhibitor of the Wnt/β-catenin pathway with potential anti-CSC properties, which suppressed the CSC marker (CD44/CD133) expression and spheroid formation capacity of LCSCs. Combining of this inhibitor with gefitinib or cisplatin diminished chemo-resistance of lung cancer [333]. Natural products have been also identified by similar effect. Curcumin inhibits β-catenin nuclear localization, hampers the Slug activation and reverses suppressed E-cadherin expression, subsequently inhibits EMT and migration of BCSCs [334]. Cucurbitacin B, inhibitor of Wnt/β-catenin signaling derived from pumpkins and guards, inhibits stemness and metastasis of non-small cell lung cancer (NSCLC). It has also the anti-angiogenic and anti-invasive potential against metastatic NSCLC [335].
Hedgehog (Hh) signaling, one of the main pathways related to stemness and CSC development, interacts with other critical molecular pathways, in particular Ras/Raf/MEK/Erk, PI3K/Akt/mTOR and Notch. Hence, combined targeting of the component belonged to different signaling pathways result in more effective anti-cancer strategies [336]. Mitogen-activated protein kinase (MAPK)/ERK signaling is one of the key pathways exploited by hypoxia to promote CSC phenotype. In response to chemotherapy, HIF promotes propagation of BCSCs and thereby tumor recurrence. One of the mechanisms proposed is activation of cystine transporter xCT and the glutamate-cysteine ligase by HIF-1α that leads to increased intracellular glutathione, which in turn inhibits mitogen-activated protein kinase MEK activity. Loss of MEK-ERK signaling causes FoxO3-mediated transcriptional activation of Nanog, a pluripotency factor required for propagation of BCSCs. Targeting this HIF-1-regulated pathway might inhibit the BCSC enrichment and tumor relapse after chemotherapy [337].
PI3K/Akt signaling is the other important pathway mediating CSC resistance. It is indicated that ERK1/2 and PI3K/Akt pathways act at downstream HIF-1α signaling in response of GCSCs to hypoxia, and that inhibition of these pathways abrogate propagation of CD133-expressing GCSCs [73]. Recent finding implicated Akt/Notch1 signaling cascade as promoter of stemness and pancreatic CSCs (PCSCs)-associated resistance, which exacerbated in collaborate with hypoxia. Blockade of this pathway augmented the cytotoxic effect of gemcitabine [338]. In hypoxic GCSCs, HIF2-α through activation of Akt and Erk1/2 pathways, upregulates prostatic acid phosphatase (PAP) to produce adenosine, which binds to adenosine receptor A2B, thereby increases proliferation and tumorigenic capacity [339]. Recently, it is demonstrated that celastrol, an anti-glioma medicine, downregulated the HIF-1α, blocked the PI3K/Akt/mTOR signaling and disrupted angiogenesis and VM formation. [340]. mTOR, a downstream mediator in PI3K/AKT pathway, complicatedly regulated by HIF-1α signaling and acts as a nutrient/hypoxia sensor to modulate protein synthesis. Marhold et al. [341], identified that mTOR was deactivated in response to HIF1α upregulation, and inhibits proliferation, but interestingly promotes quiescence and survival of PCSCs in the hypoxic niche. Its possible mechanism involves the activation of Akt signaling through mTOR/S6K/IRS-1 feedback loop. This might be an explanation for the failure of selective mTOR inhibitors in clinical trials. Altogether, given the complex regulation of the molecular pathways and their interactions in response to HIFs in CSCs, we found that targeting of several signaling molecule of these pathways provides more efficient approaches to overcome CSCs-associated resistance in hypoxia.
Conclusion and future prospectus
While hypoxia has been emerged as a key player in allowing tumor survival, dissemination and invasiveness, this review summarizes the significance of HIFs in CSC development, malignant progression and cancer resistance to chemo-, radio- and immuno-therapy. As a result, HIF stabilization in hypoxic tumor cells induces the expression of specific target genes encoding proteins that promote neo-angiogenesis (VEGF), metabolic changes (glycolytic enzymes and glucose transporters), stemness, EMT and metastasis (CXCR4, E-cadherin). Further, tumor hypoxia is thought to promote the production of cytokines and chemokines, which recruit pro-tumor immune cell and diminish tumor immune responses. Therefore, better understanding of the hypoxia signaling cascade can open new windows to design strategies for targeting HIFs and management of hypoxic microenvironment, led to (i) limit tumor expansion; (ii) sensitize CSCs; and (iii) overcome tumor resistance and recurrence.
Abbreviations
- ABC:
-
ATP-binding cassette transporter
- BCSCs:
-
Breast cancer stem cells
- bFGF:
-
Basic fibroblast growth factor
- BMDCs:
-
Bone-marrow derived cells
- BMI1:
-
Polycomb complex protein BMI-1
- CAs:
-
Carbonic anhydrases
- CAIX:
-
Carbonic anhydrase 9
- CCL28:
-
CC-chemokine ligand 28
- CTL:
-
Cytotoxic T, lymphocytes
- CXCR4:
-
C–X–C chemokine receptor type 4
- ECM:
-
Extracellular matrix
- EGF:
-
Epidermal growth factor
- EMAPII:
-
Endothelial-monocyte-activating polypeptide II
- EMT:
-
Epithelial–mesenchymal transition
- FGF2:
-
Fibroblast growth factor 2
- GBM:
-
Glioblastoma
- GLUT1:
-
Glucose transporter1
- Hh:
-
Hedgehog
- HAPs:
-
Hypoxia-activated prodrugs
- HIF1:
-
Hypoxia-inducible factor 1
- IGF-2:
-
Insulin-like growth factor-2
- iNOS:
-
Inducible nitric oxide synthase
- JAK/STAT:
-
Janus-activated kinase/signal transducer
- KLF4:
-
Krupper-like factor 4
- LDH-A:
-
Lactate dehydrogenase A
- LOX:
-
Lysyl oxidase
- MDR1:
-
Multidrug resistance 1 receptor
- MDSCs:
-
Myeloid-derived suppressor cells
- miRNA:
-
Micro RNA
- MMP:
-
Matrix metalloproteinases
- Myc:
-
Myelocytomatosis oncogene product
- NANOG:
-
Tir nan Og
- NE:
-
Neutrophil elastase
- NETs:
-
Neutrophil extracellular traps
- NF-kB:
-
Nuclear factor-kB
- OCT4:
-
Octamer-binding transcription factor
- p53:
-
Protein 53
- PAI-1:
-
Plasminogen activator inhibitor-1
- PDCD1:
-
Programmed cell death 1
- PDGF:
-
Platelet-derived growth factor
- PDK1:
-
Pyruvate dehydrogenase kinase 1
- PD-L1:
-
Programmed cell death ligand-1
- PI3K/PTEN:
-
Phosphatidylinositol 3-kinase/phosphatase, tensin homolog
- ROS:
-
Reactive oxygen species
- SOX2:
-
Sex determining region Y HMG-box 2
- TANs:
-
Tumor-associated neutrophils
- TGF-β:
-
Transforming growth factor beta
- TME:
-
Tumor microenvironment
- Tregs:
-
Regulatory T cells
- TSPs:
-
Thrombospondins
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
- Wnt:
-
Wingless
- ZEB1:
-
Zinc-finger E-box binding homeobox 1
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Balkwill FR, Capasso M, Hagemann T. The tumor microenvironment at a glance. J Cell Sci. 2012;125(Pt 23):5591–6. https://doi.org/10.1242/jcs.116392.
Folkman J. What is the evidence that tumors are angiogenesis dependent? JNCI J Natl Cancer Inst. 1990;82(1):4–7.
Vaupel P, Kallinowski F, Okunieff P. Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: a review. Cancer Res. 1989;49(23):6449–65.
Erler JT, Cawthorne CJ, Williams KJ, Koritzinsky M, Wouters BG, Wilson C, et al. Hypoxia-mediated down-regulation of Bid and Bax in tumors occurs via hypoxia-inducible factor 1-dependent and-independent mechanisms and contributes to drug resistance. Mol Cell Biol. 2004;24(7):2875–89.
Rouschop KM, Van Den Beucken T, Dubois L, Niessen H, Bussink J, Savelkouls K, et al. The unfolded protein response protects human tumor cells during hypoxia through regulation of the autophagy genes MAP1LC3B and ATG5. J Clin Investig. 2010;120(1):127–41.
Pennacchietti S, Michieli P, Galluzzo M, Mazzone M, Giordano S, Comoglio PM. Hypoxia promotes invasive growth by transcriptional activation of the met protooncogene. Cancer Cell. 2003;3(4):347–61.
Hill RP, Marie-Egyptienne DT, Hedley DW. Cancer stem cells, hypoxia and metastasis. Semin Radiat Oncol. 2009;19(2):106–11. https://doi.org/10.1016/j.semradonc.2008.12.002.
Goldmann E. The growth of malignant disease in man and the lower animals, with special reference to the vascular system. Thousand Oaks: SAGE Publications; 1908.
Kioi M, Vogel H, Schultz G, Hoffman RM, Harsh GR, Brown JM. Inhibition of vasculogenesis, but not angiogenesis, prevents the recurrence of glioblastoma after irradiation in mice. J Clin Investig. 2010;120(3):694–705.
Muz B, de la Puente P, Azab F, Azab AK. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia. 2015;3:83.
Al Tameemi W, Dale TP, Al-Jumaily RMK, Forsyth NR. Hypoxia-modified cancer cell metabolism. Frontiers in cell and developmental biology. 2019;7:4.
Cairns RA, Harris IS, Mak TW. Regulation of cancer cell metabolism. Nat Rev Cancer. 2011;11(2):85–95. https://doi.org/10.1038/nrc2981.
Guzy RD, Hoyos B, Robin E, Chen H, Liu L, Mansfield KD, et al. Mitochondrial complex III is required for hypoxia-induced ROS production and cellular oxygen sensing. Cell Metabol. 2005;1(6):401–8.
Bristow RG, Hill RP. Hypoxia and metabolism: hypoxia, DNA repair and genetic instability. Nat Rev Cancer. 2008;8(3):180.
Yotnda P, Wu D, Swanson AM. Hypoxic tumors and their effect on immune cells and cancer therapy. Immunotherapy of Cancer. Berlin: Springer; 2010. p. 1–29.
Yotnda P, Wu D, Swanson AM. Hypoxic tumors and their effect on immune cells and cancer therapy. Methods Mol Biol (Clifton NJ). 2010;651:1–29. https://doi.org/10.1007/978-1-60761-786-0_1.
Wigerup C, Påhlman S, Bexell D. Therapeutic targeting of hypoxia and hypoxia-inducible factors in cancer. Pharmacol Ther. 2016;164:152–69. https://doi.org/10.1016/j.pharmthera.2016.04.009.
Semenza GL. Hypoxia-inducible factor 1 (HIF-1) pathway. Sci STKE. 2007;2007(407):cm8. https://doi.org/10.1126/stke.4072007cm8.
Vaupel P, Harrison L. Tumor hypoxia: causative factors, compensatory mechanisms, and cellular response. Oncologist. 2004;9:4–9. https://doi.org/10.1634/theoncologist.9-90005-4.
Carmeliet P, Dor Y, Herbert J-M, Fukumura D, Brusselmans K, Dewerchin M, et al. Role of HIF-1α in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature. 1998;394(6692):485.
Wang GL, Jiang B-H, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci. 1995;92(12):5510–4.
Ohh M, Park CW, Ivan M, Hoffman MA, Kim T-Y, Huang LE, et al. Ubiquitination of hypoxia-inducible factor requires direct binding to the β-domain of the von Hippel–Lindau protein. Nat Cell Biol. 2000;2(7):423.
Jaakkola P, Mole DR, Tian Y-M, Wilson MI, Gielbert J, Gaskell SJ, et al. Targeting of HIF-α to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292(5516):468–72.
Maxwell PH, Pugh CW, Ratcliffe PJ. Activation of the HIF pathway in cancer. Curr Opin Genet Dev. 2001;11(3):293–9.
