Abstract
Background
The Global Registry of Acute Coronary Events (GRACE) risk score is widely recommended for risk assessment in patients with acute coronary syndrome (ACS). Chronic hyperglycemia [hemoglobinA1c (HbA1c)] can independently predict major adverse cardiac events (MACEs) in patients with ACS. We investigated whether the prediction of MACEs with the GRACE score could be improved with the addition of HbA1c content in ACS patients without diabetes mellitus (DM) undergoing percutaneous coronary intervention (PCI).
Methods
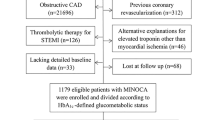
We enrolled 549 ACS patients without DM who underwent PCI. The GRACE score and HbA1c content were determined on admission. Correlation was analyzed by Spearman’s rank correlation. Cumulative MACE curve was calculated using the Kaplan–Meier method. Multivariate Cox regression was used to identify predictors of MACEs. Additionally, the predictive value of HbA1c content alone and combined with GRACE score was estimated by the area under the receiver-operating characteristic curve (AUC), continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI).
Results
During a median of 42.3 months (interquartile range 39.3–44.2 months), 16 (2.9 %) were lost to follow-up, and patients experienced 69 (12.9 %) MACEs: 51 (9.6 %) all-cause deaths and 18 (3.4 %) nonfatal myocardial infarction cases. The GRACE score was positively associated with HbA1c content. Multivariate Cox analysis showed that both GRACE score and HbA1c content were independent predictors of MACEs (hazard ratio 1.030; 95 % CI 1.020–1.040; p < 0.001; 3.530; 95 % CI 1.927–6.466; p < 0.001, respectively). Furthermore, Kaplan–Meier analysis demonstrated increased risk of MACEs with increasing HbA1c content (log-rank 33.906, p < 0.001). Adjustment of the GRACE risk estimate by HbA1c improved the predictive value of the GRACE score [increase in AUC from 0.75 for the GRACE score to 0.80 for the GRACE score plus HbA1c, p = 0.012; IDI = 0.055, p < 0.001; NRI (>0) = 0.70, p < 0.001].
Conclusions
HbA1c content is positively associated with GRACE risk score and their combination further improved the risk stratification for ACS patients without DM undergoing PCI.
Similar content being viewed by others
Background
Patients with acute coronary syndrome (ACS) are diverse in terms of clinical presentation and risk of death or disability. Accurate management decisions with comprehensive evaluation may improve the outcomes of patients at high risk. To identify high-risk patients, current guidelines recommend a standardized approach involving validated scoring systems such as the Global Registry of Acute Coronary Events (GRACE) score [1–3]. Although the GRACE risk score has been validated, the score does not include measurement of important biomarkers. Therefore, whether combining other biomarkers with the GRACE score can provide a more accurate risk estimation in ACS needs to be explored.
Long-term glycometabolic disorder implies high risk for cardiovascular disease [4, 5]. Glycosylated hemoglobin (HbA1c) is a well-known biomarker of long-term glycometabolic state and is minimally affected by stress during ACS. Previous research found elevated HbA1c content related to increased risk of cardiovascular events [6–8].
In the present study, we investigated the predictive value of HbA1c content and GRACE score individually for major adverse cardiac events (MACEs) in patients with ACS but without diabetes mellitus (DM) undergoing PCI and the potential incremental prognostic value of HbA1c content added to GRACE score.
Methods
Study cohort
We performed a single-center, observational study of consecutive non-diabetes patients with ACS performed PCI in the First Affiliated Hospital of Medical College of Xi’an Jiaotong University from December 2010 to December 2011, which included unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation MI (STEMI).
They all performed PCI using standard techniques after Qualitative and quantitative coronary angiographic analyses. All procedural decisions, including device selection and adjunctive pharmacotherapy, were made at the discretion of experienced interventional cardiologists according to 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention [9]. The diagnostic criteria of DM were: HbA1c ≥6.5 %, FPG ≥7.0 mmol/L, 2-h PG ≥11.1 mmol/L according to 2010 ADA Diagnosis and classification of diabetes mellitus [10].