Holmquist-Mengelbier L, Fredlund E, Löfstedt T, Noguera R, Navarro S, Nilsson H, et al. Recruitment of HIF-1α and HIF-2α to common target genes is differentially regulated in neuroblastoma: HIF-2α promotes an aggressive phenotype. Cancer cell. 2006;10(5):413–23.
Koh MY, Powis G. Passing the baton: the HIF switch. Trends Biochem Sci. 2012;37(9):364–72.
Lloyd MC, Cunningham JJ, Bui MM, Gillies RJ, Brown JS, Gatenby RA. Darwinian dynamics of intratumoral heterogeneity: not solely random mutations but also variable environmental selection forces. Cancer Res. 2016;76(11):3136–44. https://doi.org/10.1158/0008-5472.can-15-2962.
Vaupel P, Thews O, Hoeckel M. Treatment resistance of solid tumors. Med Oncol. 2001;18(4):243–59. https://doi.org/10.1385/MO:18:4.
Jing X, Yang F, Shao C, Wei K, Xie M, Shen H, et al. Role of hypoxia in cancer therapy by regulating the tumor microenvironment. Mol Cancer. 2019;18(1):157. https://doi.org/10.1186/s12943-019-1089-9.
Yeom CJ, Goto Y, Zhu Y, Hiraoka M, Harada H. Microenvironments and cellular characteristics in the micro tumor cords of malignant solid tumors. Int J Mol Sci. 2012;13(11):13949–65. https://doi.org/10.3390/ijms131113949.
Siemann DW. The unique characteristics of tumor vasculature and preclinical evidence for its selective disruption by tumor-vascular disrupting agents. Cancer Treat Rev. 2011;37(1):63–74.
Williams KJ, Cowen RL, Stratford IJ. Hypoxia and oxidative stress in breast cancer Tumour hypoxia–therapeutic considerations. Breast Cancer Res. 2001;3(5):328.
Zölzer F, Streffer C. Increased radiosensitivity with chronic hypoxia in four human tumor cell lines. Int J Radiat Oncol Biol Phys. 2002;54(3):910–20.
Chan N, Koritzinsky M, Zhao H, Bindra R, Glazer PM, Powell S, et al. Chronic hypoxia decreases synthesis of homologous recombination proteins to offset chemoresistance and radioresistance. Cancer Res. 2008;68(2):605–14.
Miao H, Wu N, Luan C, Yang X, Zhang R, Lv N, et al. Quantitation of intestinal Fusobacterium and butyrate- producing bacteria in patients with colorectal adenomas and colorectal cancer. Wei sheng wu xue bao Acta MicrobiolSin. 2014;54(10):1228–34.
Rofstad EK, Gaustad JV, Egeland TA, Mathiesen B, Galappathi K. Tumors exposed to acute cyclic hypoxic stress show enhanced angiogenesis, perfusion and metastatic dissemination. Int J Cancer. 2010;127(7):1535–46.
Bhaskara VK, Mohanam I, Rao JS, Mohanam S. Intermittent hypoxia regulates stem-like characteristics and differentiation of neuroblastoma cells. PLoS ONE. 2012;7(2):e30905.
Martinive P, Defresne F, Bouzin C, Saliez J, Lair F, Grégoire V, et al. Preconditioning of the tumor vasculature and tumor cells by intermittent hypoxia: implications for anticancer therapies. Cancer Res. 2006;66(24):11736–44.
Chen A, Sceneay J, Godde N, Kinwel T, Ham S, Thompson EW. Intermittent hypoxia induces a metastatic phenotype in breast cancer. Oncogene. 2018;37(31):4214–25. https://doi.org/10.1038/s41388-018-0259-3.
Seo BR, DelNero P, Fischbach C. In vitro models of tumor vessels and matrix: engineering approaches to investigate transport limitations and drug delivery in cancer. Adv Drug Deliv Rev. 2014;69:205–16.
Carmeliet P. Angiogenesis in life, disease and medicine. Nature. 2005;438(7070):932.
Wenger RH. Cellular adaptation to hypoxia: O2-sensing protein hydroxylases, hypoxia-inducible transcription factors, and O2-regulated gene expression. FASEB J. 2002;16(10):1151–62.
Less JR, Posner MC, Skalak TC, Wolmark N, Jain RK. Geometric resistance and microvascular network architecture of human colorectal carcinoma. Microcirculation. 1997;4(1):25–33.
Helmlinger G, Yuan F, Dellian M, Jain RK. Interstitial pH and pO 2 gradients in solid tumors in vivo: high-resolution measurements reveal a lack of correlation. Nat Med. 1997;3(2):177.
Hanahan D, Christofori G, Naik P, Arbeit J. Transgenic mouse models of tumour angiogenesis: the angiogenic switch, its molecular controls, and prospects for preclinical therapeutic models. Eur J Cancer. 1996;32(14):2386–93.
Goonewardene T, Sowter H, Harris A. Hypoxia-induced pathways in breast cancer. Microsc Res Tech. 2002;59(1):41–8.
Folkman J, Watson K, Ingber D, Hanahan D. Induction of angiogenesis during the transition from hyperplasia to neoplasia. Nature. 1989;339(6219):58.
Tang N, Wang L, Esko J, Giordano FJ, Huang Y, Gerber HP, et al. Loss of HIF-1alpha in endothelial cells disrupts a hypoxia-driven VEGF autocrine loop necessary for tumorigenesis. Cancer Cell. 2004;6(5):485–95. https://doi.org/10.1016/j.ccr.2004.09.026.
Skuli N, Majmundar AJ, Krock BL, Mesquita RC, Mathew LK, Quinn ZL, et al. Endothelial HIF-2alpha regulates murine pathological angiogenesis and revascularization processes. J Clin Invest. 2012;122(4):1427–43. https://doi.org/10.1172/jci57322.
Skuli N, Liu L, Runge A, Wang T, Yuan L, Patel S, et al. Endothelial deletion of hypoxia-inducible factor-2alpha (HIF-2alpha) alters vascular function and tumor angiogenesis. Blood. 2009;114(2):469–77. https://doi.org/10.1182/blood-2008-12-193581.
Krock BL, Skuli N, Simon MC. Hypoxia-induced angiogenesis: good and evil. Genes Cancer. 2011;2(12):1117–33. https://doi.org/10.1177/1947601911423654.
Wu L, Fu Z, Zhou S, Gong J, Liu CA, Qiao Z, et al. HIF-1α and HIF-2α: siblings in promoting angiogenesis of residual hepatocellular carcinoma after high-intensity focused ultrasound ablation. PLoS ONE. 2014;9(2):e88913-e. https://doi.org/10.1371/journal.pone.0088913.
Skuli N, Liu L, Runge A, Wang T, Yuan L, Patel S, et al. Endothelial deletion of hypoxia-inducible factor-2alpha (HIF-2alpha) alters vascular function and tumor angiogenesis. Blood. 2009;114(2):469–77. https://doi.org/10.1182/blood-2008-12-193581.
Sreepadmanabh M, Toley BJ. Investigations into the cancer stem cell niche using in-vitro 3-D tumor models and microfluidics. Biotechnol Adv. 2018;36(4):1094–110. https://doi.org/10.1016/j.biotechadv.2018.03.009.
Song S, Li Y, Zhang K, Zhang X, Huang Y, Xu M, et al. Cancer stem cells of diffuse large B cell lymphoma are not enriched in the CD45(+)CD19(-) cells but in the ALDH(high) cells. J Cancer. 2020;11(1):142–52. https://doi.org/10.7150/jca.35000.
Karsten U, Goletz S. What makes cancer stem cell markers different? SpringerPlus. 2013;2(1):301. https://doi.org/10.1186/2193-1801-2-301.
Chen W, Dong J, Haiech J, Kilhoffer MC, Zeniou M. Cancer stem cell quiescence and plasticity as major challenges in cancer therapy. Stem Cell Int. 2016;2016:1740936. https://doi.org/10.1155/2016/1740936.
Moore N, Lyle S. Quiescent, slow-cycling stem cell populations in cancer: a review of the evidence and discussion of significance. J Oncol. 2011. https://doi.org/10.1155/2011/396076.
Borovski T, De Sousa EMF, Vermeulen L, Medema JP. Cancer stem cell niche: the place to be. Cancer Res. 2011;71(3):634–9. https://doi.org/10.1158/0008-5472.can-10-3220.
Kubota Y, Takubo K, Suda T. Bone marrow long label-retaining cells reside in the sinusoidal hypoxic niche. Biochem Biophys Res Commun. 2008;366(2):335–9.
Simon MC, Keith B. The role of oxygen availability in embryonic development and stem cell function. Nat Rev Mol Cell Biol. 2008;9(4):285–96. https://doi.org/10.1038/nrm2354.
Das B, Tsuchida R, Malkin D, Koren G, Baruchel S, Yeger H. Hypoxia enhances tumor stemness by increasing the invasive and tumorigenic side population fraction. Stem Cells. 2008;26(7):1818–30. https://doi.org/10.1634/stemcells.2007-0724.
Jogi A, Ora I, Nilsson H, Lindeheim A, Makino Y, Poellinger L, et al. Hypoxia alters gene expression in human neuroblastoma cells toward an immature and neural crest-like phenotype. Proc Natl Acad Sci USA. 2002;99(10):7021–6. https://doi.org/10.1073/pnas.102660199.
Kim H, Lin Q, Glazer PM, Yun Z. The hypoxic tumor microenvironment in vivo selects the cancer stem cell fate of breast cancer cells. Breast Cancer Res. 2018;20(1):16.
Vadde R, Vemula S, Jinka R, Merchant N, Bramhachari PV, Nagaraju GP. Role of hypoxia-inducible factors (HIF) in the maintenance of stemness and malignancy of colorectal cancer. Crit Rev Oncol Hematol. 2017;113:22–7. https://doi.org/10.1016/j.critrevonc.2017.02.025.
Yang L, Shi P, Zhao G, Xu J, Peng W, Zhang J, et al. Targeting cancer stem cell pathways for cancer therapy. Signal Transduct Target Ther. 2020;5(1):8. https://doi.org/10.1038/s41392-020-0110-5.
Mimeault M, Batra SK. Hypoxia-inducing factors as master regulators of stemness properties and altered metabolism of cancer- and metastasis-initiating cells. J Cell Mol Med. 2013;17(1):30–54. https://doi.org/10.1111/jcmm.12004.
Chang WH, Lai AG. Aberrations in Notch-Hedgehog signalling reveal cancer stem cells harbouring conserved oncogenic properties associated with hypoxia and immunoevasion. Br J Cancer. 2019;121:666–6783.
Deng J, Bai X, Feng X, Ni J, Beretov J, Graham P, et al. Inhibition of PI3K/Akt/mTOR signaling pathway alleviates ovarian cancer chemoresistance through reversing epithelial-mesenchymal transition and decreasing cancer stem cell marker expression. BMC Cancer. 2019;19(1):618. https://doi.org/10.1186/s12885-019-5824-9.
Kim JH, Park SY, Jun Y, Kim JY, Nam JS. Roles of Wnt target genes in the journey of cancer stem cells. Int J Mol Sci. 2017. https://doi.org/10.3390/ijms18081604.
Nedaeinia R, Avan A, Manian M, Salehi R, Ghayour-Mobarhan M. EGFR as a potential target for the treatment of pancreatic cancer: dilemma and controversies. Curr Drug Targets. 2014;15(14):1293–301. https://doi.org/10.2174/1389450115666141125123003.
Soeda A, Park M, Lee D, Mintz A, Androutsellis-Theotokis A, McKay RD, et al. Hypoxia promotes expansion of the CD133-positive glioma stem cells through activation of HIF-1alpha. Oncogene. 2009;28(45):3949–59. https://doi.org/10.1038/onc.2009.252.
Yan Y, Liu F, Han L, Zhao L, Chen J, Olopade OI, et al. HIF-2alpha promotes conversion to a stem cell phenotype and induces chemoresistance in breast cancer cells by activating Wnt and Notch pathways. J Exp Clin Cancer Res CR. 2018;37(1):256. https://doi.org/10.1186/s13046-018-0925-x.
Covello KL, Kehler J, Yu H, Gordan JD, Arsham AM, Hu CJ, et al. HIF-2alpha regulates Oct-4: effects of hypoxia on stem cell function, embryonic development, and tumor growth. Genes Dev. 2006;20(5):557–70. https://doi.org/10.1101/gad.1399906.
Gordan JD, Bertout JA, Hu CJ, Diehl JA, Simon MC. HIF-2alpha promotes hypoxic cell proliferation by enhancing c-myc transcriptional activity. Cancer Cell. 2007;11(4):335–47. https://doi.org/10.1016/j.ccr.2007.02.006.
Colwell N, Larion M, Giles AJ, Seldomridge AN, Sizdahkhani S, Gilbert MR, et al. Hypoxia in the glioblastoma microenvironment: shaping the phenotype of cancer stem-like cells. Neurooncology. 2017;19(7):887–96.
Schöning JP, Monteiro M, Gu W. Drug resistance and cancer stem cells: the shared but distinct roles of hypoxia-inducible factors HIF 1α and HIF 2α. Clin Exp Pharmacol Physiol. 2017;44(2):153–61.
Bae K-M, Dai Y, Vieweg J, Siemann DW. Hypoxia regulates SOX2 expression to promote prostate cancer cell invasion and sphere formation. Am J Cancer Res. 2016;6(5):1078.
Hajizadeh F, Okoye I, Esmaily M, Chaleshtari MG, Masjedi A, Azizi G, et al. Hypoxia inducible factors in the tumor microenvironment as therapeutic targets of cancer stem cells. Life Sci. 2019;237:116952.
Johansson E, Grassi ES, Pantazopoulou V, Tong B, Lindgren D, Berg TJ, et al. CD44 interacts with HIF-2α to modulate the hypoxic phenotype of perinecrotic and perivascular glioma cells. Cell Rep. 2017;20(7):1641–53. https://doi.org/10.1016/j.celrep.2017.07.049.
Markiewicz A, Welnicka-Jaskiewicz M, Seroczynska B, Skokowski J, Majewska H, Szade J, et al. Epithelial-mesenchymal transition markers in lymph node metastases and primary breast tumors - relation to dissemination and proliferation. Am J Transl Res. 2014;6(6):793–808.
Markiewicz A, Ahrends T, Welnicka-Jaskiewicz M, Seroczynska B, Skokowski J, Jaskiewicz J, et al. Expression of epithelial to mesenchymal transition-related markers in lymph node metastases as a surrogate for primary tumor metastatic potential in breast cancer. J Transl Med. 2012;10:226. https://doi.org/10.1186/1479-5876-10-226.
Jing Y, Han Z, Zhang S, Liu Y, Wei L. Epithelial-mesenchymal transition in tumor microenvironment. Cell Biosci. 2011;1:29. https://doi.org/10.1186/2045-3701-1-29.
Floor S, van Staveren WC, Larsimont D, Dumont JE, Maenhaut C. Cancer cells in epithelial-to-mesenchymal transition and tumor-propagating-cancer stem cells: distinct, overlapping or same populations. Oncogene. 2011;30(46):4609–21. https://doi.org/10.1038/onc.2011.184.
Bao B, Azmi AS, Ali S, Ahmad A, Li Y, Banerjee S, et al. The biological kinship of hypoxia with CSC and EMT and their relationship with deregulated expression of miRNAs and tumor aggressiveness. Biochim Biophys Acta. 2012;1826(2):272–96. https://doi.org/10.1016/j.bbcan.2012.04.008.
Akbar MW, Isbilen M, Belder N, Canli SD, Kucukkaraduman B, Turk C, et al. A stemness and EMT based gene expression signature identifies phenotypic plasticity and is A predictive but not prognostic biomarker for breast cancer. J Cancer. 2020;11(4):949.
Kulshreshtha R, Ferracin M, Wojcik SE, Garzon R, Alder H, Agosto-Perez FJ, et al. A microRNA signature of hypoxia. Mol Cell Biol. 2007;27(5):1859–67.
Cascio S, D’Andrea A, Ferla R, Surmacz E, Gulotta E, Amodeo V, et al. miR-20b modulates VEGF expression by targeting HIF‐1α and STAT3 in MCF‐7 breast cancer cells. J Cell Physiol. 2010;224(1):242–9.
Liu M, Wang D, Li N. MicroRNA-20b downregulates HIF-1α and Inhibits the proliferation and invasion of osteosarcoma cells. Oncol Res Featur Preclin Clin Cancer Ther. 2016;23(5):257–66.
Wu Q, Yang Z, Wang F, Hu S, Yang L, Shi Y, et al. MiR-19b/20a/92a regulates the self-renewal and proliferation of gastric cancer stem cells. J Cell Sci. 2013;126(18):4220–9.
Shao Q, Xu J, Guan X, Zhou B, Wei W, Deng R, et al. In vitro and in vivo effects of miRNA-19b/20a/92a on gastric cancer stem cells and the related mechanism. Int J Med Sci. 2018;15(1):86.
Volinia S, Calin GA, Liu C-G, Ambs S, Cimmino A, Petrocca F, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci. 2006;103(7):2257–61.
Hua Z, Lv Q, Ye W, Wong CKA, Cai G, Gu D, et al. MiRNA-directed regulation of VEGF and other angiogenic factors under hypoxia. PLoS ONE. 2006;1(1):e116.
Moriyama T, Ohuchida K, Mizumoto K, Yu J, Sato N, Nabae T, et al. MicroRNA-21 modulates biological functions of pancreatic cancer cells including their proliferation, invasion, and chemoresistance. Mol Cancer Ther. 2009;8(5):1067–74. https://doi.org/10.1158/1535-7163.mct-08-0592.
Kadera BE, Li L, Toste PA, Wu N, Adams C, Dawson DW, et al. MicroRNA-21 in pancreatic ductal adenocarcinoma tumor-associated fibroblasts promotes metastasis. PLoS ONE. 2013;8(8):e71978. https://doi.org/10.1371/journal.pone.0071978.
Anwar SL, Sari DNI, Kartika AI, Fitria MS, Tanjung DS, Rakhmina D, et al. Upregulation of circulating MiR-21 expression as a potential biomarker for therapeutic monitoring and clinical outcome in breast cancer. Asian Pac J Cancer Prev. 2019;20(4):1223–8.
Liu B, Su F, Chen M, Li Y, Qi X, Xiao J, et al. Serum miR-21 and miR-125b as markers predicting neoadjuvant chemotherapy response and prognosis in stage II/III breast cancer. Human Pathol. 2017;64:44–52.
Jiraskova L, Ryska A. Are ENT1/ENT1, NOTCH3, and miR-21 reliable prognostic biomarkers in patients with resected pancreatic adenocarcinoma treated with adjuvant gemcitabine monotherapy? Cancers. 2019. https://doi.org/10.3390/cancers11111621.
Tu H-F, Lin S-C, Chang K-W. MicroRNA aberrances in head and neck cancer: pathogenetic and clinical significance. Curr Opin Otolaryngol Head Neck Surg. 2013;21(2):104–11.
Mamoori A, Gopalan V, Smith RA, Lam AKY. Modulatory roles of microRNAs in the regulation of different signalling pathways in large bowel cancer stem cells. Biol Cell. 2016;108(3):51–64.
Nedaeinia R, Sharifi M, Avan A, Kazemi M, Rafiee L, Ghayour-Mobarhan M, et al. Locked nucleic acid anti-miR-21 inhibits cell growth and invasive behaviors of a colorectal adenocarcinoma cell line: LNA-anti-miR as a novel approach. Cancer Gene Ther. 2016;23(8):246–53. https://doi.org/10.1038/cgt.2016.25.
Nedaeinia R, Sharifi M, Avan A, Kazemi M, Nabinejad A, Ferns GA, et al. Inhibition of microRNA-21 via locked nucleic acid-anti-miR suppressed metastatic features of colorectal cancer cells through modulation of programmed cell death 4. Tumor Biol. 2017;39(3):1010428317692261. https://doi.org/10.1177/1010428317692261.
Zhang Z, Li Z, Gao C, Chen P, Chen J, Liu W, et al. miR-21 plays a pivotal role in gastric cancer pathogenesis and progression. Lab Investig. 2008;88(12):1358–66.
Nedaeinia R, Manian M, Jazayeri MH, Ranjbar M, Salehi R, Sharifi M, et al. Circulating exosomes and exosomal microRNAs as biomarkers in gastrointestinal cancer. Cancer Gene Ther. 2017;24(2):48–56. https://doi.org/10.1038/cgt.2016.77.
Ali S, Ahmad A, Banerjee S, Padhye S, Dominiak K, Schaffert JM, et al. Gemcitabine sensitivity can be induced in pancreatic cancer cells through modulation of miR-200 and miR-21 expression by curcumin or its analogue CDF. Cancer Res. 2010;70(9):3606–17. https://doi.org/10.1158/0008-5472.can-09-4598.
Liu L-Z, Li C, Chen Q, Jing Y, Carpenter R, Jiang Y, et al. MiR-21 induced angiogenesis through AKT and ERK activation and HIF-1α expression. PLoS ONE. 2011;6(4):e19139.
Bao B, Ali S, Ahmad A, Azmi AS, Li Y, Banerjee S, et al. Hypoxia-induced aggressiveness of pancreatic cancer cells is due to increased expression of VEGF, IL-6 and miR-21, which can be attenuated by CDF treatment. PLoS ONE. 2012;7(12):e50165.
Jiao X, Qian X, Wu L, Li B, Wang Y, Kong X, et al. microRNA: the impact on cancer stemness and therapeutic resistance. Cells. 2020;9(1):8.
Javanmard SH, Vaseghi G, Ghasemi A, Rafiee L, Ferns GA, Esfahani HN, et al. Therapeutic inhibition of microRNA-21 (miR-21) using locked-nucleic acid (LNA)-anti-miR and its effects on the biological behaviors of melanoma cancer cells in preclinical studies. Cancer Cell Int. 2020;20(1):384. https://doi.org/10.1186/s12935-020-01394-6.
Li J, Zhang Y, Zhao J, Kong F, Chen Y. Overexpression of miR-22 reverses paclitaxel-induced chemoresistance through activation of PTEN signaling in p53-mutated colon cancer cells. Mol Cell Biochem. 2011;357(1–2):31–8.
Zhang J, Yang Y, Yang T, Liu Y, Li A, Fu S, et al. microRNA-22, downregulated in hepatocellular carcinoma and correlated with prognosis, suppresses cell proliferation and tumourigenicity. Br J Cancer. 2010;103(8):1215–20.
Li J, Liang S, Yu H, Zhang J, Ma D, Lu X. An inhibitory effect of miR-22 on cell migration and invasion in ovarian cancer. Gynecol Oncol. 2010;119(3):543–8.
Nakamura M, Hayashi M, Konishi H, Nunode M, Ashihara K, Sasaki H, et al. MicroRNA–22 enhances radiosensitivity in cervical cancer cell lines via direct inhibition of c–Myc binding protein, and the subsequent reduction in hTERT expression. Oncol Lett. 2020;19(3):2213–22.
Song SJ, Poliseno L, Song MS, Ala U, Webster K, Ng C, et al. MicroRNA-antagonism regulates breast cancer stemness and metastasis via TET-family-dependent chromatin remodeling. Cell. 2013;154(2):311–24.
Song SJ, Pandolfi PP. miR-22 in tumorigenesis. Cell Cycle (Georgetown Tex). 2014;13(1):11–2.
Tsuchiya N, Izumiya M, Ogata-Kawata H, Okamoto K, Fujiwara Y, Nakai M, et al. Tumor suppressor miR-22 determines p53-dependent cellular fate through post-transcriptional regulation of p21. Cancer Res. 2011;71(13):4628–39.
Bao B, Li Y, Ahmad A, Azmi S, Bao A, Ali G, et al. Targeting CSC-related miRNAs for cancer therapy by natural agents. Curr Drug Targets. 2012;13(14):1858–68.