Exclusion criteria were history of DM, treatment with diabetes drugs, HbA1c content ≥6.5 % on admission, no treatment with PCI, advanced liver disease, renal failure, cancer, valvular heart disease, stroke, idiopathic dilated or hypertrophic cardiomyopathy, peripheral arterial disease, pregnancy, receiving anti-inflammatory drugs, acute or chronic infections or autoimmune disease, and blood or thyroid disease.
The study complied with the Declaration of Helsinki and was approved by the ethics committee of the hospital. Written informed consent was obtained from all patients.
Demographic and clinical data
Main demographic data, cardiovascular risk factors and cardiovascular drugs received were obtained from medical records. Current smokers were defined as having smoked more than 100 cigarettes during their lifetime and still smoking in the past 30 days. Hypertension was defined as resting blood pressure ≥140/90 mmHg at two different visits or receiving hypertension drugs. Previous MI was based on a history of acute MI (AMI) or with signs of an infarction outside the area of the index infarction.
Blood samples
Peripheral blood was sampled from patients in a fasting state the morning following the admission day. Venous plasma concentrations of glucose, lipids, lipoproteins, serum creatinine, N-terminal pro-B-type natriuretic peptide (NT-proBNP), white blood cell, platelet count (PLT), Neutrophile count, Monocyte count and HbA1c content (normal values 4–6 %) were determined in the biochemistry department using standard biochemical techniques for the hospital. We calculated estimated glomerular filtration rate as (ml min−1 1.73 m−2) = 194 × (serum creatinine)−1.094 × (age)−0.287(× 0.739 if female).
They all performed Echocardiography for left ventricle function through left ventricle ejection fraction (LVEF).
Calculation of GRACE risk score
The GRACE risk prediction tool was previously described [11]. The score is derived from several variables (age, heart rate, systolic blood pressure, creatinine level, congestive heart failure, in-hospital percutaneous coronary intervention, in-hospital coronary aortic bypass grafting, history of MI, ST-segment depression, and elevated cardiac enzyme/marker levels) and calculated for each patient. The GRACE risk score was originally designed to predict post-discharge 6 month mortality and had been shown to provide good discrimination of mortality up to 4 years after an ischemic event [12–14].
Outcomes and follow-up
All-cause death and nonfatal MI were defined as MACEs. All patients were followed up by interview or telephone in our hospital, and the end of follow-up was the date of the first MACE occurrence obtained by reviewing hospital records. Some patients were followed up until December 2014.
Statistical analysis
Data were analyzed by use of SPSS 19.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as mean ± SD. Categorical variables were expressed as frequency and percentage. The Kolmogorov–Smirnov test was used to assess normal distribution of quantitative variables. Independent samples t test was used to compare two groups, and categorical variables were compared by Chi square test. One-way ANOVA was used to compare multiple groups. To limit the influence of extreme observations, NT-proBNP was natural logarithmically transformed to obtain Ln NT-proBNP. Correlation was analyzed by Spearman’s rank correlation. Univariate and multivariate survival analyses involved Cox regression analysis. To assess the prognostic value of HbA1c content, Kaplan–Meier survival curves were used. Additionally, the incremental predictive value resulting from adding HbA1c variable to GRACE risk score was analyzed in the validation set using several measures of improvement in discrimination: increase in the area under the receiver-operating characteristic (ROC) curve (AUC), as well as integrated discrimination improvement (IDI), and continuous net reclassification improvement (NRI). DeLong’s test was used to compare the AUC from each of models [15], which were analyzed by use of MedCalc Version 11.4.2.0. The IDI was equal to the increase in discrimination slope defined as the mean difference in predicted risks between those with and without events. The continuous NRI was a non-parametric analogue of the IDI and equals twice the difference in probabilities of upward reclassification for events minus for non-events [16], which were analyzed by use of SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
All probability values were two-tailed. P < 0.05 was considered statistically significant.