Bao B, Ali S, Banerjee S, Wang Z, Logna F, Azmi AS, et al. Curcumin analogue CDF inhibits pancreatic tumor growth by switching on suppressor microRNAs and attenuating EZH2 expression. Cancer Res. 2012;72(1):335–45.
Cao P, Deng Z, Wan M, Huang W, Cramer SD, Xu J, et al. MicroRNA-101 negatively regulates Ezh2 and its expression is modulated by androgen receptor and HIF-1α/HIF-1β. Mol Cancer. 2010;9(1):108.
Zhang J-g, Guo J-F, Liu D-L, Liu Q, Wang J-J. MicroRNA-101 exerts tumor-suppressive functions in non-small cell lung cancer through directly targeting enhancer of zeste homolog 2. J Thorac Oncol. 2011;6(4):671–8.
Sparmann A, van Lohuizen M. Polycomb silencers control cell fate, development and cancer. Nat Rev Cancer. 2006;6(11):846–56.
Zhao G, Wei Z, Guo Y. MicroRNA-107 is a novel tumor suppressor targeting POU3F2 in melanoma. Biol Res. 2020;53(1):1–10.
Datta J, Smith A, Lang JC, Islam M, Dutt D, Teknos TN, et al. microRNA-107 functions as a candidate tumor-suppressor gene in head and neck squamous cell carcinoma by downregulation of protein kinase Cɛ. Oncogene. 2012;31(36):4045–53.
Yamakuchi M, Lotterman CD, Bao C, Hruban RH, Karim B, Mendell JT, et al. P53-induced microRNA-107 inhibits HIF-1 and tumor angiogenesis. Proc Natl Acad Sci. 2010;107(14):6334–9.
Chen H, Chen Q, Fang M, Mi Y. microRNA-181b targets MLK2 in HL-60 cells. Sci China Life Sci. 2010;53(1):101–6.
Wang B, Hsu S-H, Majumder S, Kutay H, Huang W, Jacob ST, et al. TGFβ-mediated upregulation of hepatic miR-181b promotes hepatocarcinogenesis by targeting TIMP3. Oncogene. 2010;29(12):1787–97.
Wang X, Meng Q, Qiao W, Ma R, Ju W, Hu J, et al. miR-181b/Notch2 overcome chemoresistance by regulating cancer stem cell-like properties in NSCLC. Stem Cell Res Ther. 2018;9(1):327.
Shi L, Cheng Z, Zhang J, Li R, Zhao P, Fu Z, et al. hsa-mir-181a and hsa-mir-181b function as tumor suppressors in human glioma cells. Brain Res. 2008;1236:185–93.
Liu W, Cai T, Li L, Chen H, Chen R, Zhang M, et al. MiR-200a regulates nasopharyngeal carcinoma cell migration and invasion by targeting MYH10. J Cancer. 2020;11(10):3052.
Cong N, Du P, Zhang A, Shen F, Su J, Pu P, et al. Downregulated microRNA-200a promotes EMT and tumor growth through the wnt/β-catenin pathway by targeting the E-cadherin repressors ZEB1/ZEB2 in gastric adenocarcinoma. Oncol Rep. 2013;29(4):1579–87.
Burk U, Schubert J, Wellner U, Schmalhofer O, Vincan E, Spaderna S, et al. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008;9(6):582–9.
Shimono Y, Zabala M, Cho RW, Lobo N, Dalerba P, Qian D, et al. Downregulation of miRNA-200c links breast cancer stem cells with normal stem cells. Cell. 2009;138(3):592–603.
Tang T, Yang Z, Zhu Q, Wu Y, Sun K, Alahdal M, et al. Up-regulation of miR-210 induced by a hypoxic microenvironment promotes breast cancer stem cell metastasis, proliferation, and self-renewal by targeting E-cadherin. FASEB J. 2018;32(12):6965–81.
Camps C, Buffa FM, Colella S, Moore J, Sotiriou C, Sheldon H, et al. hsa-miR-210 Is induced by hypoxia and is an independent prognostic factor in breast cancer. Clinical Cancer Res. 2008;14(5):1340–8.
Kulshreshtha R, Davuluri R, Calin GA, Ivan M. A microRNA component of the hypoxic response. Cell Death Differ. 2008;15(4):667–71.
Crosby ME, Kulshreshtha R, Ivan M, Glazer PM. MicroRNA regulation of DNA repair gene expression in hypoxic stress. Cancer Res. 2009;69(3):1221–9.
Huang Q, Gumireddy K, Schrier M, Le Sage C, Nagel R, Nair S, et al. The microRNAs miR-373 and miR-520c promote tumour invasion and metastasis. Nat Cell Biol. 2008;10(2):202–10.
Wang LQ, Yu P, Li B, Guo YH, Liang ZR, Zheng LL, et al. miR-372 and miR‐373 enhance the stemness of colorectal cancer cells by repressing differentiation signaling pathways. Mol Oncol. 2018;12(11):1949–64.
Place RF, Li L-C, Pookot D, Noonan EJ, Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc Natl Acad Sci. 2008;105(5):1608–13.
Berx G, Van Roy F. The E-cadherin/catenin complex: an important gatekeeper in breast cancer tumorigenesis and malignant progression. Breast Cancer Res. 2001;3(5):289.
Chang C-J, Hsu C-C, Chang C-H, Tsai L-L, Chang Y-C, Lu S-W, et al. Let-7d functions as novel regulator of epithelial-mesenchymal transition and chemoresistant property in oral cancer. Oncol Rep. 2011;26(4):1003–10.
Kong D, Banerjee S, Ahmad A, Li Y, Wang Z, Sethi S, et al. Epithelial to mesenchymal transition is mechanistically linked with stem cell signatures in prostate cancer cells. PLoS ONE. 2010;5(8):e12445.
Li Y, VandenBoom TG, Kong D, Wang Z, Ali S, Philip PA, et al. Up-regulation of miR-200 and let-7 by natural agents leads to the reversal of epithelial-to-mesenchymal transition in gemcitabine-resistant pancreatic cancer cells. Cancer Res. 2009;69(16):6704–12.
Sun X, Xu C, Xiao G, Meng J, Wang J, Tang SC, et al. Breast cancer stem-like cells are sensitized to tamoxifen induction of self-renewal inhibition with enforced Let-7c dependent on Wnt blocking. Int J Mol Med. 2018;41(4):1967–75.
Kong D, Heath E, Chen W, Cher ML, Powell I, Heilbrun L, et al. Loss of let-7 up-regulates EZH2 in prostate cancer consistent with the acquisition of cancer stem cell signatures that are attenuated by BR-DIM. PloS ONE. 2012;7(3):e33729.
Lu J, He M-L, Wang L, Chen Y, Liu X, Dong Q, et al. MiR-26a inhibits cell growth and tumorigenesis of nasopharyngeal carcinoma through repression of EZH2. Cancer Res. 2011;71(1):225–33.
Li G, Liu H, Zhang X, Liu X, Zhang G, Liu Q. The protective effects of microRNA-26a in steroid-induced osteonecrosis of the femoral head by repressing EZH2. . Cell Cycle (GeorgetownTex). 2020;19(5):551–66.
Ma D-N, Chai Z-T, Zhu X-D, Zhang N, Zhan D-H, Ye B-G, et al. MicroRNA-26a suppresses epithelial-mesenchymal transition in human hepatocellular carcinoma by repressing enhancer of zeste homolog 2. J Hematol Oncol. 2016;9(1):1.
Peng X, Kang Q, Wan R, Wang Z. MiR-26a/HOXC9 dysregulation promotes metastasis and stem cell-like phenotype of gastric cancer. Cell Physiol Biochem. 2018;49(4):1659–76.
Holmquist-Mengelbier L, Fredlund E, Lofstedt T, Noguera R, Navarro S, Nilsson H, et al. Recruitment of HIF-1alpha and HIF-2alpha to common target genes is differentially regulated in neuroblastoma: HIF-2alpha promotes an aggressive phenotype. Cancer Cell. 2006;10(5):413–23. https://doi.org/10.1016/j.ccr.2006.08.026.
Stoeltzing O, Liu W, Reinmuth N, Fan F, Parikh AA, Bucana CD, et al. Regulation of hypoxia-inducible factor-1alpha, vascular endothelial growth factor, and angiogenesis by an insulin-like growth factor-I receptor autocrine loop in human pancreatic cancer. Am J Pathol. 2003;163(3):1001–11. https://doi.org/10.1016/s0002-9440(10)63460-8.
Gonzalez-Moreno O, Lecanda J, Green JE, Segura V, Catena R, Serrano D, et al. VEGF elicits epithelial-mesenchymal transition (EMT) in prostate intraepithelial neoplasia (PIN)-like cells via an autocrine loop. Exp Cell Res. 2010;316(4):554–67. https://doi.org/10.1016/j.yexcr.2009.11.020.
Yi ZY, Feng LJ, Xiang Z, Yao H. Vascular endothelial growth factor receptor-1 activation mediates epithelial to mesenchymal transition in hepatocellular carcinoma cells. J Investig Surg. 2011;24(2):67–76. https://doi.org/10.3109/08941939.2010.542272.
Peixoto J, Lima J. Metabolic traits of cancer stem cells. Dis Model Mech. 2018. https://doi.org/10.1242/dmm.033464.
Sun H, Wang S, Yan S, Zhang Y, Nelson PJ, Jia H, et al. Therapeutic strategies targeting cancer stem cells and their microenvironment. Front Oncol. 2019;9:1104.
Chiche J, Brahimi-Horn MC, Pouysségur J. Tumour hypoxia induces a metabolic shift causing acidosis: a common feature in cancer. J Cell Mol Med. 2010;14(4):771–94.
Chiche J, Ilc K, Laferrière J, Trottier E, Dayan F, Mazure NM, et al. Hypoxia-inducible carbonic anhydrase IX and XII promote tumor cell growth by counteracting acidosis through the regulation of the intracellular pH. Cancer Res. 2009;69(1):358–68. https://doi.org/10.1158/0008-5472.can-08-2470.
Boussadia Z, Lamberti J, Mattei F, Pizzi E, Puglisi R, Zanetti C, et al. Acidic microenvironment plays a key role in human melanoma progression through a sustained exosome mediated transfer of clinically relevant metastatic molecules. J Exp Clin Cancer Res. 2018;37(1):245. https://doi.org/10.1186/s13046-018-0915-z.
Najafi M, Farhood B, Mortezaee K, Kharazinejad E, Majidpoor J, Ahadi R. Hypoxia in solid tumors: a key promoter of cancer stem cell (CSC) resistance. J Cancer Res Clin Oncol. 2020;146(1):19–31.
Shiraishi A, Tachi K, Essid N, Tsuboi I, Nagano M, Kato T, et al. Hypoxia promotes the phenotypic change of aldehyde dehydrogenase activity of breast cancer stem cells. Cancer Sci. 2017;108(3):362–72.
Kim R-J, Park J-R, Roh K-J, Choi A-R, Kim S-R, Kim P-H, et al. High aldehyde dehydrogenase activity enhances stem cell features in breast cancer cells by activating hypoxia-inducible factor-2α. Cancer Lett. 2013;333(1):18–31.
McDonald PC, Chafe SC, Dedhar S. Overcoming hypoxia-mediated tumor progression: combinatorial approaches targeting pH regulation, angiogenesis and immune dfysfunction. Front Cell Dev Biol. 2016;4:27. https://doi.org/10.3389/fcell.2016.00027.
Ullah MS, Davies AJ, Halestrap AP. The plasma membrane lactate transporter MCT4, but not MCT1, is up-regulated by hypoxia through a HIF-1alpha-dependent mechanism. J Biol Chem. 2006;281(14):9030–7. https://doi.org/10.1074/jbc.M511397200.
Cho IJ, Lui PP, Obajdin J, Riccio F, Stroukov W, Willis TL, et al. Mechanisms, hallmarks, and implications of stem cell quiescence. Stem Cell Rep. 2019;12(6):1190–200.
Clarke MF, Dick JE, Dirks PB, Eaves CJ, Jamieson CH, Jones DL, et al. Cancer stem cells–perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer Res. 2006;66(19):9339–44. https://doi.org/10.1158/0008-5472.can-06-3126.
Carcereri de Prati A, Butturini E, Rigo A, Oppici E, Rossin M, Boriero D, et al. Metastatic breast cancer cells enter into dormant state and express cancer stem cells phenotype under chronic hypoxia. J Cell Biochem. 2017;118(10):3237–48. https://doi.org/10.1002/jcb.25972.
Goda N, Ryan HE, Khadivi B, McNulty W, Rickert RC, Johnson RS. Hypoxia-inducible factor 1alpha is essential for cell cycle arrest during hypoxia. Mol Cell Biol. 2003;23(1):359–69. https://doi.org/10.1128/mcb.23.1.359-369.2003.
Hammer S, To KK, Yoo YG, Koshiji M, Huang LE. Hypoxic suppression of the cell cycle gene CDC25A in tumor cells. Cell Cycle (Georgetown Tex). 2007;6(15):1919–26. https://doi.org/10.4161/cc.6.15.4515.
Gardner LB, Li Q, Park MS, Flanagan WM, Semenza GL, Dang CV. Hypoxia inhibits G1/S transition through regulation of p27 expression. J Biol Chem. 2001;276(11):7919–26. https://doi.org/10.1074/jbc.M010189200.
Ishii A, Kimura T, Sadahiro H, Kawano H, Takubo K, Suzuki M, et al. Histological characterization of the tumorigenic “Peri-Necrotic Niche” harboring quiescent stem-like tumor cells in glioblastoma. PLoS ONE. 2016;11(1):e0147366. https://doi.org/10.1371/journal.pone.0147366.
Koshiji M, Kageyama Y, Pete EA, Horikawa I, Barrett JC, Huang LE. HIF-1alpha induces cell cycle arrest by functionally counteracting Myc. EMBO J. 2004;23(9):1949–56. https://doi.org/10.1038/sj.emboj.7600196.
Krishnamurthy P, Ross DD, Nakanishi T, Bailey-Dell K, Zhou S, Mercer KE, et al. The stem cell marker Bcrp/ABCG2 enhances hypoxic cell survival through interactions with heme. J Biol Chem. 2004;279(23):24218–25. https://doi.org/10.1074/jbc.M313599200.
Moitra K, Lou H, Dean M. Multidrug efflux pumps and cancer stem cells: insights into multidrug resistance and therapeutic development. Clin Pharmacol Ther. 2011;89(4):491–502. https://doi.org/10.1038/clpt.2011.14.
Samanta D, Gilkes DM, Chaturvedi P, Xiang L, Semenza GL. Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cells. Proc Natl Acad Sci USA. 2014;111(50):E5429-38. https://doi.org/10.1073/pnas.1421438111.
Burger H, van Tol H, Boersma AW, Brok M, Wiemer EA, Stoter G, et al. Imatinib mesylate (STI571) is a substrate for the breast cancer resistance protein (BCRP)/ABCG2 drug pump. Blood. 2004;104(9):2940–2. https://doi.org/10.1182/blood-2004-04-1398.
Schöning JP, Monteiro M, Gu W. Drug resistance and cancer stem cells: the shared but distinct roles of hypoxia-inducible factors HIF1α and HIF2α. Clin Exp Pharmacol Physiol. 2017;44(2):153–61. https://doi.org/10.1111/1440-1681.12693.
Le QT, Shi G, Cao H, Nelson DW, Wang Y, Chen EY, et al. Galectin-1: a link between tumor hypoxia and tumor immune privilege. J Clin Oncol. 2005;23(35):8932–41. https://doi.org/10.1200/jco.2005.02.0206.
Czekay R-P, Aertgeerts K, Curriden SA, Loskutoff DJ. Plasminogen activator inhibitor-1 detaches cells from extracellular matrices by inactivating integrins. J Cell Biol. 2003;160(5):781–91.
Murphy-Ullrich JE. The de-adhesive activity of matricellular proteins: is intermediate cell adhesion an adaptive state? J Clin Invest. 2001;107(7):785–90. https://doi.org/10.1172/jci12609.
Foekens JA, Peters HA, Look MP, Portengen H, Schmitt M, Kramer MD, et al. The urokinase system of plasminogen activation and prognosis in 2780 breast cancer patients. Cancer Res. 2000;60(3):636–43.
Andreasen P, Egelund R, Petersen H. The plasminogen activation system in tumor growth, invasion, and metastasis. Cell Mol Life Sci CMLS. 2000;57(1):25–40.
Hanahan D, Christofori G, Naik P, Arbeit J. Transgenic mouse models of tumour angiogenesis: the angiogenic switch, its molecular controls, and prospects for preclinical therapeutic models. Eur J Cancer. 1996;32A(14):2386–93. https://doi.org/10.1016/s0959-8049(96)00401-7.
Goonewardene TI, Sowter HM, Harris AL. Hypoxia-induced pathways in breast cancer. Microsc Res Tech. 2002;59(1):41–8. https://doi.org/10.1002/jemt.10175.
Schietke R, Warnecke C, Wacker I, Schodel J, Mole DR, Campean V, et al. The lysyl oxidases LOX and LOXL2 are necessary and sufficient to repress E-cadherin in hypoxia: insights into cellular transformation processes mediated by HIF-1. J Biol Chem. 2010;285(9):6658–69. https://doi.org/10.1074/jbc.M109.042424.
Erler JT, Bennewith KL, Nicolau M, Dornhofer N, Kong C, Le QT, et al. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature. 2006;440(7088):1222–6. https://doi.org/10.1038/nature04695.
Tian J, Sun HX, Li YC, Jiang L, Zhang SL, Hao Q. LOXL 2 promotes the epithelial-mesenchymal transition and malignant progression of cervical cancer. OncoTargets Ther. 2019;12:8947–54. https://doi.org/10.2147/ott.s217794.
Wong CCL, Gilkes DM, Zhang H, Chen J, Wei H, Chaturvedi P, et al. Hypoxia-inducible factor 1 is a master regulator of breast cancer metastatic niche formation. Proc Natl Acad Sci. 2011;108(39):16369–74.
Krishnamachary B, Zagzag D, Nagasawa H, Rainey K, Okuyama H, Baek JH, et al. Hypoxia-inducible factor-1-dependent repression of E-cadherin in von Hippel-Lindau tumor suppressor-null renal cell carcinoma mediated by TCF3, ZFHX1A, and ZFHX1B. Cancer Res. 2006;66(5):2725–31. https://doi.org/10.1158/0008-5472.can-05-3719.
Kang N, Choi SY, Kim BN, Yeo CD, Park CK, KimKim YK, et al. Hypoxia attenuates the expression of E-cadherin via up-regulation of SNAIL in ovarian carcinoma cells. Am J Pathol. 2003;163(4):1437–47. https://doi.org/10.1016/s0002-9440(10)63501-8.
Kang N, Choi SY, Kim BN, Yeo CD, Park CK, Kim YK et al. Hypoxia-induced cancer stemness acquisition is associated with CXCR4 activation by its aberrant promoter demethylation. BMC Cancer. 2019;19(1):148. https://doi.org/10.1186/s12885-019-5360-7.
Fiaschi T, Marini A, Giannoni E, Taddei ML, Gandellini P, De Donatis A, et al. Reciprocal metabolic reprogramming through lactate shuttle coordinately influences tumor-stroma interplay. Cancer Res. 2012;72(19):5130–40. https://doi.org/10.1158/0008-5472.can-12-1949.
Zeng L, Morinibu A, Kobayashi M, Zhu Y, Wang X, Goto Y, et al. Aberrant IDH3alpha expression promotes malignant tumor growth by inducing HIF-1-mediated metabolic reprogramming and angiogenesis. Oncogene. 2015;34(36):4758–66. https://doi.org/10.1038/onc.2014.411.
Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16(9):582–98. https://doi.org/10.1038/nrc.2016.73.
Hielscher A, Qiu C, Porterfield J, Smith Q, Gerecht S. Hypoxia affects the structure of breast cancer cell-derived matrix to support angiogenic responses of endothelial cCells. J Carcinogenesis Mutagenesis. 2013. https://doi.org/10.4172/2157-2518.s13-005.
Kai AK, Chan LK, Lo RC, Lee JM, Wong CC, Wong JC, et al. Down-regulation of TIMP2 by HIF-1alpha/miR-210/HIF-3alpha regulatory feedback circuit enhances cancer metastasis in hepatocellular carcinoma. Hepatology. 2016;64(2):473–87. https://doi.org/10.1002/hep.28577.
Colpaert CG, Vermeulen PB, Fox SB, Harris AL, Dirix LY, Van Marck EA. The presence of a fibrotic focus in invasive breast carcinoma correlates with the expression of carbonic anhydrase IX and is a marker of hypoxia and poor prognosis. Breast Cancer Res Treat. 2003;81(2):137–47. https://doi.org/10.1023/a:1025702330207.
Sitkovsky M, Lukashev D. Regulation of immune cells by local-tissue oxygen tension: HIF1α and adenosine receptors. Nat Rev Immunol. 2005;5(9):712.
Chiu DK, Xu IM, Lai RK, Tse AP, Wei LL, Koh HY, et al. Hypoxia induces myeloid-derived suppressor cell recruitment to hepatocellular carcinoma through chemokine (C-C motif) ligand 26. Hepatology. 2016;64(3):797–813. https://doi.org/10.1002/hep.28655.
Chiu DK-C, Tse AP-W, Xu IM-J, Di Cui J, Lai RK-H, Li LL, et al. Hypoxia inducible factor HIF-1 promotes myeloid-derived suppressor cells accumulation through ENTPD2/CD39L1 in hepatocellular carcinoma. Nat Commun. 2017;8(1):517.
Corzo CA, Condamine T, Lu L, Cotter MJ, Youn J-I, Cheng P, et al. HIF-1α regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med. 2010;207(11):2439–53.
Noman MZ, Janji B, Hu S, Wu JC, Martelli F, Bronte V, et al. Tumor-promoting effects of myeloid-derived suppressor cells are potentiated by hypoxia-induced expression of miR-210. Cancer Res. 2015;75(18):3771–87.
Pastuła A, Marcinkiewicz J. Myeloid-derived suppressor cells: a double‐edged sword? Int J Exp Pathol. 2011;92(2):73–8.
Liu G, Bi Y, Shen B, Yang H, Zhang Y, Wang X, et al. SIRT1 limits the function and fate of myeloid-derived suppressor cells in tumors by orchestrating HIF-1α–dependent glycolysis. Cancer Res. 2014;74(3):727–37.
Andrea C, Damya L, Mathias W, Rizzolio S, Nicklas B, Marco M, et al. Impeding macrophage entry into hypoxic tumor areas by Sema3A/Nrp1 signaling blockade inhibits angiogenesis and restores antitumor immunity. Cancer Cell. 2013;24:695–709.
Matschurat S, Knies UE, Person V, Fink L, Stoelcker B, Ebenebe C, et al. Regulation of EMAP II by hypoxia. Am J Pathol. 2003;162(1):93–103.
Murdoch C, Giannoudis A, Lewis CE. Mechanisms regulating the recruitment of macrophages into hypoxic areas of tumors and other ischemic tissues. Blood. 2004;104(8):2224–34.
Colegio OR, Chu N-Q, Szabo AL, Chu T, Rhebergen AM, Jairam V, et al. Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature. 2014;513(7519):559.
Doedens AL, Stockmann C, Rubinstein MP, Liao D, Zhang N, DeNardo DG, et al. Macrophage expression of hypoxia-inducible factor-1α suppresses T-cell function and promotes tumor progression. Cancer Res. 2010;70(19):7465–75.
Imtiyaz HZ, Williams EP, Hickey MM, Patel SA, Durham AC, Yuan L-J, et al. Hypoxia-inducible factor 2α regulates macrophage function in mouse models of acute and tumor inflammation. J Clin Invest. 2010;120(8):2699–714.