Results
Baseline characteristics of patients
During a median of 42.3 months (interquartile range 39.3–44.2 months), 16 (2.9 %) were lost to follow-up. In the study, a total of 533 consecutive patients (a mean age of 59.96 ± 12.65 years, 67.7 % man) included 203 unstable angina, 95 NSTEMI and 235 STEMI, the HbA1c content in each type of ACS was respectively 5.588 ± 0.45 %, 5.598 ± 0.51 %, 5.610 ± 0.45 %, in which there was no statistical differences (p = 0.878). Among the 533 patients, 69 (12.9 %) experienced a MACE, including 51 (9.6 %) all-cause deaths and 18 (3.4 %) nonfatal myocardial infarction cases. The event rate of each type of ACS was 9.85 % (20/203), 15.78 % (15/95), 14.46 % (34/235). All patients were segregated into three groups by tertiles of baseline HbA1c content (≤5.4 %, 5.5–5.8 %, 5.9–6.4 %). Baseline characteristics were shown in Additional file 1: Table S1: Patients in the higher HbA1c levels more often had a prior history of PCI, were lower ejection fraction, eGFR level, as well as higher in Monocyte count and LnNT-ProBNP.
Clinical characteristics of patients with and without MACEs
Patients with MACEs were elderly, had more frequent prior history of hypertension, prior history of MI, prior history of PCI and were higher LnNT-ProBNP, PLT, monocyte count, GRACE score and HbA1c content as well as lower ejection fraction compared to patients without MACEs (Table 1). We carried out the correlation analysis between the GRACE risk score and HbA1c levels as continuous variables and showed that GRACE score was positively correlated with HbA1c content (R = 0.192, p < 0.001).
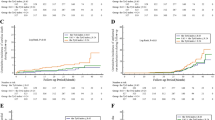
HbA1c content as an independent predictor of MACE occurrence
On univariate Cox analysis, significant predictors of a MACE were age, hypertension, prior MI,prior PCI, LVEF, LnNT-ProBNP, PLT, monocyte count, HbA1c content and GRACE score (Table 2). On multivariate Cox analysis, HbA1c content was a significant and independent predictor of a MACE [hazard ratio (HR) 3.530; 95 % confidence interval (95 % CI) 1.927–6.466; p < 0.001] as was GRACE score (HR 1.030; 95 % CI 1.020–1.0403; p < 0.001) (Table 3). The cumulative risk of a MACE generally increased with elevated HbA1c content by Kaplan–Meier analysis (log-rank 33.906, p < 0.001; Fig. 1).
Effect of HbA1c content and GRACE score combined on MACE occurrence
Since both HbA1c content and GRACE score were independent risk factors of a MACE, we assessed the effect of their combination on predicting long-term risk of MACE occurrence. The AUC increased from 0.75 (95 % CI 0.69–0.82) for GRACE score alone to 0.80 (95 % CI 0.75–0.85) for GRACE score adjustment by HbA1c content (difference in the AUCs, 0.05; z value 2.521, p = 0.012) (Fig. 2). Addition of HbA1c content improved GRACE score alone model discrimination, which was confirmed by the IDI and the continuous, category-free NRI (>0). The IDI for HbA1c content was 0.055 (95 % CI 0.035–0.075, P < 0.001), suggesting further average separation of events from non-events by the HbA1c; the NRI (>0) for HbA1c content was 0.70, (95 % CI 0.47–0.94, P < 0.001), with events contributing 0.42 and non-events 0.28 (Table 4), showing that the HbA1c content led to a significant net reclassification of patients, risk in the appropriate directions.