Sagiv JY, Michaeli J, Assi S, Mishalian I, Kisos H, Levy L, et al. Phenotypic diversity and plasticity in circulating neutrophil subpopulations in cancer. Cell Rep. 2015;10(4):562–73. https://doi.org/10.1016/j.celrep.2014.12.039.
Triner D, Shah YM. Hypoxic regulation of neutrophils in cancer. Int J Mol Sci. 2019;20(17):4189.
Campbell EL, Bruyninckx WJ, Kelly CJ, Glover LE, McNamee EN, Bowers BE, et al. Transmigrating neutrophils shape the mucosal microenvironment through localized oxygen depletion to influence resolution of inflammation. Immunity. 2014;40(1):66–77. https://doi.org/10.1016/j.immuni.2013.11.020.
Xu L, Xie K, Mukaida N, Matsushima K, Fidler IJ. Hypoxia-induced elevation in interleukin-8 expression by human ovarian carcinoma cells. Cancer Res. 1999;59(22):5822–9.
Blaisdell A, Crequer A, Columbus D, Daikoku T, Mittal K, Dey SK, et al. Neutrophils oppose uterine epithelial carcinogenesis via debridement of hypoxic tumor cells. Cancer Cell. 2015;28(6):785–99. https://doi.org/10.1016/j.ccell.2015.11.005.
Kong T, Eltzschig HK, Karhausen J, Colgan SP, Shelley CS. Leukocyte adhesion during hypoxia is mediated by HIF-1-dependent induction of beta2 integrin gene expression. Proc Natl Acad Sci USA. 2004;101(28):10440–5. https://doi.org/10.1073/pnas.0401339101.
Triner D, Xue X, Schwartz AJ, Jung I, Colacino JA, Shah YM. Epithelial hypoxia-inducible factor 2alpha facilitates the progression of colon tumors through recruiting neutrophils. Mol Cell Biol. 2017. https://doi.org/10.1128/mcb.00481-16.
Tohme S, Yazdani HO, Al-Khafaji AB, Chidi AP, Loughran P, Mowen K, et al. Neutrophil extracellular traps promote the development and progression of liver metastases after surgical stress. Cancer Res. 2016;76(6):1367–80.
Jung HS, Gu J, Kim J-E, Nam Y, Song JW, Kim HK. Cancer cell–induced neutrophil extracellular traps promote both hypercoagulability and cancer progression. PLoS ONE. 2019;14(4):e0216055.
Snoderly HT, Boone BA, Bennewitz MF. Neutrophil extracellular traps in breast cancer and beyond: current perspectives on NET stimuli, thrombosis and metastasis, and clinical utility for diagnosis and treatment. Breast Cancer Res. 2019;21(1):145. https://doi.org/10.1186/s13058-019-1237-6.
Tohme S, Yazdani HO, Al-Khafaji AB, Chidi AP, Loughran P, Mowen K, et al. Neutrophil extracellular traps promote the development and progression of liver metastases after surgical stress. Cancer Res. 2016;76(6):1367–80. https://doi.org/10.1158/0008-5472.can-15-1591.
Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell. 2009;16(3):183–94. https://doi.org/10.1016/j.ccr.2009.06.017.
Chang C-H, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD, et al. Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell. 2015;162(6):1229–41.
Very N, Steenackers A, Dubuquoy C, Vermuse J, Dubuquoy L, Lefebvre T, et al. Cross regulation between mTOR signaling and O-GlcNAcylation. J Bioenerg Biomembr. 2018;50(3):213–22. https://doi.org/10.1007/s10863-018-9747-y.
Zhang Y, Kurupati R, Liu L, Zhou XY, Zhang G, Hudaihed A, et al. Enhancing CD8(+) T cell fatty acid catabolism within a metabolically challenging tumor microenvironment increases the efficacy of melanoma immunotherapy. Cancer Cell. 2017;32(3):377-91.e9. https://doi.org/10.1016/j.ccell.2017.08.004.
Laplagne C, Domagala M, Le Naour A, Quemerais C, Hamel D, Fournié J-J, et al. Latest advances in targeting the tumor microenvironment for tumor suppression. Int J Mol Sci. 2019;20(19):4719.
Paluskievicz CM, Cao X, Abdi R, Zheng P, Liu Y, Bromberg JS. T regulatory cells and priming the suppressive tumor microenvironment. Front Immunol. 2019;10:2453. https://doi.org/10.3389/fimmu.2019.02453.
Ren L, Yu Y, Wang L, Zhu Z, Lu R, Yao Z. Hypoxia-induced CCL28 promotes recruitment of regulatory T cells and tumor growth in liver cancer. Oncotarget. 2016;7(46):75763–73. https://doi.org/10.18632/oncotarget.12409.
Facciabene A, Peng X, Hagemann IS, Balint K, Barchetti A, Wang LP, et al. Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature. 2011;475(7355):226–30. https://doi.org/10.1038/nature10169.
Hansen W, Hutzler M, Abel S, Alter C, Stockmann C, Kliche S, et al. Neuropilin 1 deficiency on CD4 + Foxp3 + regulatory T cells impairs mouse melanoma growth. J Exp Med. 2012;209(11):2001–16. https://doi.org/10.1084/jem.20111497.
Hagar A, Wang Z, Koyama S, Serrano JA, Melo L, Vargas S, et al. Endurance training slows breast tumor growth in mice by suppressing Treg cells recruitment to tumors. BMC Cancer. 2019;19(1):536. https://doi.org/10.1186/s12885-019-5745-7.
Clambey ET, McNamee EN, Westrich JA, Glover LE, Campbell EL, Jedlicka P, et al. Hypoxia-inducible factor-1 alpha-dependent induction of FoxP3 drives regulatory T-cell abundance and function during inflammatory hypoxia of the mucosa. Proc Natl Acad Sci USA. 2012;109(41):E2784-93. https://doi.org/10.1073/pnas.1202366109.
Karhausen J, Haase VH, Colgan SP. Inflammatory hypoxia: role of hypoxia-inducible factor. Cell Cycle (Georgetown Tex). 2005;4(2):256–8.
Hsu TS, Lai MZ. Hypoxia-inducible factor 1alpha plays a predominantly negative role in regulatory T cell functions. J Leukoc Biol. 2018;104(5):911–8. https://doi.org/10.1002/jlb.mr1217-481r.
Hsiao H-W, Hsu T-S, Liu W-H, Hsieh W-C, Chou T-F, Wu Y-J, et al. Deltex1 antagonizes HIF-1α and sustains the stability of regulatory T cells in vivo. Nat Commun. 2015;6:6353.
Noman MZ, Desantis G, Janji B, Hasmim M, Karray S, Dessen P, et al. PD-L1 is a novel direct target of HIF-1alpha, and its blockade under hypoxia enhanced MDSC-mediated T cell activation. J Exp Med. 2014;211(5):781–90. https://doi.org/10.1084/jem.20131916.
Ruf M, Moch H, Schraml P. PD-L1 expression is regulated by hypoxia inducible factor in clear cell renal cell carcinoma. Int J Cancer. 2016;139(2):396–403. https://doi.org/10.1002/ijc.30077.
Pinato DJ, Black JR, Trousil S, Dina RE, Trivedi P, Mauri FA, et al. Programmed cell death ligands expression in phaeochromocytomas and paragangliomas: Relationship with the hypoxic response, immune evasion and malignant behavior. Oncoimmunology. 2017;6(11):e1358332. https://doi.org/10.1080/2162402x.2017.1358332.
Messai Y, Gad S, Noman MZ, Le Teuff G, Couve S, Janji B, et al. Renal cell carcinoma programmed death-ligand 1, a new direct target of hypoxia-inducible factor-2 alpha, is regulated by von Hippel–Lindau gene mutation status. Eur Urol. 2016;70(4):623–32.
Palazon A, Tyrakis PA, Macias D, Velica P, Rundqvist H, Fitzpatrick S, et al. An HIF-1alpha/VEGF-A axis in cytotoxic T cells regulates tumor progression. Cancer Cell. 2017;32(5):669-83.e5. https://doi.org/10.1016/j.ccell.2017.10.003.
Topalian SL, Taube JM, Anders RA, Pardoll DM. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer. 2016;16(5):275–87. https://doi.org/10.1038/nrc.2016.36.
Doedens AL, Phan AT, Stradner MH, Fujimoto JK, Nguyen JV, Yang E, et al. Hypoxia-inducible factors enhance the effector responses of CD8(+) T cells to persistent antigen. Nat Immunol. 2013;14(11):1173–82. https://doi.org/10.1038/ni.2714.
Mohapatra SR, Sadik A, Tykocinski LO, Dietze J, Poschet G, Heiland I, et al. Hypoxia inducible factor 1alpha inhibits the expression of immunosuppressive tryptophan-2,3-dioxygenase in glioblastoma. Front Immunol. 2019;10:2762. https://doi.org/10.3389/fimmu.2019.02762.
Tyrakis PA, Palazon A, Macias D, Lee KL, Phan AT, Velica P, et al. S-2-hydroxyglutarate regulates CD8(+) T-lymphocyte fate. Nature. 2016;540(7632):236–41. https://doi.org/10.1038/nature20165.
Gropper Y, Feferman T, Shalit T, Salame TM, Porat Z, Shakhar G. Culturing CTLs under hypoxic conditions enhances their cytolysis and improves their anti-tumor function. Cell Rep. 2017;20(11):2547–55. https://doi.org/10.1016/j.celrep.2017.08.071.
Barsoum IB, Hamilton TK, Li X, Cotechini T, Miles EA, Siemens DR, et al. Hypoxia induces escape from innate immunity in cancer cells via increased expression of ADAM10: role of nitric oxide. Cancer Res. 2011;71(24):7433–41. https://doi.org/10.1158/0008-5472.can-11-2104.
Graham C, Barsoum I, Kim J, Black M, Siemens RD. Mechanisms of hypoxia-induced immune escape in cancer and their regulation by nitric oxide. Redox Biol. 2015;5:417. https://doi.org/10.1016/j.redox.2015.09.022.
Coulibaly A, Bettendorf A, Kostina E, Figueiredo AS, Velasquez SY, Bock HG, et al. Interleukin-15 signaling in HIF-1alpha regulation in natural killer cells, insights through mathematical models. Front immunol. 2019;10:2401. https://doi.org/10.3389/fimmu.2019.02401.
Velásquez SY, Killian D, Schulte J, Sticht C, Thiel M, Lindner HA. Short term hypoxia synergizes with interleukin 15 priming in driving glycolytic gene transcription and supports human natural killer cell activities. J Biol Chem. 2016;291(25):12960–77.
Maddika S, Ande SR, Panigrahi S, Paranjothy T, Weglarczyk K, Zuse A, et al. Cell survival, cell death and cell cycle pathways are interconnected: implications for cancer therapy. Drug Resist Updates. 2007;10(1–2):13–29.
Rohwer N, Cramer T. Hypoxia-mediated drug resistance: novel insights on the functional interaction of HIFs and cell death pathways. Drug Resist Updates. 2011;14(3):191–201.
Li HS, Zhou YN, Li L, Li SF, Long D, Chen XL, et al. HIF-1alpha protects against oxidative stress by directly targeting mitochondria. Redox Biol. 2019;25:101109. https://doi.org/10.1016/j.redox.2019.101109.
Hao J, Song X, Song B, Liu Y, Wei L, Wang X, et al. Effects of lentivirus-mediated HIF-1alpha knockdown on hypoxia-related cisplatin resistance and their dependence on p53 status in fibrosarcoma cells. Cancer Gene Ther. 2008;15(7):449–55. https://doi.org/10.1038/cgt.2008.4.
Rohwer N, Dame C, Haugstetter A, Wiedenmann B, Detjen K, Schmitt CA, et al. Hypoxia-inducible factor 1alpha determines gastric cancer chemosensitivity via modulation of p53 and NF-kappaB. PLoS ONE. 2010;5(8):e12038. https://doi.org/10.1371/journal.pone.0012038.
Vaupel P, Kelleher DK, Höckel M, editors. Oxygenation status of malignant tumors: pathogenesis of hypoxia and significance for tumor therapy. Seminars in oncology. New York: Elsevier; 2001.