Discussion
Management decisions in ACS should be based on risk stratification of patients. The GRACE score provides validated prognostic information for MACEs in ACS patients [12, 14]. In accordance with previous research results, the GRACE score could independently predict a MACE in our ACS patients without DM undergoing PCI. However, the AUC with the GRACE score alone was only 0.75, which might be due to some potential risk factors not fully captured by the scoring system. Growing epidemiological evidence supports that HbA1c content in the general population and in patients with and without diabetes is an independent risk factor of cardiovascular events including MI [6, 8, 17]. However, HbA1c content has not been considered with the GRACE scoring system in previous research. In our patients, the GRACE score increased with increasing HbA1c content at baseline, and the 2 variables were correlated. Moreover, the GRACE score adjustment by HbA1c content on admission enhanced the predictive value for ACS patients without DM undergoing PCI (AUC increased from 0.75 for GRACE score alone to 0.80 for GRACE score plus HbA1c).To better assess the improvement in discrimination of GRACE score adjustment by HbA1c variable, we used new statistical metrics [IDI and a category-free, continuous NRI (>0)], and IDI for HbA1c showed further average separation of events from non-events by the HbA1c; Using the a category-free, continuous NRI (>0),we fund that a net 28 % of the patients without events were reclassified into lower risk and that a net 42 % of patients with events were reclassified into higher risk. The category-free, continuous NRI (>0) thus reached an impressive 0.70, which suggested that the HbA1c content led to a significant net reclassification of patients, risk in the appropriate directions.
In the present study, the long-term event rate seems low compared previous researches. It may attribute to followed reasons. Firstly, the enrolled patients were non-DM, which were lower in the cardiovascular events rate than that in patients with diabetic mellitus, especially in the patients of poor nocturnal glycemic control [18]. Secondly, Recent some reports have shown ethnic differences effect the MACE occurrence rate after PCI not only between African Americans and whites [19, 20],but also in Asian subpopulations, such as compared to Indian, Chinese patients have lower Major Adverse Cardiovascular Events [21–23]. In addition, our results was comparable compared with the MACE rate documented by Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study [24, 25].
Although some research had found that higher level of admission glucose predict a worse prognosis including mortality and MI in ACS patients [26–28], recent studies showed that the prediction value of admission glucose was not improved by combining GRACE score [29]. As different from admission glucose, HbA1c is an indicator of general glycometabolic state and is minimally affected by acute stress and also acute glucose management. Increased HbA1c content was not only showed as a indictor of complications including ACS [30] but also a predictor of long-term survival in ACS patients with and without DM [31–33]. Whether the HbA1c content in ACS patients without DM undergoing PCI could be an independent predictor of cardiovascular events is uncertain. In our study, HbA1c content at baseline was higher in patients with than without a MACE, and HbA1c content could independently predict a long-term MACE in ACS patients without DM undergoing PCI. Furthermore, we found that the predictive value on MACE of adding HbA1c on the top of GRACE score system.
Researches have found that C-reactive protein [34], NT-proBNP [35], erythrocyte fatty acids [36], growth differentiation factor-15 [37], cystatin C [38], dikkopf [39], RDW/PDW [40], high-sensitivity troponin [41], mean platelet volume(MPV) [42] and other factors add value to a scoring system for predicting adverse cardiovascular events after ACS. We found that GRACE score and baseline HbA1c content were positively correlated, and their combination improved the predictive value. Whether this combination can improve the outcome of ACS patients with DM needs further comprehensive investigation in clinical practice.
Limitations
The number of patients in the cohort was relatively small. Therefore, these findings need to be verified by multicenter and larger cohort studies. In addition, this study was limited to Chinese subjects, so conclusions for other ethnic groups are cautioned.
Conclusions
HbA1c content measured in ACS patients without DM undergoing PCI could predict a MACE and was positively related with GRACE score. The combination of the two factors may improve on risk stratification of ACS patients without DM undergoing PCI.
Abbreviations
- BMI:
-
body mass index
- Prior MI:
-
prior myocardial infarction
- Prior PCI:
-
prior percutaneous coronary intervention
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- eGFR:
-
estimated glomerular filtration rate
- FBS:
-
fasting blood sugar
- TC:
-
total cholesterol
- TG:
-
triglycerides
- HDL-C:
-
high-density lipoprotein cholesterol
- LDL-C:
-
low-density lipoprotein cholesterol
- Apo-A1:
-
apolipoprotein A1
- Apo-B:
-
apolipoprotein B
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- PLT:
-
platelets
- LVEF:
-
left ventricle ejection fraction
- WBC:
-
white blood cell count
- ACEI:
-
angiotensin-converting enzyme inhibition
- ARB:
-
angiotensin receptor blocker
- ANOVA:
-
one-way analysis of variance
- HbA1c:
-
HemoglobinA1c
- MACEs:
-
major adverse cardiac events
- DM:
-
diabetes mellitus
- ACS:
-
acute coronary syndrome
- AUC:
-
the receiver-operating characteristic curve
- ROC:
-
receiver-operating characteristic
- GRACE:
-
the Global Registry of Acute Coronary Events
- NSTEMI:
-
non-ST-segment elevation myocardial infarction
- STEMI:
-
ST-segment elevation MI
- IDI:
-
integrated discrimination improvement
- NRI:
-
net reclassification improvement
References
Aragam KG, Tamhane UU, Kline-Rogers E, Li J, Fox KA, Goodman SG et al (2009) Does simplicity compromise accuracy in ACS risk prediction? A retrospective analysis of the TIMI and GRACE risk scores. PLoS One 4(11):e7947. doi:10.1371/journal.pone.0007947
Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H et al (2012) ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). G Ital Cardiol (Rome) 13(3):171–228. doi:10.1714/1038.11322
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr et al (2013) 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 127(23):e663–e828. doi:10.1161/CIR.0b013e31828478ac
Kang DO, Seo HS, Choi BG, Lee E, Kim JP, Lee SK et al (2015) Absolute change in fasting plasma glucose over 12 months is associated with 2-year and 5-year major adverse cardiovascular events in patients with drug-eluting stent implants. Int J Cardiol 179:146–152. doi:10.1016/j.ijcard.2014.10.164
Lin B, Koibuchi N, Hasegawa Y, Sueta D, Toyama K, Uekawa K et al (2014) Glycemic control with empagliflozin, a novel selective SGLT2 inhibitor, ameliorates cardiovascular injury and cognitive dysfunction in obese and type 2 diabetic mice. Cardiovasc Diabetol 13(1):148. doi:10.1186/s12933-014-0148-1
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412
Gerstein HC, Pogue J, Mann JF, Lonn E, Dagenais GR, McQueen M et al (2005) The relationship between dysglycaemia and cardiovascular and renal risk in diabetic and non-diabetic participants in the HOPE study: a prospective epidemiological analysis. Diabetologia 48(9):1749–1755. doi:10.1007/s00125-005-1858-4
Corpus RA, O’Neill WW, Dixon SR, Timmis GC, Devlin WH (2003) Relation of hemoglobin A1c to rate of major adverse cardiac events in nondiabetic patients undergoing percutaneous coronary revascularization. Am J Cardiol 92(11):1282–1286
King SB 3rd, Smith SC Jr, Hirshfeld JW Jr, Jacobs AK, Morrison DA, Williams DO et al (2008) 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol 51(2):172–209. doi:10.1016/j.jacc.2007.10.002
(2010) Diagnosis and classification of diabetes mellitus. Diabetes Care. 33(Suppl 1):S62–S69. doi:10.2337/dc10-S062
Fox KA, Dabbous OH, Goldberg RJ, Pieper KS, Eagle KA, Van de Werf F et al (2006) Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 333(7578):1091. doi:10.1136/bmj.38985.646481.55
Tang EW, Wong CK, Herbison P (2007) Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J 153(1):29–35. doi:10.1016/j.ahj.2006.10.004
Ramsay G, Podogrodzka M, McClure C, Fox KA (2007) Risk prediction in patients presenting with suspected cardiac pain: the GRACE and TIMI risk scores versus clinical evaluation. QJM Mon J Assoc Phys 100(1):11–18. doi:10.1093/qjmed/hcl133
Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F et al (2004) A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA 291(22):2727–2733. doi:10.1001/jama.291.22.2727