Comerford KM, Wallace TJ, Karhausen J, Louis NA, Montalto MC, Colgan SP. Hypoxia-inducible factor-1-dependent regulation of the multidrug resistance (MDR1) gene. Cancer Res. 2002;62(12):3387–94.
Muz B, Kusdono HD, Azab F, de la Puente P, Federico C, Fiala M, et al. Tariquidar sensitizes multiple myeloma cells to proteasome inhibitors via reduction of hypoxia-induced P-gp-mediated drug resistance. Leukemia Lymphoma. 2017;58(12):2916–25. https://doi.org/10.1080/10428194.2017.1319052.
Abraham J, Salama NN, Azab AK. The role of P-glycoprotein in drug resistance in multiple myeloma. Leukemia Lymphoma. 2015;56(1):26–33. https://doi.org/10.3109/10428194.2014.907890.
Vaupel P, Mayer A, Höckel M. Tumor hypoxia and malignant progression. Methods in enzymology. New York: Elsevier; 2004. p. 335–54.
Maroufi NF, Amiri M, Dizaji BF, Vahedian V, Akbarzadeh M, Roshanravan N, et al. Inhibitory effect of melatonin on hypoxia-induced vasculogenic mimicry via suppressing epithelial-mesenchymal transition (EMT) in breast cancer stem cells. Eur J Pharmacol. 2020;881:173282. https://doi.org/10.1016/j.ejphar.2020.173282.
Saint-Martin A, Martinez-Rios J, Castaneda-Patlan MC, Sarabia-Sanchez MA, Tejeda-Munoz N. Functional interaction of hypoxia-inducible factor 2-alpha and autophagy mediates drug resistance in colon cancer cells. Cancers. 2019. https://doi.org/10.3390/cancers11060755.
Bertout JA, Majmundar AJ, Gordan JD, Lam JC, Ditsworth D, Keith B, et al. HIF2alpha inhibition promotes p53 pathway activity, tumor cell death, and radiation responses. Proc Natl Acad Sci USA. 2009;106(34):14391–6. https://doi.org/10.1073/pnas.0907357106.
Baran N, Konopleva M. Molecular pathways: hypoxia-activated prodrugs in cancer therapy. Clin Cancer Res. 2017;23(10):2382–90. https://doi.org/10.1158/1078-0432.ccr-16-0895.
Graham K, Unger E. Overcoming tumor hypoxia as a barrier to radiotherapy, chemotherapy and immunotherapy in cancer treatment. Int J Nanomed. 2018;13:6049.
Borad MJ, Reddy SG, Bahary N, Uronis HE, Sigal D, Cohn AL, et al. Randomized phase II trial of gemcitabine plus TH-302 versus gemcitabine in patients with advanced pancreatic cancer. J Clin Oncol. 2015;33(13):1475–81. https://doi.org/10.1200/jco.2014.55.7504.
Chawla SP, Cranmer LD, Van Tine BA, Reed DR, Okuno SH, Butrynski JE, et al. Phase II study of the safety and antitumor activity of the hypoxia-activated prodrug TH-302 in combination with doxorubicin in patients with advanced soft tissue sarcoma. J Clin Oncol. 2014;32(29):3299–306. https://doi.org/10.1200/jco.2013.54.3660.
Jayaprakash P, Ai M, Liu A, Budhani P, Bartkowiak T, Sheng J, et al. Targeted hypoxia reduction restores T cell infiltration and sensitizes prostate cancer to immunotherapy. J Clin Invest. 2018;128(11):5137–49. https://doi.org/10.1172/jci96268.
Onnis B, Rapisarda A, Melillo G. Development of HIF-1 inhibitors for cancer therapy. J Cell Mol Med. 2009;13(9a):2780–6. https://doi.org/10.1111/j.1582-4934.2009.00876.x.
Mossenta M, Busato D, Baboci L, Cintio FD, Toffoli G, Bo MD. New insight into therapies targeting angiogenesis in hepatocellular carcinoma. Cancers. 2019. https://doi.org/10.3390/cancers11081086.
Oliner J, Min H, Leal J, Yu D, Rao S, You E, et al. Suppression of angiogenesis and tumor growth by selective inhibition of angiopoietin-2. Cancer Cell. 2004;6(5):507–16. https://doi.org/10.1016/j.ccr.2004.09.030.
Coxon A, Bready J, Min H, Kaufman S, Leal J, Yu D, et al. Context-dependent role of angiopoietin-1 inhibition in the suppression of angiogenesis and tumor growth: implications for AMG 386, an angiopoietin-1/2-neutralizing peptibody. Mol Cancer Ther. 2010;9(10):2641–51. https://doi.org/10.1158/1535-7163.mct-10-0213.
Abdel-Mohsen HT, Abdullaziz MA, Kerdawy AME, Ragab FAF, Flanagan KJ, Mahmoud AEE, et al. Targeting receptor tyrosine kinase VEGFR-2 in hepatocellular cancer: rational design, synthesis and biological evaluation of 1,2-disubstituted benzimidazoles. Molecules. 2020. https://doi.org/10.3390/molecules25040770.
Wilson WR, Hay MP. Targeting hypoxia in cancer therapy. Nat Rev Cancer. 2011;11(6):393.
McIntyre A, Harris AL. Metabolic and hypoxic adaptation to anti-angiogenic therapy: a target for induced essentiality. EMBO Mol Med. 2015;7(4):368–79. https://doi.org/10.15252/emmm.201404271.
Molls M, Anscher MS, Nieder C, Vaupel P. The impact of tumor biology on cancer treatment and multidisciplinary strategies. Berlin: Springer; 2009.
Becker HM. Carbonic anhydrase IX and acid transport in cancer. Br J Cancer. 2020;122(2):157–67. https://doi.org/10.1038/s41416-019-0642-z.
Le Floch R, Chiche J, Marchiq I, Naiken T, Ilc K, Murray CM, et al. CD147 subunit of lactate/H + symporters MCT1 and hypoxia-inducible MCT4 is critical for energetics and growth of glycolytic tumors. Proc Natl Acad Sci USA. 2011;108(40):16663–8. https://doi.org/10.1073/pnas.1106123108.
Reshkin SJ, Cardone RA, Harguindey S. Na+-H + exchanger, pH regulation and cancer. Recent Patents Anti Cancer Drug Discov. 2013;8(1):85–99. https://doi.org/10.2174/15748928130108.
Schwab A, Stock C. Ion channels and transporters in tumour cell migration and invasion. Philos Trans R Soc Lond Ser B Biol Sci. 2014;369(1638):20130102. https://doi.org/10.1098/rstb.2013.0102.
Litan A, Langhans SA. Cancer as a channelopathy: ion channels and pumps in tumor development and progression. Front Cell Neurosci. 2015;9:86. https://doi.org/10.3389/fncel.2015.00086.
Lang F, Stournaras C. Ion channels in cancer: future perspectives and clinical potential. Philos Trans R Soc Lond Ser B Biol Sci. 2014;369(1638):20130108. https://doi.org/10.1098/rstb.2013.0108.
Di Sario A, Bendia E, Omenetti A, De Minicis S, Marzioni M, Kleemann HW, et al. Selective inhibition of ion transport mechanisms regulating intracellular pH reduces proliferation and induces apoptosis in cholangiocarcinoma cells. Digest Liver Dis. 2007;39(1):60–9. https://doi.org/10.1016/j.dld.2006.07.013.
Letai AG. Diagnosing and exploiting cancer’s addiction to blocks in apoptosis. Nat Rev Cancer. 2008;8(2):121–32. https://doi.org/10.1038/nrc2297.
Tamtaji OR, Mirzaei H. New trends in glioma cancer therapy: targeting Na(+) /H (+) exchangers. J Cell Physiol. 2020;235(2):658–65. https://doi.org/10.1002/jcp.29014.
Harguindey S, Polo Orozco J, Alfarouk KO, Devesa J. Hydrogen ion dynamics of cancer and a new molecular, biochemical and metabolic approach to the etiopathogenesis and treatment of brain malignancies. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20174278.
Lee Y-Y, Jeon H-K, Hong JE, Cho YJ, Ryu JY, Choi J-J, et al. Proton pump inhibitors enhance the effects of cytotoxic agents in chemoresistant epithelial ovarian carcinoma. Oncotarget. 2015;6(33):35040.
Lomelino C, McKenna R. Carbonic anhydrase inhibitors: a review on the progress of patent literature (2011–2016). Expert Opin Ther Pat. 2016;26(8):947–56. https://doi.org/10.1080/13543776.2016.1203904.
Ledaki I, McIntyre A, Wigfield S, Buffa F, McGowan S, Baban D, et al. Carbonic anhydrase IX induction defines a heterogeneous cancer cell response to hypoxia and mediates stem cell-like properties and sensitivity to HDAC inhibition. Oncotarget. 2015;6(23):19413–27. https://doi.org/10.18632/oncotarget.4989.
Lock FE, McDonald PC, Lou Y, Serrano I, Chafe SC, Ostlund C, et al. Targeting carbonic anhydrase IX depletes breast cancer stem cells within the hypoxic niche. Oncogene. 2013;32(44):5210–9. https://doi.org/10.1038/onc.2012.550.
Webb BA, Chimenti M, Jacobson MP, Barber DL. Dysregulated pH: a perfect storm for cancer progression. Nat Rev Cancer. 2011;11(9):671–7. https://doi.org/10.1038/nrc3110.
Lacroix R, Rozeman EA, Kreutz M, Renner K, Blank CU. Targeting tumor-associated acidity in cancer immunotherapy. Cancer immunol Immunother CII. 2018;67(9):1331–48. https://doi.org/10.1007/s00262-018-2195-z.
Sukumar M, Liu J, Ji Y, Subramanian M, Crompton JG, Yu Z, et al. Inhibiting glycolytic metabolism enhances CD8 + T cell memory and antitumor function. J Clin Investig. 2013;123(10):4479–88.
Bosticardo M, Ariotti S, Losana G, Bernabei P, Forni G, Novelli F. Biased activation of human T lymphocytes due to low extracellular pH is antagonized by B7/CD28 costimulation. Eur J Immunol. 2001;31(9):2829–38.
Huber V, Camisaschi C, Berzi A, Ferro S, Lugini L, Triulzi T, et al editors. Cancer acidity: An ultimate frontier of tumor immune escape and a novel target of immunomodulation. Seminars in cancer biology. Berlin: Elsevier; 2017.
Pilon-Thomas S, Kodumudi KN, El-Kenawi AE, Russell S, Weber AM, Luddy K, et al. Neutralization of tumor acidity improves antitumor responses to immunotherapy. Cancer Res. 2016;76(6):1381–90. https://doi.org/10.1158/0008-5472.can-15-1743.
Shen YA, Pan SC, Chu I, Lai RY, Wei YH. Targeting cancer stem cells from a metabolic perspective. Exp Biol Med. 2020;245(5):465–76. https://doi.org/10.1177/1535370220909309.
Mast JM, Kuppusamy P. Hyperoxygenation as a therapeutic supplement for treatment of triple negative breast cancer. Front Oncol. 2018;8:527. https://doi.org/10.3389/fonc.2018.00527.
Teicher BA. Hypoxia and drug resistance. Cancer Metastasis Rev. 1994;13(2):139–68. https://doi.org/10.1007/bf00689633.
Durand RE. Keynote address: the influence of microenvironmental factors on the activity of radiation and drugs. Int J Radiat Oncol Biol Phys. 1991;20(2):253–8. https://doi.org/10.1016/0360-3016(91)90100-i.
Trédan O, Galmarini CM, Patel K, Tannock IF. Drug resistance and the solid tumor microenvironment. J Natl Cancer Inst. 2007;99(19):1441–54. https://doi.org/10.1093/jnci/djm135.
Minassian LM, Cotechini T, Huitema E, Graham CH. Hypoxia-induced resistance to chemotherapy in cancer. Adv Exp Med Biol. 2019;1136:123–39. https://doi.org/10.1007/978-3-030-12734-3_9.