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 44(3):837–845
Pencina MJ, D’Agostino RB Sr, Steyerberg EW (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30(1):11–21. doi:10.1002/sim.4085
Khaw KT, Wareham N, Luben R, Bingham S, Oakes S, Welch A et al (2001) Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of european prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 322(7277):15–18
Timmer JR, Ottervanger JP, de Boer MJ, Boersma E, Grines CL, Westerhout CM et al (2007) Primary percutaneous coronary intervention compared with fibrinolysis for myocardial infarction in diabetes mellitus: results from the Primary Coronary Angioplasty vs Thrombolysis-2 trial. Arch Intern Med 167(13):1353–1359. doi:10.1001/archinte.167.13.1353
Leborgne L, Cheneau E, Wolfram R, Pinnow EE, Canos DA, Pichard AD et al (2004) Comparison of baseline characteristics and one-year outcomes between African-Americans and Caucasians undergoing percutaneous coronary intervention. Am J Cardiol 93(4):389–393. doi:10.1016/j.amjcard.2003.10.029
Pradhan J, Schreiber TL, Niraj A, Veeranna V, Ramesh K, Saigh L et al (2008) Comparison of five-year outcome in African Americans versus Caucasians following percutaneous coronary intervention. Catheter Cardiovasc Interv 72(1):36–44. doi:10.1002/ccd.21556
Mak KH, Chia KS, Kark JD, Chua T, Tan C, Foong BH et al (2003) Ethnic differences in acute myocardial infarction in Singapore. Eur Heart J 24(2):151–160
Koh AS, Khin LW, Choi LM, Sim LL, Chua TS, Koh TH et al (2011) Percutaneous coronary intervention in Asians–are there differences in clinical outcome? BMC Cardiovasc disord 11:22. doi:10.1186/1471-2261-11-22
Han YL, Zhang L, Yang LX, Liu HL, Qu P, Li WM et al (2012) A new generation of biodegradable polymer-coated sirolimus-eluting stents for the treatment of coronary artery disease: final 5-year clinical outcomes from the CREATE study. EuroIntervention 8(7):815–822. doi:10.4244/EIJV8I7A124
Gao R, Patel A, Gao W, Hu D, Huang D, Kong L et al (2008) Prospective observational study of acute coronary syndromes in China: practice patterns and outcomes. Heart 94(5):554–560. doi:10.1136/hrt.2007.119750
Bi Y, Gao R, Patel A, Su S, Gao W, Hu D et al (2009) Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am Heart J. 157(3):509–516.e1. doi:10.1016/j.ahj.2008.09.026
Ayhan H, Durmaz T, Keles T, Bayram NA, Bilen E, Akcay M et al (2014) The relationship between acute coronary syndrome and stress hyperglycemia. Exp Clin Endocrinol Diabetes 122(4):222–226. doi:10.1055/s-0034-1367002
Yang JH, Song PS, Song YB, Hahn JY, Choi SH, Choi JH et al (2013) Prognostic value of admission blood glucose level in patients with and without diabetes mellitus who sustain ST segment elevation myocardial infarction complicated by cardiogenic shock. Crit Care 17(5):R218. doi:10.1186/cc13035
David RB, Almeida ED, Cruz LV, Sebben JC, Feijo IP, Schmidt KE et al (2014) Diabetes mellitus and glucose as predictors of mortality in primary coronary percutaneous intervention. Arquivos brasileiros de cardiologia
de Mulder M, van der Ploeg T, de Waard GA, Boersma E, Umans VA (2011) Admission glucose does not improve GRACE score at 6 months and 5 years after myocardial infarction. Cardiology. 120(4):227–234. doi:10.1159/000335715
Penno G, Solini A, Zoppini G, Orsi E, Fondelli C, Zerbini G et al (2013) Hemoglobin A1c variability as an independent correlate of cardiovascular disease in patients with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian multicenter study. Cardiovasc Diabetol 12:98. doi:10.1186/1475-2840-12-98
Malmberg K, Norhammar A, Wedel H, Ryden L (1999) Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation 99(20):2626–2632
Gustafsson I, Kistorp CN, James MK, Faber JO, Dickstein K, Hildebrandt PR (2007) Unrecognized glycometabolic disturbance as measured by hemoglobin A1c is associated with a poor outcome after acute myocardial infarction. Am Heart J 154(3):470–476. doi:10.1016/j.ahj.2007.04.057
Tenerz A, Nilsson G, Forberg R, Ohrvik J, Malmberg K, Berne C et al (2003) Basal glucometabolic status has an impact on long-term prognosis following an acute myocardial infarction in non-diabetic patients. J Intern Med 254(5):494–503
Schiele F, Meneveau N, Seronde MF, Chopard R, Descotes-Genon V, Dutheil J et al (2010) C-reactive protein improves risk prediction in patients with acute coronary syndromes. Eur Heart J 31(3):290–297. doi:10.1093/eurheartj/ehp273
Ang DS, Wei L, Kao MP, Lang CC, Struthers AD (2009) A comparison between B-type natriuretic peptide, global registry of acute coronary events (GRACE) score and their combination in ACS risk stratification. Heart 95(22):1836–1842. doi:10.1136/hrt.2008.160234
Harris WS, Kennedy KF, O’Keefe JH Jr, Spertus JA (2013) Red blood cell fatty acid levels improve GRACE score prediction of 2-yr mortality in patients with myocardial infarction. Int J Cardiol 168(1):53–59. doi:10.1016/j.ijcard.2012.09.076
Widera C, Pencina MJ, Meisner A, Kempf T, Bethmann K, Marquardt I et al (2012) Adjustment of the GRACE score by growth differentiation factor 15 enables a more accurate appreciation of risk in non-ST-elevation acute coronary syndrome. Eur Heart J 33(9):1095–1104. doi:10.1093/eurheartj/ehr444
Wang L, Hu XB, Zhang W, Wu LD, Liu YS, Hu B et al (2013) Dickkopf-1 as a novel predictor is associated with risk stratification by GRACE risk scores for predictive value in patients with acute coronary syndrome: a retrospective research. PLoS One 8(1):e54731. doi:10.1371/journal.pone.0054731
Eggers KM, Kempf T, Venge P, Wallentin L, Wollert KC, Lindahl B (2010) Improving long-term risk prediction in patients with acute chest pain: the Global Registry of Acute Coronary Events (GRACE) risk score is enhanced by selected nonnecrosis biomarkers. Am Heart J 160(1):88–94. doi:10.1016/j.ahj.2010.05.002
Timoteo AT, Papoila AL, Lousinha A, Alves M, Miranda F, Ferreira ML et al (2015) Predictive impact on medium term mortality of hematological parameters in Acute Coronary Syndromes: added value on top of GRACE risk score. Eur Heart J Acute Cardiovasc Care. 4(2):172–179. doi:10.1177/2048872614547690
Stahli BE, Yonekawa K, Altwegg LA, Wyss C, Hof D, Fischbacher P et al (2014) Clinical criteria replenish high-sensitive troponin and inflammatory markers in the stratification of patients with suspected acute coronary syndrome. PLoS One 9(6):e98626. doi:10.1371/journal.pone.0098626
Wan ZF, Zhou D, Xue JH, Wu Y, Wang H, Zhao Y et al (2014) Combination of mean platelet volume and the GRACE risk score better predicts future cardiovascular events in patients with acute coronary syndrome. Platelets 25(6):447–451. doi:10.3109/09537104.2013.830708
Authors’ contributions
XJL, ZFW, NZ and ZYY: participated in the study design and performed the data analysis; XJL: wrote the manuscript; ZYY: provided supervision and revised the manuscript; NZ and ZFW: assisted with the editing of the manuscript; YPZ, DZ, ZFW, XHW, LM and XJL: involved in data acquisition, recruited subjects and collected samples. All authors participated in the analytic discussion of the results. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Laura Smales and Yue Wu for critical evaluation of the manuscript. Thank Jie Zheng for checking the data. This work was supported by the National Natural Science Foundation of China (91339116, 81400181), the National Natural Science Fund for Distinguished Young Scholars of China (81025002), and the National Basic Research Program of China (“973 Project” No. 2012CB517804).
Compliance with ethical guidelines
Competing interests The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Table S1. Baseline characteristics of 533 non-diabetes mellitus (DM) patients with acute coronary syndrome (ACS) undergoing Percutaneous Coronary Intervention (PCI) by tertiles of HbA1c content.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, XJ., Wan, ZF., Zhao, N. et al. Adjustment of the GRACE score by HemoglobinA1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol 14, 110 (2015). https://doi.org/10.1186/s12933-015-0274-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-015-0274-4