Pawlik TM, Keyomarsi K. Role of cell cycle in mediating sensitivity to radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59(4):928–42. https://doi.org/10.1016/j.ijrobp.2004.03.005.
Horsman MR, Vaupel P. Pathophysiological basis for the formation of the tumor microenvironment. Front Oncol. 2016;6:66.
Wu HM, Jiang ZF, Ding PS, Shao LJ, Liu RY. Hypoxia-induced autophagy mediates cisplatin resistance in lung cancer cells. Sci Rep. 2015;5:12291. https://doi.org/10.1038/srep12291.
Lee JG, Shin JH, Shim HS, Lee CY, Kim DJ, Kim YS, et al. Autophagy contributes to the chemo-resistance of non-small cell lung cancer in hypoxic conditions. Respir Res. 2015;16:138. https://doi.org/10.1186/s12931-015-0285-4.
Fletcher GH. Radiation and drug resistance of breast cancer. Am J Clin Oncol. 1984;7(6):617–24.
Al Tameemi W, Dale TP, Al-Jumaily RMK, Forsyth NR. Hypoxia-modified cancer cell metabolism. Front Cell Dev Biol. 2019;7:4.
Wan M, Ning B, Spiegel S, Lyon CJ, Hu TY. Tumor-derived exosomes (TDEs): how to avoid the sting in the tail. Med Res Rev. 2020;40(1):385–412. https://doi.org/10.1002/med.21623.
Kumar A, Deep G. Hypoxia in tumor microenvironment regulates exosome biogenesis: molecular mechanisms and translational opportunities. Cancer Lett. 2020;479:23–30. https://doi.org/10.1016/j.canlet.2020.03.017.
Patton MC, Zubair H, Khan MA, Singh S, Singh AP. Hypoxia alters the release and size distribution of extracellular vesicles in pancreatic cancer cells to support their adaptive survival. J Cell Biochem. 2020;121(1):828–39. https://doi.org/10.1002/jcb.29328.
Govaert KM, Emmink BL, Nijkamp MW, Cheung ZJ, Steller EJ, Fatrai S, et al. Hypoxia after liver surgery imposes an aggressive cancer stem cell phenotype on residual tumor cells. Ann Surg. 2014;259(4):750–9. https://doi.org/10.1097/SLA.0b013e318295c160.
Calabrese C, Poppleton H, Kocak M, Hogg TL, Fuller C, Hamner B, et al. A perivascular niche for brain tumor stem cells. Cancer Cell. 2007;11(1):69–82. https://doi.org/10.1016/j.ccr.2006.11.020.
Burkhardt JK, Hofstetter CP, Santillan A, Shin BJ, Foley CP, Ballon DJ, et al. Orthotopic glioblastoma stem-like cell xenograft model in mice to evaluate intra-arterial delivery of bevacizumab: from bedside to bench. J Clin Neurosci. 2012;19(11):1568–72. https://doi.org/10.1016/j.jocn.2012.03.012.
Folkins C, Man S, Xu P, Shaked Y, Hicklin DJ, Kerbel RS. Anticancer therapies combining antiangiogenic and tumor cell cytotoxic effects reduce the tumor stem-like cell fraction in glioma xenograft tumors. Cancer Res. 2007;67(8):3560–4. https://doi.org/10.1158/0008-5472.can-06-4238.
Cui B, Luo Y, Tian P, Peng F, Lu J, Yang Y, et al. Stress-induced epinephrine enhances lactate dehydrogenase A and promotes breast cancer stem-like cells. J Clin Invest. 2019;129(3):1030–46. https://doi.org/10.1172/jci121685.
De Francesco EM, Bonuccelli G, Maggiolini M, Sotgia F, Lisanti MP. Vitamin C and doxycycline: a synthetic lethal combination therapy targeting metabolic flexibility in cancer stem cells (CSCs). Oncotarget. 2017;8(40):67269–86. https://doi.org/10.18632/oncotarget.18428.
Mao P, Joshi K, Li J, Kim SH, Li P, Santana-Santos L, et al. Mesenchymal glioma stem cells are maintained by activated glycolytic metabolism involving aldehyde dehydrogenase 1A3. Proc Natl Acad Sci USA. 2013;110(21):8644–9. https://doi.org/10.1073/pnas.1221478110.
Zhou Y, Zhou Y, Shingu T, Feng L, Chen Z, Ogasawara M, et al. Metabolic alterations in highly tumorigenic glioblastoma cells: preference for hypoxia and high dependency on glycolysis. J Biol Chem. 2011;286(37):32843–53. https://doi.org/10.1074/jbc.M111.260935.
Michelakis ED, Sutendra G, Dromparis P, Webster L, Haromy A, Niven E, et al. Metabolic modulation of glioblastoma with dichloroacetate. Sci Transl Med. 2010;2(31):31ra4. https://doi.org/10.1126/scitranslmed.3000677.
Tataranni T, Piccoli C. Dichloroacetate (DCA) and cancer: an overview towards clinical applications. Oxid Med Cell Longev. 2019. https://doi.org/10.1155/2019/8201079.
Liu C, Zhao G, Liu J, Ma N, Chivukula P, Perelman L, et al. Novel biodegradable lipid nano complex for siRNA delivery significantly improving the chemosensitivity of human colon cancer stem cells to paclitaxel. J Control Release. 2009;140(3):277–83. https://doi.org/10.1016/j.jconrel.2009.08.013.
Deng J, Shao J, Markowitz JS, An G. ABC transporters in multi-drug resistance and ADME-Tox of small molecule tyrosine kinase inhibitors. Pharm Res. 2014;31(9):2237–55. https://doi.org/10.1007/s11095-014-1389-0.
McIntosh K, Balch C, Tiwari AK. Tackling multidrug resistance mediated by efflux transporters in tumor-initiating cells. Expert Opin Drug Metab Toxicol. 2016;12(6):633–44. https://doi.org/10.1080/17425255.2016.1179280.
Qiang L, Wu T, Zhang HW, Lu N, Hu R, Wang YJ, et al. HIF-1α is critical for hypoxia-mediated maintenance of glioblastoma stem cells by activating Notch signaling pathway. Cell Death Differ. 2012;19(2):284–94. https://doi.org/10.1038/cdd.2011.95.
Harrison H, Farnie G, Howell SJ, Rock RE, Stylianou S, Brennan KR, et al. Regulation of breast cancer stem cell activity by signaling through the Notch4 receptor. Cancer Res. 2010;70(2):709–18. https://doi.org/10.1158/0008-5472.can-09-1681.
Zhou L, Wang D, Sheng D, Xu J, Chen W, Qin Y, et al. NOTCH4 maintains quiescent mesenchymal-like breast cancer stem cells via transcriptionally activating SLUG and GAS1 in triple-negative breast cancer. Theranostics. 2020;10(5):2405–21. https://doi.org/10.7150/thno.38875.
Seo EJ, Kim DK, Jang IH, Choi EJ, Shin SH, Lee SI, et al. Hypoxia-NOTCH1-SOX2 signaling is important for maintaining cancer stem cells in ovarian cancer. Oncotarget. 2016;7(34):55624–38. https://doi.org/10.18632/oncotarget.10954.
Yadav AK, Desai NS, Implications T. Cancer stem cells: acquisition, characteristics. Target Strategies Future Prospects. 2019;15(3):331–55. https://doi.org/10.1007/s12015-019-09887-2.
Yan Y, Liu F, Han L, Zhao L, Chen J, Olopade OI, et al. HIF-2α promotes conversion to a stem cell phenotype and induces chemoresistance in breast cancer cells by activating Wnt and Notch pathways. J Exp Clin Cancer Res CR. 2018;37(1):256. https://doi.org/10.1186/s13046-018-0925-x.
Giambra V, Jenkins CE, Lam SH, Hoofd C, Belmonte M, Wang X, et al. Leukemia stem cells in T-ALL require active Hif1α and Wnt signaling. Blood. 2015;125(25):3917–27. https://doi.org/10.1182/blood-2014-10-609370.
Zhang X, Lou Y, Zheng X, Wang H, Sun J, Dong Q, et al. Wnt blockers inhibit the proliferation of lung cancer stem cells. Drug Des Devel Ther. 2015;9:2399–407. https://doi.org/10.2147/dddt.s76602.
Wen Z, Feng S, Wei L, Wang Z, Hong D, Wang Q. Evodiamine, a novel inhibitor of the Wnt pathway, inhibits the self-renewal of gastric cancer stem cells. Int J Mol Med. 2015;36(6):1657–63. https://doi.org/10.3892/ijmm.2015.2383.
Yeh CT, Wu AT, Chang PM, Chen KY, Yang CN, Yang SC, et al. Trifluoperazine, an antipsychotic agent, inhibits cancer stem cell growth and overcomes drug resistance of lung cancer. Am J Respir Crit Care Med. 2012;186(11):1180–8. https://doi.org/10.1164/rccm.201207-1180OC.
Mukherjee S, Mazumdar M, Chakraborty S, Manna A, Saha S, Khan P, et al. Curcumin inhibits breast cancer stem cell migration by amplifying the E-cadherin/β-catenin negative feedback loop. Stem Cell Res Ther. 2014;5(5):116. https://doi.org/10.1186/scrt506.
Shukla S, Sinha S, Khan S, Kumar S, Singh K, Mitra K, et al. Cucurbitacin B inhibits the stemness and metastatic abilities of NSCLC via downregulation of canonical Wnt/β-catenin signaling axis. Sci Rep. 2016;6:21860. https://doi.org/10.1038/srep21860.
Brechbiel J, Miller-Moslin K, Adjei AA. Crosstalk between hedgehog and other signaling pathways as a basis for combination therapies in cancer. Cancer Treat Rev. 2014;40(6):750–9. https://doi.org/10.1016/j.ctrv.2014.02.003.
Lu H, Samanta D, Xiang L, Zhang H, Hu H, Chen I, et al. Chemotherapy triggers HIF-1-dependent glutathione synthesis and copper chelation that induces the breast cancer stem cell phenotype. Proc Natl Acad Sci USA. 2015;112(33):E4600-9. https://doi.org/10.1073/pnas.1513433112.
Zhang Z, Han H, Rong Y, Zhu K, Zhu Z, Tang Z, et al. Hypoxia potentiates gemcitabine-induced stemness in pancreatic cancer cells through AKT/Notch1 signaling. J Exp Clin Cancer Res CR. 2018;37(1):291. https://doi.org/10.1186/s13046-018-0972-3.
Liu TZ, Wang X, Bai YF, Liao HZ, Qiu SC, Yang YQ, et al. The HIF-2alpha dependent induction of PAP and adenosine synthesis regulates glioblastoma stem cell function through the A2B adenosine receptor. Int J Biochem Cell Biol. 2014;49:8–16. https://doi.org/10.1016/j.biocel.2014.01.007.
Zhu Y, Liu X, Zhao P, Zhao H, Gao W, Wang L. Celastrol suppresses glioma vasculogenic mimicry formation and angiogenesis by blocking the PI3K/Akt/mTOR signaling pathway. Front Pharmacol. 2020;11:25. https://doi.org/10.3389/fphar.2020.00025.
Marhold M, Tomasich E, El-Gazzar A, Heller G, Spittler A, Horvat R, et al. HIF1α regulates mTOR signaling and viability of prostate cancer stem cells. Mol Cancer Res MCR. 2015;13(3):556–64. https://doi.org/10.1158/1541-7786.mcr-14-0153-t.
Acknowledgements
We would like to express our gratitude to Gordon A. Ferns at Brighton and Sussex Medical School for reviewing and improving the text.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: AEN, BS and MM. Data curation: AEN and SN. Investigation: AR and AS. Methodology: MM, SS and ME. Writing-original draft: AEN. Writing-review and editing: RN, SH and RS. Analysis and/or interpretation of data: MT and MA. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
For this type of study, formal consent is not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Emami Nejad, A., Najafgholian, S., Rostami, A. et al. The role of hypoxia in the tumor microenvironment and development of cancer stem cell: a novel approach to developing treatment. Cancer Cell Int 21, 62 (2021). https://doi.org/10.1186/s12935-020-01719-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-020-01719-5